Design of a Sensor-Technology-Augmented Gait and Balance Monitoring System for Community-Dwelling Older Adults in Hong Kong: A Pilot Feasibility Study
Abstract
:1. Introduction
2. Methods
2.1. Design of the System Architecture
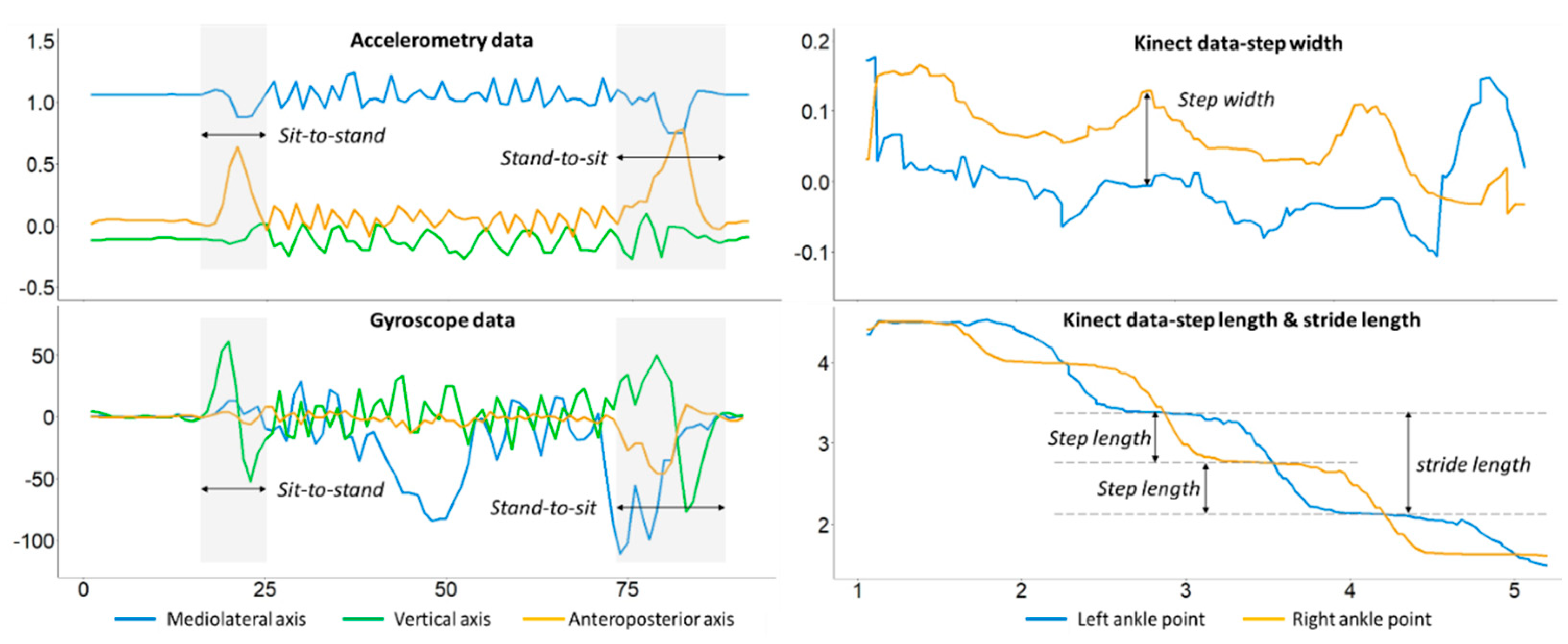
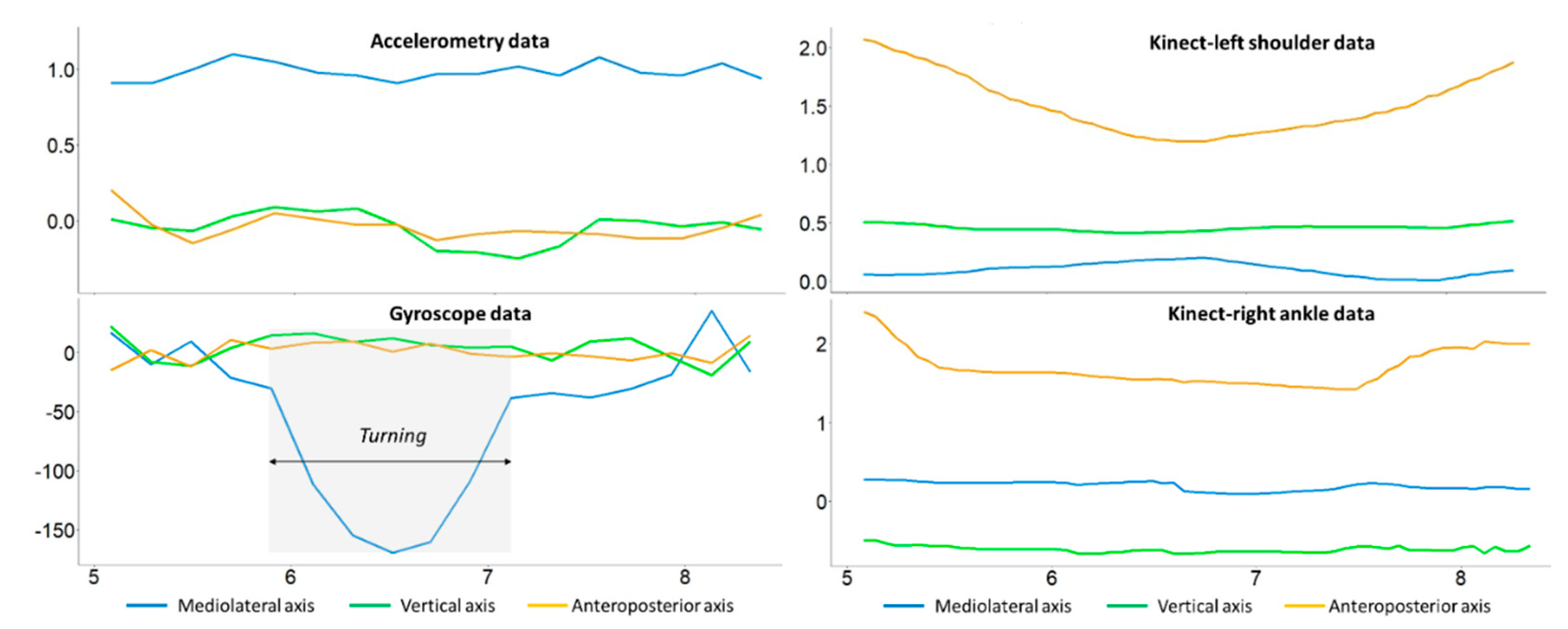
- Task-1: 3-m timed up and go (3M-TUG) test
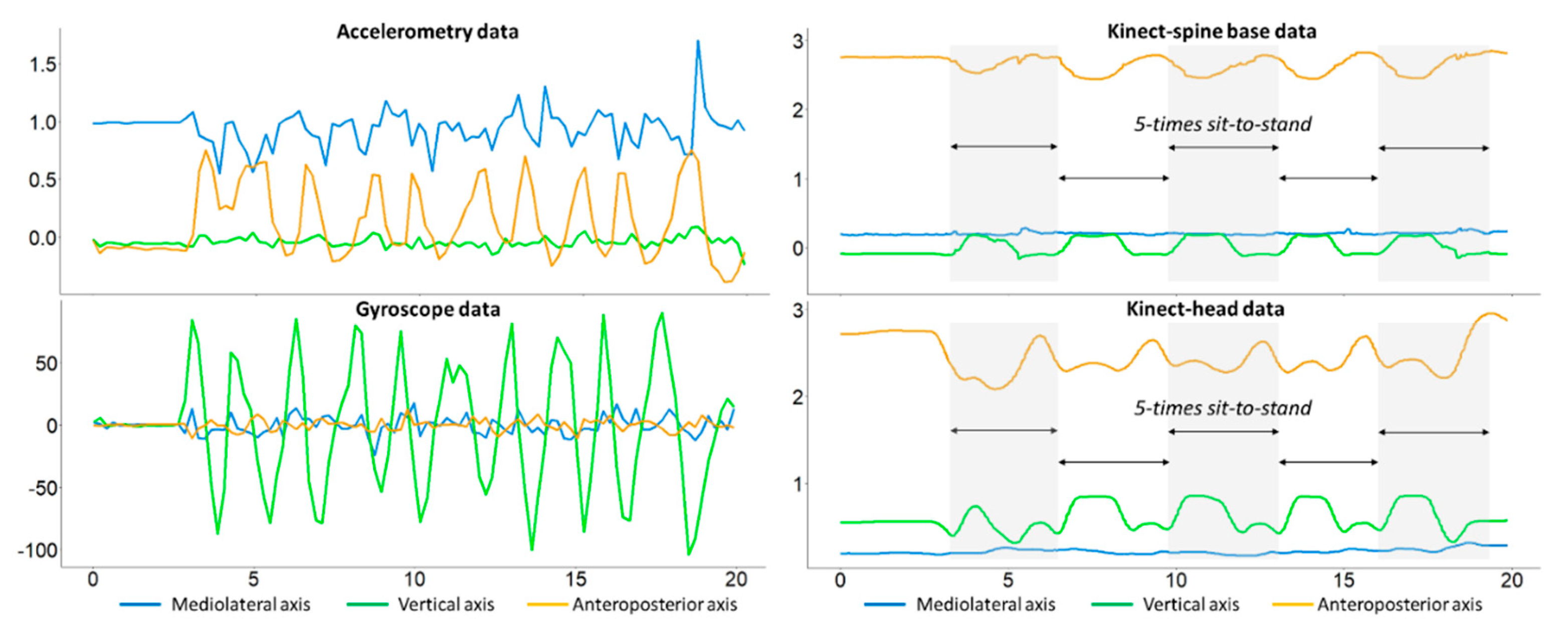
- Task-2: Five-times-sit-to-stand (FTSTS) test
- Task 3: Romberg test
- Gait and balance evaluation-1: BBS
- Gait and balance evaluation-2: Brief-BESTest (Balance evaluation systems test)
2.2. Feature Extraction and Prediction Models
2.3. Testing Protocol
2.3.1. Participants
2.3.2. Data Collection
2.3.3. Data Summary
3. Results and Discussion
3.1. Demographics
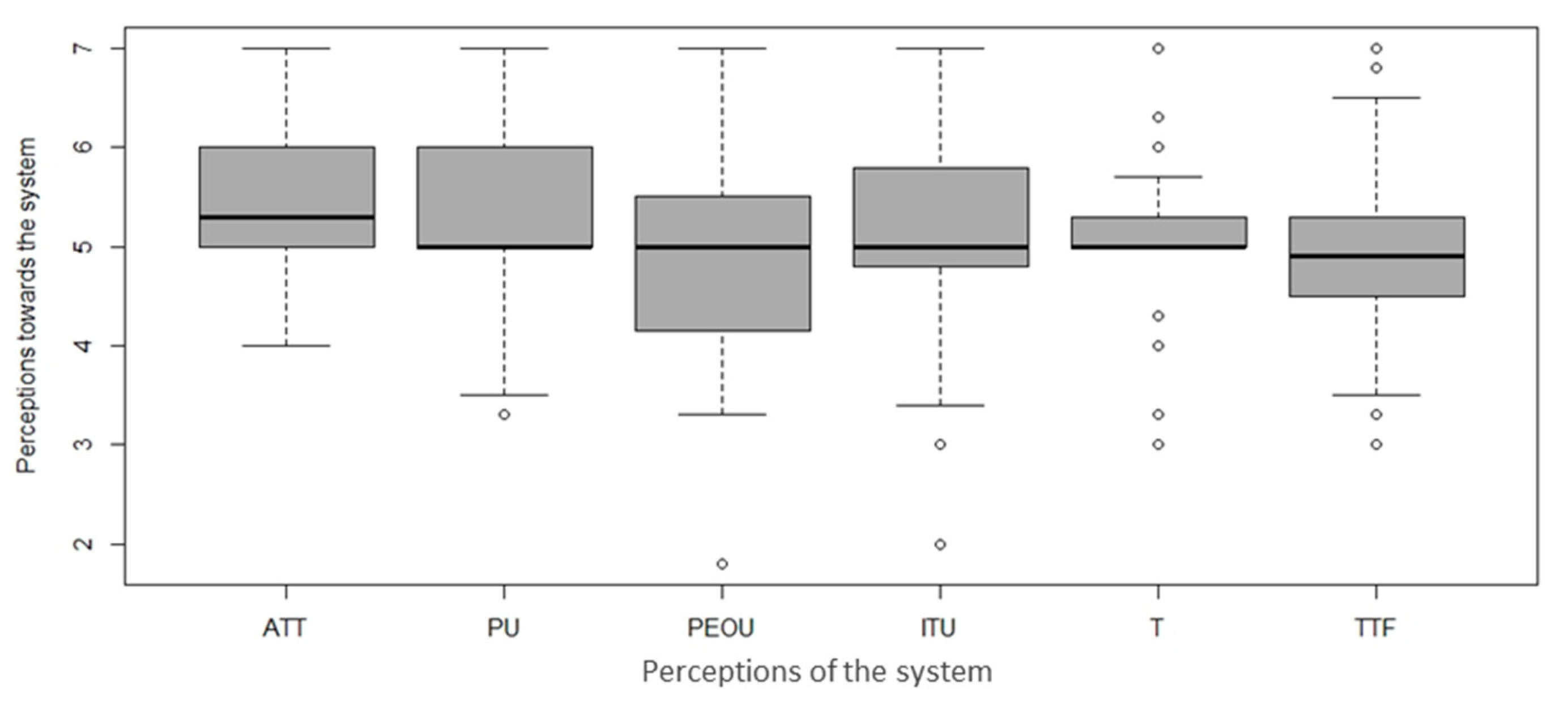
3.2. Feasibility
3.3. Sensor Data
3.4. Implications and Limitations
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| SD | Standard deviation |
| 3M-TUG | 3-m timed up and go |
| FTSTS | Five times sit o stand |
| BBS | Berg balance scale |
| IMU | Inertial measurement unit |
| AI | Artificial intelligence |
