Accuracy and Acceptability of Wearable Motion Tracking for Inpatient Monitoring Using Smartwatches
Abstract
1. Introduction
2. Materials and Methods
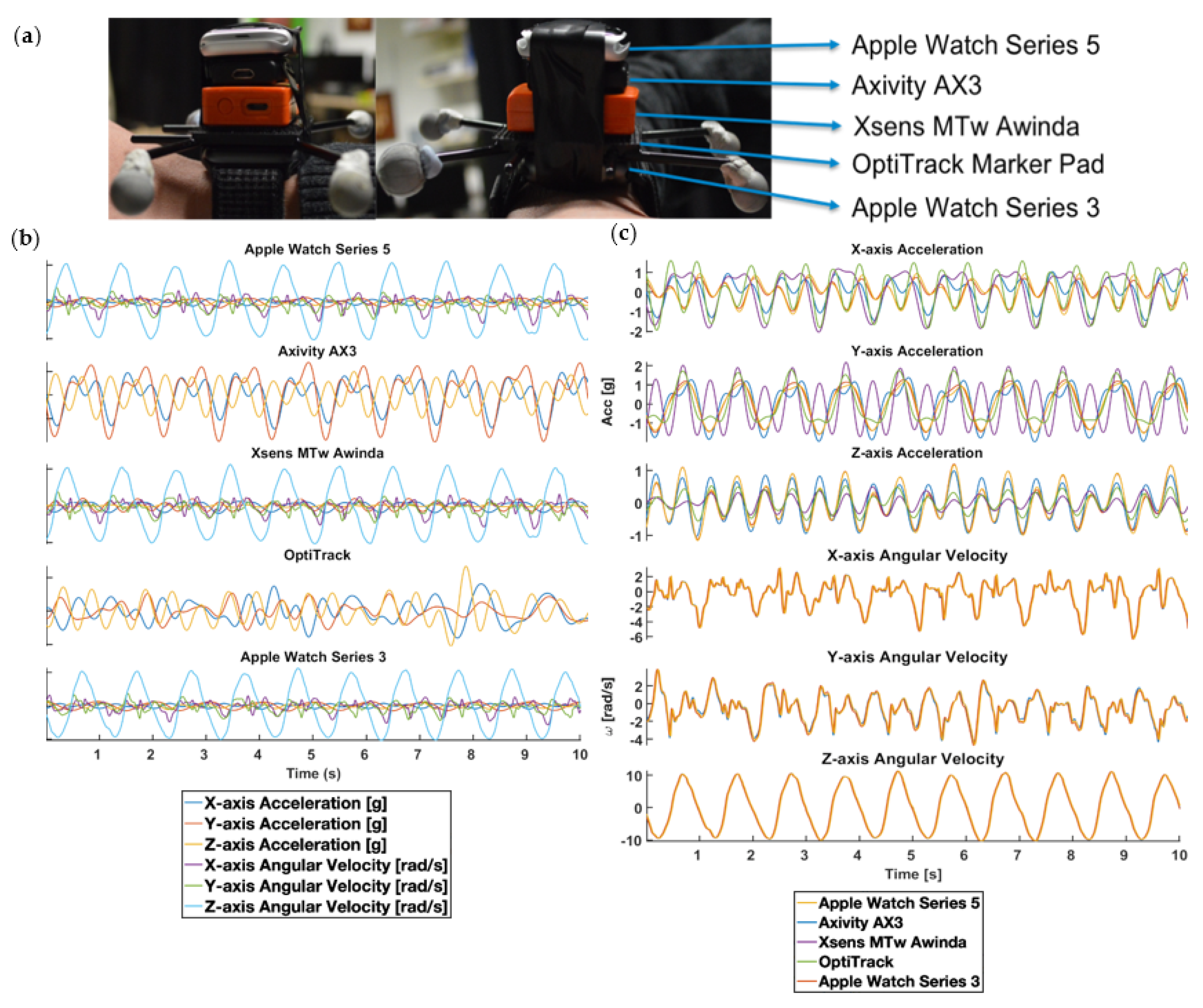
2.1. Material
2.2. Sensor Signal Quality Study
2.2.1. Population
2.2.2. Data Collection
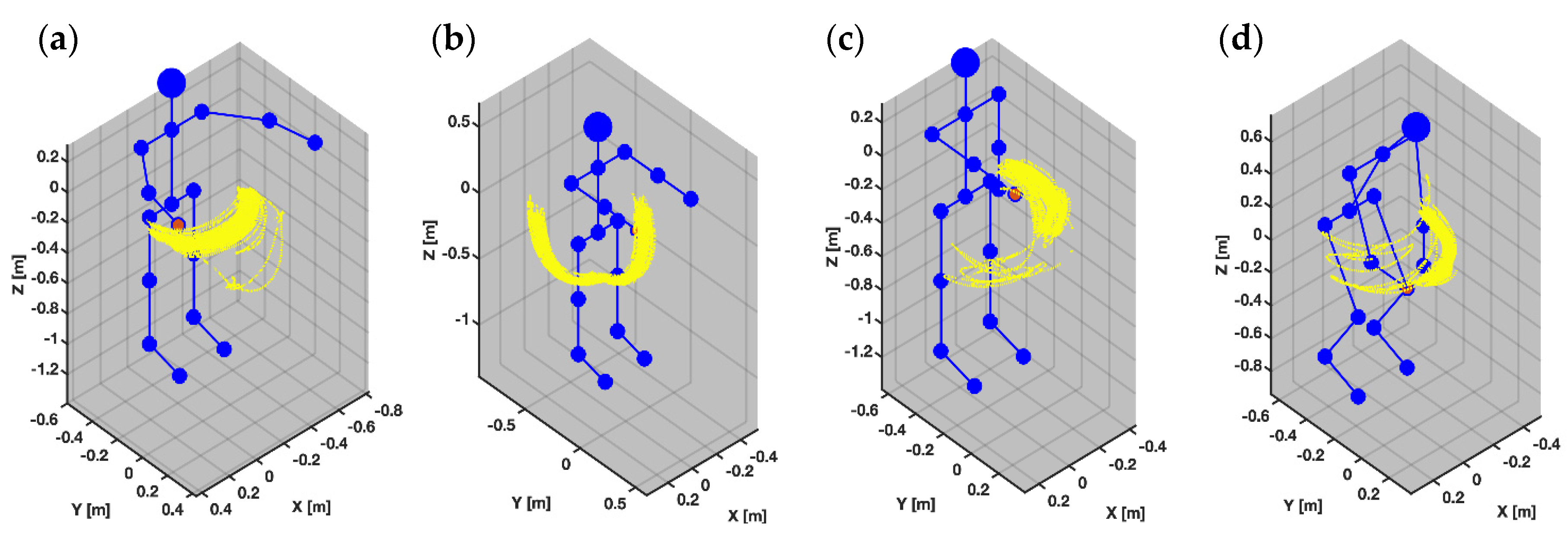
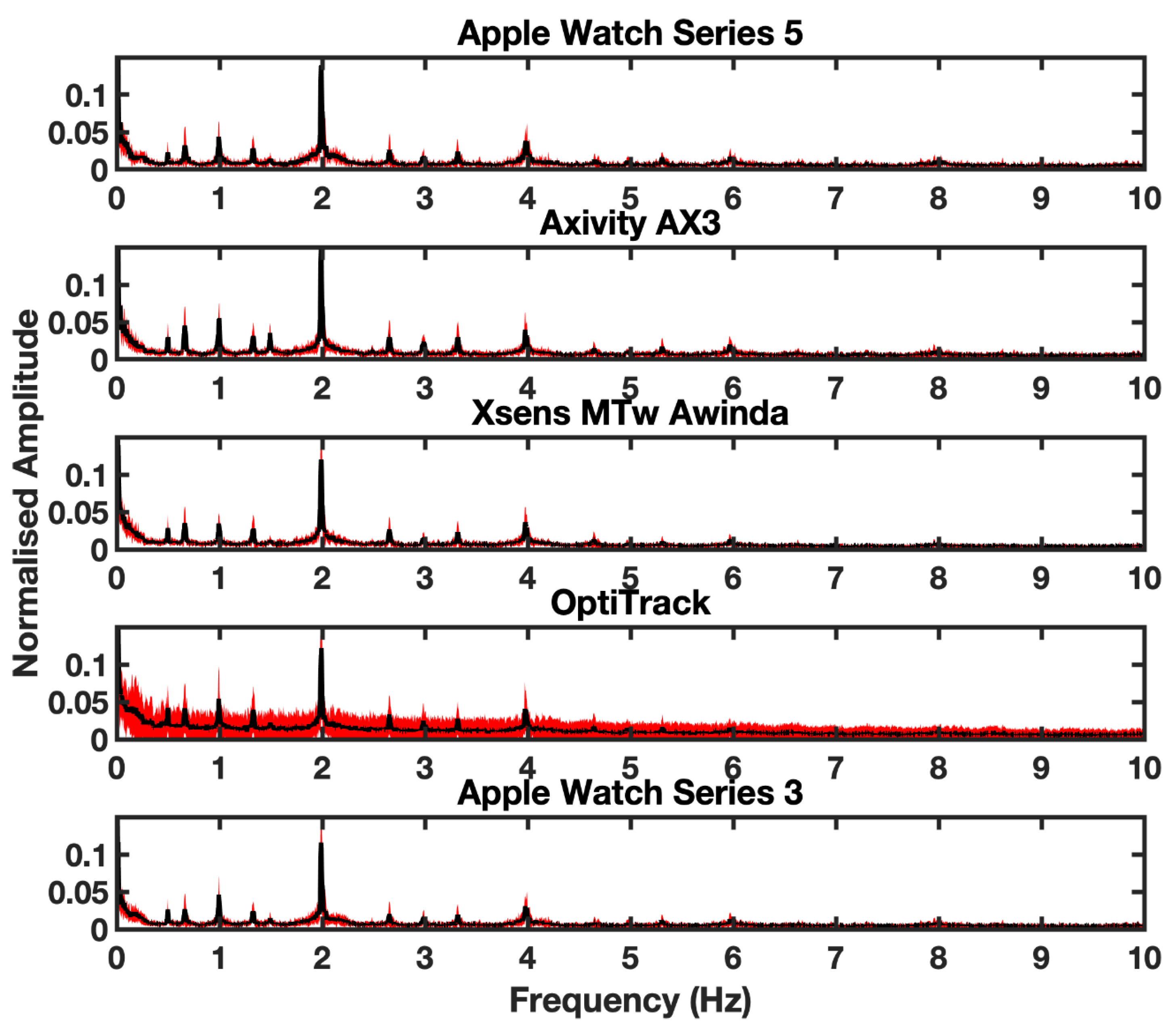
2.2.3. Data Processing
2.2.4. Analysis
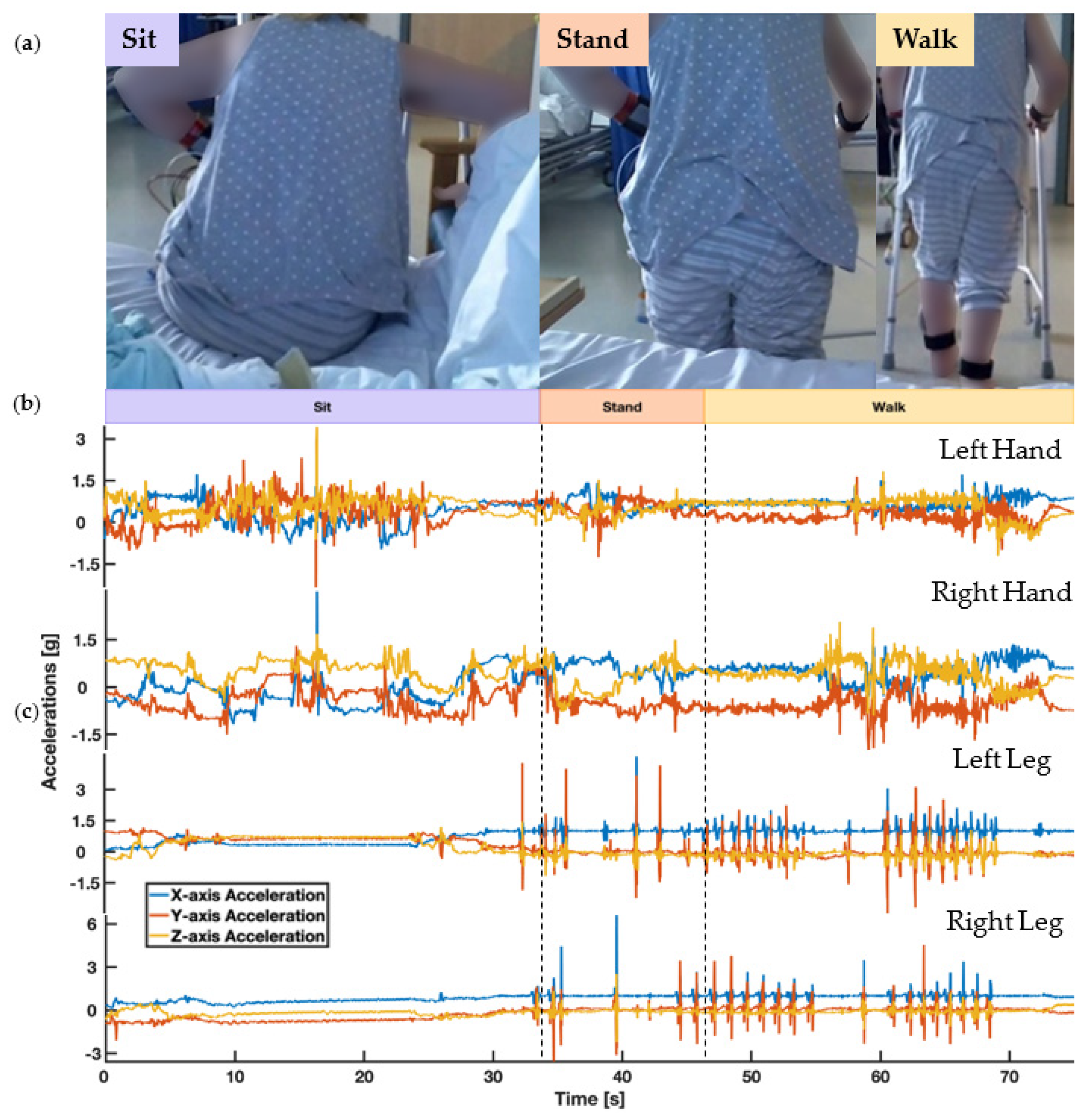
2.3. Sensor Acceptability Study
2.3.1. Population
2.3.2. Data Collection
- icQ1–10 used a 1 to 7 rating scale: 1 to 2 (strongly disagree); 3 to 4 (somewhat agree); and 5 to 7 (strongly agree).
- hcQ1–2 used a 1 to 7 rating scale: 1 to 2 (strongly disagree); 3 to 4 (somewhat agree); and 5 to 7 (strongly agree).
- hcQ3 used a 1 to 10 rating scale: 0 to 5 (no opportunity); and 6 to 10 (great opportunity).
- hcQ4 used a 1 to 10 rating scale: 0 to 5 (no danger/safe); and 6 to 10 (danger).
