Abstract
The objective of this exploratory randomized controlled trial (RCT) was to provide evidence for the feasibility and therapeutic value of a novel game-based dual-task balance exercise program in children with cerebral palsy (CP). Twenty children with CP were recruited and randomized into two groups: (a) the conventional balance training group (CG) and (b) the experimental group (XG), which received a game-based dual-task (DT) balance exercise program. Both groups received their respective therapy programs for 12 weeks at a frequency of three sessions per week. Semi-structured interviews with the parents and children and qualitative analysis were conducted to evaluate the children’s experiences with the game-based exercise program. The quantitative analysis included (a) the Pediatric Balance Scale (PBS), (b) Gross Motor Function Measure-88 (GMFM-88), and (c) computerized measures of standing balance performance during various dual-task conditions. Compliance was 100% for all 20 participants. Four themes captured the range of each participant’s experiences and opinions: (a) reasons for participation, (b) likes and dislikes with the technologies, (c) positive effects of the program, and (d) future expectations. Children in the XG demonstrated greater improvements in PBS, GMFM, and DT balance measures as compared to children in the CG. The findings demonstrate feasible trial procedures and acceptable DT-oriented training with a high compliance rate and positive outcomes. These findings support further research and development and progression to the next phase of a full-scale RCT to evaluate the clinical effectiveness of the game-based DT balance exercise program for children with CP.
1. Introduction
Cerebral palsy (CP) is one of the most common motor neurodevelopmental disorders, which affects five of every thousand live births in India and three of every thousand live births in North America [1,2]. Balance impairments and mobility limitations are common in children with CP [3,4,5]. Due to the many problems associated with reduced balance control, providing an effective rehabilitation program is essential in the development of the child’s mobility skills and in helping to prevent non-use sequelae, such as bone deformities, contractures, and obesity [6,7]. Clinicians and researchers have established the importance of task-specific repetitive training in the rehabilitation of motor function in children with cerebral palsy [7,8]. If improved balance is an expected outcome, training in tasks involving the facilitation of balance reactions in standing would be beneficial [9].
Balance is a functional term, and its control is a complex multidimensional process.
Independent community walking requires adequate balance skills and cognitive flexibility to manage a variety of environmental demands, which include attending to and interacting with various objects, searching for information, processing what is being seen, reading, etc. Balance and cognitive abilities are closely linked, and several studies have demonstrated dual-task interference with balance in children with CP when performing a concurrent cognitive task [5,6,7,8,9]. Therefore, DT training programs that use graded balance challenges combined with information processing loads would enhance rehabilitation outcomes.
An emerging approach to increase compliance is to combine balance exercises with computer games, making training a more engaging experience [10,11,12,13]. Several gaming systems have been used in the rehabilitation of balance in children with CP, which include Nintendo Wii Fit [14,15,16], Microsoft Xbox Kinect [16,17], Dance Mat [18], and PlayStation Eye Toy [19]. Other purpose-built rehabilitation gaming systems include various force platforms/pressure mats, which record the center of foot pressure signals (COPs), or video cameras to interact with computer games [20,21,22].
Game-based rehabilitation approaches have the potential to improve clinical outcomes and enhance the active participation of children with neuromotor deficits [12,23,24]. However, there are only a small number of exercise games available for either commercial gaming systems or custom exergaming systems. Therefore, there is a limited selection of cognitive activities, whereas there is a large number of inexpensive and readily available common and modern commercial computer games that are engaging, are therapeutic, and have a broad range of cognitive activities that can be played with a computer mouse or equivalent [25,26]. Based on this limitation, a low-cost, engaging dual-task computer game-based rehabilitation system (GRS) was developed for an integrated approach to balance, visuomotor, and executive cognitive training appropriate for children with CP. It uses an inertial-based (IB) mouse, a novel hands-free plug-and-play computer game controller, to interact with cognitive computer games while performing a wide range of balance exercises [27,28,29,30,31]. The IB mouse functions as a responsive USB plug-and-play computer mouse, and this allows common and modern computer games to be used and enjoyed as part of the rehabilitation program. Therefore, therapists and children can choose from a large variety of existing common and modern computer games. Many inexpensive, commercially available games involve multitasking. Hence, the tasks also engage key attentional, perceptual, and executive cognitive skills.
The purpose of this exploratory randomized clinical trial (RCT) is to provide evidence for the feasibility of conducting a full-scale RCT using the GRS for DT gait training in CP children with balance impairments. The first objective was to explore the implementation, acceptability, and appropriateness of the game-based DT balance program. Semi-structured interviews were conducted to explore children’s parents’ experiences with their respective exercise programs. The qualitative findings of participants’ experiences help to identify (a) perceived exercise benefits, (b) difficulties with the exercises and using the technologies, and (c) the engagement and motivational value of the computer games. The secondary objective was to estimate the treatment effect size of the DT balance program compared to usual physiotherapy. The working hypothesis was that the group receiving the DT balance program would demonstrate significantly greater improvement in balance, gait performance, and cognitive measures compared to usual physiotherapy.
2. Methods
Children diagnosed with CP were recruited for this single-blind randomized clinical trial with an active control arm (see Figure 1 for CONSORT diagram). The study was conducted according to international standards of Good Clinical Practice. Ethics approval was obtained from the Health Research Ethics Board (HREB), University of Manitoba, Winnipeg, Canada, and the Institutional Ethical Committee of Shree Dharmasthala Manjunatheshwara (SDM). University, Karnataka, India. This study is registered at ClinicalTrial.gov with the identifier # NCT03873441. The study participants were recruited from the Pediatric Physiotherapy Outpatient Department (OPD) of SDM College of Medical Sciences and Hospital. Successfully screened participants were randomized to the experimental group (XG) or control group (CG) by having them choose one of 20 sealed opaque envelopes that contained a letter signifying the group assignment. A graduate student not involved in the study produced the envelopes: 10 that contained a letter for the experimental group and 10 for the control group. The envelopes were thoroughly shuffled before each selection.
