Abstract
The real-time artery diameter waveform assessment during cardio cycle can allow the measurement of beat-to-beat pressure change and the long-term blood pressure monitoring. The aim of this study is to develop a self-calibrated bio-impedance-based sensor, which can provide regular measurement of the blood-pressure-dependence time variable parameters such as the artery diameter waveform and the elasticity. This paper proposes an algorithm based on analytical models which need prior geometrical and physiological patient parameters for more appropriate electrode system selection and hence location to provide accurate blood pressure measurement. As a result of this study, the red cell orientation effect contribution was estimated and removed from the bio-impedance signal obtained from the artery to keep monitoring the diameter waveform correspondence to the change of blood pressure.
1. Introduction
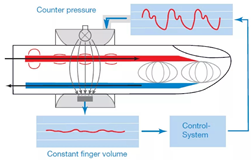
Arterial blood pressure is the main physiological indicator of cardiovascular system [1,2]. However, a deviation from normal range can be used to identify different diseases such as thrombosis and atherosclerosis, which can lead to mortality if the medical intervention is not started on time [3,4]. The arterial blood pressure parameters tend to change over time, so long-term monitoring helps to provide more accurate evaluation of the patient’s condition, as well as beat-by-beat measurement of blood pressure, which could offer several advantages toward the early detection and the patient response to specific therapy and medication [5]. Currently, there are several approaches for blood pressure measurement [6,7,8,9,10,11,12,13,14]. The blood pressure assessment by sphygomomanometry is the widely used method in medical practice due to its simplicity and sufficient accuracy; however, this method cannot provide long-term measurements due to frequent occlusion [11]. The noninvasive arterial blood pressure waveform estimation based on an arterial cross-sectional area measurement combined with an elasticity measurement of the vessel has been developed using ultrasound [6]. However, the devices created by scientists based on these approaches are either stationary or more dimensional. The optical based methods are unreliable for obese patients, while the tonometry methods require a specific anatomical structure with superficial artery supported by bone and so is sensitive to the device placement [15,16,17]. The analysis of blood pressure estimation methods is summarized in Table 1.

Table 1.
Blood pressure estimation techniques.
Recently, the pulse transit time-based methods have been widely used in order to develop a wearable device that can measure blood pressure continuously. Two sensors located at two different sites can measure the pulse waveforms, which can be used to calculate the pulse transit time (PTT) value. The change of the PTT value shows a strong correlation with blood pressure [3]; however, the standard model equation used for this calculation depends on the artery diameter, which cannot be identified for large measurement segments [35]. In [6], there is an attempt to develop a portable blood pressure device based on local PTT measurements. However, the mathematical model used in this work is identified for the volume change in the whole segment under study, which makes the estimation based on this model not accurate and not related to diameter change. Thus, the aim of this study is to develop a wearable bio-impedance sensor for blood pressure waveform monitoring. This method is based on electrical impedance measurement in a small segment with uniform artery diameter and depth. The sensor provides regular measurement of the pressure-dependent physiological parameters such as the artery diameter waveform and elasticity, which allow the accurate measurement of blood pressure. This work proposes the use of a mathematical model for diameter waveform assessment; however, the required ultrasound-based information before the measurement provides specific sensor parameters, which lead to a more accurate determination of blood pressure. According to [35,36,37], the arterial wall elasticity changes with the blood pressure change; thus, this work proposes an additional measurement of pulse transit time, which can help the regular estimation of arterial elasticity change. The idea of red cell orientation effect estimation was suggested by [38,39] to better understand the impedance cardiography waveforms. However, the idea of understanding the orientation effect contribution to the peripheral bio-impedance signal obtained from the specific small segment illustrated in this study is the first according to our knowledge.
As a result, a key objective of this study is to improve the accuracy of the existing algorithm based on PTT measurement to estimate the arterial blood pressure by taking into account the contribution of red cell orientation effects as well as the artery diameter and stiffness change during long-term monitoring.
2. Materials and Methods
2.1. Mathematical Model
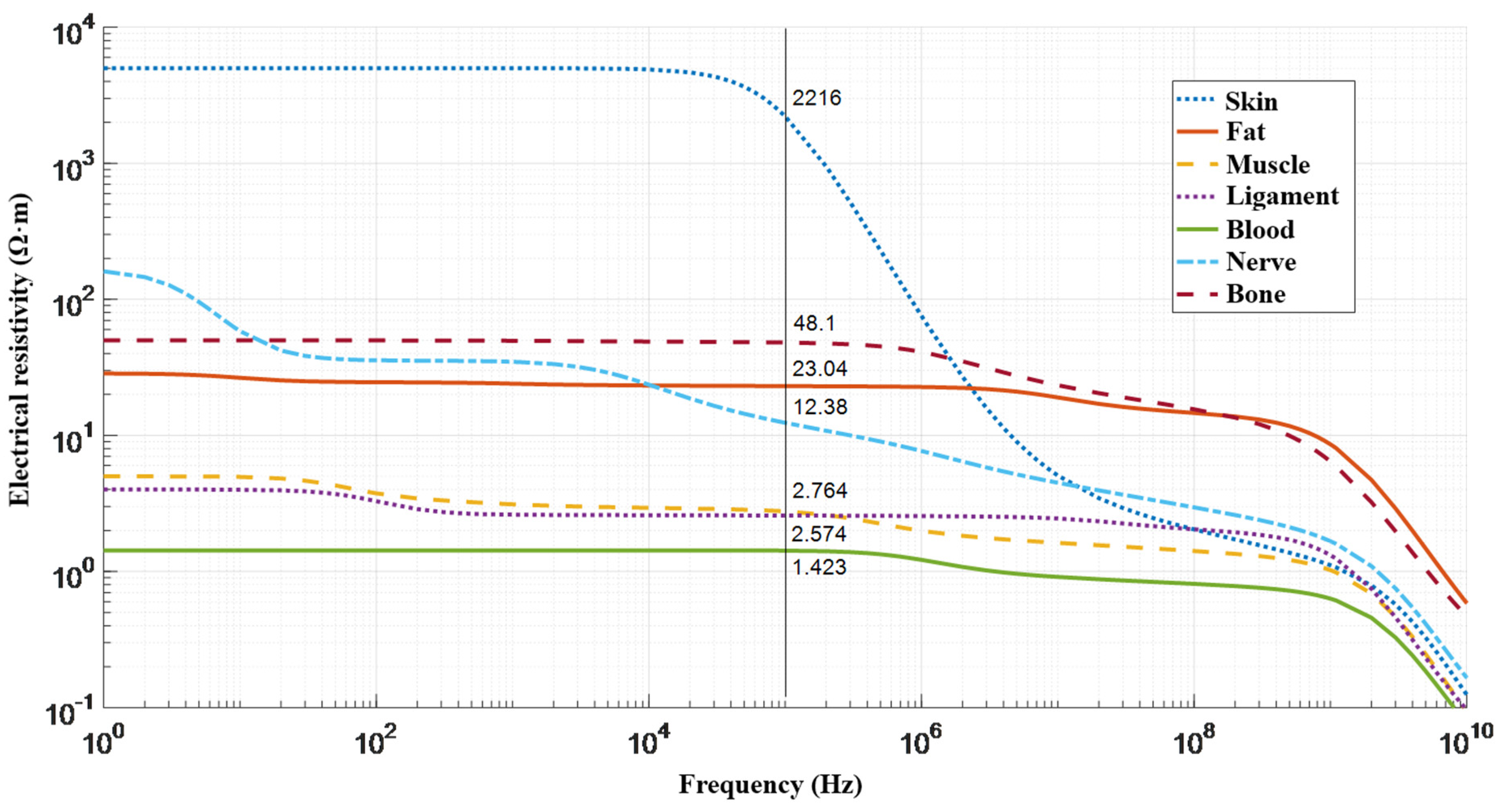
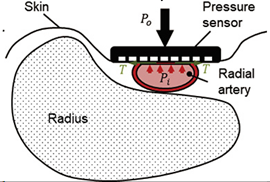
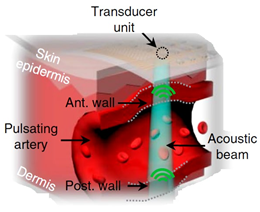
For artery diameter waveform assessment from the corresponding electrical bio-impedance signal, it is required to develop a justified mathematical model which characterizes the region of interest with full details [40]. To solve this problem, both analytical and numerical methods can be used. As a rule, numerical methods for solving problems, describing the electric current distribution through biological tissues, involve powerful computing systems, which do not solve the issue of calculating the necessary numerical estimates in real time, inherent in wearable monitoring systems. However, in the case of a semi-homogenous study area, the analytical approaches with some assumptions are promising towards the solution of this problem. Accordingly, the region of interest should be a place with a peripheral artery that can be isolated from the adjacent artery branches and veins to obtain the required bio-impedance measurement without any deterioration and additional sources that can affect the desired signal from the selected artery. However, the region of interest, where the major arteries widely used for such measurement [41] are the carotid, brachial, and radial arteries, comprises such tissues which have different conductivity [42]. The electrical resistivities of different tissues in the region of interest as a function of frequency are shown in Figure 1.
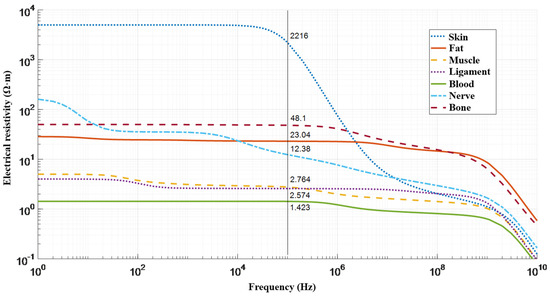
Figure 1.
