Sensorized T-Shirt with Intarsia-Knitted Conductive Textile Integrated Interconnections: Performance Assessment of Cardiac Measurements during Daily Living Activities
Abstract
:1. Introduction
2. Materials and Methods
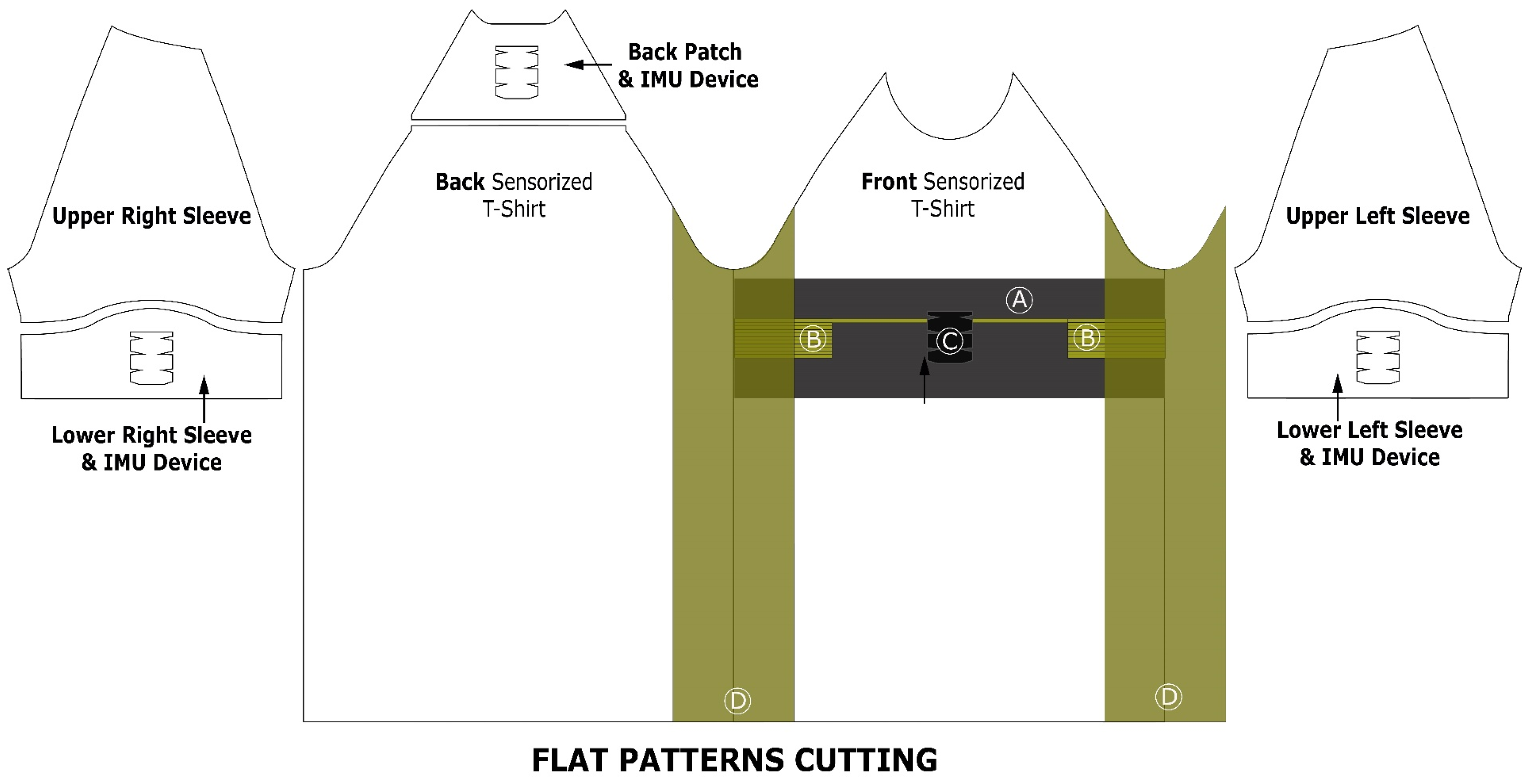
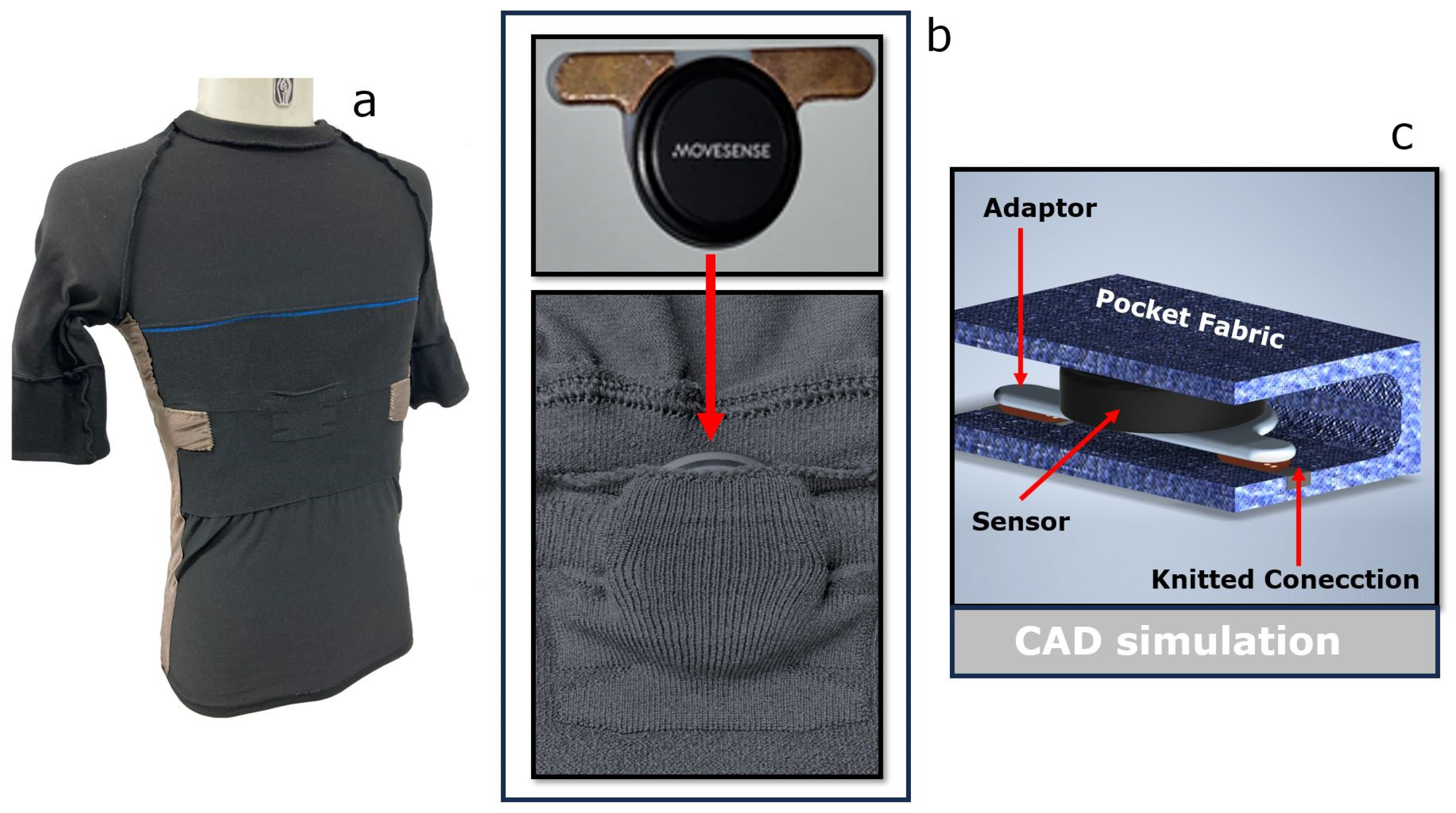
2.1. Sensorized T-Shirt
2.2. Acquisition Device
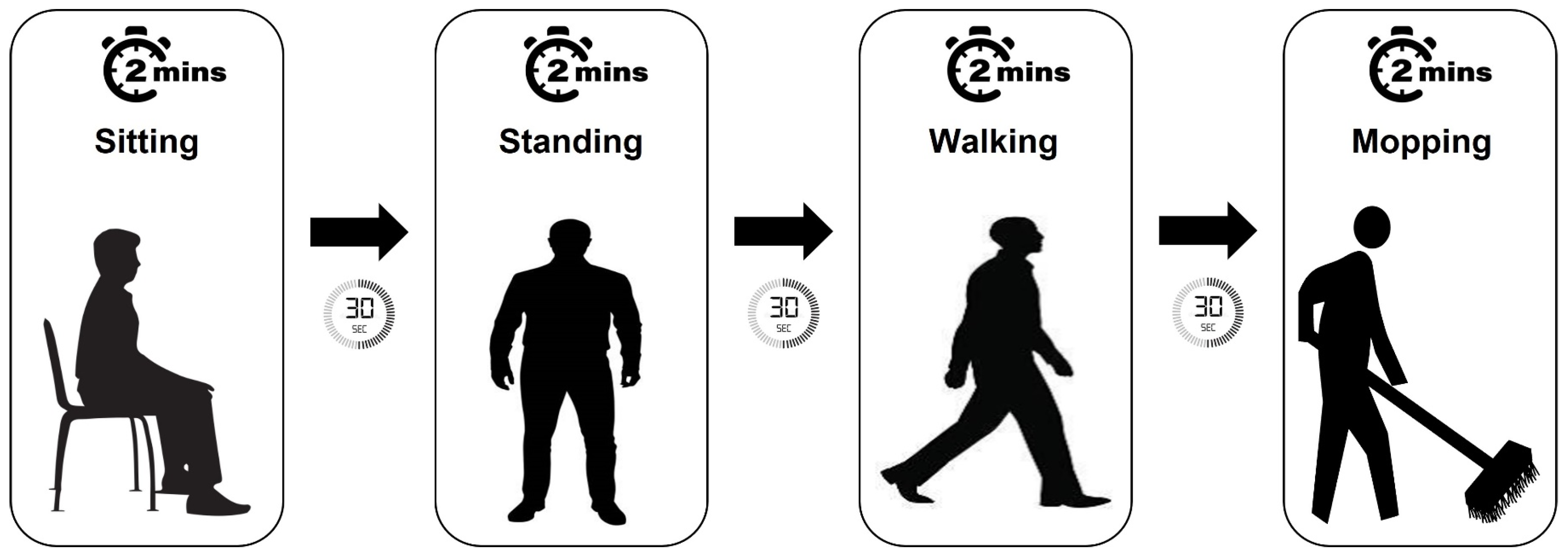
2.3. Experimental Measurement Setup
2.4. Data Analysis and Pre-Processing
3. Results
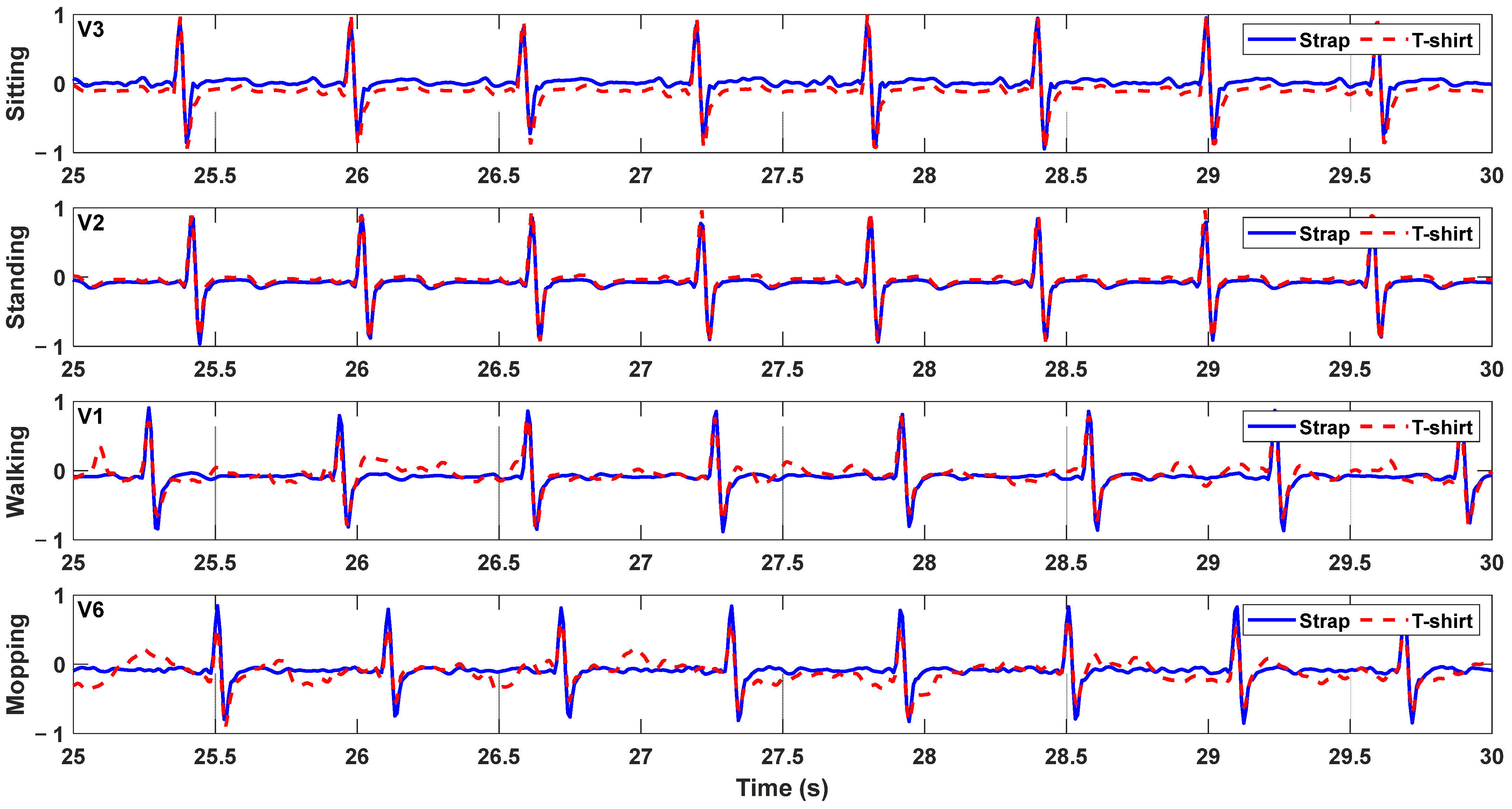
3.1. ECG Signal Recording
3.2. Heart Rate
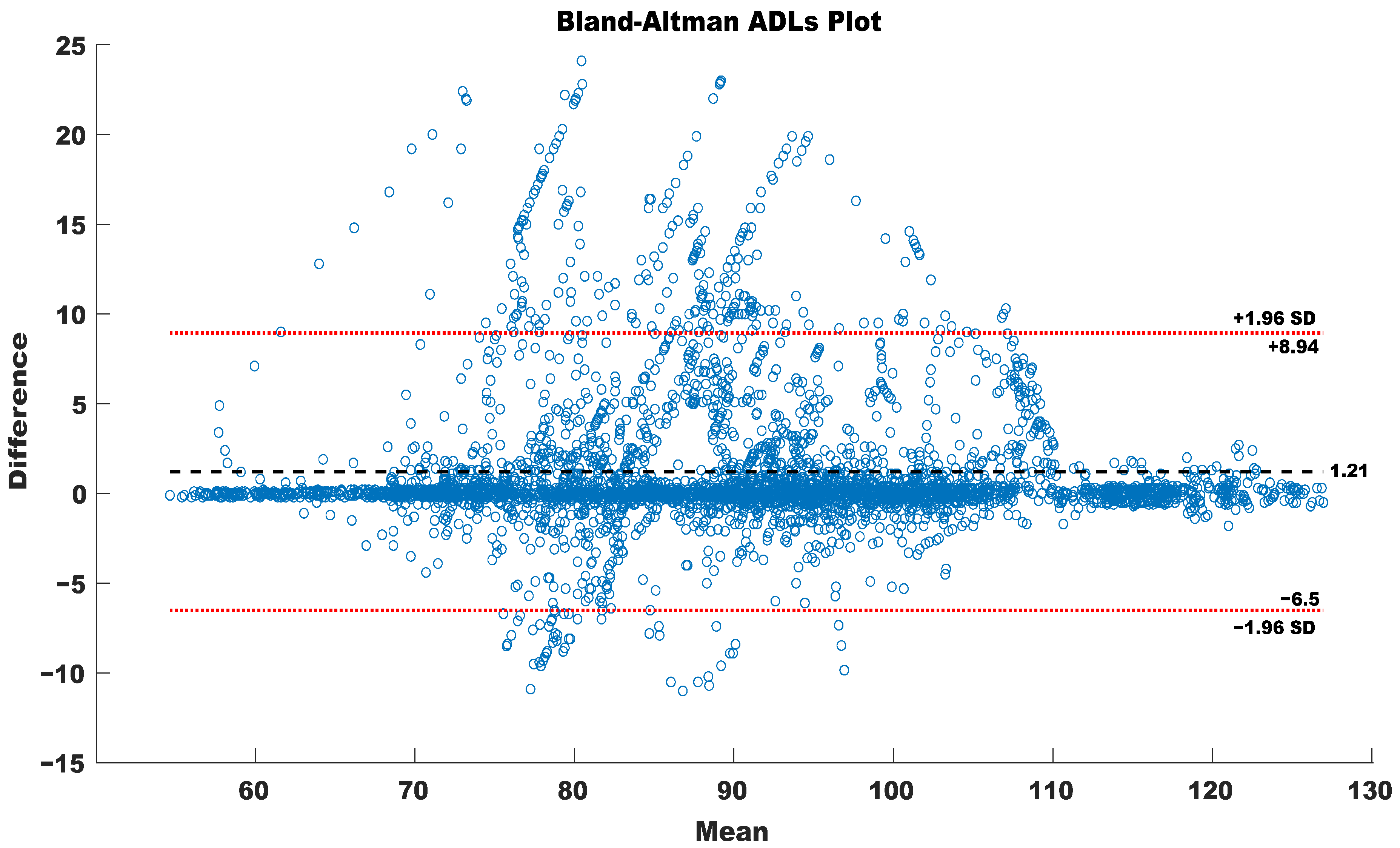
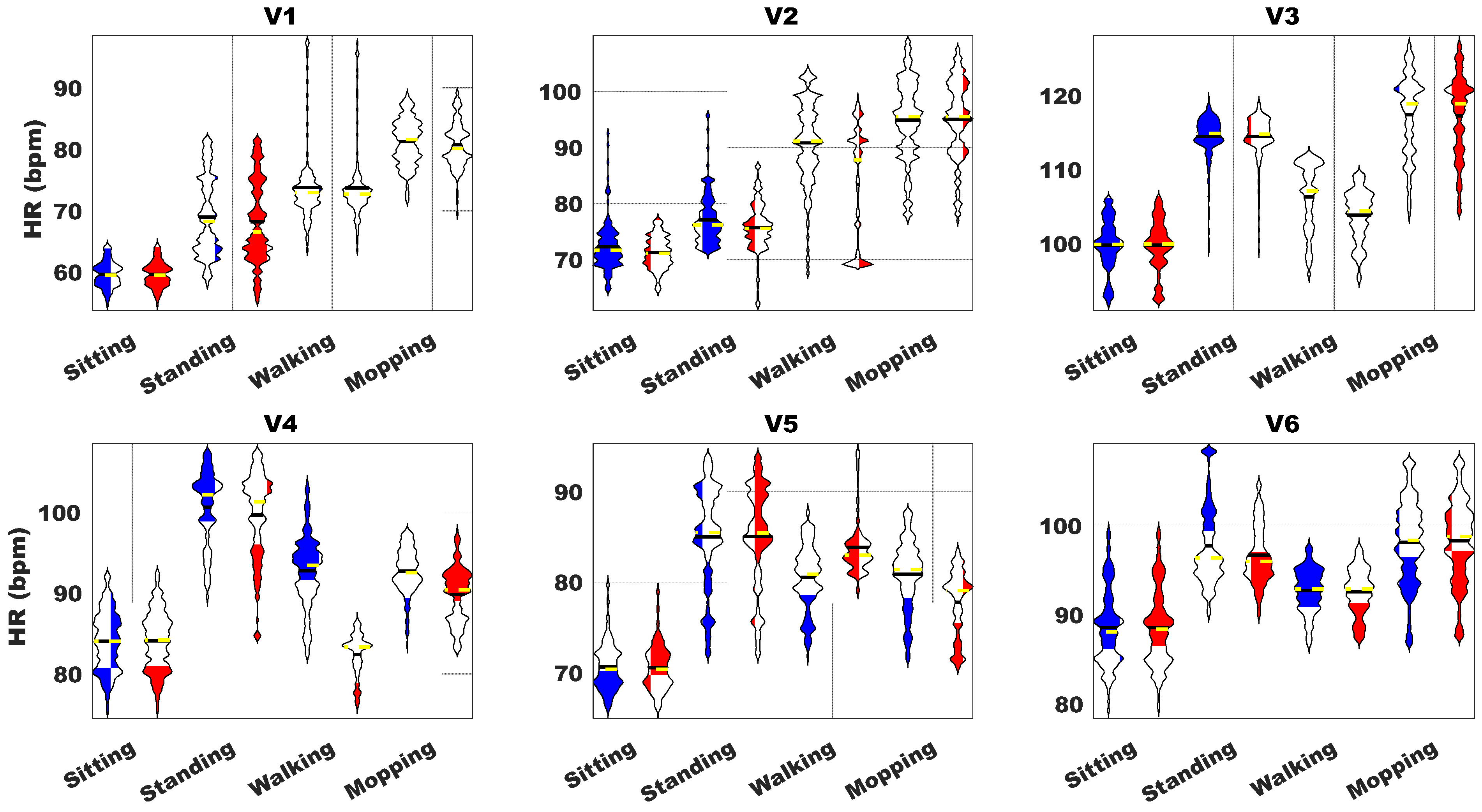
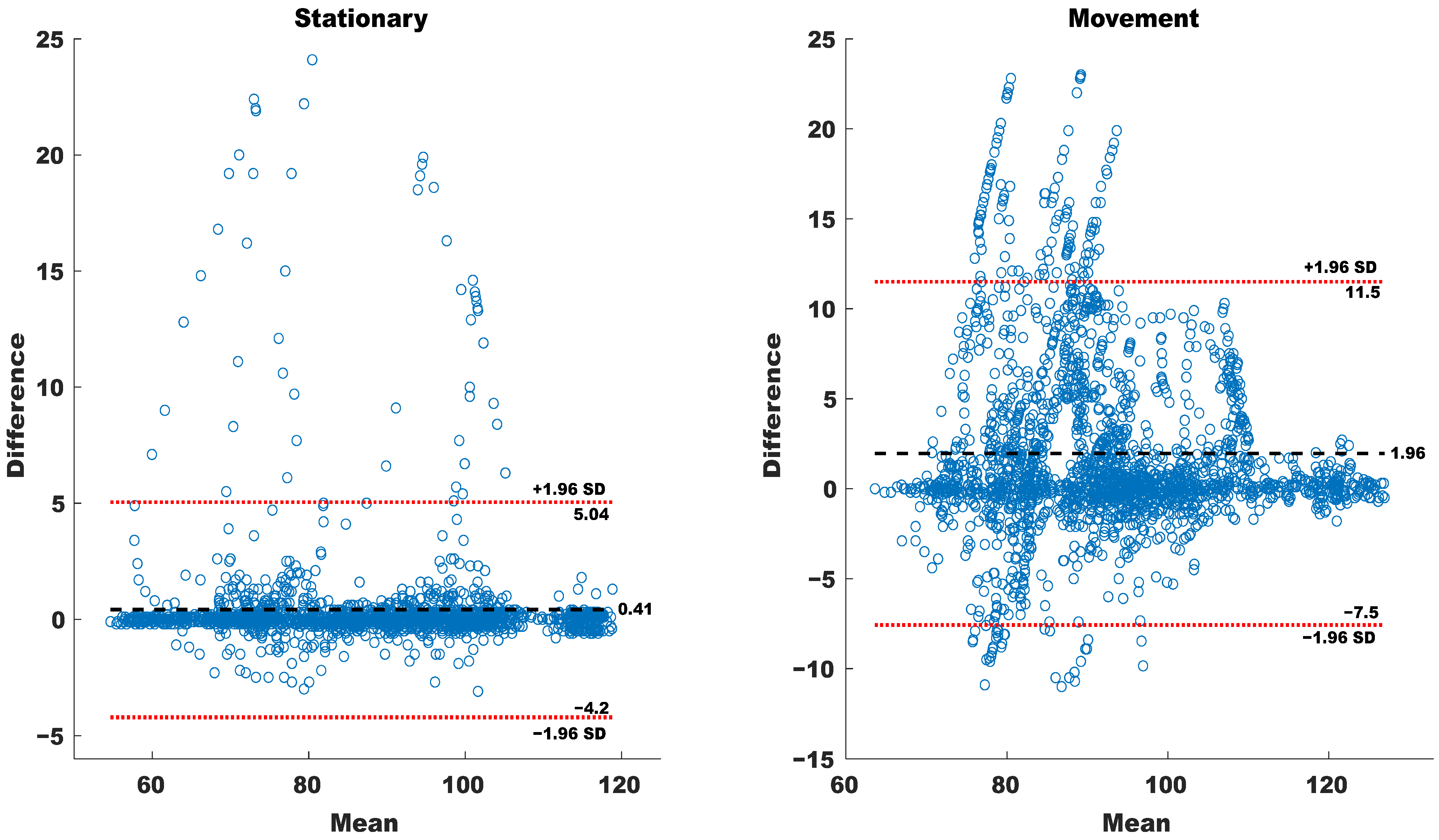
3.3. Activity of Daily Living
4. Discussion
4.1. Measurement Settings and Sensorized T-Shirt
4.2. ECG Measurement Performance
4.3. HR Measurement Performance
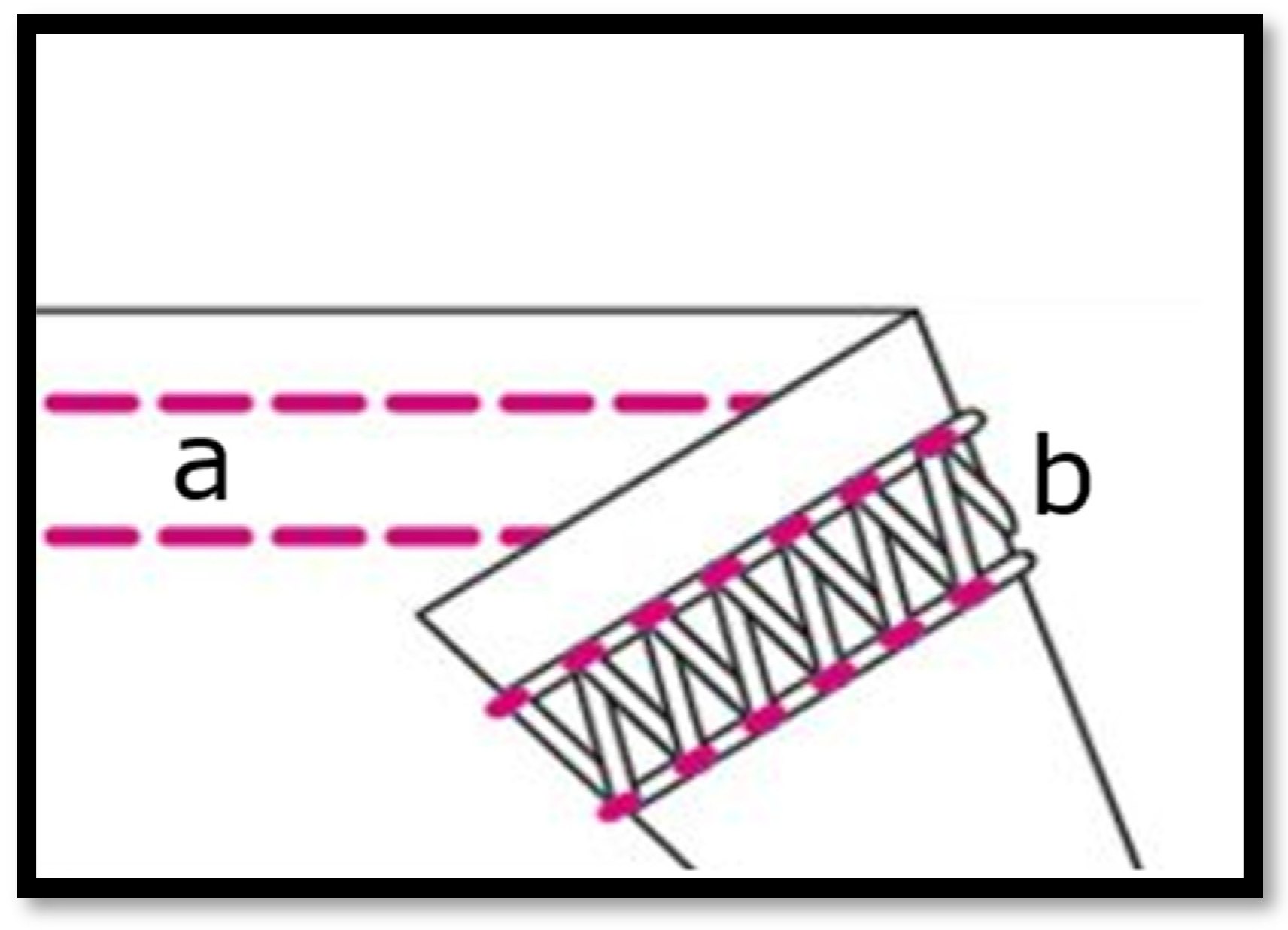
4.4. Selection of Bottom-Chain Stitch Sewing Method for Garment Seams
5. Conclusions and Future
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Iqbal, S.M.; Mahgoub, I.; Du, E.; Leavitt, M.A.; Asghar, W. Advances in healthcare wearable devices. NPJ Flex. Electron. 2021, 5, 9. [Google Scholar] [CrossRef]
- Kalantari, M. Consumers’ adoption of wearable technologies: Literature review, synthesis, and future research agenda. Int. J. Technol. Mark. 2017, 12, 274–307. [Google Scholar] [CrossRef]
- Sultan, N. Reflective thoughts on the potential and challenges of wearable technology for healthcare provision and medical education. Int. J. Inf. Manag. 2015, 35, 521–526. [Google Scholar] [CrossRef]
- Iqbal, M.H.; Aydin, A.; Brunckhorst, O.; Dasgupta, P.; Ahmed, K. A review of wearable technology in medicine. J. R. Soc. Med. 2016, 109, 372–380. [Google Scholar] [CrossRef] [PubMed]