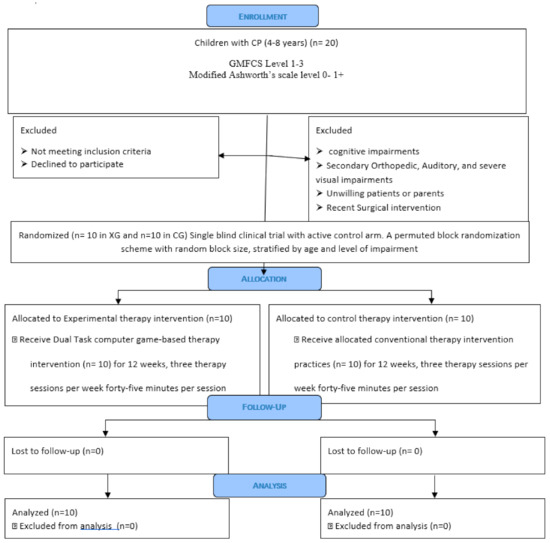
Figure 1.
CONSORT Flow Diagram.
Inclusion criteria: (a) children with a confirmed medical diagnosis of CP, ages 4–8 years, (b) Gross Motor Function Classification System level 1–3 [32], and (c) Modified Ashworth Scale level 0 to +1 [33]. Exclusion criteria: (a) visual or auditory impairment preventing them from seeing and interacting with the video games, (b) secondary orthopedic complications, (c) recent surgical intervention, (d) cognitive impairment, (e) seizures, or (f) complex communication disorders.
3. Procedures, Tests, and Instrumentation
The following outcome measures were obtained pre- and post-intervention by a physiotherapist masked to the intervention assignment.
- Pediatric Balance Scale (PBS): It consists of 14 items, which include: standing unsupported, standing with a narrow base of support (BOS), tandem standing, turning, and forward reach [34].
- Gross Motor Function Measure-88 (GMFM-88): The GMFM-88 is an observational clinical tool designed to evaluate a change in gross motor function in children with CP aged between 5 months and 16 years. The standing and the walking, running, and jumping subtests were used [35].
- Modified Clinical Test of Sensory Integration in Balance (MCTSIB) and computerized dual-task (DT) balance assessment: This assessment included four tasks that were first performed on a fixed floor surface and then on a compliant sponge pad. The children were asked to stand still for a duration of 30 s with eyes open (EO) or with eyes closed (EC) while performing a visuomotor tracking task and a visual cognitive game task described by Bhatt et al., (2019) 31] and Szturm et al., (2015) [36]. The VMT module, as described in Figure 2A,B, involved tracking a visual target that moved horizontally on a computer display for several cycles. As presented in Panel B, the participant stands while viewing a computer monitor. An inertial-based mouse is secured to the sports cap, and head rotation is used to interact with the visuospatial cognitive games. Panels A and C present snapshots of the VMT and VCG modules. Panel A (VMT) shows cursors of different shapes appearing on the computer monitor. The target is a circle, and its motion was computer-controlled and moved at a predetermined frequency of 0.5 Hz with an amplitude of 70% of the monitor width. The second cursor is a rectangle, which is slaved to the head-mounted IB mouse. Children were instructed to rotate their heads and overlap the rectangle cursor with the target circle for several cycles (i.e., 30 s). The coordinates of the rectangle and target cursor were recorded at 100 Hz for offline analysis. Panel D presents synchronous plots of the target cursor motion and user movement trajectory (head rotation) for a typical VM tracking task. The maximum is the leftmost position, and the minimum is the right-most position. Panel C (VCG) objects are categorized as targets or distractors. The game objects appear at random locations at the top of the display every 2 s and move in a diagonal trajectory to the bottom of the display. Children were required to move the paddle to catch the target objects while avoiding the distractors. The coordinates of the game paddle and target objects were recorded (100 Hz) for offline analysis of the success rate (SR). Panel E presents the trajectory for one VCG game movement response from target appearance to target disappearance. Panel F presents overlay trajectories of all game movement responses for one game session.
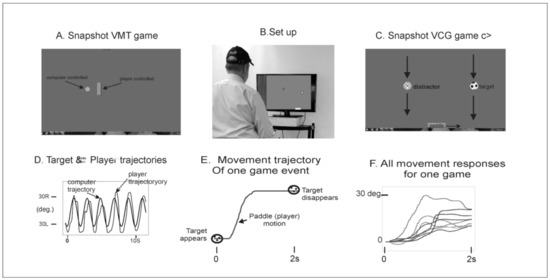 Figure 2. Illustration of the assessment game setup. As presented in Panel (B), the participant stands while viewing a computer monitor. An inertial-based mouse is secured to the sports cap, and head rotation is used to interact with the visuospatial cognitive games. Panels (A,C) present snapshots of the VMT and VCG modules. Panel (A) (VMT) shows cursors of different shapes appearing on the computer monitor. The target is a circle, and its motion was computer-controlled and moved at a predetermined frequency of 0.5 Hz with an amplitude of 70% of the monitor width. The second cursor is a rectangle, which is slaved to the head-mounted IB mouse. Children were instructed to rotate their heads and overlap the rectangle cursor with the target circle for several cycles (i.e., 30 s). The coordinates of the rectangle and target cursor were recorded at 100 Hz for offline analysis. Panel (D) presents synchronous plots of the target cursor motion and user movement trajectories (head rotation) for a typical VM tracking task. The maximum is the leftmost position, and the minimum is the right-most position. Panel (C) (VCG) objects are categorized as targets or distractors. The game objects appear at random locations at the top of the display every 2 s and move in a diagonal trajectory to the bottom of the display. Children were required to move the paddle to catch the target objects while avoiding the distractors. The coordinates of the game paddle and target objects were recorded (100 Hz) for offline analysis of the success rate (SR). Panel (E) presents the trajectory for one VCG game movement response from target appearance to target disappearance. Panel (F) presents overlay trajectories of all game movement responses for one game session.