| PTs | Physiotherapists |
| BESTest | Balance evaluation systems test |
| ABC | Activities-specific balance confidence |
| MoCA | Montreal cognitive assessment |
| ATT | Attitude |
| PU | Perceived usefulness |
| PEOU | Perceived ease of use |
| ITU | Intention to use |
| T | Trust |
| TTF | Task–technology fit |
| OR | Odds ratio |
References
- Yu, L.; Zhao, Y.; Wang, H.; Sun, T.-L.; Murphy, T.E.; Tsui, K.-L. Assessing elderly’s functional balance and mobility via analyzing data from waist-mounted tri-axial wearable accelerometers in timed up and go tests. BMC Med. Inform. Decis. Mak. 2021, 21, 108. [Google Scholar] [CrossRef] [PubMed]
- Gillespie, L.D.; Robertson, M.C.; Gillespie, W.J.; Sherrington, C.; Gates, S.; Clemson, L.; Lamb, S.E. Interventions for preventing falls in older people living in the community. Cochrane Database Syst. Rev. 2012, 9, CD007146. [Google Scholar]
- Berg, K.; Wood-Dauphine, S.; Williams, J.I.; Gayton, D. Measuring balance in the elderly: Preliminary development of an instrument. Physiother. Can. 1989, 41, 304–311. [Google Scholar] [CrossRef]
