A Vision-Based System for Stage Classification of Parkinsonian Gait Using Machine Learning and Synthetic Data
Abstract
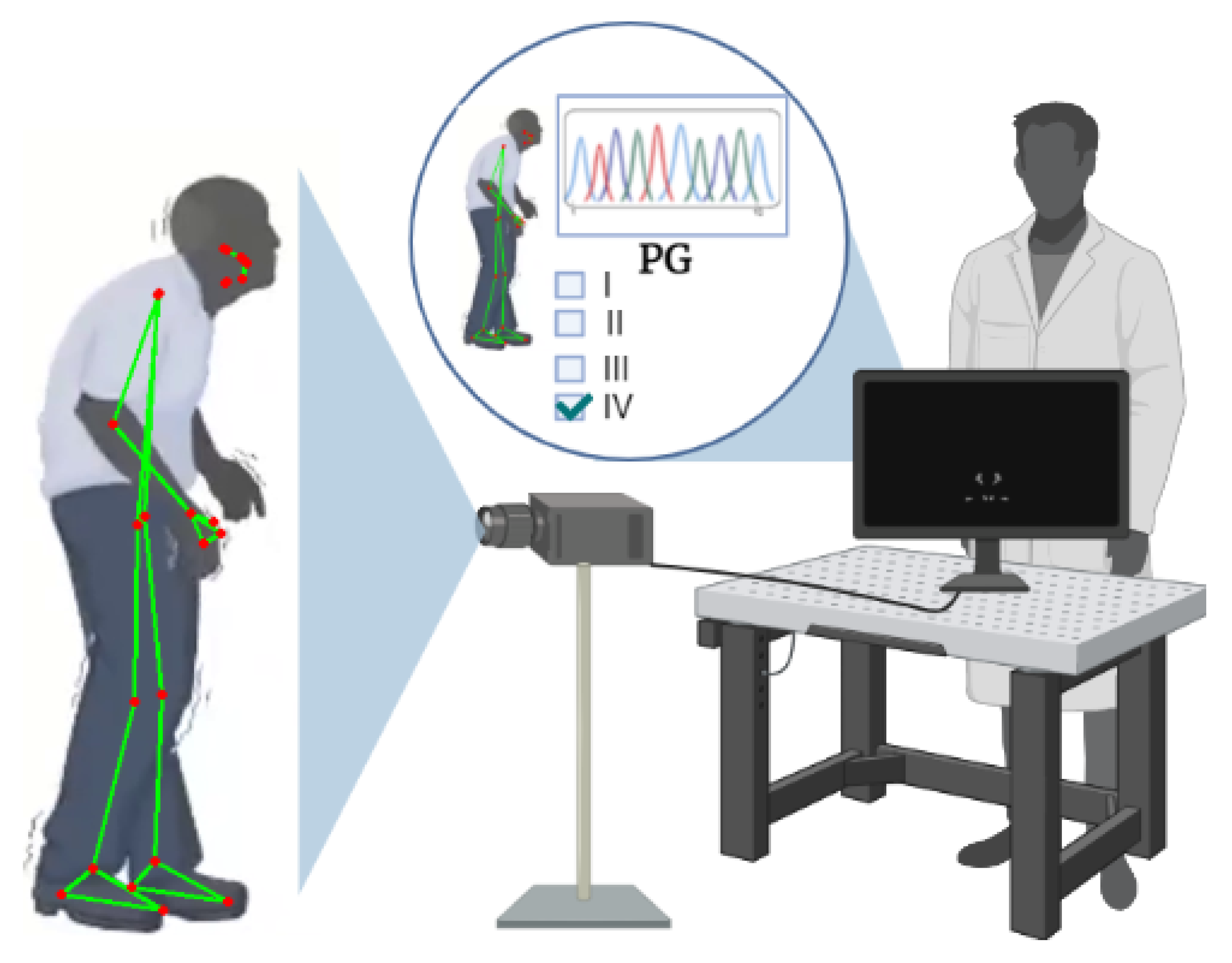
:1. Introduction
2. Materials and Methods
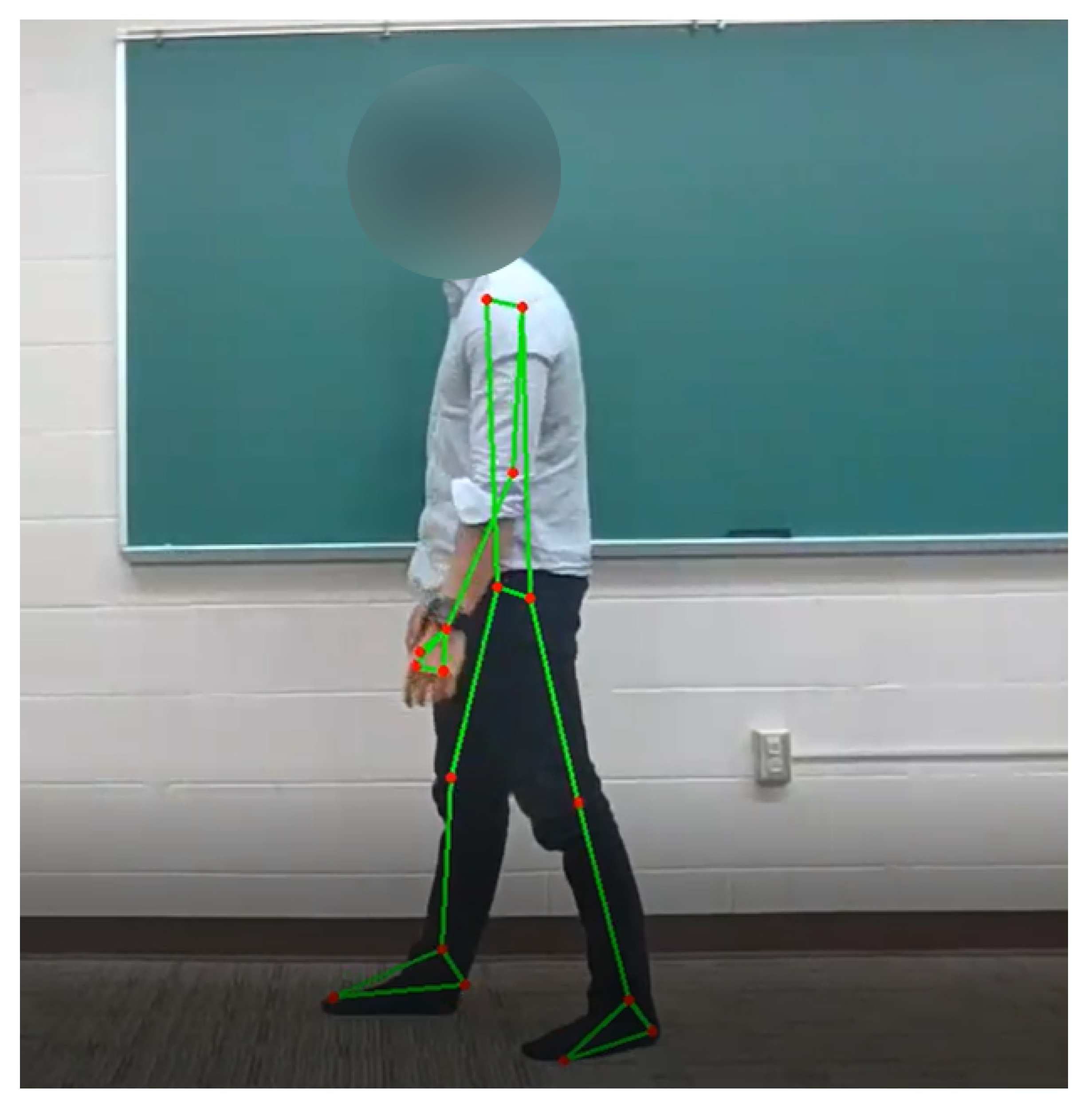
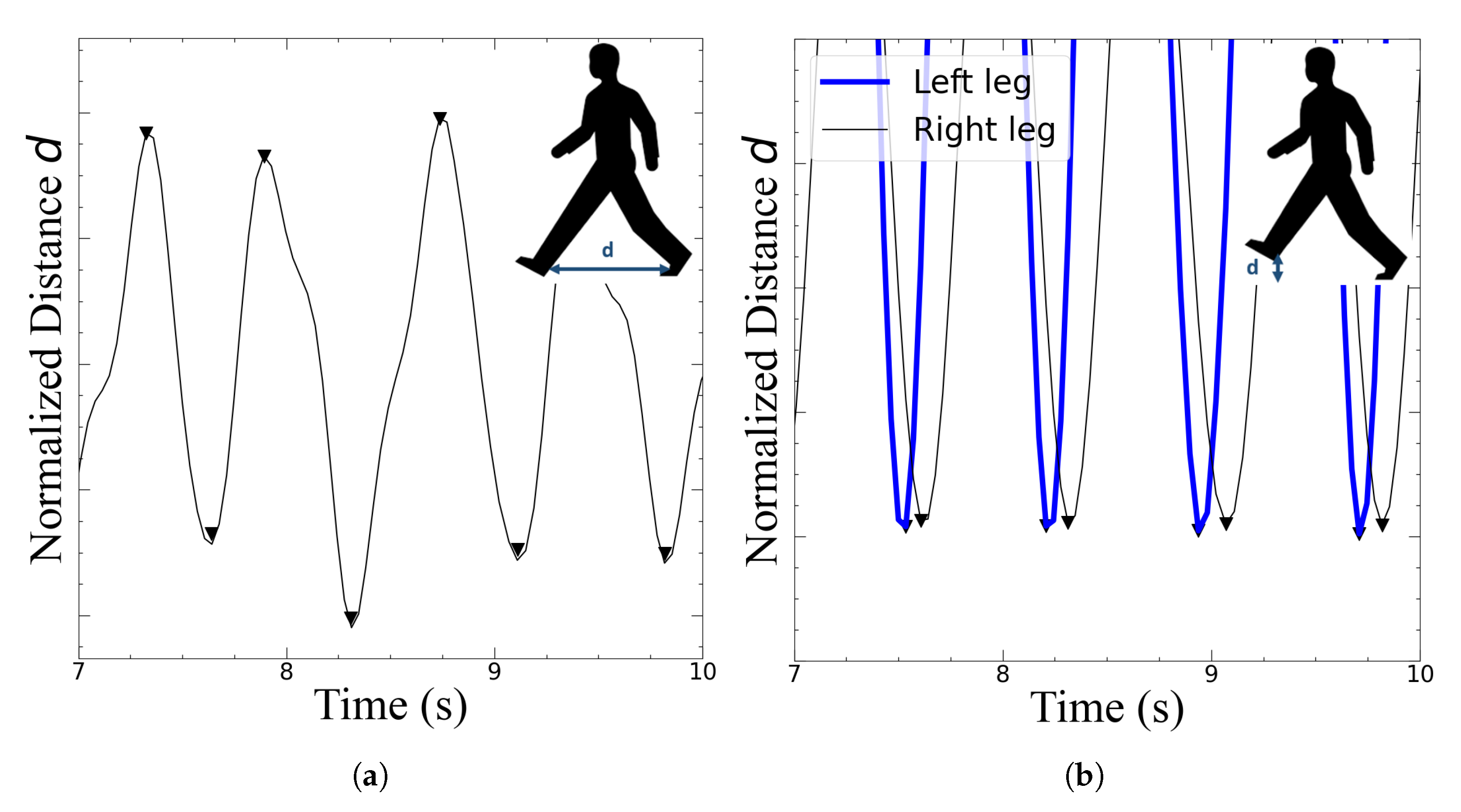
2.1. Skeleton Extraction and Feature Analysis
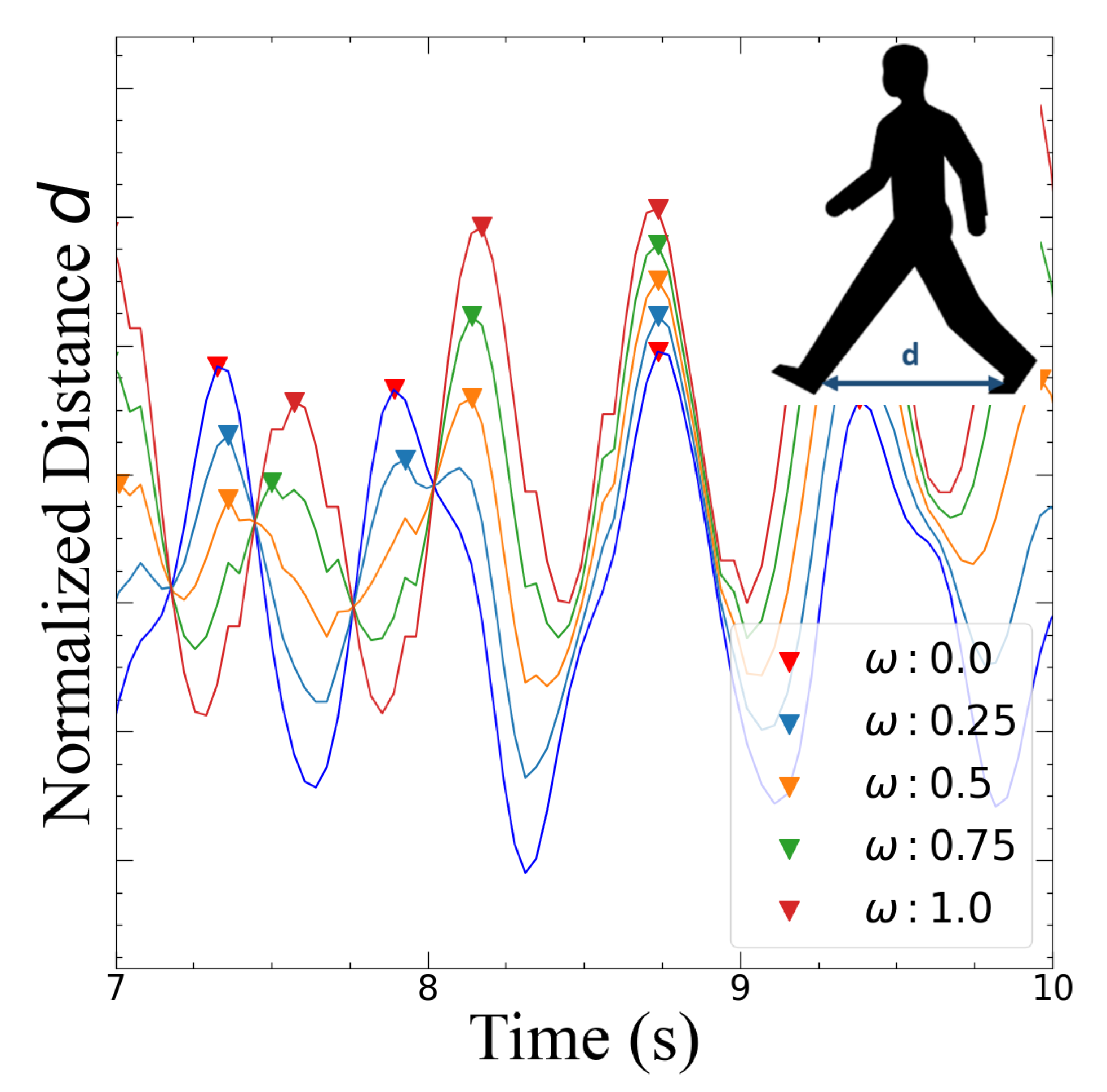
2.2. Selecting Synthetic Dataset and Hyper-Parameters
2.2.1. Data Generation
2.2.2. Classification Models
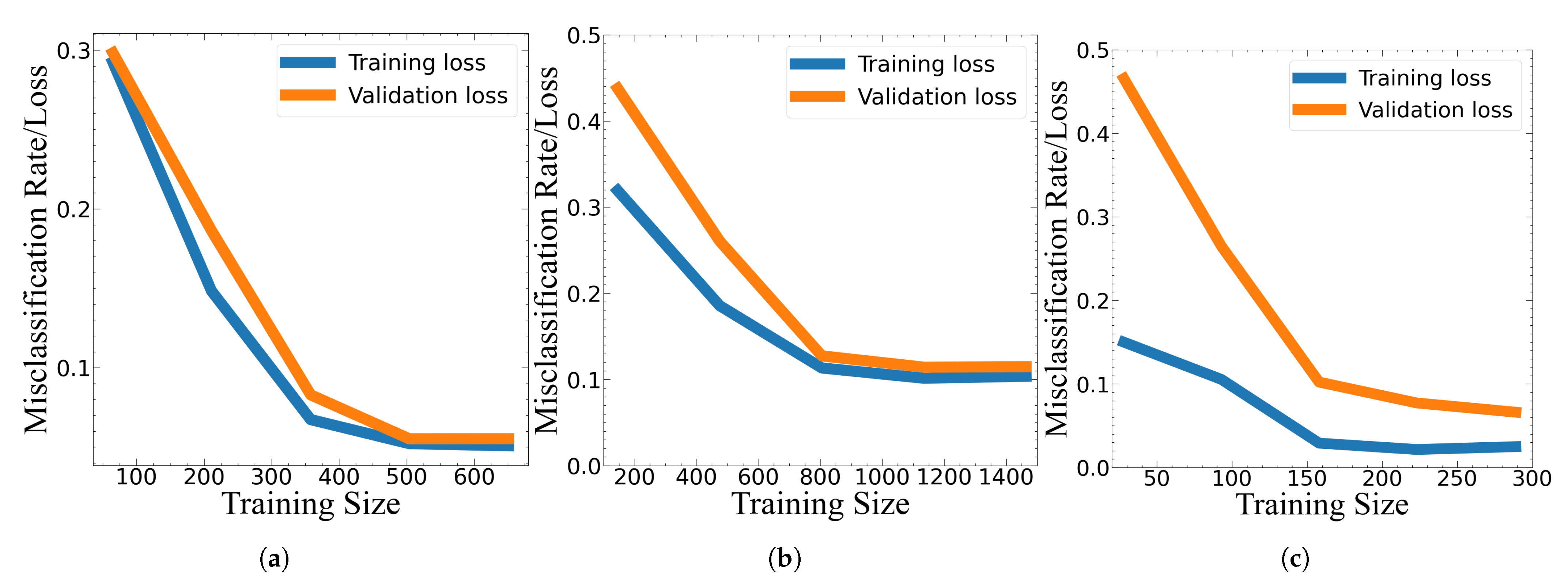
2.2.3. Learning Curves to Test Quality of Fit
2.3. Performance Evaluation
2.4. Test Data on Trained Models
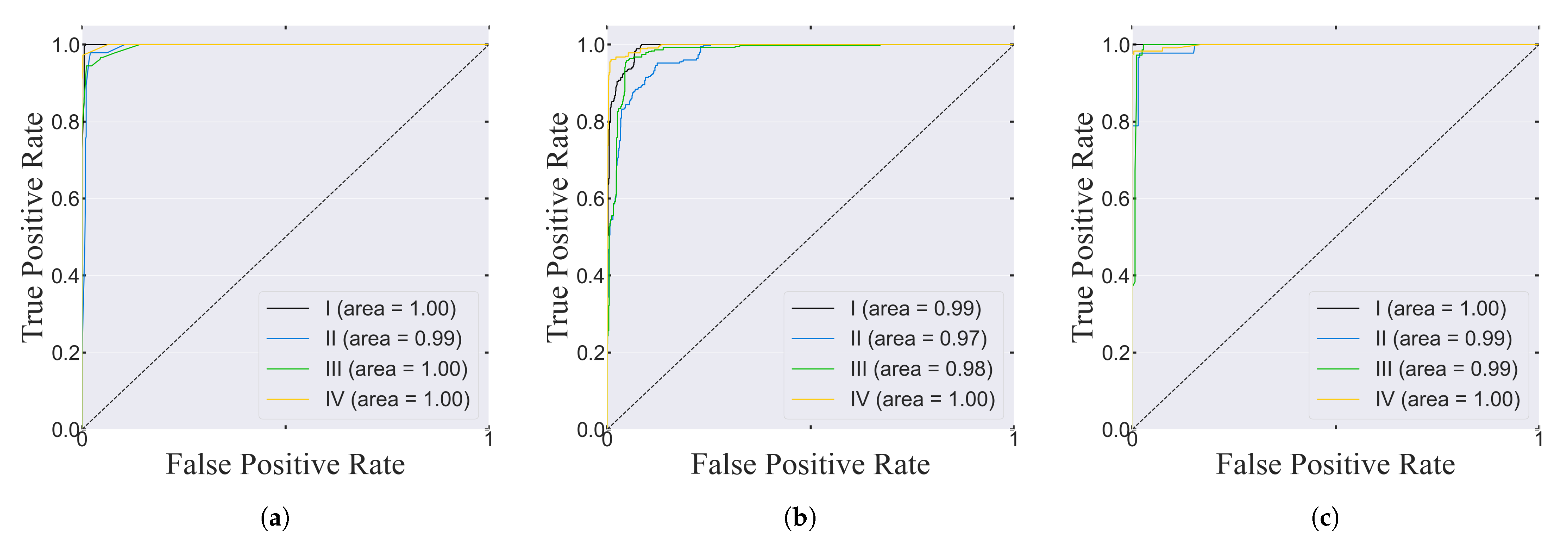
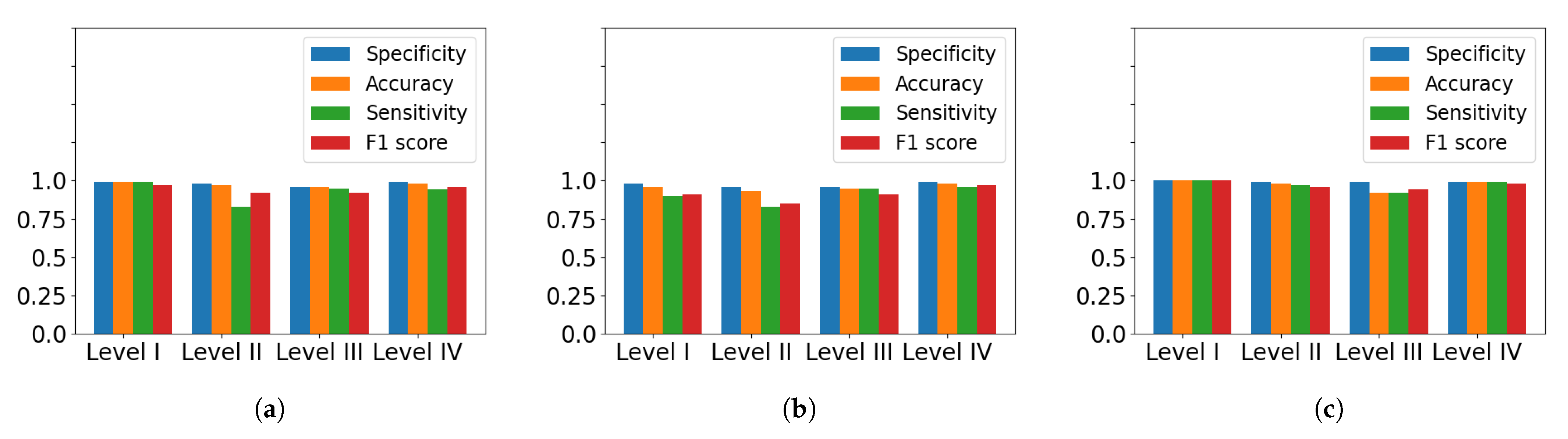
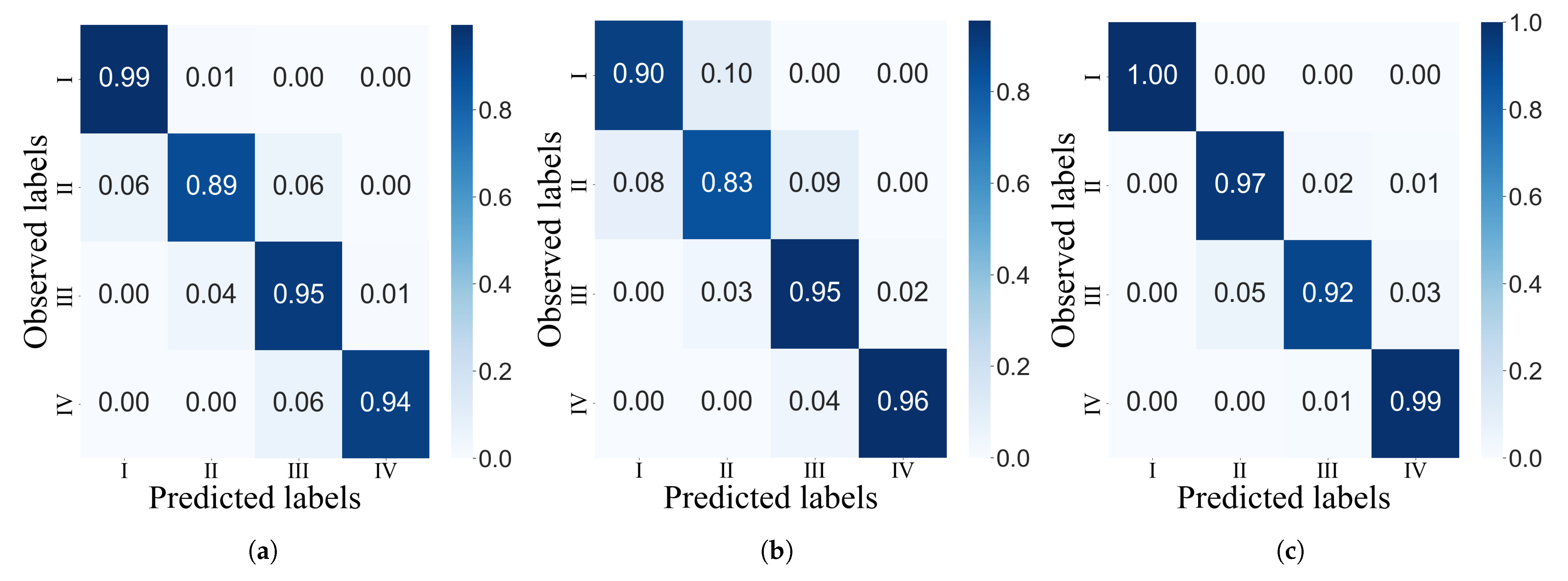
3. Results
4. Discussion
4.1. Generation of Synthetic Data
4.2. Result Interpretation
4.3. Practical Applications
4.4. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Jankovic, J. Parkinson’s disease: Clinical features and diagnosis. J. Neurol. Neurosurg. Psychiatry 2008, 79, 368–376. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Serrao, M.; Chini, G.; Bergantino, M.; Sarnari, D.; Casali, C.; Conte, C.; Ranavolo, A.; Marcotulli, C.; Rinaldi, M.; Coppola, G.; et al. Identification of specific gait patterns in patients with cerebellar ataxia, spastic paraplegia, and Parkinson’s disease: A non-hierarchical cluster analysis. Hum. Mov. Sci. 2018, 57, 267–279. [Google Scholar] [CrossRef] [PubMed]
