Validation of Pressure-Sensing Insoles in Patients with Parkinson’s Disease during Overground Walking in Single and Cognitive Dual-Task Conditions
Abstract
:1. Introduction
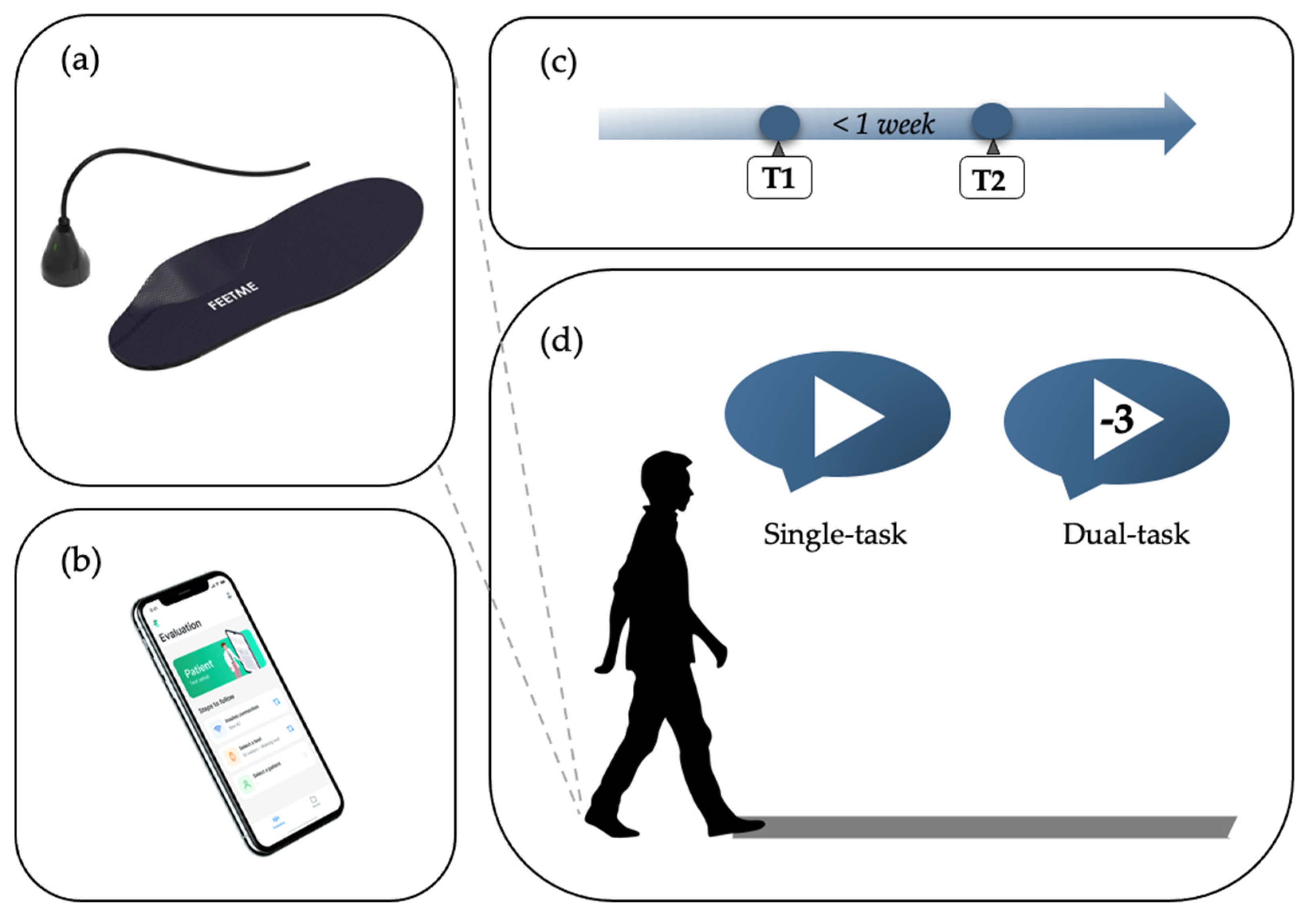
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.3. Instrumentation
2.4. Procedure
2.5. Data Analysis and Statistical Methods
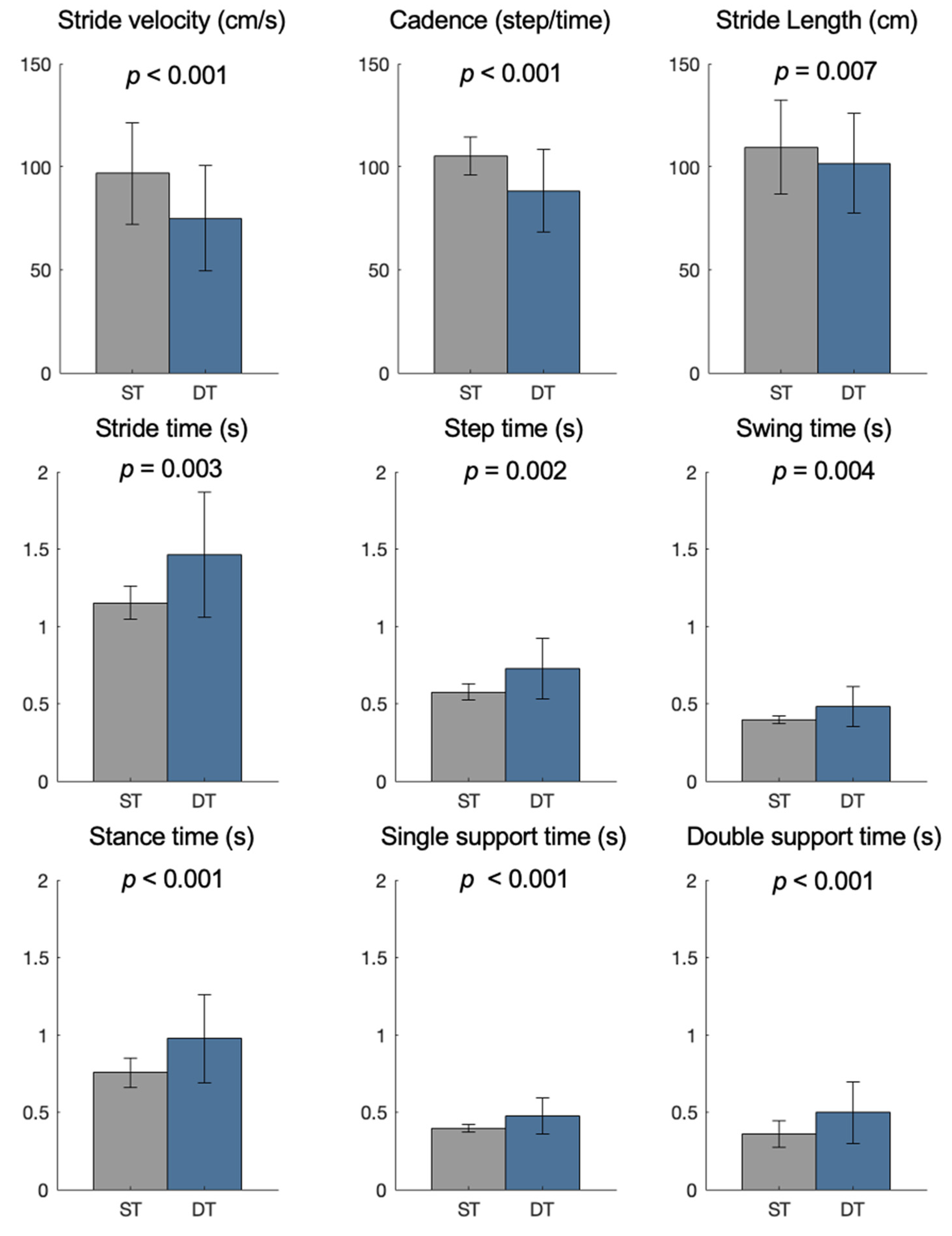
3. Results
3.1. Test–Retest Reliability
3.2. Concurrent Validity
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Mirelman, A.; Bonato, P.; Camicioli, R.; Ellis, T.D.; Giladi, N.; Hamilton, J.L.; Hass, C.J.; Hausdorff, J.M.; Pelosin, E.; Almeida, Q.J. Gait impairments in Parkinson’s disease. Lancet Neurol. 2019, 18, 697–708. [Google Scholar] [CrossRef]
- Jankovic, J. Pathophysiology and clinical assessment of parkinsonian symptoms and signs. In Handbook of Parkinson’s Disease, 3rd ed.; CRC Press: Boca Raton, FL, USA, 2003; pp. 71–107. [Google Scholar]
- Yogev-Seligmann, G.; Hausdorff, J.M.; Giladi, N. The role of executive function and attention in gait. Mov. Disord. 2008, 23, 329–342. [Google Scholar] [CrossRef]
- Kelly, V.E.; Eusterbrock, A.J.; Shumway-Cook, A. A review of dual-task walking deficits in people with Parkinson’s disease: Motor and cognitive contributions, mechanisms, and clinical implications. Parkinsons Dis. 2012, 2012, 918719. [Google Scholar] [CrossRef]
- Rochester, L.; Hetherington, V.; Jones, D.; Nieuwboer, A.; Willems, A.M.; Kwakkel, G.; Van Wegen, E. Attending to the task: Interference effects of functional tasks on walking in Parkinson’s disease and the roles of cognition, depression, fatigue, and balance. Arch. Phys. Med. Rehabil. 2004, 85, 1578–1585. [Google Scholar] [CrossRef] [PubMed]
- Fuller, R.L.; Van Winkle, E.P.; Anderson, K.E.; Gruber-Baldini, A.L.; Hill, T.; Zampieri, C.; Weiner, W.J.; Shulman, L.M. Dual task performance in Parkinson’s disease: A sensitive predictor of impairment and disability. Park. Relat. Disord. 2013, 19, 325–328. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.; Wang, T.; Liu, H.; Jiang, Y.; Wang, Z.; Zhuang, J. Dual-task training on gait, motor symptoms, and balance in patients with Parkinson’s disease: A systematic review and meta-analysis. Clin. Rehabil. 2020, 34, 1355–1367. [Google Scholar] [CrossRef] [PubMed]
