Measuring Gait Stability in People with Multiple Sclerosis Using Different Sensor Locations and Time Scales
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
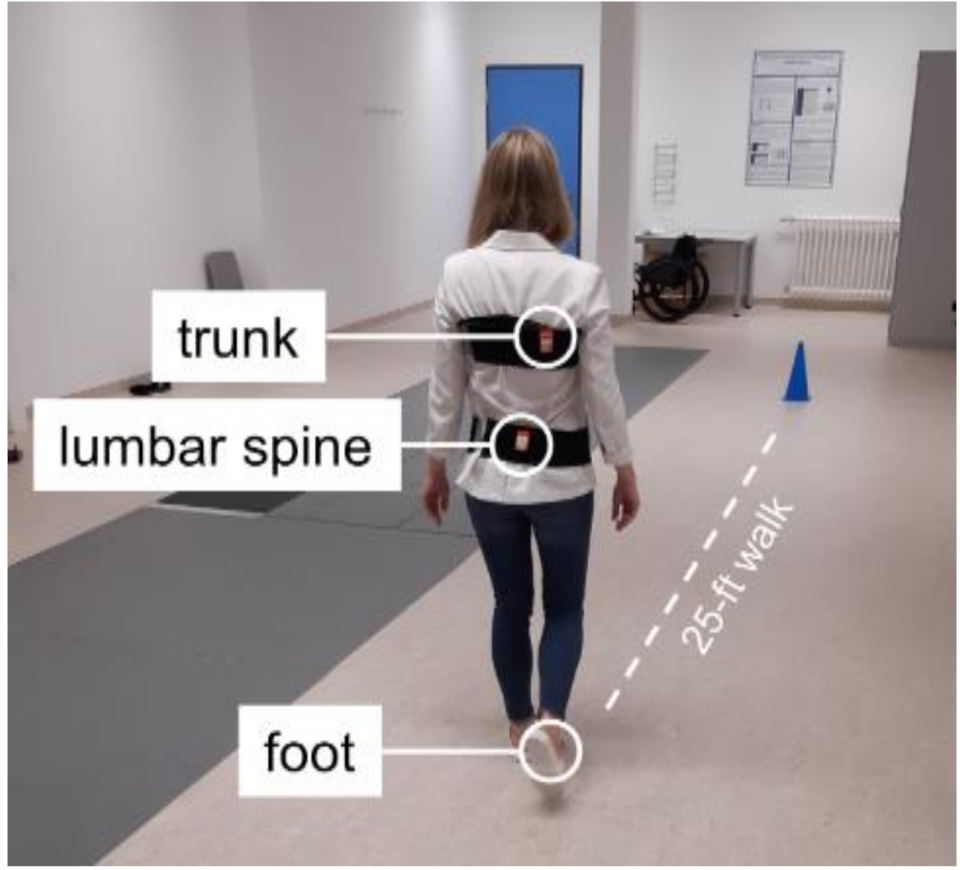
2.2. Procedure
2.3. Data Processing
2.4. Statistical Analysis
3. Results
3.1. PwMS vs. Healthy Comparison Group
3.2. PwMS with a Varying Level of Disability
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Allali, G.; Laidet, M.; Herrmann, F.R.; Armand, S.; Elsworth-Edelsten, C.; Assal, F.; Lalive, P.H. Gait variability in multiple sclerosis: A better falls predictor than EDSS in patients with low disability. J. Neural Transm. 2016, 123, 447–450. [Google Scholar] [CrossRef]
- Huisinga, J.M.; Mancini, M.; George, R.J.S.; Horak, F.B. Accelerometry reveals differences in gait variability between patients with multiple sclerosis and healthy controls. Ann. Biomed. Eng. 2013, 41, 1670–1679. [Google Scholar] [CrossRef]
- Moon, Y.; Wajda, D.A.; Motl, R.W.; Sosnoff, J.J. Stride-Time Variability and Fall Risk in Persons with Multiple Sclerosis. Mult. Scler. Int. 2015, 2015, 964790. [Google Scholar] [CrossRef] [PubMed]
- Peebles, A.T.; Reinholdt, A.; Bruetsch, A.P.; Lynch, S.G.; Huisinga, J.M. Dynamic margin of stability during gait is altered in persons with multiple sclerosis. J. Biomech. 2016, 49, 3949–3955. [Google Scholar] [CrossRef]
- Hilfiker, R.; Vaney, C.; Gattlen, B.; Meichtry, A.; Deriaz, O.; Lugon-Moulin, V.; Anchisi-Bellwald, A.-M.; Palaci, C.; Foinant, D.; Terrier, P. Local dynamic stability as a responsive index for the evaluation of rehabilitation effect on fall risk in patients with multiple sclerosis: A longitudinal study. BMC Res. Notes 2013, 6, 260. [Google Scholar] [CrossRef]
- Lizama, L.E.C.; Bruijn, S.M.; Galea, M.P. Gait stability at early stages of multiple sclerosis using different data sources. Gait Posture 2020, 77, 214–217. [Google Scholar] [CrossRef] [PubMed]
- Reynard, F.; Vuadens, P.; Deriaz, O.; Terrier, P. Could Local Dynamic Stability Serve as an Early Predictor of Falls in Patients with Moderate Neurological Gait Disorders? A Reliability and Comparison Study in Healthy Individuals and in Patients with Paresis of the Lower Extremities. PLoS ONE 2014, 9, e100550. [Google Scholar] [CrossRef] [PubMed]
- Tajali, S.; Mehravar, M.; Negahban, H.; van Dieën, J.H.; Shaterzadeh-Yazdi, M.J.; Mofateh, R. Impaired local dynamic stability during treadmill walking predicts future falls in patients with multiple sclerosis: A prospective cohort study. Clin. Biomech. 2019, 67, 197–201. [Google Scholar] [CrossRef]
