The Reliability and Validity of Wearable Inertial Sensors Coupled with the Microsoft Kinect to Measure Shoulder Range-of-Motion
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Raters
2.3. Instruments
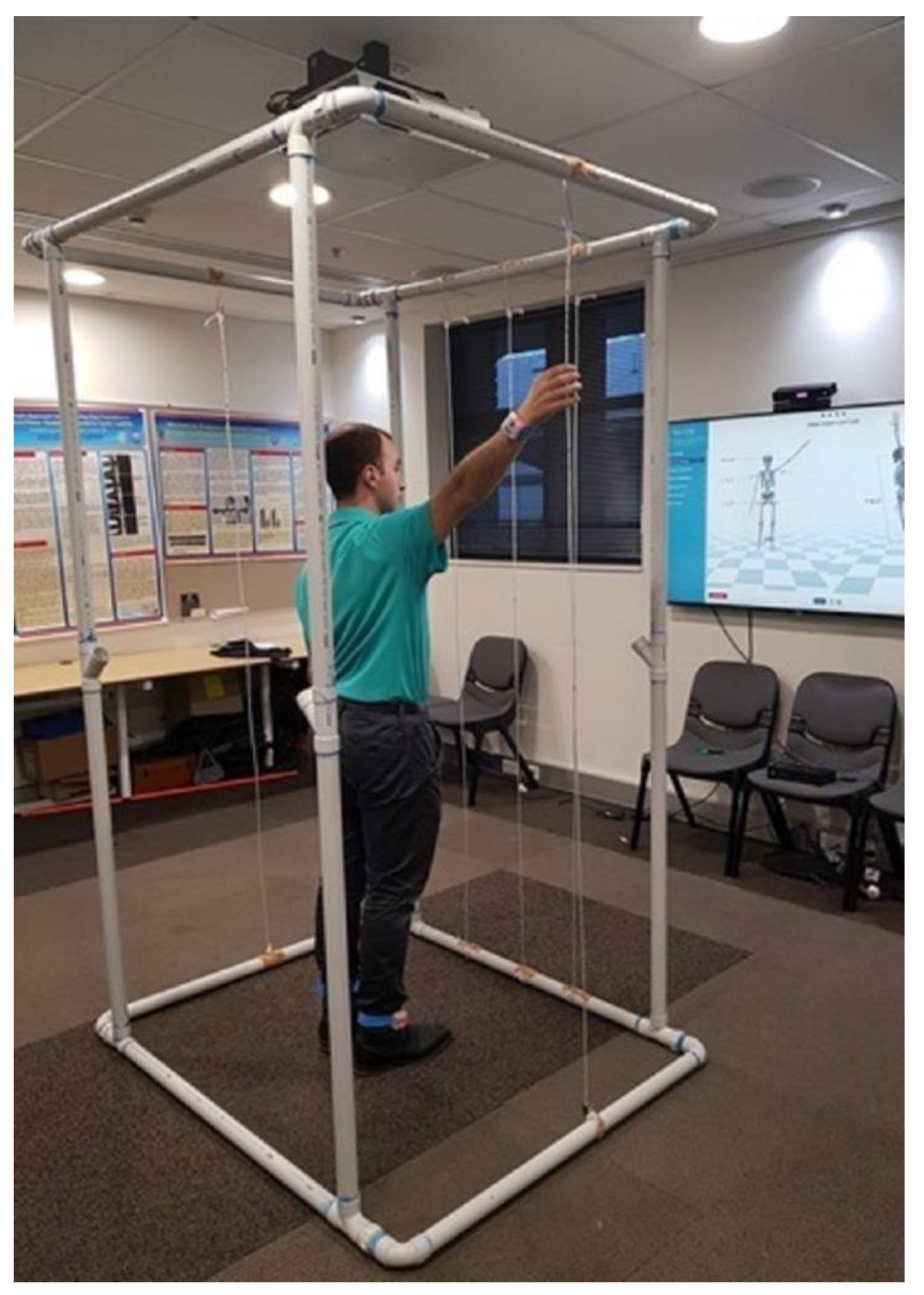
2.3.1. HumanTrak
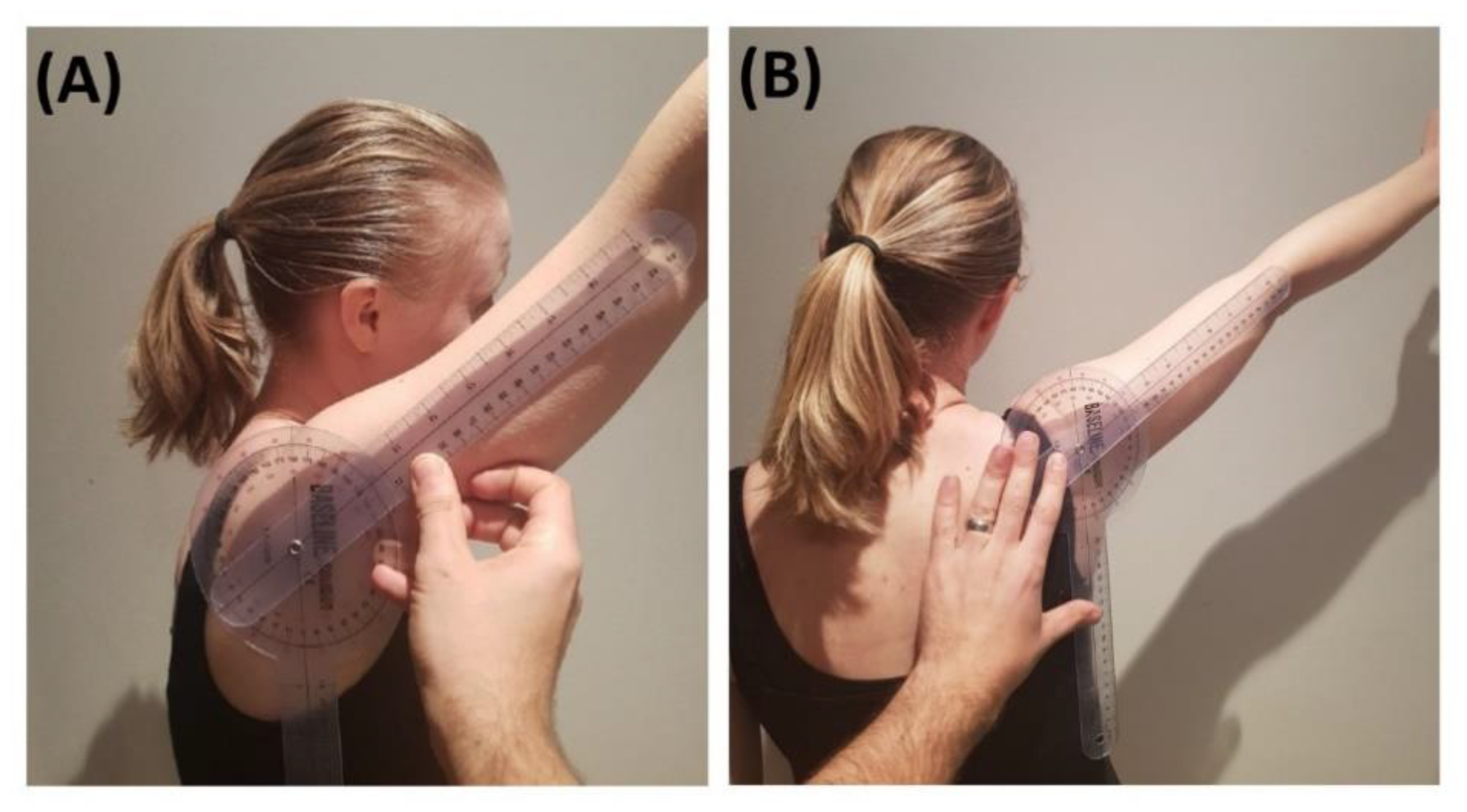
2.3.2. Goniometer
2.4. Procedures
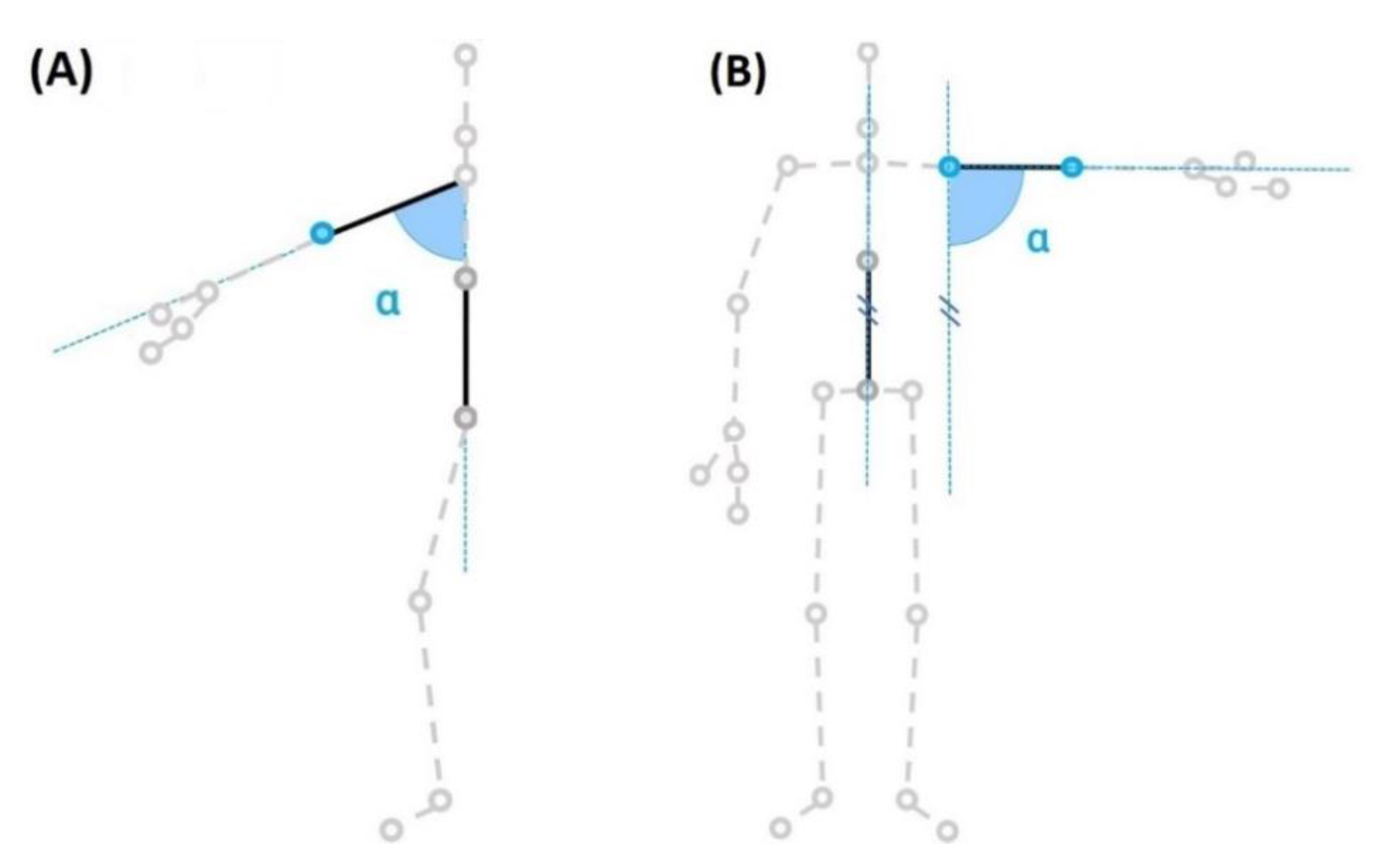
2.5. Data Capture and Processing
2.6. Statistical Analysis
2.7. Quality Criteria
3. Results
3.1. Intra-Rater Reliability
3.2. Inter-Rater Reliability
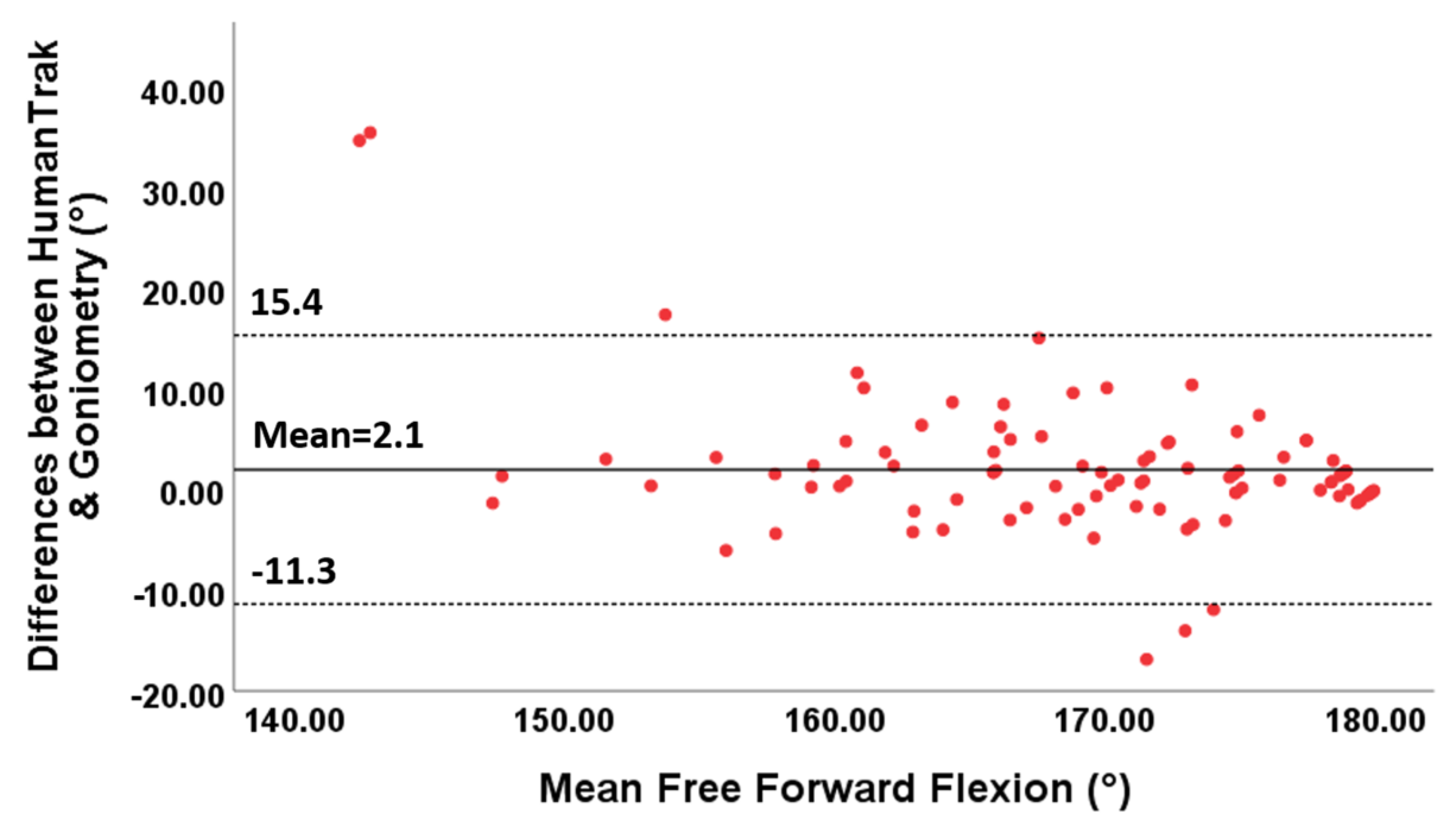
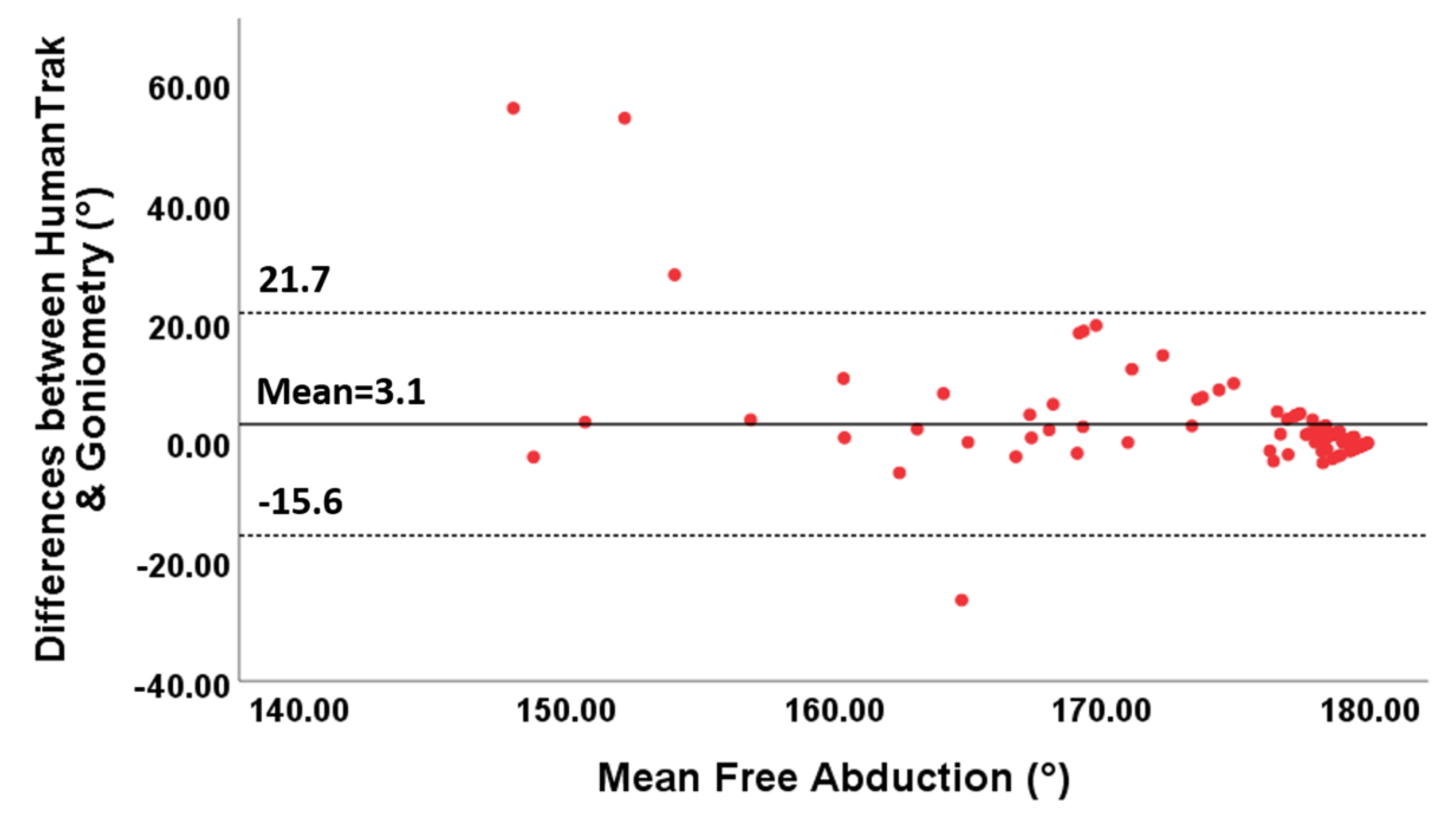
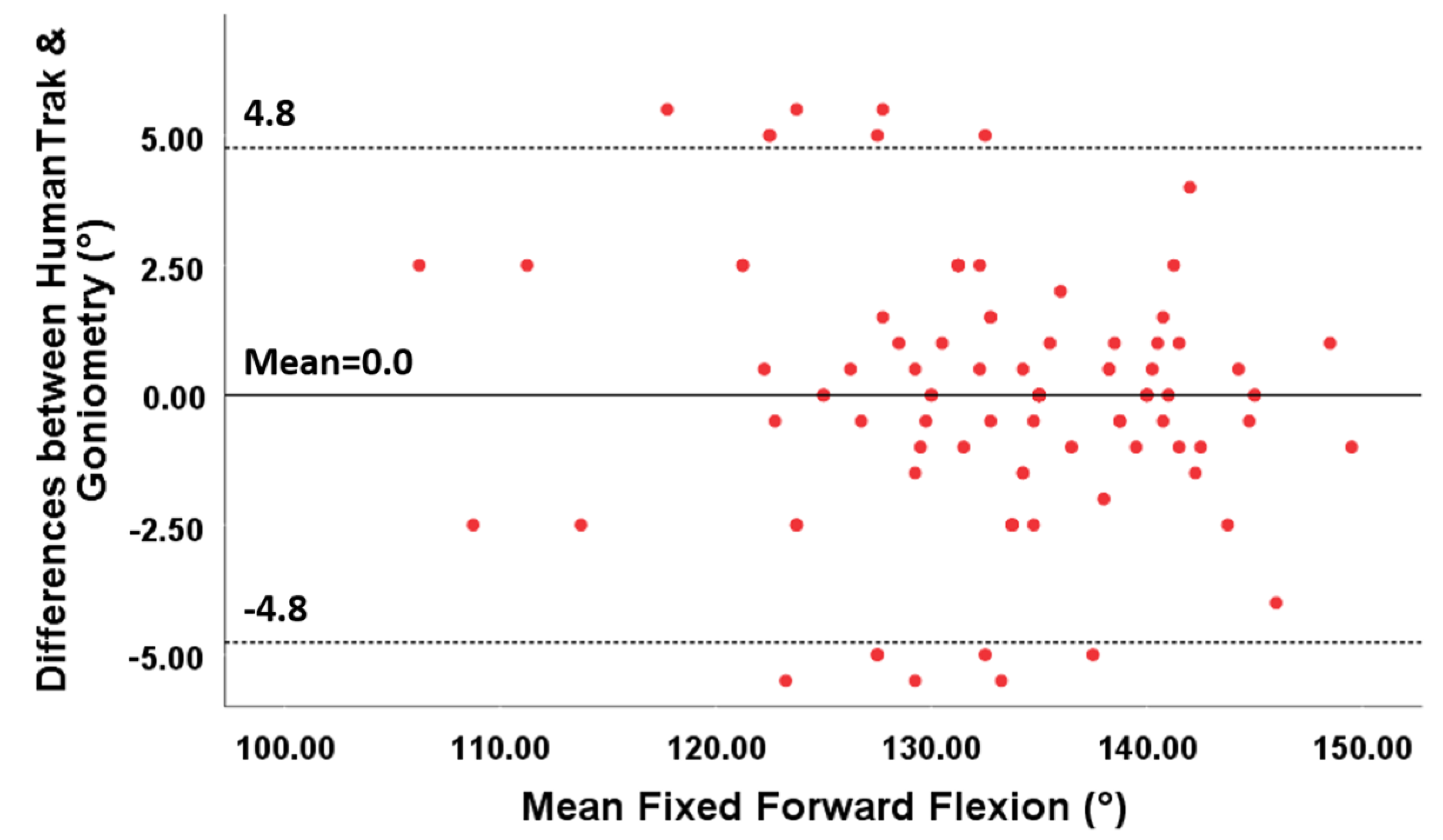
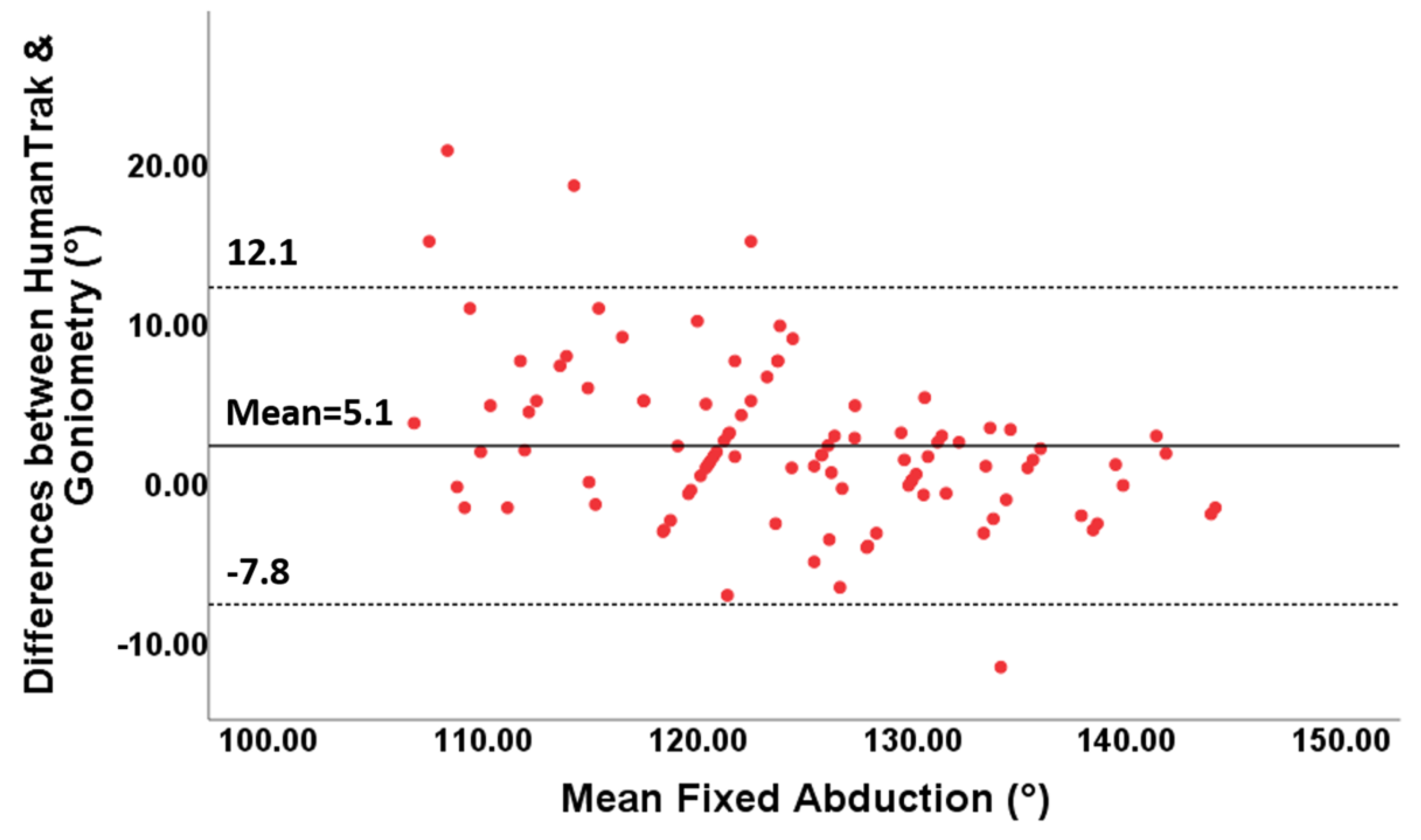
3.3. Construct Validity
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Muir, S.W.; Corea, C.L.; Beaupre, L. Evaluating change in clinical status: Reliability and measures of agreement for the assessment of glenohumeral range of motion. N. Am. J. Sports Phys. Ther. NAJSPT 2010, 5, 98–110. [Google Scholar] [PubMed]
- Terwee, C.; De Winter, A.F.; Scholten, R.J.; Jans, M.P.; Devillé, W.; Van Schaardenburg, D.; Bouter, L.M. Interobserver Reproducibility of the Visual Estimation of Range of Motion of the Shoulder. Arch. Phys. Med. Rehabil. 2005, 86, 1356–1361. [Google Scholar] [CrossRef] [PubMed]
- Gajdosik, R.; Bohannon, R. Clinical measurement of range of motion: Review of goniometry emphasizing reliability and validity. Phys. Ther. 1987, 67, 1867–1872. [Google Scholar] [CrossRef] [PubMed]
- Milanese, S.; Gordon, S.J.; Buettner, P.; Flavell, C.; Ruston, S.; Coe, D.; O’Sullivan, W.; McCormack, S. Reliability and concurrent validity of knee angle measurement: Smart phone app versus universal goniometer used by experienced and novice clinicians. Man. Ther. 2014, 19, 569–574. [Google Scholar] [CrossRef] [PubMed]
- Brosseau, L.; Tousignant, M.; Budd, J.; Chartier, N.; Duciaume, L.; Plamondon, S.; O’Sullivan, J.P.; O’Donoghue, S.; Balmer, S. Intratester and intertester reliability and criterion validity of the parallelogram and universal goniometers for active knee flexion in healthy subjects. Physiother. Res. Int. 1997, 2, 150–166. [Google Scholar] [CrossRef] [PubMed]