- Alberto, S.; Cabral, S.; Proença, J.; Pona-Ferreira, F.; Leitão, M.; Bouça-Machado, R.; Kauppila, L.A.; Veloso, A.P.; Costa, R.M.; Ferreira, J.J.; et al. Validation of quantitative gait analysis systems for Parkinson’s disease for use in supervised and unsupervised environments. BMC Neurol. 2021, 21, 1–14. [Google Scholar] [CrossRef]
- Parati, M.; Ambrosini, E.; DE Maria, B.; Gallotta, M.; Vecchia, L.A.D.; Ferriero, G.; Ferrante, S. The reliability of gait parameters captured via instrumented walkways: A systematic review and meta-analysis. Eur. J. Phys. Rehabil. Med. 2022, 58, 363–377. [Google Scholar] [CrossRef]
- SSalchow-Hömmen, C.; Skrobot, M.; Jochner, M.C.E.; Schauer, T.; Kühn, A.A.; Wenger, N. Review—Emerging Portable Technologies for Gait Analysis in Neurological Disorders. Front. Hum. Neurosci. 2022, 16, 1–24. [Google Scholar] [CrossRef]
- Channa, A.; Popescu, N.; Ciobanu, V. Wearable Solutions for Patients with Parkinson’s Disease and Neurocognitive Disorder: A Systematic Review. Sensors 2020, 20, 2713. [Google Scholar] [CrossRef]
- Subramaniam, S. Insole-Based Systems for Health Monitoring: Current Solutions. Sensors 2022, 22, 438. [Google Scholar] [CrossRef] [PubMed]
- Renner, K.E.; Williams, D.B.; Queen, R.M. The Reliability and Validity of the Loadsol® under Various Walking and Running Conditions. Sensors 2019, 19, 265. [Google Scholar] [CrossRef] [PubMed]
- Price, C.; Parker, D.; Nester, C. Validity and repeatability of three in-shoe pressure measurement systems. Gait Posture 2016, 46, 69–74. [Google Scholar] [CrossRef] [PubMed]
- Loukovitis, A.; Ziagkas, E.; Zekakos, D.X.; Petrelis, A.; Grouios, G. Test-Retest Reliability of PODOSmart® Gait Analysis Insoles. Sensors 2021, 21, 7532. [Google Scholar] [CrossRef]
- Oerbekke, M.S.; Stukstette, M.J.; Schütte, K.; de Bie, R.A.; Pisters, M.F.; Vanwanseele, B. Concurrent validity and reliability of wireless instrumented insoles measuring postural balance and temporal gait parameters. Gait Posture 2017, 51, 116–124. [Google Scholar] [CrossRef]
