Use of a Wearable Biosensor to Study Heart Rate Variability in Chronic Obstructive Pulmonary Disease and Its Relationship to Disease Severity
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Heart Rate Variability
2.3. Other Measurements
2.4. Statistical Analysis
3. Results
3.1. Baseline Characteristics
3.2. HRV and COPD Severity
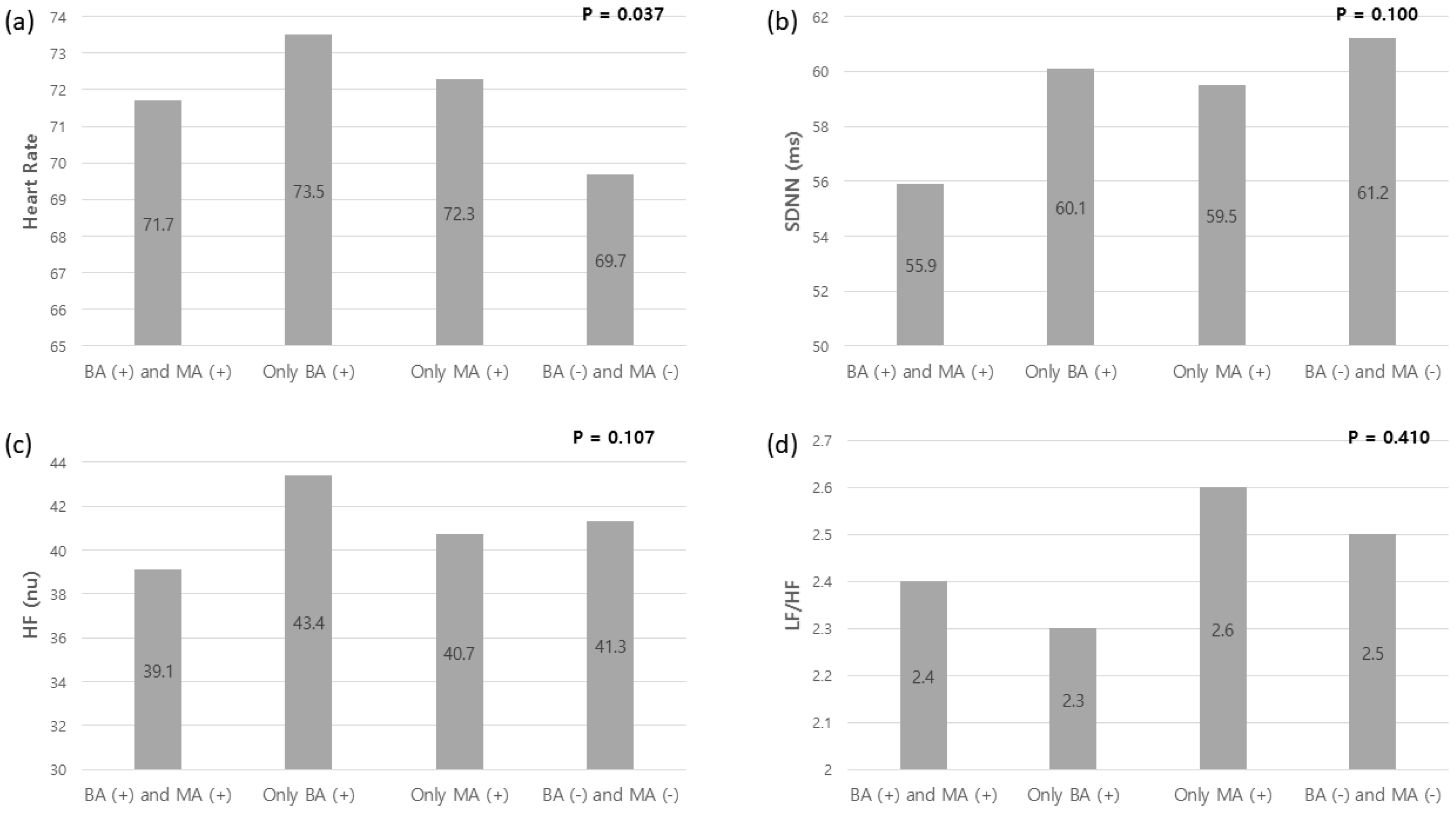
3.3. HRV and COPD Medications (Beta-Sympathomimetic Agonists and Muscarinic Antagonists)
3.4. Correlation between HRV and Patient Reported Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Heart Rate Variability: Standards of Measurement, Physiological Interpretation and Clinical Use. Circulation 1996, 93, 1043–1065. [Google Scholar] [CrossRef]
- Benichou, T.; Pereira, B.; Mermillod, M.; Tauveron, I.; Pfabigan, D.; Maqdasy, S.; Dutheil, F. Heart rate variability in type 2 diabetes mellitus: A systematic review and meta-analysis. PLoS ONE 2018, 13, e0195166. [Google Scholar] [CrossRef]
- Oikawa, K.; Ishihara, R.; Maeda, T.; Yamaguchi, K.; Koike, A.; Kawaguchi, H.; Tabata, Y.; Murotani, N.; Itoh, H. Prognostic value of heart rate variability in patients with renal failure on hemodialysis. Int. J. Cardiol. 2009, 131, 370–377. [Google Scholar] [CrossRef]
- Oyelade, T.; Canciani, G.; Carbone, G.; Alqahtani, J.S.; Moore, K.; Mani, A.R. Heart rate variability in patients with cirrhosis: A systematic review and meta-analysis. Physiol. Meas. 2021, 42. [Google Scholar] [CrossRef]
- Kloter, E.; Barrueto, K.; Klein, S.D.; Scholkmann, F.; Wolf, U. Heart Rate Variability as a Prognostic Factor for Cancer Survival—A Systematic Review. Front Physiol. 2018, 9, 623. [Google Scholar] [CrossRef]
- Sgoifo, A.; Carnevali, L.; Alfonso Mde, L.; Amore, M. Autonomic dysfunction and heart rate variability in depression. Stress 2015, 18, 343–352. [Google Scholar] [CrossRef]
- Tsuji, H.; Larson, M.G.; Venditti, F.J., Jr.; Manders, E.S.; Evans, J.C.; Feldman, C.L.; Levy, D. Impact of reduced heart rate variability on risk for cardiac events. The Framingham Heart Study. Circulation 1996, 94, 2850–2855. [Google Scholar] [CrossRef]
