ECG QT-I nterval Measurement Using Wavelet Transformation
Abstract
1. Introduction
2. Subjects and Methods
2.1. Subjects
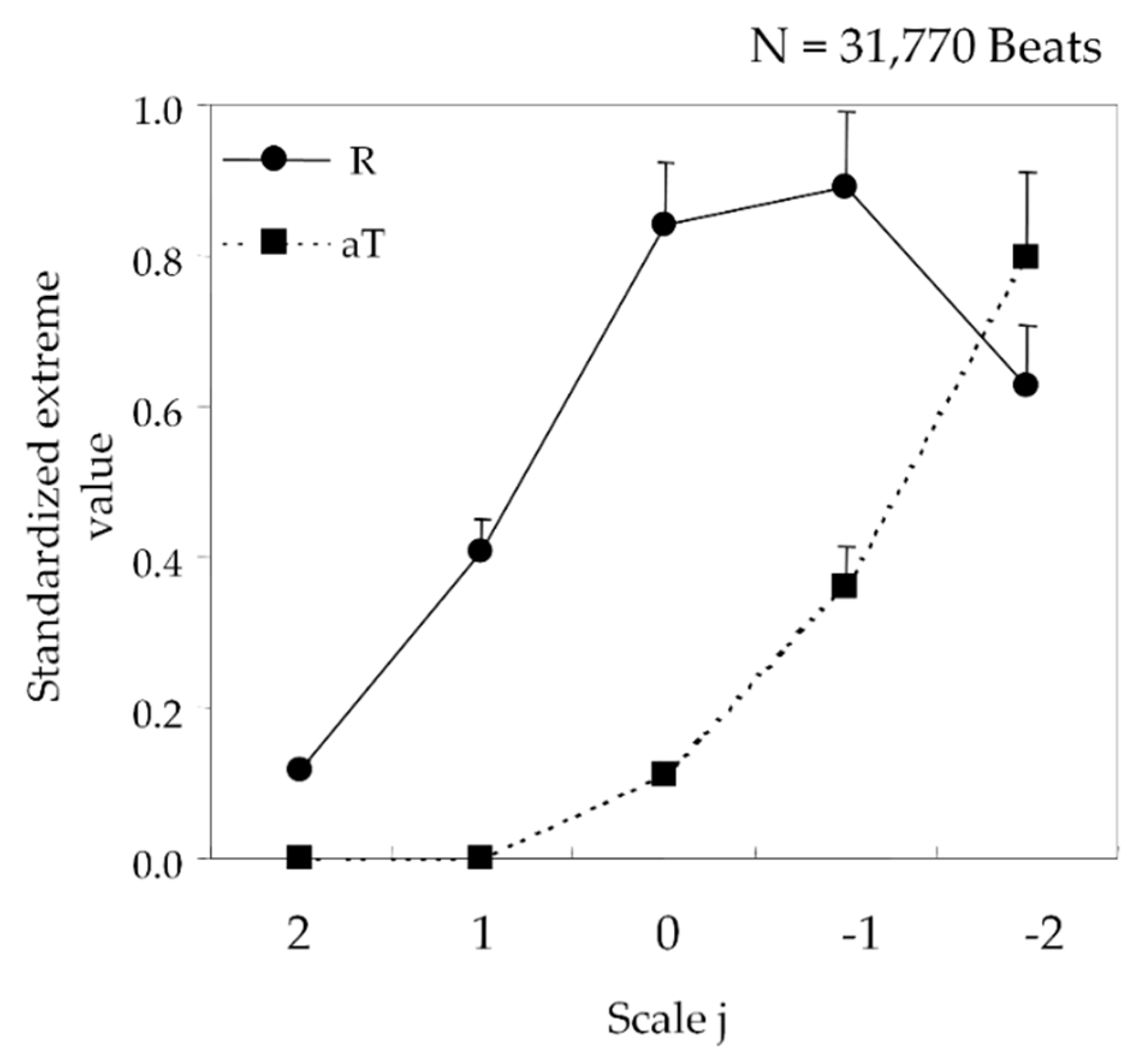
2.2. ECG Recognition Using Wavelet Transformation
3. Validation of ECG Recognition Efficacy
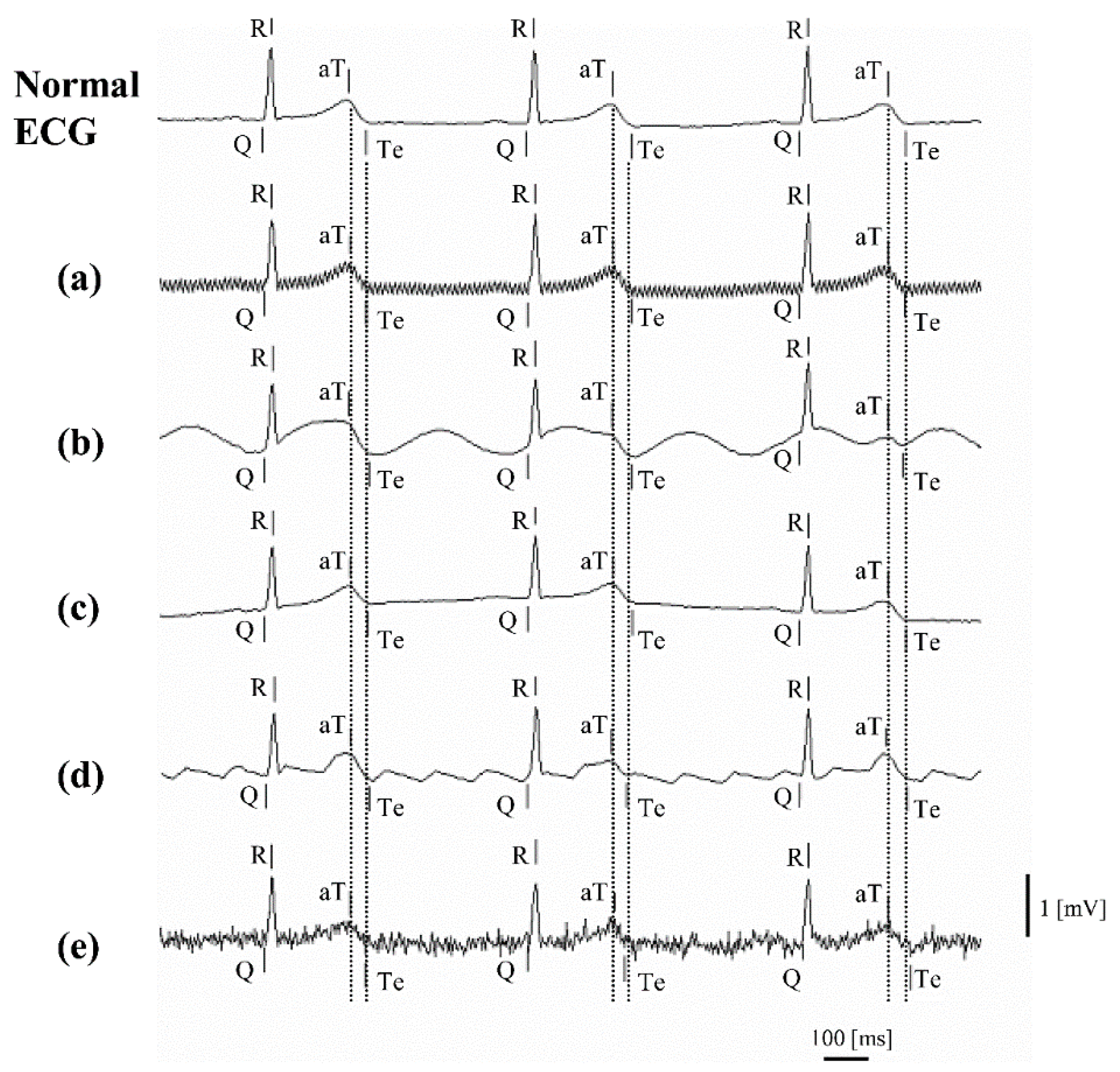
3.1. Noise Tolerance Simulation
- (a)
- commercial power noise: 0.2 mV, 50/60 Hz sine wave
- (b)
- ambulatory noise: 0.5 mV, 2 Hz sine wave
- (c)
- respiratory noise: 0.5 mV, 0.25 Hz sine wave
- (d)
- atrial flutter noise: 0.4 mV, 5 Hz sawtooth wave
- (e)
- electromyographic (EMG) noise: white noise and 1 mV, 20–40 Hz sine wave.