- hcQ5 was collected with a −3 to +3 rating scale: −3 (would not use the intervention); −2 to 0 (would only use the intervention if controlled by a human caregiver); and 1 to 3 (would use the intervention and it could replace some interventions currently implemented by human caregivers).
2.3.3. Analysis
3. Results
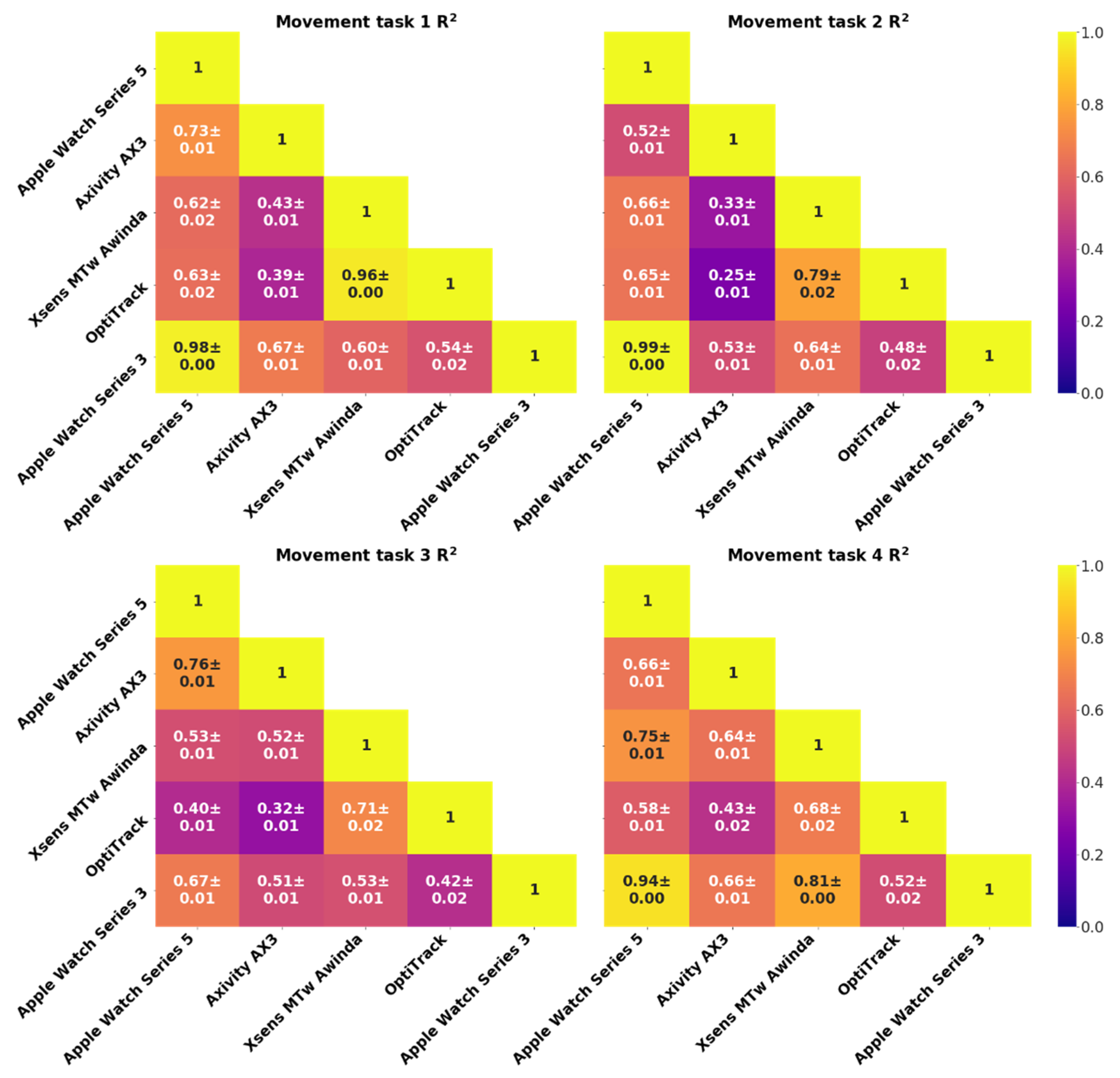
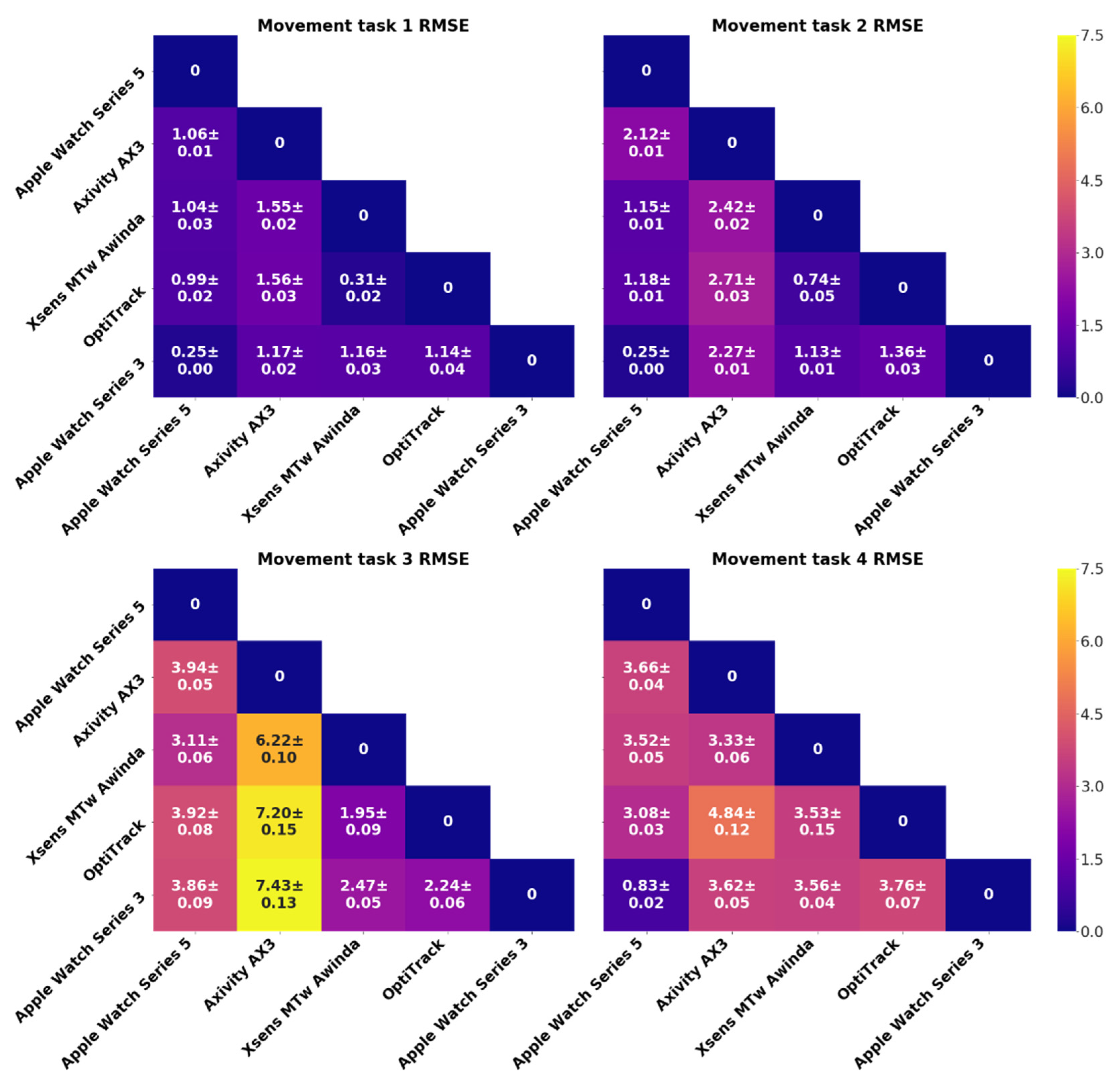
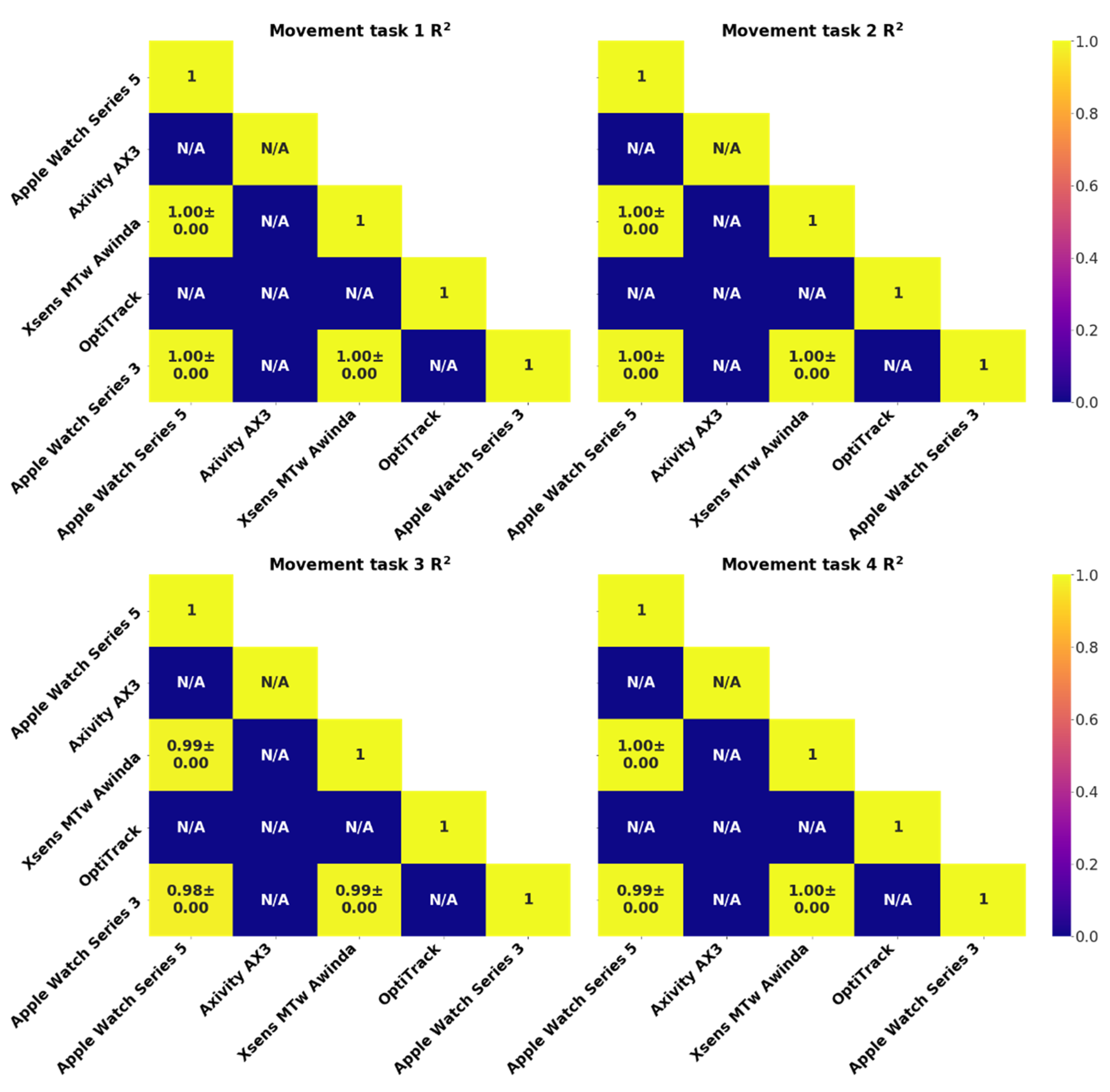
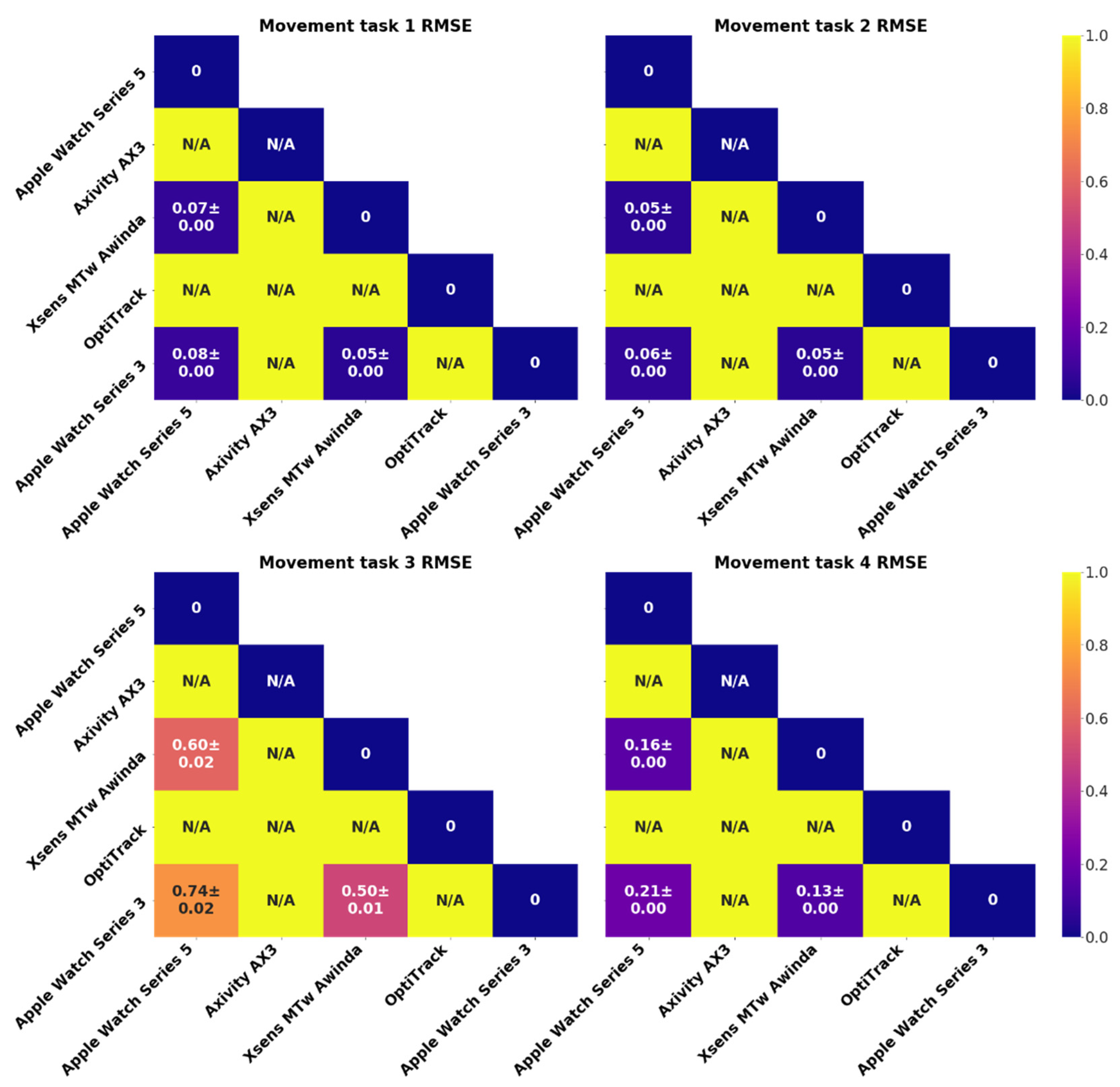
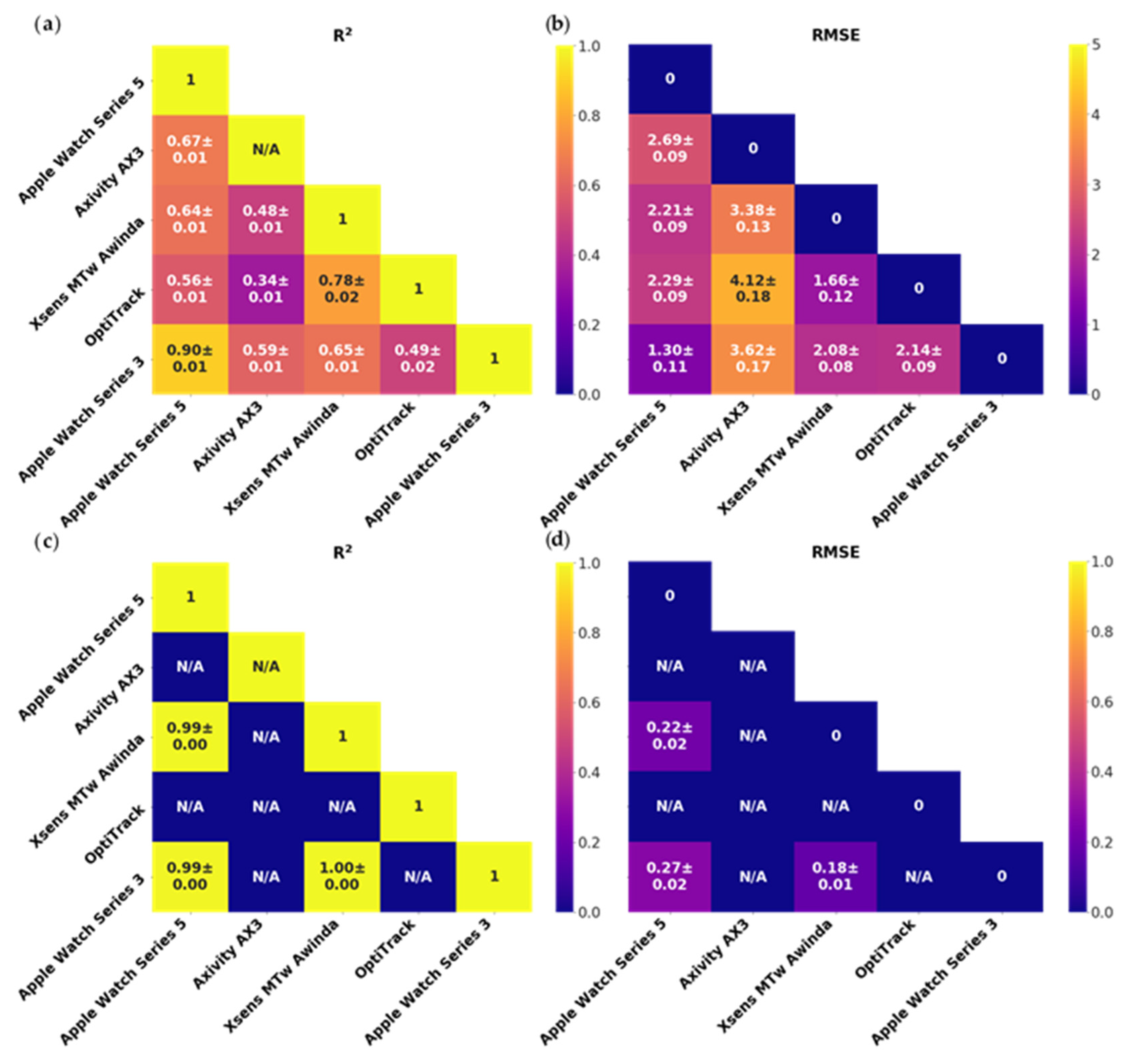
3.1. Sensor Signal Quality Study Results
3.2. Sensor Acceptability Study Results
4. Discussion
4.1. Sensor Signal Quality Study
4.2. Sensor Acceptability Study
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A
| Action | TPA 2 | BPA 1 | REPS 3 | TOT 4 |
|---|---|---|---|---|
| Handclap | ||||
| 0.5 | 1 | 5 | 2.5 |
| Horizontal Arm Movement (Both arms) | ||||
| 2 | 4 | 30 | 60 |
| Vertical Arm Movement (Both arms) | ||||
| 2 | 4 | 30 | 60 |
| 2 | 4 | 30 | 60 |
| Rotational Arm Movement | ||||
| 1 | 2 | 30 | 30 |
| 1 | 2 | 30 | 30 |
| 1 | 2 | 30 | 30 |
| Composite Cross-Body Movement | ||||
| 1 | 2 | 30 | 30 |
| Handclap | ||||