- Zhao, A.; Qi, L.; Li, J.; Dong, J.; Yu, H. A hybrid spatio-temporal model for detection and severity rating of Parkinson’s disease from gait data. Neurocomputing 2018, 315, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Hu, Q.; Tang, X.; Tang, W. A Smart Chair Sitting Posture Recognition System Using Flex Sensors and FPGA Implemented Artificial Neural Network. IEEE Sens. J. 2020, 20, 8007–8016. [Google Scholar] [CrossRef]
- Hu, Q.; Tang, X.; Tang, W. A Real-Time Patient-Specific Sleeping Posture Recognition System Using Pressure Sensitive Conductive Sheet and Transfer Learning. IEEE Sens. J. 2020, 21, 1–11. [Google Scholar] [CrossRef]
- Brognara, L.; Palumbo, P.; Grimm, B.; Palmerini, L. Assessing gait in Parkinson’s disease using wearable motion sensors: A systematic review. Diseases 2019, 7, 18. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, K.; Tang, W. A Fully Wireless Wearable Motion Tracking System with 3D Human Model for Gait Analysis. Sensors 2021, 21, 4051. [Google Scholar] [CrossRef]
- Mitoma, H.; Yoneyama, M.; Orimo, S. 24-hour recording of parkinsonian gait using a portable gait rhythmogram. Intern. Med. 2010, 49, 2401–2408. [Google Scholar] [CrossRef] [Green Version]
- Morris, S.J.; Paradiso, J.A. Shoe-integrated sensor system for wireless gait analysis and real-time feedback. In Proceedings of the 24th Annual Conference and the Annual Fall Meeting of the Biomedical Engineering Society EMBS/BMES Conference (Second Joint), Houston, TX, USA, 23–26 October 2002; Volume 3, pp. 2468–2469. [Google Scholar]
- Darwish, A.; Hassanien, A.E. Wearable and implantable wireless sensor network solutions for healthcare monitoring. Sensors 2011, 11, 5561–5595. [Google Scholar] [CrossRef] [Green Version]
