Non-Contact Hand Movement Analysis for Optimal Configuration of Smart Sensors to Capture Parkinson’s Disease Hand Tremor
Abstract
:1. Introduction
2. Methods
2.1. Inclusion Criteria
2.2. Exclusion Criteria
2.3. Data Collection and Measurement
2.4. Data Analysis
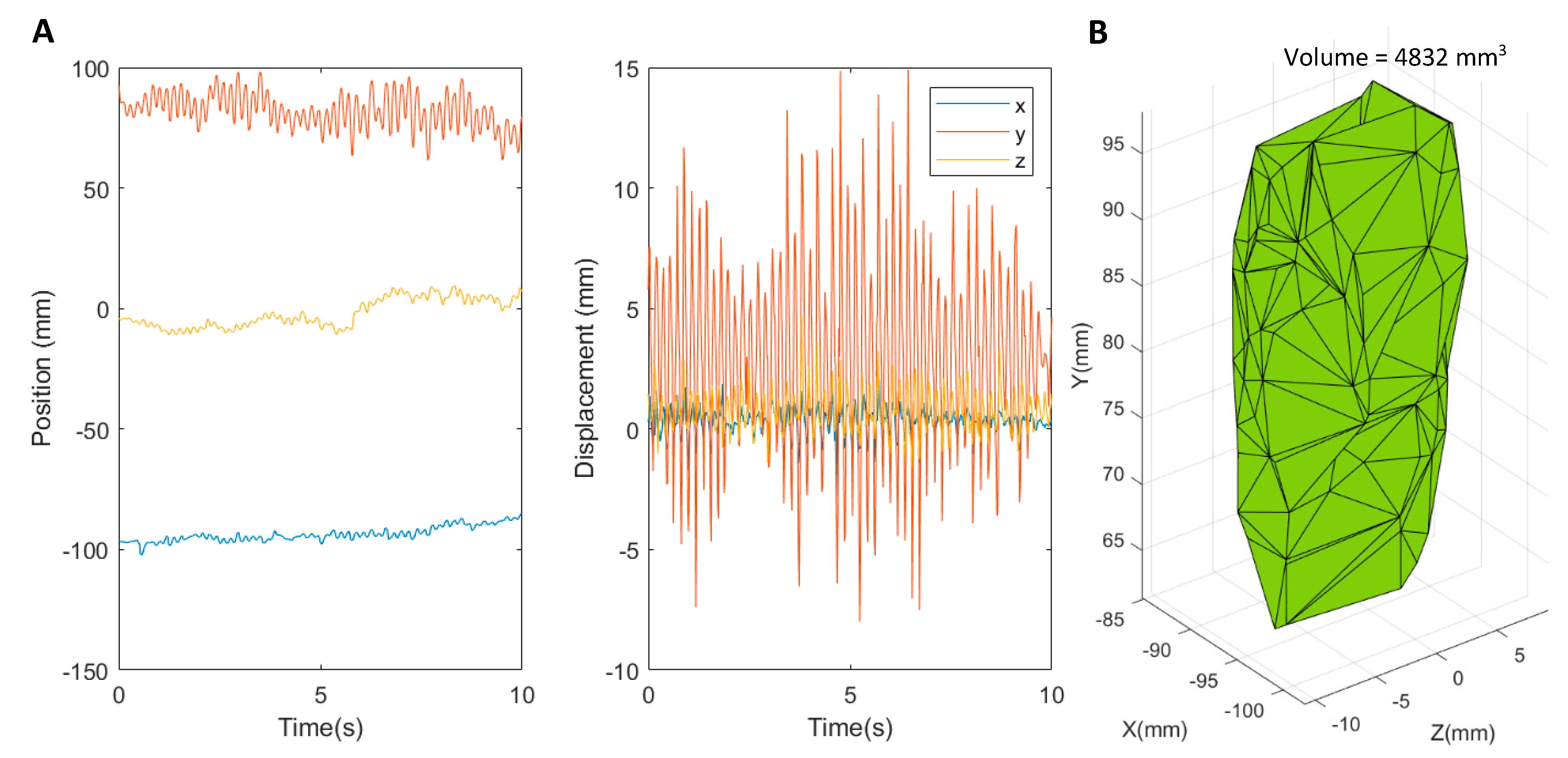
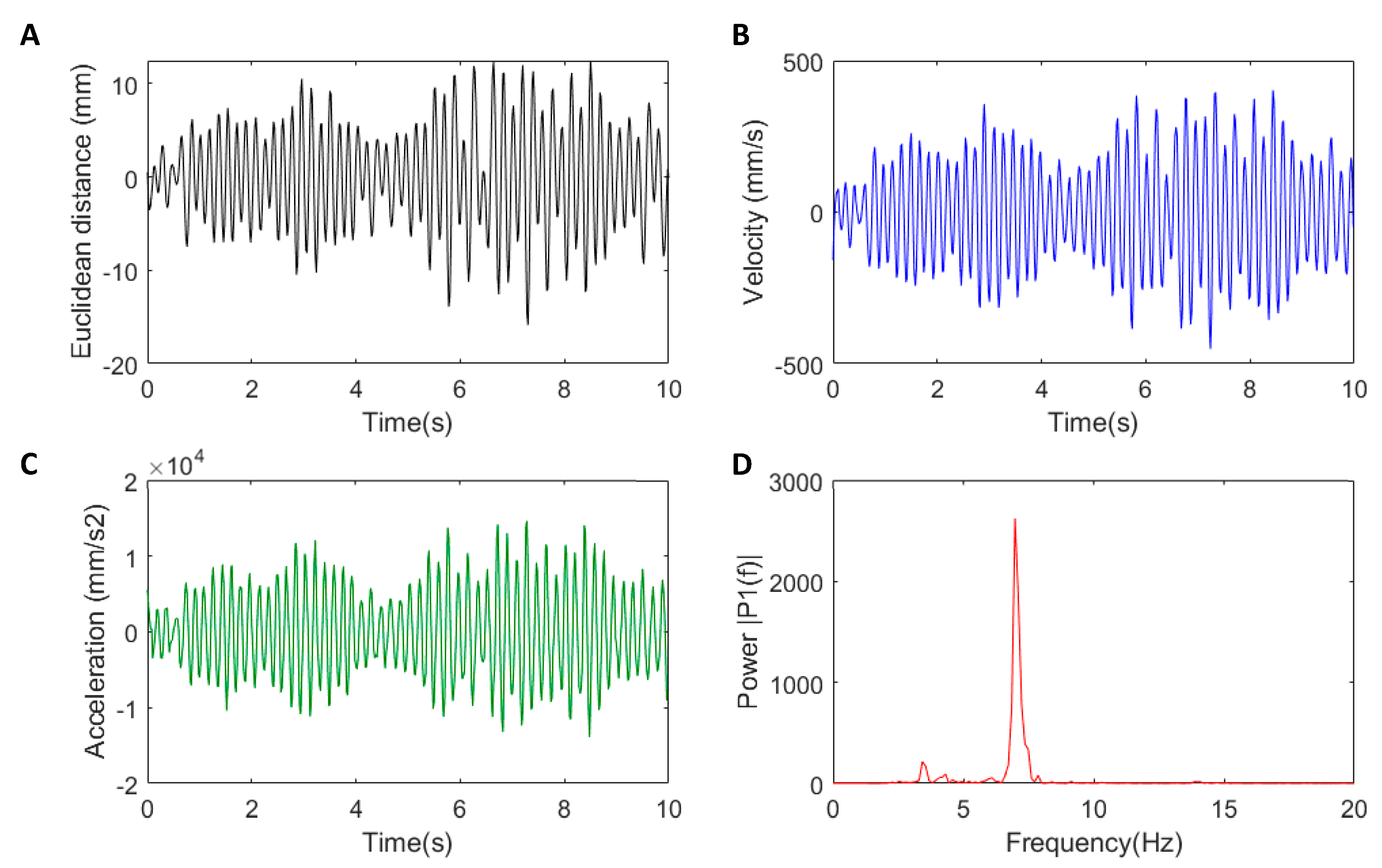
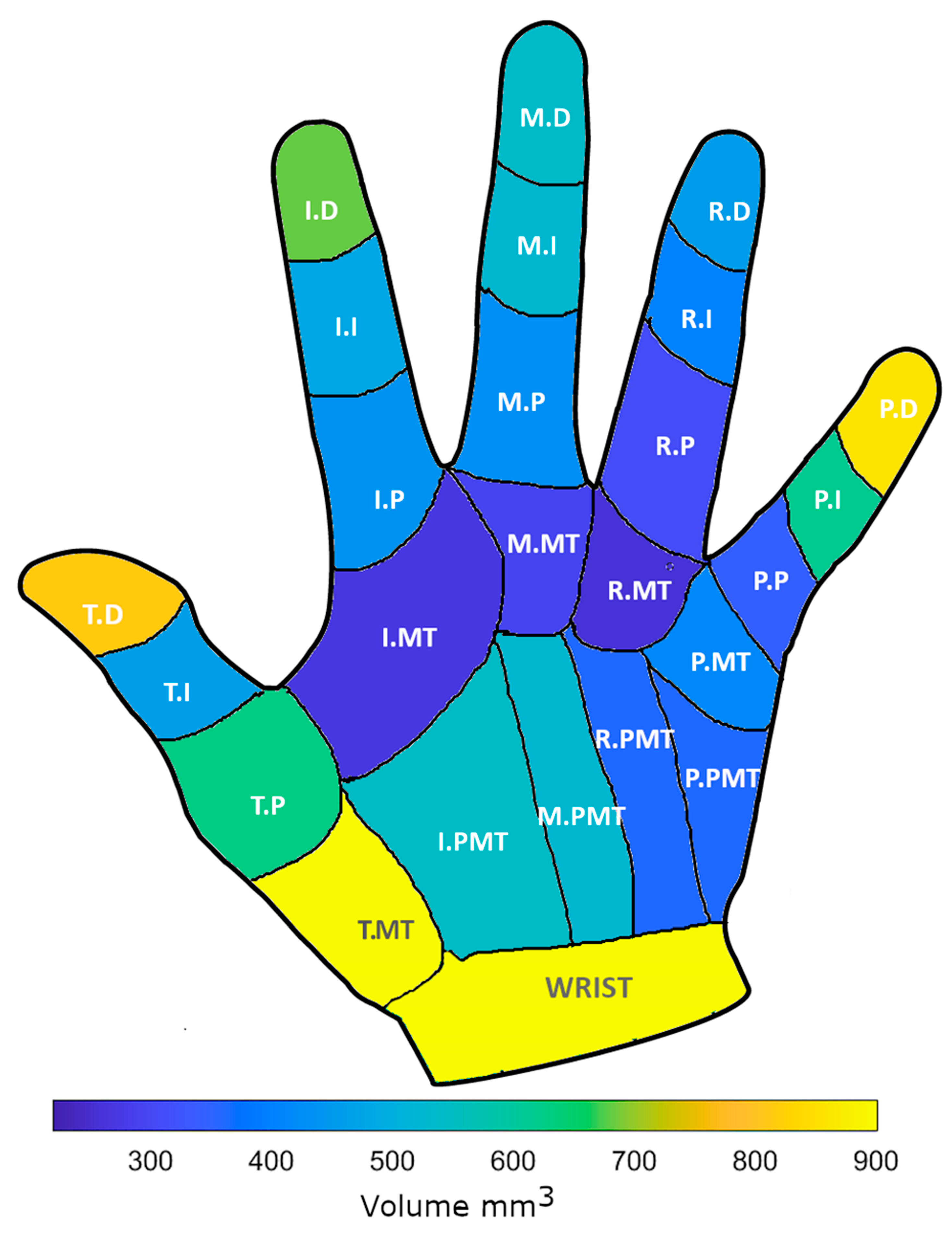
2.4.1. Volumes
2.4.2. Tremor Metrics
2.4.3. Statistical Analyses
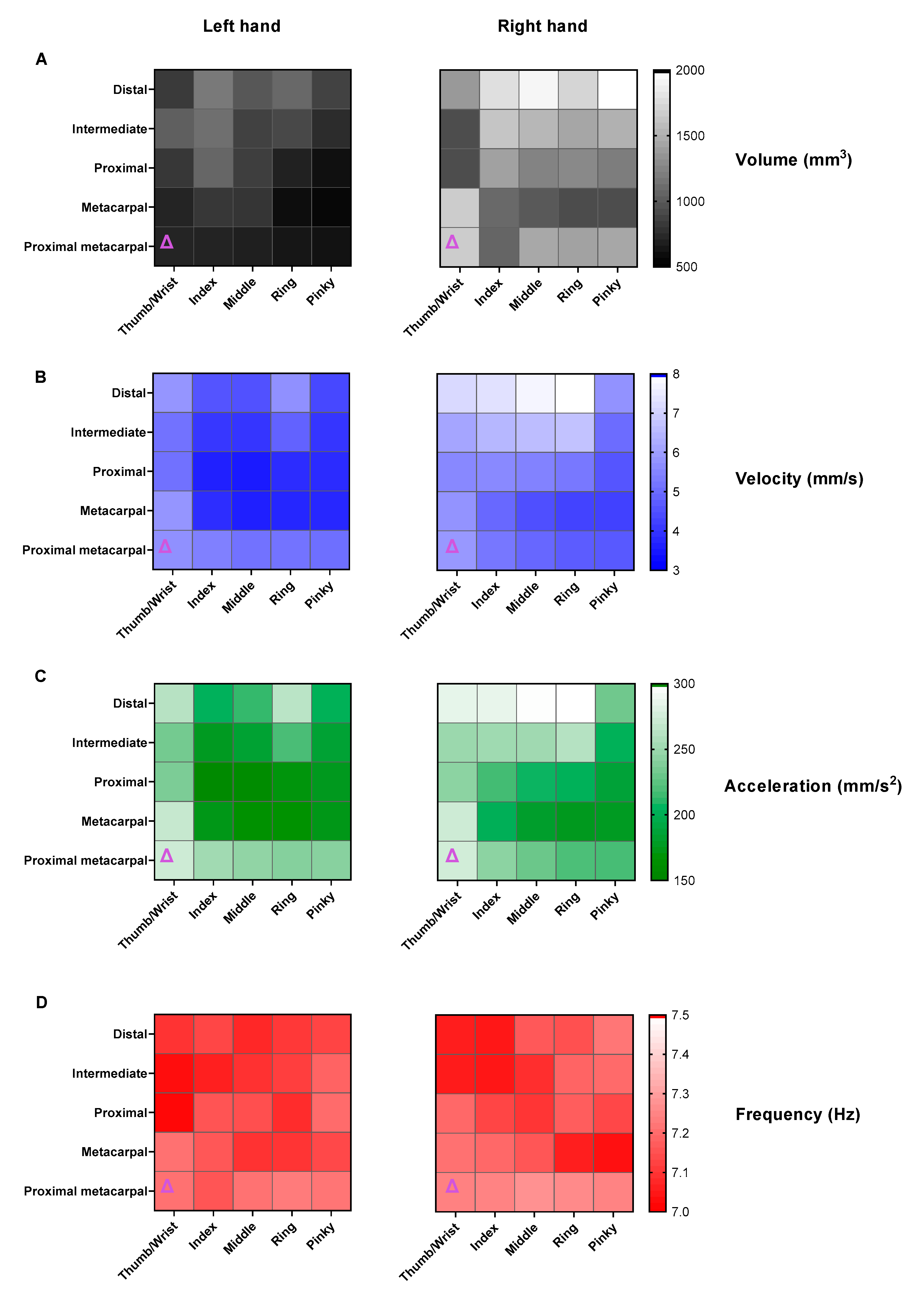
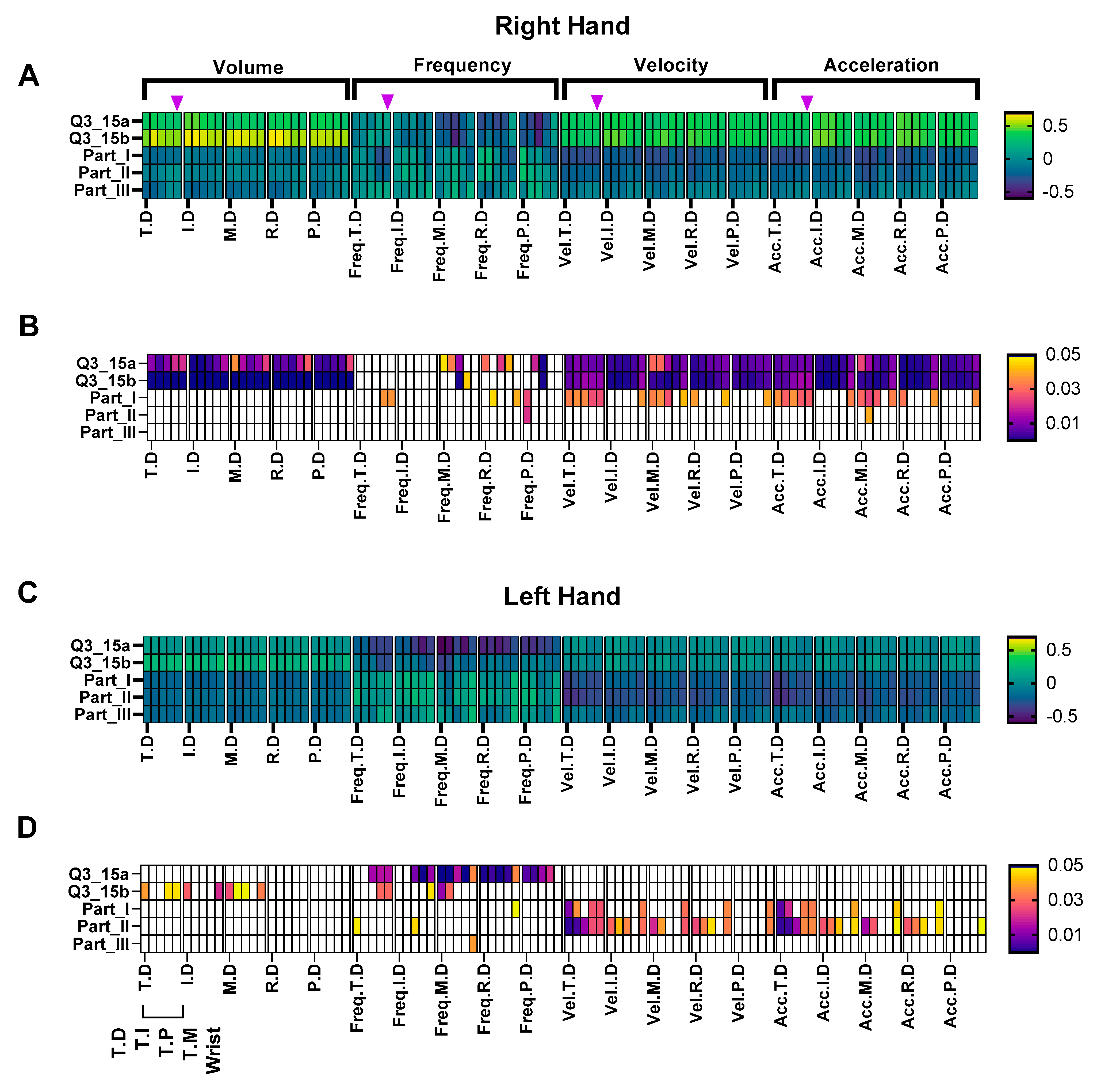
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Tysnes, O.-B.; Storstein, A. Epidemiology of Parkinson’s Disease. J. Neural Transm. 2017, 124, 901–905. [Google Scholar] [CrossRef] [PubMed]
- Bloem, B.R.; Okun, M.S.; Klein, C. Parkinson’s Disease. Lancet 2021, 397, 2284–2303. [Google Scholar] [CrossRef]
- Moustafa, A.A.; Chakravarthy, S.; Phillips, J.R.; Gupta, A.; Keri, S.; Polner, B.; Frank, M.J.; Jahanshahi, M. Motor Symptoms in Parkinson’s Disease: A Unified Framework. Neurosci. Biobehav. Rev. 2016, 68, 727–740. [Google Scholar] [CrossRef] [PubMed]
- Schapira, A.H.V.; Chaudhuri, K.R.; Jenner, P. Non-Motor Features of Parkinson Disease. Nat. Rev. Neurosci. 2017, 18, 435–450. [Google Scholar] [CrossRef] [PubMed]
- Alamri, Y.; Pitcher, T.; Anderson, T.J. Variations in the Patterns of Prevalence and Therapy in Australasian Parkinson’s Disease Patients of Different Ethnicities. BMJ Neurol. Open 2020, 2, e000033. [Google Scholar] [CrossRef] [PubMed]
- Myall, D.J.; Pitcher, T.L.; Pearson, J.F.; Dalrymple-Alford, J.C.; Anderson, T.J.; MacAskill, M.R. Parkinson’s in the Oldest Old: Impact on Estimates of Future Disease Burden. Parkinsonism Relat. Disord. 2017, 42, 78–84. [Google Scholar] [CrossRef]