- Fieseler, G.; Laudner, K.G.; Irlenbusch, L.; Meyer, H.; Schulze, S.; Delank, K.-S.; Hermassi, S.; Bartels, T.; Schwesig, R. Inter- and intrarater reliability of goniometry and hand held dynamometry for patients with subacromial impingement syndrome. J. Exerc. Rehabil. 2017, 13, 704–710. [Google Scholar] [CrossRef] [PubMed]
- Lau, T.; Lin, S.; True, T.; Wu, W.; McKivigan, J.M. Reliability and Validity of a Smartphone-Based Inclinometer Application Measuring Shoulder Internal Rotation. J. Phys. Fit. Med. Treat. Sports 2020, 7, e555725. [Google Scholar] [CrossRef]
- Hayes, K.; Walton, J.R.; Szomor, Z.L.; Murrell, G.A. Reliability of five methods for assessing shoulder range of motion. Aust. J. Physiother. 2001, 47, 289–294. [Google Scholar] [CrossRef]
- Kolber, M.J.; Hanney, W.J. The reliability and concurrent validity of shoulder mobility measurements using a digital inclinometer and goniometer: A technical report. Int. J. Sports Phys. Ther. 2012, 7, 306–313. [Google Scholar]
- Greene, B.L.; Wolf, S.L. Upper extremity joint movement: Comparison of two measurement devices. Arch. Phys. Med. Rehabil. 1989, 70, 288–290. [Google Scholar]
- Sabari, J.S.; Maltzev, I.; Lubarsky, D.; Liszkay, E.; Homel, P. Goniometric assessment of shoulder range of motion: Comparison of testing in supine and sitting positions. Arch. Phys. Med. Rehabil. 1998, 79, 647–651. [Google Scholar] [CrossRef]
- Lea, R.D.; Gerhardt, J.J. Range-of-motion measurements. J. Bone Joint Surg. Am. 1995, 77, 784–798. [Google Scholar] [CrossRef] [PubMed]
- Akizuki, K.; Yamaguchi, K.; Morita, Y.; Ohashi, Y. The effect of proficiency level on measurement error of range of motion. J. Phys. Ther. Sci. 2016, 28, 2644–2651. [Google Scholar] [CrossRef][Green Version]
- Zhang, Z.; Ji, L.; Huang, Z.; Wu, J. Adaptive Information Fusion for Human Upper Limb Movement Estimation. IEEE Trans. Syst. Man Cybern. Part A Syst. Hum. 2012, 42, 1100–1108. [Google Scholar] [CrossRef]