- Pavón, I.; Sigcha, L.; Arezes, P.; Costa, N.; Arcas, G.; López, J.M. Wearable technology for occupational risk assessment: Potential avenues for applications. Occup. Saf. Hyg. VI 2018, 447–452. [Google Scholar]
- Najafi, B.; Armstrong, D.G.; Mohler, J. Novel wearable technology for assessing spontaneous daily physical activity and risk of falling in older adults with diabetes. SAGE J. 2013, 2013, 1147–1160. [Google Scholar] [CrossRef] [PubMed]
- Ananthanarayan, S.; Siek, K.A. Persuasive wearable technology design for health and wellness. In Proceedings of the 2012 6th International Conference on Pervasive Computing Technologies for Healthcare (PervasiveHealth) and Workshops, San Diego, CA, USA, 21–24 May 2012; pp. 236–240. [Google Scholar]
- Cheung, C.C.; Krahn, A.D.; Andrade, J.G. The emerging role of wearable technologies in detection of arrhythmia. Can. J. Cardiol. 2018, 34, 1083–1087. [Google Scholar] [CrossRef]
- Prieto-Avalos, G.; Cruz-Ramos, N.A.; Alor-Hernández, G.; Sánchez-Cervantes, J.L.; Rodríguez-Mazahua, L.; Guarneros-Nolasco, L.R. Wearable devices for physical monitoring of heart: A review. Biosensors 2022, 12, 292. [Google Scholar] [CrossRef]
- Hughes, A.; Shandhi MM, H.; Master, H.; Dunn, J.; Brittain, E. Wearable devices in cardiovascular medicine. Circ. Res. 2023, 132, 652–670. [Google Scholar] [CrossRef] [PubMed]
- Nigusse, A.B.; Mengistie, D.A.; Malengier, B.; Tseghai, G.B.; Langenhove, L.V. Wearable smart textiles for long-term electrocardiography monitoring—A review. Sensors 2021, 21, 4174. [Google Scholar] [CrossRef]
- Meziane, N.; Webster, J.; Attari, M.; Nimunkar, A.J.P.M. Dry electrodes for electrocardiography. Physiol. Meas. 2013, 34, R47. [Google Scholar] [CrossRef] [PubMed]
- Fu, Y.; Zhao, J.; Dong, Y.; Wang, X. Dry electrodes for human bioelectrical signal monitoring. Sensors 2020, 20, 3651. [Google Scholar] [CrossRef] [PubMed]