Figure 2. Illustration of the assessment game setup. As presented in Panel (B), the participant stands while viewing a computer monitor. An inertial-based mouse is secured to the sports cap, and head rotation is used to interact with the visuospatial cognitive games. Panels (A,C) present snapshots of the VMT and VCG modules. Panel (A) (VMT) shows cursors of different shapes appearing on the computer monitor. The target is a circle, and its motion was computer-controlled and moved at a predetermined frequency of 0.5 Hz with an amplitude of 70% of the monitor width. The second cursor is a rectangle, which is slaved to the head-mounted IB mouse. Children were instructed to rotate their heads and overlap the rectangle cursor with the target circle for several cycles (i.e., 30 s). The coordinates of the rectangle and target cursor were recorded at 100 Hz for offline analysis. Panel (D) presents synchronous plots of the target cursor motion and user movement trajectories (head rotation) for a typical VM tracking task. The maximum is the leftmost position, and the minimum is the right-most position. Panel (C) (VCG) objects are categorized as targets or distractors. The game objects appear at random locations at the top of the display every 2 s and move in a diagonal trajectory to the bottom of the display. Children were required to move the paddle to catch the target objects while avoiding the distractors. The coordinates of the game paddle and target objects were recorded (100 Hz) for offline analysis of the success rate (SR). Panel (E) presents the trajectory for one VCG game movement response from target appearance to target disappearance. Panel (F) presents overlay trajectories of all game movement responses for one game session.
Prior to testing, the participants were allowed to play the tracking and game tasks while sitting for a few minutes to become familiar with each task.
The displacement of the center of foot pressure (COP) was recorded using a flexible force sensor array (FSA) mat (Vista Medical, sampling frequency 80 Hz). The FSA pressure mat was placed on top of the sponge to record the instantaneous COP position during each task condition [31,36,37,38].
4. Interventions
Two therapists delivered the therapy protocols, one to the XG and one to the CG. Each group received the protocol for 12 weeks at a frequency of three therapy sessions per week. Each session was 45 min long.
The control group (CG) received a conventional physical therapy balance program.
This included (a) active-assisted stretching exercises and (b) balance and weight-shifting exercises with arm reaching and trunk bending movements. These activities were initially performed on a fixed surface, gradually progressing to unstable surfaces. As tolerated, the balance challenge was progressed by increasing the thickness of the sponge pads and using air-bladder-type balance disks and bolsters.
The experimental group (XG) received the game-based DT balance training program.
Children were fitted with a headband/cap instrumented with the miniature IB mouse to play various cognitive computer video games. The children were asked to stand and balance on an unstable surface (as tolerated) while playing various computer video games. As with the CG, the balance challenge was progressed by increasing the thickness of the sponge pads and then using balance disks and bolsters. The amount of cognitive demand was graded by selecting different computer video games and adjusting the difficulty level of the games. Many real-life tasks involve head movements to search and track various objects, avoid distractors, and process information on what is being seen. Appendix A presents a list of computer games used in the present study.
5. Qualitative Analysis
The qualitative analysis, i.e., post-intervention interviews, was conducted only on the experimental group to explore the experiences of the children using the gaming technology and game-based DT exercise program. The interview focused on generating information on experiences and the views of the parents and children about the expectations, likes and dislikes, and outcomes of using the balance gaming exercise program. The following questions were asked during the interview.
- When you agreed to participate, how did you and your child hope to benefit from the therapy program?
- Were there things about the game or exercise program that you liked and things you did not like?
- What did you think about the computer games your child was asked to play? Did your child enjoy the games? Were there games that you did not seem to enjoy?
- Did you feel that this therapy program helped?
- If you were provided with the right setting, would you want to continue with these game-based exercises?
A research assistant who was blinded to the interventions conducted the interviews. A second person was present to record all responses in writing. The analytical framework of interpretive description was used for thematic interpretation. One researcher who developed the coding system by paraphrasing, generalizing, and abstracting the written responses of each interview initially read the written response transcripts. A second researcher scrutinized the coded data and identified any additional unique responses. The two researchers then met, and a final coded response category was produced and organized into final themes [39].
6. Quantitative Analysis
The following outcome measures were obtained pre- and post-intervention:
- Balance performance: The total path length (TPL) of COP excursion over the 30 s task duration was computed [31]. A decrease in TPL was interpreted as improved balance performance.
- Visuomotor (VMT) performance measure: Synchronous plots of the target motion and user’s head rotation (rectangle cursor) for a typical VMT task are presented in Figure 2. The total residual error (TRE) was determined by computing the difference between the trajectories of the target and head cursor motions and expressed as a percentage of display width [31,36].
- Visual cognitive game (VCG) performance measure: Figure 2 depicts the overlay trajectories of game paddle displacements (head movements) for all game events in one 60 s game session. Each game event lasted for two seconds from initial target appearance to target disappearance. The success rate (SR)—the percentage of targets caught—was quantified [31,36].
7. Statistical Analysis
Descriptive statistics, including means, standard error of mean (SEM), and percentages, were used to describe demographic variables and outcome measures. Effect size was calculated using Cohen’s d [40]. A value of 2 is a “small” effect size, 0.5 represents a “medium” effect size, and 0.7 is a “large” effect size. The normality of the data was assessed using the Shapiro–Wilks test. This test revealed a normal distribution, p > 0.1, for all outcome measures. A two-way repeated-measures ANOVA was used to examine the effects of time (pre- and post-intervention) in each group (XG vs. CG) and time*group interaction on balance, VMT, and VCG outcome measures. The effect size was calculated using Cohen’s d [31,36]. The significance level was set at 0.05, and statistical analysis was conducted using SPSS (version 27) (IBM SPSS Science, Chicago, IL, USA).