| 0.5 | 1 | 5 | 2.5 |
| Total time (Not including rest periods between each action) | 305 s | |||
| In-Patient Characteristics | n (Weights) |
|---|---|
| Age (years)—Avg (IQR) | 64 (24–92) |
| Female sex—n (%) | 22 (50) |
| Male sex—n (%) | 22 (50) |
| Asthma—n (%) | 4 (9) |
| Chronic obstructive pulmonary disease—n (%) | 3 (7) |
| Other respiratory diseases—n (%) | 2 (5) |
| Diabetes—n (%) | 4 (9) |
| Thyroid disorders—n (%) | 3 (7) |
| High blood pressure—n (%) | 29 (66) |
| Dyslipidemia—n (%) | 13 (30) |
| Other cardiac or vascular diseases—n (%) | 5 (11) |
| Chronic kidney diseases—n (%) | 2 (5) |
| Rheumatologic conditions—n (%) | 6 (13) |
| Digestive conditions—n (%) | 10 (23) |
| Neurological conditions—n (%) | 4 (9) |
| Cancer (including blood cancer)—n (%) | 2 (5) |
| Depression—n (%) | 2 (5) |
| Ischemic stroke—n (%) | 29 (66) |
| Hemorrhagic stroke—n (%) | 5 (11) |
| Transient Ischemic Attack—n (%) | 10 (23) |
| Stroke mimic (Stroke symptoms but non-stroke)—n (%) | 10 (23) |
| Characteristics | Doctor (n = 5) | Nurses (n = 4) | HCA (n = 3) | Therapist (n = 3) |
|---|---|---|---|---|
| Age (years)—Avg (IQR) | 28 (27–32) | 40 (31–58) | 48 (30–55) | 33 (28–45) |
