WATCH-BPM—Comparison of a WATCH-Type Blood Pressure Monitor with a Conventional Ambulatory Blood Pressure Monitor and Auscultatory Sphygmomanometry
Abstract
:1. Introduction
2. Methods
2.1. Study Population for the Single Measurements and Long-Term Measurement
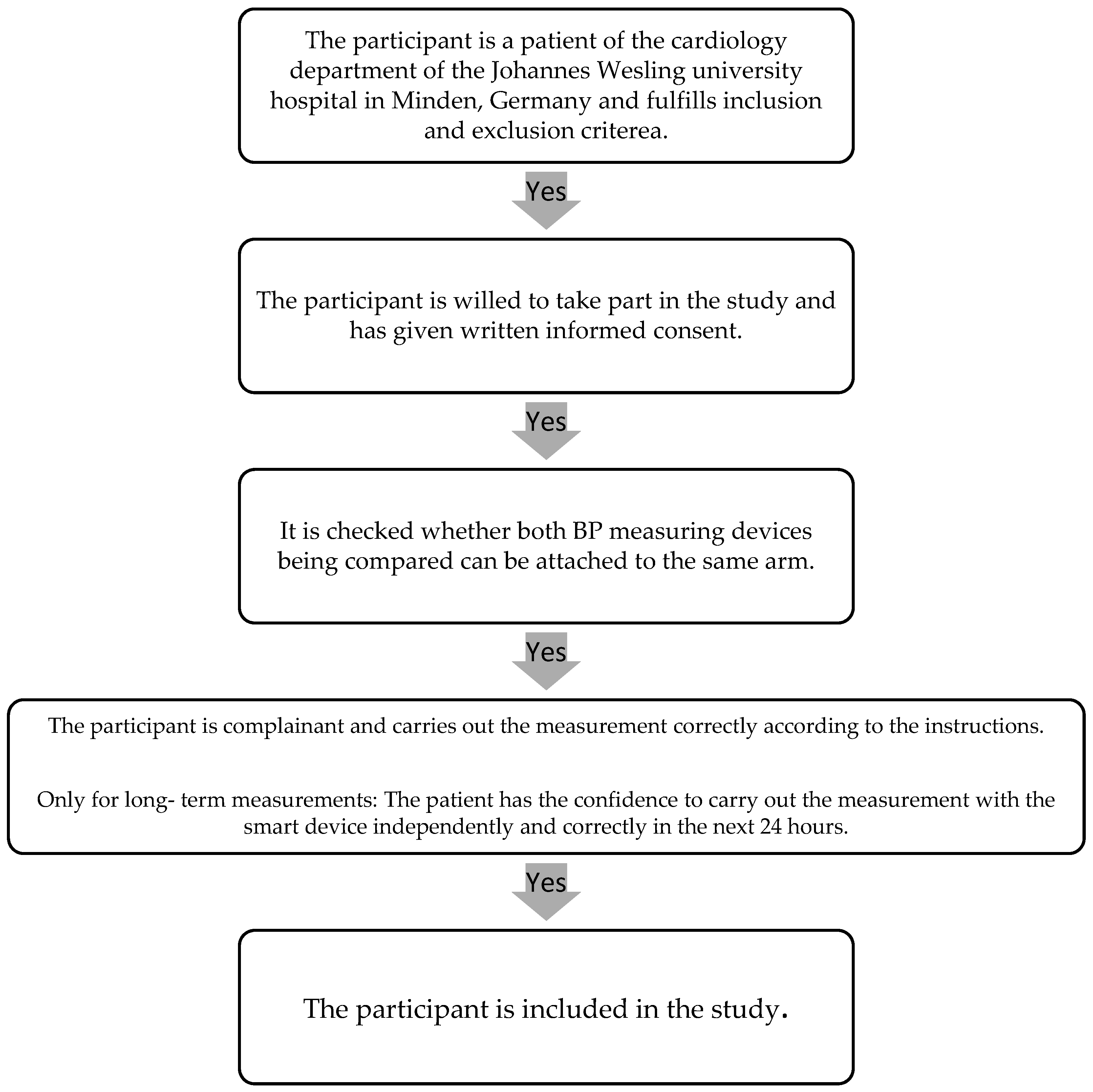
2.2. Participant Selection Process
2.3. BP Measurement Devices
2.4. BP Measurement Protocol in the Single Measurements
2.5. BP Measurement Protocol in the Long-Term Measurements
2.6. Statistical Analysis of the Single and Long-Term Measurements
3. Results
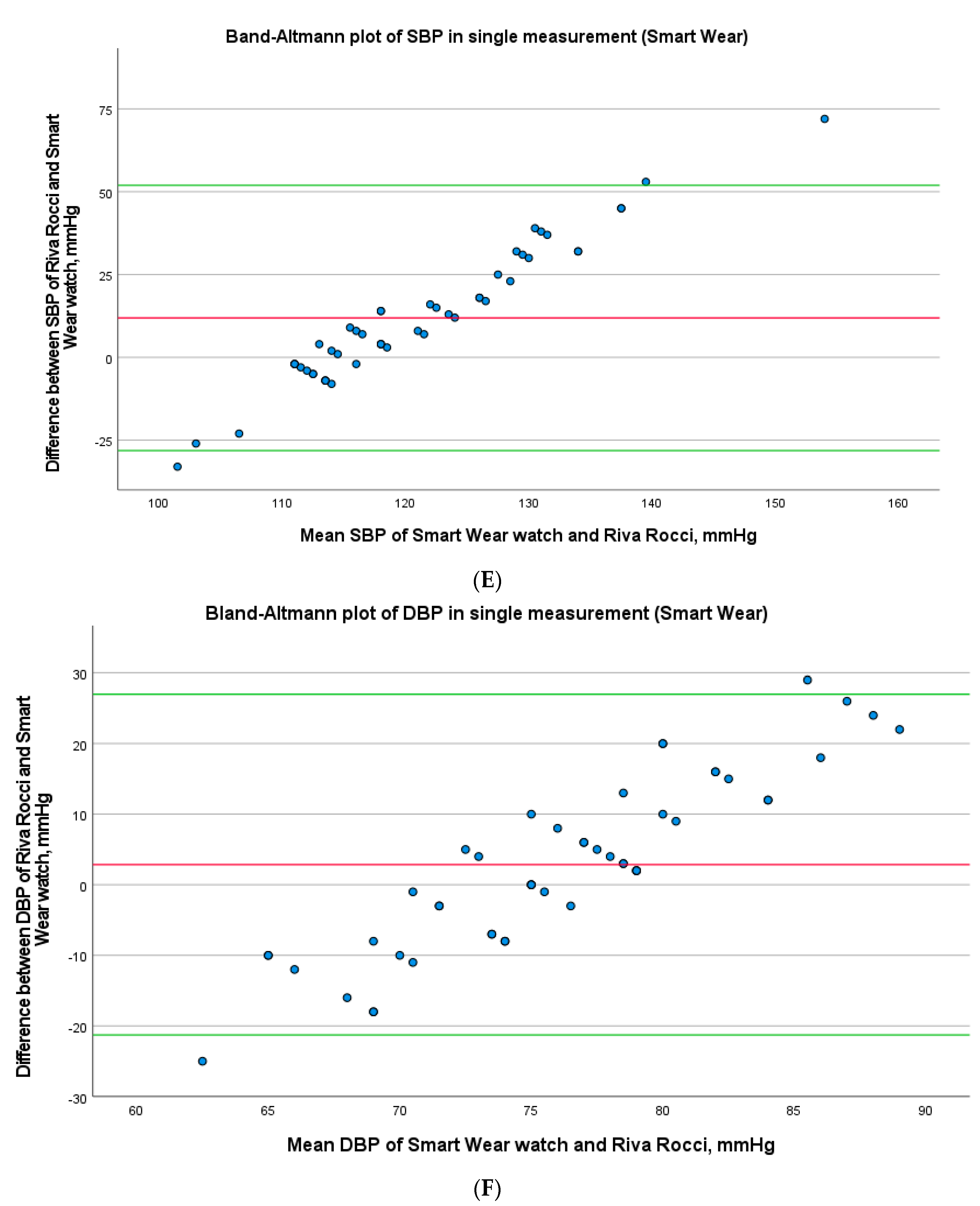
3.1. Single Measurement
3.2. Long-Term Measurement
4. Discussion
4.1. Single Measurement
4.2. Long-Term Measurement
4.3. Smart Wear Watch
4.4. Advantages and Disadvantages of BP Detection using the Smart Device and Outlook
4.5. Mismeasurements
4.6. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lewington, S.; Clarke, R.; Qizilbash, N.; Peto, R.; Collins, R. Age-specific relevance of usual blood pressure to vascular mortality: A meta-analysis of individual data for one million adults in 61 prospective studies. Lancet 2002, 360, 1903–1913. [Google Scholar] [CrossRef]
- Pickering, T.G.; Schwartz, J.E.; James, G.D. Ambulatory blood pressure monitoring for evaluating the relationships between lifestyle, hypertension and cardiovascular risk. Clin. Exp. Pharmacol. Physiol. 1995, 22, 226–231. [Google Scholar] [CrossRef] [PubMed]
- Miceli, F.; Presta, V.; Citoni, B.; Canichella, F.; Figliuzzi, I.; Ferrucci, A.; Volpe, M.; Tocci, G. Conventional and new electrocardiographic criteria for hypertension-mediated cardiac organ damage: A narrative review. J. Clin. Hypertens. 2019, 21, 1863–1871. [Google Scholar] [CrossRef] [PubMed]