- Schoene, D.; Wu, S.M.-S.; Mikolaizak, A.S.; Menant, J.C.; Smith, S.T.; Delbaere, K.; Lord, S.R. Discriminative ability and predictive validity of the timed up and go test in identifying older people who fall: Systematic review and meta-analysis. J. Am. Geriatr. Soc. 2013, 61, 202–208. [Google Scholar] [CrossRef] [PubMed]
- Trommelen, R.D.; Buttone, L.F.; Dicharry, D.Z.; Jacobs, R.M.; Karpinski, A. The Use of Five Repetition Sit to Stand Test to Assess Fall Risk in the Assisted Living Population. Phys. Occup. Ther. Geriatr. 2015, 33, 152–162. [Google Scholar] [CrossRef]
- Kim, S.; Kim, M.; Kim, N.; Kim, S.; Han, G. Quantification and Validity of Modified Romberg Tests Using Three-Axis Accelerometers. In Green and Smart Technology with Sensor Applications; Springer: Berlin/Heidelberg, Germany, 2012. [Google Scholar]
- Horak, F.B.; Wrisley, D.M.; Frank, J. The Balance Evaluation Systems Test (BESTest) to Differentiate Balance Deficits. Phys. Ther. 2009, 89, 484–498. [Google Scholar] [CrossRef] [PubMed]
- Physiotherapists Board, List of Registrants. Available online: www.smp-council.org.hk/pt/en/content.php?page=reg_reg (accessed on 9 August 2023).