- Dingwell, J.B.; Cusumano, J.P.; Cavanagh, P.R.; Sternad, D. Local dynamic stability versus kinematic variability of continuous overground and treadmill walking. J. Biomech. Eng. 2001, 123, 27–32. [Google Scholar] [CrossRef] [PubMed]
- Peebles, A.T.; Bruetsch, A.P.; Lynch, S.G.; Huisinga, J.M. Dynamic Balance Is Related to Physiological Impairments in Persons with Multiple Sclerosis. Arch. Phys. Med. Rehabil. 2018, 99, 2030–2037. [Google Scholar] [CrossRef] [PubMed]
- Bruijn, S.M.; Meijer, O.G.; Beek, P.J.; Van Dieen, J.H. Assessing the stability of human locomotion: A review of current measures. J. R. Soc. Interface 2013, 10, 20120999. [Google Scholar] [CrossRef] [PubMed]
- Mehdizadeh, S. The largest Lyapunov exponent of gait in young and elderly individuals: A systematic review. Gait Posture 2018, 60, 241–250. [Google Scholar] [CrossRef]
- Hamacher, D.; Singh, N.B.; Taylor, W.R.; Schega, L. Towards the assessment of local dynamic stability of level-grounded walking in an older population. Med. Eng. Phys. 2015, 37, 1152–1155. [Google Scholar] [CrossRef] [PubMed]
- Kurtzke, J.F. Rating neurologic impairment in multiple sclerosis: An expanded disability status scale (EDSS). Neurology 1983, 33, 1444–1452. [Google Scholar] [CrossRef] [PubMed]
- Burschka, J.M.; Keune, P.M.; Menge, U.; Hofstadt-van Oy, U.; Oschmann, P.; Hoos, O. An exploration of impaired walking dynamics and fatigue in Multiple Sclerosis. BMC Neurol. 2012, 12, 161. [Google Scholar] [CrossRef] [PubMed]
- Goldman, M.D.; Marrie, R.; Cohen, J.A. Evaluation of the six-minute walk in multiple sclerosis subjects and healthy controls. Mult. Scler. J. 2008, 14, 383–390. [Google Scholar] [CrossRef] [PubMed]
- Leone, C.; Severijns, D.; Doležalová, V.; Baert, I.; Dalgas, U.; Romberg, A.; Bethoux, F.; Gebara, B.; Medina, C.S.; Rasova, K.; et al. Prevalence of walking-related motor fatigue in persons with multiple sclerosis: Decline in walking distance induced by the 6-minute walk test. Neurorehabilit. Neural Repair 2016, 30, 373–383. [Google Scholar] [CrossRef]
- Arpan, I.; Fino, P.C.; Fling, B.W.; Horak, F. Local dynamic stability during long-fatiguing walks in people with multiple sclerosis. Gait Posture 2020, 76, 122–127. [Google Scholar] [CrossRef]
- Sauder, T.; Keune, P.M.; Müller, R.; Schenk, T.; Oschmann, P.; Hansen, S. Trait mindfulness is primarily associated with depression and not with fatigue in multiple sclerosis (MS): Implications for mindfulness-based interventions. BMC Neurol. 2021, 21, 1–7. [Google Scholar] [CrossRef]