- Welser, L.; Pfeiffer, K.A.; Silveira, J.F.d.C.; Valim, A.R.d.M.; Renner, J.D.P.; Reuter, C.P. Incidência de Hipertensão Arterial está Associada com Adiposidade em Crianças e Adolescentes. Arq. Bras. Cardiol. 2023, 120, e20220070. [Google Scholar] [CrossRef]
- Thijs, L.; Den Hond, E.; Nawrot, T.; Staessen, J.A. Prevalence, pathophysiology and treatment of isolated systolic hypertension in the elderly. Expert Rev. Cardiovasc. Ther. 2004, 2, 761–769. [Google Scholar] [CrossRef]
- Ott, C.; Schmieder, R.E. Diagnosis and treatment of arterial hypertension 2021. Kidney Int. 2022, 101, 36–46. [Google Scholar] [CrossRef]
- Pickering, T.G.; Miller, N.H.; Ogedegbe, G.; Krakoff, L.R.; Artinian, N.T.; Goff, D. Call to action on use and reimbursement for home blood pressure monitoring: Executive summary: A joint scientific statement from the American Heart Association, American Society Of Hypertension, and Preventive Cardiovascular Nurses Association. Hypertension 2008, 52, 1–9. [Google Scholar] [CrossRef]
- Williams, B.; Mancia, G.; Spiering, W.; Agabiti Rosei, E.; Azizi, M.; Burnier, M.; Clement, D.L.; Coca, A.; de Simone, G.; Dominiczak, A.; et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur. Heart J. 2018, 39, 3021–3104. [Google Scholar] [CrossRef] [PubMed]
- Greaves, F.; Joshi, I.; Campbell, M.; Roberts, S.; Patel, N.; Powell, J. What is an appropriate level of evidence for a digital health intervention? Lancet 2019, 392, 2665–2667. [Google Scholar] [CrossRef]