- Tsuji, H.; Venditti, F.J., Jr.; Manders, E.S.; Evans, J.C.; Larson, M.G.; Feldman, C.L.; Levy, D. Reduced heart rate variability and mortality risk in an elderly cohort. The Framingham Heart Study. Circulation 1994, 90, 878–883. [Google Scholar] [CrossRef]
- Global Initiative for Chronic Obstructive Lung Disease. 2021 Global Strategy for Prevention, Diagnosis, and Management of COPD. Available online: https://goldcopd.org/2021-gold-reports (accessed on 28 July 2021).
- World Health Organization. Global Health Estimates: Life Expectancy and Leading Causes of Death and Disability. Available online: https://www.who.int/data/gho/data/themes/mortality-and-global-health-estimates (accessed on 28 July 2021).
- Volterrani, M.; Scalvini, S.; Mazzuero, G.; Lanfranchi, P.; Colombo, R.; Clark, A.L.; Levi, G. Decreased heart rate variability in patients with chronic obstructive pulmonary disease. Chest 1994, 106, 1432–1437. [Google Scholar] [CrossRef]
- Gunduz, H.; Talay, F.; Arinc, H.; Ozyildirim, S.; Akdemir, R.; Yolcu, M.; Kanat, M.; Uyan, C. Heart rate variability and heart rate turbulence in patients with chronic obstructive pulmonary disease. Cardiol. J. 2009, 16, 553–559. [Google Scholar]
- Zupanic, E.; Zivanovic, I.; Kalisnik, J.M.; Avbelj, V.; Lainscak, M. The effect of 4-week rehabilitation on heart rate variability and QTc interval in patients with chronic obstructive pulmonary disease. COPD 2014, 11, 659–669. [Google Scholar] [CrossRef]
- Borghi-Silva, A.; Reis, M.S.; Mendes, R.G.; Pantoni, C.B.; Simões, R.P.; Martins, L.E.; Catai, A.M. Noninvasive ventilation acutely modifies heart rate variability in chronic obstructive pulmonary disease patients. Respir. Med. 2008, 102, 1117–1123. [Google Scholar] [CrossRef]
- Ferguson, G.T.; Make, B. Stable COPD: Initial Pharmacologic Management. UpToDate. 2019. Available online: https://www.uptodate.com/contents/stable-copd-initial-pharmacologic-management (accessed on 24 February 2022).
