A Nudge-Inspired AI-Driven Health Platform for Self-Management of Diabetes
Abstract
:1. Introduction
- Presentation of a holistic diabetes self-management platform that has been co-designed with patients and clinicians to ensure the platform is fit for purpose. Through the co-design process, it was identified that a self-management platform requires a cross-platform mobile app that is personalized to the patient’s cultural nuances and a clinician web app that allows for an improved patient–clinician communication pipeline.
- The development and implementation of a macronutrient detection algorithm (MDA) that uses AI-driven image analytics for nutrition management and behavior intervention through the incorporation of nudge theory. The platform aims to improve self-management among patients and enable them to undergo a sustained behavior change. An application of the platform has been demonstrated through an illustrative case study. Further, a technical evaluation is conducted to understand the performance of the MDA to meet the personalization requirements of patients with type II diabetes.
2. Related Work
2.1. Current mHealth Applications
2.2. Nutrition Recommendation
- Collaborative Filtering Recommender (CF) Systems: CF systems are known to be one of the most researched recommender systems [21]. This system uses a nearest neighbors approach, where it identifies other users who have a similar taste in the recommendation items as the user and recommends items that the neighbors like [25]. For this system to work, the user needs to have rated some of the existing items so the CF system can learn what the user likes and does not like.
- Content-based Recommender (CB) Systems: CB systems analyze the profile metadata of a user (likes, dislikes, etc.) to create a criterion, which is then used to find items that fulfill the criterion [20,21]. Usually, this method involves a text-mining algorithm that allows the system to identify key terms to match with the criterion [20].