- Solla, P.; Masala, C.; Pinna, I.; Ercoli, T.; Loy, F.; Orofino, G.; Fadda, L.; Defazio, G. Frequency and Determinants of Olfactory Hallucinations in Parkinson’s Disease Patients. Brain Sci. 2021, 11, 841. [Google Scholar] [CrossRef]
- Rizek, P.; Kumar, N.; Jog, M.S. An Update on the Diagnosis and Treatment of Parkinson Disease. CMAJ 2016, 188, 1157–1165. [Google Scholar] [CrossRef] [Green Version]
- Brooks, D.J. Optimizing Levodopa Therapy for Parkinson’s Disease with Levodopa/Carbidopa/Entacapone: Implications from a Clinical and Patient Perspective. Neuropsychiatr. Dis. Treat. 2008, 4, 39. [Google Scholar] [CrossRef] [Green Version]
- Pieterman, M.; Adams, S.; Jog, M. Method of Levodopa Response Calculation Determines Strength of Association with Clinical Factors in Parkinson Disease. Front. Neurol. 2018, 9, 260. [Google Scholar] [CrossRef] [Green Version]
- Heijmans, M.; Habets, J.G.V.; Herff, C.; Aarts, J.; Stevens, A.; Kuijf, M.L.; Kubben, P.L. Monitoring Parkinson’s Disease Symptoms during Daily Life: A Feasibility Study. NPJ Park. Dis. 2019, 5, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Lu, R.; Xu, Y.; Li, X.; Fan, Y.; Zeng, W.; Tan, Y.; Ren, K.; Chen, W.; Cao, X. Evaluation of Wearable Sensor Devices in Parkinson’s Disease: A Review of Current Status and Future Prospects. Park. Dis. 2020, 2020, 4693019. [Google Scholar] [CrossRef] [PubMed]
- Thorp, J.E.; Adamczyk, P.G.; Ploeg, H.-L.; Pickett, K.A. Monitoring Motor Symptoms During Activities of Daily Living in Individuals With Parkinson’s Disease. Front. Neurol. 2018, 9, 1036. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rovini, E.; Maremmani, C.; Cavallo, F. How Wearable Sensors Can Support Parkinson’s Disease Diagnosis and Treatment: A Systematic Review. Front. Neurosci. 2017, 11, 555. [Google Scholar] [CrossRef] [PubMed]
- Channa, A.; Popescu, N.; Ciobanu, V. Wearable Solutions for Patients with Parkinson’s Disease and Neurocognitive Disorder: A Systematic Review. Sensors 2020, 20, 2713. [Google Scholar] [CrossRef] [PubMed]
