Is a Wearable Sensor-Based Characterisation of Gait Robust Enough to Overcome Differences Between Measurement Protocols? A Multi-Centric Pragmatic Study in Patients with Multiple Sclerosis
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
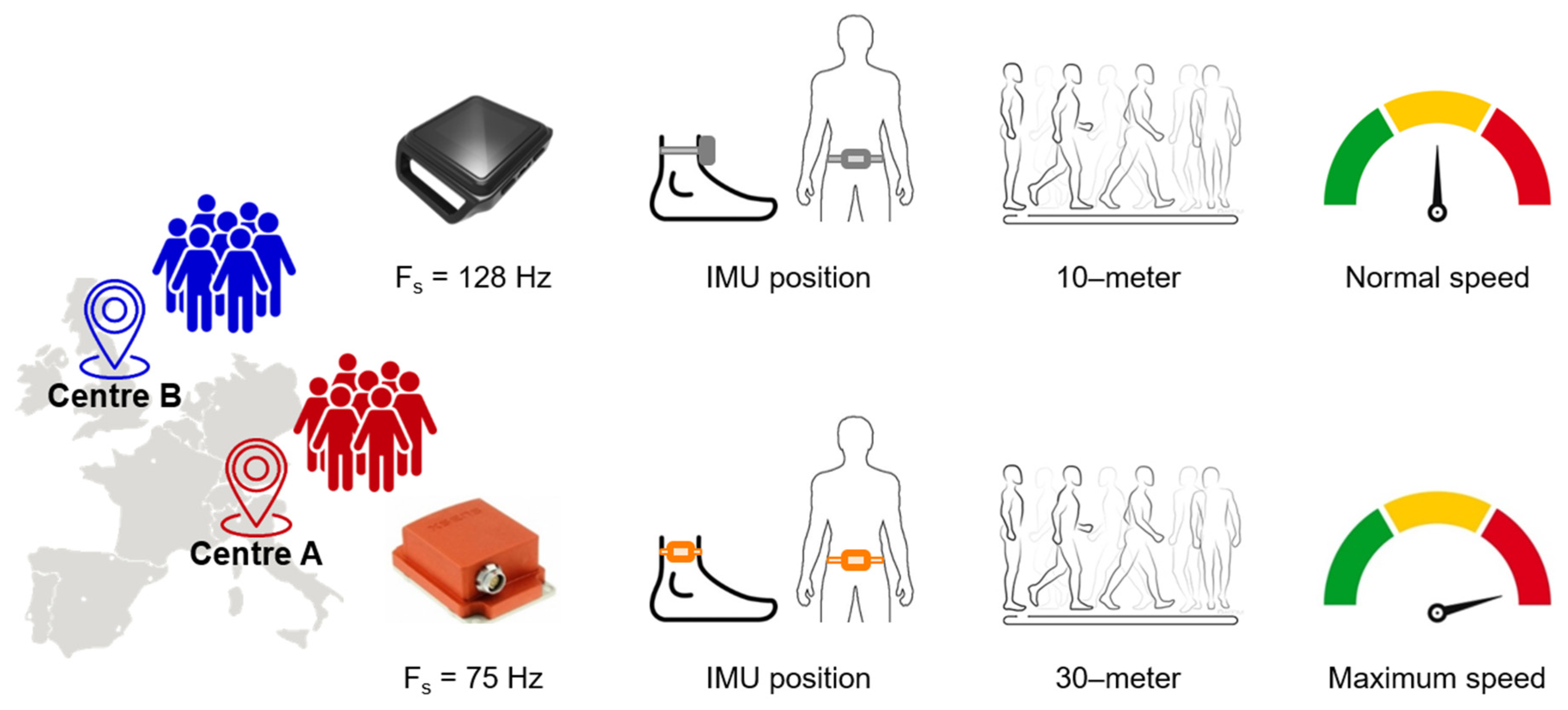
2.2. Experimental Protocol
2.3. Data Processing
2.4. Statistical Analysis
3. Results
3.1. Effect of Sampling Frequency
3.2. Between-Day Test-Retest Reliability
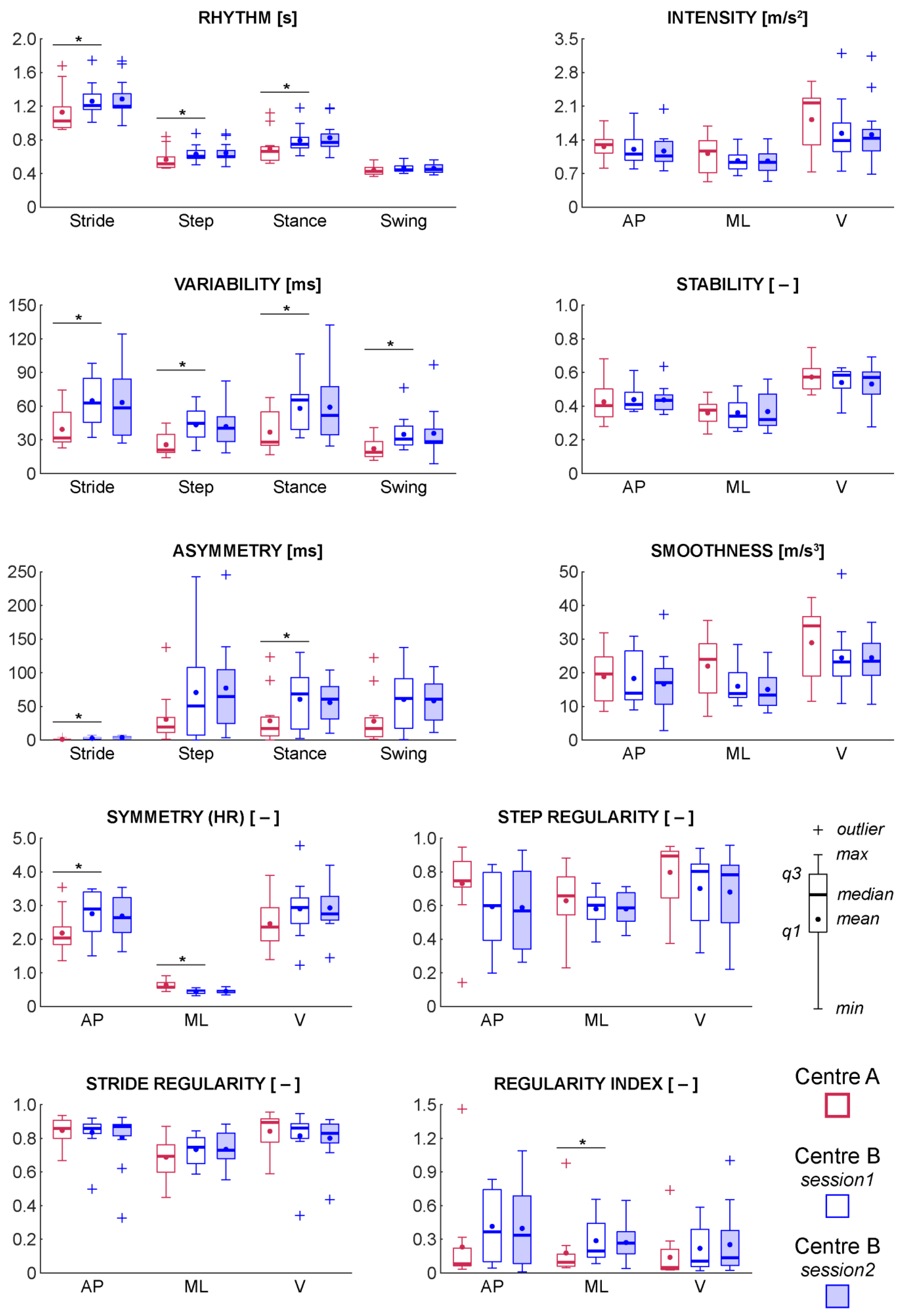
3.3. Between-Centre Differences
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Data Availability
References
- Browne, P.; Chandraratna, D.; Angood, C.; Tremlett, H.; Baker, C.; Taylor, B.V.; Thompson, A.J. Atlas of Multiple Sclerosis 2013: A growing global problem with widespread inequity. Neurology 2014, 83, 1022–1024. [Google Scholar] [CrossRef]
- Pugliatti, M.; Rosati, G.; Carton, H.; Riise, T.; Drulovic, J.; Vécsei, L.; Milanov, I. The epidemiology of multiple sclerosis in Europe. Eur. J. Neurol. 2006, 13, 700–722. [Google Scholar] [CrossRef]
- Cattaneo, D.; Lamers, I.; Bertoni, R.; Feys, P.; Jonsdottir, J. Participation Restriction in People with Multiple Sclerosis: Prevalence and Correlations With Cognitive, Walking, Balance, and Upper Limb Impairments. Arch. Phys. Med. Rehabil. 2017, 98, 1308–1315. [Google Scholar] [CrossRef]
- Martin, C.L.; Phillips, B.A.; Kilpatrick, T.J.; Butzkueven, H.; Tubridy, N.; McDonald, E.; Galea, M.P. Gait and balance impairment in early multiple sclerosis in the absence of clinical disability. Mult. Scler. J. 2006, 12, 620–628. [Google Scholar] [CrossRef]
- LaRocca, N.G. Impact of Walking Impairment in Multiple Sclerosis. Patient Patient-Cent. Outcomes Res. 2011, 4, 189–201. [Google Scholar] [CrossRef]
- Donzé, C. Update on rehabilitation in multiple sclerosis. La Presse Med. 2015, 44, e169–e176. [Google Scholar] [CrossRef]
- Kurtzke, J.F. Rating neurologic impairment in multiple sclerosis. Neurology 1983, 33, 1444. [Google Scholar] [CrossRef]
- Sebastião, E.; Sandroff, B.M.; Learmonth, Y.C.; Motl, R.W. Validity of the Timed Up and Go Test as a Measure of Functional Mobility in Persons with Multiple Sclerosis. Arch. Phys. Med. Rehabil. 2016, 97, 1072–1077. [Google Scholar] [CrossRef]
- Phan-Ba, R.; Pace, A.; Calay, P.; Grodent, P.; Douchamps, F.; Hyde, R.; Hotermans, C.; Delvaux, V.; Hansen, I.; Moonen, G.; et al. Comparison of the timed 25-foot and the 100-meter walk as performance measures in multiple sclerosis. Neurorehabil. Neural Repair. 2011, 25, 672–679. [Google Scholar] [CrossRef]
- Goldman, M.D.; Marrie, R.A.; Cohen, J.A. Evaluation of the six-minute walk in multiple sclerosis subjects and healthy controls. Mult. Scler. J. 2008, 14, 383–390. [Google Scholar] [CrossRef]
- Horak, F.; King, L.; Mancini, M. Role of body-worn movement monitor technology for balance and gait rehabilitation. Phys. Ther. 2015, 95, 461–470. [Google Scholar] [CrossRef]
- Kaufman, M.; Moyer, D.; Norton, J. The significant change for the Timed 25-Foot Walk in the Multiple Sclerosis Functional Composite. Mult. Scler. J. 2000, 6, 286–290. [Google Scholar] [CrossRef]
- Kragt, J.J.; van der Linden, F.A.; Nielsen, J.M.; Uitdehaag, B.M.; Polman, C.H. Clinical impact of 20% worsening on Timed 25-foot Walk and 9-hole Peg Test in multiple sclerosis. Mult. Scler. J. 2006, 12, 594–598. [Google Scholar] [CrossRef]
- Nieuwenhuis, M.M.; Van Tongeren, H.; Sorensen, P.S.; Ravnborg, M. The six spot step test: A new measurement for walking ability in multiple sclerosis. Mult. Scler. J. 2006, 12, 495–500. [Google Scholar] [CrossRef]