Resistivities for various human tissues in the region of interest as a function of frequency [43].
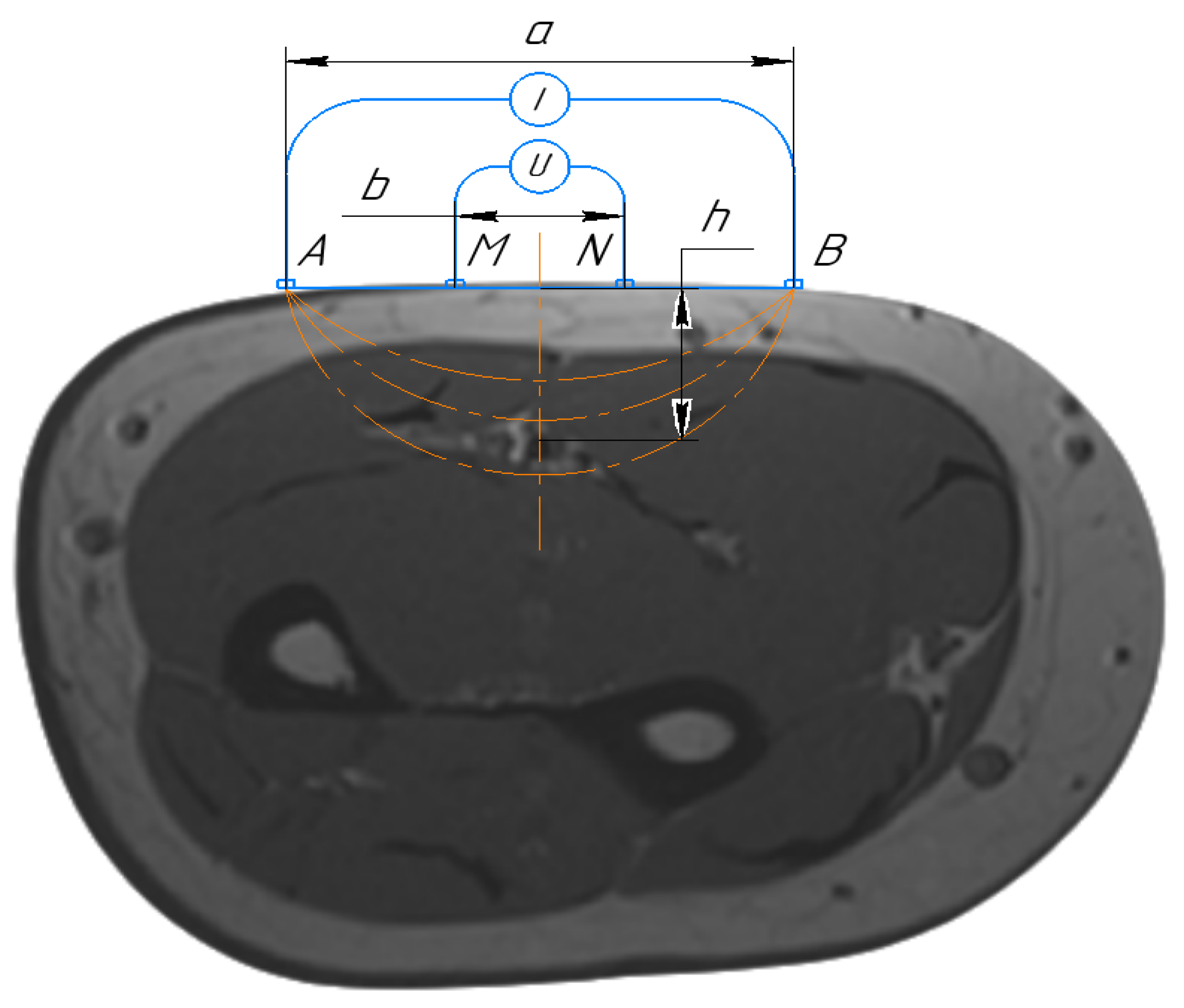
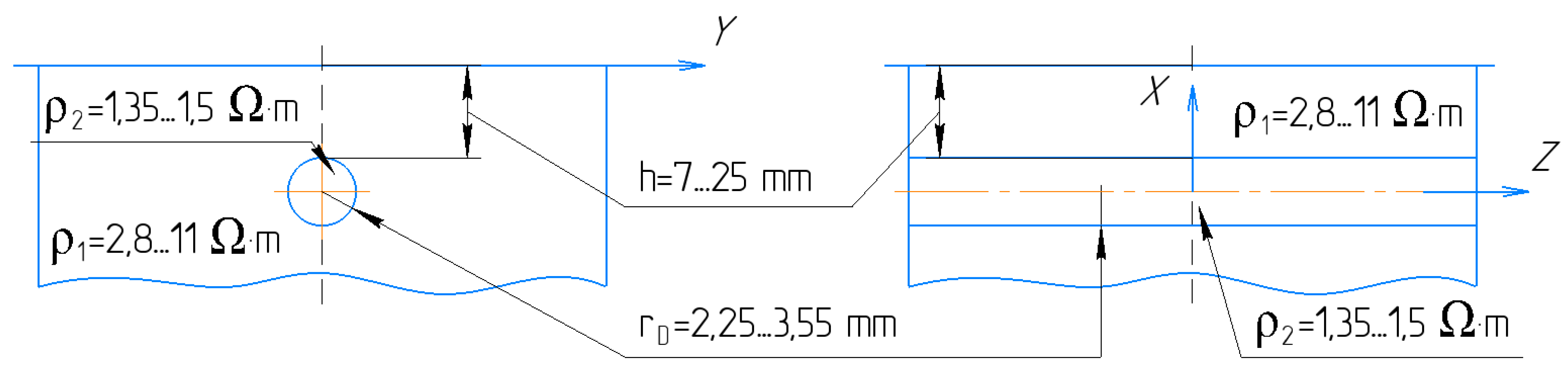
Thus, an electrical current with 100 kHz was considered in this work as the impact of the capacitive part, which was determined by the heterogeneity of tissue structures in the region of interest as less than 10%. Morever, a four-electrode system configuration, which is shown in Figure 2, was proposed in this study to provide the desired accuracy for bio-impedance measurement; thus, two outer electrodes were used to inject a small alternating current into the human body. The voltage drop between the inner electrodes was measured to calculate the impedance, while the electrode impedances did not contribute to the measured voltage.
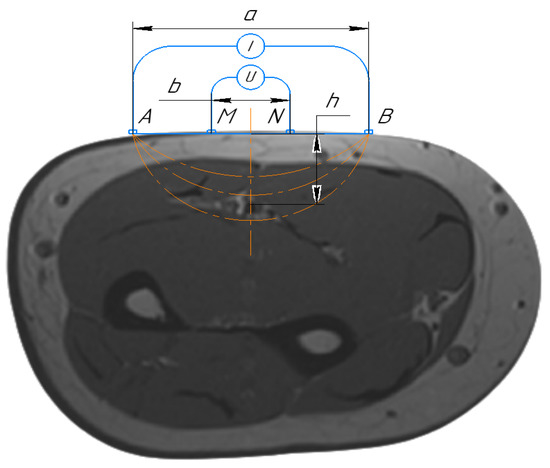
Figure 2.
Schematic diagram of the four-electrode setup. A and B are the current electrodes, M and N are the measuring electrodes.
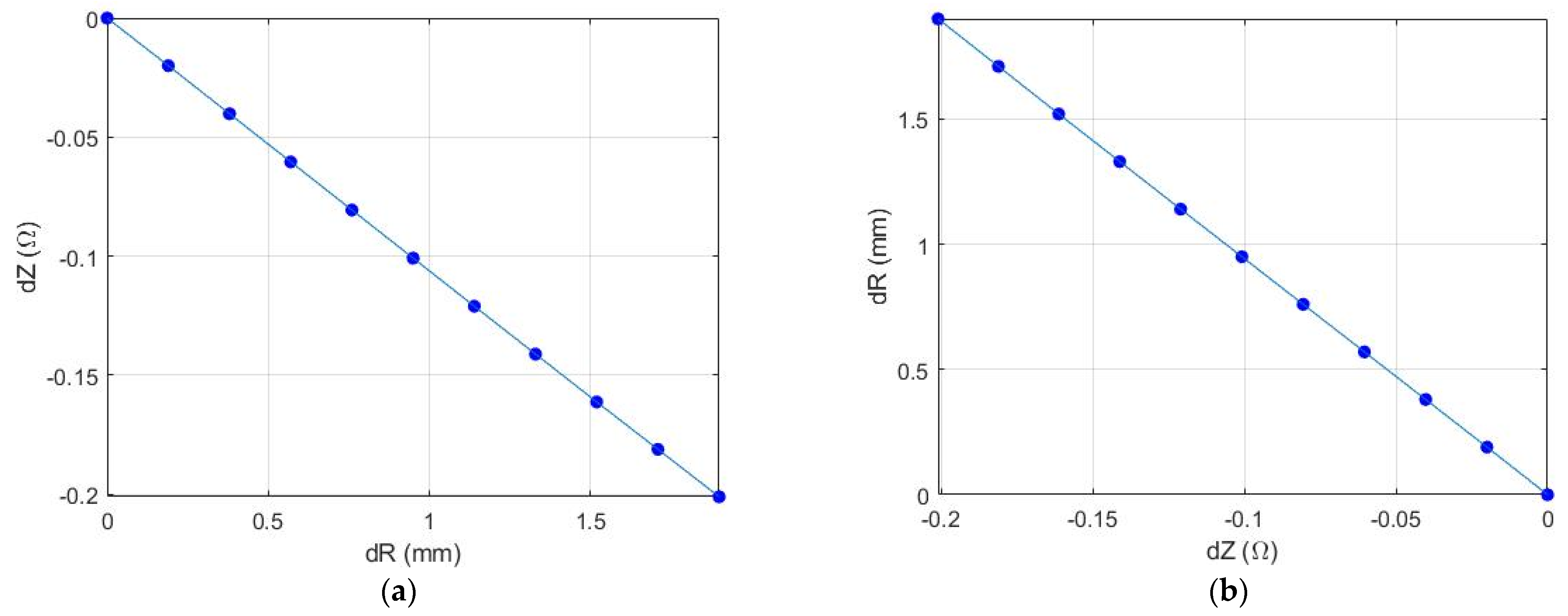
Thereby, for small segment selection, where the change of blood volume is dominated by the artery diameter, it is acceptable to join all tissues around the artery with common apparent resistivity . This assumption could minimize the requirement of the mathematical model as well as the calculation time without losing the desired accuracy. As a result, an analytical solution for the mathematical model of uniform space with cylinder inclusion was proposed in this work, while the artery and the surrounding tissues are modeled by a cylinder and uniform half-space, respectively, as shown in Figure 3.