- McDonald, W.I.; Compston, A.; Edan, G.; Goodkin, D.; Hartung, H.P.; Lublin, F.D.; McFarland, H.F.; Paty, D.W.; Polman, C.H.; Sandberg-Wollheim, M.; et al. Recommended diagnostic criteria for multiple sclerosis: Guidelines from the International Panel on the diagnosis of multiple sclerosis. Ann. Neurol. Off. J. Am. Neurol. Assoc. Child Neurol. Soc. 2001, 50, 121–127. [Google Scholar] [CrossRef] [PubMed]
- Keune, P.M.; Cocks, A.J.; Young, W.R.; Burschka, J.M.; Hansen, S.; Hofstadt-van Oy, U.; Oschmann, P.; Muenssinger, J. Dynamic walking features and improved walking performance in multiple sclerosis patients treated with fampridine (4-aminopyridine). BMC Neurol. 2015, 15, 171. [Google Scholar] [CrossRef] [PubMed]
- Hamacher, D.; Hamacher, D.; Taylor, W.R.; Singh, N.B.; Schega, L. Towards clinical application: Repetitive sensor position re-calibration for improved reliability of gait parameters. Gait Posture 2014, 39, 1146–1148. [Google Scholar] [CrossRef]
- Hamacher, D.; Müller, R.; Schega, L.; Zech, A. Exploring phase dependent functional gait variability. Hum. Mov. Sci. 2017, 52, 191–196. [Google Scholar] [CrossRef]
- Bruijn, S.M.; van Dieën, J.H.; Meijer, O.G.; Beek, P.J. Statistical precision and sensitivity of measures of dynamic gait stability. J. Neurosci. Methods 2009, 178, 327–333. [Google Scholar] [CrossRef] [PubMed]
- Bisi, M.C.; Riva, F.; Stagni, R. Measures of gait stability: Performance on adults and toddlers at the beginning of independent walking. J. Neuroeng. Rehabil. 2014, 11, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Hamacher, D.; Liebl, D.; Hödl, C.; Heßler, V.; Kniewasser, C.K.; Thönnessen, T.; Zech, A. Gait Stability and Its Influencing Factors in Older Adults. Front. Physiol. 2019, 9, 1955. [Google Scholar] [CrossRef] [PubMed]
- Petersen, E.; Zech, A.; Hamacher, D. Walking barefoot vs. with minimalist footwear – influence on gait in younger and older adults. BMC Geriatr. 2020, 20, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Rosenstein, M.T.; Collins, J.J.; De Luca, C.J. A practical method for calculating largest Lyapunov exponents from small data sets. Phys. D Nonlinear Phenom. 1993, 65, 117–134. [Google Scholar] [CrossRef]
- Rogge, A.K.; Hamacher, D.; Cappagli, G.; Kuhne, L.; Hötting, K.; Zech, A.; Gori, M.; Röder, B. Balance, gait, and navigation performance are related to physical exercise in blind and visually impaired children and adolescents. Exp. Brain Res. 2021, 239, 1111–1123. [Google Scholar] [CrossRef]
- Hollander, K.; Petersen, E.; Zech, A.; Hamacher, D. Effects of barefoot vs. shod walking during indoor and outdoor conditions in younger and older adults. Gait Posture 2021. [Google Scholar] [CrossRef] [PubMed]