- Lee, S.Y.; Lee, J.S.; Lee, S.W.; Oh, Y.M. Effects of treatment with long-acting muscarinic antagonists (LAMA) and long-acting beta-agonists (LABA) on lung function improvement in patients with bronchiectasis: An observational study. J. Thorac. Dis. 2021, 13, 169–177. [Google Scholar] [CrossRef]
- Liu, B.; Zan, S.; Luo, W. Safety evaluation of revefenacin at the approved dose in patients with chronic obstructive pulmonary disease: A meta-analysis. Heart Lung 2021, 52, 52–60. [Google Scholar] [CrossRef]
- Cekici, L.; Valipour, A.; Kohansal, R.; Burghuber, O.C. Short-term effects of inhaled salbutamol on autonomic cardiovascular control in healthy subjects: A placebo-controlled study. Br. J. Clin. Pharmacol. 2009, 67, 394–402. [Google Scholar] [CrossRef]
- Eryonucu, B.; Uzun, K.; Güler, N.; Bilge, M. Comparison of the acute effects of salbutamol and terbutaline on heart rate variability in adult asthmatic patients. Eur. Respir. J. 2001, 17, 863–867. [Google Scholar] [CrossRef]
- Bédard, M.E.; Marquis, K.; Poirier, P.; Provencher, S. Reduced heart rate variability in patients with chronic obstructive pulmonary disease independent of anticholinergic or β-agonist medications. COPD 2010, 7, 391–397. [Google Scholar] [CrossRef]
- Chhabra, S.K.; De, S. Cardiovascular autonomic neuropathy in chronic obstructive pulmonary disease. Respir. Med. 2005, 99, 126–133. [Google Scholar] [CrossRef][Green Version]
- Antonelli Incalzi, R.; Corsonello, A.; Trojano, L.; Pedone, C.; Acanfora, D.; Spada, A.; D’Addio, G.; Maestri, R.; Rengo, F.; Rengo, G. Heart rate variability and drawing impairment in hypoxemic COPD. Brain Cogn. 2009, 70, 163–170. [Google Scholar] [CrossRef]
- Tug, T.; Terzi, S.M.; Yoldas, T.K. Relationship between the frequency of autonomic dysfunction and the severity of chronic obstructive pulmonary disease. Acta Neurol. Scand. 2005, 112, 183–188. [Google Scholar] [CrossRef]
- Camillo, C.A.; Pitta, F.; Possani, H.V.; Barbosa, M.V.; Marques, D.S.; Cavalheri, V.; Probst, V.S.; Brunetto, A.F. Heart rate variability and disease characteristics in patients with COPD. Lung 2008, 186, 393–401. [Google Scholar] [CrossRef]
- Chan, M.; Estève, D.; Fourniols, J.Y.; Escriba, C.; Campo, E. Smart wearable systems: Current status and future challenges. Artif. Intell. Med. 2012, 56, 137–156. [Google Scholar] [CrossRef]
- Dolezal, B.A.; Boland, D.M.; Carney, J.; Abrazado, M.; Smith, D.L.; Cooper, C.B. Validation of heart rate derived from a physiological status monitor-embedded compression shirt against criterion ECG. J. Occup. Environ. Hyg. 2014, 11, 833–839. [Google Scholar] [CrossRef]
- Nazari, G.; Bobos, P.; MacDermid, J.C.; Sinden, K.E.; Richardson, J.; Tang, A. Psychometric properties of the Zephyr bioharness device: A systematic review. BMC Sports Sci. Med. Rehabil. 2018, 10, 6. [Google Scholar] [CrossRef]