8. Results
The recruitment target of 20 children was reached in 6 months. All children screened and randomized to their respective exercise groups completed the pre- and post-intervention assessments and attended all exercise sessions (compliance of 100%). There were no adverse events or problems with the use of the technology or computer games in therapy. These findings demonstrate excellent feasibility.
Table 1 presents the demographic data. The mean age of children in the XG was 6.34 years, and for the CG, it was 6.33 years. There was no significant difference in age between the two groups (p = 0.3). Both groups had the same number of females and males, and both groups had similar numbers of GMFCS levels one to three.

Table 1.
Demographic data.
The following four themes captured the range of parents’ and children’s experiences and parents’ opinions about their child’s exercise program. Table 2, Table 3, Table 4 and Table 5 present parents’ direct quotes for each theme.

Table 2.
Expectations and problem list.

Table 3.
Likes and dislikes.

Table 4.
Effects of the game-based exercise program.

Table 5.
Future expectations.
- Expectations of therapy (Table 2): All parents expressed their concerns regarding their child’s poor balance, limited mobility, and inability to participate in play and most school activities. Of note, all participants had been undergoing conventional therapy to improve balance for at least one year.
- Likes and dislikes (Table 3): Most parents mentioned that balance activities on the different surfaces, especially the balance disks, were very difficult to carry out while playing the computer games and that this frustrated the children. Most parents and children reported that the chosen computer games were fun to play. One parent commented that it was easier to convince children to perform balance exercises when using computer games than conventional exercises.
- Effects of therapy (Table 4): All parents gave positive feedback, such as improvement in balance performance, enhanced concentration, increased confidence, improved walking abilities, improvement in stair climbing, and improved functional activity.
- Future expectations (Table 5): All parents and children expressed their interest in continuing this therapy if they were provided with the gaming system.
Table 6 presents the ANOVA results for time, group, and interaction effects for all outcome measures. Group means and standard errors of means (SEM) by group and time period are presented in Figure 3. A significant improvement in PBS and GMFM subscores pre- to post-intervention (time effect) was seen for both groups. Effect sizes were medium to large, ranging from 0.2 to 0.6. There were no significant time*group effects. On average, PBS increased by 5 for the XG and 0.8 for the CG, GMFM standing increased by 10.4 for the XG and 5.8 for the CG, and GMFM walking, running, and jumping increased by 5.5 for the XG and 1.2 for the CG.

Table 6.
Presented ANOVA results are f-statistic (f), p-value (p), and effect size (ef) for each outcome measure. All conditions, eyes open (EO), eyes closed (EC), VCG, and VMT, were performed while standing on a sponge.
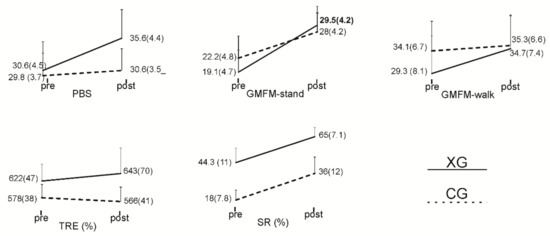
Figure 3.
Line plots presenting group means and standard errors of means (SEM) pre- and post-intervention.
In the case of COP TPL, there was no significant time effect, but there was a significant time*group effect for all task conditions except for the VCG condition. In the case of the VCG condition, there was a significant decrease in TPL for both groups, with a large effect size of 0.5. There was no time*group or group effect. The results of further statistical comparisons of time effects by group revealed a significant decrease in COP TPL pre- to post-intervention for the XG, but no significant change was observed for the CG (Table 7). The effect size for the XG results was large, ranging from 0.5 to 1.1. There was one exception in each group. There was no significant change in TPL for the eyes-closed condition in XG, while there was a significant increase in TPL post-intervention for the VCG condition in CG.

Table 7.
Results of paired t-test of comparison between pre- and post-intervention COP-TPL. Presented are group, means and standard errors of means (SEM), t-statistic, p-value, and effect size.
As presented in Table 6 and Figure 3, there was a significant improvement in SR pre- to post-intervention in both the XG and CG and no significant time*group effect. The effect size was moderate, with a value of 0.3. In the case of TRE, no significant effects were observed for time or time*group.
There were no significant group effects observed for any of the outcome measures except for VCG SR, where performance was significantly better in the XG as compared to the CG.
The VCG module, as described in Figure 3, involved moving a game paddle (head rotation) to interact with moving game objects.
9. Discussion
The purpose of the present study was to evaluate the feasibility of conducting an RCT using a game-based DT exercise program in children with CP. The present study findings demonstrate that the parents recognized that their expectations related to improving children’s balance skills were addressed during the 12-week therapy program. Parents also shared the challenges that they faced regarding children’s participation in therapy. There are several likely reasons for the 100% compliance. Continued guidance, instructions, and assistance were provided to the children throughout the intervention to ensure that they understood how to play the games, and they were provided a variety of games with appropriate difficulty levels, as well as cognitive activities. As reported by most of the participants, the interactive commercial computer games used in the present study were engaging and fun, and most of the content was deemed appropriate.
There was little difficulty in using the technology (i.e., a wireless plug-and-play computer mouse and computer games), although it was noted by all participants that the dual-task exercise program was challenging. The acceptability of the gaming system and game-based exercise program was shown through the comments of all participants.
The present study observed a significant decline in COP excursion post-intervention for all task conditions for the XG with a medium to large effect size, ranging from 0.5 to 1.1. In contrast, there was no significant change observed in the CG. Other studies have used COP excursion to evaluate the effects of game-based balance exercise programs in CP children [41,42,43,44]. In these studies, the coordinates of the COP were used to control the motion of a game sprite to catch falling game targets. A 2.6% decrease in COP excursion post-intervention was observed when assessed while children stood on a fixed floor surface with eyes open. The present study extends these results and observed greater decreases in COP excursion when balance was assessed while standing on a sponge surface and while performing the visual tracking and cognitive game activities.