- Spain, R.I.; St. George, R.J.; Salarian, A.; Mancini, M.; Wagner, J.M.; Horak, F.B.; Bourdette, D. Body-worn motion sensors detect balance and gait deficits in people with multiple sclerosis who have normal walking speed. Gait Posture 2012, 35, 573–578. [Google Scholar] [CrossRef]
- Liparoti, M.; Della Corte, M.; Rucco, R.; Sorrentino, P.; Sparaco, M.; Capuano, R.; Minino, R.; Lavorgna, L.; Agosti, V.; Sorrentino, G.; et al. Gait abnormalities in minimally disabled people with Multiple Sclerosis: A 3D-motion analysis study. Mult. Scler. Relat. Disord. 2019, 29, 100–107. [Google Scholar] [CrossRef]
- Pau, M.; Mandaresu, S.; Pilloni, G.; Porta, M.; Coghe, G.; Marrosu, M.G.; Cocco, E. Smoothness of gait detects early alterations of walking in persons with multiple sclerosis without disability. Gait Posture 2017, 58, 307–309. [Google Scholar] [CrossRef]
- Muro-de-la-Herran, A.; Garcia-Zapirain, B.; Mendez-Zorrilla, A. Gait analysis methods: an overview of wearable and non-wearable systems, highlighting clinical applications. Sensors 2014, 14, 3362–3394. [Google Scholar] [CrossRef]
- Vienne-Jumeau, A.; Quijoux, F.; Vidal, P.P.; Ricard, D. Wearable inertial sensors provide reliable biomarkers of disease severity in multiple sclerosis: A systematic review and meta-analysis. Ann. Phys. Rehabil. Med. 2019. [Google Scholar] [CrossRef]
- Vienne, A.; Barrois, R.P.; Buffat, S.; Ricard, D.; Vidal, P.P. Inertial Sensors to Assess Gait Quality in Patients with Neurological Disorders: A Systematic Review of Technical and Analytical Challenges. Front. Psychology 2017, 8, 817. [Google Scholar] [CrossRef]
- Motl, R.W.; Pilutti, L.; Sandroff, B.M.; Dlugonski, D.; Sosnoff, J.J.; Pula, J.H. Accelerometry as a measure of walking behavior in multiple sclerosis. Acta Neurol. Scand. 2013, 127, 384–390. [Google Scholar] [CrossRef]
- Storm, F.A.; Nair, K.P.S.; Clarke, A.J.; Van der Meulen, J.M.; Mazzà, C. Free-living and laboratory gait characteristics in patients with multiple sclerosis. PLoS ONE 2018, 13, e0196463. [Google Scholar] [CrossRef]
- Huisinga, J.M.; Mancini, M.; St George, R.J.; Horak, F.B. Accelerometry reveals differences in gait variability between patients with multiple sclerosis and healthy controls. Ann. Biomed. Eng. 2013, 41, 1670–1679. [Google Scholar] [CrossRef]
- Moon, Y.; Wajda, D.A.; Motl, R.W.; Sosnoff, J.J. Stride-Time Variability and Fall Risk in Persons with Multiple Sclerosis. Mult. Scler. Int. 2015, 2015, 7. [Google Scholar] [CrossRef]
- Motta, C.; Palermo, E.; Studer, V.; Germanotta, M.; Germani, G.; Centonze, D.; Cappa, P.; Rossi, S.; Rossi, S. Disability and Fatigue Can Be Objectively Measured in Multiple Sclerosis. PLoS ONE 2016, 11, e0148997. [Google Scholar] [CrossRef]
- Engelhard, M.M.; Dandu, S.R.; Patek, S.D.; Lach, J.C.; Goldman, M.D. Quantifying six-minute walk induced gait deterioration with inertial sensors in multiple sclerosis subjects. Gait Posture 2016, 49, 340–345. [Google Scholar] [CrossRef]
- Psarakis, M.; Greene, D.A.; Cole, M.H.; Lord, S.R.; Hoang, P.; Brodie, M. Wearable technology reveals gait compensations, unstable walking patterns and fatigue in people with multiple sclerosis. Phys. Meas. 2018, 39, 075004. [Google Scholar] [CrossRef]
- Moon, Y.; McGinnis, R.S.; Seagers, K.; Motl, R.W.; Sheth, N.; Wright, J.A., Jr.; Ghaffari, R.; Sosnoff, J.J. Monitoring gait in multiple sclerosis with novel wearable motion sensors. PLoS ONE 2017, 12, e0171346. [Google Scholar] [CrossRef]
- Craig, J.J.; Bruetsch, A.P.; Lynch, S.G.; Huisinga, J.M. The relationship between trunk and foot acceleration variability during walking shows minor changes in persons with multiple sclerosis. Clin. Biomech. 2017, 49, 16–21. [Google Scholar] [CrossRef]