- Schroll, A. Der Maximale Lyapunov Exponent—Methodische Beiträge zur Theorie und Anwendung in der Sportwissenschaft. Ph.D. Thesis, Humboldt-Universität, Berlin, Germany, 2020. [Google Scholar]
- Müller, R.; Vielemeyer, J.; Häufle, D.F. Negotiating ground level perturbations in walking: Visual perception and expectation of curb height modulate muscle activity. J. Biomech. 2020, 113. [Google Scholar] [CrossRef]
- Müller, R.; Grimmer, S.; Blickhan, R. Running on uneven ground: Leg adjustments by muscle pre-activation control. Hum. Mov. Sci. 2010, 29, 299–310. [Google Scholar] [CrossRef]
- Haeufle, D.F.; Schmortte, B.; Geyer, H.; Müller, R.; Schmitt, S. The benefit of combining neuronal feedback and feed-forward control for robustness in step down perturbations of simulated human walking depends on the muscle function. Front. Comput. Neurosci. 2018, 12, 80. [Google Scholar] [CrossRef]
- Bruijn, S.M.; Meijer, O.G.; Beek, P.J.; van Dieën, J.H. The effects of arm swing on human gait stability. J. Exp. Biol. 2010, 213, 3945–3952. [Google Scholar] [CrossRef] [PubMed]
- Vielemeyer, J.; Grießbach, E.; Müller, R. Ground reaction forces intersect above the center of mass even when walking down visible and camouflaged curbs. J. Exp. Biol. 2019, 222, jeb.204305. [Google Scholar] [CrossRef] [PubMed]
- Müller, R.; Rode, C.; Aminiaghdam, S.; Vielemeyer, J.; Blickhan, R. Force direction patterns promote whole body stability even in hip-flexed walking, but not upper body stability in human upright walking. Proc. R. Soc. A Math. Phys. Eng. Sci. 2017, 473, 20170404. [Google Scholar] [CrossRef] [PubMed]
- Contreras-Reyes, J.E. Analyzing fish condition factor index through skew-gaussian information theory quantifiers. Fluct. Noise Lett. 2016, 15, 1650013. [Google Scholar] [CrossRef]
- Tarnopolski, M. Correlation between the Hurst exponent and the maximal Lyapunov exponent: Examining some low-dimensional conservative maps. Phys. A Stat. Mech. Appl. 2018, 490, 834–844. [Google Scholar] [CrossRef]
- Himann, J.E.; Cunningham, D.A.; Rechnitzer, P.A.; Paterson, D.H. Age-related changes in speed of walking. Med. Sci. Sports Exerc. 1988, 20, 161–166. [Google Scholar] [CrossRef] [PubMed]
- Terrier, P.; Reynard, F. Effect of age on the variability and stability of gait: A cross-sectional treadmill study in healthy indi-viduals between 20 and 69 years of age. Gait Posture 2015, 41, 170–174. [Google Scholar] [CrossRef] [PubMed]


| Healthy | PwMS | p-Value | |
|---|---|---|---|
| mean ± sd | mean ± sd | ||
| Age [years] | 34.7 ± 8.9 | 41.7 ± 11.4 | 0.003 |
| Height [cm] | 172.8 ± 8.5 | 170.9 ± 8.1 | 0.368 |
| Weight [kg] | 71.7 ± 11.9 | 79.2 ± 18.3 | 0.085 |
| Sex [f/m] | 21/9 | 62/24 | 0.827 |