- Ye, M.; Yang, C.; Stankovic, V.; Stankovic, L.; Cheng, S. Distinct feature extraction for video-based gait phase classification. IEEE Trans. Multimed. 2019, 22, 1113–1125. [Google Scholar] [CrossRef] [Green Version]
- Valencia-Marin, C.K.; Pulgarin-Giraldo, J.D.; Velasquez-Martinez, L.F.; Alvarez-Meza, A.M.; Castellanos-Dominguez, G. An Enhanced Joint Hilbert Embedding-Based Metric to Support Mocap Data Classification with Preserved Interpretability. Sensors 2021, 21, 4443. [Google Scholar] [CrossRef] [PubMed]
- Sun, K.; Xiao, B.; Liu, D.; Wang, J. Deep high-resolution representation learning for human pose estimation. In Proceedings of the IEEE Conference on Computer Vision and Pattern Recognition, Long Beach, CA, USA, 16–20 June 2019; pp. 5693–5703. [Google Scholar]
- Fang, H.-S.; Xie, S.; Tai, Y.-W.; Lu, C. RMPE: Regional Multi-person Pose Estimation. In Proceedings of the 2017 IEEE International Conference on Computer Vision (ICCV), Venice, Italy, 22–29 October 2017; pp. 2353–2362. [Google Scholar]
- Zheng, C.; Wu, W.; Yang, T.; Zhu, S.; Chen, C.; Liu, R.; Shen, J.; Kehtarnavaz, N.; Shah, M. Deep learning-based human pose estimation: A survey. arXiv 2020, arXiv:2012.13392. [Google Scholar]
- Nandy, A. Statistical methods for analysis of Parkinson’s disease gait pattern and classification. Multimed. Tools Appl. 2019, 78, 19697–19734. [Google Scholar] [CrossRef]
- Balaji, E.; Brindha, D.; Balakrishnan, R. Supervised machine learning based gait classification system for early detection and stage classification of Parkinson’s disease. Appl. Soft Comput. 2020, 94, 106494. [Google Scholar]