- Omboni, S.; Ferrari, R. The role of telemedicine in hypertension management: Focus on blood pressure telemonitoring. Curr. Hypertens. Rep. 2015, 17, 535. [Google Scholar] [CrossRef]
- Omboni, S.; Panzeri, E.; Campolo, L. E-Health in Hypertension Management: An Insight into the Current and Future Role of Blood Pressure Telemonitoring. Curr. Hypertens. Rep. 2020, 22, 42. [Google Scholar] [CrossRef] [PubMed]
- Bayoumy, K.; Gaber, M.; Elshafeey, A.; Mhaimeed, O.; Dineen, E.H.; Marvel, F.A.; Martin, S.S.; Muse, E.D.; Turakhia, M.P.; Tarakji, K.G.; et al. Smart wearable devices in cardiovascular care: Where we are and how to move forward. Nat. Rev. Cardiol. 2021, 18, 581–599. [Google Scholar] [CrossRef]
- HeartGuide. Available online: https://www.omron-healthcare.de/de/blutdruckmessgeraete/heartguide.html (accessed on 29 November 2021).
- Kario, K.; Shimbo, D.; Tomitani, N.; Kanegae, H.; Schwartz, J.E.; Williams, B. The first study comparing a wearable watch-type blood pressure monitor with a conventional ambulatory blood pressure monitor on in-office and out-of-office settings. J. Clin. Hypertens. 2020, 22, 135–141. [Google Scholar] [CrossRef] [PubMed]
- Kuwabara, M.; Harada, K.; Hishiki, Y.; Kario, K. Validation of two watch-type wearable blood pressure monitors according to the ANSI/AAMI/ISO81060-2:2013 guidelines: Omron HEM-6410T-ZM and HEM-6410T-ZL. J. Clin. Hypertens. 2019, 21, 853–858. [Google Scholar] [CrossRef]
- OMRON HeartAdvisor–Apps Bei Google Play. Available online: https://play.google.com/store/apps/details?id=com.omronhealthcare.heartadvisor&hl=de&gl=US (accessed on 17 June 2022).