- Teufl, W.; Miezal, M.; Taetz, B.; Fröhlich, M.; Bleser, G. Validity of inertial sensor based 3D joint kinematics of static and dynamic sport and physiotherapy specific movements. PLoS ONE 2019, 14, e0213064. [Google Scholar] [CrossRef] [PubMed]
- Morrow, M.M.; Lowndes, B.R.; Fortune, E.; Kaufman, K.R.; Hallbeck, M.S. Validation of Inertial Measurement Units for Upper Body Kinematics. J. Appl. Biomech. 2017, 33, 227–232. [Google Scholar] [CrossRef] [PubMed]
- Schall, M.C., Jr.; Fethke, N.B.; Chen, H.; Oyama, S.; Douphrate, D.I. Accuracy and repeatability of an inertial. measurement unit system for field-based occupational studies. Ergonomics 2016, 59, 591–602. [Google Scholar] [CrossRef]
- Zhou, H.; Stone, T.; Hu, H.; Harris, N. Use of multiple wearable inertial sensors in upper limb motion tracking. Med. Eng. Phys. 2008, 30, 123–133. [Google Scholar] [CrossRef]
- Cutti, A.G.; Giovanardi, A.; Rocchi, L.; Davalli, A.; Sacchetti, R. Ambulatory measurement of shoulder and elbow kinematics through inertial and magnetic sensors. Med. Biol. Eng. Comput. 2008, 46, 169–178. [Google Scholar] [CrossRef]
- El-Gohary, M.; McNames, J. Shoulder and Elbow Joint Angle Tracking With Inertial Sensors. IEEE Trans. Biomed. Eng. 2012, 59, 2635–2641. [Google Scholar] [CrossRef]
- Picerno, P.; Viero, V.; Donati, M.; Triossi, T.; Tancredi, V.; Melchiorri, G. Ambulatory assessment of shoulder abduction strength curve using a single wearable inertial sensor. J. Rehabil. Res. Dev. 2015, 52, 171–180. [Google Scholar] [CrossRef] [PubMed]
- Rigoni, M.; Gill, S.; Babazadeh, S.; Elsewaisy, O.; Gillies, H.; Nguyen, N.; Pathirana, P.N.; Page, R. Assessment of Shoulder Range of Motion Using a Wireless Inertial Motion Capture Device-A Validation Study. Sensors 2019, 19, 1781. [Google Scholar] [CrossRef] [PubMed]
- Xu, X.; Robertson, M.; Chen, K.B.; Lin, J.-H.; McGorry, R.W. Using the Microsoft Kinect™ to assess 3-D shoulder kinematics during computer use. Appl. Ergon. 2017, 65, 418–423. [Google Scholar] [CrossRef] [PubMed]