- Lee, S.H.; Lim, J.S. Parkinson’s disease classification using gait characteristics and wavelet-based feature extraction. Expert Syst. Appl. 2012, 39, 7338–7344. [Google Scholar] [CrossRef]
- Di Biase, L.; Di Santo, A.; Caminiti, M.L.; De Liso, A.; Shah, S.A.; Ricci, L.; Di Lazzaro, V. Gait analysis in Parkinson’s disease: An overview of the most accurate markers for diagnosis and symptoms monitoring. Sensors 2020, 20, 3529. [Google Scholar] [CrossRef]
- Rupprechter, S.; Morinan, G.; Peng, Y.; Foltynie, T.; Sibley, K.; Weil, R.S.; Leyland, L.A.; Baig, F.; Morgante, F.; Gilron, R.; et al. A Clinically Interpretable Computer-Vision Based Method for Quantifying Gait in Parkinson’s Disease. Sensors 2021, 21, 5437. [Google Scholar] [CrossRef]
- Firmino, J. Using Deep Learning for Gait Abnormality Classification. Master’s Thesis, Instituto Superior Técnico, Lisbon, Portugal, 2019. [Google Scholar]
- Chen, R.J.; Lu, M.Y.; Chen, T.Y.; Williamson, D.F.; Mahmood, F. Synthetic data in machine learning for medicine and healthcare. Nat. Biomed. Eng. 2021, 5, 493–497. [Google Scholar] [CrossRef]
- Emam, K.; Mosquera, L.; Hoptroff, R. Practical Synthetic Data Generation: Balancing Privacy and the Broad Availability of Data; O’Reilly Media, Incorporated: Sebastopol, CA, USA, 2020. [Google Scholar]
- Nikolenko, S.I. Synthetic data for deep learning. arXiv 2019, arXiv:1909.11512. [Google Scholar]