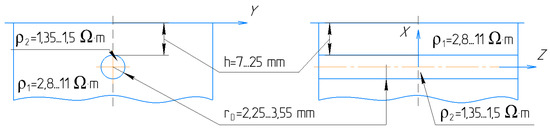
Figure 3.
The mathematical model of artery in the region of interest.
In the proposed mathematical model, the electrical potential is a solution of Laplace’s equation in cylindrical coordinates with appropriate boundary conditions associated with a cylinder [44]. This model considers orthogonal electrode system placement regarding the artery, and with prior information about the artery depth and diameter, the appropriate electrode system can be set. The analytical solution of the proposed mathematical model is a function, which depends on serval parameters shown in Equation (1). The limit values for the model parameters that can be measured are illustrated in Figure 3. Thus, depending on the prior obtained information, the doctor can also select the right place for sensor placement, which can be the brachial, radial, or carotid artery depending on patient obesity.
where a is the distance between current electrodes, b the distance between potential electrodes, r the artery radius, h artery depth, x is the displacement of the electrode system relative to the center of the artery. This work proposes accurate placement of the electrode system regarding the artery position, which is why the x parameter is equal to zero.
The apparent resistivity of the surrounding tissues can be calculated from the measured base impedance value according to [40] which is a quasi-constant value, while the resistivity of blood is a function, which depends on different factors such as hematocrit, temperature, viscosity, velocity, and share rate [45,46].
Basically, for artery diameter change estimation based on the corresponding bio-impedance measurement, the inverse problem for the proposed model should be obtained as shown in Equation (2). However, this approach requires multichannel measurements and sophisticated calculation, which make it undesirable for a portable monitoring system.
The initial calibration step which requires prior information such as the artery diameter and depth as well as the blood velocity allows minimizing the multi-parameter model to one unknown parameter function. The only unknown dynamic parameter of the proposed model is the diameter change of a cylinder, which simulates the artery diameter change and the blood volume change in arteries. This unknown parameter can be estimated from the measured pulse impedance from an artery by means of the dependence dR = func(dZ), which is the inverse of the forward dependence dZ = func(dR) that can be obtained on the basis of the proposed analytical model. Figure 4 shows the pulse impedance change depending on artery diameter change and vice versa. The observed decrease in impedance with an increase in artery diameter can be explained by the fact that blood is a more conductive medium comparing with the surrounding tissues. However, since the function dZ = func(dR) is monotone, then there is a unique inverse solution for this function. Thus, an iterative algorithm to address the linear inverse value of the diameter change was proposed in this paper.
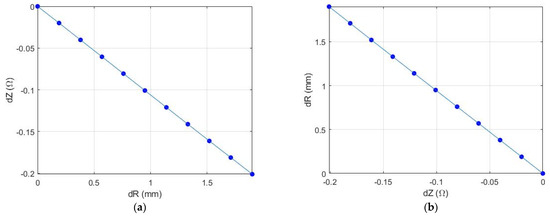
Figure 4.
The dependence of electrical impedance changes due to artery diameter change: (a) The forward problem; (b) the inverse problem.
This model, nevertheless, has an assumption of point electrodes and does not take into consideration the electrodes’ dimensions. It was verified for adequacy in previous study by this author [40] and concluded for its application to resolve the forward and inverse problem. Moreover, the use of spherical electrodes can minimize this error as the current distribution from a point physically not differing from the sphere.
2.2. Red Blood Cell Orientation Effect Estimation
The generation of shear forces across the width of a blood artery vessel during flow causes the cells to align with the minimal cross-sectional area facing the direction of flow. This in turn results in a larger cross-sectional area of plasma and a reduction in the resistivity of the blood as the flow increases [38]. Understanding the contribution of this effect on the peripheral impedance signal is a vital step in achieving the artery diameter waveform [12,13,36]. The experimental study, which was conducted in vitro on rigid tubes [38], showed a blood resistivity change of 15–30% due to erythrocyte orientation, and according to [38,39], the change of blood resistivity due to velocity can be estimated using Equation (3). This equation was deduced for the longitudinal electrode system position regarding the artery axis. However, the red cell contribution of the blood electrical resistivity change on the orthogonal direction is the same in value but with opposite direction [47].
where is the blood electrical resistivity, is the shear rate averaged over the cross section of the vessel, and H is the hematocrit [48].
The shear rate averaged over the cross-section of the vessel is determined by Equation (4) [49].
where is the maximum velocity in the center of the vessel estimated using spectral Doppler [50,51], R is the radius of the vessel, n is the exponent of the power law, n = 2 for a parabolic profile and more than 2 for a flat profile.
2.3. Elastic Modulus Estimation
The elastic response of a blood vessel can be expressed in terms of compliance, dispensability, stiffness, or elastic modulus [52,53]. According to [53], the elasticity modulus is not a constant parameter and can vary in a wide range, depending on internal and external factors. These changes will cause an additional error in blood pressure; thus, the blood pressure estimation is based on mathematical models, which contain such parameters as the diameter change and the elasticity modulus. The elastic modulus is related to the pulse wave velocity and the artery thickness by the Moens–Korteweg Equation (5) below [54].
where V is the pulse wave propagation speed, E is elastic modulus of the artery wall, is the arterial blood density, d is the radius of the artery, ha is the vessel thickness.
The measurement of local pulse wave velocity (PWV), which can be achieved by measuring the pulse waveform from two different points, can determine the actual elasticity of the artery in the region of interest, while adding a sensor that can provide the monitoring of this value and recalibrate the system according to this change can allow the accurate beat-to-beat blood pressure measurement.
2.4. Experimental Setup
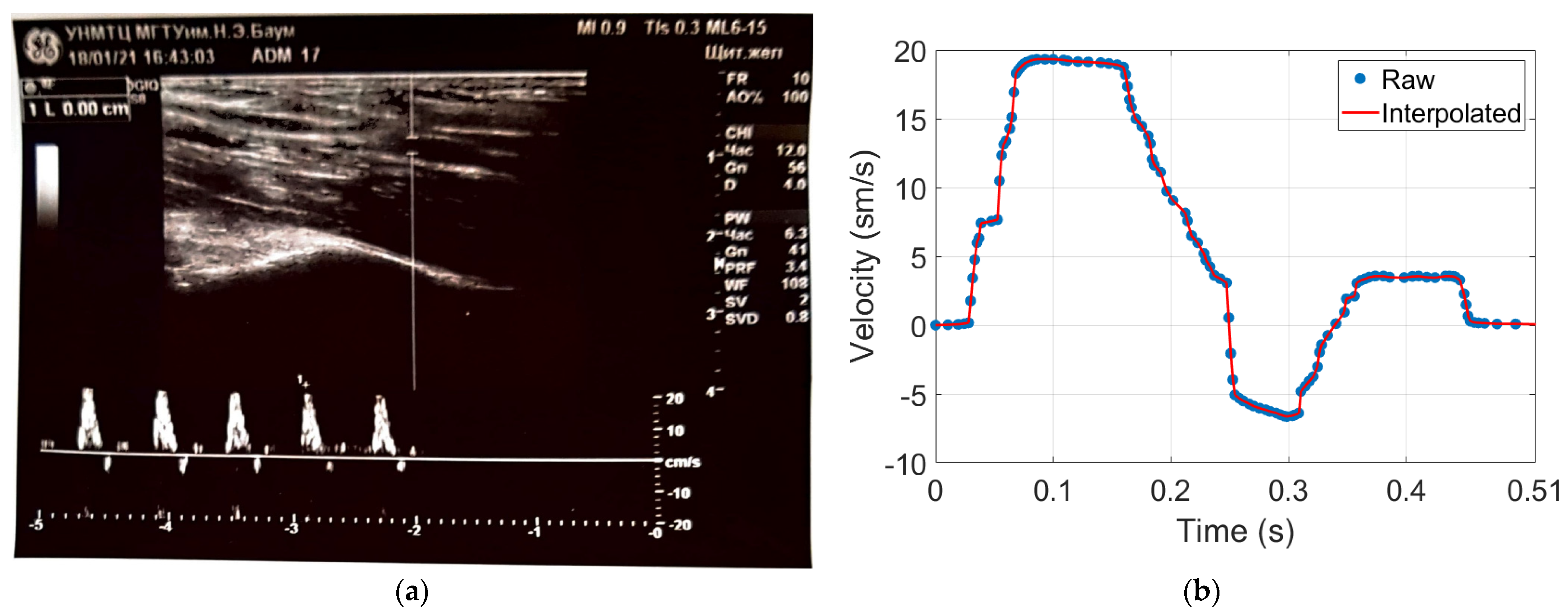
The experimental study was conducted at the medical center of Bauman Moscow State Technical University and the research ethics was followed. Four healthy young subjects were involved in this study. The measurements were performed on the arm in the area of the elbow joint, at the distal end of the brachial artery before the bifurcation into radial and ulnar arteries. The advantage of this location is the access to control the right electrode position regarding the artery location [55]. The General Electric model LOGIC S8 with an ML6-15-D ultrasonic transducer at a frequency of 6.3 MHz was used during this study to obtain prior information such as the arterial blood velocity, diameter, depth, and the wall thickness as shown in Figure 5. Figure 5a shows the brachial artery velocity, which can be used for red cell orientation effect estimation, while the artery diameter and depth were also determined. These data have been used as inputs for the mathematical model to select the appropriate electrodes system as well as the further estimation of red cell orientation effect and the brachial artery waveform diameter. The blood velocity curves for all subjects obtained using US were digitized and averaged as shown in Figure 5b.