- Hssayeni, M.D.; Jimenez-Shahed, J.; Burack, M.A.; Ghoraani, B. Wearable Sensors for Estimation of Parkinsonian Tremor Severity during Free Body Movements. Sensors 2019, 19, 4215. [Google Scholar] [CrossRef] [Green Version]
- Morris, T.R.; Cho, C.; Dilda, V.; Shine, J.M.; Naismith, S.L.; Lewis, S.J.G.; Moore, S.T. A Comparison of Clinical and Objective Measures of Freezing of Gait in Parkinson’s Disease. Parkinsonism Relat. Disord. 2012, 18, 572–577. [Google Scholar] [CrossRef]
- Mancini, M.; Shah, V.V.; Stuart, S.; Curtze, C.; Horak, F.B.; Safarpour, D.; Nutt, J.G. Measuring Freezing of Gait during Daily-Life: An Open-Source, Wearable Sensors Approach. J. Neuroeng. Rehabilitation 2021, 18, 1. [Google Scholar] [CrossRef]
- Çakmak, Y.Ö.; Ölçek, S.C.; Özsoy, B.; Gökçay, D. Quantitative Measurement of Bradykinesia in Parkinson’s Disease Using Commercially Available Leap Motion. In Proceedings of the 11th International Joint Conference on Biomedical Engineering Systems and Technologies, Madeira, Portuga, 1 January 2018; SCITEPRESS—Science and Technology Publications: Setúbal, Portugal, 2018; pp. 227–232. [Google Scholar]
- Teshuva, I.; Hillel, I.; Gazit, E.; Giladi, N.; Mirelman, A.; Hausdorff, J.M. Using Wearables to Assess Bradykinesia and Rigidity in Patients with Parkinson’s Disease: A Focused, Narrative Review of the Literature. J. Neural Transm. 2019, 126, 699–710. [Google Scholar] [CrossRef]
- Hssayeni, M.D.; Jimenez-Shahed, J.; Burack, M.A.; Ghoraani, B. Dyskinesia Estimation during Activities of Daily Living Using Wearable Motion Sensors and Deep Recurrent Networks. Sci. Rep. 2021, 11, 7865. [Google Scholar] [CrossRef]