- Orand, A.; Aksoy, E.E.; Miyasaka, H.; Levy, C.W.; Zhang, X.; Menon, C. Bilateral Tactile Feedback-Enabled Training for Stroke Survivors Using Microsoft KinectTM. Sensors 2019, 19, 3474. [Google Scholar] [CrossRef]
- Ma, Y.; Mithraratne, K.; Wilson, N.C.; Wang, X.; Ma, Y.; Zhang, Y. The Validity and Reliability of a Kinect v2-Based Gait Analysis System for Children with Cerebral Palsy. Sensors 2019, 19, 1660. [Google Scholar] [CrossRef]
- Fern’Ndez-Baena, A.; Susin, A.; Lligadas, X. Biomechanical Validation of Upper-Body and Lower-Body Joint Movements of Kinect Motion Capture Data for Rehabilitation Treatments. In Proceedings of the 2012 Fourth International Conference on Intelligent Networking and Collaborative Systems, Bucharest, Romania, 19–21 September 2012; pp. 656–661. [Google Scholar]
- Huber, M.E.; Seitz, A.; Leeser, M.; Sternad, D. Validity and reliability of Kinect skeleton for measuring shoulder joint angles: A feasibility study. Physiotherapy 2015, 101, 389–393. [Google Scholar] [CrossRef] [PubMed]
- López, N.; Perez, E.; Tello, E.; Rodrigo, A.; Valentinuzzi, M.E. Statistical Validation for Clinical Measures: Repeatability and Agreement of Kinect™-Based Software. BioMed Res. Int. 2018, 2018, 6710595. [Google Scholar] [CrossRef]
- Hawi, N.; Liodakis, E.; Musolli, D.; Suero, E.M.; Stübig, T.; Claassen, L.; Kleiner, C.; Krettek, C.; Ahlers, V.; Citak, M. Range of motion assessment of the shoulder and elbow joints using a motion sensing input device: A pilot study. Technol. Health Care 2014, 22, 289–295. [Google Scholar] [CrossRef]
- Bonnechère, B.; Jansen, B.; Salvia, P.; Bouzahouene, H.; Omelina, L.; Moiseev, F.; Sholukha, V.; Cornelis, J.; Rooze, M.; Jan, S.V.S. Validity and reliability of the Kinect within functional assessment activities: Comparison with standard stereophotogrammetry. Gait Posture 2014, 39, 593–598. [Google Scholar] [CrossRef]
- Hondori, H.M.; Khademi, M. A Review on Technical and Clinical Impact of Microsoft Kinect on Physical Therapy and Rehabilitation. J. Med. Eng. 2014, 2014, 1–16. [Google Scholar] [CrossRef]
