Wearable Cardiopulmonary Function Evaluation System for Six-Minute Walking Test
Abstract
1. Background
2. Related Work
3. Motivation
4. System Design and Implementation
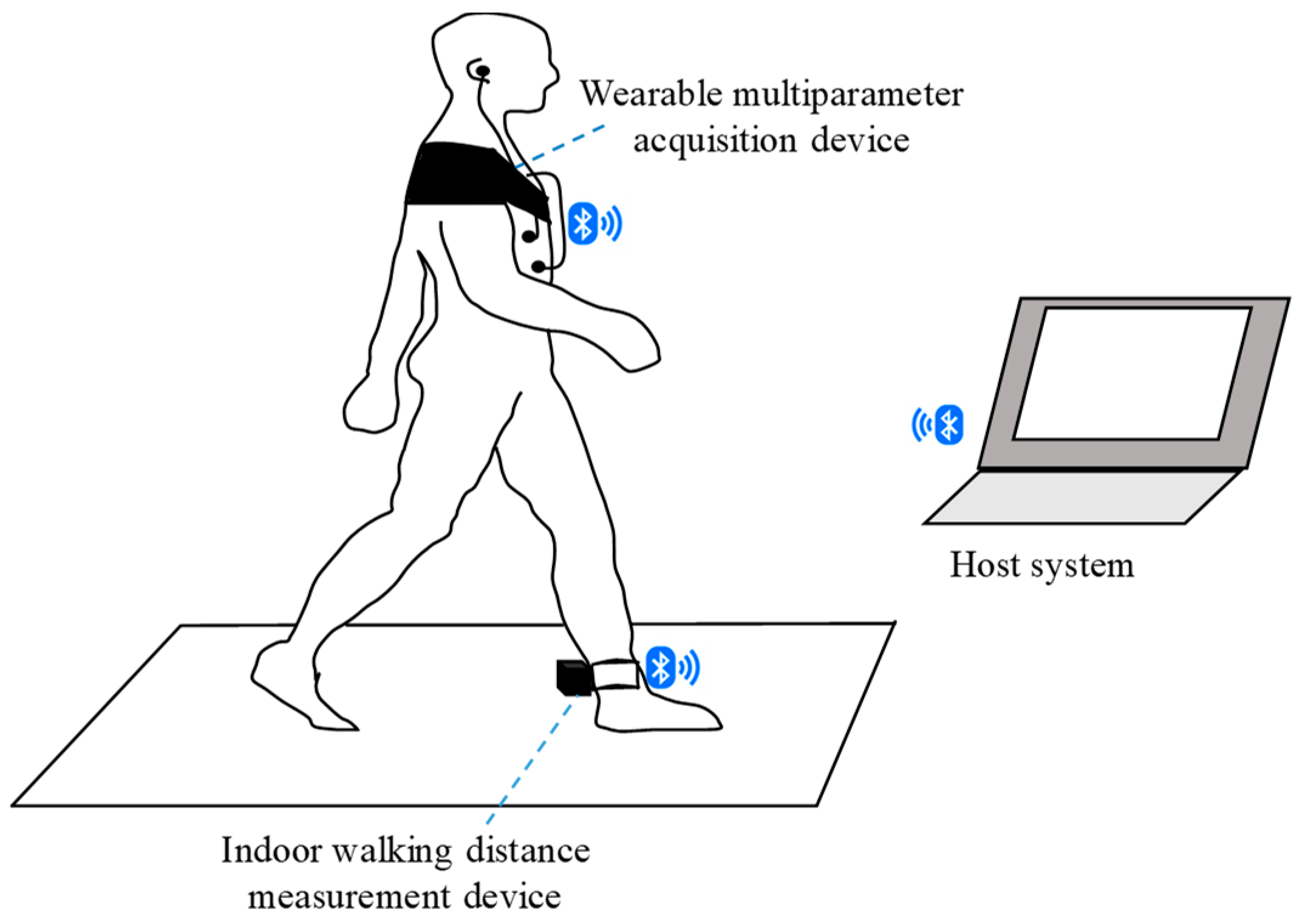
4.1. System Architecture
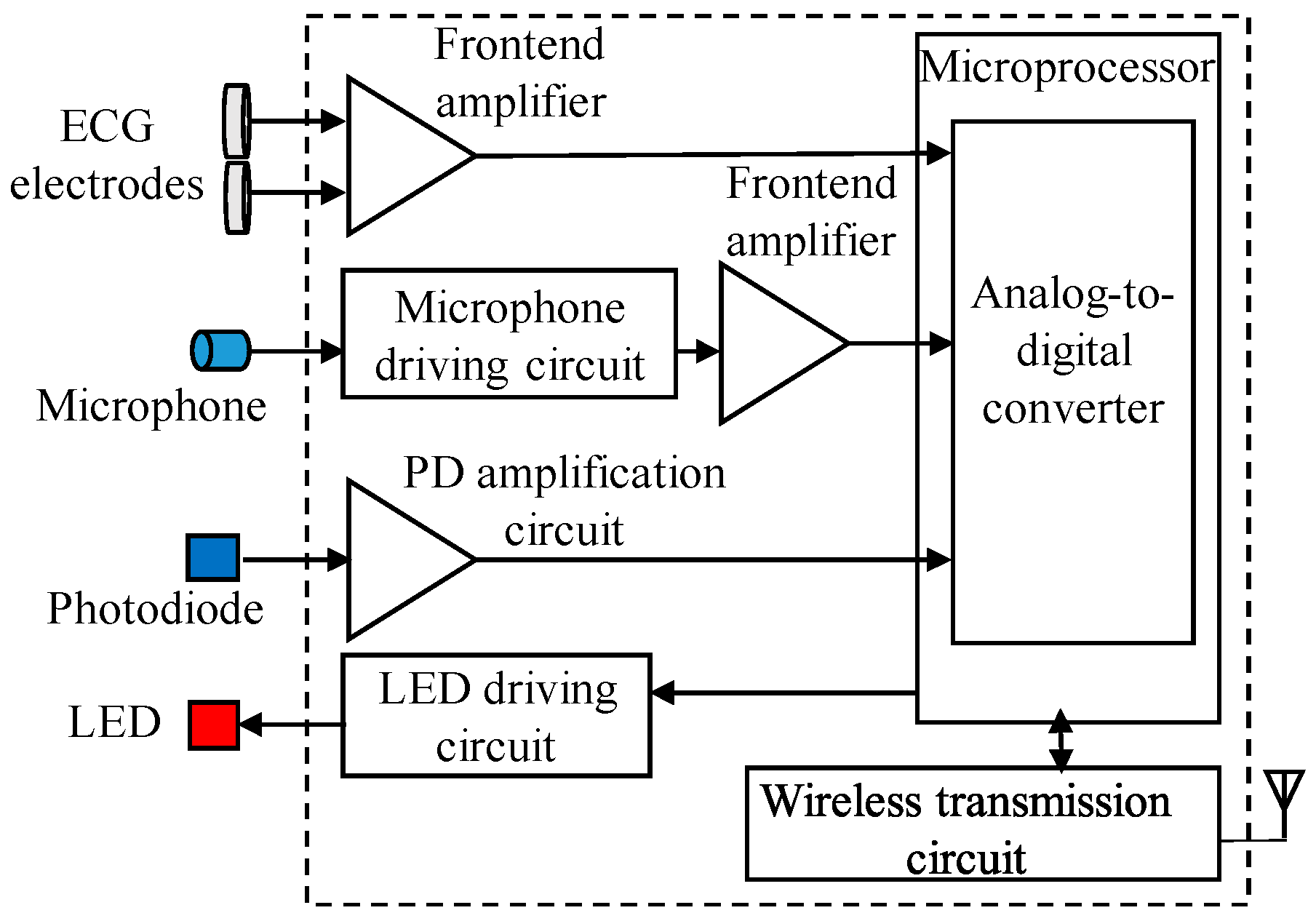