| Female sex—n (%) | 2 (40%) | 2 (50%) | 3 (100%) | 3 (100%) |
| Male sex—n (%) | 3 (60%) | 2 (50%) | 0 (0%) | 0 (0%) |
| Educational level (%) | Medical degree (60%), MSc (40%) | Degree level (100%) | Degree level (33%), NVQ3 (33%), N/A (33%) | Degree (66%), N/A (33%) |
| Clinical speciality or training level | 1 Stroke SHO, 1 CT medicine, 1 Geriatrics ST3, 1 GPS 2, 1 SPR | Student Nurse (25%), B5 Nurse (75%) | HCA level 2 (33%), N/A (66%) | 1 Rehab assistant, 1 B5 Occupational therapist, 1 B6 Physiotherapist |
| Previous use of e-health or m-health technology | Yes (40%), No (60%) | Yes (25%), No (75%) | No (100%) | Yes (33%), No (66%) |
 is horizontal arm movements,
is horizontal arm movements,  is vertical arm movements,
is vertical arm movements,  is rotational arm movements, and
is rotational arm movements, and  is composite cross-body movements.
is composite cross-body movements.
 is horizontal arm movements,
is horizontal arm movements,  is vertical arm movements,
is vertical arm movements,  is rotational arm movements, and
is rotational arm movements, and  is composite cross-body movements.
is composite cross-body movements.