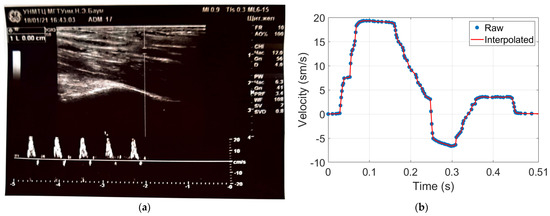
Figure 5.
The obtained data using Doppler US: (a) brachial blood velocity assessment during 5 cardio cycles; (b) the averaged blood velocity curve.
The multichannel system Reo-32 was used for bio-impedance measurement. The system provides a 4-electrode technique by applying an alternating current of frequency of 100 kHz and constant amplitude to a 3-mA-current electrode, and provides simultaneous measurement through different measuring channels [56]. The technical specifications of the multichannel system are illustrated in Table 2.

Table 2.
The technical specification of Reo-32.
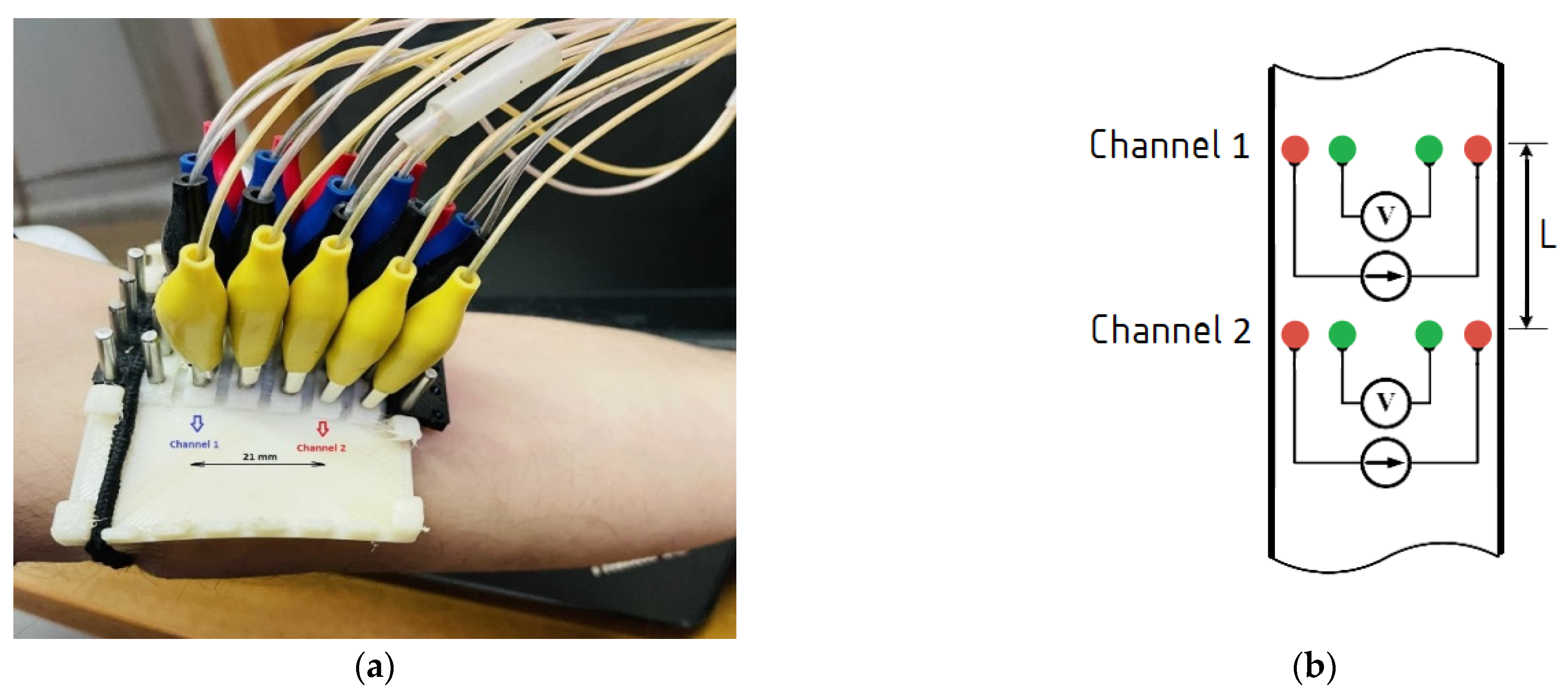
The electrode system array shown in Figure 6 was designed for the multichannel measurement. The electrode array provides electrical impedance mapping from 5 adjacent points. Dry electrodes with a diameter of 5 mm and a distance between adjacent electrodes of 7 mm were used to provide symmetrical and identical requirements for measurements for the bio-impedance signal obtained from the artery, which depend also on the electrode system spacing. The advantage of this electrode system is the ability to control the desired artery position.
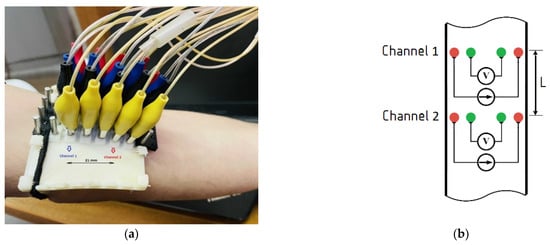
Figure 6.
The electrode system prototype: (a) multichannel electrode system placement; (b) the layout scheme of the relative electrodes’ positions and channels in the region of interest.
Figure 6a shows the experimental setup and the electrode placement in the region of interest. Skin preparation prior to electrode placement on a patient was performed to increase the conductivity for the dry electrodes. The right location of the electrode system was controlled by the obtained signals from all the measuring channels. Non-inversion behavior of signals was observed, which testifies that the whole artery length was located in the positive sensitivity region of the electrode system.
The obtained bio-impedance signals were used for both diameter estimation and the local brachial artery stiffness index, which were performed from 2 channels located in parallel at a distance of L = 21 mm as shown in Figure 6b.
3. Results
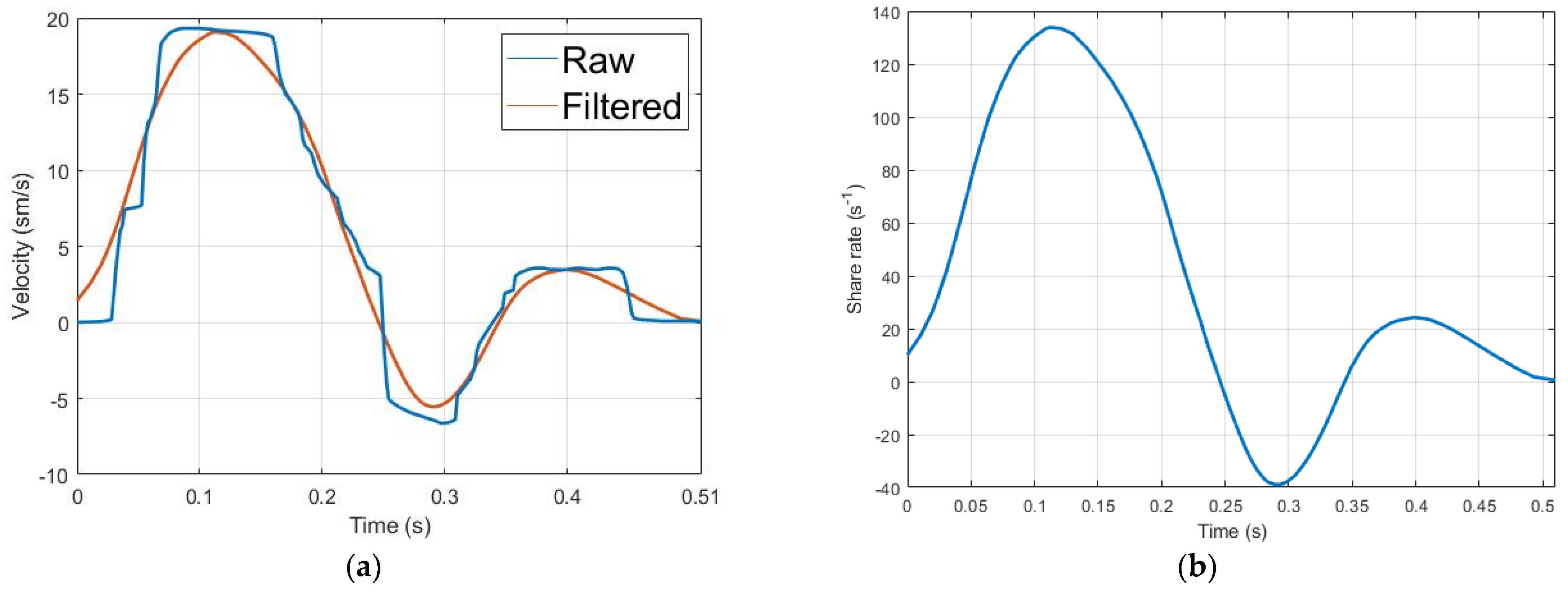
As shown in Figure 7a, the blood velocity curve obtained from US was digitized and approximated by linear interpolation, then filtered by a Savitzky–Golay filter to get an adequate signal for shear rate estimation. Thus, Savitzky–Golay filtering can provide accurate smoothing by using polynomial approximation of local least-squares [57]. The obtained filtered curve of blood velocity was used for share rate assessment using Equation (4), while the exponent of the power law (n) was equal to 2 as the velocity profile was parabolic. Figure 7b shows the obtained share rate curve, which has been used as an input for the blood cell orientation effect estimation model shown in Equation (3). The hematocrit value during this calculation was accepted to be equal to 47%, which corresponds to a normal healthy value.