- Kachuee, M.; Kiani, M.M.; Mohammadzade, H.; Shabany, M. Cuffless Blood Pressure Estimation Algorithms for Continuous Health-Care Monitoring. IEEE Trans. Biomed. Eng. 2017, 64, 859–869. [Google Scholar] [CrossRef] [PubMed]
- Veerman, D.P.; Lenders, J.; Thien, T.; van Montfrans, G.V. LAM 100/Marshall F-88: Accuracy and precision of a new device for discontinuous finger blood pressure measurement. J. Hum. Hypertens. 1993, 7, 113–115. [Google Scholar]
- Anlauf, M.; Tholl, U.; Högermeyer, D.; Hirche, H.; Roggenbuck, U.; Simonides, R. Devices for blood pressure self measurement: Tested in comparison. Z. Kardiol. 1996, 85 (Suppl. S3), 20–25. [Google Scholar] [PubMed]
- Parati, G.; Stergiou, G.S.; Asmar, R.; Bilo, G.; de Leeuw, P.; Imai, Y.; Kario, K.; Lurbe, E.; Manolis, A.; Mengden, T.; et al. European Society of Hypertension practice guidelines for home blood pressure monitoring. J. Hum. Hypertens. 2010, 24, 779–785. [Google Scholar] [CrossRef] [PubMed]
- Breaux-Shropshire, T.L.; Judd, E.; Vucovich, L.A.; Shropshire, T.S.; Singh, S. Does home blood pressure monitoring improve patient outcomes? A systematic review comparing home and ambulatory blood pressure monitoring on blood pressure control and patient outcomes. Integr. Blood Press. Control 2015, 8, 43–49. [Google Scholar] [CrossRef]
- Methoden und Systeme zur Nichtinvasiven, Kontinuierlichen und Belastungsfreien Blutdruckmessung. Available online: https://d-nb.info/1013872142/34 (accessed on 30 April 2020).
- Kikuya, M.; Chonan, K.; Imai, Y.; Goto, E.; Ishii, M. Accuracy and reliability of wrist-cuff devices for self-measurement of blood pressure. J. Hypertens. 2002, 20, 629–638. [Google Scholar] [CrossRef]
- Yarows, S. Comparison of the omron HEM-637 wrist monitor to the auscultation method with the wrist position sensor on or disabled. Am. J. Hypertens. 2004, 17, 54–58. [Google Scholar] [CrossRef]
- Kikuya, M.; Hozawa, A.; Ohokubo, T.; Tsuji, I.; Michimata, M.; Matsubara, M.; Ota, M.; Nagai, K.; Araki, T.; Satoh, H.; et al. Prognostic Significance of Blood Pressure and Heart Rate Variabilities. Hypertension 2000, 36, 901–906. [Google Scholar] [CrossRef]
- Kario, K.; James, G.D.; Marion, R.; Ahmed, M.; Pickering, T.G. The Influence of Work and Home-Related Stress on the Levels and Diurnal Variation of Ambulatory Blood Pressure and Neurohumoral Factors in Employed Women. Hypertens. Res. 2002, 25, 499–506. [Google Scholar] [CrossRef] [PubMed]
- Guyton, A.C.; Coleman, T.G.; Granger, H.J. Circulation: Overall regulation. Annu. Rev. Physiol. 1972, 34, 13–46. [Google Scholar] [CrossRef]
- Kurki, T.; Smith, N.T.; Head, N.; Dec-Silver, H.; Quinn, A. Noninvasive continuous blood pressure measurement from the finger: Optimal measurement conditions and factors affecting reliability. J. Clin. Monitor. Comput. 1987, 3, 6–13. [Google Scholar] [CrossRef] [PubMed]
- Lane, J.D.; Greenstadt, L.; Shapiro, D.; Rubinstein, E. Pulse transit time and blood pressure: An intensive analysis. Psychophysiology 1983, 20, 45–49. [Google Scholar] [CrossRef] [PubMed]
- Bird, K.; Chan, G.; Lu, H.; Greeff, H.; Allen, J.; Abbott, D.; Menon, C.; Lovell, N.H.; Howard, N.; Chan, W.-S.; et al. Assessment of Hypertension Using Clinical Electrocardiogram Features: A First-Ever Review. Front. Med. 2020, 7, 583331. [Google Scholar] [CrossRef]