| EDSS | 2.00 ± 1.10 | ||
| Walking speed [m/s] | |||
| begin | 1.68 ± 0.20 | 1.46 ± 0.23 | 0.000 |
| mid | 1.66 ± 0.19 | 1.42 ± 0.23 | 0.000 |
| end | 1.67 ± 0.17 | 1.42 ± 0.23 | 0.000 |
| Stride length [m] | |||
| begin | 1.60 ± 0.16 | 1.45 ± 0.17 | 0.000 |
| mid | 1.59 ± 0.16 | 1.44 ± 0.17 | 0.000 |
| end | 1.60 ± 0.15 | 1.44 ± 0.17 | 0.000 |
| Stride time [s] | |||
| begin | 0.96 ± 0.06 | 1.00 ± 0.08 | 0.005 |
| mid | 0.96 ± 0.06 | 1.02 ± 0.08 | 0.001 |
| end | 0.96 ± 0.06 | 1.02 ± 0.08 | 0.000 |
| N | 30 | 86 |
| Group | Model Estimates | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Healthy | PwMS | Intercept | Group | Time | Time2 | Group × Time | Group × Time2 | ||
| Trunk | begin | 0.92 ± 0.13 | 0.97 ± 0.16 | b = −0.27 β = 0.92 | b = 0.37 | b = 0.11 | b = −0.17 | b = 0.41 | b = 0.55 |
| (short) | mid | 0.92 ± 0.15 | 0.97 ± 0.17 | β = 0.06 | β = 0.02 | β = −0.03 | β = 0.07 | β = 0.09 | |
| end | 0.92 ± 0.17 | 0.99 ± 0.15 | p = 0.047 | p = 0.928 | p = 0.891 | p = 0.771 | p = 0.696 | ||
| Lumbar spine | begin | 1.01 ± 0.14 | 1.08 ± 0.19 | b = −0.22 β = 1.03 | b = 0.30 | b = 2.08 | b = −0.06 | b = −2.12 | b = 0.14 |
| (short) | mid | 1.03 ± 0.16 | 1.08 ± 0.18 | β = 0.05 | β = 0.36 | β = −0.01 | β = −0.37 | β = 0.02 | |
| end | 1.05 ± 0.17 | 1.08 ± 0.16 | p = 0.124 | p = 0.039 | p = 0.948 | p = 0.074 | p = 0.907 | ||
| Foot | begin | 2.21 ± 0.26 | 2.23 ± 0.28 | b = 0.04 β = 2.21 | b = −0.05 | b = 0.07 | b = −0.27 | b = −1.03 | b = 1.61 |
| (short) | mid | 2.22 ± 0.29 | 2.17 ± 0.26 | β = −0.01 | β = 0.02 | β = −0.07 | β = −0.28 | β = 0.43 | |
| end | 2.21 ± 0.31 | 2.20 ± 0.25 | p = 0.760 | p = 0.960 | p = 0.837 | p = 0.500 | p = 0.289 | ||
| Trunk | begin | 14.09 ± 1.65 | 14.34 ± 1.58 | b = −0.18 β = 13.98 | b = 0.24 | b = −0.73 | b = 0.30 | b = 1.41 | b = −0.40 |
| (very short) | mid | 13.93 ± 1.48 | 14.45 ± 2.01 | β = 0.45 | β = −1.39 | β = 0.58 | β = 2.68 | β = −0.77 | |
| end | 13.91 ± 1.71 | 14.51 ± 2.05 | p = 0.239 | p = 0.341 | p = 0.694 | p = 0.116 | p = 0.651 | ||
| Lumbar spine | begin | 12.24 ± 1.14 | 12.58 ± 1.31 | b = −0.27 β = 12.17 | b = 0.37 | b = 0.21 | b = 1.55 | b = 1.09 | b = −1.35 |
| (very short) | mid | 12.01 ± 1.40 | 12.67 ± 1.44 | β = 0.52 | β = 0.30 | β = 2.17 | β = 1.53 | β = −1.90 | |
| end | 12.28 ± 1.53 | 12.82 ± 1.38 | p = 0.066 | p = 0.798 | p = 0.066 | p = 0.268 | p = 0.171 | ||
| Foot | begin | 13.61 ± 1.10 | 14.44 ± 1.48 | b = −0.50 β = 13.72 | b = 0.68 | b = 0.84 | b = −0.39 | b = 1.68 | b = −0.13 |
| (very short) | mid | 13.76 ± 1.30 | 14.76 ± 1.37 | β = 0.99 | β = 1.22 | β = −0.57 | β = 2.45 | β = −0.19 | |