- Knowledge-based Recommender (KB) Systems: KB systems use knowledge about the user and items to pursue recommendations based on reasoning related to whether the items meet the requirements of the user [26]. An example in relation to nutrition would be already having information such as what dishes the user likes/dislikes, what ingredients the user likes or dislikes, known allergies, etc.
- Deep Learning Recommender (DL) Systems: DL systems can capture nonlinear and nontrivial relationship between the user and the item, which may not be as quickly identifiable through a CB, CF, or KB system [27,28]. DL systems are the newer recommender system in this list, as a survey suggests exponential growth in research publications around DL recommender systems [27].
- Hybrid Recommender (HR) Systems: HR systems are based on the combination of the above-mentioned techniques. Studies have found HR systems to be the preferred approach as these systems could allow one system to cover the disadvantages of the other system [18,29]. For example, a well-known problem with the CF system is a “cold-start” problem [30]. This problem highlights the lack of information about the user unless the user starts using the system so that over time the system improves its recommendations. A way to overcome the cold-start issue is by pairing the CF system with the KB or CB system. Given the nutrition space, one can see that now there is some foundational information inherited from the user (through CF/KB system strategies) even before the user is required to use the system to log and rate meals. This allows for improved recommendations from the very beginning.
2.3. Behavioral Intervention
2.4. Summary of Gaps
3. Behavioral Intervention: Nudge Theory
- The political philosophy—libertarian paternalism, where individuals are “actively guided in their best interest but they remain at liberty to behave differently” [45].
- Framing: The presentation of a subject matter in order to subtly influence an individual’s choice and behaviors [49];