- Rankin, D.; Black, M.; Bond, R.; Wallace, J.; Mulvenna, M.; Epelde, G. Reliability of supervised machine learning using synthetic data in health care: Model to preserve privacy for data sharing. JMIR Med. Inform. 2020, 8, e18910. [Google Scholar] [CrossRef]
- BioRender. Available online: https://biorender.com (accessed on 10 March 2022).
- Cao, Z.; Hidalgo, G.; Simon, T.; Wei, S.; Sheikh, Y. OpenPose: Realtime Multi-Person 2D Pose Estimation Using Part Affinity Fields. IEEE Trans. Pattern Anal. Mach. Intell. 2021, 43, 172–186. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bradski, G. The OpenCV Library. Dr. Dobb’s J. Softw. Tools 2000, 25, 120–123. [Google Scholar]
- Nakano, N.; Sakura, T.; Ueda, K.; Omura, L.; Kimura, A.; Iino, Y.; Fukashiro, S.; Yoshioka, S. Evaluation of 3D markerless motion capture accuracy using OpenPose with multiple video cameras. Front. Sport. Act. Living 2020, 2, 50. [Google Scholar] [CrossRef] [PubMed]
- Virtanen, P.; Gommers, R.; Oliphant, T.E.; Haberland, M.; Reddy, T.; Cournapeau, D.; Burovski, E.; Peterson, P.; Weckesser, W.; Bright, J.; et al. SciPy 1.0: Fundamental Algorithms for Scientific Computing in Python. Nat. Methods 2020, 17, 261–272. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Harris, C.R.; Millman, K.J.; van der Walt, S.J.; Gommers, R.; Virtanen, P.; Cournapeau, D.; Wieser, E.; Taylor, J.; Berg, S.; Smith, N.J.; et al. Array programming with NumPy. Nature 2020, 585, 357–362. [Google Scholar] [CrossRef]
- Parkinsonian Gait Video. Available online: https://www.youtube.com/watch?v=B5hrxKe2nP8&t=92s (accessed on 20 February 2022).