| end | 13.78 ± 1.06 | 14.92 ± 1.48 | p < 0.001 | p = 0.304 | p = 0.631 | p = 0.078 | p = 0.893 | ||
| Model Estimates | ||||||
|---|---|---|---|---|---|---|
| Intercept | EDSS | Time | Time2 | EDSS × Time | EDSS × Time2 | |
| Trunk | b = −0.42 | b = 0.21 | b = −0.38 | b = −0.84 | b = 0.41 | b = 0.59 |
| (short) | β = 0.91 | β = 0.03 | β = −0.06 | β = −0.14 | β = 0.07 | β = 0.09 |
| p = 0.012 | p = 0.772 | p = 0.518 | p = 0.471 | p = 0.306 | ||
| Lumbar spine | b = −0.46 | b = 0.23 | b = 0.25 | b = −0.87 | b = −0.14 | b = 0.46 |
| (short) | β = 1.00 | β = 0.04 | β = 0.04 | β = −0.15 | β = −0.02 | β = 0.08 |
| p = 0.014 | p = 0.825 | p = 0.440 | p = 0.776 | p = 0.346 | ||
| Foot | b = −0.22 | b = 0.11 | b = 0.54 | b = 2.25 | b = −0.70 | b = −0.53 |
| (short) | β = 2.14 | β = 0.03 | β = 0.15 | β = 0.59 | β = −0.18 | β = −0.14 |
| p = 0.210 | p = 0.645 | p = 0.065 | p = 0.188 | p = 0.318 | ||
| Trunk | b = −0.30 | b = 0.15 | b = −0.97 | b = −1.00 | b = 0.76 | b = 0.46 |
| (very short) | β = 13.83 | β = 0.30 | β = −1.92 | β = −1.99 | β = 1.51 | β = 0.91 |
| p = 0.110 | p = 0.184 | p = 0.169 | p = 0.018 | p = 0.150 | ||
| Lumbar spine | b = −0.26 | b = 0.13 | b = −1.22 | b = −1.72 | b = 1.17 | b = 0.93 |
| (very short) | β = 12.33 | β = 0.18 | β = −1.69 | β = −2.38 | β = 1.62 | β = 1.29 |
| p = 0.178 | p = 0.160 | p = 0.049 | p = 0.002 | p = 0.014 | ||
| Foot | b = −0.52 | b = 0.26 | b = 0.97 | b = −1.67 | b = 0.60 | b = 0.61 |
| (very short) | β = 13.95 | β = 0.38 | β = 1.41 | β = −2.43 | β = 0.87 | β = 0.89 |
| p = 0.004 | p = 0.271 | p = 0.059 | p = 0.120 | p = 0.114 | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Müller, R.; Schreff, L.; Koch, L.-E.; Oschmann, P.; Hamacher, D. Measuring Gait Stability in People with Multiple Sclerosis Using Different Sensor Locations and Time Scales. Sensors 2021, 21, 4001. https://doi.org/10.3390/s21124001
Müller R, Schreff L, Koch L-E, Oschmann P, Hamacher D. Measuring Gait Stability in People with Multiple Sclerosis Using Different Sensor Locations and Time Scales. Sensors. 2021; 21(12):4001. https://doi.org/10.3390/s21124001
Chicago/Turabian StyleMüller, Roy, Lucas Schreff, Lisa-Eyleen Koch, Patrick Oschmann, and Daniel Hamacher. 2021. "Measuring Gait Stability in People with Multiple Sclerosis Using Different Sensor Locations and Time Scales" Sensors 21, no. 12: 4001. https://doi.org/10.3390/s21124001
APA StyleMüller, R., Schreff, L., Koch, L.-E., Oschmann, P., & Hamacher, D. (2021). Measuring Gait Stability in People with Multiple Sclerosis Using Different Sensor Locations and Time Scales. Sensors, 21(12), 4001. https://doi.org/10.3390/s21124001