- Jacobs, D.; Farid, L.; Ferré, S.; Herraez, K.; Gracies, J.-M.; Hutin, E. Evaluation of the Validity and Reliability of Connected Insoles to Measure Gait Parameters in Healthy Adults. Sensors 2021, 21, 6543. [Google Scholar] [CrossRef]
- Lunardini, F.; Malavolti, M.; Pedrocchi, A.L.G.; Borghese, N.A.; Ferrante, S. A mobile app to transparently distinguish single- from dual-task walking for the ecological monitoring of age-related changes in daily-life gait. Gait Posture 2021, 86, 27–32. [Google Scholar] [CrossRef]
- Farid, L.; Jacobs, D.; Do Santos, J.; Simon, O.; Gracies, J.-M.; Hutin, E. FeetMe® Monitor-connected insoles are a valid and reliable alternative for the evaluation of gait speed after stroke. Top. Stroke Rehabil. 2020, 28, 127–134. [Google Scholar] [CrossRef]
- FeetMe® Insoles. Available online: https://feetmehealth.com/ (accessed on 17 June 2022).
- McDonough, A.L.; Batavia, M.; Chen, F.C.; Kwon, S.; Ziai, J. The validity and reliability of the GAITRite system’s measurements: A preliminary evaluation. Arch. Phys. Med. Rehabil. 2001, 82, 419–425. [Google Scholar] [CrossRef]
- Koo, T.K.; Li, M.Y. A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research. J. Chiropr. Med. 2016, 15, 155–163. [Google Scholar] [CrossRef] [Green Version]
- Beninato, M.; Portney, L.G. Applying Concepts of Responsiveness to Patient Management in Neurologic Physical Therapy. J. Neurol. Phys. Ther. 2011, 35, 75–81. [Google Scholar] [CrossRef] [PubMed]
- Atkinson, G.; Nevill, A.M. Statistical Methods For Assessing Measurement Error (Reliability) in Variables Relevant to Sports Medicine. Sports Med. 1998, 26, 217–238. [Google Scholar] [CrossRef] [PubMed]
- Mukaka, M.M. Statistics corner: A guide to appropriate use of correlation coefficient in medical research. Malawi Med. J. 2012, 24, 69–71. [Google Scholar] [PubMed]
- Bland, J.M.; Altman, D.G. Measuring agreement in method comparison studies. Stat. Methods Med. Res. 1999, 8, 135–160. [Google Scholar] [CrossRef]