- Anzanello, M.J.; Fogliatto, F.S. Learning curve models and applications: Literature review and research directions. Int. J. Ind. Ergon. 2011, 41, 573–583. [Google Scholar] [CrossRef]
- Perlich, C. Learning Curves in Machine Learning. In Encyclopedia of Machine Learning; Springer: Berlin/Heidelberg, Germany, 2011; pp. 577–580. [Google Scholar]
- Ying, X. An overview of overfitting and its solutions. J. Phys. Conf. Ser. 2019, 1168, 022022. [Google Scholar] [CrossRef]
- Dietterich, T. Overfitting and undercomputing in machine learning. ACM Comput. Surv. 1995, 27, 326–327. [Google Scholar] [CrossRef]
- Jabbar, H.; Khan, R.Z. Methods to avoid over-fitting and under-fitting in supervised machine learning (comparative study). Comput. Sci. Commun. Instrum. Devices 2015, 70. [Google Scholar] [CrossRef]
- Gareth, J.; Daniela, W.; Trevor, H.; Robert, T. An Introduction to Statistical Learning: With Applications in R; Spinger: Berlin, Germany, 2013. [Google Scholar]
- Pedregosa, F.; Varoquaux, G.; Gramfort, A.; Michel, V.; Thirion, B.; Grisel, O.; Blondel, M.; Prettenhofer, P.; Weiss, R.; Dubourg, V.; et al. Scikit-learn: Machine Learning in Python. J. Mach. Learn. Res. 2011, 12, 2825–2830. [Google Scholar]
- Davis, J.; Goadrich, M. The relationship between Precision-Recall and ROC curves. In Proceedings of the 23rd International Conference on Machine Learning, Pittsburgh, PA, USA, 25–29 June 2006; pp. 233–240. [Google Scholar]
- Parkinson’s Disease & Low Back Pain—Case Study 21. Available online: https://www.youtube.com/watch?v=h2d2sPwD_mU (accessed on 15 March 2022).