Both the XG and CG showed significant improvements post-intervention in clinical measures of balance and locomotion with medium to large effect sizes. The minimal clinically important difference (MCID) for the PBS is reported to be 3.7 for children with CP. In the present study, a greater improvement in the PBS score of 5 was observed for the XG. The MCID reported for the standing subtest of GMFM ranges from 3 to 5 for children at GMFCS levels 1–3. In the present study, greater improvements were observed for both groups: 10.4 for the XG and 5.8 for the CG. The MCID reported for the walking, running, and jumping subtest of GMFM ranges from 1.8 to 4 for children at GMFCS levels 1–3. In the present study, a greater improvement of 5.5 was observed for the XG. These improvements in PBS and GMFM are complemented by qualitative data: i.e., the parents reported a change in the children’s level of independence in their daily tasks at home, at school, and in play.
In the present study, different sponge pads and air-bladder balance disks were used during the DT exercise program to grade the balance challenge. A compliant support surface cannot reciprocate the normal forces from the feet as the body sways. The result is an increase in the frequency and amplitude of body sway movements in all directions [37,45], a condition to which the child must quickly sense and correct to minimize body sway and prevent loss of balance. The increased cognitive demand during balance activities can also result in increased body sway, i.e., a dual-task interference effect [40,45]. The computer games used in the present study require executive cognitive functions to process what is being seen, such as visual attention, visual search, and spatial processing of randomly moving game targets and distractors (cognitive inhibition). The ability to maintain and restore standing balance on a compliant surface also requires processing and organizing spatial information from multiple sensory systems, including vision, to determine body orientation and the direction and amplitude of body motion. Neuroimaging studies have shown that the prefrontal cortex is strongly activated in CP children when performing dual tasks [46,47,48,49,50]. Dual-task balance training on unstable surfaces involves more unpredictable balance disturbances as compared to that received during the CG training. Therefore, the children in the XG would be exposed to considerably more situations that require reactive balance control needed to restore balance. This is likely the reason that a significant post-intervention reduction in COP excursion was observed in children in the XG but not the CG.
Adding a gaming element was intended to provide extra motivation for the children in the form of a challenge and a more enjoyable means of encouraging them to follow repetitive movements that are a part of the rehabilitation process. Most parents commented that the combination of games and balance exercises was challenging yet engaging and that their children enjoyed playing the games. As parents mentioned, the addition of game tasks with colorful backgrounds and attractive characters enhanced their children’s concentration and improved children’s compliance with the intensive balance gaming tasks. Studies in the past comparing the use of video games to that of traditional therapy showed similar results [47,48,49].
10. Conclusions
The game-based DT methods presented in this study broaden the type of visuospatial cognitive activities that can be combined with balance training in children with CP. The findings demonstrate evidence on recruitment, the feasibility of trial procedures, 100% compliance, the acceptance of the game-based DT exercise program, and the usability of the gaming system (mouse and computer games). Clinically meaningful changes in balance performance were observed with moderate to large effect sizes. One limitation relates to how children spontaneously prioritize their attention between balancing and tracking/cognitive tasks during DT testing. It is possible that balance was prioritized and that the children did not fully attend to and process the cognitive information on the computer monitor. Alternatively, the information was received and processed, but the performance was affected due to dual-task interference. Modest, fair to good performance levels were observed for cognitive game tasks during testing. This demonstrates that the children were attending to and processing the information seen on the display. However, they may have stopped intermittently for a few seconds and prioritized balance processing.
The long-term effects of DT balance exercise in children with CP will need to be confirmed in future adequately powered randomized controlled trials. In addition to measures of structure and function, future randomized controlled trials should also include outcome measures such as health-related quality of life and level of participation to validate the findings. For children, outcome measures such as the Goal Attainment Scale could be used [51]. A clinical trial is also planned to extend the present application to include game-based DT treadmill training.
Author Contributions
The authors contributed to the manuscript in the following capacities. Conceptualization, assessment, and treatment: T.S., S.T.P., K.M., D.R.S. and A.K. Data analysis, writing original draft, review, and editing: T.S., S.T.P., K.M., D.R.S., A.K., R.E. and N.G. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Ethical approval was obtained from two institutes. The study was approved by The Ethics Committee of College of Rehabilitation Sciences, University of Mannitoba, Winnipeg, MB, Canada on 14-01-2022 Ref: H2019:081 (HS22614) and The Ethics Committee of SDM College of Medical Sciences & Hospital on 05-03-2020 Ref: SDMIEC:11: 2020.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study. Written informed consent has been obtained from the patient(s) to publish this paper.
Data Availability Statement
On request the data is available with the corresponding author.
Conflicts of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that can be construed as a potential conflict of interest.
Appendix A

Table A1.
List of computer video games used in this study, obtained from www.bigfishgames.com (15 November 2021). Note that matching and shooting games require children to use a small wireless hand-held clicker with a left mouse button to press when needed for game play.
Table A1.
List of computer video games used in this study, obtained from www.bigfishgames.com (15 November 2021). Note that matching and shooting games require children to use a small wireless hand-held clicker with a left mouse button to press when needed for game play.