- Sun, R.; Sosnoff, J.J. Novel sensing technology in fall risk assessment in older adults: A systematic review. BMC Geriatr. 2018, 18, 14. [Google Scholar] [CrossRef] [PubMed]
- Ghislieri, M.; Gastaldi, L.; Pastorelli, S.; Tadano, S.; Agostini, V. Wearable inertial sensors to assess standing balance: A systematic review. Sensors 2019, 19, 4075. [Google Scholar] [CrossRef]
- Hsu, Y.-C.; Wang, H.; Zhao, Y.; Chen, F.; Tsui, K.-L. Automatic recognition and analysis of balance activity in community-dwelling older adults: Algorithm validation. J. Med. Internet Res. 2021, 23, e30135. [Google Scholar] [CrossRef]
- Colagiorgio, P.; Romano, F.; Sardi, F.; Moraschini, M.; Sozzi, A.; Bejor, M.; Ricevuti, G.; Buizza, A.; Ramat, S. Affordable, automatic quantitative fall risk assessment based on clinical balance scales and Kinect data. In Proceedings of the 2014 36th Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Chicago, IL, USA, 26–30 August 2014; pp. 3500–3503. [Google Scholar]
- Kargar, B.A.H.; Mollahosseini, A.; Struemph, T.; Pace, W.; Nielsen, R.D.; Mahoor, M.H. Automatic measurement of physical mobility in Get-Up-and-Go Test using Kinect sensor. In Proceedings of the 2014 36th Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Chicago, IL, USA, 26–30 August 2014; pp. 3492–3495. [Google Scholar]
- Steffen, T.M.; Hacker, T.A.; Mollinger, L. Age- and Gender-Related Test Performance in Community-Dwelling Elderly People: Six-Minute Walk Test, Berg Balance Scale, Timed Up & Go Test, and Gait Speeds. Phys. Ther. 2002, 82, 128–137. [Google Scholar] [CrossRef]
- Shumway-Cook, A.; Brauer, S.; Woollacott, M. Predicting the probability for falls in community-dwelling older adults using the Timed Up & Go Test. Phys. Ther. 2000, 80, 896–903. [Google Scholar] [PubMed]
- Barry, E.; Galvin, R.; Keogh, C.; Horgan, F.; Fahey, T. Is the Timed Up and Go test a useful predictor of risk of falls in community dwelling older adults: A systematic review and meta- analysis. BMC Geriatr. 2014, 14, 14. [Google Scholar] [CrossRef]
- Weiss, A.; Herman, T.; Plotnik, M.; Brozgol, M.; Maidan, I.; Giladi, N.; Gurevich, T.; Hausdorff, J.M. Can an accelerometer enhance the utility of the Timed Up & Go Test when evaluating patients with Parkinson’s disease? Med. Eng. Phys. 2010, 32, 119–125. [Google Scholar] [PubMed]
- Sai, A.; Gallagher, J.C.; Smith, L.M.; Logsdon, S. Fall predictors in the community dwelling elderly: A cross sectional and prospective cohort study. J. Musculoskelet. Neuronal Interact. 2010, 10, 142–150. [Google Scholar] [PubMed]
- Crenshaw, J.R.; Bernhardt, K.A.; Atkinson, E.J.; Khosla, S.; Kaufman, K.R.; Amin, S. The relationships between compensatory stepping thresholds and measures of gait, standing postural control, strength, and balance confidence in older women. Gait Posture 2018, 65, 74–80. [Google Scholar] [CrossRef]
- Gras, L.Z.; Pohl, P.S.; Epidy, J.; Godin, B.; Hoessle, N. Use of the sharpened romberg as a screening for fall risk: A pilot study. Top. Geriatr. Rehabil. 2017, 33, 113–117. [Google Scholar] [CrossRef]
- Murray, N.; Salvatore, A.; Powell, D.; Reed-Jones, R. Reliability and validity evidence of multiple balance assessments in athletes with a concussion. J. Athl. Train. 2014, 49, 540–549. [Google Scholar] [CrossRef]
- Jácome, C.; Cruz, J.; Oliveira, A.; Marques, A. Validity, Reliability, and Ability to Identify Fall Status of the Berg Balance Scale, BESTest, Mini-BESTest, and Brief-BESTest in Patients With COPD. Phys. Ther. 2016, 96, 1807–1815. [Google Scholar] [CrossRef]