- Reminders: Use of smartly constructed reminders [49];
- Gamification: Using the principle of gameplay mechanics to influence behavior [49];
- Social modeling: E.g., running group sessions where individuals learn from each other’s experiences [49];
- Social influence: Use of external factors as a point of influence, e.g., a weekly summary of the patients’ performance, in relation to a group of individuals [49].
4. Adapted 4-Cycle Design Science Research Methodology for Design of a Diabetes Self-Management Platform
5. Diabetes Self-Management Platform Architecture
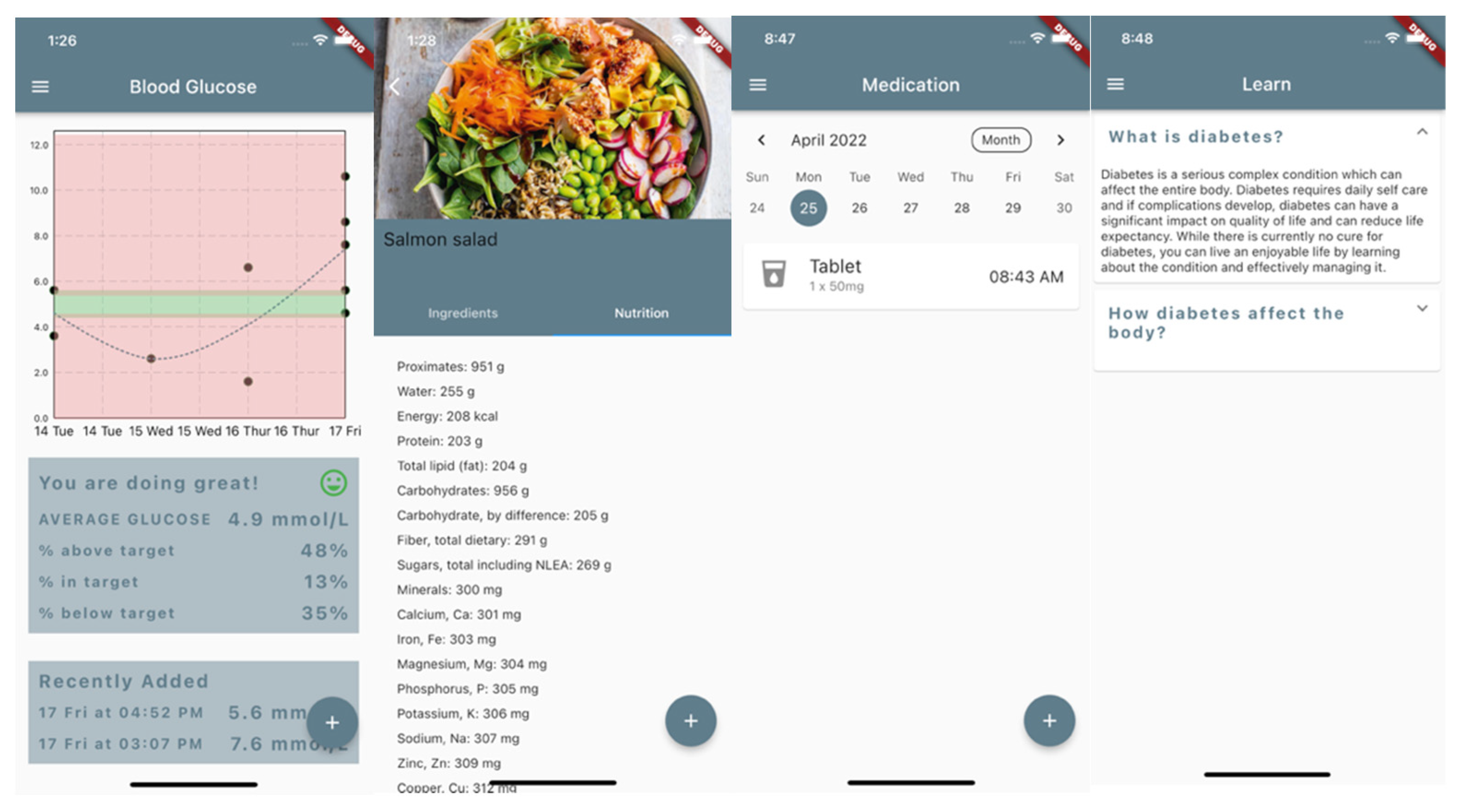
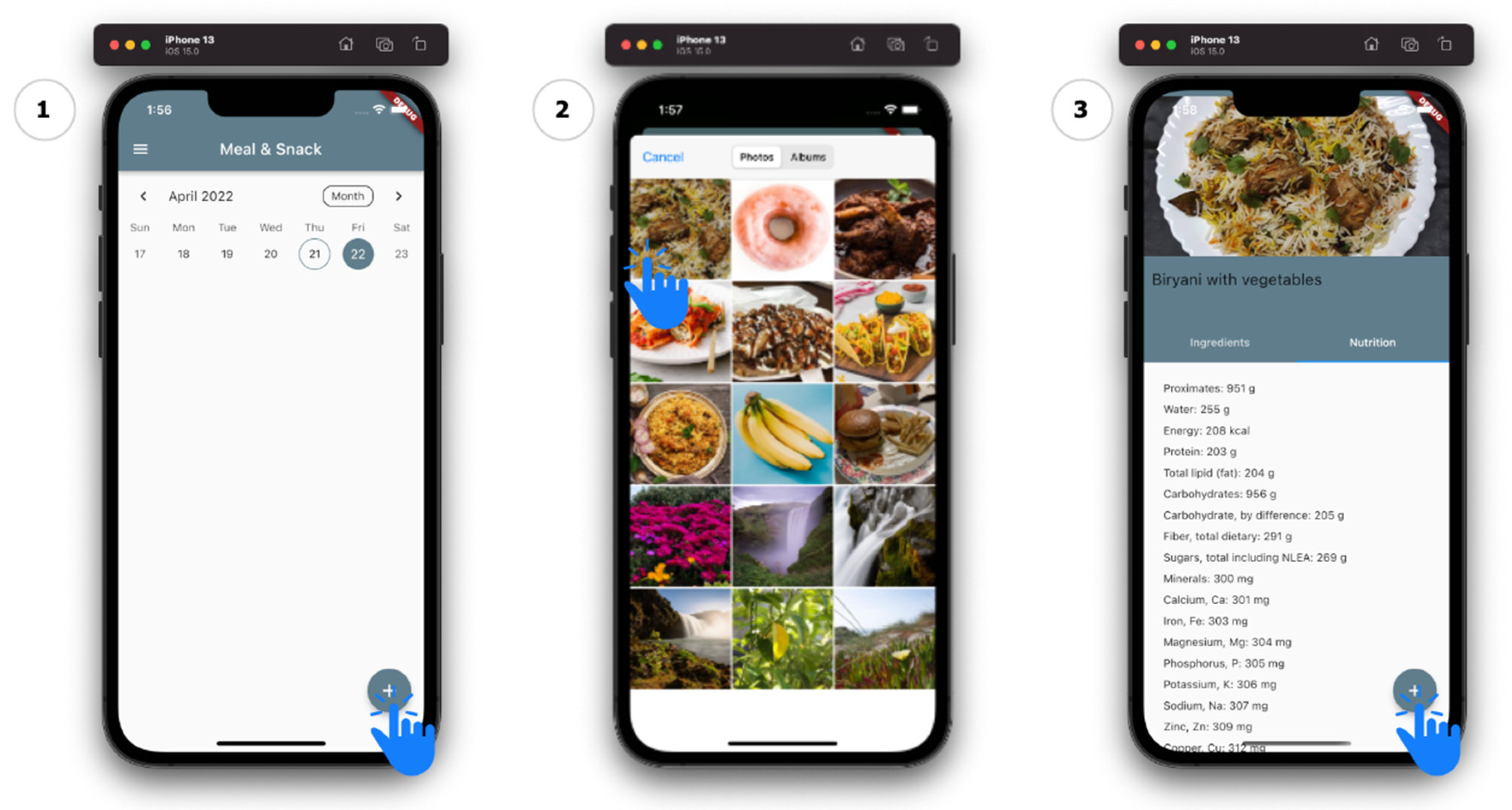
5.1. Diabetes Self-Management: Mobile App
| Algorithm 1. MDA Pseudocode |
| 1: input: meal image img 2: output: nutrition information of meal image res 3: function getimage 4: pass in: nothing 5: img ← picked image from gallery 6: pass out: img 7: endfunction 8: function predict 9: pass in: img 10: o ← NULL 11: recognitions ← Deep Learning Model (img) 12: for each r in recognitions do 13: if o = NULL then 14: o ← r 15: else 16: if r.confidence > o.confidence then 17: o ← r 18: endif 19: endif 20: endfor 21: pass out: o 22: endfunction 23: function getnutrition 24: pass in: name 25: res ← send request to API for info 26: pass out: res 27: endfunction 28: begin 29: img ← getimage 30: prediction ← predict(img) 31: if prediction ≠ NULL 32: res ← getnutrition(prediction.name) 33: endif 34: return res 35: end |
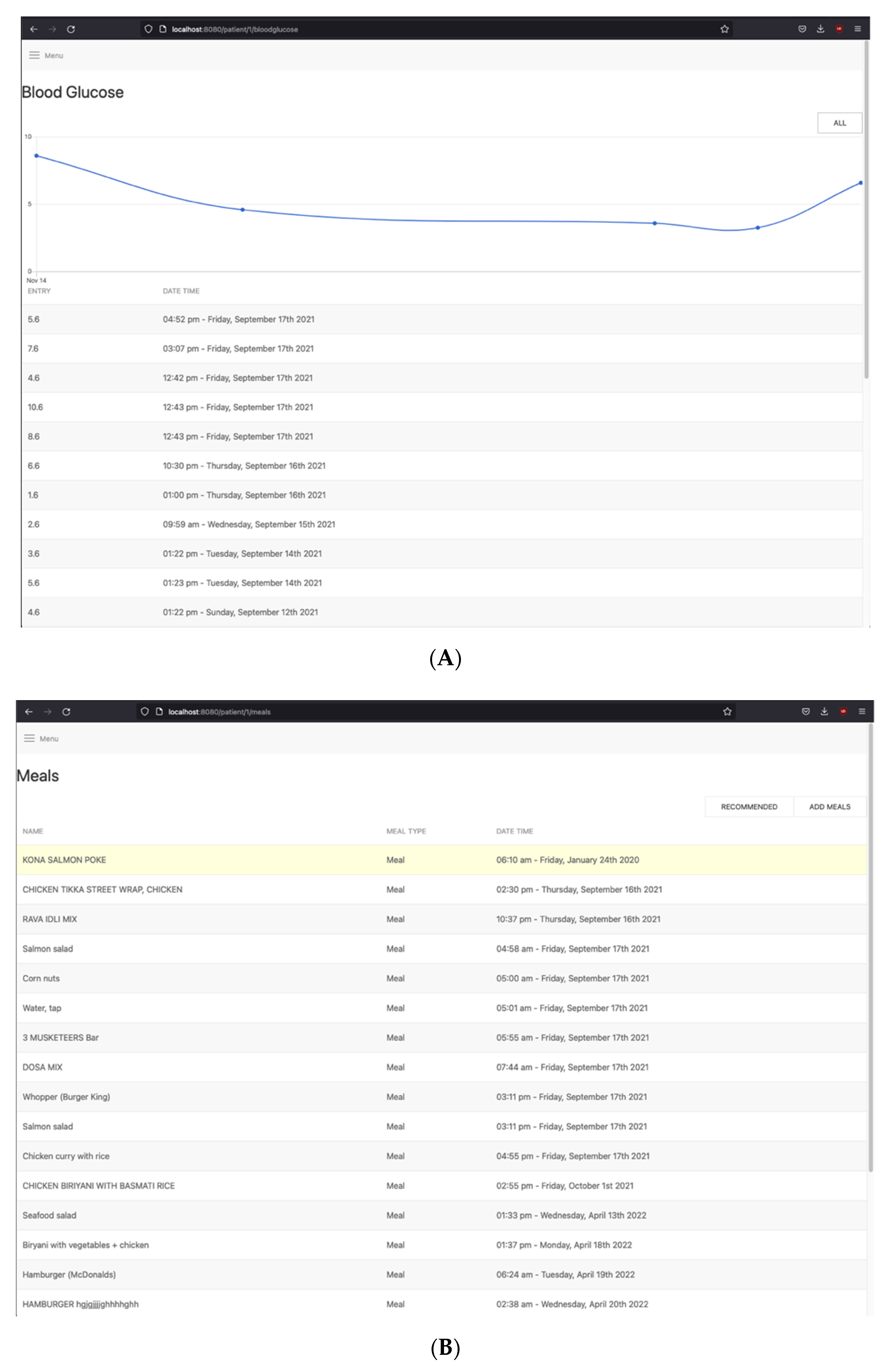
5.2. Diabetes Self-Management: Clinician Web App
5.3. Middleware
6. Diabetes Self-Management Platform Implementation and Evaluation
6.1. Diabetes Self-Management Platform: Mobile App Implementation
6.2. Macronutrient Detection Algorithm (MDA)—Implementation and Evaluation
- The pretrained model is converted to a mobile-device-compatible TensorFlow Lite (tflite) model and deployed on the mobile app along with the list of classes that the model can classify correctly.