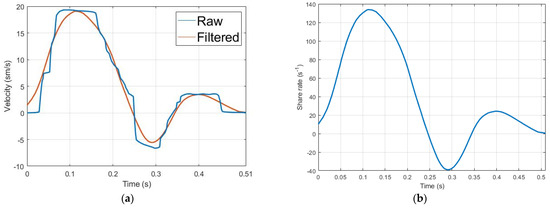
Figure 7.
The red blood cells’ orientation effect estimation; (a) the averaged and smooth arterial blood velocity curve; (b) blood share rate curve.
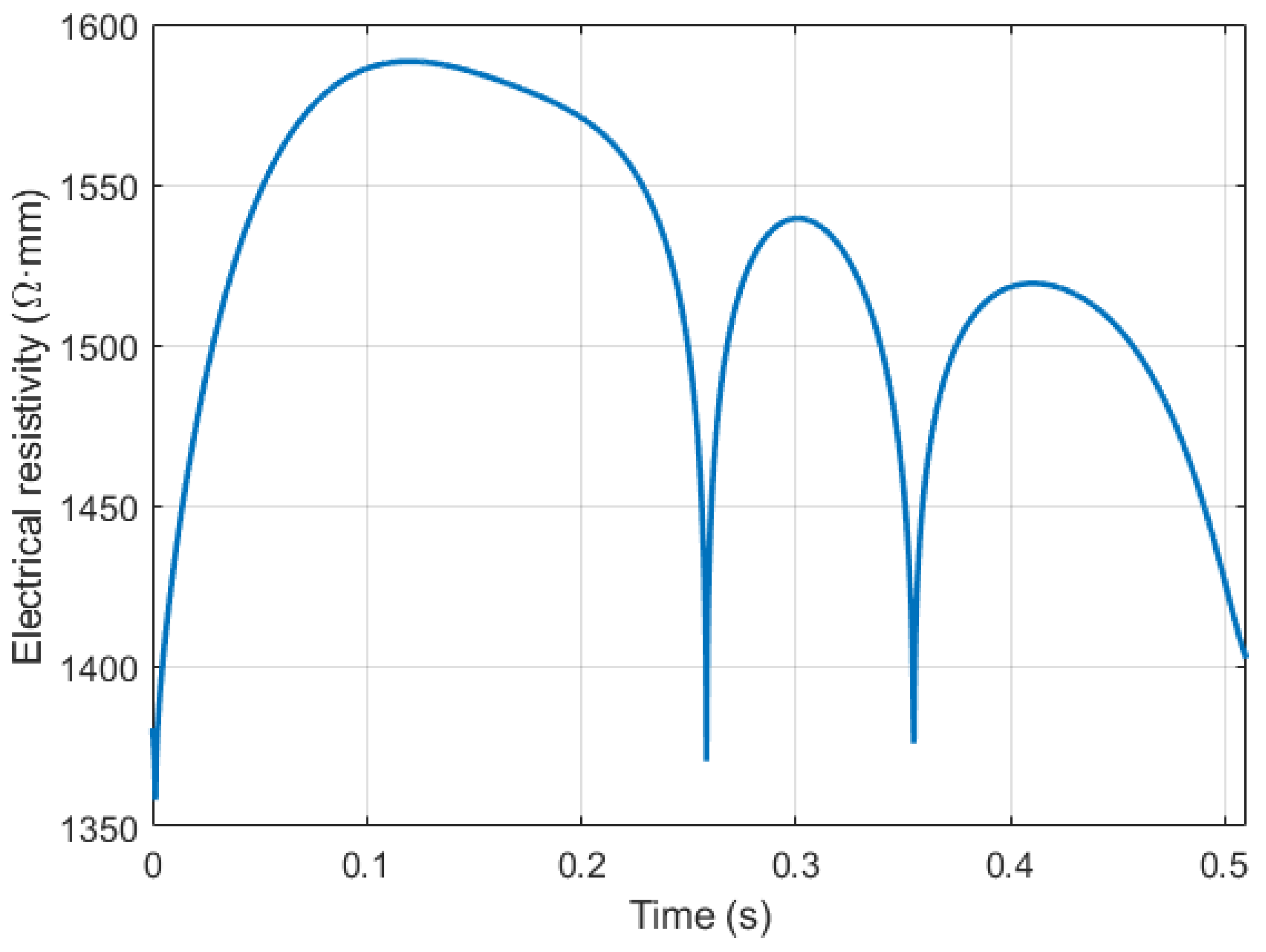
Figure 8 shows the blood resistivity change due to red cell orientation effect for one of the involved subjects, which corresponds to a 16% increase compared with the initial blood resistivity value 1.35 Ohm·m. [58]. The obtained results from the first step showed the high contribution of brachial blood velocity in the electrical impedance change, respectively; the change behavior of this value during the cardiac cycle should be taken into consideration for the following steps and calculations.
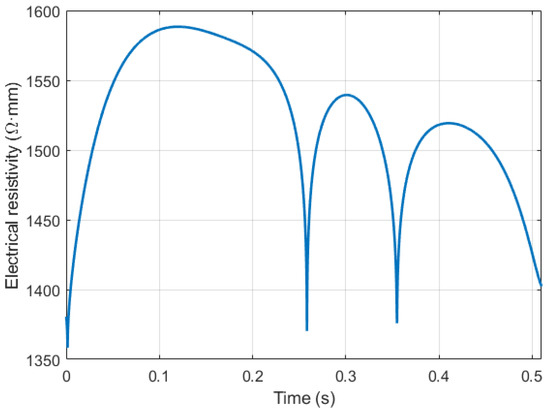
Figure 8.
The blood resistivity change caused by red blood cells’ orientation effect.
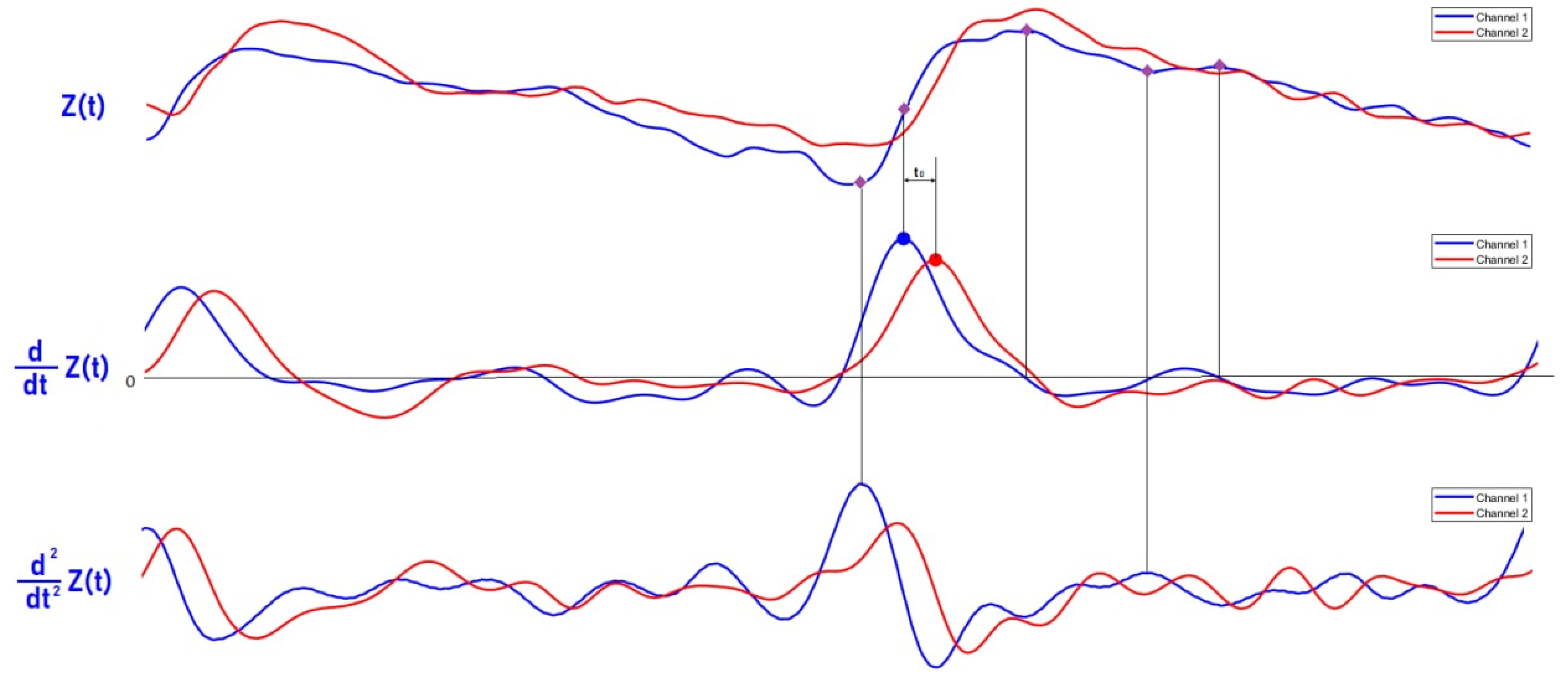
Figure 9 shows the electrical bio-impedance signals obtained from the brachial artery. Simultaneously, the base impedance and the pulse impedance were recorded. Nevertheless, the designed electrode system provides simultaneous measurement from five adjacent locations; two signals were selected for further processing. The selected signals were far from each other by 21 mm, which were enough to get the PTT [6,58]. Moreover, this distance was enough to select a uniform segment of artery as the recoding signals were equal in amplitude but have a shift in time due to different location of the measuring electrodes.