- Kizony, R.; Weiss, P.L.; Elion, O.; Harel, S.; Baum-Cohen, I.; Krasovsky, T.; Feldman, Y.; Shani, M. Development and validation of tele-health system for stroke rehabilitation. Int. J. Disabil. Hum. Dev. 2014, 13, 361–368. [Google Scholar] [CrossRef]
- Wilson, J.D.; Khan-Perez, J.; Marley, D.; Buttress, S.; Walton, M.; Li, B.; Roy, B. Can shoulder range of movement be measured accurately using the Microsoft Kinect sensor plus Medical Interactive Recovery Assistant (MIRA) software? J. Shoulder Elb. Surg. 2017, 26, e382–e389. [Google Scholar] [CrossRef] [PubMed]
- Çubukçu, B.; Yüzgeç, U.; Zileli, R.; Zileli, A. Reliability and validity analyzes of Kinect V2 based measurement system for shoulder motions. Med. Eng. Phys. 2019, 76, 20–31. [Google Scholar] [CrossRef] [PubMed]
- Hwang, S.; Tsai, C.-Y.; Koontz, A.M. Feasibility study of using a Microsoft Kinect for virtual coaching of wheelchair transfer techniques. Biomed. Eng. 2017, 62, 307–313. [Google Scholar] [CrossRef] [PubMed]
- Neto, J.S.D.C.; Filho, P.P.R.; Da Silva, G.P.F.; Olegario, N.B.D.C.; Duarte, J.B.F.; Albuquerque, V.H.C. Dynamic Evaluation and Treatment of the Movement Amplitude Using Kinect Sensor. IEEE Access 2018, 6, 17292–17305. [Google Scholar] [CrossRef]
- Guneysu, A.; Siyli, R.D.; Salah, A.A. Auto-evaluation of motion imitation in a child-robot imitation game for upper arm rehabilitation. In Proceedings of the the 23rd IEEE International Symposium on Robot and Human Interactive Communication, Edinburgh, UK, 25–29 August 2014; pp. 199–204. [Google Scholar]
- Milgrom, R.; Otd, B.; Foreman, M.; Standeven, J.; Engsberg, J.; Morgan, K.A. Reliability and validity of the Microsoft Kinect for assessment of manual wheelchair propulsion. J. Rehabil. Res. Dev. 2016, 53, 901–918. [Google Scholar] [CrossRef]
- Luinge, H.J.; Veltink, P.H. Measuring orientation of human body segments using miniature gyroscopes and accelerometers. Med. Biol. Eng. Comput. 2005, 43, 273–282. [Google Scholar] [CrossRef]