- Chawla, N.V.; Bowyer, K.W.; Hall, L.O.; Kegelmeyer, W.P. SMOTE: Synthetic minority over-sampling technique. J. Artif. Intell. Res. 2002, 16, 321–357. [Google Scholar] [CrossRef]
- He, H.; Ma, Y. Imbalanced Learning: Foundations, Algorithms, and Applications; John Wiley & Sons: Hoboken, NJ, USA, 2013. [Google Scholar]
- Wahid, F.; Begg, R.K.; Hass, C.J.; Halgamuge, S.; Ackland, D.C. Classification of Parkinson’s disease gait using spatial-temporal gait features. IEEE J. Biomed. Health Inform. 2015, 19, 1794–1802. [Google Scholar] [CrossRef] [PubMed]
- Sousa, L.R.; Martins, B.C.R.; Oliveira, L.T.; Hallal, C.Z. Swing time as a predictive variable for Parkinson’s disease. Fisioter. E Pesqui. 2021, 28, 214–219. [Google Scholar]
- Vila, M.; Pérez, R.; Mollinedo, I.; Cancela, J.M. Analysis of gait for disease stage in patients with Parkinson’s disease. Int. J. Environ. Res. Public. Health 2021, 18, 720. [Google Scholar] [CrossRef] [PubMed]
- Mehrizi, R.; Peng, X.; Zhang, S.; Liao, R.; Li, K. Automatic health problem detection from gait videos using deep neural networks. arXiv 2019, arXiv:1906.01480. [Google Scholar]
- Albuquerque, P.; Machado, J.; Verlekar, T.T.; Soares, L.D.; Correia, P.L. Remote Pathological Gait Classification System. arXiv 2021, arXiv:2105.01634. [Google Scholar]
- Abdulhay, E.; Arunkumar, N.; Narasimhan, K.; Vellaiappan, E.; Venkatraman, V. Gait and tremor investigation using machine learning techniques for the diagnosis of Parkinson disease. Futur. Gener. Comput. Syst. 2018, 83, 366–373. [Google Scholar] [CrossRef]
- Moody, G.; Mark, R.; Goldberger, A. PhysioNet: A Web-based resource for the study of physiologic signals. IEEE Eng. Med. Biol. Mag. 2001, 20, 70–75. [Google Scholar] [CrossRef]
- Aich, S.; Youn, J.; Chakraborty, S.; Pradhan, P.M.; Park, J.; Park, S.; Park, J. A supervised machine learning approach to detect the on/off state in Parkinson’s disease using wearable based gait signals. Diagnostics 2020, 10, 421. [Google Scholar] [CrossRef]
- Abe, K.; Tabei, K.I.; Matsuura, K.; Kobayashi, K.; Ohkubo, T. OpenPose-based Gait Analysis System For Parkinson’s Disease Patients From Arm Swing Data. In Proceedings of the 2021 International Conference on Advanced Mechatronic Systems (ICAMechS), Tokyo, Japan, 9–12 December 2021. [Google Scholar]
- Pinceti, A.; Sankar, L.; Kosut, O. Generation of Synthetic Multi-Resolution Time Series Load Data. arXiv 2021, arXiv:2107.03547. [Google Scholar]
- Prudêncio, R.B.; Ludermir, T.B. Learning Weights for Linear Combination of Forecasting Methods. In Proceedings of the 2006 Ninth Brazilian Symposium on Neural Networks (SBRN’06), Ribeirao Preto, Brazil, 23–27 October 2006; pp. 113–118. [Google Scholar]
- Pereira, T.; Morgado, J.; Silva, F.; Pelter, M.M.; Dias, V.R.; Barros, R.; Freitas, C.; Negrão, E.; Flor de Lima, B.; Correia da Silva, M.; et al. Sharing biomedical data: Strengthening ai development in healthcare. Healthcare 2021, 9, 827. [Google Scholar] [CrossRef]
- Zhang, Y.; Gu, D. A Deep Convolutional-Recurrent Neural Network for Freezing of Gait Detection in Patients with Parkinson’s Disease. In Proceedings of the 2019 12th International Congress on Image and Signal Processing, BioMedical Engineering and Informatics (CISP-BMEI), Suzhou, China, 19–21 October 2019; pp. 1–6. [Google Scholar]
- Wen, Q.; Sun, L.; Yang, F.; Song, X.; Gao, J.; Wang, X.; Xu, H. Time series data augmentation for deep learning: A survey. arXiv 2020, arXiv:2002.12478. [Google Scholar]
- Moon, S.; Song, H.J.; Sharma, V.D.; Lyons, K.E.; Pahwa, R.; Akinwuntan, A.E.; Devos, H. Classification of Parkinson’s disease and essential tremor based on balance and gait characteristics from wearable motion sensors via machine learning techniques: A data-driven approach. J. Neuroeng. Rehabil. 2020, 17, 1–8. [Google Scholar] [CrossRef]
- Avasthi, A. Preserve and strengthen family to promote mental health. Indian J. Psychiatry 2010, 52, 113. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.; Lach, J.; Lo, B.; Yang, G.Z. Toward pervasive gait analysis with wearable sensors: A systematic review. IEEE J. Biomed. Health Inform. 2016, 20, 1521–1537. [Google Scholar] [CrossRef] [PubMed]
- Hu, Q.; Yi, C.; Kliewer, J.; Tang, W. Asynchronous communication for wireless sensors using ultra wideband impulse radio. In Proceedings of the 2015 IEEE 58th International Midwest Symposium on Circuits and Systems (MWSCAS), Ft. Collins, CO, USA, 2–5 August 2015; pp. 1–4. [Google Scholar]