4.2. Wearable Multiparameter Acquisition Device
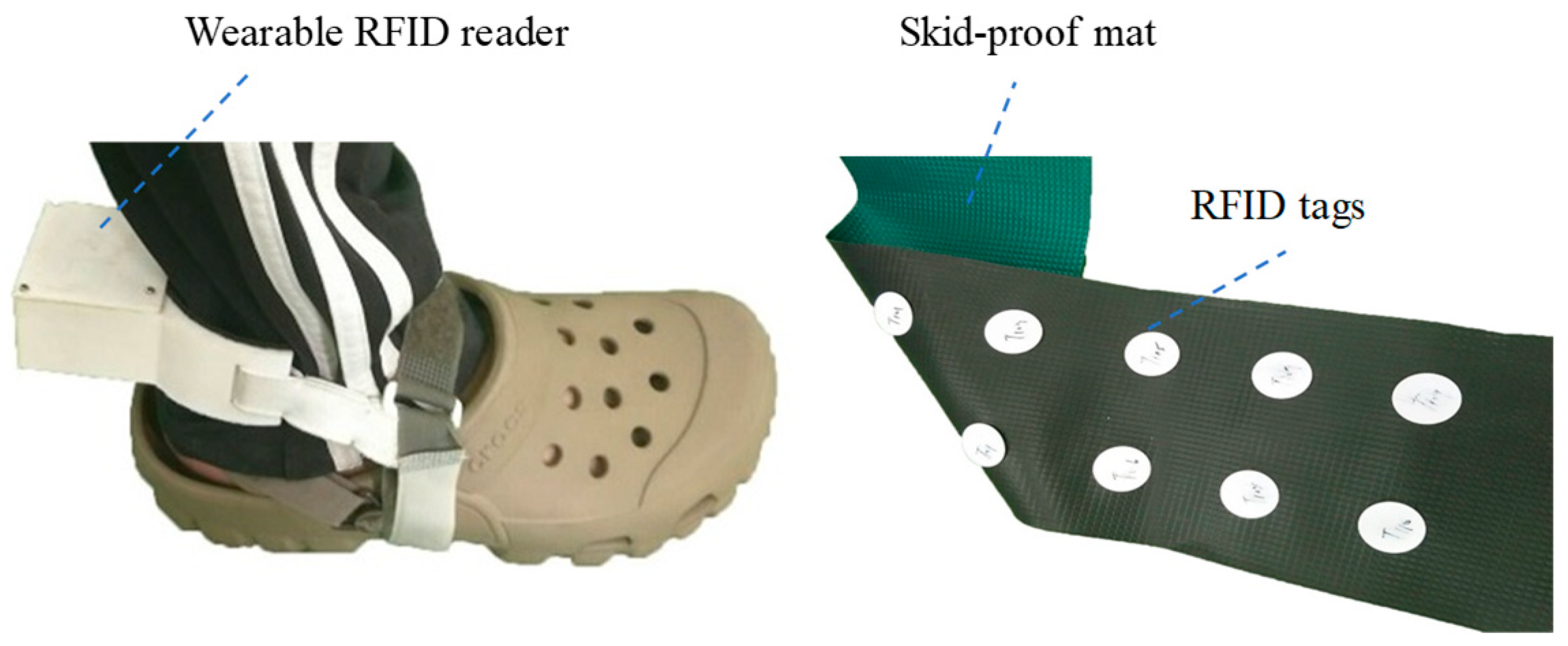
4.3. Indoor Walking Distance Measurement Device
4.4. Host System