| Big Fish Game | Axis Play | Start Difficulty | Type | Clicker | Precision | Background | Distractor | Executive Function |
|---|---|---|---|---|---|---|---|---|
| Abundante | Horizontal | Difficult | Match 3 | Yes | Moderate | Low optokinetic | No | Matching and puzzle solving |
| Action ball | Horizontal | Moderate | Brick Buster | No | Moderate | High optokinetic | Yes | Visual tracking and spatial |
| Acqua Ball | Horizontal | Easy | Brick Buster | No | Low | Medium optokinetic | Yes | Visual tracking and spatial |
| Astrobugs Revenge | Horizontal | Difficult | Match 3 | Yes | High | Medium optokinetic | No | Matching |
| Ark Light | Variable | Moderate | Shooting | Yes | Moderate | Medium optokinetic | Yes | Search and select |
| Birds Town | Horizontal | Moderate | Match 3 | Yes | High | Low optokinetic | No | Matching |
| Brave Piglet | Vertical | Moderate | Shooting | Yes | High | Low optokinetic | Yes | Visual tracking and spatial |
| Bricks of Egypt | Horizontal | Easy | Brick Buster | No | Variable | Low optokinetic | Yes | Visual tracking and spatial |
| Butterfly Escape | Horizontal | Moderate | Match 3 | Yes | High | Low optokinetic | Yes | Visual tracking and spatial |
| Chicken Invaders | Variable | High | Shooting | Yes | Moderate | High optokinetic | Yes | Search and select |
| Digby Donuts | Horizontal | Moderate | Catch and Sort | Yes | Moderate | Low optokinetic | No | Search precision sort |
| Feeding Frenzy | Variable | Difficult | Aim and Move | No | High | Low optokinetic | Yes | Visual tracking and spatial |
| Invadazoid | Horizontal | Difficult | Brick Buster | No | High | Moderate optokinetic | Yes | Visual tracking and spatial |
| Jar of Marbles | Horizontal | Easy | Match 3 | Yes | Medium | Low optokinetic | No | Matching three, aligning |
| Jet Jumper | Variable | Difficult | Driving Game | Yes | High | High optokinetic | Yes | Visual tracking and driving |
| Luxor 3 | Horizontal | Moderate | Match 3 | Yes | High | Moderate optokinetic | Yes | Match 3, aligning |
| Luxor HD | Horizontal | Moderate | Match 3 | Yes | High | Moderate optokinetic | Yes | Match 3, aligning |
| Reaxion | Horizontal | Moderate | Brick Buster | No | Variable | Moderate optokinetic | Yes | Visual tracking and spatial |
| Ricochet Recharge | Horizontal | Moderate | Brick Buster | No | High | Moderate optokinetic | No | Visual tracking and spatial |
References
- Silberberg, D.H. Neurodevelopmental disorders in India: From epidemiology to public policy. World Neurol. 2014, 29, 2–3. [Google Scholar]
- Stavsky, M.; Mor, O.; Mastrolia, S.A.; Greenbaum, S.; Than, N.G.; Erez, O. Cerebral palsy-trends in epidemiology and recent development in prenatal mechanisms of disease, treatment, and prevention. Front. Pediatrics 2017, 5, 21. [Google Scholar] [CrossRef] [Green Version]
- Rosenbaum, P.; Paneth, N.; Leviton, A.; Goldstein, M.; Bax, M.; Damiano, D.; Dan, B.; Jacobsson, B. A report: The definition and classification of cerebral palsy April 2006. Dev. Med. Child Neurol. 2007, 109, 8–14. [Google Scholar]
- Donker, S.F.; Ledebt, A.; Roerdink, M.; Savelsbergh, G.J.; Beek, P.J. Children with cerebral palsy exhibit greater and more regular postural sway than typically developing children. Exp. Brain Res. 2008, 184, 363–370. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tracy, J.B.; Petersen, D.A.; Pigman, J.; Conner, B.C.; Wright, H.G.; Modlesky, C.M.; Miller, F.; Johnson, C.L.; Crenshaw, J.R. Dynamic stability during walking in children with and without cerebral palsy. Gait Posture 2019, 72, 182–187. [Google Scholar] [CrossRef]
- Peterson, M.D. Physical inactivity and secondary health complications in cerebral palsy: Chicken or egg? Dev. Med. Child Neurol. 2015, 57, 114–115. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Novak, I.; Morgan, C.; Fahey, M.; Finch-Edmondson, M.; Galea, C.; Hines, A.; Langdon, K.; Namara, M.M.; Paton, M.C.; Popat, H.; et al. State of the Evidence Traffic Lights 2019: Systematic Review of Interventions for Preventing and Treating Children with Cerebral Palsy. Curr. Neurol. Neurosci. Rep. 2020, 20, 3. [Google Scholar] [CrossRef] [Green Version]
- Ryan, J.M.; Cassidy, E.E.; Noorduyn, S.G.; O’Connell, N.E. Exercise interventions for cerebral palsy. Cochrane Database Syst. Rev. 2017, 6, CD011660. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pin, T.W. Active computer play on balance and postural control for children with cerebral palsy: A systematic review. Gait Posture 2019, 73, 126–139. [Google Scholar] [CrossRef]
- Carcreff, L.; Fluss, J.; Allali, G.; Valenza, N.; Aminian, K.; Newman, C.J.; Armand, S. The effects of dual tasks on gait in children with cerebral palsy. Gait Posture 2019, 70, 148–155. [Google Scholar] [CrossRef] [PubMed]
- Katz-Leurer, M.; Rotem, H.; Meyer, S. Effect of concurrent cognitive tasks on temporo-spatial parameters of gait among children with cerebral palsy and typically developed controls. Dev. Neurorehabil. 2014, 17, 363–367. [Google Scholar] [CrossRef] [PubMed]
- Blanchard, Y.; Carey, S.; Coffey, J.; Cohen, A.; Harris, T.; Michlik, S.; Pellecchia, G.L. The influence of concurrent cognitive tasks on postural sway in children. Pediatr. Phys. Ther. 2005, 17, 189–193. [Google Scholar] [CrossRef]