- Walter, S.D.; Eliasziw, M.; Donner, A. Sample size and optimal designs for reliability studies. Stat. Med. 1998, 17, 101–110. [Google Scholar] [CrossRef]
- Penko, A.L.; Streicher, M.C.; Koop, M.M.; Dey, T.; Rosenfeldt, A.B.; Bazyk, A.S.; Alberts, J.L. Dual-task Interference Disrupts Parkinson’s Gait Across Multiple Cognitive Domains. Neuroscience 2018, 379, 375–382. [Google Scholar] [CrossRef]
- Galletly, R.; Brauer, S.G. Does the type of concurrent task affect preferred and cued gait in people with Parkinson’s disease? Aust. J. Physiother. 2005, 51, 175–180. [Google Scholar] [CrossRef]
- O’Shea, S.; Morris, M.E.; Iansek, R. Dual Task Inference During Gait in People With Parkinson Disease: Effects of Motor Versus Cognitive Secondary Tasks. Phys. Ther. 2002, 82, 888–897. [Google Scholar] [CrossRef]
- Lord, S.; Rochester, L.; Hetherington, V.; Allcock, L.M.; Burn, D. Executive dysfunction and attention contribute to gait interference in “off” state Parkinson’s Disease. Gait Posture. 2010, 31, 169–174. [Google Scholar] [CrossRef]
- Álvarez, I.; Latorre, J.; Aguilar, M.; Pastor, P.; Llorens, R. Validity and sensitivity of instrumented postural and gait assessment using low-cost devices in Parkinson’s disease. J. Neuroeng. Rehabil. 2020, 17, 1–10. [Google Scholar] [CrossRef]
- de Vet, H.C.W.; Terwee, C.B.; Knol, D.L.; Bouter, L.M. When to use agreement versus reliability measures. J. Clin. Epidemiol. 2006, 59, 1033–1039. [Google Scholar] [CrossRef] [PubMed]
- Kimmeskamp, S.; Hennig, E.M. Heel to toe motion characteristics in Parkinson patients during free walking. Clin. Biomech. 2001, 16, 806–812. [Google Scholar] [CrossRef]
- Terwee, C.B.; Bot, S.D.M.; de Boer, M.R.; van der Windt, D.A.W.M.; Knol, D.L.; Dekker, J.; Bouter, L.M.; de Vet, H.C.W. Quality criteria were proposed for measurement properties of health status questionnaires. J. Clin. Epidemiol. 2007, 60, 34–42. [Google Scholar] [CrossRef] [PubMed]
- Soulard, J.; Vaillant, J.; Balaguier, R.; Vuillerme, N. Spatio-temporal gait parameters obtained from foot-worn inertial sensors are reliable in healthy adults in single- and dual-task conditions. Sci. Rep. 2021, 11, 1–15. [Google Scholar] [CrossRef]