- Renaudin, V.; Afzal, M.H.; Lachapelle, G. Complete Triaxis Magnetometer Calibration in the Magnetic Domain. J. Sens. 2010, 2010, 967245. [Google Scholar] [CrossRef]
- Clark, R.A.; Pua, Y.-H.; Fortin, K.; Ritchie, C.; Webster, K.E.; Denehy, L.; Bryant, A.L. Validity of the Microsoft Kinect for assessment of postural control. Gait Posture 2012, 36, 372–377. [Google Scholar] [CrossRef]
- Atrsaei, A.; Salarieh, H.; Alasty, A. Human Arm Motion Tracking by Orientation-Based Fusion of Inertial Sensors and Kinect Using Unscented Kalman Filter. J. Biomech. Eng. 2016, 138, 091005. [Google Scholar] [CrossRef]
- Bo, A.P.L.; Hayashibe, M.; Poignet, P. Joint angle estimation in rehabilitation with inertial sensors and its integration with Kinect. In Proceedings of the 2011 Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Boston, MA, USA, 30 August–3 September 2011; Institute of Electrical and Electronics Engineers (IEEE): New York, NY, USA, 2011; pp. 3479–3483. [Google Scholar]
- Roy, G.; Bhuiya, A.; Mukherjee, A.; Bhaumik, S. Kinect Camera Based Gait Data Recording and Analysis for Assistive Robotics-An Alternative to Goniometer Based Measurement Technique. Procedia Comput. Sci. 2018, 133, 763–771. [Google Scholar] [CrossRef]
- Cai, L.; Ma, Y.; Xiong, S.; Zhang, Y. Validity and Reliability of Upper Limb Functional Assessment Using the Microsoft Kinect V2 Sensor. Appl. Bionics Biomech. 2019, 2019, 7175240. [Google Scholar] [CrossRef] [PubMed]
- Mangal, N.K.; Tiwari, A.K. Kinect v2 tracked Body Joint Smoothing for Kinematic Analysis in Musculoskeletal Disorders. In Proceedings of the 2020 42nd Annual International Conference of the IEEE Engineering in Medicine & Biology Society (EMBC), Montreal, QC, Canada, 20–24 July 2020; pp. 5769–5772. [Google Scholar] [CrossRef]
- HumanTrak Validation Case Study. Australian Catholic University Biomechanics Laboratory. Available online: https://www.valdperformance.com/wp-content/uploads/2018/12/HumanTrak-Validation-Case-Study-ACU-Melbourne-2.0.pdf (accessed on 10 December 2018).