- Holbein-Jenny, M.A.; Billek-Sawhney, B.; Beckman, E.; Smith, T. Balance in personal care home residents: A comparison of the Berg Balance Scale, the Multi-Directional Reach Test, and the Activities-Specific Balance Confidence Scale. J. Geriatr. Phys. Ther. 2005, 28, 48–53. [Google Scholar] [CrossRef]
- Chou, C.-Y.; Chien, C.-W.; Hsueh, I.-P.; Sheu, C.-F.; Wang, C.-H.; Hsieh, C.-L. Developing a short form of the Berg Balance Scale for people with stroke. Phys. Ther. 2006, 86, 195–204. [Google Scholar] [CrossRef]
- Padgett, P.K.; Jacobs, J.V.; Kasser, S.L. Is the BESTest at its best? A suggested brief version based on interrater reliability, validity, internal consistency, and theoretical construct. Phys. Ther. 2012, 92, 1197–1207. [Google Scholar] [CrossRef] [PubMed]
- Montesinos, L.; Castaldo, R.; Pecchia, L. Wearable inertial sensors for fall risk assessment and prediction in older adults: A systematic review and meta-analysis. IEEE Trans. Neural Syst. Rehabil. Eng. 2018, 26, 573–582. [Google Scholar] [CrossRef] [PubMed]
- Howcroft, J.; Kofman, J.; Lemaire, E.D. Review of fall risk assessment in geriatric populations using inertial sensors. J. Neuroeng. Rehabil. 2013, 10, 91. [Google Scholar] [CrossRef] [PubMed]
- Muro-De-La-Herran, A.; Garcia-Zapirain, B.; Mendez-Zorrilla, A. Gait analysis methods: An overview of wearable and non-wearable systems, highlighting clinical applications. Sensors 2014, 14, 3362–3394. [Google Scholar] [CrossRef] [PubMed]
- Millor, N.; Lecumberri, P.; Gomez, M.; Martinez-Ramirez, A.; Izquierdo, M. Kinematic parameters to evaluate functional performance of sit-to-stand and stand-to-sit transitions using motion sensor devices: A systematic review. IEEE Trans. Neural Syst. Rehabil. Eng. 2014, 22, 926–936. [Google Scholar] [CrossRef]
- Sprint, G.; Cook, D.J.; Weeks, D.L. Toward automating clinical assessments: A survey of the timed up and go. IEEE Rev. Biomed. Eng. 2015, 8, 64–77. [Google Scholar] [CrossRef]
- Doi, T.; Hirata, S.; Ono, R.; Tsutsumimoto, K.; Misu, S.; Ando, H. The harmonic ratio of trunk acceleration predicts falling among older people: Results of a 1-year prospective study. J. Neuroeng. Rehabil. 2013, 10, 7. [Google Scholar] [CrossRef]
- Weiss, A.; Brozgol, M.; Dorfman, M.; Herman, T.; Shema, S.; Giladi, N.; Hausdorff, J.M. Does the evaluation of gait quality during daily life provide insight into fall risk? A novel approach using 3-day accelerometer recordings. Neurorehabilit. Neural Repair 2013, 27, 742–752. [Google Scholar] [CrossRef]
- Ejupi, A.; Brodie, M.; Gschwind, Y.J.; Lord, S.R.; Zagler, W.L.; Delbaere, K. Kinect-Based Five-Times-Sit-to-Stand Test for Clinical and In-Home Assessment of Fall Risk in Older People. Gerontology 2015, 62, 118–124. [Google Scholar] [CrossRef]
- Obdržálek, Š.; Kurillo, G.; Ofli, F.; Bajcsy, R.; Seto, E.; Jimison, H.; Pavel, M. Accuracy and robustness of Kinect pose estimation in the context of coaching of elderly population. In Proceedings of the 2012 Annual International Conference of the IEEE Engineering in Medicine and Biology Society, San Diego, CA, USA, 28 August–1 September 2012; pp. 1188–1193. [Google Scholar]
- Hoerl, A.E.; Kennard, R.W. Ridge regression: Biased estimation for nonorthogonal problems. Technometrics 1970, 12, 55–67. [Google Scholar] [CrossRef]
- Tibshirani, R. Regression shrinkage and selection via the lasso. J. R. Stat. Soc. Ser. B Methodol. 1996, 58, 267–288. [Google Scholar] [CrossRef]
- Hong Kong Christian Service. Elderly Core Business. Available online: http://www.hkcs.org/en/services/ecb (accessed on 25 May 2020).