Appendix B. WatchOS Application and Server
References
- Salter, K.; Campbell, N.; Richardson, M.; Mehta, S.; Jutai, J.; Zettler, L.; Moses, M.B.A.; McClure, A.; Mays, R.; Foley, N.; et al. EBRSR [Evidence-Based Review of Stroke Rehabilitation] 20 Outcome Measures in Stroke Rehabilitation. Available online: http://www.ebrsr.com/evidence-review/20-outcome-measures-stroke-rehabilitationb (accessed on 22 June 2019).
- Johansson, D.; Malmgren, K.; Alt Murphy, M. Wearable sensors for clinical applications in epilepsy, Parkinson’s disease, and stroke: A mixed-methods systematic review. J. Neurol. 2018, 265, 1740–1752. [Google Scholar] [CrossRef]
- Kim, C.M.; Eng, J.J. Magnitude and pattern of 3D kinematic and kinetic gait profiles in persons with stroke: Relationship to walking speed. Gait Posture 2004, 20, 140–146. [Google Scholar] [CrossRef]
- Cuesta-Vargas, A.I.; Galan-Mercant, A.; Williams, J.M. The use of inertial sensors system for human motion analysis. Phys. Ther. Rev. 2010, 15, 462–473. [Google Scholar] [CrossRef] [PubMed]
- Kavanagh, J.J.; Menz, H.B. Accelerometry: A technique for quantifying movement patterns during walking. Gait Posture 2008, 28, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Patel, S.; Park, H.; Bonato, P.; Chan, L.; Rodgers, M. A review of wearable sensors and systems with application in rehabilitation. J. Neuroeng. Rehabil. 2012, 9, 21. [Google Scholar] [CrossRef] [PubMed]
- Maetzler, W.; Domingos, J.; Srulijes, K.; Ferreira, J.J.; Bloem, B.R. Quantitative wearable sensors for objective assessment of Parkinson’s disease. Mov. Disord. 2013, 28, 1628–1637. [Google Scholar] [CrossRef]
- Sim, N.; Gavriel, C.; Abbott, W.W.; Faisal, A.A. The head mouse—Head gaze estimation “In-the-Wild” with low-cost inertial sensors for BMI use. In Proceedings of the 2013 6th International IEEE/EMBS Conference on Neural Engineering (NER), San Diego, CA, USA, 6–8 November 2013; pp. 735–738. [Google Scholar]
- Gavriel, C.; Faisal, A.A. Wireless kinematic body sensor network for low-cost neurotechnology applications “in-the-wild”. In Proceedings of the 2013 6th International IEEE/EMBS Conference on Neural Engineering (NER), San Diego, CA, USA, 6–8 November 2013; pp. 1279–1282. [Google Scholar]
- Lopez-Nava, I.H.; Angelica, M.M. Wearable Inertial Sensors for Human Motion Analysis: A Review; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2016. [Google Scholar]
- Reeder, B.; David, A. Health at hand: A systematic review of smart watch uses for health and wellness. J. Biomed. Inform. 2016, 63, 269–276. [Google Scholar] [CrossRef]
- King, C.E.; Sarrafzadeh, M. A Survey of Smartwatches in Remote Health Monitoring. J. Healthc. Inform. Res. 2018, 2, 1–24. [Google Scholar] [CrossRef]
- Piwek, L.; Ellis, D.A.; Andrews, S.; Joinson, A. The Rise of Consumer Health Wearables: Promises and Barriers. PLoS Med. 2016, 13, e1001953. [Google Scholar] [CrossRef]
- Wallen, M.P.; Gomersall, S.R.; Keating, S.E.; Wisloff, U.; Coombes, J.S. Accuracy of Heart Rate Watches: Implications for Weight Management. PLoS ONE 2016, 11, e0154420. [Google Scholar] [CrossRef]
- Xie, J.; Wen, D.; Liang, L.; Jia, Y.; Gao, L.; Lei, J. Evaluating the Validity of Current Mainstream Wearable Devices in Fitness Tracking Under Various Physical Activities: Comparative Study. JMIR Mhealth Uhealth 2018, 6, e94. [Google Scholar] [CrossRef] [PubMed]
- Evenson, K.R.; Goto, M.M.; Furberg, R.D. Systematic review of the validity and reliability of consumer-wearable activity trackers. Int. J. Behav. Nutr. Phys. Act. 2015, 12, 159. [Google Scholar] [CrossRef] [PubMed]
- Dooley, E.E.; Golaszewski, N.M.; Bartholomew, J.B. Estimating Accuracy at Exercise Intensities: A Comparative Study of Self-Monitoring Heart Rate and Physical Activity Wearable Devices. JMIR Mhealth Uhealth 2017, 5, e34. [Google Scholar] [CrossRef] [PubMed]
- An, H.S.; Jones, G.C.; Kang, S.K.; Welk, G.J.; Lee, J.M. How valid are wearable physical activity trackers for measuring steps? Eur. J. Sport Sci. 2017, 17, 360–368. [Google Scholar] [CrossRef] [PubMed]
- Kooiman, T.J.; Dontje, M.L.; Sprenger, S.R.; Krijnen, W.P.; van der Schans, C.P.; de Groot, M. Reliability and validity of ten consumer activity trackers. BMC Sports Sci. Med. Rehabil. 2015, 7, 24. [Google Scholar] [CrossRef]
- Shcherbina, A.; Mattsson, C.M.; Waggott, D.; Salisbury, H.; Christle, J.W.; Hastie, T.; Wheeler, M.T.; Ashley, E.A. Accuracy in Wrist-Worn, Sensor-Based Measurements of Heart Rate and Energy Expenditure in a Diverse Cohort. J. Pers. Med. 2017, 7, 3. [Google Scholar] [CrossRef]
- Kaewkannate, K.; Kim, S. A comparison of wearable fitness devices. BMC Public Health 2016, 16, 433. [Google Scholar] [CrossRef]
- Liang, J.; Xian, D.; Liu, X.; Fu, J.; Zhang, X.; Tang, B.; Lei, J. Usability Study of Mainstream Wearable Fitness Devices: Feature Analysis and System Usability Scale Evaluation. JMIR Mhealth Uhealth 2018, 6, e11066. [Google Scholar] [CrossRef]
- Wen, D.; Zhang, X.; Lei, J. Consumers’ perceived attitudes to wearable devices in health monitoring in China: A survey study. Comput. Methods Programs Biomed. 2017, 140, 131–137. [Google Scholar] [CrossRef]
- Tran, V.-T.; Riveros, C.; Ravaud, P. Patients’ views of wearable devices and AI in healthcare: Findings from the ComPaRe e-cohort. NPJ Digit. Med. 2019, 2, 53. [Google Scholar] [CrossRef]
- Hsiao, K.-L.; Chen, C.-C. What drives smartwatch purchase intention? Perspectives from hardware, software, design, and value. Telemat. Inform. 2018, 35, 103–113. [Google Scholar] [CrossRef]
- Market Share of Smartwatch Unit Shipments Worldwide from the 2Q’14 to 1Q’20*, by Vendor. Available online: https://www.statista.com/statistics/524830/global-smartwatch-vendors-market-share/ (accessed on 22 June 2020).