- The model is configured to return three predictions of what it believes the item to be, where the structure of the object includes the label, the confidence, and the class index.
- The result is sorted based on the confidence and provided what the model thinks is the item. To handle incorrect classifications, the Add Meal page allows the user to manually edit the item identified.
- Food_v1 [54]
- Model based off the Mobilenet v1 architecture
- Trained on 2000+ images, on various dataset
- Monk_v1 Classifier [55]
- Model based off the Gluon VGG13bn architecture
- Trained on the Food101 dataset
- Pretrained YOLOv3s [56]
- Model based off the Efficientnet-B4 classification model
- Self-collected dataset
- Correctness: A score of 0, 0.5, or 1 was provided based on the correctness of the prediction. This indicator helps better understand the skill of the model in predicting different meals accurately.
- E.g., If a model predicted “Napolitana Pizza” instead of “Margherita Pizza”, it was given a score of 0.5 as it was able to identify that the item was pizza.
- If incorrect, the model was given a score of 0.
- If correct, the model was given a score of 1.
- Confidence: In deep learning models, confidence defines the probability of the classification for various classes. In our study, this indicator is used to verify the confidence of the model for a given cuisine.
- Speed: Model prediction speed. This indicator highlights the prediction time of a model in a mobile device.
6.3. Diabetes Self-Management Platform: Clinician Web App
6.4. Middleware
7. Application of the Personalized Diabetes Self-Management Platform in Use
7.1. Use Case 1: Patient–Clinician Pipeline and Nutrition Recommendation
7.2. Use Case 2: Nudge-Inspired MDA
8. Discussion and Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Cho, N.H.; Shaw, J.E.; Karuranga, S.; Huang, Y.; da Rocha Fernandes, J.D.; Ohlrogge, A.W.; Malanda, B. IDF Diabetes Atlas: Global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res. Clin. Pract. 2018, 138, 271–281. [Google Scholar] [CrossRef]
- Saeedi, P.; Petersohn, I.; Salpea, P.; Malanda, B.; Karuranga, S.; Unwin, N.; Colagiuri, S.; Guariguata, L.; Motala, A.A.; Ogurtsova, K.; et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: Results from the International Diabetes Federation Diabetes Atlas, 9th edition. Diabetes Res. Clin. Pract. 2019, 157, 107843. [Google Scholar] [CrossRef] [Green Version]
- Kharroubi, A.T.; Darwish, H.M. Diabetes Mellitus: The Epidemic of the Century. World J. Diabetes 2015, 6, 850–867. [Google Scholar] [CrossRef]
- Magliano, D.J.; Peeters, A.; Vos, T.; Sicree, R.; Shaw, J.; Sindall, C.; Haby, M.; Begg, S.J.; Zimmet, P.Z. Projecting the burden of diabetes in Australia—What is the size of the matter? Aust. N. Z. J. Public Health 2009, 33, 540–543. [Google Scholar] [CrossRef]
- National Diabetes Services. Diabetes-Related Complication. Available online: https://www.ndss.com.au/ (accessed on 7 February 2022).
- Khan, R.M.M.; Chua, Z.J.Y.; Tan, J.C.; Yang, Y.; Liao, Z.; Zhao, Y. From Pre-Diabetes to Diabetes: Diagnosis, Treatments and Translational Research. Medicina 2019, 55, 546. [Google Scholar] [CrossRef] [Green Version]
- Wu, Y.; Ding, Y.; Tanaka, Y.; Zhang, W. Risk Factors Contributing to Type 2 Diabetes and Recent Advances in the Treatment and Prevention. Int. J. Med. Sci. 2014, 11, 1185–1200. [Google Scholar] [CrossRef] [Green Version]
- Adu, M.D.; Malabu, U.H.; Malau-Aduli, A.E.O.; Malau-Aduli, B.S. Enablers and barriers to effective diabetes self-management: A multi-national investigation. PLoS ONE 2019, 14, e0217771. [Google Scholar] [CrossRef] [Green Version]
- Joachim, S.; Jayaraman, P.P.; Forkan, A.R.M.; Morshed, A. Design and Development of a Diabetes Self-Management Platform: A Case for Responsible Information System Development. In Proceedings of the 54th Hawaii International Conference on System Sciences, Maui, HI, USA, 5 January 2021. [Google Scholar]
- Cortez, N.G.; Cohen, I.G.; Kesselheim, A.S. FDA Regulation of Mobile Health Technologies. N. Engl. J. Med. 2014, 371, 372–379. [Google Scholar] [CrossRef] [Green Version]
- Fu, H.; McMahon, S.; Gross, C.R.; Adam, T.J.; Wyman, J.F. Usability and clinical efficacy of diabetes mobile applications for adults with type 2 diabetes: A systematic review. Diabetes Res. Clin. Pract. 2017, 131, 70–81. [Google Scholar] [CrossRef]
- Chavez, S.; Fedele, D.; Guo, Y.; Bernier, A.; Smith, M.; Warnick, J.; Modave, F. Mobile Apps for the Management of Diabetes. Diabetes Care 2017, 40, e145–e146. [Google Scholar] [CrossRef] [Green Version]