- Giuffrida, J.P.; Riley, D.E.; Maddux, B.N.; Heldman, D.A. Clinically Deployable KinesiaTM Technology for Automated Tremor Assessment. Mov. Disord. 2009, 24, 723–730. [Google Scholar] [CrossRef] [PubMed]
- van Brummelen, E.M.J.; Ziagkos, D.; de Boon, W.M.I.; Hart, E.P.; Doll, R.J.; Huttunen, T.; Kolehmainen, P.; Groeneveld, G.J. Quantification of Tremor Using Consumer Product Accelerometry Is Feasible in Patients with Essential Tremor and Parkinson’s Disease: A Comparative Study. J. Clin. Mov. Disord. 2020, 7, 4–11. [Google Scholar] [CrossRef]
- Sica, M.; Tedesco, S.; Crowe, C.; Kenny, L.; Moore, K.; Timmons, S.; Barton, J.; O’Flynn, B.; Komaris, D.-S. Continuous Home Monitoring of Parkinson’s Disease Using Inertial Sensors: A Systematic Review. PLoS ONE 2021, 16, e0246528. [Google Scholar] [CrossRef] [PubMed]
- Yang, H.; Shen, Y.; Zhuang, W.; Gao, C.; Dai, D.; Zhang, W. A Smart Wearable Ring Device for Sensing Hand Tremor of Parkinson’s Patients. CMES Comput. Modeling Eng. Sci. 2021, 126, 1217–1238. [Google Scholar] [CrossRef]
- Hoehn, M.M.; Yahr, M.D. Parkinsonism: Onset, Progression and Mortality. Neurology 1967, 17, 427–442. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shetty, A.S.; Bhatia, K.P.; Lang, A.E. Dystonia and Parkinson’s Disease: What Is the Relationship? Neurobiol. Dis. 2019, 132, 104462. [Google Scholar] [CrossRef]
- Butt, A.H.; Rovini, E.; Dolciotti, C.; Bongioanni, P.; de Petris, G.; Cavallo, F. Leap Motion Evaluation for Assessment of Upper Limb Motor Skills in Parkinson’s Disease. In Proceedings of the 2017 International Conference on Rehabilitation Robotics (ICORR), London, UK, 17–20 July 2017; IEEE: Piscataway, NJ, USA, 2017; pp. 116–121. [Google Scholar]
- Butt, A.H.; Rovini, E.; Dolciotti, C.; de Petris, G.; Bongioanni, P.; Carboncini, M.C.; Cavallo, F. Objective and Automatic Classification of Parkinson Disease with Leap Motion Controller. BioMedical Eng. OnLine 2018, 17, 168. [Google Scholar] [CrossRef] [Green Version]