- Corporaal, S.H.A.; Gensicke, H.; Kuhle, J.; Kappos, L.; Allum, J.H.J.; Yaldizli, Ö. Balance control in multiple sclerosis: Correlations of trunk sway during stance and gait tests with disease severity. Gait Posture 2013, 37, 55–60. [Google Scholar] [CrossRef]
- Anastasi, D.; Carpinella, I.; Gervasoni, E.; Matsuda, P.N.; Bovi, G.; Ferrarin, M.; Cattaneo, D. Instrumented Version of the Modified Dynamic Gait Index in Patients with Neurologic Disorders. PM&R 2019. [Google Scholar] [CrossRef]
- Pau, M.; Corona, F.; Pilloni, G.; Porta, M.; Coghe, G.; Cocco, E. Texting while walking differently alters gait patterns in people with multiple sclerosis and healthy individuals. Mult. Scler. Relat. Disord. 2018, 19, 129–133. [Google Scholar] [CrossRef]
- Carpinella, I.; Gervasoni, E.; Anastasi, D.; Lencioni, T.; Cattaneo, D.; Ferrarin, M. Instrumental Assessment of Stair Ascent in People with Multiple Sclerosis, Stroke, and Parkinson’s Disease: A Wearable-Sensor-Based Approach. IEEE Trans. Neural Syst. Rehabil. Eng. 2018, 26, 2324–2332. [Google Scholar] [CrossRef]
- Craig, J.J.; Bruetsch, A.P.; Lynch, S.G.; Horak, F.B.; Huisinga, J.M. Instrumented balance and walking assessments in persons with multiple sclerosis show strong test-retest reliability. J. Neuroeng. Rehabil. 2017, 14, 43. [Google Scholar] [CrossRef]
- Riva, F.; Grimpampi, E.; Mazzà, C.; Stagni, R. Are gait variability and stability measures influenced by directional changes? Biomed. Eng. Online 2014, 13, 56. [Google Scholar] [CrossRef]
- Brønd, J.C.; Arvidsson, D. Sampling frequency affects the processing of Actigraph raw acceleration data to activity counts. J. Appl. Physiol. 2015, 120, 362–369. [Google Scholar] [CrossRef]
- England, S.A.; Granata, K.P. The influence of gait speed on local dynamic stability of walking. Gait Posture 2007, 25, 172–178. [Google Scholar] [CrossRef]
- Brodie, M.A.D.; Menz, H.B.; Lord, S.R. Age-associated changes in head jerk while walking reveal altered dynamic stability in older people. Exp. Brain Res. 2014, 232, 51–60. [Google Scholar] [CrossRef]
- Mazzà, C.; Iosa, M.; Pecoraro, F.; Cappozzo, A. Control of the upper body accelerations in young and elderly women during level walking. J. Neuroengineering Rehabil. 2008, 5, 30. [Google Scholar] [CrossRef]
- Brach, J.S.; McGurl, D.; Wert, D.; Vanswearingen, J.M.; Perera, S.; Cham, R.; Studenski, S. Validation of a measure of smoothness of walking. J. Gerontology. Ser. A Biol. Sci. Med. Sci. 2010, 66, 136–141. [Google Scholar] [CrossRef]
- Helbostad, J.L.; Moe-Nilssen, R. The effect of gait speed on lateral balance control during walking in healthy elderly. Gait Posture 2003, 18, 27–36. [Google Scholar] [CrossRef]
- Rabuffetti, M.; Scalera, M.G.; Ferrarin, M. Effects of Gait Strategy and Speed on Regularity of Locomotion Assessed in Healthy Subjects Using a Multi-Sensor Method. Sensors 2019, 19, 513. [Google Scholar] [CrossRef] [PubMed]
- Latt, M.D.; Menz, H.B.; Fung, V.S.; Lord, S.R. Walking speed, cadence and step length are selected to optimize the stability of head and pelvis accelerations. Exp. Brain Res. 2008, 184, 201–209. [Google Scholar] [CrossRef]
- Menz, H.B.; Lord, S.R.; Fitzpatrick, R.C. Acceleration patterns of the head and pelvis when walking on level and irregular surfaces. Gait Posture 2003, 18, 35–46. [Google Scholar] [CrossRef]
- Lowry, K.A.; Lokenvitz, N.; Smiley-Oyen, A.L. Age- and speed-related differences in harmonic ratios during walking. Gait Posture 2012, 35, 272–276. [Google Scholar] [CrossRef]