- Viennot, N.; Garcia, E.; Nieh, J. A Measurement Study of Google Play. In Proceedings of the 2014 ACM International Conference on Measurement and Modeling of Computer Systems, Austin, TX, USA, 16–20 June 2014; pp. 221–233. [Google Scholar]
- Danaher, B.; Brendryen, H.; Seeley, J.R.; Tyler, M.S.; Woolley, T. From Black Box to Toolbox: Outlining Device Functionality, Engagement Activities, and the Pervasive Information Architecture of Mhealth Interventions. Internet Interv. 2015, 2, 91–101. [Google Scholar] [CrossRef] [Green Version]
- Jimenez, G.; Lum, E.; Car, J. Examining Diabetes Management Apps Recommended from a Google Search: Content Analysis. JMIR mHealth uHealth 2019, 7, e11848. [Google Scholar] [CrossRef] [Green Version]
- Huang, Z.; Soljak, M.; Boehm, B.O.; Car, J. Clinical relevance of smartphone apps for diabetes management: A global overview. Diabetes Metab. Res. Rev. 2018, 34, e2990. [Google Scholar] [CrossRef]
- Villalba-Mora, E.; Peinado-Martínez, I.; Pozo, F. eHealth and Diabetes: Designing a Novel System for Remotely Monitoring Older Adults with Type 2 Diabetes. In Diabetes in Old Age; Wiley: Hoboken, NJ, USA, 2017. [Google Scholar]
- Sami, W.; Tahir, A.; Butt, N.; Ab Hamid, M.R. Effect of Diet on Type 2 Diabetes Mellitus: A Review. Int. J. Health Sci. 2017, 11, 65–71. [Google Scholar]
- Marshall, M.C. Diabetes in African Americans. Postgrad. Med J. 2005, 81, 734–740. [Google Scholar] [CrossRef]
- Valdez, A.C.; Ziefle, M.; Verbert, K.; Felfernig, A.; Holzinger, A. Recommender Systems for Health Informatics: State-of-the-Art and Future Perspectives. In Machine Learning for Health Informatics; Lecture Notes in Computer Science; Springer: Cham, Switzerland, 2016; Volume 9605. [Google Scholar]
- Tran, T.N.T.; Atas, M.; Felfernig, A.; Stettinger, M. An Overview of Recommender Systems in the Healthy Food Domain. J. Intell. Inf. Syst. 2018, 50, 501–526. [Google Scholar] [CrossRef]
- Agapito, G.; Simeoni, M.; Calabrese, B.; Caré, I.; Lamprinoudi, T.; Guzzi, P.H.; Pujia, A.; Fuiano, G.; Cannataro, M. DIETOS: A dietary recommender system for chronic diseases monitoring and management. Comput. Methods Programs Biomed. 2018, 153, 93–104. [Google Scholar] [CrossRef]
- Phanich, M.; Pholkul, P.; Phimoltares, S. Food Recommendation System Using Clustering Analysis for Diabetic Patients. In Proceedings of the 2010 International Conference on Information Science and Applications, ICISA, Seoul, Korea, 21–23 April 2010. [Google Scholar]
- Yang, L.; Hsieh, C.K.; Yang, H.; Pollak, J.P.; Dell, N.; Belongie, S.; Cole, C.; Estrin, D. Yum-Me: A Personalized Nutrient-Based Meal Recommender System. ACM Trans. Inf. Syst. 2017, 36, 7. [Google Scholar] [CrossRef]
- Ekstrand, M.; John, D.; Riedl, T.; Konstan, J.A. Collaborative Filtering Recommender Systems. Found. Trends Hum. Comput. Interact. 2011, 4, 81–173. [Google Scholar] [CrossRef]
- Burke, R. Knowledge-Based Recommender Systems. In Encyclopedia of Library and Information Systems; Routledge: Oxfordshire, UK, 2000; Volume 69. [Google Scholar]
- Zhang, S.; Yao, L.; Sun, A.; Tay, Y. Deep Learning Based Recommender System: A Survey and New Perspectives. ACM Comput. Surv. 2019, 52, 5. [Google Scholar] [CrossRef] [Green Version]
- Zhou, L.; Zhang, Z.; Zhao, L.; Yang, P. Attention-Based Bilstm Models for Personality Recognition from User-Generated Content. Inf. Sci. 2022, 596, 460–471. [Google Scholar] [CrossRef]
- Abhari, S.; Safdari, R.; Azadbakht, L.; Lankarani, K.B.; Kalhori, S.R.N.; Honarvar, B.; Abhari, K.; Ayyoubzadeh, S.M.; Karbasi, Z.; Zakerabasali, S.; et al. A Systematic Review of Nutrition Recommendation Systems: With Focus on Technical Aspects. J. Biomed. Phys. Eng. 2019, 9, 591–602. [Google Scholar] [CrossRef]
- Lam, X.; Vu, T.; Le, T.; Duong, A. Addressing Cold-Start Problem in Recommendation Systems. In Proceedings of the 2nd International Conference on Ubiquitous Information Management and Communication, Suwon, Korea, 31 January–1 February 2008; pp. 208–211. [Google Scholar]
- Balducci, S.; D’errico, V.; Haxhi, J.; Sacchetti, M.; Orlando, G.; Cardelli, P.; Vitale, M.; Bollanti, L.; Conti, F.; Zanuso, S.; et al. Effect of a Behavioral Intervention Strategy on Sustained Change in Physical Activity and Sedentary Behavior in Patients with Type 2 Diabetes. JAMA 2019, 321, 880–890. [Google Scholar] [CrossRef] [Green Version]
- Wickramasinghe, N.; John, B.; George, J.; Vogel, D. Achieving Value-Based Care in Chronic Disease Management: Intervention Study. JMIR Diabetes 2019, 4, e10368. [Google Scholar] [CrossRef] [Green Version]