- Miller, M.R.; Crapo, R.; Hankinson, J.; Brusasco, V.; Burgos, F.; Casaburi, R.; Coates, A.; Enright, P.; van der Grinten, C.P.; Gustafsson, P.; et al. General considerations for lung function testing. Eur. Respir. J. 2005, 26, 153–161. [Google Scholar] [CrossRef]
- Mahler, D.A.; Ward, J.; Fierro-Carrion, G.; Waterman, L.A.; Lentine, T.F.; Mejia-Alfaro, R.; Baird, J.C. Development of self-administered versions of modified baseline and transition dyspnea indexes in COPD. COPD 2004, 1, 165–172. [Google Scholar] [CrossRef]
- Myers, J.; Bader, D.; Madhavan, R.; Froelicher, V. Validation of a specific activity questionnaire to estimate exercise tolerance in patients referred for exercise testing. Am. Heart J. 2001, 142, 1041–1046. [Google Scholar] [CrossRef]
- Ware, J., Jr.; Kosinski, M.; Keller, S.D. A 12-Item Short-Form Health Survey: Construction of scales and preliminary tests of reliability and validity. Med. Care 1996, 34, 220–233. [Google Scholar] [CrossRef]
- Meguro, M.; Barley, E.A.; Spencer, S.; Jones, P.W. Development and Validation of an Improved, COPD-Specific Version of the St. George Respiratory Questionnaire. Chest 2007, 132, 456–463. [Google Scholar] [CrossRef]
- Jones, P.W.; Harding, G.; Berry, P.; Wiklund, I.; Chen, W.H.; Kline Leidy, N. Development and first validation of the COPD Assessment Test. Eur. Respir. J. 2009, 34, 648–654. [Google Scholar] [CrossRef]
- ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories. ATS statement: Guidelines for the six-minute walk test. Am. J. Respir. Crit. Care Med. 2002, 166, 111–117. [Google Scholar] [CrossRef]
- Celli, B.R.; Cote, C.G.; Marin, J.M.; Casanova, C.; Montes de Oca, M.; Mendez, R.A.; Pinto Plata, V.; Cabral, H.J. The body-mass index, airflow obstruction, dyspnea, and exercise capacity index in chronic obstructive pulmonary disease. N. Engl. J. Med. 2004, 350, 1005–1012. [Google Scholar] [CrossRef]
- Akoglu, H. User’s guide to correlation coefficients. Turk. J. Emerg. Med. 2018, 18, 91–93. [Google Scholar] [CrossRef]
- Bartels, M.N.; Jelic, S.; Ngai, P.; Basner, R.C.; DeMeersman, R.E. High-frequency modulation of heart rate variability during exercise in patients with COPD. Chest 2003, 124, 863–879. [Google Scholar] [CrossRef]
- Camillo, C.A.; Laburu Vde, M.; Gonçalves, N.S.; Cavalheri, V.; Tomasi, F.P.; Hernandes, N.A.; Ramos, D.; Marquez Vanderlei, L.C.; Cipulo Ramos, E.M.; Probst, V.S.; et al. Improvement of heart rate variability after exercise training and its predictors in COPD. Respir. Med. 2011, 105, 1054–1062. [Google Scholar] [CrossRef]
- Ricci-Vitor, A.L.; Bonfim, R.; Fosco, L.C.; Bertolini, G.N.; Ramos, E.M.; Ramos, D.; Pastre, C.M.; Godoy, M.; Vanderlei, L.C. Influence of the resistance training on heart rate variability, functional capacity and muscle strength in the chronic obstructive pulmonary disease. Eur. J. Phys. Rehabil. Med. 2013, 49, 793–801. [Google Scholar]
- Leite, M.R.; Ramos, E.M.; Kalva-Filho, C.A.; Rodrigues, F.M.; Freire, A.P.; Tacao, G.Y.; de Toledo, A.C.; Cecílio, M.J.; Vanderlei, L.C.; Ramos, D. Correlation between heart rate variability indexes and aerobic physiological variables in patients with COPD. Respirology 2015, 20, 273–278. [Google Scholar] [CrossRef]