- Pecoraro, F.; Mazzà, C.; Cappozzo, A.; Thomas, E.E.; Macaluso, A. Reliability of the intrinsic and extrinsic patterns of level walking in older women. Gait Posture 2007, 26, 386–392. [Google Scholar] [CrossRef]
- Cappozzo, A. Analysis of the linear displacement of the head and trunk during walking at different speeds. J. Biomech. 1981, 14, 411–425. [Google Scholar] [CrossRef]
- Moe-Nilssen, R. A new method for evaluating motor control in gait under real-life environmental conditions. Part 1: The instrument. Clin. Biomech. 1998, 13, 320–327. [Google Scholar] [CrossRef]
- Salarian, A.; Horak, F.B.; Zampieri, C.; Carlson-Kuhta, P.; Nutt, J.G.; Aminian, K. iTUG, a Sensitive and Reliable Measure of Mobility. IEEE Trans. Neural Syst. Rehabil. Eng. 2010, 18, 303–310. [Google Scholar] [CrossRef]
- Killick, R.; Fearnhead, P.; Eckley, I.A. Optimal Detection of Changepoints With a Linear Computational Cost. J. Am. Stat. Assoc. 2012, 107, 1590–1598. [Google Scholar] [CrossRef]
- Palmerini, L.; Rocchi, L.; Mazilu, S.; Gazit, E.; Hausdorff, J.M.; Chiari, L. Identification of Characteristic Motor Patterns Preceding Freezing of Gait in Parkinson’s Disease Using Wearable Sensors. Front. Neurol. 2017, 8, 394. [Google Scholar] [CrossRef] [PubMed]
- Lord, S.; Galna, B.; Rochester, L. Moving forward on gait measurement: toward a more refined approach. Movement Disorders 2013, 28, 1534–1543. [Google Scholar] [CrossRef] [PubMed]
- Buckley, C.; Galna, B.; Rochester, L.; Mazzà, C. Upper body accelerations as a biomarker of gait impairment in the early stages of Parkinson’s disease. Gait Posture 2019, 71, 289–295. [Google Scholar] [CrossRef] [PubMed]
- Salarian, A.; Russmann, H.; Vingerhoets, F.J.; Dehollain, C.; Blanc, Y.; Burkhard, P.R.; Aminian, K. Gait assessment in Parkinson’s disease: toward an ambulatory system for long-term monitoring. IEEE Trans. Biomed. Eng. 2004, 51, 1434–1443. [Google Scholar] [CrossRef] [PubMed]
- Galna, B.; Lord, S.; Rochester, L. Is gait variability reliable in older adults and Parkinson’s disease? Towards an optimal testing protocol. Gait Posture 2013, 37, 580–585. [Google Scholar] [CrossRef]
- Godfrey, A.; Del Din, S.; Barry, G.; Mathers, J.C.; Rochester, L. Instrumenting gait with an accelerometer: A system and algorithm examination. Med. Eng. Phys. 2015, 37, 400–407. [Google Scholar] [CrossRef]
- Pasciuto, I.; Bergamini, E.; Iosa, M.; Vannozzi, G.; Cappozzo, A. Overcoming the limitations of the Harmonic Ratio for the reliable assessment of gait symmetry. J. Biomech. 2017, 53, 84–89. [Google Scholar] [CrossRef]
- Sekine, M.; Tamura, T.; Yoshida, M.; Suda, Y.; Kimura, Y.; Miyoshi, H.; Kijima, Y.; Higashi, Y.; Fujimoto, T. A gait abnormality measure based on root mean square of trunk acceleration. J. Neuroeng. Rehabil. 2013, 10, 118. [Google Scholar] [CrossRef]
- Fazio, P.; Granieri, G.; Casetta, I.; Cesnik, E.; Mazzacane, S.; Caliandro, P.; Pedrielli, F.; Granieri, E. Gait measures with a triaxial accelerometer among patients with neurological impairment. Neurol. Sci. 2013, 34, 435–440. [Google Scholar] [CrossRef]
- Gage, S.H. Microscopy in America (1830–1945). Trans. Am. Microsc. Soc. 1964, 83, 1–125. [Google Scholar] [CrossRef]
- Smidt, G.L.; Arora, J.S.; Johnston, R.C. Accelerographic analysis of several types of walking. Am. J. Phys. Med. Rehabil. 1971, 50, 285–300. [Google Scholar]
- Moe-Nilssen, R.; Helbostad, J.L. Estimation of gait cycle characteristics by trunk accelerometry. J. Biomech. 2004, 37, 121–126. [Google Scholar] [CrossRef]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria; Available online: http://cran.fhcrc.org/web/packages/dplR/vignettes/intro-dplR.pdf (accessed on 20 December 2019).