- Vivar, G.; Almanza-Ojeda, D.-L.; Cheng, I.; Gomez, J.C.; Andrade-Lucio, J.A.; Ibarra-Manzano, M.-A. Contrast and Homogeneity Feature Analysis for Classifying Tremor Levels in Parkinson’s Disease Patients. Sensors 2019, 19, 2072. [Google Scholar] [CrossRef] [Green Version]
- Kaji, H.; Sugano, M. A Noncontact Tremor Measurement System Using Leap Motion. In Proceedings of the ACM International Conference Proceeding Series, Leipzig, Germany, 23–27 August 2017. [Google Scholar]
- Garcia-Agundez, A.; Eickhoff, C. Towards Objective Quantification of Hand Tremors and Bradykinesia Using Contactless Sensors: A Systematic Review. Front. Aging Neurosci. 2021, 13, 694. [Google Scholar] [CrossRef]
- Weichert, F.; Bachmann, D.; Rudak, B.; Fisseler, D. Analysis of the Accuracy and Robustness of the Leap Motion Controller. Sensors 2013, 13, 6380–6393. [Google Scholar] [CrossRef] [Green Version]
- Beuter, A.; Edwards, R. Using Frequency Domain Characteristics to Discriminate Physiologic and Parkinsonian Tremors. J. Clin. Neurophysiol. 1999, 16, 484. [Google Scholar] [CrossRef] [PubMed]
- Atas, M. Hand Tremor Based Biometric Recognition Using Leap Motion Device. IEEE Access 2017, 5, 23320–23326. [Google Scholar] [CrossRef]
- de Oliveira Andrade, A.; Paixão, A.P.S.; Cabral, A.M.; Rabelo, A.G.; Luiz, L.M.D.; Dionísio, V.C.; Vieira, M.F.; Pereira, J.M.; Rueda, A.; Krishnan, S.; et al. Task-Specific Tremor Quantification in a Clinical Setting for Parkinson’s Disease. J. Med. Biol. Eng. 2020, 40, 821–850. [Google Scholar] [CrossRef]
- Zhang, H.; Deng, K.; Li, H.; Albin, R.L.; Guan, Y. Deep Learning Identifies Digital Biomarkers for Self-Reported Parkinson’s Disease. Patterns 2020, 1, 100042. [Google Scholar] [CrossRef] [PubMed]