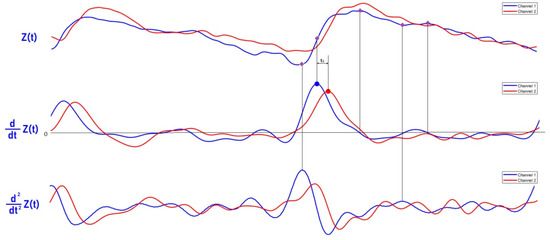
Figure 9.
The recording of the bio-impedance signal with the first and second derivative.
The analytical solution of the proposed mathematical model is an infinite sum of Bessel functions. Thus, in order to reduce the computation time, an algorithm based on the first and the second derivative was developed for five points per cardiac cycle extraction from the measured pulse waveforms. The first point is the diastolic point that corresponds to the maximum of the second derivative; the second point is the maximum slope point in the middle of the ascending point section that corresponds to the maximum of first derivative; the third point is the systolic point that corresponds to the zero value of the first derivative; the fourth point is the dicrotic notch that corresponds to the maximum of the second derivative; and the fifth point is the reflection point. The selected points are necessary for full restoration of the diameter waveform shape and its correct amplitude; thus, the time derivative of the bio-impedance signal was obtained by the following transfer function:
where T is the sampling period; z is the recorded bio-impedance signal.
According to the obtained data from the previous sections, the diameter waveform was estimated by the following algorithm: as the electrode system was located against the artery, the red cell orientation effect increased the blood electrical resistivity; correspondingly, the shown in Figure 8 was added to the actual blood resistivity , which was equal to 1.35 Ohm.m. The rest of the model parameters such as the radius and depth are constant as shown in Equation (7).
The base impedance was used to estimate the apparent resistivity of the region of interest according to Equation (8) [40], while the is the recorded pulse impedance signal shown in Figure 9.
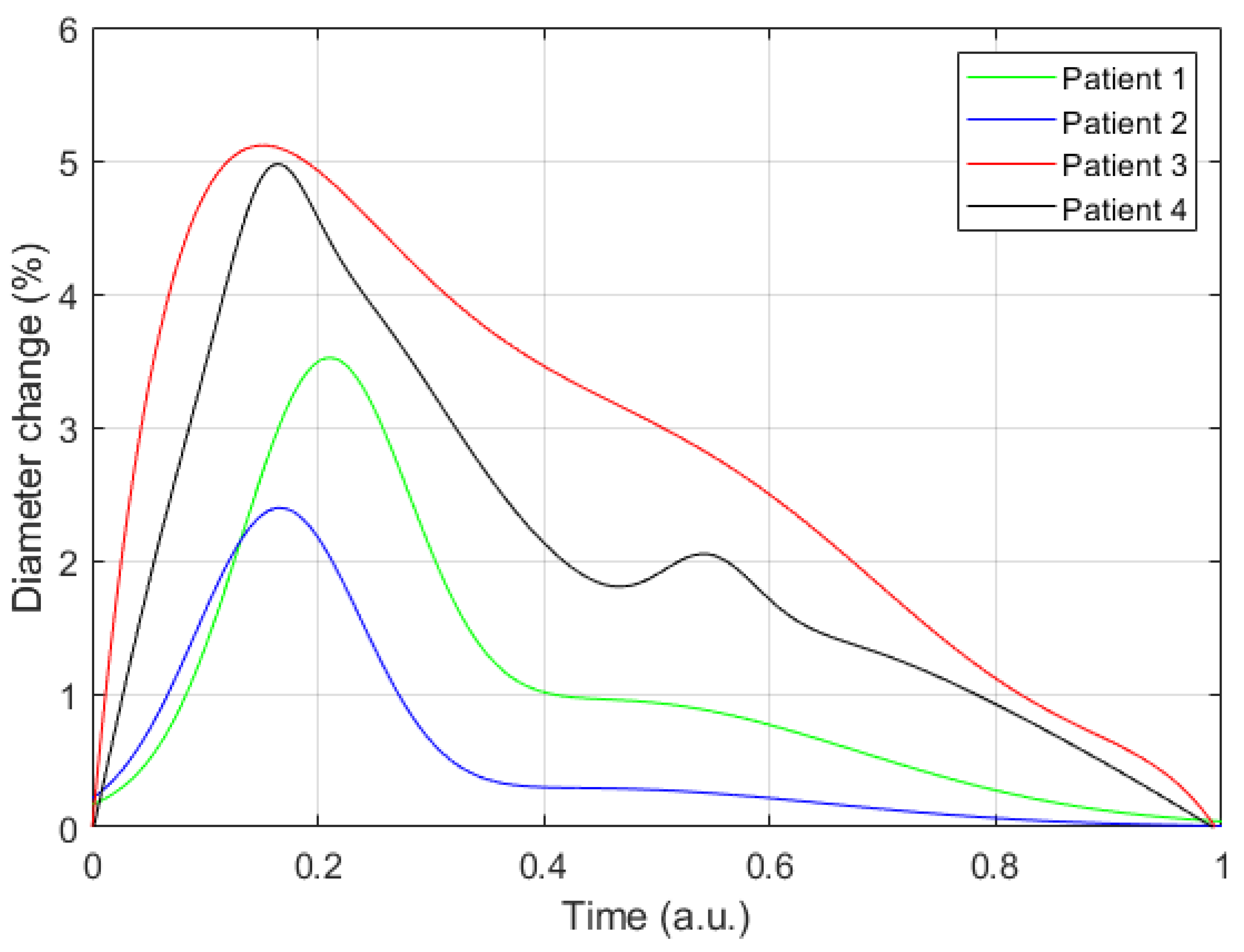
For every selected point based on the derivative-based algorithm, the artery diameter change was evaluated and, correspondingly, the diameter artery waveform was restored. Figure 10 shows the obtained diameter change for the four involved subjects; these curves show the percentage change in artery diameter relative to diastolic diameter DD. However, the obtained curves of diameter waveform reflect the nature of blood pressure change during the cardio cycle.
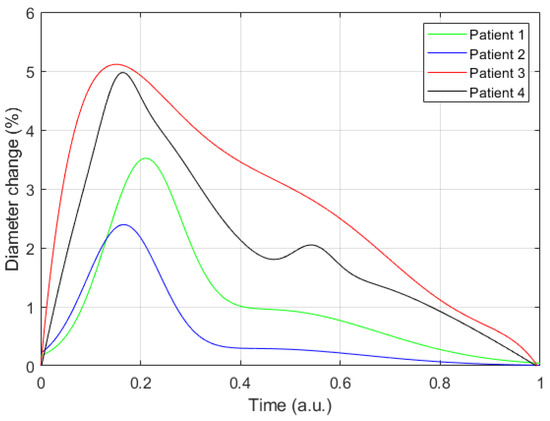
Figure 10.
The resulting curves of diameter changing for four patients.
Basically, the local brachial elasticity was estimated from the time delay between the two recorded signals. The maximum of the first derivative was selected as a specific point to get the PTT between two points with an inaccuracy of ±0.001 s corresponding to a sample frequency of 500 Hz. According to Equation (5) and based on the obtained PTT values, the local brachial artery elastic modulus was determined and illustrated in Table 3: the obtained values correspond to healthy arteries [59]. However, these values can vary significantly with blood pressure change and the bio sensor should be recalibrated according to the possible change.

Table 3.
The obtained results from experimental studies.