- Dey, N.; Ashour, A.S.; Shi, F.; Fong, S.J.; Sherratt, R.S. Developing residential wireless sensor networks for ECG healthcare monitoring. IEEE Trans. Consum. Electron. 2017, 63, 442–449. [Google Scholar] [CrossRef]
- Bayoumy, K.; Gaber, M.; Elshafeey, A.; Mhaimeed, O.; Dineen, E.H.; Marvel, F.A.; Elshazly, M.B. Smart wearable devices in cardiovascular care: Where we are and how to move forward. Nat. Rev. Cardiol. 2021, 18, 581–599. [Google Scholar] [CrossRef]
- Liu, J.; Liu, M.; Bai, Y.; Zhang, J.; Liu, H.; Zhu, W. Recent progress in flexible wearable sensors for vital sign monitoring. Sensors 2020, 20, 4009. [Google Scholar] [CrossRef] [PubMed]
- Wu, W.; Pirbhulal, S.; Sangaiah, A.K.; Mukhopadhyay, S.C.; Li, G. Optimization of signal quality over comfortability of textile electrodes for ECG monitoring in fog computing based medical applications. Future Gener. Comput. Syst. 2018, 86, 515–526. [Google Scholar] [CrossRef]
- Fouassier, D.; Roy, X.; Blanchard, A.; Hulot, J.S. Assessment of signal quality measured with a smart 12-lead ECG acquisition T-shirt. Ann. Noninvasive Electrocardiol. 2020, 25, e12682. [Google Scholar] [CrossRef]
- Cho, H.S.; Koo, S.M.; Lee, J.; Cho, H.; Kang, D.H.; Song, H.Y.; Lee, J.W.; Lee, K.H.; Lee, Y.J. Heart monitoring garments using textile electrodes for healthcare applications. J. Med. Syst. 2011, 35, 189–201. [Google Scholar] [CrossRef]
- Hanic, M.; Sládek, L.U.; Horínek, F.; Jagelka, M.; Donoval, M.; Dařícek, M.; Donoval, D. BIO-monitoring system with conductive textile electrodes integrated into t-shirt. In Proceedings of the 2014 24th International Conference Radioelektronika, Bratislava, Slovakia, 15–16 June 2014; pp. 1–4. [Google Scholar]