- Powers, R.; Etezadi-Amoli, M.; Arnold, E.M.; Kianian, S.; Mance, I.; Gibiansky, M.; Trietsch, D.; Alvarado, A.S.; Kretlow, J.D.; Herrington, T.M.; et al. Smartwatch Inertial Sensors Continuously Monitor Real-World Motor Fluctuations in Parkinson’s Disease. Sci. Transl. Med. 2021, 13, eabd7865. [Google Scholar] [CrossRef] [PubMed]
- Edwards, R.; Beuter, A. Using Time Domain Characteristics to Discriminate Physiologic and Parkinsonian Tremors. J. Clin. Neurophysiol. 2000, 17, 87–100. [Google Scholar] [CrossRef]
- Chen, L.; Cai, G.; Weng, H.; Yu, J.; Yang, Y.; Huang, X.; Chen, X.; Ye, Q. More Sensitive Identification for Bradykinesia Compared to Tremors in Parkinson’s Disease Based on Parkinson’s KinetiGraph (PKG). Front. Aging Neurosci. 2020, 12, 356. [Google Scholar] [CrossRef] [Green Version]
- Goetz, C.G.; Tilley, B.C.; Shaftman, S.R.; Stebbins, G.T.; Fahn, S.; Martinez-Martin, P.; Poewe, W.; Sampaio, C.; Stern, M.B.; Dodel, R.; et al. Movement Disorder Society-Sponsored Revision of the Unified Parkinson’s Disease Rating Scale (MDS-UPDRS): Scale Presentation and Clinimetric Testing Results. Mov. Disord. 2008, 23, 2129–2170. [Google Scholar] [CrossRef]
- Lee, H.J.; Lee, W.W.; Kim, S.K.; Park, H.; Jeon, H.S.; Kim, H.B.; Jeon, B.S.; Park, K.S. Tremor Frequency Characteristics in Parkinson’s Disease under Resting-State and Stress-State Conditions. J. Neurol. Sci. 2016, 362, 272–277. [Google Scholar] [CrossRef]
- Jitkritsadakul, O.; Jagota, P.; Bhidayasiri, R. Pathophysiology of Parkinsonian Tremor: A Focused Narrative Review. Asian Biomed. 2016, 10, S15–S22. [Google Scholar] [CrossRef]
- Bain, P.G. The Management of Tremor. J. Neurol. Neurosurg. Psychiatry 2002, 72 (Suppl. S1), I3–I9. [Google Scholar] [CrossRef] [PubMed]
- Vaillancourt, D.E.; Newell, K.M. The Dynamics of Resting and Postural Tremor in Parkinson’s Disease. Clin. Neurophysiol. 2000, 111, 2046–2056. [Google Scholar] [CrossRef]