- Dolatabadi, E.; Taati, B.; Mihailidis, A. Concurrent validity of the Microsoft Kinect for Windows v2 for measuring spatiotemporal gait parameters. Med. Eng. Phys. 2016, 38, 952–958. [Google Scholar] [CrossRef]
- Turcato, A.M.; Godi, M.; Giardini, M.; Arcolin, I.; Nardone, A.; Giordano, A.; Schieppati, M. Abnormal gait pattern emerges during curved trajectories in high-functioning Parkinsonian patients walking in line at normal speed. PLoS ONE 2018, 13, e0197264. [Google Scholar] [CrossRef]
- Martínez, M.; Villagra, F.; Castellote, J.M.; Pastor, M.A. Kinematic and Kinetic Patterns Related to Free-Walking in Parkinson’s Disease. Sensors 2018, 18, 4224. [Google Scholar] [CrossRef]
- Chatzaki, C.; Skaramagkas, V.; Tachos, N.; Christodoulakis, G.; Maniadi, E.; Kefalopoulou, Z.; Fotiadis, D.; Tsiknakis, M. The Smart-Insole Dataset: Gait Analysis Using Wearable Sensors with a Focus on Elderly and Parkinson’s Patients. Sensors 2021, 21, 2821. [Google Scholar] [CrossRef]
- Lu, H.; He, B.; Gao, B. Emerging electrochemical sensors for life healthcare. Eng. Regen. 2021, 2, 175–181. [Google Scholar] [CrossRef]
- Asci, F.; Vivacqua, G.; Zampogna, A.; D’Onofrio, V.; Mazzeo, A.; Suppa, A. Wearable Electrochemical Sensors in Parkinson’s Disease. Sensors 2022, 22, 951. [Google Scholar] [CrossRef]
| Characteristics | N = 25 |
|---|---|
| Age | 69 (7) |
| Gender (Male/Female) | 21/4 |
| Weight (kg) | 75.0 (10.2) |
| Height (cm) | 169.2 (8.8) |
| BMI (kg/m2) | 26.2 (3.4) |
| Duration of the disease (years) | 4 (3) |
| UPDRS-part III | 16.9 (3.7) |
| mH&Y score | 2.0 (0.6) |
| Condition | Gait Parameter | Visit T1 Mean (SD) | Visit T2 Mean (SD) | T1 vs. T2 p-Value | ICC [95%CI] | MDC | MDC% |
|---|---|---|---|---|---|---|---|
| Single-task | Stride velocity (cm/s) | 95.6 (24.4) | 92.7 (22.7) | 0.185 | 0.95 [0.88–0.98] | 15.04 | 16.0 |
| Cadence (step/min) | 105.4 (9.3) | 104.4 (9.9) | 0.376 | 0.91 [0.80–0.96] | 7.94 | 7.6 | |
| Stride length (cm) | 107.5 (22.2) | 105.6 (21.3) | 0.248 | 0.97 [0.92–0.99] | 11.12 | 10.4 | |