- Rossi, G.P.; Bisogni, V.; Rossitto, G.; Maiolino, G.; Cesari, M.; Zhu, R.; Seccia, T.M. Practice Recommendations for Diagnosis and Treatment of the Most Common Forms of Secondary Hypertension. High Blood Press. Cardiovasc. Prev. 2020, 27, 547–560. [Google Scholar] [CrossRef]
- Citoni, B.; Figliuzzi, I.; Presta, V.; Volpe, M.; Tocci, G. Home Blood Pressure and Telemedicine: A Modern Approach for Managing Hypertension During and After COVID-19 Pandemic. High Blood Press. Cardiovasc. Prev. 2022, 29, 1–14. [Google Scholar] [CrossRef]
- McManus, R.J.; Little, P.; Stuart, B.; Morton, K.; Raftery, J.; Kelly, J.; Bradbury, K.; Zhang, J.; Zhu, S.; Murray, E.; et al. Home and Online Management and Evaluation of Blood Pressure (HOME BP) using a digital intervention in poorly controlled hypertension: Randomised controlled trial. BMJ 2021, 372, m4858. [Google Scholar] [CrossRef]




| Single Measurement | Long-Term Measurement | |
|---|---|---|
| Age, y | 69.8 ± 13.6 | 52.3 ± 14.5 |
| Men:women, n | 57:52 | 27:23 |
| Wrist circumference, cm | 17.9 ± 1.6 | 17.6 ± 1.3 |
| Height, meter | 1.71 ± 0.1 | 1.75 ± 0.1 |
| Weight, kg | 81.8 ± 18.5 | 90.0 ± 20.9 |
| BMI kg/m2 | 27.8 ± 5.5 | 29.3 ± 6.1 |
| Omron HeartGuide (WBPM) | Riva Rocci | Difference (Riva Rocci-WBPM) | Correlation Coefficient (ICC) | |
|---|---|---|---|---|
| SBP, mmHg | 132.96 ± 21.10 | 127.68 ± 18.89 | −5.28 ± 1.71 | 0.765 |
| DBP, mmHg | 76.41 ± 14.11 | 75.60 ± 11.22 | −0.81 ± 1.17 | 0.732 |
| Omron HeartGuide (WBPM) | Ambulatory Blood Presaure Monitor | Difference (ABPM-WBPM) | Correlation Coefficient (ICC) | |
|---|---|---|---|---|
| SBP, mmHg | 119.89 ± 15.21 | 120.61 ± 15.75 | 0.72 ± 1.44 | 0.880 |
| DBP, mmHg | 71.28 ± 9.65 | 75.54 ± 10.43 | 4.27 ± 0.97 | 0.829 |
| Single Measurement n = 109 | Long-Term Measurement n = 50 | |
|---|---|---|
| Smoker (N=) | 16 | 10 |
| Cardiovascular disease | 107 | 38 |
| 93 | 35 |
| 22 | 0 |
| Antihypertensive medication | 90 | 31 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vaseekaran, M.; Kaese, S.; Görlich, D.; Wiemer, M.; Samol, A. WATCH-BPM—Comparison of a WATCH-Type Blood Pressure Monitor with a Conventional Ambulatory Blood Pressure Monitor and Auscultatory Sphygmomanometry. Sensors 2023, 23, 8877. https://doi.org/10.3390/s23218877
Vaseekaran M, Kaese S, Görlich D, Wiemer M, Samol A. WATCH-BPM—Comparison of a WATCH-Type Blood Pressure Monitor with a Conventional Ambulatory Blood Pressure Monitor and Auscultatory Sphygmomanometry. Sensors. 2023; 23(21):8877. https://doi.org/10.3390/s23218877
Chicago/Turabian StyleVaseekaran, Mathini, Sven Kaese, Dennis Görlich, Marcus Wiemer, and Alexander Samol. 2023. "WATCH-BPM—Comparison of a WATCH-Type Blood Pressure Monitor with a Conventional Ambulatory Blood Pressure Monitor and Auscultatory Sphygmomanometry" Sensors 23, no. 21: 8877. https://doi.org/10.3390/s23218877
APA StyleVaseekaran, M., Kaese, S., Görlich, D., Wiemer, M., & Samol, A. (2023). WATCH-BPM—Comparison of a WATCH-Type Blood Pressure Monitor with a Conventional Ambulatory Blood Pressure Monitor and Auscultatory Sphygmomanometry. Sensors, 23(21), 8877. https://doi.org/10.3390/s23218877