- Heinrichs-Graham, E.; Santamaria, P.M.; Gendelman, H.E.; Wilson, T.W. The Cortical Signature of Symptom Laterality in Parkinson’s Disease. Neuroimage Clin. 2017, 14, 433–440. [Google Scholar] [CrossRef] [PubMed]

| Characteristics | Participants with Parkinson’s Disease |
|---|---|
| n (male) | 55 (38) |
| side of onset (left, right, bilateral) | 20, 34, 1 |
| age (years) | 72 ± 7 (53–87) |
| Hoehn and Yahr (1–5) | 2.0 ± 0.5 (2–3) |
| Levodopa equivalent dose (mg) | 1050 ± 586 (155–2900) |
| Disease duration (years) | 11 ± 5 (3–27) |
| MDS-UPDRS I | 10 ± 5 (2–24) |
| MDS-UPDRS II | 11 ± 6 (1–29) |
| MDS-UPDRS III | 34 ± 12 (14–61) |
| Q3_15a (Postural Tremor Right hand) | 1 ± 0.5 (0–3) |
| Q3_15b (Postural Tremor Left hand) | 1 ± 0.5 (0–3) |
| Wrist Compared to | Velocities | Acceleration | ||||||
|---|---|---|---|---|---|---|---|---|
| LH | RH | LH | RH | |||||
| T.D | ns | >0.999 | ns | >0.999 | ns | >0.999 | ns | >0.999 |
| T.I | ns | >0.999 | ns | >0.999 | ns | >0.999 | ns | >0.999 |
| T.P | ns | >0.999 | ns | >0.999 | ns | >0.999 | ns | >0.999 |
| T.MT | ns | >0.999 | ns | >0.999 | ns | >0.999 | ns | >0.999 |
| I.D | *** | <0.001 | ns | 0.147 | *** | <0.001 | ns | 0.106 |
| I.I | *** | <0.001 | *** | <0.001 | *** | <0.001 | *** | <0.001 |
| I.P | *** | <0.001 | *** | <0.001 | *** | <0.001 | *** | <0.001 |
| I.MT | *** | <0.001 | *** | <0.001 | *** | <0.001 | *** | <0.001 |
| I.PMT | ns | 0.999 | ns | 0.969 | *** | <0.001 | *** | <0.001 |
| M.D | *** | <0.001 | ns | 0.723 | *** | <0.001 | ns | 0.963 |
| M.I | *** | <0.001 | *** | <0.001 | *** | <0.001 | * | 0.014 |
| M.P | *** | <0.001 | *** | <0.001 | *** | <0.001 | *** | <0.001 |
| M.MT | *** | <0.001 | *** | <0.001 | *** | <0.001 | *** | <0.001 |
| M.PMT | ns | 0.937 | ns | 0.380 | *** | <0.001 | *** | <0.001 |
| R.D | * | 0.026 | ns | >0.999 | ns | 0.238 | ns | >0.999 |