- Li, L.; Zeng, L.; Lin, Z.-J.; Cazzell, M.; Liu, H. Tutorial on use of intraclass correlation coefficients for assessing intertest reliability and its application in functional near-infrared spectroscopy–based brain imaging. J. Biomed. Opt. 2015, 20, 050801. [Google Scholar] [CrossRef] [PubMed]
- Cicchetti, D.V. Methodological Commentary The Precision of Reliability and Validity Estimates Re-Visited: Distinguishing Between Clinical and Statistical Significance of Sample Size Requirements. J. Clin. Exp. Neuropsychology 2001, 23, 695–700. [Google Scholar] [CrossRef]
- Almarwani, M.; Perera, S.; VanSwearingen, J.M.; Sparto, P.J.; Brach, J.S. The test–retest reliability and minimal detectable change of spatial and temporal gait variability during usual over-ground walking for younger and older adults. Gait Posture 2016, 44, 94–99. [Google Scholar] [CrossRef]
- Cohen, J. CHAPTER 3—The Significance of a Product Moment rs. In Statistical Power Analysis for the Behavioral Sciences; Available online: http://www.utstat.toronto.edu/~brunner/oldclass/378f16/readings/CohenPower.pdf (accessed on 20 December 2019).
- Compston, A.; Coles, A. Multiple sclerosis. Lancet 2008, 372, 1502–1517. [Google Scholar] [CrossRef]
- Dujmovic, I.; Radovanovic, S.; Martinovic, V.; Dackovic, J.; Maric, G.; Mesaros, S.; Pekmezovic, T.; Kostic, V.; Drulovic, J. Gait pattern in patients with different multiple sclerosis phenotypes. Mult. Scler. Relat. Disord. 2017, 13, 13–20. [Google Scholar] [CrossRef]
- Cole, M.H.; Sweeney, M.; Conway, Z.J.; Blackmore, T.; Silburn, P.A. Imposed Faster and Slower Walking Speeds Influence Gait Stability Differently in Parkinson Fallers. Arch. Phys. Med. Rehabil. 2017, 98, 639–648. [Google Scholar] [CrossRef]
- Riva, F.; Bisi, M.C.; Stagni, R. Gait variability and stability measures: Minimum number of strides and within-session reliability. Comput. Biol. Med. 2014, 50, 9–13. [Google Scholar] [CrossRef]
- Shema-Shiratzky, S.; Gazit, E.; Sun, R.; Regev, K.; Karni, A.; Sosnoff, J.J.; Herman, T.; Mirelman, A.; Hausdorff, J.M. Deterioration of specific aspects of gait during the instrumented 6-min walk test among people with multiple sclerosis. J. Neurol. 2019, 266, 3022–3030. [Google Scholar] [CrossRef]
| Centre A (n = 13) | Centre B (n = 13) | Statistics | |
|---|---|---|---|
| Age [years] | 51 (35–63) | 57 (34–64) | U = 58, p = 0.18 |
| Gender [men/women] | 3/10 | 3/10 | X2(1) = 0.00, p = 1.00 |
| EDSS score (0–10) | 4.5 (2.0–6.5) | 4.5 (2.5–6.5) | U = 83, p = 0.93 |
| Mild (2.0–2.5) | 1 | 1 | |
| Moderate (3.0–4.5) | 6 | 6 | |
| Severe (5.0–6.5) | 6 | 6 | |
| Assistive devices | |||
| Walker | 1 pwMS | 1 pwMS | – |
| Cane | 2 pwMS | 2 pwMS | – |
| Walking speed [m/s] | 1.1 (0.5–1.4) | 0.7 (0.4–1.0) | U = 31, p < 0.01 * |
| Domain | Fs of 128 Hz | Fs of 75 Hz | z | p | r |
|---|---|---|---|---|---|
| Rhythm [s] | |||||
| Stride duration | 1.20 (1.01–1.74) | 1.21 (1.01–1.74) | −0.82 | 0.41 | −0.16 |
| Step duration | 0.60 (0.51–0.87) | 0.60 (0.50–0.87) | 0.00 | 1.00 | 0.00 |
| Stance duration | 0.75 (0.61–1.18) | 0.75 (0.61–1.18) | −1.83 | 0.07 | −0.36 |
| Swing duration | 0.44 (0.40–0.58) | 0.44 (0.40–0.58) | −1.85 | 0.06 | −0.36 |
| Variability [ms] | |||||
| Stride duration | 61 (32–100) | 63 (32–98) | −1.55 | 0.12 | −0.30 |
| Step duration | 46 (20–69) | 45 (20–68) | −1.33 | 0.18 | −0.26 |
| Stance duration | 65 (34–105) | 65 (32–106) | −0.18 | 0.86 | −0.04 |
| Swing duration | 29 (23–74) | 30 (21–76) | −0.41 | 0.68 | −0.08 |
| Asymmetry [ms] | |||||
| Stride duration | 2 (0–7) | 2 (1–7) | −0.09 | 0.93 | −0.02 |
| Step duration | 56 (0–238) | 51 (0–242) | −1.49 | 0.14 | −0.29 |
| Stance duration | 61 (3–149) | 69 (2–130) | −1.58 | 0.11 | −0.31 |
| Swing duration | 54 (1–155) | 62 (0–138) | −1.33 | 0.18 | −0.26 |