| Step time (s) | 0.58 (0.06) | 0.59 (0.06) | 0.136 | 0.92 [0.82–0.97] | 0.04 | 7.6 | |
| Stride time (s) | 1.14 (0.11) | 1.16 (0.11) | 0.344 | 0.92 [0.82–0.96] | 0.09 | 7.6 | |
| Swing time (s) | 0.39 (0.04) | 0.39 (0.04) | 0.956 | 0.91 [0.80–0.96] | 0.03 | 8.3 | |
| Stance time (s) | 0.77 (0.08) | 0.78 (0.08) | 0.139 | 0.92 [0.82–0.97] | 0.06 | 8.0 | |
| Single support time (s) | 0.39 (0.04) | 0.39 (0.04) | 0.861 | 0.91 [0.81–0.96] | 0.03 | 8.8 | |
| Double support time (s) | 0.36 (0.05) | 0.37 (0.05) | 0.087 | 0.88 [0.73–0.95] | 0.05 | 12.9 | |
| Dual-task | Stride velocity (cm/s) | 73.0 (26.0) | 75.0 (24.3) | 0.449 | 0.93 [0.85–0.97] | 18.03 | 24.5 |
| Cadence (step/min) | 87.0 (21.0) | 88.8 (19.7) | 0.343 | 0.94 [0.87–0.98] | 13.48 | 15.3 | |
| Stride length (cm) | 99.8 (21.9) | 100.3 (22.7) | 0.801 | 0.95 [0.89–0.98] | 13.53 | 13.5 | |
| Step time (s) | 0.74 (0.20) | 0.73 (0.19) | 0.657 | 0.93 [0.85–0.97] | 0.14 | 18.7 | |
| Stride time (s) | 1.49 (0.44) | 1.44 (0.40) | 0.968 | 0.90 [0.78–0.96] | 0.37 | 25.0 | |
| Swing time (s) | 0.51 (0.16) | 0.49 (0.14) | 0.382 | 0.91 [0.80–0.96] | 0.12 | 24.7 | |
| Stance time (s) | 0.96 (0.25) | 0.96 (0.27) | 0.607 | 0.92 [0.81–0.96] | 0.21 | 21.8 | |
| Single-support time (s) | 0.50 (0.14) | 0.49 (0.14) | 0.510 | 0.94 [0.86–0.97] | 0.10 | 19.4 | |
| Double-support time (s) | 0.46 (0.13) | 0.46 (0.15) | 0.737 | 0.80 [0.53–0.91] | 0.17 | 38.2 |
| Condition | Gait Parameter | Visit T1 Mean (SD) | Visit T2 Mean (SD) | T1 vs. T2 p-Value | ICC [95%CI] | MDC | MDC% |
|---|---|---|---|---|---|---|---|
| Single-task | Stride velocity (cm/s) | 97.6 (25.0) | 95.7 (24.6) | 0.242 | 0.97 [0.94–0.99] | 18.20 | 24.6 |
| Cadence (step/min) | 105.8 (9.1) | 104.6 (9.9) | 0.317 | 0.91 [0.80–0.96] | 7.92 | 7.5 | |
| Stride length (cm) | 109.8 (22.8) | 109.1 (22.8) | 0.455 | 0.99 [0.97–0.99] | 6.93 | 6.3 | |
| Step time (s) | 0.57 (0.05) | 0.58 (0.06) | 0.291 | 0.92 [0.81–0.96] | 0.05 | 7.8 | |
| Stride time (s) | 1.15 (0.11) | 1.16 (0.12) | 0.250 | 0.92 [0.82–0.96] | 0.09 | 7.7 | |