- Yoon, T.-L. Validity and Reliability of an Inertial Measurement Unit-Based 3D Angular Measurement of Shoulder Joint Motion. J. Korean Phys. Ther. 2017, 29, 145–151. [Google Scholar] [CrossRef]
- Lee, S.H.; Yoon, C.; Chung, S.G.; Kim, H.C.; Kwak, Y.; Park, H.-W.; Kim, K. Measurement of Shoulder Range of Motion in Patients with Adhesive Capsulitis Using a Kinect. PLoS ONE 2015, 10, e0129398. [Google Scholar] [CrossRef]
- Schiefer, C.; Kraus, T.; Ellegast, R.; Ochsmann, E. A technical support tool for joint range of motion determination in functional diagnostics—An inter-rater study. J. Occup. Med. Toxicol. 2015, 10, 1–13. [Google Scholar] [CrossRef]
- Poitras, I.; Dupuis, F.; Bielmann, M.; Campeau-Lecours, A.; Mercier, C.; Bouyer, L.J.; Roy, J.S. Validity and Reliability of Wearable Sensors for Joint Angle Estimation: A Systematic Review. Sensors 2019, 19, 1555. [Google Scholar] [CrossRef]
- Puh, U.; Hoelhlein, B.; Deutsch, J.E. Validity and Reliability of the Kinect for Assessment of Standardized Transitional Movements and Balance: Systematic Review and Translation into Practice. Phys. Med. Rehabil. Clin. N. Am. 2019, 30, 399–422. [Google Scholar] [CrossRef]
- Walmsley, C.P.; Williams, S.A.; Grisbrook, T.; Elliot, C.; Imms, C.; Campbell, A. Measurement of Upper Limb Range of Motion Using Wearable Sensors: A Systematic Review. Sports Med Open. 2018, 4, 53. [Google Scholar] [CrossRef]
- Cools, A.M.; De Wilde, L.; Van Tongel, A.; Ceyssens, C.; Ryckewaert, R.; Cambier, D.C. Measuring shoulder external and internal rotation strength and range of motion: Comprehensive intra-rater and inter-rater reliability study of several testing protocols. J. Shoulder Elb. Surg. 2014, 23, 1454–1461. [Google Scholar] [CrossRef]
- Mullaney, M.J.; McHugh, M.P.; Johnson, C.P.; Tyler, T.F. Reliability of shoulder range of motion comparing a goniometer to a digital level. Physiother. Theory Pract. 2010, 26, 327–333. [Google Scholar] [CrossRef]
- Riddle, D.L.; Rothstein, J.M.; Lamb, R.L. Goniometric reliability in a clinical setting. Shoulder measurements. Phys. Ther. 1987, 67, 668–673. [Google Scholar] [CrossRef] [PubMed]
- Hanney, W.J.; Kolber, M.J.; Marshall, J.S. The reliability of clinical measurements designed to quantify shoulder mobility. Phys. Ther. Rev. 2011, 16, 413–422. [Google Scholar] [CrossRef]
- Beshara, P.; Chen, J.; Lagadec, P.; Walsh, W.R. Test-Retest and Intra-rater Reliability of Using Inertial Sensors and Its Integration with Microsoft Kinect™ to Measure Shoulder Range-of-Motion. In Internet of Things Technologies for HealthCare; Lecture Notes of the Institute for Computer Sciences, Social Informatics and Telecommunications Engineering Series; Springer International Publishing: Cham, Switzerland, 2016; Volume 187. [Google Scholar] [CrossRef]
- Jain, N.B.; Wilcox, R.; Katz, J.N.; Higgins, L.D. Clinical Examination of the Rotator Cuff. PM R. 2013, 5, 45–56. [Google Scholar] [CrossRef] [PubMed]
- Koo, T.K.; Li, M.Y. A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research. J. Chiropr. Med. 2016, 15, 155–163. [Google Scholar] [CrossRef] [PubMed]
- Shrout, P.E.; Fleiss, J.L. Intraclass correlations: Uses in assessing rater reliability. Psychol. Bull. 1979, 86, 420–428. [Google Scholar] [CrossRef] [PubMed]
- Weir, J.P. Quantifying Test-Retest Reliability Using the Intraclass Correlation Coefficient and the SEM. J. Strength Cond. Res. 2005, 19, 231–240. [Google Scholar] [CrossRef]
- Portney, L.G.; Watkins, M.P. Foundations of Clinical Research: Applications to Practice, 3rd ed.; Pearson Prentice Hall: Upper Saddle River, NJ, USA, 2009; ISBN 978-0131716407. [Google Scholar]
- Bland, J.M.; Altman, D. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986, 327, 307–310. [Google Scholar] [CrossRef]
- De Winter, A.F.; Heemskerk, M.; Terwee, C.; Jans, M.P.; Devillé, W.; Van Schaardenburg, D.-J.; Scholten, R.J.P.M.; Bouter, L.M. Inter-observer reproducibility of measurements of range of motion in patients with shoulder pain using a digital inclinometer. BMC Musculoskelet. Disord. 2004, 5, 18. [Google Scholar] [CrossRef]
- Terwee, C.; Bot, S.D.; De Boer, M.R.; Van Der Windt, D.A.; Knol, D.L.; Dekker, J.; Bouter, L.M.; De Vet, H.C. Quality criteria were proposed for measurement properties of health status questionnaires. J. Clin. Epidemiol. 2007, 60, 34–42. [Google Scholar] [CrossRef]