- Palluel, E.; Chauvel, G.; Bourg, V.; Commare, M.C.; Prado, C.; Farigoule, V.; Nougier, V.; Olivier, I. Effects of dual tasking on postural and gait performances in children with cerebral palsy and healthy children. Int. J. Dev. Neurosci. 2019, 79, 54–64. [Google Scholar] [CrossRef]
- Reilly, D.S.; Woollacott, M.H.; van Donkelaar, P.; Saavedra, S. The interaction between executive attention and postural control in dual-task conditions: Children with cerebral palsy. Arch. Phys. Med. Rehabil. 2008, 89, 834–842. [Google Scholar] [CrossRef] [PubMed]
- Bonnechère, B.; Omelina, L.; Jansen, B.; Van Sint Jan, S. Balance improvement after physical therapy training using specially developed serious games for cerebral palsy children: Preliminary results. Disabil. Rehabil. 2017, 39, 403–406. [Google Scholar] [CrossRef] [PubMed]
- Schröder, J.; van Criekinge, T.; Embrechts, E.; Celis, X.; Van Schuppen, J.; Truijen, S.; Saeys, W. Combining the benefits of tele-rehabilitation and virtual reality based balance training: A systematic review on feasibility and effectiveness. Disabil. Rehabil. Assist. Technol. 2019, 14, 2–11. [Google Scholar] [CrossRef]
- Wu, J.; Loprinzi, P.D.; Ren, Z. The Rehabilitative Effects of Virtual Reality Games on Balance Performance among Children with Cerebral Palsy: A Meta-Analysis of Randomized Controlled Trials. Int. J. Environ. Res. Public Health 2019, 16, 4161. [Google Scholar] [CrossRef] [Green Version]
- Gatica-Rojas, V.; Méndez-Rebolledo, G.; Guzman-Muñoz, E.; Soto-Poblete, A.; Cartes-Velásquez, R.; Elgueta-Cancino, E.; Cofré Lizama, E. Does Nintendo Wii Balance Board improve standing balance? A randomized controlled trial in children with cerebral palsy. Eur. J. Phys. Rehabil. Med. 2017, 53, 535–544. [Google Scholar] [CrossRef]
- Sajan, J.E.; John, J.A.; Grace, P.; Sabu, S.S.; Tharion, G. Wii-based interactive video games as a supplement to conventional therapy for rehabilitation of children with cerebral palsy: A pilot, randomized controlled trial. Dev. Neurorehabilit. 2017, 20, 361–367. [Google Scholar] [CrossRef]
- Kachmar, O.; Kushnir, A.; Fedchyshyn, B.; Cristiano, J.; O’Flaherty, J.; Helland, K.; Johnson, G.; Puig, D. Nintendo WIIFIT Personalized balance games for children with cerebral palsy: A pilot study. J. Pediatric Rehabil. Med. Interdiscip. Approach Throughout Lifesp. 2021, 14, 237–245. [Google Scholar] [CrossRef]
- Cheung, J.; Maron, M.; Tatla, S.; Jarus, T. Virtual reality as balance rehabilitation for children with brain injury: A case study. Technol. Disabil. 2013, 25, 207–219. [Google Scholar] [CrossRef]
- Camara Machado, F.R.; Antunes, P.P.; Souza, J.D.; Santos, A.C.; Levandowski, D.C.; Oliveira, A.A. Motor Improvement Using Motion Sensing Game Devices for Cerebral Palsy Rehabilitation. J. Mot. Behav. 2017, 49, 273–280. [Google Scholar] [CrossRef]
- Jha, K.K.; Karunanithi, G.B.; Sahana, A.; Karthikbabu, S. Randomised trial of virtual reality gaming and physiotherapy on balance, gross motor performance and daily functions among children with bilateral spastic cerebral palsy. Somatosens. Mot. Res. 2021, 38, 117–126. [Google Scholar] [CrossRef]
- Kozyavkin, V.I.; Kachmar, B.O.; Terletskyy, O.I.; Kachmar, O.O.; Ablikova, I.V. Stepping games with Dance Mat for motor rehabilitation. In Proceedings of the International Conference on Virtual Rehabilitation (ICVR), Philadelphia, PA, USA, 26–29 August 2013; pp. 174–175. [Google Scholar] [CrossRef]
- Sandlund, M.; Lindh Waterworth, E.; Häger, C. Using motion interactive games to promote physical activity and enhance motor performance in children with cerebral palsy. Dev. Neurorehabilit. 2011, 14, 15–21. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ledebt, A.; Becher, J.; Savelsberg. Balance training with visual feedback in children with hemiplegic cerebral palsy. Gait Posture 2005, 21, S86. [Google Scholar] [CrossRef]
- Da Silva, T.D.; da Silva, P.L.; de Jesus Valenzuela, E.; Dias, E.D.; Simcsik, A.O.; de Carvalho, M.G.; Fontes, A.M.; de Oliveira Alberissi, C.A.; de Araújo, L.V.; da Costa Brandão, M.V.; et al. Serious Game Platform as a Possibility for Home-Based Telerehabilitation for Individuals with Cerebral Palsy During COVID-19 Quarantine—A Cross-Sectional Pilot Study. Front. Psychol. 2021, 12, 622678. [Google Scholar] [CrossRef]
- Arnoni, J.L.; Pavao, S.L.; dos Santos Silva, F.P.; Rocha, N.A. Effects of virtual reality in body oscillation and motor performance of children with cerebral palsy: A preliminary randomized controlled clinical trial. Complem. Ther. Clin. Pract. 2019, 35, 189–194. [Google Scholar] [CrossRef] [PubMed]
- Ren, Z.; Wu, J. The effect of virtual reality games on the gross motor skills of children with cerebral palsy: A meta-analysis of randomized controlled trials. Int. J. Environ. Res. Public Health 2019, 16, 3885. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cooper, T.; Williams, J.M. Does an exercise programme integrating the Nintendo Wii-Fit Balance Board improve balance in ambulatory children with cerebral palsy? Phys. Rev. 2017, 22, 229–237. [Google Scholar] [CrossRef]