| Intensity [m/s2] | |||||
| Antero-Posterior | 1.10 (0.80–1.96) | 1.10 (0.80–1.95) | −0.94 | 0.34 | −0.19 |
| Medio-Lateral | 0.93 (0.65–1.41) | 0.93 (0.65–1.41) | −1.44 | 0.15 | −0.28 |
| Vertical | 1.37 (0.76–3.16) | 1.38 (0.75–3.20) | −1.28 | 0.20 | −0.25 |
| Stability [–] | |||||
| Antero-Posterior | 0.41 (0.37–0.61) | 0.41 (0.37–0.61) | −0.30 | 0.77 | −0.06 |
| Medio-Lateral | 0.34 (0.25–0.52) | 0.34 (0.25–0.52) | −0.89 | 0.37 | −0.18 |
| Vertical | 0.58 (0.36–0.62) | 0.58 (0.36–0.63) | −0.29 | 0.77 | −0.06 |
| Smoothness [m/s3] | |||||
| Antero-Posterior | 13.97 (8.86–30.75) | 13.95 (8.93–30.82) | 0.00 | 1.00 | 0.00 |
| Medio-Lateral | 13.92 (10.13–28.61) | 13.87 (10.19–28.45) | −1.06 | 0.29 | −0.21 |
| Vertical | 23.31 (11.06–48.81) | 23.21 (10.89–49.38) | −0.75 | 0.45 | −0.15 |
| Symmetry (HR) [–] | |||||
| Antero-Posterior | 2.94 (1.49–3.73) | 2.89 (1.50–3.49) | −2.32 | 0.02 * | −0.45 |
| Medio-Lateral | 0.44 (0.32–0.56) | 0.45 (0.32–0.56) | −2.19 | 0.03 * | −0.43 |
| Vertical | 3.01 (1.21–4.84) | 2.94 (1.23–4.78) | −3.01 | 0.00 * | −0.59 |
| Regularity [–] | |||||
| Step regularity | |||||
| Antero-Posterior | 0.60 (0.20–0.85) | 0.60 (0.20–0.84) | −1.70 | 0.09 | −0.33 |
| Medio-Lateral | −0.62 (−0.74–−0.37) | −0.60 (−0.73–−0.38) | −1.89 | 0.06 | −0.37 |
| Vertical | 0.81 (0.32–0.95) | 0.80 (0.32–0.94) | −1.44 | 0.15 | −0.28 |
| Stride regularity | |||||
| Anterior-Posterior | 0.86 (0.50–0.93) | 0.86 (0.50–0.92) | 0.00 | 1.00 | 0.00 |
| Medio-Lateral | 0.77 (0.58–0.85) | 0.75 (0.59–0.85) | −1.67 | 0.09 | −0.33 |
| Vertical | 0.86 (0.34–0.95) | 0.86 (0.34–0.95) | −1.80 | 0.07 | −0.35 |
| Regularity index | |||||
| Antero-Posterior | 0.37 (0.04–0.82) | 0.37 (0.04–0.83) | −1.10 | 0.27 | −0.22 |
| Medio-Lateral | −0.20 (−0.70–−0.08) | −0.20 (−0.66–−0.08) | −0.41 | 0.68 | −0.08 |
| Vertical | 0.11 (0.02–0.59) | 0.11 (0.02–0.59) | 0.00 | 1.00 | 0.00 |
| Domains | ICC | 95% CI | SEM | MDC | |
|---|---|---|---|---|---|
| Lower | Upper | ||||
| Rhythm [s] | |||||
| Stride duration | 0.97 | 0.90 | 0.99 | 0.04 | 0.10 |
| Step duration | 0.97 | 0.90 | 0.99 | 0.02 | 0.05 |
| Stance duration | 0.96 | 0.86 | 0.99 | 0.03 | 0.09 |
| Swing duration | 0.97 | 0.91 | 0.99 | 0.01 | 0.03 |
| Variability [ms] | |||||
| Stride duration | 0.92 | 0.73 | 0.97 | 8 | 21 |
| Step duration | 0.92 | 0.74 | 0.98 | 5 | 13 |
| Stance duration | 0.94 | 0.80 | 0.98 | 6 | 18 |
| Swing duration | 0.95 | 0.85 | 0.99 | 4 | 11 |
| Asymmetry [ms] | |||||
| Stride duration | 0.72 | 0.13 | 0.91 | 1 | 4 |
| Step duration | 0.98 | 0.93 | 0.99 | 10 | 29 |
| Stance duration | 0.90 | 0.67 | 0.97 | 12 | 33 |
| Swing duration | 0.89 | 0.62 | 0.97 | 13 | 36 |
| Intensity [m/s2] | |||||
| Antero-Posterior | 0.97 | 0.90 | 0.99 | 0.06 | 0.16 |
| Medio-Lateral | 0.98 | 0.93 | 0.99 | 0.04 | 0.11 |
| Vertical | 0.97 | 0.92 | 0.99 | 0.10 | 0.29 |
| Stability [–] | |||||
| Antero-Posterior | 0.93 | 0.78 | 0.98 | 0.02 | 0.05 |
| Medio-Lateral | 0.93 | 0.76 | 0.98 | 0.03 | 0.08 |
| Vertical | 0.91 | 0.69 | 0.97 | 0.03 | 0.09 |
| Smoothness [m/s3] | |||||
| Antero-Posterior | 0.92 | 0.73 | 0.97 | 2.46 | 6.83 |
| Medio-Lateral | 0.93 | 0.79 | 0.98 | 1.55 | 4.29 |
| Vertical | 0.95 | 0.82 | 0.98 | 2.31 | 6.41 |
| Symmetry (HR) [–] | |||||
| Antero-Posterior | 0.95 | 0.85 | 0.99 | 0.14 | 0.38 |
| Medio-Lateral | 0.75 | 0.15 | 0.92 | 0.04 | 0.10 |
| Vertical | 0.92 | 0.74 | 0.98 | 0.21 | 0.59 |
| Regularity [–] | |||||
| Step regularity | |||||
| Antero-Posterior | 0.91 | 0.70 | 0.97 | 0.07 | 0.19 |
| Medio-Lateral | 0.86 | 0.52 | 0.96 | 0.04 | 0.11 |
| Vertical | 0.97 | 0.92 | 0.99 | 0.04 | 0.10 |
| Stride regularity | |||||
| Antero-Posterior | 0.88 | 0.64 | 0.96 | 0.05 | 0.13 |
| Medio-Lateral | 0.85 | 0.50 | 0.96 | 0.04 | 0.10 |
| Vertical | 0.93 | 0.77 | 0.98 | 0.04 | 0.10 |