- Goulart Cda, L.; Simon, J.C.; Schneiders Pde, B.; San Martin, E.A.; Cabiddu, R.; Borghi-Silva, A.; Trimer, R.; da Silva, A.L. Respiratory muscle strength effect on linear and nonlinear heart rate variability parameters in COPD patients. Int. J. Chron. Obstruct. Pulmon. Dis. 2016, 11, 1671–1677. [Google Scholar] [CrossRef]
- Skorodin, M.S. Beta-adrenergic agonists. A problem. Chest 1993, 103, 1587–1590. [Google Scholar] [CrossRef]
- Salpeter, S.R.; Ormiston, T.M.; Salpeter, E.E. Cardiovascular effects of beta-agonists in patients with asthma and COPD: A meta-analysis. Chest 2004, 125, 2309–2321. [Google Scholar] [CrossRef]
- Sears, M.R. Adverse effects of beta-agonists. J. Allergy Clin. Immunol. 2002, 110 (Suppl. 6), S322–S328. [Google Scholar] [CrossRef] [PubMed]
- de Geus, E.J.C.; Gianaros, P.J.; Brindle, R.C.; Jennings, J.R.; Berntson, G.G. Should heart rate variability be “corrected” for heart rate? Biological, quantitative, and interpretive considerations. Psychophysiology 2019, 56, e13287. [Google Scholar] [CrossRef] [PubMed]
- Mathers, C.D.; Loncar, D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006, 3, e442. [Google Scholar] [CrossRef]
- Li, L.S.K.; Butler, S.; Goldstein, R.; Brooks, D. Comparing the impact of different exercise interventions on fatigue in individuals with COPD: A systematic review and meta-analysis. Chron. Respir. Dis. 2019, 16, 1479973119894855. [Google Scholar] [CrossRef]
- Cooper, C.B.; Sirichana, W.; Arnold, M.T.; Neufeld, E.V.; Taylor, M.; Wang, X.; Dolezal, B.A. Remote Patient Monitoring for the Detection of COPD Exacerbations. Int. J. Chron. Obstruct. Pulmon. Dis. 2020, 15, 2005–2013. [Google Scholar] [CrossRef]
- Goldhill, D.R.; McNarry, A.F.; Mandersloot, G.; McGinley, A. A physiologically-based early warning score forward patients: The association between score and outcome. Anaesthesia 2005, 60, 547–553. [Google Scholar] [CrossRef]
- Izmailova, E.S.; Wagner, J.A.; Perakslis, E.D. Wearable Devices in Clinical Trials: Hype and Hypothesis. Clin. Pharmacol. Ther. 2018, 104, 42–52. [Google Scholar] [CrossRef]
- Tiwari, A.; Liaqat, S.; Liaqat, D.; Gabel, M.; de Lara, E.; Falk, T.H. Remote COPD Severity and Exacerbation Detection Using Heart Rate and Activity Data Measured from a Wearable Device. In Proceedings of the Annual International Conference of the IEEE Engineering in Medicine & Biology Society, Guadalajara, Mexico, 1–5 November 2021; pp. 7450–7454. [Google Scholar]
- Rutkowski, S.; Buekers, J.; Rutkowska, A.; Cieślik, B.; Szczegielniak, J. Monitoring Physical Activity with a Wearable Sensor in Patients with COPD during In-Hospital Pulmonary Rehabilitation Program: A Pilot Study. Sensors 2021, 21, 2742. [Google Scholar] [CrossRef]