- Powell, L.E.; Myers, A.M. The activities-specific balance confidence (ABC) scale. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 1995, 50, M28–M34. [Google Scholar] [CrossRef] [PubMed]
- Wong, A.; Xiong, Y.Y.; Kwan, P.W.; Chan, A.Y.; Lam, W.W.; Wang, K.; Chu, W.C.; Nyenhuis, D.L.; Nasreddine, Z.; Wong, L.K.; et al. The validity, reliability and clinical utility of the Hong Kong Montreal Cognitive Assessment (HK-MoCA) in patients with cerebral small vessel disease. Dement. Geriatr. Cogn. Disord. 2009, 28, 81–87. [Google Scholar] [CrossRef] [PubMed]
- Fan, X.; Zhao, Y.; Wang, H.; Tsui, K.L. Forecasting one-day-forward wellness conditions for community-dwelling elderly with single lead short electrocardiogram signals. BMC Med. Inform. Decis. Mak. 2019, 19, 285. [Google Scholar] [CrossRef] [PubMed]
- Huang, M.; Pang, M.Y.C. Psychometric properties of Brief-Balance Evaluation Systems Test (Brief-BESTest) in evaluating balance performance in individuals with chronic stroke. Brain Behav. 2017, 7, e00649. [Google Scholar] [CrossRef]
- Davis, F.D.; Bagozzi, R.P.; Warshaw, P.R. User acceptance of computer technology: A comparison of two theoretical models. Manag. Sci. 1989, 35, 982–1003. [Google Scholar] [CrossRef]
- Wang, H.; Tao, D.; Yu, N.; Qu, X. Understanding consumer acceptance of healthcare wearable devices: An integrated model of UTAUT and TTF. Int. J. Med. Inform. 2020, 139, 104156. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.K.; Ji, Y.G. Investigating the Importance of Trust on Adopting an Autonomous Vehicle. Int. J. Hum. Comput. Interact. 2015, 31, 692–702. [Google Scholar] [CrossRef]
- Venkatesh, V.; Morris, M.G.; Davis, G.B.; Davis, F.D. User Acceptance of Information Technology: Toward a Unified View. MIS Q. Manag. Inf. Syst. 2003, 27, 425–478. [Google Scholar] [CrossRef]
- Nasreddine, Z.S.; Phillips, N.A.; Bédirian, V.; Charbonneau, S.; Whitehead, V.; Collin, I.; Cummings, J.L.; Chertkow, H. The Montreal Cognitive Assessment, MoCA: A Brief Screening Tool For Mild Cognitive Impairment. J. Am. Geriatr. Soc. 2005, 53, 695–699. [Google Scholar] [CrossRef]
- Lajoie, Y.; Gallagher, S. Predicting falls within the elderly community: Comparison of postural sway, reaction time, the Berg balance scale and the Activities-specific Balance Confidence (ABC) scale for comparing fallers and non-fallers. Arch. Gerontol. Geriatr. 2004, 38, 11–26. [Google Scholar] [CrossRef] [PubMed]
- Davis, F. Perceived usefulness, perceived ease of use, and user acceptance of information technology. MIS Q. 1989, 13, 319–340. [Google Scholar] [CrossRef]
- Chen, K.; Chan, A.H. Predictors of gerontechnology acceptance by older Hong Kong Chinese. Technovation 2014, 34, 126–135. [Google Scholar] [CrossRef]
- Samuelson, W.; Zeckhauser, R. Status quo bias in decision making. J. Risk Uncertain. 1988, 1, 7–59. [Google Scholar] [CrossRef]
- Shany, T.; Redmond, S.; Marschollek, M.; Lovell, N. Assessing fall risk using wearable sensors: A practical discussion. Z. Gerontol. Geriatr. 2012, 45, 694–706. [Google Scholar] [CrossRef] [PubMed]
- Shany, T.; Redmond, S.J.; Narayanan, M.R.; Lovell, N.H. Sensors-based wearable systems for monitoring of human movement and falls. IEEE Sens. J. 2012, 12, 658–670. [Google Scholar] [CrossRef]
- Higashi, Y.; Yamakoshi, K.; Fujimoto, T.; Sekine, M.; Tamura, T. Quantitative evaluation of movement using the timed up-and-go test. IEEE Eng. Med. Biol. Mag. 2008, 27, 38–46. [Google Scholar] [CrossRef]
- Cheng, P.-T.; Wu, S.-H.; Liaw, M.-Y.; Wong, A.M.; Tang, F.-T. Symmetrical body-weight distribution training in stroke patients and its effect on fall prevention. Arch. Phys. Med. Rehabil. 2001, 82, 1650–1654. [Google Scholar] [CrossRef]