- Soroudi, A.; Hernández, N.; Berglin, L.; Nierstrasz, V. Electrode placement in electrocardiography smart garments: A review. J. Electrocardiol. 2019, 57, 27–30. [Google Scholar] [CrossRef]
- Wu, T.; Redouté, J.M.; Yuce, M. A wearable, low-power, real-time ECG monitor for smart t-shirt and IoT healthcare applications. In Advances in Body Area Networks I: Post-Conference Proceedings of BodyNets 2017; Springer: Cham, Switzerland, 2019; pp. 165–173. [Google Scholar]
- Masihi, S.; Panahi, M.; Maddipatla, D.; Hanson, A.J.; Fenech, S.; Bonek, L.; Sapoznik, N.; Fleming, P.D.; Bazuin, B.J.; Atashbar, M.Z. Development of a flexible wireless ECG monitoring device with dry fabric electrodes for wearable applications. IEEE Sens. J. 2021, 22, 11223–11232. [Google Scholar] [CrossRef]
- Dai, M.; Xiao, X.; Chen, X.; Lin, H.; Wu, W.; Chen, S. A low-power and miniaturized electrocardiograph data collection system with smart textile electrodes for monitoring of cardiac function. Australas. Phys. Eng. Sci. Med. 2016, 39, 1029–1040. [Google Scholar] [CrossRef] [PubMed]
- de Mulatier, S.; Nasreldin, M.; Delattre, R.; Ramuz, M.; Djenizian, T. Electronic circuits integration in textiles for data processing in wearable technologies. Adv. Mater. Technol. 2018, 3, 1700320. [Google Scholar] [CrossRef]
- Li, M.; Xiong, W.; Li, Y. Applications. Wearable measurement of ECG signals based on smart clothing. Int. J. Telemed. Appl. 2020, 2020, 6329360. [Google Scholar]
- Malek, A.S.; Elnahrawy, A.; Anwar, H.; Naeem, M. From fabric to smart T-shirt: Fine tuning an improved robust system to detect arrhythmia. Text. Res. J. 2022, 92, 3204–3220. [Google Scholar] [CrossRef]
- Choudhry, N.A.; Arnold, L.; Rasheed, A.; Khan, I.A.; Wang, L. Textronics—A review of textile-based wearable electronics. Adv. Eng. Mater. 2021, 23, 2100469. [Google Scholar] [CrossRef]