| Swing time (s) | 0.40 (0.03) | 0.40 (0.03) | 0.928 | 0.88 [0.72–0.95] | 0.03 | 6.9 | |
| Stance time (s) | 0.75 (0.09) | 0.76 (0.10) | 0.206 | 0.94 [0.87–0.98] | 0.06 | 8.5 | |
| Single support time (s) | 0.40 (0.03) | 0.39 (0.03) | 0.830 | 0.87 [0.70–0.94] | 0.03 | 7.1 | |
| Double support time (s) | 0.36 (0.09) | 0.36 (0.09) | 0.058 | 0.98 [0.95–0.99] | 0.04 | 10.3 | |
| Dual-task | Stride velocity (cm/s) | 74.3 (26.6) | 75.7 (25.6) | 0.561 | 0.94 [0.88–0.98] | 17.13 | 22.8 |
| Cadence (step/min) | 87.6 (20.9) | 89.1 (20.0) | 0.436 | 0.94 [0.87–0.98] | 13.42 | 15.2 | |
| Stride length (cm) | 101.6 (24.2) | 101.4 (24.8) | 0.989 | 0.98 [0.95–0.99] | 10.51 | 10.4 | |
| Step time (s) | 0.74 (0.21) | 0.72 (0.20) | 0.932 | 0.93 [0.83–0.97] | 0.16 | 21.3 | |
| Stride time (s) | 1.48 (0.44) | 1.44 (0.41) | 0.989 | 0.91 [0.80–0.96] | 0.35 | 23.8 | |
| Swing time (s) | 0.49 (0.14) | 0.47 (0.12) | 0.476 | 0.94 [0.87–0.97] | 0.09 | 18.9 | |
| Stance time (s) | 0.97 (0.29) | 0.96 (0.30) | 0.732 | 0.88 [0.73–0.95] | 0.29 | 29.5 | |
| Single-support time (s) | 0.48 (0.13) | 0.47 (0.11) | 0.536 | 0.87 [0.71–0.94] | 0.12 | 25.5 | |
| Double-support time (s) | 0.50 (0.20) | 0.49 (0.22) | 0.619 | 0.86 [0.67–0.94] | 0.22 | 44.7 |
| Gait Parameter | Single-Task Condition | Dual-Task Condition | ||
|---|---|---|---|---|
| Bias [95% LoA] | Corr | Bias [95% LoA] | Corr | |
| Stride velocity (cm/s) | 2.50 [−4.17,9.17] | 0.99 | 0.97 [−4.09,6.02] | 1.00 |
| Cadence (step/min) | 0.27 [−2.70,3.25] | 0.99 | 0.42 [−1.14,1.98] | 1.00 |
| Stride length (cm) | 2.89 [−4.04,9.82] | 0.99 | 1.45 [−6.67,9.56] | 0.99 |
| Step time (s) | −0.01 [−0.04,0.02] | 0.96 | 0.00 [−0.10,0.09] | 0.97 |
| Stride time (s) | 0.00 [−0.04,0.04] | 0.98 | −0.02 [−0.02,0.02] | 1.00 |
| Swing time (s) | 0.00 [−0.06,0.06] | 0.61 | −0.02 [−0.10,0.06] | 0.94 |
| Stance time (s) | −0.02 [−0.10,0.06] | 0.92 | 0.01 [−0.10,0.11] | 0.99 |
| Single support time (s) | 0.00 [−0.06,0.06] | 0.68 | −0.02 [−0.14,0.10] | 0.90 |
| Double support time (s) | −0.01 [−0.13,0.11] | 0.73 | 0.04 [−0.14,0.22] | 0.94 |
| Gait Parameter | Single-Task Condition | Dual-Task Condition | ||