- Tseng, C.Y.; Chang, J.C.; Chen, Y.C.; Huang, H.H.; Lin, C.S.; How, C.K.; Yen, D.H. Changes of heart rate variability predicting patients with acute exacerbation of chronic obstructive pulmonary disease requiring hospitalization after Emergency Department treatment. J. Chin. Med. Assoc. 2018, 81, 47–52. [Google Scholar] [CrossRef]
- Zamarrón, C.; Lado, M.J.; Teijeiro, T.; Morete, E.; Vila, X.A.; Lamas, P.F. Heart rate variability in patients with severe chronic obstructive pulmonary disease in a home care program. Technol. Health Care 2014, 22, 91–98. [Google Scholar] [CrossRef]
- Mohammed, J.; Meeus, M.; Derom, E.; Da Silva, H.; Calders, P. Evidence for Autonomic Function and Its Influencing Factors in Subjects With COPD: A Systematic Review. Respir. Care 2015, 60, 1841–1851. [Google Scholar] [CrossRef] [PubMed]
| Total COPD (n = 79) | |
|---|---|
| Age (years) | 70.6 ± 7.2 |
| Male n (%) | 48 (60.0) |
| Smoking (pack-years) | 47.6 ± 30.5 |
| BMI (kg/m2) | 27.3 ± 5.1 |
| FVC (% reference) | 88.7 ± 20.6 |
| FEV1 (% reference) | 62.7 ± 23.1 |
| FEV1/FVC | 52.0 ± 14.3 |
| Health status questionnaires | |
| mMRC (0–4) | 1.2 ± 1.1 |
| VSAQ (1–13) | 5.5 ± 3.0 |
| SF-12 (0–100) | 64.4 ± 23.5 |
| SGRQ (0–100) | 32.7 ± 23.4 |
| CAT (0–40) | 13.6 ± 8.9 |
| 6MWD (m) | 381.6 ± 133.8 |
| Maximal handgrip strength (kg) | 28.5 ± 9.9 |
| Home oxygen | 6 (7.6) |
| Comorbidities n (%) | |
| Cardiovascular disease | 47 (58.8) |
| Asthma | 17 (21.3) |
| Cancer | 22 (27.5) |
| Medications n (%) | |
| SABA | 43 (53.8) |
| LABA | 2 (2.5) |
| LAMA | 26 (32.5) |
| ICS | 6 (7.5) |
| LABA/LAMA | 4 (5.0) |
| LABA/ICS | 27 (33.8) |
| LABA/LAMA/ICS | 7 (8.8) |
| PDE4 inhibitor | 2 (2.5) |
| HRV | |
| HR (/min) | 71.4 ± 3.3 |
| SDNN (ms) | 58.5 ± 8.1 |
| HFn (normalized units) | 40.3 ± 5.2 |
| LF/HF | 2.4 ± 0.5 |
| Grade 0 (n = 4) | Grade 1 (n = 16) | Grade 2 (n = 30) | Grade 3 (n = 23) | Grade 4 (n = 6) | p Value | |
|---|---|---|---|---|---|---|
| HR (min) | 68.3 ± 1.9 | 71.2 ± 3.3 | 71.8 ± 3.3 | 71.7 ± 3.8 | 71.4 ± 1.2 | 0.305 |
| SDNN (ms) | 58.6 ± 10.4 | 62.3 ± 5.1 | 56.1 ± 9.1 | 58.1 ± 8.3 | 61.6 ± 2.9 | 0.184 |
| HF (normalized units) | 41.1 ± 0.3 | 42.7 ± 4.8 | 39.9 ± 5.6 | 39.5 ± 5.3 | 38.8 ± 5.4 | 0.121 |
| LF/HF | 2.3 ± 0.1 | 2.5 ± 0.3 | 2.5 ± 0.6 | 2.2 ± 0.5 | 2.3 ± 0.4 | 0.205 |
| HR | SDNN | HF | LF/HF | |
|---|---|---|---|---|
| Smoking (pack-years) | 0.020 | 0.031 | −0.080 | −0.182 |
| BMI (kg/m2) | −0.144 | 0.103 | 0.140 | −0.132 |
| % FVC (% reference) | −0.060 | 0.049 | 0.045 | 0.205 |
| % FEV1 (% reference) | −0.129 | 0.059 | 0.108 | 0.151 |
| Health status questionnaires | ||||
| mMRC (0–4) | 0.169 | −0.234 * | −0.184 | −0.081 |
| VSAQ (1–13) | −0.241 * | 0.308 ** | 0.269 * | 0.101 |
| SF-12 (0–100) | −0.229 * | 0.194 | 0.251 * | 0.236 * |
| SGRQ (0–100) | 0.155 | −0.298 ** | −0.290 ** | −0.027 |
| CAT (0–40) | 0.151 | −0.280 * | −0.221 | 0.065 |
| 6MWD (m) | −0.272 * | 0.207 | 0.160 | 0.010 |
| Handgrip strength (kg) | −0.294 ** | 0.285* | 0.184 | −0.029 |
| BODE index | 0.140 | −0.269 * | −0.248 * | −0.081 |