- Li, L.; Au, W.M.; Li, Y.; Wan, K.M.; Wan, S.H.; Wong, K.S. Design of intelligent garment with transcutaneous electrical nerve stimulation function based on the intarsia knitting technique. Text. Res. J. 2010, 80, 279–286. [Google Scholar] [CrossRef]
- Brown, S.; Ortiz-Catalan, M.; Petersson, J.; Rödby, K.; Seoane, F. Intarsia-sensorized band and textrodes for real-time myoelectric pattern recognition. In Proceedings of the 2016 38th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Orlando, FL, USA, 16–20 August 2016; pp. 6074–6077. [Google Scholar]
- Hashimoto, Y.; Sato, R.; Takagahara, K.; Ishihara, T.; Watanabe, K.; Togo, H. Validation of Wearable Device Consisting of a Smart Shirt with Built-In Bioelectrodes and a Wireless Transmitter for Heart Rate Monitoring in Light to Moderate Physical Work. Sensors 2022, 22, 9241. [Google Scholar] [CrossRef] [PubMed]
- Montes, J.; Young, J.C.; Tandy, R.; Navalta, J.W. Reliability and validation of the hexoskin wearable bio-collection device during walking conditions. Int. J. Exerc. Sci. 2018, 11, 806. [Google Scholar]
- Mekruksavanich, S.; Jantawong, P.; Jitpattanakul, A. Recognition of Human Activity from ECG and IMU Signals Using Deep Learning Networks. In Proceedings of the 2022 IEEE Region 10 Symposium (TENSYMP), Mumbai, India, 1–3 July 2022; pp. 1–5. [Google Scholar]
- Ni, Q.; Garcia Hernando, A.B.; De la Cruz, I.P. The elderly’s independent living in smart homes: A characterization of activities and sensing infrastructure survey to facilitate services development. Sensors 2015, 15, 11312–11362. [Google Scholar] [CrossRef]
- Tanantong, T.; Nantajeewarawat, E.; Thiemjarus, S. False alarm reduction in BSN-based cardiac monitoring using signal quality and activity type information. Sensors 2015, 15, 3952–3974. [Google Scholar] [CrossRef]