- Nuzik, S.; Lamb, R.; VanSant, A.; Hirt, S. Sit-to-stand movement pattern: A kinematic study. Phys. Ther. 1986, 66, 1708–1713. [Google Scholar] [CrossRef]
- Faria, C.D.C.d.M.; Saliba, V.A.; Teixeira-Salmela, L.F. Musculoskeletal biomechanics in sit-to-stand and stand-to-sit activities with stroke subjects: A systematic review. Fisioter. Mov. 2010, 23, 35–52. [Google Scholar] [CrossRef]
- Adusumilli, G.; Lancia, S.; Levasseur, V.A.; Amblee, V.; Orchard, M.; Wagner, J.M.; Naismith, R.T. Turning is an important marker of balance confidence and walking limitation in persons with multiple sclerosis. PLoS ONE 2018, 13, e0198178. [Google Scholar] [CrossRef] [PubMed]
- Peel, N.M.; Kuys, S.S.; Klein, K. Gait speed as a measure in geriatric assessment in clinical settings: A systematic review. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2013, 68, 39–46. [Google Scholar] [CrossRef] [PubMed]
- Clark, R.A.; Bower, K.J.; Mentiplay, B.F.; Paterson, K.; Pua, Y.-H. Concurrent validity of the Microsoft Kinect for assessment of spatiotemporal gait variables. J. Biomech. 2013, 46, 2722–2725. [Google Scholar] [CrossRef] [PubMed]
- Springer, S.; Yogev Seligmann, G. Validity of the Kinect for Gait Assessment: A Focused Review. Sensors 2016, 16, 194. [Google Scholar] [CrossRef] [PubMed]
- Clark, R.A.; Vernon, S.; Mentiplay, B.F.; Miller, K.J.; McGinley, J.L.; Pua, Y.H.; Paterson, K.; Bower, K.J. Instrumenting gait assessment using the Kinect in people living with stroke: Reliability and association with balance tests. J. Neuroeng. Rehabil. 2015, 12, 15. [Google Scholar] [CrossRef] [PubMed]
- Trojaniello, D.; Ravaschio, A.; Hausdorff, J.M.; Cereatti, A. Comparative assessment of different methods for the estimation of gait temporal parameters using a single inertial sensor: Application to elderly, post-stroke, Parkinson’s disease and Huntington’s disease subjects. Gait Posture 2015, 42, 310–316. [Google Scholar] [CrossRef]
- Zhou, H.; Stone, T.; Hu, H.; Harris, N. Use of multiple wearable inertial sensors in upper limb motion tracking. Med. Eng. Phys. 2008, 30, 123–133. [Google Scholar] [CrossRef]
- Tunca, C.; Pehlivan, N.; Ak, N.; Arnrich, B.; Salur, G.; Ersoy, C. Inertial Sensor-Based Robust Gait Analysis in Non-Hospital Settings for Neurological Disorders. Sensors 2017, 17, 825. [Google Scholar] [CrossRef]
- Mihailovic, A.; De Luna, R.M.; West, S.K.; Friedman, D.S.; Gitlin, L.N.; Ramulu, P.Y. Gait and Balance as Predictors and/or Mediators of Falls in Glaucoma. Investig. Opthalmol. Vis. Sci. 2020, 61, 30. [Google Scholar] [CrossRef]
- Dorsey, E.R.; Topol, E.J. State of Telehealth. N. Engl. J. Med. 2016, 375, 154–161. [Google Scholar] [CrossRef]
- Kvedar, J.; Coye, M.J.; Everett, W. Connected health: A review of technologies and strategies to improve patient care with telemedicine and telehealth. Health Aff. 2014, 33, 194–199. [Google Scholar] [CrossRef]

| Numerical Variables | Mean (SD) | Median | Range |
|---|---|---|---|
| Age, years | 78.5 (6.2) | 78.0 | 68.0–88.0 |
| Stature, cm | 153.5 (7.3) | 153.0 | 137.0–175.0 |
| Body weight, kg | 57 (10.8) | 57.8 | 33.8–79.7 |
| Body mass index, kg/m2 | 24.2 (4) | 24.1 | 15.6–35.9 |
| Health index (1–5) | 3.7 (1.1) | 4.0 | 1–5 |
| MoCA (0–30) | 22.9 (4) | 23.0 | 12–29 |
| ABC (0–100%) | 54.5 (29.8) | 61.3 | 0–96.9 |
| BBS (0–56) | 48.0 (7.1) | 49.0 | 22–56 |
| Brief-BESTest (0–24) | 14.5 (4.5) | 16.0 | 1–21 |
| Categorical variables | Number, n (%) | ||
| Female gender | 38 (86.4%) | ||
| Chronic disease | |||
| Hypertension | 33 (75.0%) | ||
| Diabetes mellitus | 8 (18.2%) | ||
| Heart disease | 9 (20.5%) | ||
| Fracture | 6 (13.6%) | ||
| Arthritis | 27 (61.4%) | ||
| Cataract | 26 (59.1%) | ||
| Rheumatic pain | 22 (50.0%) | ||
| Fall history in the past 12 months | 17 (38.6%) | ||
| One fall | 12 (27.3%) | ||
| Two falls | 3 (6.8%) | ||
| Three falls | 2 (4.5%) | ||