- Quinn, C.C.; Swasey, K.K.; Torain, J.M.; Shardell, M.D.; Terrin, M.L.; A Barr, E.; Gruber-Baldini, A.L.; Gee, P.; Farmer, A. An mHealth Diabetes Intervention for Glucose Control: Health Care Utilization Analysis. JMIR mHealth uHealth 2018, 6, e10776. [Google Scholar] [CrossRef] [Green Version]
- Saponaro, M.; Vemuri, A.; Dominick, G.; Decker, K. Contextualization and Individualization for Just-in-Time Adaptive Interventions to Reduce Sedentary Behavior. In Proceedings of the Conference on Health, Inference, and Learning, Virtual, 8–10 April 2021; pp. 246–256. [Google Scholar]
- Misawa, D.; Fukuyoshi, J.; Sengoku, S. Cancer Prevention Using Machine Learning, Nudge Theory and Social Impact Bond. Int. J. Environ. Res. Public Health 2020, 17, 790. [Google Scholar] [CrossRef] [Green Version]
- Yom-Tov, E.; Feraru, G.; Kozdoba, M.; Mannor, S.; Tennenholtz, M.; Hochberg, I. Encouraging Physical Activity in Patients with Diabetes: Intervention Using a Reinforcement Learning System. J. Med Internet Res. 2017, 19, e338. [Google Scholar] [CrossRef]
- Rabbi, M.; Aung, M.; Zhang, M.; Choudhury, T. Mybehavior: Automatic Personalized Health Feedback from User Behaviors and Preferences Using Smartphones. In Proceedings of the 2015 ACM International Joint Conference on Pervasive and Ubiquitous Computing, Osaka, Japan, 7–11 September 2015; pp. 707–718. [Google Scholar]
- Oftedal, B.; Bru, E.; Karlsen, B. Motivation for diet and exercise management among adults with type 2 diabetes. Scand. J. Caring Sci. 2011, 25, 735–744. [Google Scholar] [CrossRef]
- Weinger, K. The Effect of a Structured Behavioral Intervention on Poorly Controlled Diabetes. Arch. Intern. Med. 2011, 171, 1990–1999. [Google Scholar] [CrossRef] [Green Version]
- Lauffenburger, J.C.; Ghazinouri, R.; Jan, S.; Makanji, S.; Ferro, C.A.; Lewey, J.; Wittbrodt, E.; Lee, J.; Haff, N.; Fontanet, C.; et al. Impact of a novel pharmacist-delivered behavioral intervention for patients with poorly-controlled diabetes: The Enhancing outcomes through Goal Assessment and Generating Engagement in Diabetes Mellitus (ENGAGE-DM) pragmatic randomized trial. PLoS ONE 2019, 14, e0214754. [Google Scholar] [CrossRef]
- Quinn, C.C.; Shardell, M.D.; Terrin, M.L.; Barr, E.A.; Ballew, S.H.; Gruber-Baldini, A.L. Cluster-Randomized Trial of a Mobile Phone Personalized Behavioral Intervention for Blood Glucose Control. Diabetes Care 2011, 36, 3850. [Google Scholar] [CrossRef] [Green Version]
- Debong, F.; Mayer, H.; Kober, J. Real-World Assessments of Mysugr Mobile Health App. Diabetes Technol. Ther. 2019, 21, S235–S240. [Google Scholar] [CrossRef]
- Osborn, C.Y.; Van Ginkel, J.R.; Rodbard, D.; Heyman, M.; Marrero, D.G.; Huddleston, B.; Dachis, J. One Drop | Mobile: An Evaluation of Hemoglobin A1c Improvement Linked to App Engagement. JMIR Diabetes 2017, 2, e21. [Google Scholar] [CrossRef] [Green Version]
- Thaler, R.; Sunstein, C.R. Nudge: Improving Decisions About Health, Wealth, and Happiness; Yale University Press: New Haven, CT, USA, 2008. [Google Scholar]
- Marteau, T.M.; Ogilvie, D.; Roland, M.; Suhrcke, M.; Kelly, M. Judging Nudging: Can Nudging Improve Population Health? BMJ 2011, 342, d228. [Google Scholar] [CrossRef] [Green Version]
- Arno, A.; Thomas, S. The Efficacy of Nudge Theory Strategies in Influencing Adult Dietary Behaviour: A Systematic Review and Meta-Analysis. BMC Public Health 2016, 16, 676. [Google Scholar] [CrossRef] [Green Version]
- Li, M.; Chapman, G.B. Nudge to Health: Harnessing Decision Research to Promote Health Behavior. Soc. Pers. Psychol. Compass 2013, 7, 187–198. [Google Scholar] [CrossRef]
- Schomakers, E.; Chantal, L.; Ziefle, M. Exploring the Acceptance of Mhealth Applications—Do Acceptance Patterns Vary Depending on Context? In Advances in Human Factors in Wearable Technologies and Game Design; Springer: Amsterdam, The Netherlands, 2019; pp. 53–64. [Google Scholar]
- Kwan, Y.H.; Cheng, T.Y.; Yoon, S.; Ho, L.Y.-C.; Huang, C.; Chew, E.H.; Thumboo, J.; Ostbye, T.; Low, L.L. A systematic review of nudge theories and strategies used to influence adult health behaviour and outcome in diabetes management. Diabetes Metab. 2020, 46, 450–460. [Google Scholar] [CrossRef]
- Drechsler, A.; Hevner, A. A Four-Cycle Model of Is Design Science Research: Capturing the Dynamic Nature of Is Artifact Design. In Proceedings of the 11th International Conference on Design Science Research in Information Systems and Technology (DESRIST), St John, NL, Canada, 23–25 May 2016. [Google Scholar]
- Goodhue, D.L.; Thompson, R.L. Task-Technology Fit and Individual Performance. MIS Q. 1995, 19, 213–236. [Google Scholar] [CrossRef]
- United States Department of Agriculture. Fooddata Central. Available online: https://fdc.nal.usda.gov/ (accessed on 14 February 2022).