- Muhlsteff, J.; Such, O.; Schmidt, R.; Perkuhn, M.; Reiter, H.; Lauter, J.; Thijs, J.; Musch, G.; Harris, M. Wearable approach for continuous ECG-and activity patient-monitoring. In Proceedings of the The 26th Annual International Conference of the IEEE Engineering in Medicine and Biology Society, San Francisco, CA, USA, 1–5 September 2004; pp. 2184–2187. [Google Scholar]
- Van Steenis, H.; Tulen, J. The effects of physical activities on cardiovascular variability in ambulatory situations [ECG/accelerometry analysis]. In Proceedings of the 19th Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Magnificent Milestones and Emerging Opportunities in Medical Engineering (Cat. No. 97CH36136), Chicago, IL, USA, 30 October–2 November 1997; pp. 105–108. [Google Scholar]
- Miao, F.; Cheng, Y.; He, Y.; He, Q.; Li, Y. A wearable context-aware ECG monitoring system integrated with built-in kinematic sensors of the smartphone. Sensors 2015, 15, 11465–11484. [Google Scholar] [CrossRef] [PubMed]
- Gjoreski, H.; Rashkovska, A.; Kozina, S.; Lustrek, M.; Gams, M. Telehealth using ECG sensor and accelerometer. In Proceedings of the 2014 37th International Convention on Information and Communication Technology, Electronics and Microelectronics (MIPRO), Opatija, Croatia, 26–30 May 2014; pp. 270–274. [Google Scholar]
- Hafid, A.; Gunnarsson, E.; Rödby, K.; Seoane, F. Seamless integration of textile-electronics in knitted fabrics for personalized health. In Proceedings of the Autex Conference, 21st World Conference AUTEX 2022, Lodz, Poland, 7–10 June 2022. [Google Scholar]
- Rogers, B.; Schaffarczyk, M.; Clauß, M.; Mourot, L.; Gronwald, T. The Movesense Medical Sensor Chest Belt Device as Single Channel ECG for RR Interval Detection and HRV Analysis during Resting State and Incremental Exercise: A Cross-Sectional Validation Study. Sensors 2022, 22, 2032. [Google Scholar] [CrossRef] [PubMed]