| Selected Studies | Age (Years) | FEV1 (%) | SDNN (ms) | HF (nu) | HF/LF | Principal Outcomes |
|---|---|---|---|---|---|---|
| Bédard, et al. (n = 41) | 67 | 45 | NA | NA | 1.9 | HRV correlated with disease severity and did not seem to be influenced by anticholinergic or adrenergic medications. |
| Camillo, et al. (n = 31) | 66 | 46 | 33 | 55 | NA | HRV was not related to disease severity but mainly to the level of physical activity in daily life. |
| Bartels, et al. (n = 53) | 61 | 35 | NA | NA | 3.1 | The balance of sympathetic to parasympathetic cardiac modulation decreased in patients with COPD during maximal volitional exercise. |
| Camillo, et al. (n = 20) | 67 | 40 | 29 | 56 | 0.9 | High-intensity exercise training improved HRV at rest and during orthostatic stimulus in patients with COPD. |
| Ricci-Vitor, et al. (n = 13) | 67 | 48.3 | 17 | NA | NA | The exclusive resistance training improved sympathetic and parasympathetic components of autonomic nervous system representing by SDNN, LF, and HF. |
| Zupanic, et al. (n = 31) | 61 | NA | 24 | 45 | 1.8 | A 4-week rehabilitation improved HRV (SDNN). |
| Leite et al. (n = 37) | 63 | 46 | 20 | 37 | 1.7 | HRV indexes at rest was correlated with aerobic physiological variables obtained at a maximal exercise test. |
| Goulart, et al. (n = 10) | 61 | 32 | NA | 54 | 0.9 | COPD patients with impaired respiratory muscle strength showed marked sympathetic modulation and a reduced parasympathetic response; reduced HRV complexity was observed during a respiratory sinus arrhythmia maneuver. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Park, S.-C.; Saiphoklang, N.; Jung, D.; Gomez, D.; Phillips, J.E.; Dolezal, B.A.; Tashkin, D.P.; Barjaktarevic, I.; Cooper, C.B. Use of a Wearable Biosensor to Study Heart Rate Variability in Chronic Obstructive Pulmonary Disease and Its Relationship to Disease Severity. Sensors 2022, 22, 2264. https://doi.org/10.3390/s22062264
Park S-C, Saiphoklang N, Jung D, Gomez D, Phillips JE, Dolezal BA, Tashkin DP, Barjaktarevic I, Cooper CB. Use of a Wearable Biosensor to Study Heart Rate Variability in Chronic Obstructive Pulmonary Disease and Its Relationship to Disease Severity. Sensors. 2022; 22(6):2264. https://doi.org/10.3390/s22062264
Chicago/Turabian StylePark, Seon-Cheol, Narongkorn Saiphoklang, Donghyun Jung, David Gomez, Jonathan E. Phillips, Brett A. Dolezal, Donald P. Tashkin, Igor Barjaktarevic, and Christopher B. Cooper. 2022. "Use of a Wearable Biosensor to Study Heart Rate Variability in Chronic Obstructive Pulmonary Disease and Its Relationship to Disease Severity" Sensors 22, no. 6: 2264. https://doi.org/10.3390/s22062264
APA StylePark, S.-C., Saiphoklang, N., Jung, D., Gomez, D., Phillips, J. E., Dolezal, B. A., Tashkin, D. P., Barjaktarevic, I., & Cooper, C. B. (2022). Use of a Wearable Biosensor to Study Heart Rate Variability in Chronic Obstructive Pulmonary Disease and Its Relationship to Disease Severity. Sensors, 22(6), 2264. https://doi.org/10.3390/s22062264