- Google Community. Flutter. Available online: https://flutter.dev/ (accessed on 14 February 2022).
- Google AIY, Vision. “Food_V1.” Google AIY, TenserflowHub. Available online: https://tfhub.dev/google/aiy/vision/classifier/food_V1/1 (accessed on 12 March 2022).
- Tessellate-Imaging. Monk—A Computer Vision Toolkit for Everyone. Available online: https://github.com/Tessellate-Imaging/monk_v1 (accessed on 12 March 2022).
- Nguyen, H.L. Food-Recognition (Yolov3). Available online: https://github.com/lannguyen0910/food-recognition (accessed on 12 March 2022).
- You, E. Vue.Js. Available online: https://vuejs.org/ (accessed on 17 February 2022).
- OpenJS Foundation; Dahl, R. Node.Js. Available online: https://nodejs.org/en/ (accessed on 17 February 2022).
- Auth0. Json Web Tokens (JWT). Available online: https://jwt.io/ (accessed on 17 February 2022).
- Biryukov, A.; Dinu, D.; Khovratovich, D. Argon2: New Generation of Memory-Hard Functions for Password Hashing and Other Applications. In Proceedings of the 2016 IEEE European Symposium on Security and Privacy (EuroS&P), Saarbruecken, Germany, 21–24 March 2016. [Google Scholar]
- Yin, R.K. Case Study Research and Applications: Design and Methods; Sage: Thousand Oaks, CA, USA, 2018. [Google Scholar]
- Kludacz-Alessandri, M.; Hawrysz, L.; Korneta, P.; Gierszewska, G.; Pomaranik, W.; Walczak, R. The impact of medical teleconsultations on general practitioner-patient communication during COVID-19: A case study from Poland. PLoS ONE 2021, 16, e0254960. [Google Scholar] [CrossRef]
- Sui, Z.; Raubenheimer, D.; Rangan, A. Exploratory analysis of meal composition in Australia: Meat and accompanying foods. Public Health Nutr. 2017, 20, 2157–2165. [Google Scholar] [CrossRef] [Green Version]


| Author(s), Year | Study Design | Sample Size | Duration | Intervention(s) | Outcome |
|---|---|---|---|---|---|
| Charlene et al. 2018 [33] | c-RCT | n = 213 | 2 years | Group 1: Usual care. Group 2: Coaching only. Group 3: Coaching and patient care provider portal (PCPP). Group 4: Coaching, PCPP with decision support. | Reduced HbA1c. Reduced physician visits. Unknown effect on diabetes, distress, depression, blood pressure, and lipid values. |
| Saponaro et al. 2021 [34] | Pilot study | n = 33 | 2 weeks | Just-in-time notifications and messages (smartphone + Fitbit). Fitness activity suggestion. | Participants were more active. Nudges worked better when participants were at work versus home. |
| Daitaro et al. 2020 [35] | - | - | - | Recommendation Material 1 (RM1): General advice covering easy, attractive, social, and timely (EAST) framework. Recommendation Material 2 (RM2): Personalized patients’ risk against potential risk factors. | RM 2 had higher uptake of the CRC test. |
| Elad et al. 2017 [36] | Study | n = 27 | 26 weeks | Once-a- day and once-a-week messages created by the RL algorithm and pushed to the mobile app. | Overall improved adherence to exercise in diabetic patients. Reduced HbA1c. Increased activity and pace of walking. |
| Rabbi et al. 2015 [37] | Study | n = 16 | 14 weeks | Three weeks of no nudge (baseline). Four weeks of 8 generic prescriptive suggestions from a list of 42. Seven weeks of targeted suggestions. Prioritized low-effort suggestions. | High suggestion adherence. High user satisfaction. Low-effort suggestions had higher actionability rate. |