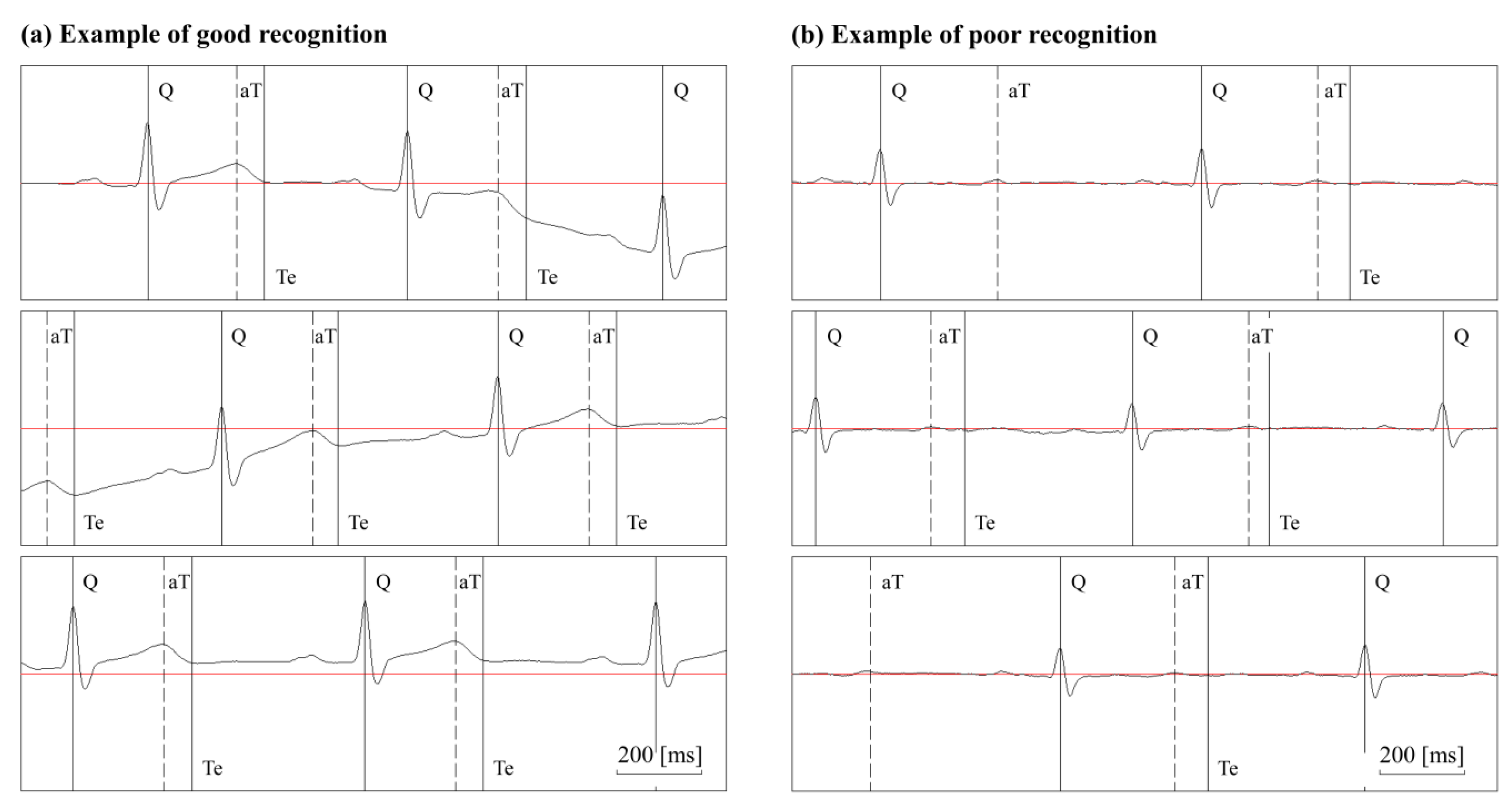
3.2. Validation of Recognition Points
4. Results
4.1. Results of Noise Tolerance Simulation
4.2. Validity of Recognition Points
5. Discussion
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Shimizu, W.; Antzelevitch, C. Cellular basis for the electrocardiographic features of the LQT1 form of the long QT syndrome. Effects of β adrenergic agonists, antagonists and sodium channel blockers on transmural dispersion of repolarization and torsades de pointes. Circulation 1998, 31, 2. [Google Scholar] [CrossRef][Green Version]
- Schwartz, P.J.; Stramba-Badiale, M.; Segantini, A.; Austoni, P.; Bosi, G.; Giorgetti, R.; Grancini, F.; Marni, E.D.; Perticone, F.; Rosti, D.; et al. Prolongation of the QT Interval and the Sudden Infant Death Syndrome. N. Engl. J. Med. 1998, 338, 1709–1714. [Google Scholar] [CrossRef] [PubMed]
- Nitaro, S.; Kazuo, K.; Shin, I.; Kazuyuki, M.; Junichiro, H. QT interval in an Electrocardiogram and the autonomous nerve [Translated from Japanese.]. Tokyo Heart J. 2002, 22, 67–78. [Google Scholar]
- Lepeschkin, E.; Surawicz, B. The Measurement of the Q-T Interval of the Electrocardiogram. Circulation 1952, 6, 378–388. [Google Scholar] [CrossRef] [PubMed]
- Fujiki, A.; Sugao, M.; Nishida, K.; Sakabe, M.; Tsuneda, T.; Mizumaki, K.; Inoue, H. Repolarization Abnormality in Idiopathic Ventricular Fibrillation: Assessment using 24 hour QT-RR and QaT-RR relationships. J. Cardiovasc. Electrophysiol. 2004, 15, 59–63. [Google Scholar] [CrossRef] [PubMed]