- Hu, Q.; Tang, X.; Tang, W. Integrated asynchronous ultrawideband impulse radio with intrinsic clock and data recovery. IEEE Microw. Wirel. Components Lett. 2017, 27, 416–418. [Google Scholar] [CrossRef]
- Liu, Y.; Furth, P.M.; Tang, W. Hardware-efficient delta sigma-based digital signal processing circuits for the internet-of-things. J. Low Power Electron. Appl. 2015, 5, 234–256. [Google Scholar] [CrossRef] [Green Version]
- Rehman, R.Z.U.; Del Din, S.; Guan, Y.; Yarnall, A.J.; Shi, J.Q.; Rochester, L. Selecting clinically relevant gait characteristics for classification of early parkinson’s disease: A comprehensive machine learning approach. Sci. Rep. 2019, 9, 17269. [Google Scholar] [CrossRef] [Green Version]
- Raghunathan, T.E. Synthetic data. Annu. Rev. Stat. Its Appl. 2021, 8, 129–140. [Google Scholar] [CrossRef]



| Feature | Segmentation | Description | Calculation |
|---|---|---|---|
| Stride time | Type I | Duration between the first contact of the two consecutive footesteps of the same foot | t − t where for i = 1, 2, 3... |
| Stride length | Type I | Distance between successive points of contact of the same foot | + for i = 1, 2, 3... |
| Step time | Type I | Duration between consecutive heel strikes | t − t where for i = 1, 2, 3... |
| Step length | Type I | Distance between the contact of one foot and contact of the opposite | for i = 1, 2, 3 |
| Double Support | Type II | Period in which both feet are in contact with the floor | t − t where and for i = j = 1, 2, 3... |
| Swing time | Type II | Period in which only one foot is the ground | t − t where − for i = 1, 2, 3... |
| Classification Models | Hyper-Parameters Selected |
|---|---|
| KNN | n_neighbors = [1, 3, 5, 7, 9, 11, 13, 15], metric = [euclidean, manhattan, minkowski], weights = [uniform, distance] |
| SVM | C = [0.01, 0.1, 1, 10, 100], kernel = [linear, rbf], gamma = [scale] |
| GB | n_estimators = [1, 2, 5, 20, 50, 100] |
| Model | KNN | SVM | GB |
|---|---|---|---|
| Hyper-parameters | metric: euclidean, n_neighbors: 15, weights: uniform | C: 0.1, gamma: scale, kernel: rbf | n_estimators: 2 |
| Number of linear combinations | 80 | 200 | 40 |
| Model | Severity Level | TN | TP | FN | FP | Accuracy | Sensitivity | Specificity | F1 Score |
|---|---|---|---|---|---|---|---|---|---|
| KNN | I | 532 | 183 | 1 | 8 | 0.99 | 0.99 | 0.99 | 0.98 |
| II | 573 | 126 | 16 | 9 | 0.97 | 0.83 | 0.98 | 0.91 | |
| III | 521 | 172 | 9 | 22 | 0.96 | 0.95 | 0.96 | 0.92 | |
| IV | 506 | 203 | 14 | 1 | 0.98 | 0.94 | 0.99 | 0.96 | |
| SVM | I | 1396 | 359 | 41 | 34 | 0.96 | 0.90 | 0.98 | 0.91 |
| II | 1349 | 354 | 71 | 56 | 0.93 | 0.83 | 0.96 | 0.85 | |
| III | 1324 | 421 | 23 | 62 | 0.95 | 0.95 | 0.96 | 0.91 | |
| IV | 1261 | 536 | 25 | 8 | 0.98 | 0.96 | 0.99 | 0.97 | |
| GB | I | 282 | 80 | 0 | 0 | 1 | 1 | 1 | 1 |
| II | 268 | 87 | 3 | 4 | 0.98 | 0.97 | 0.99 | 0.96 | |
| III | 286 | 67 | 6 | 3 | 0.98 | 0.92 | 0.99 | 0.94 | |
| IV | 240 | 118 | 1 | 3 | 0.99 | 0.99 | 0.99 | 0.98 |
| Performance Evaluation Measurements | KNN | SVM | GB |
|---|---|---|---|
| Sensitivity | 0.94 | 0.91 | 0.97 |
| Specificity | 0.98 | 0.97 | 0.99 |
| Accuracy | 0.97 | 0.96 | 0.99 |
| PPV | 0.95 | 0.91 | 0.97 |
| NPV | 0.98 | 0.97 | 0.99 |
| F1 score | 0.94 | 0.90 | 0.97 |
| References | Data acquisition | Methods | Accuracy |
|---|---|---|---|
| Rupprechter et al. [20] | 729 subjects | RFC, LDA, LOGIS, ANN, SVM, XGBoost | 47.0–50.0% |
| Balaji et al. [17] | Physionet | DT, SVM, EC, BC | 69.7–99.4% |
| Abdulhay et al. [49] | Physionet | Medium Tree, Medium Gaussian SVM | 90.0–94.8% |
| Aich et al. [51] | 20 PD subjects | RF, SVM, KNN, Naïve Bayes | 86.0–96.7% |
| Proposed method | Synthetic data | SVM, GB, KNN | 96.0–99.0% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marquez Chavez, J.; Tang, W. A Vision-Based System for Stage Classification of Parkinsonian Gait Using Machine Learning and Synthetic Data. Sensors 2022, 22, 4463. https://doi.org/10.3390/s22124463
Marquez Chavez J, Tang W. A Vision-Based System for Stage Classification of Parkinsonian Gait Using Machine Learning and Synthetic Data. Sensors. 2022; 22(12):4463. https://doi.org/10.3390/s22124463
Chicago/Turabian StyleMarquez Chavez, Jorge, and Wei Tang. 2022. "A Vision-Based System for Stage Classification of Parkinsonian Gait Using Machine Learning and Synthetic Data" Sensors 22, no. 12: 4463. https://doi.org/10.3390/s22124463
APA StyleMarquez Chavez, J., & Tang, W. (2022). A Vision-Based System for Stage Classification of Parkinsonian Gait Using Machine Learning and Synthetic Data. Sensors, 22(12), 4463. https://doi.org/10.3390/s22124463