- Zhao, J.; Itti, L. Shapedtw: Shape dynamic time warping. Pattern Recognit. 2018, 74, 171–184. [Google Scholar] [CrossRef]
- Fink, P.L.; Sayem AS, M.; Teay, S.H.; Ahmad, F.; Shahariar, H.; Albarbar, A. Development and wearer trial of ECG-garment with textile-based dry electrodes. Sens. Actuators A Phys. 2021, 328, 112784. [Google Scholar] [CrossRef]
- Boehm, A.; Yu, X.; Neu, W.; Leonhardt, S.; Teichmann, D. A novel 12-lead ECG T-shirt with active electrodes. Electronics 2016, 5, 75. [Google Scholar] [CrossRef]
- Hafid, A.; Gunnarsson, E.; Rödby, K.; Ramos, A.; Abtahi, F.; Seoane, F. Sensorized T-shirt with fully integrated textrodes and measurement leads with textile-friendly methods. In Proceedings of the International Conference on Biomedical and Health Informatics (ICBHI 2022), Concepcion, Chile, 24–26 November 2022. [Google Scholar]
- ISO 4915: 1991; Stitches and Seams-Part 1: Classification and Terminology of Stitch Types. International Organization for Standardization: Geneva, Switzerland, 1991.





| (mV) | Sitting | Standing | Walking | Mopping |
|---|---|---|---|---|
| V1 | 2.33 | 2.12 | 6.97 | 11.14 |
| V2 | 1.70 | 4.05 | 10.48 | 7.02 |
| V3 | 6.42 | 5.49 | 5.00 | 10.08 |
| V4 | 1.61 | 3.00 | 9.20 | 14.05 |
| V5 | 6.30 | 5.70 | 9.00 | 12.20 |
| V6 | 2.68 | 3.44 | 4.70 | 5.44 |
| Mean ± STD | 3.50 ± 2.05 | 3.96 ± 1.28 | 7.55 ± 2.17 | 9.98 ± 2.95 |
| Stationary: 3.73 ± 0.23 | Movement: 8.77 ± 1.21 | |||
| (%) | Stationary | Movement |
|---|---|---|
| V1 | 0.73 | 0.53 |
| V2 | 1.50 | 2.00 |
| V3 | 0.26 | 1.37 |
| V4 | 0.23 | 3.67 |
| V5 | 0.19 | 4.49 |
| V6 | 0.24 | 0.45 |
| Mean ± STD | 0.53 ± 0.47 | 2.17 ± 1.53 |
| (%) | Sitting | Standing | Walking | Mopping |
|---|---|---|---|---|