- Emori, T.; Ohe, T.; Aihara, N.; Kurita, T.; Shimizu, W.; Kamakura, S.; Shimomura, K. Dynamic Relationship Between the Q-aT Interval and Heart Rate in Patients with Long QT Syndrome During 24-Hour Holter ECG Monitoring. Pacing Clin. Electrophysiol. 1995, 18, 1909–1918. [Google Scholar] [CrossRef] [PubMed]
- Cuadros, J.; Dugarte, N.; Wong, S.; Vanegas, P.; Morocho, V.; Medina, R. ECG Multilead QT Interval Estimation Using Support Vector Machines. J. Healthc. Eng. 2019, 2019, 6371871. [Google Scholar] [CrossRef] [PubMed]
- Postema, P.G.; Wilde, A.A. The Measurement of the QT Interval. Curr. Cardiol. Rev. 2014, 10, 287–294. [Google Scholar] [CrossRef] [PubMed]
- Ghaffari, A.; Homaeinezhad, M.; Akraminia, M.; Atarod, M.; Daevaeiha, M. A robust wavelet-based multi-lead electrocardiogram delineation algorithm. Med. Eng. Phys. 2009, 31, 1219–1227. [Google Scholar] [CrossRef] [PubMed]
- Martínez, J.P.; Almeida, R.; Olmos, S.; Rocha, A.P.; Laguna, P. A Wavelet-Based ECG Delineator: Evaluation on Standard Databases. IEEE Trans. Biomed. Eng. 2004, 51, 570–581. [Google Scholar] [CrossRef] [PubMed]
- Ohmuta, T.; Iimura, K.; Mitsui, K.; Shibata, N. Development of a QT measurement method by applying wavelet transform analysis and its correlation with QaT measurement [Translated from Japanese.]. Jpn. J. Electrocardiol. 2006, 26, 803–809. [Google Scholar] [CrossRef]
- Ishikawa, Y. Wavelet Analysis for Clinical Medicine [Translated from Japanese.], 1st ed.; Medical Publication (IGAKU-SHUPPAN): Tokyo, Japan, 2000; pp. 221–240. [Google Scholar]
- ICH. The Clinical Evaluation of QT/QTc Interval Prolongation and Proarrhythmic Potential for Non-Antiarrhythmic Drugs E14; Step 4; EMEA: London, UK, 2005. [Google Scholar]

| Type of Noise | Q | R | aT | Te | QTe |
|---|---|---|---|---|---|