|---|---|---|---|---|
| Bias [95% LoA] | Corr | Bias [95% LoA] | Corr | |
| Stride velocity (cm/s) | 2.04 [−9.11,13.20] | 0.97 | 0.35 [−9.98,10.68] | 0.98 |
| Cadence (step/min) | 0.16 [−10.43,10.75] | 0.87 | 0.49 [−9.72,10.71] | 0.96 |
| Stride length (cm) | 2.48 [−9.13,14.10] | 0.96 | 0.37 [−12.63,13.37] | 0.95 |
| Step time (s) | −0.01 [−0.10,0.08] | 0.79 | −0.01 [−0.21,0.19] | 0.84 |
| Stride time (s) | 0.00 [−0.08,0.08] | 0.94 | 0.00 [−0.11,0.11] | 0.99 |
| Swing time (s) | 0.00 [−0.08,0.07] | 0.61 | −0.03 [−0.15,0.10] | 0.86 |
| Stance time (s) | −0.01 [−0.12,0.11] | 0.84 | 0.01 [−0.22,0.24] | 0.88 |
| Single support time (s) | 0.00 [−0.09,0.09] | 0.54 | −0.03 [−0.19,0.14] | 0.73 |
| Double support time (s) | 0.01 [−0.13,0.14] | 0.69 | 0.05 [−0.17,0.27] | 0.83 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Parati, M.; Gallotta, M.; Muletti, M.; Pirola, A.; Bellafà, A.; De Maria, B.; Ferrante, S. Validation of Pressure-Sensing Insoles in Patients with Parkinson’s Disease during Overground Walking in Single and Cognitive Dual-Task Conditions. Sensors 2022, 22, 6392. https://doi.org/10.3390/s22176392
Parati M, Gallotta M, Muletti M, Pirola A, Bellafà A, De Maria B, Ferrante S. Validation of Pressure-Sensing Insoles in Patients with Parkinson’s Disease during Overground Walking in Single and Cognitive Dual-Task Conditions. Sensors. 2022; 22(17):6392. https://doi.org/10.3390/s22176392
Chicago/Turabian StyleParati, Monica, Matteo Gallotta, Manuel Muletti, Annalisa Pirola, Alice Bellafà, Beatrice De Maria, and Simona Ferrante. 2022. "Validation of Pressure-Sensing Insoles in Patients with Parkinson’s Disease during Overground Walking in Single and Cognitive Dual-Task Conditions" Sensors 22, no. 17: 6392. https://doi.org/10.3390/s22176392
APA StyleParati, M., Gallotta, M., Muletti, M., Pirola, A., Bellafà, A., De Maria, B., & Ferrante, S. (2022). Validation of Pressure-Sensing Insoles in Patients with Parkinson’s Disease during Overground Walking in Single and Cognitive Dual-Task Conditions. Sensors, 22(17), 6392. https://doi.org/10.3390/s22176392