| Regularity index | |||||
| Antero-Posterior | 0.76 | 0.17 | 0.93 | 0.17 | 0.47 |
| Medio-Lateral | 0.88 | 0.62 | 0.96 | 0.06 | 0.17 |
| Vertical | 0.89 | 0.63 | 0.97 | 0.09 | 0.24 |
| Domain | Centre B (session1) | Centre B (session2) | z | p | r |
|---|---|---|---|---|---|
| Rhythm [s] | |||||
| Stride duration | 1.21 (1.01–1.74) | 1.20 (0.97–1.74) | −0.70 | 0.48 | −0.14 |
| Step duration | 0.60 (0.50–0.87) | 0.60 (0.48–0.87) | −0.56 | 0.58 | −0.11 |
| Stance duration | 0.75 (0.61–1.18) | 0.77 (0.59–1.18) | −1.57 | 0.12 | −0.31 |
| Swing duration | 0.44 (0.40–0.58) | 0.45 (0.38–0.56) | −1.99 | 0.05 | −0.39 |
| Variability [ms] | |||||
| Stride duration | 63 (32–98) | 58 (27–124) | −0.35 | 0.72 | −0.07 |
| Step duration | 45 (20–68) | 40 (18–83) | −0.35 | 0.72 | −0.07 |
| Stance duration | 65 (32–106) | 52 (24–132) | −0.03 | 0.97 | −0.01 |
| Swing duration | 30 (21–76) | 28 (9–97) | −0.53 | 0.60 | −0.10 |
| Asymmetry [ms] | |||||
| Stride duration | 2 (1–7) | 4 (0–7) | −1.34 | 0.18 | −0.26 |
| Step duration | 51 (0–242) | 65 (4–245) | −1.30 | 0.20 | −0.25 |
| Stance duration | 69 (2–130) | 61 (10–104) | −0.52 | 0.60 | −0.10 |
| Swing duration | 62 (0–138) | 61 (12–109) | −0.38 | 0.70 | −0.08 |
| Intensity [m/s2] | |||||
| Antero-Posterior | 1.10 (0.80–1.95) | 1.07 (0.76–2.04) | −1.22 | 0.22 | −0.24 |
| Medio-Lateral | 0.93 (0.65–1.41) | 0.93 (0.53–1.42) | −0.08 | 0.94 | −0.02 |
| Vertical | 1.38 (0.75–3.20) | 1.43 (0.68–3.14) | −0.38 | 0.70 | −0.08 |
| Stability [–] | |||||
| Antero-Posterior | 0.41 (0.37–0.61) | 0.43 (0.35–0.64) | −0.28 | 0.78 | −0.05 |
| Medio-Lateral | 0.34 (0.25–0.52) | 0.32 (0.24–0.56) | 0.00 | 1.00 | 0.00 |
| Vertical | 0.58 (0.36–0.63) | 0.57 (0.28–0.69) | −0.27 | 0.79 | −0.05 |
| Smoothness [m/s3] | |||||
| Antero-Posterior | 13.95 (8.93–30.82) | 17.11 (2.76–37.32) | −1.17 | 0.24 | −0.23 |
| Medio-Lateral | 13.87 (10.19–28.45) | 13.42 (8.04–26.07) | −1.24 | 0.22 | −0.24 |
| Vertical | 23.21 (10.89–49.38) | 23.43 (10.67–50.74) | −0.41 | 0.68 | −0.08 |
| Symmetry (HR) [–] | |||||
| Antero-Posterior | 2.89 (1.50–3.49) | 2.64 (1.62–3.54) | −0.31 | 0.75 | −0.06 |
| Medio-Lateral | 0.45 (0.32–0.56) | 0.46 (0.34–0.59) | −0.82 | 0.41 | −0.16 |
| Vertical | 2.94 (1.23–4.78) | 2.75 (1.45–4.19) | −0.51 | 0.61 | −0.10 |
| Regularity [–] | |||||
| Step regularity | |||||
| Antero-Posterior | 0.60 (0.20–0.84) | 0.57 (0.26–0.93) | −0.12 | 0.91 | −0.02 |
| Medio-Lateral | −0.60 (−0.73–−0.38) | −0.58 (−0.71–−0.42) | −0.07 | 0.94 | −0.01 |
| Vertical | 0.80 (0.32–0.94) | 0.78 (0.22–0.96) | −1.26 | 0.21 | −0.25 |
| Stride regularity | |||||
| Anterior-Posterior | 0.86 (0.50–0.92) | 0.87 (0.33–0.92) | −0.98 | 0.33 | −0.19 |
| Medio-Lateral | 0.75 (0.59–0.85) | 0.73 (0.55–0.88) | −0.03 | 0.97 | −0.01 |
| Vertical | 0.86 (0.34–0.95) | 0.83 (0.44–0.91) | −0.52 | 0.60 | −0.10 |
| Regularity index | |||||
| Antero-Posterior | 0.37 (0.04–0.83) | 0.34 (0.01–1.09) | −0.04 | 0.97 | −0.01 |
| Medio-Lateral | −0.20 (−0.66–−0.08) | −0.27 (−0.65–−0.04) | −0.14 | 0.89 | −0.03 |
| Vertical | 0.11 (0.02–0.59) | 0.14 (0.02–1.00) | −0.43 | 0.67 | −0.08 |
| Domain | Centre A | Centre B | U | p | r |
|---|---|---|---|---|---|
| Rhythm [s] | |||||
| Stride duration | 1.03 (0.92–1.68) | 1.21 (1.01–1.74) | 43.5 | 0.04 * | 0.41 |
| Step duration | 0.51 (0.46–0.84) | 0.60 (0.50–0.87) | 44.0 | 0.04 * | 0.41 |
| Stance duration | 0.66 (0.52–1.12) | 0.75 (0.61–1.18) | 40.0 | 0.02 * | 0.45 |
| Swing duration | 0.43 (0.37–0.56) | 0.44 (0.40–0.58) | 57.0 | 0.17 | 0.28 |
| Variability [ms] | |||||
| Stride duration | 32 (23–74) | 63 (32–98) | 26.0 | 0.00 * | 0.59 |
| Step duration | 21 (14–45) | 45 (20–68) | 27.5 | 0.00 * | 0.57 |
| Stance duration | 28 (17–68) | 65 (32–106) | 30.0 | 0.01 * | 0.55 |
| Swing duration | 19 (12–41) | 30 (21–76) | 33.0 | 0.01 * | 0.52 |