| R.I | *** | <0.001 | ** | 0.005 | *** | <0.001 | ns | 0.117 |
| R.P | *** | <0.001 | *** | <0.001 | *** | <0.001 | *** | <0.001 |
| R.MT | *** | <0.001 | *** | <0.001 | *** | <0.001 | *** | <0.001 |
| R.PMT | ns | 0.782 | ns | 0.067 | *** | <0.001 | *** | <0.001 |
| P.D | *** | <0.001 | * | 0.010 | *** | <0.001 | ns | 0.201 |
| P.I | *** | <0.001 | *** | <0.001 | *** | <0.001 | ** | 0.002 |
| P.P | *** | <0.001 | *** | <0.001 | *** | <0.001 | *** | <0.001 |
| P.MT | *** | <0.001 | *** | <0.001 | *** | <0.001 | *** | <0.001 |
| P.PMT | ns | 0.894 | * | 0.041 | *** | <0.001 | *** | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Khwaounjoo, P.; Singh, G.; Grenfell, S.; Özsoy, B.; MacAskill, M.R.; Anderson, T.J.; Çakmak, Y.O. Non-Contact Hand Movement Analysis for Optimal Configuration of Smart Sensors to Capture Parkinson’s Disease Hand Tremor. Sensors 2022, 22, 4613. https://doi.org/10.3390/s22124613
Khwaounjoo P, Singh G, Grenfell S, Özsoy B, MacAskill MR, Anderson TJ, Çakmak YO. Non-Contact Hand Movement Analysis for Optimal Configuration of Smart Sensors to Capture Parkinson’s Disease Hand Tremor. Sensors. 2022; 22(12):4613. https://doi.org/10.3390/s22124613
Chicago/Turabian StyleKhwaounjoo, Prashanna, Gurleen Singh, Sophie Grenfell, Burak Özsoy, Michael R. MacAskill, Tim J. Anderson, and Yusuf O. Çakmak. 2022. "Non-Contact Hand Movement Analysis for Optimal Configuration of Smart Sensors to Capture Parkinson’s Disease Hand Tremor" Sensors 22, no. 12: 4613. https://doi.org/10.3390/s22124613
APA StyleKhwaounjoo, P., Singh, G., Grenfell, S., Özsoy, B., MacAskill, M. R., Anderson, T. J., & Çakmak, Y. O. (2022). Non-Contact Hand Movement Analysis for Optimal Configuration of Smart Sensors to Capture Parkinson’s Disease Hand Tremor. Sensors, 22(12), 4613. https://doi.org/10.3390/s22124613