| V1 | 0.10 | 1.36 | 0.51 | 0.54 |
| V2 | 0.29 | 2.71 | 3.68 | 1.31 |
| V3 | 0.28 | 0.25 | 2.36 | 0.39 |
| V4 | 0.17 | 0.29 | 4.24 | 3.09 |
| V5 | 0.18 | 0.21 | 5.14 | 3.84 |
| V6 | 0.12 | 0.37 | 0.53 | 0.37 |
| Mean ± STD | 0.19 ± 0.07 | 0.86 ± 0.92 | 2.74 ± 1.77 | 1.59 ± 1.38 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hafid, A.; Gunnarsson, E.; Ramos, A.; Rödby, K.; Abtahi, F.; Bamidis, P.D.; Billis, A.; Papachristou, P.; Seoane, F. Sensorized T-Shirt with Intarsia-Knitted Conductive Textile Integrated Interconnections: Performance Assessment of Cardiac Measurements during Daily Living Activities. Sensors 2023, 23, 9208. https://doi.org/10.3390/s23229208
Hafid A, Gunnarsson E, Ramos A, Rödby K, Abtahi F, Bamidis PD, Billis A, Papachristou P, Seoane F. Sensorized T-Shirt with Intarsia-Knitted Conductive Textile Integrated Interconnections: Performance Assessment of Cardiac Measurements during Daily Living Activities. Sensors. 2023; 23(22):9208. https://doi.org/10.3390/s23229208
Chicago/Turabian StyleHafid, Abdelakram, Emanuel Gunnarsson, Alberto Ramos, Kristian Rödby, Farhad Abtahi, Panagiotis D. Bamidis, Antonis Billis, Panagiotis Papachristou, and Fernando Seoane. 2023. "Sensorized T-Shirt with Intarsia-Knitted Conductive Textile Integrated Interconnections: Performance Assessment of Cardiac Measurements during Daily Living Activities" Sensors 23, no. 22: 9208. https://doi.org/10.3390/s23229208
APA StyleHafid, A., Gunnarsson, E., Ramos, A., Rödby, K., Abtahi, F., Bamidis, P. D., Billis, A., Papachristou, P., & Seoane, F. (2023). Sensorized T-Shirt with Intarsia-Knitted Conductive Textile Integrated Interconnections: Performance Assessment of Cardiac Measurements during Daily Living Activities. Sensors, 23(22), 9208. https://doi.org/10.3390/s23229208