- Anderson, D.B.; Mathieson, S.; Eyles, J.; Maher, C.G.; Van Gelder, J.M.; Tomkins-Lane, C.C.; Ammendolia, C.; Bella, V.; Ferreira, M.L.; Ammendiola, C. Measurement properties of walking outcome measures for neurogenic claudication: A systematic review and meta analysis. Spine J. 2019, 19, 1378–1396. [Google Scholar] [CrossRef]
- Jordan, K.; Dziedzic, K.; Jones, P.W.; Ong, B.N.; Dawes, P.T. The reliability of the three-dimensional FASTRAK measurement system in measuring cervical spine and shoulder range of motion in healthy subjects. Rheumatology 2000, 39, 382–388. [Google Scholar] [CrossRef]
- Springer, S.; Seligmann, G.Y. Validity of the Kinect for Gait Assessment: A Focused Review. Sensors 2016, 16, 194. [Google Scholar] [CrossRef]


| Study | Target Population (n) | Intra-Rater Reliability ICC | Inter-Rater Reliability ICC | ||
|---|---|---|---|---|---|
| Shoulder Flexion | Shoulder Abduction | Shoulder Flexion | Shoulder Abduction | ||
| Hawi et al. | Healthy, free ROM without deficits (n = 7) | 0.99 | 0.96 | - | - |
| Bonnechère et al. | Healthy (n = 48) | - | 0.73 | - | - |
| Çubukçu et al. | Healthy (n = 40) | 0.851 | 0.861 | - | - |
| Hwang et al. | Wheelchair usage for 1 year, able to sit upright for at least 4 h a day, use a wheelchair for >40 h/week (n = 8) | L = 0.96 R = 0.92 | L = 0.92 R = 0.96 | - | - |
| Da Cunha Neto et al. | Healthy (n = 10) | 0.97 | 0.98 | 0.91 | 0.97 |
| Guneysu et al. | Healthy, children aged 3–11 (n = 8) | - | - | 0.8961 | 0.7935 |
| Milgrom et al. | Spinal cord injury, ability to self-propel a manual wheelchair, wheelchair usage for at least 75% of daily activities (n = 5) | - | - | 0.97 | 0.94 |
| Free AROM | Mean ± SD (°) | ICC3,1 | 95% CI | SEM (°) | MDC (°) | r |
|---|---|---|---|---|---|---|
| Forward flexion | 169.7 ± 8.4 | 0.93 | 0.89–0.96 | 2.2 | 6.1 | 0.89 |
| Abduction | 175.8 ± 6.8 | 0.85 | 0.77–0.90 | 2.7 | 7.5 | 0.73 |
| Fixed AROM | ||||||
| Forward flexion | 134.8 ± 8.2 | 0.81 | 0.72–0.87 | 3.6 | 10.0 | 0.69 |
| Abduction | 124.5 ± 10.8 | 0.94 | 0.91–0.96 | 2.7 | 7.5 | 0.91 |
| Free AROM | Mean ± SD (°) | ICC3,1 | 95% CI | SEM (°) | MDC (°) | r |
|---|---|---|---|---|---|---|
| Forward flexion | 168.5 ± 10.3 | 0.75 | 0.64–0.82 | 5.2 | 14.4 | 0.75 |
| Abduction | 172.5 ± 10.8 | 0.53 | 0.38–0.66 | 7.4 | 20.5 | 0.53 |
| Fixed AROM | ||||||
| Forward flexion | 132.5 ± 9.2 | 0.70 | 0.50–0.82 | 5.0 | 13.9 | 0.58 |
| Abduction | 124.4 ± 8.2 | 0.93 | 0.88–0.96 | 2.7 | 7.4 | 0.87 |
| Free AROM | ICC2,k | 95% CI | SEM (°) | MDC (°) |
| Forward flexion | 0.92 | 0.87–0.96 | 2.0 | 5.6 |
| Abduction | 0.88 | 0.77–0.93 | 1.5 | 4.3 |
| Fixed AROM | ICC2,k | 95% CI | SEM (°) | MDC (°) |
| Forward flexion | 0.65 | 0.41–0.80 | 4.6 | 12.7 |
| Abduction | 0.98 | 0.96–0.99 | 1.9 | 5.1 |
| Free AROM | Mean ± SD (°) | ICC | 95% CI | Mean diff (°) | r |
| Forward flexion | 169.4 ± 9.5 | 0.84 | 0.72–0.87 | 2.05 | 0.77 |
| Abduction | 174.5 ± 9.1 | 0.59 | 0.60–0.82 | 3.05 | 0.50 |
| Fixed AROM | Mean ± SD (°) | ICC | 95% CI | Mean diff (°) | r |
| Forward flexion | 133.0 ± 8.2 | 0.98 | 0.97–0.99 | 0.00 | 0.96 |
| Abduction | 124.3 ± 9.4 | 0.91 | 0.84–0.94 | 2.18 | 0.87 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Beshara, P.; Chen, J.F.; Read, A.C.; Lagadec, P.; Wang, T.; Walsh, W.R. The Reliability and Validity of Wearable Inertial Sensors Coupled with the Microsoft Kinect to Measure Shoulder Range-of-Motion. Sensors 2020, 20, 7238. https://doi.org/10.3390/s20247238
Beshara P, Chen JF, Read AC, Lagadec P, Wang T, Walsh WR. The Reliability and Validity of Wearable Inertial Sensors Coupled with the Microsoft Kinect to Measure Shoulder Range-of-Motion. Sensors. 2020; 20(24):7238. https://doi.org/10.3390/s20247238
Chicago/Turabian StyleBeshara, Peter, Judy F. Chen, Andrew C. Read, Pierre Lagadec, Tian Wang, and William Robert Walsh. 2020. "The Reliability and Validity of Wearable Inertial Sensors Coupled with the Microsoft Kinect to Measure Shoulder Range-of-Motion" Sensors 20, no. 24: 7238. https://doi.org/10.3390/s20247238
APA StyleBeshara, P., Chen, J. F., Read, A. C., Lagadec, P., Wang, T., & Walsh, W. R. (2020). The Reliability and Validity of Wearable Inertial Sensors Coupled with the Microsoft Kinect to Measure Shoulder Range-of-Motion. Sensors, 20(24), 7238. https://doi.org/10.3390/s20247238