- Nayak, A.; Alhasani, R.; Kanitkar, A.; Szturm, T. Dual-Task Training Program for Older Adults: Blending Gait, Visuomotor and Cognitive Training. Front. Netw. Physiol. 2021. [Google Scholar] [CrossRef]
- Bhatt, M.; Mahana, B.; Ko, J.; Kolesar, T.; Kanitkar, A.; Szturm, T. Computerized Dual-Task Testing of Gait Visuomotor and Cognitive Functions in Parkinson’s disease: Test-Retest Reliability and Validity. Front. Hum. Neurosci. 2021, 15, 706230. [Google Scholar] [CrossRef]
- Bodkin, A.W.; Robinson, C.; Perales, F.P. Reliability and validity of the gross motor function classification system for cerebral palsy. Pediatric Phys. Ther. 2003, 15, 247–252. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mutlu, A.; Livanelioglu, A.; Gunel, M.K. Reliability of Ashworth and Modified Ashworth scale in children with spastic cerebral palsy. BMC Musculoskelet. Disord. 2008, 9, 44. [Google Scholar] [CrossRef] [Green Version]
- Chen, C.L.; Shen, I.H.; Chen, C.Y.; Wu, C.Y.; Liu, W.Y.; Chung, C.Y. Validity, responsiveness, minimal detectable change, and minimal clinically important change of Pediatric Balance Scale in children with cerebral palsy. Res. Dev. Disabil. 2013, 34, 916–922. [Google Scholar] [CrossRef]
- Alotaibi, M.; Long, T.; Kennedy, E.; Bavishi, S. The efficacy of GMFM-88 and GMFM-66 to detect changes in gross motor function in children with cerebral palsy (CP): A literature review. Disabil. Rehabil. 2014, 36, 617–627. [Google Scholar] [CrossRef]
- Bhatt, M.; Mahana, B.; Marotta, J.J.; Ko, J.H.; Hobson, D.E.; Szturm, T. A new technique to test the effect of cognition on standing balance in Parkinson’s disease. Open J. Parkinson’s Dis. Treat. 2019, 2, 6–13. [Google Scholar] [CrossRef] [Green Version]
- Szturm, T.; Sakhalkar, V.; Boreskie, S.; Marotta, J.J.; Wu, C.; Kanitkar, A. Integrated testing of standing balance and cognition: Test-retest reliability and construct validity. Gait Posture 2015, 41, 146–152. [Google Scholar] [CrossRef]
- Betker, A.L.; Moussavi, Z.M.; Szturm, T. On modeling center of foot pressure distortion through a medium. IEEE Trans Biomed. Eng. 2005, 52, 345–352. [Google Scholar] [CrossRef] [PubMed]
- Desai, A.; Goodman, V.; Kapadia, N.; Shay, B.L.; Szturm, T. Relationship between dynamic balance measures and functional performance in community-dwelling elderly people. Phys. Ther. 2010, 90, 748–760. [Google Scholar] [CrossRef] [PubMed]
- Teodoro, I.P.; Rebouças, V.D.; Thorne, S.E.; Souza, N.K.; Brito, L.S.; Alencar, A.M. Interpretive description: A viable methodological approach for nursing research. Esc. Anna Nery 2018, 22, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Larner, A.J. Effect Size (Cohen’s d) of Cognitive Screening Instruments Examined in Pragmatic Diagnostic Accuracy Studies. Dement. Geriatr. Cogn. Disord. Extra 2014, 4, 236–241. [Google Scholar] [CrossRef]
- Oeffinger, D.; Bagley, A.; Rogers, S.; Gorton, G.; Kryscio, R.; Abel, M.; Damiano, D.; Barnes, D.; Tylkowski, C. Outcome tools used for ambulatory children with cerebral palsy: Responsiveness and minimum clinically important differences. Dev. Med. Child Neurol. 2008, 50, 918–925. [Google Scholar] [CrossRef]
- El-Shamy, S.M.; Abd El Kafy, E.M. Effect of balance training on postural balance control and risk of fall in children with diplegic cerebral palsy. Disabil. Rehabil. 2014, 36, 1176–1183. [Google Scholar] [CrossRef]
- El-Gohary, T.M.; Emara, H.A.; Al-Shenqiti, A.; Hegazy, F.A. Biodex balance training versus conventional balance training for children with spastic diplegia. J. Taibah Univ. Med. Sci. 2017, 12, 534–540. [Google Scholar] [CrossRef] [PubMed]
- Fransson, P.A.; Gomez, S.; Patel, M.; Johansson, L. Changes in multi-segmented body movements and EMG activity while standing on firm and sponge support surfaces. Eur. J. Appl. Physiol. 2007, 101, 81–89. [Google Scholar] [CrossRef] [Green Version]
- Surkar, S.M.; Hoffman, R.M.; Harbourne, R.; Kurz, M.J. Cognitive-Motor Interference Heightens the Prefrontal Cortical Activation and Deteriorates the Task Performance in Children with Hemiplegic Cerebral Palsy. Arch. Phys. Med. Rehabil. 2021, 102, 225–232. [Google Scholar] [CrossRef]
- Peungsuwan, P.; Parasin, P.; Siritaratiwat, W.; Prasertnu, J.; Yamauchi, J. Effects of Combined Exercise Training on Functional Performance in Children with Cerebral Palsy: A Randomized-Controlled Study. Pediatric Phys. Ther. 2017, 29, 39–46. [Google Scholar] [CrossRef]
- Kelders, S.M.; Sommers-Spijkerman, M.; Goldberg, J. Investigating the Direct Impact of a Gamified Versus Nongamified Well-Being Intervention: An Exploratory Experiment. J. Med. Internet Res. 2018, 20, e247. [Google Scholar] [CrossRef]
- Palmer, K.K.; Chinn, K.M.; Robinson, L.E. Using achievement goal theory in motor skill instruction: A systematic review. Sports Med. 2017, 47, 2569–2583. [Google Scholar] [CrossRef] [PubMed]
- Steenbeek, D.; Ketelaar, M.; Galama, K.; Gorter, J.W. Goal attainment scaling in paediatric rehabilitation: A critical review of the literature. Dev. Med. Child Neurol. 2007, 49, 550–556. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).