4. Discussion
This work presents a new method for real-time arterial diameter waveform estimation, which can improve the accuracy of blood pressure measurement. This method is based on an electrical bio-impedance signal obtained from an artery using appropriate electrode system with dry electrodes. The bio-impedance pulse obtained from the artery dominantly contains different mechanisms, which have absolutely different behaviors depending on the location of the bio-impedance sensor against the artery. According to the proposed electrode system position in this study, the diameter change leads to increase in the blood conductivity while the velocity effect goes in the absolute opposite direction, which makes the diameter waveform assessment a big challenge to be extracted from the integral signal that has these two coherent mechanisms. In this study, a mathematical model, which is a function of different geometrical and electrophysiological parameters, was proposed to get the artery diameter waveform. However, the inverse problem of this model requires sophisticated mathematical calculations, which makes it not suitable for a wearable device for the blood pressure monitoring. Alternatively, the prior information required for this study using the US allowed minimizing the multi-parameter model to one unknown parameter function. The change of the peripheral arteries’ diameter during the cardio cycle was very low compared with its own diameter, hence, the electrical bio-impedance change due to this variation was also very low. Thus, the prior calculation using the mathematical model helps to select not only the appropriate electrode system parameters but also the right arterial site position for measuring the bio-impedance signal, which can be in the brachial, carotid, or radial artery, in order to provide accurate blood pressure measurement. The effect of the red cell orientation on the electrical bio-impedance of pulsatile blood flow through the brachial artery, which was considered in this study, is the first for the implications of artery diameter waveform estimation. Although the pulse transit time has been a promising non-invasive and cuff-less method to measure blood pressure, the blood pressure–PTT relationship, which is modelled by the Moens–Korteweg, was derived from a simplified mechanical model, which was insensitive to the artery diameter change. This can lead to an error with arterial pressure measurement, especially in young patients where the artery diameter can be noticeably changed with the change of blood pressure. Thus, improving the accuracy of the existing algorithm based on PTT measurement to estimate the arterial blood pressure, by taking into account the contribution of red cell orientation effects and the artery diameter and stiffness change during long-term monitoring, is a very important task and this paper completely covers and answers all of these lacking questions.
Author Contributions
Conceptualization, M.A.-h.; methodology, M.A.-h.; software, D.K. and M.Y.; validation, M.A.-h., D.K., S.S., and M.Y.; formal analysis, D.K. and M.Y.; investigation, M.A.-h.; resources, M.A.-h., and S.S.; data curation, M.A.-h.; writing—original draft preparation, M.A.-h., D.K., and M.Y.; writing—review and editing, M.A.-h. and S.S.; visualization, D.K. and M.Y.; supervision, S.S.; project administration, M.A.-h. and S.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This research was approved by the medical center of Bauman Moscow State technical University and approved by the University of Bauman Institutional Review Board.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Zakrzewski, A.M.; Anthony, B.W. Noninvasive Blood Pressure Estimation Using Ultrasound and Simple Finite Element Models. IEEE Trans. Biomed. Eng. 2018, 65, 2011–2022. [Google Scholar] [CrossRef]
- Seo, J.; Pietrangelo, S.J.; Lee, H.-S.; Sodini, C.G. Noninvasive arterial blood pressure waveform monitoring using two- element ultrasound system. IEEE Trans. Ultrason. Ferroelectr. Freq. Control 2015, 62, 776–784. [Google Scholar] [CrossRef]
- Oliver, J.J.; Webb, D.J. Noninvasive assessment of arterial stiffness and risk of atherosclerotic events. Arterioscler. Thromb. Vasc. Biol. 2003, 23, 554–566. [Google Scholar] [CrossRef] [Green Version]
- Hirai, T.; Sasayama, S.; Kawasaki, T.; Yagi, S. Stiffness of systemic arteries in patients with myocardial infarction. A noninvasive method to predict severity of coronary atherosclerosis. Circulation 1989, 80, 78–86. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Seo, J.; Lee, H.-S.; Sodini, C. Non-Invasive Evaluation of a Carotid Arterial Pressure Waveform Using Motion-Tolerant Ultrasound Measurements During the Valsalva Maneuver. IEEE J. Biomed. Health Inform. 2021, 25, 163–174. [Google Scholar] [CrossRef]
- Nabeel, P.M.; Joseph, J.; Karthik, S.; Sivaprakasam, M.; Chenniappan, M. Bi-Modal Arterial Compliance Probe for Calibration-Free Cuffless Blood Pressure Estimation. IEEE Trans. Biomed. Eng. 2018, 65, 2392–2404. [Google Scholar] [CrossRef]
- Mukherjee, R.; Ghosh, S.; Gupta, B.; Chakravarty, T. A Literature Review on Current and Proposed Technologies of Noninvasive Blood Pressure Measurement. Telemed. J. E-Health Off. J. Am. Telemed. Assoc. 2018, 24, 185–193. [Google Scholar] [CrossRef]
- Nitzan, M.; Adar, Y.; Hoffman, E.; Shalom, E.; Engelberg, S.; Ben-Dov, I.Z.; Bursztyn, M. Comparison of systolic blood pressure values obtained by photoplethysmography and by Korotkoff sounds. Sensors 2013, 13, 14797–14812. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pickering, T.; Appel, L.; Falkner, B.; Jones, D.; Kurtz, T.; Sheps, S.; Roccella, E. Recommendations for Blood Pressure Measurement in Humans and Experimental Animals. Hypertension 2005, 45, 142–161. [Google Scholar] [CrossRef] [PubMed]
- Chung, E.; Chen, G.; Alexander, B.; Cannesson, M. Non-invasive continuous blood pressure monitoring: A review of current applications. Front. Med. 2013, 7, 91–101. [Google Scholar] [CrossRef]
- Forouzanfar, M.; Dajani, H.R.; Groza, V.Z.; Bolic, M.; Rajan, S.; Batkin, I. Oscillometric blood pressure estimation: Past, present, and future. IEEE Rev. Biomed. Eng. 2015, 8, 44–63. [Google Scholar] [CrossRef]
- Gemignani, V.; Faita, F.; Ghiadoni, L.; Poggianti, E.; Demi, M. A system for real-time measurement of the brachial artery diameter in B-mode ultrasound images. IEEE Trans. Med. Imaging 2007, 26, 393–404. [Google Scholar] [CrossRef] [PubMed]
- Cary, T.W.; Reamer, C.B.; Sultan, L.R.; Mohler III, E.R.; Sehgal, C.M. Brachial artery vasomotion and transducer pressure effect on measurements by active contour segmentation on ultrasound. Med. Phys. 2014, 41, 022901. [Google Scholar] [CrossRef] [Green Version]
- Wang, C.; Li, X.; Hu, H.; Zhang, L.; Huang, Z.; Lin, M.; Zhang, Z.; Yin, Z.; Huang, B.; Gong, H. Monitoring of the central blood pressure waveform via a conformal ultrasonic device. Nat. Biomed. Eng. 2018, 2, 687–695. [Google Scholar] [CrossRef]
- Xing, X.; Sun, M. Optical blood pressure estimation with photoplethysmography and FFT-based neural networks. Biomed. Opt. Express 2016, 7, 3007–3020. [Google Scholar] [CrossRef] [Green Version]
- Terry, S.; Eckerle, J.; Kornbluh, R.; Low, T.; Ablow, C. Silicon pressure transducer arrays for blood-pressure measurement. Sens. Actuators Phys. 1990, 23, 1070–1079. [Google Scholar] [CrossRef]
- Mukkamala, R.; Hahn, J.-O.; Inan, O.T.; Mestha, L.K.; Kim, C.-S.; Töreyin, H.; Kyal, S. Toward Ubiquitous Blood Pressure Monitoring via Pulse Transit Time: Theory and Practice. IEEE Trans. Biomed. Eng. 2015, 62, 1879–1901. [Google Scholar] [CrossRef] [Green Version]
- Chio, S.-S.; Urbina, E.M.; Lapointe, J.; Tsai, J.; Berenson, G.S. Korotkoff sound versus oscillometric cuff sphygmomanometers: Comparison between auscultatory and DynaPulse blood pressure measurements. J. Am. Soc. Hypertens. JASH 2011, 5, 12–20. [Google Scholar] [CrossRef] [PubMed]
- Babbs, C.F. The origin of Korotkoff sounds and the accuracy of auscultatory blood pressure measurements. J. Am. Soc. Hypertens. JASH 2015, 9, 935–950.e3. [Google Scholar] [CrossRef] [Green Version]
- John, O.; Campbell, N.R.C.; Brady, T.M.; Farrell, M.; Varghese, C.; Velazquez Berumen, A.; Velez Ruiz Gaitan, L.A.; Toffelmire, N.; Ameel, M.; Mideksa, M.; et al. The 2020 “WHO Technical Specifications for Automated Non-Invasive Blood Pressure Measuring Devices With Cuff”. Hypertens. Dallas Tex 1979 2021, 77, 806–812. [Google Scholar] [CrossRef] [PubMed]
- Daochai, S.; Sroykham, W.; Kajornpredanon, Y.; Apaiwongse, C. Non-invasive blood pressure measurement: Auscultatory method versus oscillometric method. In Proceedings of the 4th 2011 Biomedical Engineering International Conference, Chiang Mai, Thailand, 29–31 January 2012. [Google Scholar] [CrossRef]
- Kapse, C.D.; Patil, B.R. Auscultatory and Oscillometric methods of Blood pressure measurement: A Survey. Int. J. Eng. Res. Appl. 2013, 3, 528–533. [Google Scholar]
- Bonnafoux, P. Auscultatory and oscillometric methods of ambulatory blood pressure monitoring, advantages and limits: A technical point of view. Blood Press. Monit. 1996, 1, 181–185. [Google Scholar] [PubMed]
- Lamb, T.S.; Thakrar, A.; Ghosh, M.; Wilson, M.P.; Wilson, T.W. Comparison of two oscillometric blood pressure monitors in subjects with atrial fibrillation. Clin. Investig. Med. Med. Clin. Exp. 2010, 33, E54–E62. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Benmira, A.; Perez-Martin, A.; Schuster, I.; Aichoun, I.; Coudray, S.; Bereksi-Reguig, F.; Dauzat, M. From Korotkoff and Marey to automatic non-invasive oscillometric blood pressure measurement: Does easiness come with reliability? Expert Rev. Med. Devices 2016, 13, 179–189. [Google Scholar] [CrossRef] [PubMed]
- Babbs, C.F. Oscillometric measurement of systolic and diastolic blood pressures validated in a physiologic mathematical model. Biomed. Eng. Online 2012, 11, 56. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sahu, D.; Bhaskaran, M. Palpatory method of measuring diastolic blood pressure. J. Anaesthesiol. Clin. Pharmacol. 2010, 26, 528–530. [Google Scholar]
- Penaz, J. Photoelectric measurement of blood pressure, volume and flow in the finger. In Proceedings of the Digest of the 10th International Conference on Medical and Biological Engineering, Dresden, Germany; 1973. [Google Scholar]
- Antsiperov, V.; Mansurov, G.; Danilychev, M.; Churikov, D. Non-Invasive Blood Pressure Monitoring with Positionable Three-chamber Pneumatic Sensor. In Proceedings of the 12th International Joint Conference on Biomedical Engineering Systems and Technologies (HEALTHINF), Prague, Czech Republic, 22–24 February 2019; pp. 462–465. [Google Scholar]
- Sensor Technology to Realize Continuous Blood Pressure Monitoring|OMRON TECHNICS|Technology|OMRON Global. Available online: https://www.omron.com/global/en/technology/omrontechnics/vol50/004.html (accessed on 28 November 2021).