- Zhao, Y.; Heida, T.; Van Wegen, E.E.H.; Bloem, B.R.; Van Wezel, R.J.A. E-health support in people with Parkinson’s disease with smart glasses: A survey of user requirements and expectations in The Netherlands. J. Parkinson’s Dis. 2015, 5, 369–378. [Google Scholar] [CrossRef] [PubMed]
- Brooke, J. SUS: A retrospective. J. Usability Stud. 2013, 8, 29–40. [Google Scholar]
- Zhang, J.-T.; Novak, A.C.; Brouwer, B.; Li, Q. Concurrent validation of Xsens MVN measurement of lower limb joint angular kinematics. Physiol. Meas. 2013, 34, N63–N69. [Google Scholar] [CrossRef]
- Thies, S.B.; Tresadern, P.; Kenney, L.; Howard, D.; Goulermas, J.Y.; Smith, C.; Rigby, J. Comparison of linear accelerations from three measurement systems during “reach & grasp”. Med. Eng. Phys. 2007, 29, 967–972. [Google Scholar] [CrossRef]
- Cloete, T.; Scheffer, C. Benchmarking of a full-body inertial motion capture system for clinical gait analysis. In Proceedings of the 2008 30th Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Vancouver, BC, Canada, 20–25 August 2008; pp. 4579–4582. [Google Scholar]
- Robert-Lachaine, X.; Mecheri, H.; Larue, C.; Plamondon, A. Validation of inertial measurement units with an optoelectronic system for whole-body motion analysis. Med. Biol. Eng. Comput. 2017, 55, 609–619. [Google Scholar] [CrossRef]
- Teufl, W.; Lorenz, M.; Miezal, M.; Taetz, B.; Frohlich, M.; Bleser, G. Towards Inertial Sensor Based Mobile Gait Analysis: Event-Detection and Spatio-Temporal Parameters. Sensors 2018, 19, 38. [Google Scholar] [CrossRef]
- Teufl, W.; Miezal, M.; Taetz, B.; Frohlich, M.; Bleser, G. Validity, Test-Retest Reliability and Long-Term Stability of Magnetometer Free Inertial Sensor Based 3D Joint Kinematics. Sensors 2018, 18, 1980. [Google Scholar] [CrossRef]
- Karatsidis, A.; Jung, M.; Schepers, H.M.; Bellusci, G.; de Zee, M.; Veltink, P.H.; Andersen, M.S. Musculoskeletal model-based inverse dynamic analysis under ambulatory conditions using inertial motion capture. Med. Eng. Phys. 2019, 65, 68–77. [Google Scholar] [CrossRef]
- Del Din, S.; Godfrey, A.; Rochester, L. Validation of an Accelerometer to Quantify a Comprehensive Battery of Gait Characteristics in Healthy Older Adults and Parkinson’s Disease: Toward Clinical and at Home Use. IEEE J. Biomed. Health Inform. 2016, 20, 838–847. [Google Scholar] [CrossRef]
- Godfrey, A.; Del Din, S.; Barry, G.; Mathers, J.C.; Rochester, L. Instrumenting gait with an accelerometer: A system and algorithm examination. Med. Eng. Phys. 2015, 37, 400–407. [Google Scholar] [CrossRef] [PubMed]
- Doherty, A.; Jackson, D.; Hammerla, N.; Plotz, T.; Olivier, P.; Granat, M.H.; White, T.; van Hees, V.T.; Trenell, M.I.; Owen, C.G.; et al. Large Scale Population Assessment of Physical Activity Using Wrist Worn Accelerometers: The UK Biobank Study. PLoS ONE 2017, 12, e0169649. [Google Scholar] [CrossRef] [PubMed]
- Carse, B.; Meadows, B.; Bowers, R.; Rowe, P. Affordable clinical gait analysis: An assessment of the marker tracking accuracy of a new low-cost optical 3D motion analysis system. Physiotherapy 2013, 99, 347–351. [Google Scholar] [CrossRef] [PubMed]
- Ehara, Y.; Fujimoto, H.; Miyazaki, S.; Mochimaru, M.; Tanaka, S.; Yamamoto, S. Comparison of the performance of 3D camera systems II. Gait Posture 1997, 5, 251–255. [Google Scholar] [CrossRef]
- Maciejewski, M.; Piszczek, M.; Pomianek, M. Testing the SteamVR Trackers Operation Correctness with the OptiTrack System; SPIE: Bellingham, WA, USA, 2018; Volume 10830. [Google Scholar]
- Mortazavi, B.; Nemati, E.; Wall, K.V.; Flores-Rodriguez, H.G.; Cai, J.Y.J.; Lucier, J.; Naeim, A.; Sarrafzadeh, M. Can smartwatches replace smartphones for posture tracking? Sensors 2015, 15, 26783–26800. [Google Scholar] [CrossRef]
- Roetenberg, D.; Slycke, P.J.; Veltink, P.H. Ambulatory Position and Orientation Tracking Fusing Magnetic and Inertial Sensing. IEEE Trans. Biomed. Eng. 2007, 54, 883–890. [Google Scholar] [CrossRef]
- O’Donovan, K.J.; Kamnik, R.; O’Keeffe, D.T.; Lyons, G.M. An inertial and magnetic sensor based technique for joint angle measurement. J. Biomech. 2007, 40, 2604–2611. [Google Scholar] [CrossRef]
- Zhang, M.; Hol, J.D.; Slot, L.; Luinge, H. Second Order Nonlinear Uncertainty Modeling in Strapdown Integration Using MEMS IMUs. In Proceedings of the 14th International Conference on Information Fusion, Chicago, IL, USA, 5–8 July 2011; pp. 1–7. [Google Scholar]
- Bortz, J.E. A New Mathematical Formulation for Strapdown Inertial Navigation. IEEE Trans. Aerosp. Electron. Syst. 1971, AES-7, 61–66. [Google Scholar] [CrossRef]
- Paulich, M.; Schepers, M.; Rudigkeit, N.; Bellusci, G. Xsens MTw Awinda: Miniature Wireless Inertial-Magnetic Motion Tracker for Highly Accurate 3D Kinematic Applications; Xsens: Enschede, The Netherlands, 2018. [Google Scholar] [CrossRef]
- Bergamini, E.; Ligorio, G.; Summa, A.; Vannozzi, G.; Cappozzo, A.; Sabatini, A.M. Estimating orientation using magnetic and inertial sensors and different sensor fusion approaches: Accuracy assessment in manual and locomotion tasks. Sensors 2014, 14, 18625–18649. [Google Scholar] [CrossRef]
- Walch, O.; Huang, Y.; Forger, D.; Goldstein, C. Sleep stage prediction with raw acceleration and photoplethysmography heart rate data derived from a consumer wearable device. Sleep 2019, 42. [Google Scholar] [CrossRef]
- Amroun, H.; Temkit, M.; Ammi, M. DNN-Based Approach for Recognition of Human Activity Raw Data in Non-Controlled Environment. In Proceedings of the 2017 IEEE International Conference on AI & Mobile Services (AIMS), Honolulu, HI, USA, 25–30 June 2017; pp. 121–124. [Google Scholar]
- Kwon, M.C.; Park, G.; Choi, S. Smartwatch User Interface Implementation Using CNN-Based Gesture Pattern Recognition. Sensors 2018, 18, 2997. [Google Scholar] [CrossRef]
- Esser, P.; Dawes, H.; Collett, J.; Howells, K. IMU: Inertial sensing of vertical CoM movement. J. Biomech. 2009, 42, 1578–1581. [Google Scholar] [CrossRef] [PubMed]
- Chuah, S.H.-W.; Rauschnabel, P.A.; Krey, N.; Nguyen, B.; Ramayah, T.; Lade, S. Wearable technologies: The role of usefulness and visibility in smartwatch adoption. Comput. Hum. Behav. 2016, 65, 276–284. [Google Scholar] [CrossRef]
- Xiloyannis, M.; Gavriel, C.; Thomik, A.A.C.; Faisal, A.A. Gaussian Process Autoregression for Simultaneous Proportional Multi-Modal Prosthetic Control with Natural Hand Kinematics. IEEE Trans. Neural Syst. Rehabil. Eng. 2017, 25, 1785–1801. [Google Scholar] [CrossRef] [PubMed]