| Walking assistance (Yes) | 14 (31.8%) |
| Demographic | Positive Attitude | Perceived Usefulness | Perceived Ease of Use | Intention to Use | Trust | Task–Technology Fit |
|---|---|---|---|---|---|---|
| Age | 1.03 (0.92, 1.16) | 1.1 (0.97, 1.24) | 1.08 (0.96, 1.21) | 1.05 (0.93, 1.18) | 1.11 (0.97, 1.26) | 0.95 (0.85, 1.07) |
| Male a | 3.99 (0.4, 40.15) | 2.84 (0.29, 28.31) | 2 (0.21, 18.76) | 2.09 (0.23, 19.49) | 0.92 (0.08, 10.33) | 4.01 (0.41, 38.97) |
| Chronic disease b | ||||||
| Hypertension | 0.76 (0.17, 3.55) | 7.17 (1.42, 36.06) * | 4.51 (0.96, 21.26) | 2.08 (0.46, 9.39) | 2.08 (0.39, 11.21) | 1.76 (0.39, 7.92) |
| Diabetes mellitus | 0.8 (0.16, 4.13) | 0.67 (0.13, 3.5) | 1.24 (0.25, 6.23) | 0.58 (0.12, 2.88) | 2.08 (0.34, 12.73) | 0.57 (0.11, 2.88) |
| Heart disease | 0.36 (0.08, 1.58) | 0.33 (0.07, 1.45) | 1.05 (0.25, 4.44) | 0.42 (0.1, 1.79) | 0.6 (0.12, 2.91) | 0.59 (0.14, 2.51) |
| Fracture | 0.46 (0.07, 3.25) | 0.9 (0.13, 6.27) | 13.04 (1.55, 109.86) * | 0.74 (0.11, 5.01) | 1.89 (0.24, 15.24) | 15.89 (2, 126.39) ** |
| Arthritis | 2.49 (0.43, 14.48) | 0.59 (0.1, 3.34) | 0.27 (0.05, 1.55) | 0.39 (0.07, 2.12) | 0.71 (0.11, 4.48) | 0.61 (0.11, 3.37) |
| Cataract | 2.89 (0.74, 11.39) | 1.9 (0.49, 7.37) | 4.5 (1.14, 17.72) * | 3.03 (0.79, 11.59) | 1.28 (0.3, 5.43) | 2.84 (0.74, 10.86) |
| Rheumatic pain | 0.23 (0.04, 1.18) | 0.69 (0.14, 3.38) | 1.14 (0.24, 5.41) | 1.07 (0.23, 5.05) | 0.38 (0.07, 2.15) | 1.36 (0.29, 6.49) |
| Falls c | 0.39 (0.08, 2.05) | 1.81 (0.35, 9.36) | 1.32 (0.26, 6.78) | 0.59 (0.12, 2.92) | 0.89 (0.15, 5.19) | 0.38 (0.08, 1.95) |
| Walking aids d | 2.23 (0.45, 10.94) | 8.66 (1.6, 46.8) * | 5.86 (1.15, 29.93) * | 2.5 (0.53, 11.74) | 8.43 (1.37, 51.94) * | 1.57 (0.33, 7.42) |
| ABC score | 1.01 (0.99, 1.04) | 1.02 (0.99, 1.05) | 1.03 (1, 1.05) * | 1.02 (0.99, 1.04) | 1.02 (1, 1.05) | 1.04 (1.01, 1.06) ** |
| MoCA score | 1.17 (0.97, 1.4) | 1.28 (1.06, 1.54) * | 1.23 (1.02, 1.47) * | 1.1 (0.92, 1.31) | 1.25 (1.03, 1.53) * | 1.4 (1.15, 1.71) ** |
| Health index | 0.99 (0.49, 1.98) | 0.83 (0.42, 1.67) | 0.95 (0.48, 1.88) | 1.14 (0.58, 2.24) | 0.67 (0.31, 1.47) | 1 (0.5, 1.98) |
| Stature | 0.68 (0.3, 1.54) | 0.7 (0.31, 1.59) | 0.51 (0.22, 1.15) | 1.02 (0.46, 2.24) | 0.62 (0.26, 1.48) | 0.87 (0.39, 1.93) |
| Body weight | 1.62 (0.55, 4.77) | 1.52 (0.52, 4.49) | 2.29 (0.78, 6.72) | 0.99 (0.35, 2.83) | 1.92 (0.61, 6.04) | 1.17 (0.41, 3.36) |
| Body mass index | 0.34 (0.03, 3.75) | 0.39 (0.03, 4.38) | 0.16 (0.02, 1.8) | 0.95 (0.09, 9.83) | 0.27 (0.02, 3.4) | 0.85 (0.08, 8.89) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhao, Y.; Yu, L.; Fan, X.; Pang, M.Y.C.; Tsui, K.-L.; Wang, H. Design of a Sensor-Technology-Augmented Gait and Balance Monitoring System for Community-Dwelling Older Adults in Hong Kong: A Pilot Feasibility Study. Sensors 2023, 23, 8008. https://doi.org/10.3390/s23188008
Zhao Y, Yu L, Fan X, Pang MYC, Tsui K-L, Wang H. Design of a Sensor-Technology-Augmented Gait and Balance Monitoring System for Community-Dwelling Older Adults in Hong Kong: A Pilot Feasibility Study. Sensors. 2023; 23(18):8008. https://doi.org/10.3390/s23188008
Chicago/Turabian StyleZhao, Yang, Lisha Yu, Xiaomao Fan, Marco Y. C. Pang, Kwok-Leung Tsui, and Hailiang Wang. 2023. "Design of a Sensor-Technology-Augmented Gait and Balance Monitoring System for Community-Dwelling Older Adults in Hong Kong: A Pilot Feasibility Study" Sensors 23, no. 18: 8008. https://doi.org/10.3390/s23188008
APA StyleZhao, Y., Yu, L., Fan, X., Pang, M. Y. C., Tsui, K.-L., & Wang, H. (2023). Design of a Sensor-Technology-Augmented Gait and Balance Monitoring System for Community-Dwelling Older Adults in Hong Kong: A Pilot Feasibility Study. Sensors, 23(18), 8008. https://doi.org/10.3390/s23188008