- Hansen, S.; Staber, M. Oscillometric blood pressure measurement used for calibration of the arterial tonometry method contributes significantly to error. Eur. J. Anaesthesiol. 2006, 23, 781–787. [Google Scholar] [CrossRef]
- Beulen, B.W.A.M.M.; Bijnens, N.; Koutsouridis, G.G.; Brands, P.J.; Rutten, M.C.M.; van de Vosse, F.N. Toward noninvasive blood pressure assessment in arteries by using ultrasound. Ultrasound Med. Biol. 2011, 37, 788–797. [Google Scholar] [CrossRef]
- Reddy, A.K.; Taffet, G.E.; Madala, S.; Michael, L.H.; Entman, M.L.; Hartley, C.J. Noninvasive blood pressure measurement in mice using pulsed Doppler ultrasound. Ultrasound Med. Biol. 2003, 29, 379–385. [Google Scholar] [CrossRef]
- Ma, Y.; Choi, J.; Hourlier-Fargette, A.; Xue, Y.; Chung, H.U.; Lee, J.Y.; Wang, X.; Xie, Z.; Kang, D.; Wang, H.; et al. Relation between blood pressure and pulse wave velocity for human arteries. Proc. Natl. Acad. Sci. USA 2018, 115, 11144–11149. [Google Scholar] [CrossRef] [Green Version]
- Vappou, J.; Luo, J.; Okajima, K.; Di Tullio, M.; Konofagou, E.E. Non-invasive measurement of local pulse pressure by pulse wave-based ultrasound manometry (PWUM). Physiol. Meas. 2011, 32, 1653–1662. [Google Scholar] [CrossRef]
- Laurent, S.; Cockcroft, J.; Van Bortel, L.; Boutouyrie, P.; Giannattasio, C.; Hayoz, D.; Pannier, B.; Vlachopoulos, C.; Wilkinson, I.; Struijker-Boudier, H.; et al. Expert consensus document on arterial stiffness: Methodological issues and clinical applications. Eur. Heart J. 2006, 27, 2588–2605. [Google Scholar] [CrossRef] [Green Version]
- Khamdaeng, T.; Luo, J.; Vappou, J.; Terdtoon, P.; Konofagou, E. Arterial stiffness identification of the human carotid artery using the stress–strain relationship in vivo. Ultrasonics 2012, 52, 402–411. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Visser, K. Electric conductivity of stationary and flowing human blood at low frequencies. Med. Biol. Eng. Comput. 2006. [Google Scholar] [CrossRef]
- Gaw, R.L. The Effect of Red Blood Cell Orientation on the Electrical Impedance of Pulsatile Blood with Implications for Impedance Cardiography. Ph.D. Thesis, Queensland University of Technology, Brisbane, QLD, Australia, 2010. [Google Scholar]
- Al-Harosh, M.; Shchukin, S. Numerical Modeling of the Electrical Impedance Method of Peripheral Veins Localization; Springer: Berlin/Heidelberg, Germany, 2015; pp. 1683–1686. [Google Scholar]
- Ogedegbe, G.; Pickering, T. Principles and techniques of blood pressure measurement. Cardiol. Clin. 2010, 28, 571–586. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Teschner, E.; Imhoff, M.; Leonhardt, S. Electrical Impedance Tomography: The Realization of Regional Ventilation Monitoring; Dräger Medical GmbH: Lübeck, Germany, 2011. [Google Scholar]
- Tissue Frequency Chart » IT’IS Foundation. Available online: https://itis.swiss/virtual-population/tissue-properties/database/tissue-frequency-chart/ (accessed on 7 December 2021).
- Laplace’s Equation in Cylindrical Coordinates. Available online: https://farside.ph.utexas.edu/teaching/jk1/Electromagnetism/node36.html (accessed on 31 October 2021).
- 20.2 Blood Flow, Blood Pressure, and Resistance–Anatomy & Physiology. Available online: https://open.oregonstate.education/aandp/chapter/20-2-blood-flow-blood-pressure-and-resistance/ (accessed on 31 October 2021).
- Visser, K. Electric properties of flowing blood and impedance cardiography. Ann. Biomed. Eng. 2006, 17, 463–473. [Google Scholar] [CrossRef] [PubMed]
- Fujii, M.; Nakajima, K.; Sakamoto, K.; Kanai, H. Orientation and Deformation of Erythrocytes in Flowing Blood. Ann. N. Y. Acad. Sci. 1999. [Google Scholar] [CrossRef] [PubMed]
- Hill, D.W.; Thompson, F.D. The effect of haematocrit on the resistivity of human blood at 37 degrees C and 100 kHz. Med. Biol. Eng. 1975, 13, 182–186. [Google Scholar] [CrossRef]
- Nagaoka, R.; Ishikawa, K.; Mozumi, M.; Cinthio, M.; Hasegawa, H. Basic study on estimation method of wall shear stress in common carotid artery using blood flow imaging. Jpn. J. Appl. Phys. 2020, 59, SKKE16. [Google Scholar] [CrossRef]
- Cloutier, G.; Qin, Z.; Durand, L.G.; Teh, B.G. Power Doppler ultrasound evaluation of the shear rate and shear stress dependences of red blood cell aggregation. IEEE Trans. Biomed. Eng. 1996, 43, 441–450. [Google Scholar] [CrossRef]
- Hoskins, P. Estimation of blood velocity, volumetric flow and wall shear rate using Doppler ultrasound. Ultrasound 2011, 19, 120–129. [Google Scholar] [CrossRef]
- Caro, C.G.; Schroter, R.C.; Pedley, T.J.; Seed, W.A. (Eds.) Solid mechanics and the properties of blood vessel walls. In The Mechanics of the Circulation; Cambridge University Press: Cambridge, UK, 2011; pp. 86–104. ISBN 978-0-521-15177-1. [Google Scholar]
- Elastic Properties of Blood Vessels-Arteries and Veins-The Cardiovascular System-Medical Physiology, 3rd Edition. Available online: https://doctorlib.info/physiology/medical/104.html (accessed on 31 October 2021).
- Callaghan, F.J.; Geddes, L.A.; Babbs, C.F.; Bourland, J.D. Relationship between pulse-wave velocity and arterial elasticity. Med. Biol. Eng. Comput. 1986, 24, 248–254. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Al Talalwah, W.; Regassa, D.; Soames, R. Morphological feature of brachial artery and its clinical significance. J. Morphol. Sci. 2015, 32, 129–134. [Google Scholar] [CrossRef]
- Mugeb, A.; Ivan, K.; Volkov, A. The brachial artery localization for blood pressure monitoring using electrical impedance measurement. In Proceedings of the IEEE 2018 Ural Symposium on Biomedical Engineering, Radioelectronics and Information Technology (USBEREIT), Yekaterinburg, Russia, 7–8 May 2018; pp. 79–82. [Google Scholar]
- Hammoud, A.; Tikhomirov, A.; Shaheen, Z. Automatic Bio-impedance Signal Analysis: Smoothing Processes Efficacy Evaluation in Determining the Vascular Tone Type. In Proceedings of the 2021 Ural Symposium on Biomedical Engineering, Radioelectronics and Information Technology (USBEREIT), Yekaterinburg, Russia, 13–14 May 2021; pp. 0113–0116. [Google Scholar]
- Huynh, T.H.; Jafari, R.; Chung, W.-Y. An Accurate Bioimpedance Measurement System for Blood Pressure Monitoring. Sensors 2018, 18, 2095. [Google Scholar] [CrossRef] [Green Version]
- Sorace, A.G.; Robbin, M.L.; Umphrey, H.; Abts, C.A.; Berry, J.L.; Lockhart, M.E.; Allon, M.; Hoyt, K. Ultrasound Measurement of Brachial Artery Elasticity Before Hemodialysis Access Placement. J. Ultrasound Med. Off. J. Am. Inst. Ultrasound Med. 2012, 31, 1581–1588. [Google Scholar]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).