- Fara, S.; Vikram, C.S.; Gavriel, C.; Faisal, A.A. Robust, ultra low-cost MMG system with brain-machine-interface applications. In Proceedings of the 2013 6th International IEEE/EMBS Conference on Neural Engineering (NER), San Diego, CA, USA, 6–8 November 2013; pp. 723–726. [Google Scholar]
- Rinne, P.; Mace, M.; Nakornchai, T.; Zimmerman, K.; Fayer, S.; Sharma, P.; Liardon, J.L.; Burdet, E.; Bentley, P. Democratizing Neurorehabilitation: How Accessible are Low-Cost Mobile-Gaming Technologies for Self-Rehabilitation of Arm Disability in Stroke? PLoS ONE 2016, 11, e0163413. [Google Scholar] [CrossRef]
| In-Patient Closed Questions | |
| The device was easy to put on and take off? |
| I would feel comfortable wearing the device even if it is visible to others? |
| I feel I could do most of my normal activities (except those involving water) wearing the device? |
| The device did not interfere with washing or going to the toilet? |
| I would find it easy to learn to use the device? |
| I did not experience any itchiness or skin irritations using the device? |
| I did not experience any discomfort wearing the device? |
| I did not feel anxious wearing the device? |
| I would be willing to wear the device continuously for long term use? |
| I did not find the appearance or design of the sensors obtrusive? |
| Healthcare Professional Closed Questions | |
| The device was easy to put on and take off? |
| I would find it easy to learn to use the device? |
| Do you think that the increasing use of wearable tracking technology and Artificial Intelligence in healthcare is an opportunity? |
| Do you think that the increasing use of wearable tracking technology in Artificial Intelligence in healthcare is a danger? |
| If there were strong clinical evidence that the intervention would be equivalent or better than current neurological observations alone in a Neurology and Stroke setting, would you agree to use the new intervention in your own management of your patients? |
| In-patient Open Questions | |
| What do you like about the device? |
| What sort of characteristics and functions do you expect from the device? |
| Is there anything you don’t like about the device? |
| Healthcare Professional Open Questions | |
| What do you like about the device? |
| What sort of characteristics and functions do you expect from the device? |
| Is there anything you don’t like about the device? |
| What do you think are the benefits and risks you perceive when using these new technologies? |
| In-Patient Questionnaires | Under 65 | Over 65 | ||||
| Strongly Disagree | Somewhat Agree | Strongly Agree | Strongly Disagree | Somewhat Agree | Strongly Agree | |
| 1 | 0 | 20 | 1 | 2 | 19 |
| 0 | 2 | 19 | 0 | 3 | 19 |
| 0 | 1 | 20 | 0 | 1 | 21 |
| 1 | 1 | 20 | 3 | 1 | 18 |
| 1 | 0 | 20 | 1 | 4 | 17 |
| 1 | 0 | 21 | 0 | 1 | 21 |
| 2 | 1 | 19 | 0 | 1 | 21 |
| 2 | 0 | 20 | 0 | 0 | 22 |
| 2 | 1 | 19 | 1 | 4 | 17 |
| 0 | 3 | 18 | 1 | 0 | 21 |
| Healthcare Professional Questionnaires | Strongly Disagree | Somewhat Agree | Strongly Agree | |||
| 2 | 0 | 13 | |||
| 2 | 0 | 13 | |||
| No Opportunity | Great Opportunity | |||||
| 6 | 9 | ||||
| Dangerous | Safe | |||||
| 0 | 15 | ||||
| Would not use | Would only use if human-controlled | Would use and replace | ||||
| 0 | 6 | 9 | |||
| Themes | Details and Example Quotes |
|---|---|
| Likes | |
| ‘Fine’, ‘good’, ‘stylish’, ‘beautiful’, ‘modern’, ‘simple’ design |
| ‘unobtrusive’, ‘neutral’ or ‘unaware’ of the device. Sensor felt just like a ‘normal watch’, ‘non-invasive’ |
| ‘Easy to wear’, ‘simple to wear’ |
| Not concerned about the visibility of sensors to others as ‘appearance is fine’ |
| ‘Helpful for research’ and can improve healthcare |
| Dislikes | |
| Would like a ‘colour scheme’ |
| Skin ‘irritation’ from sensors |
| Cumbersome to wear with other ‘medical contraptions’ |
| Would like ‘stretchy’ and ‘magnetic straps’, straps ‘hard to get on’ |
| ‘too big’ |
| Expected characteristics and functions | |
| ‘Better looking’ straps |
| ‘beautiful design’, ‘brighter’ colour scheme |
| ‘Heart rate’ and ‘time’ functionalities |
| ‘Suitable’ to wear when going for ‘MRI scans’ |
| ‘Helpful for research’, ‘beneficial for other patients’ |
| ‘Smaller’ size |
| Themes | Details and Example Quotes |
|---|---|
| Benefits | |
| ‘Able to monitor movements to the development of new therapy’ |
| ‘Tailored therapy’ |
| Way of engaging with patients in their own health |
| ‘Wearer could be tracked’ to know ‘where they are’ |
| ‘Gather information … in objective way & patients didn’t seem inconvenienced’ |
| Ease of use and quick set-up |
| ‘convenient in the modern days of medicine’ |
| Risks | |
| ‘Ability for it to be shared with others that a patient did not consent to’ |
| ‘It can be lost as it is easy to remove’ |
| ‘Not comfortable on skin and can contribute to skin wounds’ |
| ‘Risk of false-positive results’ |
| Use …’ depends on patient compliance’ |
| Likes | |
| ‘Easy to wear and use’ |
| System used for health monitoring |
| Lightweight |
| System is not obtrusive for patients or healthcare professionals |
| It’s ‘portable’ so it is possible to ‘monitor’ whilst the patient is ‘mobile’ |
| Dislikes | |
| ‘Too bulky’ |
| Frustrated by having to ‘remove’ the sensors to accommodate ‘medical scans’ |
| Expected characteristics and functions | |
| Alerts to dangerous changes in ‘symptoms’ e.g., ‘GCS scores’ and area breaches within the ward |
| Combine with other important clinical measurements e.g., ‘Temperature ‘and ‘peripheral capillary oxygen saturation’. |
| ‘Instructions’ on how to use device. |
| On-screen ‘notifications’ on device |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Auepanwiriyakul, C.; Waibel, S.; Songa, J.; Bentley, P.; Faisal, A.A. Accuracy and Acceptability of Wearable Motion Tracking for Inpatient Monitoring Using Smartwatches. Sensors 2020, 20, 7313. https://doi.org/10.3390/s20247313
Auepanwiriyakul C, Waibel S, Songa J, Bentley P, Faisal AA. Accuracy and Acceptability of Wearable Motion Tracking for Inpatient Monitoring Using Smartwatches. Sensors. 2020; 20(24):7313. https://doi.org/10.3390/s20247313
Chicago/Turabian StyleAuepanwiriyakul, Chaiyawan, Sigourney Waibel, Joanna Songa, Paul Bentley, and A. Aldo Faisal. 2020. "Accuracy and Acceptability of Wearable Motion Tracking for Inpatient Monitoring Using Smartwatches" Sensors 20, no. 24: 7313. https://doi.org/10.3390/s20247313
APA StyleAuepanwiriyakul, C., Waibel, S., Songa, J., Bentley, P., & Faisal, A. A. (2020). Accuracy and Acceptability of Wearable Motion Tracking for Inpatient Monitoring Using Smartwatches. Sensors, 20(24), 7313. https://doi.org/10.3390/s20247313