| Asymmetry [ms] | |||||
| Stride duration | 1 (0–4) | 2 (1–7) | 45.0 | 0.04 * | 0.40 |
| Step duration | 19 (1–138) | 51 (0–242) | 68.0 | 0.40 | 0.17 |
| Stance duration | 17 (0–123) | 69 (2–130) | 46.0 | 0.04 * | 0.39 |
| Swing duration | 17 (1–122) | 62 (0–138) | 48.0 | 0.06 | 0.37 |
| Intensity [m/s2] | |||||
| Antero-Posterior | 1.30 (0.81–1.80) | 1.10 (0.80–1.95) | 68.0 | 0.41 | 0.17 |
| Medio-Lateral | 1.17 (0.53–1.69) | 0.93 (0.65–1.41) | 62.0 | 0.26 | 0.23 |
| Vertical | 2.17 (0.73–2.62) | 1.38 (0.75–3.20) | 59.5 | 0.21 | 0.25 |
| Stability [–] | |||||
| Antero-Posterior | 0.40 (0.28–0.68) | 0.41 (0.37–0.61) | 69.0 | 0.44 | 0.16 |
| Medio-Lateral | 0.38 (0.23–0.48) | 0.34 (0.25–0.52) | 83.0 | 0.96 | 0.02 |
| Vertical | 0.57 (0.47–0.75) | 0.58 (0.36–0.63) | 72.5 | 0.55 | 0.12 |
| Smoothness [m/s3] | |||||
| Antero-Posterior | 19.68 (8.56–31.85) | 13.95 (8.93–30.82) | 82.0 | 0.92 | 0.03 |
| Medio-Lateral | 24.01 (7.04–35.54) | 13.87 (10.19–28.45) | 52.5 | 0.11 | 0.32 |
| Vertical | 33.90 (11.56–42.39) | 23.21 (10.89–49.38) | 59.0 | 0.20 | 0.26 |
| Symmetry (HR) [–] | |||||
| Antero-Posterior | 2.04 (1.36–3.54) | 2.89 (1.50–3.49) | 43.5 | 0.04 * | 0.41 |
| Medio-Lateral | 0.57 (0.44–0.91) | 0.45 (0.32–0.56) | 14.0 | 0.00 * | 0.71 |
| Vertical | 2.35 (1.39–3.89) | 2.94 (1.23–4.78) | 52.5 | 0.11 | 0.32 |
| Regularity [–] | |||||
| Step regularity | |||||
| Antero-Posterior | 0.75 (0.14–0.95) | 0.60 (0.20–0.84) | 55.5 | 0.14 | 0.29 |
| Medio-Lateral | −0.66 (−0.88–−0.23) | −0.60 (−0.73–−0.38) | 63.0 | 0.28 | 0.22 |
| Vertical | 0.89 (0.37–0.95) | 0.80 (0.32–0.94) | 51.5 | 0.10 | 0.33 |
| Stride regularity | |||||
| Anterior-Posterior | 0.86 (0.67–0.93) | 0.86 (0.50–0.92) | 81.5 | 0.90 | 0.03 |
| Medio-Lateral | 0.69 (0.45–0.87) | 0.75 (0.59–0.85) | 63.0 | 0.28 | 0.22 |
| Vertical | 0.89 (0.59–0.96) | 0.86 (0.34–0.95) | 72.5 | 0.55 | 0.12 |
| Regularity index | |||||
| Antero-Posterior | 0.08 (0.03–1.46) | 0.37 (0.04–0.83) | 50.0 | 0.08 | 0.35 |
| Medio-Lateral | −0.10 (−0.98–−0.05) | −0.20 (−0.66–−0.08) | 40.5 | 0.03 * | 0.44 |
| Vertical | 0.05 (0.02–0.74) | 0.11 (0.02–0.59) | 51.5 | 0.09 | 0.33 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Angelini, L.; Carpinella, I.; Cattaneo, D.; Ferrarin, M.; Gervasoni, E.; Sharrack, B.; Paling, D.; Nair, K.P.S.; Mazzà, C. Is a Wearable Sensor-Based Characterisation of Gait Robust Enough to Overcome Differences Between Measurement Protocols? A Multi-Centric Pragmatic Study in Patients with Multiple Sclerosis. Sensors 2020, 20, 79. https://doi.org/10.3390/s20010079
Angelini L, Carpinella I, Cattaneo D, Ferrarin M, Gervasoni E, Sharrack B, Paling D, Nair KPS, Mazzà C. Is a Wearable Sensor-Based Characterisation of Gait Robust Enough to Overcome Differences Between Measurement Protocols? A Multi-Centric Pragmatic Study in Patients with Multiple Sclerosis. Sensors. 2020; 20(1):79. https://doi.org/10.3390/s20010079
Chicago/Turabian StyleAngelini, Lorenza, Ilaria Carpinella, Davide Cattaneo, Maurizio Ferrarin, Elisa Gervasoni, Basil Sharrack, David Paling, Krishnan Padmakumari Sivaraman Nair, and Claudia Mazzà. 2020. "Is a Wearable Sensor-Based Characterisation of Gait Robust Enough to Overcome Differences Between Measurement Protocols? A Multi-Centric Pragmatic Study in Patients with Multiple Sclerosis" Sensors 20, no. 1: 79. https://doi.org/10.3390/s20010079
APA StyleAngelini, L., Carpinella, I., Cattaneo, D., Ferrarin, M., Gervasoni, E., Sharrack, B., Paling, D., Nair, K. P. S., & Mazzà, C. (2020). Is a Wearable Sensor-Based Characterisation of Gait Robust Enough to Overcome Differences Between Measurement Protocols? A Multi-Centric Pragmatic Study in Patients with Multiple Sclerosis. Sensors, 20(1), 79. https://doi.org/10.3390/s20010079