| Name | Research | Feature Set | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Published | Theory | Medication | Blood Glucose (BG) | Fitness | Nutrition | Clinical | BI | |||||||||||||||
| Log Medication | Add medication by Search | Custom Medication | Log BG Levels | BG Visualization | Set BG Goals/THRESHOLDS | BG Statistics | Log BP Levels | BP Visualization | Calories Burned Estimator | Log nutrition Content | Search Online for Meals | Custom Meals | Nutritional Info of Meal | Nutrition Planner | Nutrition Recommender | Support Network (Coach, etc.) | Assigned Clinician Info | Remote Clinician Monitoring | Any Behavioral INTERVENTION | |||
| MySugr | ✓ [42] | ✕ | ✓ | ✕ | ✓ | ✓ | ✓ | ✓ | ✓ | ✕ | ✕ | ✕ | ✓ | ✕ | ✓ | ✕ | ✕ | ✕ | ✕ | ✕ | ✕ | ✕ |
| Blood Sugar Log | ✕ | ✕ | ✓ | ✕ | ✓ | ✓ | ✓ | ✕ | ✓ | ✕ | ✕ | ✕ | ✕ | ✕ | ✕ | ✕ | ✕ | ✕ | ✕ | ✕ | ✕ | ✕ |
| Glucose Tracker & Diabetic Diary | ✕ | ✕ | ✓ | ✕ | ✓ | ✓ | ✓ | ✓ | ✓ | – | ✕ | ✕ | – | ✕ | ✕ | ✕ | ✕ | ✕ | ✕ | ✕ | ✕ | ✕ |
| Diabetes:M | ✕ | ✕ | ✓ | – | ✓ | ✓ | ✓ | ✓ | ✓ | ✕ | ✕ | ✕ | ✓ | ✓ | ✓ | ✕ | ✕ | ✕ | ✓ | ✓ | ✓ | ✕ |
| Glucose Buddy Diabetes Tracker | ✕ | ✕ | ✓ | ✕ | ✓ | ✓ | ✓ | ✕ | ✓ | ✓ | ✓ | – | ✓ | – | ✓ | ✓ | ✕ | ✕ | ✓ | ✕ | ✕ | ✕ |
| One drop diabetes management | ✓ [43] | ✕ | ✓ | – | ✓ | ✓ | ✓ | ✓ | ✓ | – | – | – | ✓ | ✓ | ✓ | ✓ | – | ✕ | ✓ | ✕ | ✕ | ✕ |
| Blood sugar monitor by Dario | ✕ | ✕ | ✕ | ✕ | ✕ | ✓ | ✓ | ✓ | ✓ | – | ✕ | ✕ | ✓ | ✓ | ✓ | ✓ | ✕ | ✕ | ✕ | ✕ | ✕ | ✕ |
| Blood Glucose Tracker | ✕ | ✕ | ✓ | ✕ | ✓ | ✓ | ✓ | ✓ | ✓ | ✕ | ✕ | ✕ | ✓ | ✕ | ✓ | ✕ | ✕ | ✕ | ✕ | ✕ | ✕ | ✕ |
| ForDiabetes: diabetes self-management app | ✕ | ✕ | ✓ | ✕ | ✓ | ✓ | ✓ | ✓ | ✓ | – | – | – | – | ✕ | ✕ | ✕ | ✕ | ✕ | ✕ | ✕ | ✕ | ✕ |
| Glucose—blood sugar tracker (iOS only) | ✕ | ✕ | – | ✕ | – | ✓ | ✓ | ✓ | ✓ | ✕ | ✕ | ✕ | – | ✕ | ✕ | ✕ | ✕ | ✕ | ✕ | ✕ | ✕ | ✕ |
| Meals | ||
|---|---|---|
| European | Indian | Mediterranean |
| Burger | Biryani | Dolmas |
| Chicken Burger | Butter Chicken | Falafel |
| Donut | Daal | Greek Salad |
| Grilled Cheese | Dosa | Paella |
| Chicken Parmigiana | Idli | Pasta Fettuccini |
| Cheese Steak | Naan | Pasta Napoli |
| Roast Chicken | Paani Puri | Pita |
| Sandwich | Papadum | Margherita Pizza |
| Sausages | Mutton Curry | Ratatouille |
| Steak | Vada | Risotto |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Joachim, S.; Forkan, A.R.M.; Jayaraman, P.P.; Morshed, A.; Wickramasinghe, N. A Nudge-Inspired AI-Driven Health Platform for Self-Management of Diabetes. Sensors 2022, 22, 4620. https://doi.org/10.3390/s22124620
Joachim S, Forkan ARM, Jayaraman PP, Morshed A, Wickramasinghe N. A Nudge-Inspired AI-Driven Health Platform for Self-Management of Diabetes. Sensors. 2022; 22(12):4620. https://doi.org/10.3390/s22124620
Chicago/Turabian StyleJoachim, Shane, Abdur Rahim Mohammad Forkan, Prem Prakash Jayaraman, Ahsan Morshed, and Nilmini Wickramasinghe. 2022. "A Nudge-Inspired AI-Driven Health Platform for Self-Management of Diabetes" Sensors 22, no. 12: 4620. https://doi.org/10.3390/s22124620
APA StyleJoachim, S., Forkan, A. R. M., Jayaraman, P. P., Morshed, A., & Wickramasinghe, N. (2022). A Nudge-Inspired AI-Driven Health Platform for Self-Management of Diabetes. Sensors, 22(12), 4620. https://doi.org/10.3390/s22124620