| (a) Commercial power noise 50 Hz | −0.5 | −0.6 | −0.9 | 0.4 | 1.0 |
| Commercial power noise 60 Hz | −0.5 | −2.3 | 0.1 | 0.0 | 0.5 |
| (b) Respiratory noise | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| (c) EMG noise | −3.6 | −2.2 | 7.4 | 0.0 | 3.6 |
| (d) Atrial flutter noise | −5.8 | 0.0 | 11.3 | 3.5 | 9.4 |
| (e) Ambulatory noise | 0.1 | 0.1 | −0.2 | 1.1 | 1.0 |
| Subjects | Heartbeats Used for Comparison | Difference from Visual Evaluation (ms) |
|---|---|---|
| (1) 21 M | 100 | 3.8 |
| (2) 22 M | 100 | 2.1 |
| (3) 22 M | 100 | 2.0 |
| (4) 22 M | 100 | 3.9 |
| (5) 22 M | 100 | 4.2 |
| (6) 22 M | 100 | 7.8 |
| (7) 22 M | 70 | 5.8 |
| (8) 23 M | 100 | 12.3 |
| (9) 32 M | 100 | 5.3 |
| (10) 55 M | 100 | 4.3 |
| (11) 56 M | 100 | 4.0 |
| (12) 72 M | 80 | 4.5 |
| (13) 25 F | 60 | 3.8 |
| (14) 49 F | 100 | 3.0 |
| (15) 61 F | 100 | 3.8 |
| (16) 65 F | 100 | 8.5 |
| (17) 71 F | 100 | 2.0 |
| - | 1610 | 4.8 ± 2.6 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ohmuta, T.; Mitsui, K.; Shibata, N. ECG QT-I nterval Measurement Using Wavelet Transformation. Sensors 2020, 20, 4578. https://doi.org/10.3390/s20164578
Ohmuta T, Mitsui K, Shibata N. ECG QT-I nterval Measurement Using Wavelet Transformation. Sensors. 2020; 20(16):4578. https://doi.org/10.3390/s20164578
Chicago/Turabian StyleOhmuta, Takao, Kazuyuki Mitsui, and Nitaro Shibata. 2020. "ECG QT-I nterval Measurement Using Wavelet Transformation" Sensors 20, no. 16: 4578. https://doi.org/10.3390/s20164578
APA StyleOhmuta, T., Mitsui, K., & Shibata, N. (2020). ECG QT-I nterval Measurement Using Wavelet Transformation. Sensors, 20(16), 4578. https://doi.org/10.3390/s20164578