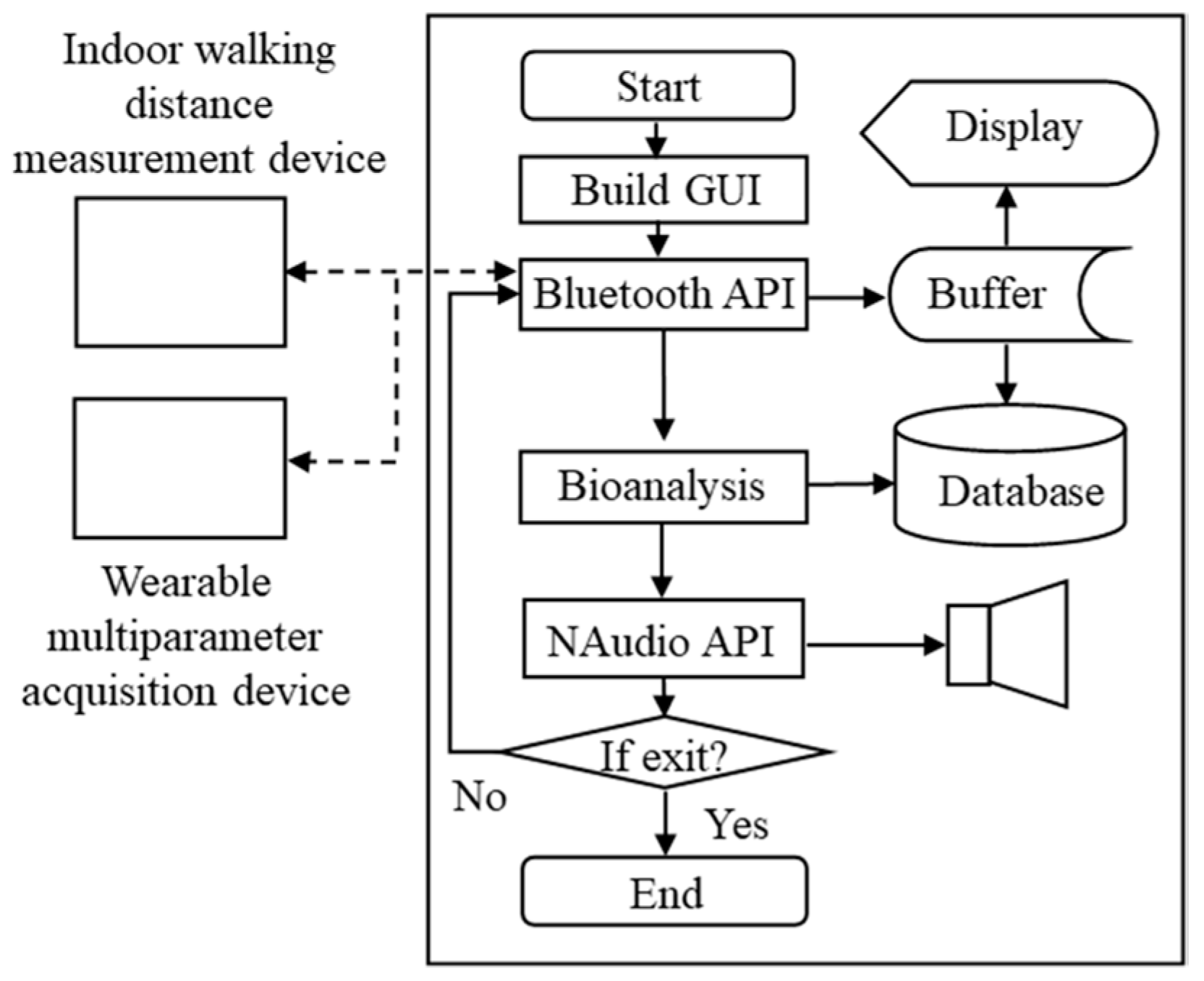
5. System Software Design
6. Multiparameter Analysis Algorithm
7. Experiment Design and Procedures
8. Results
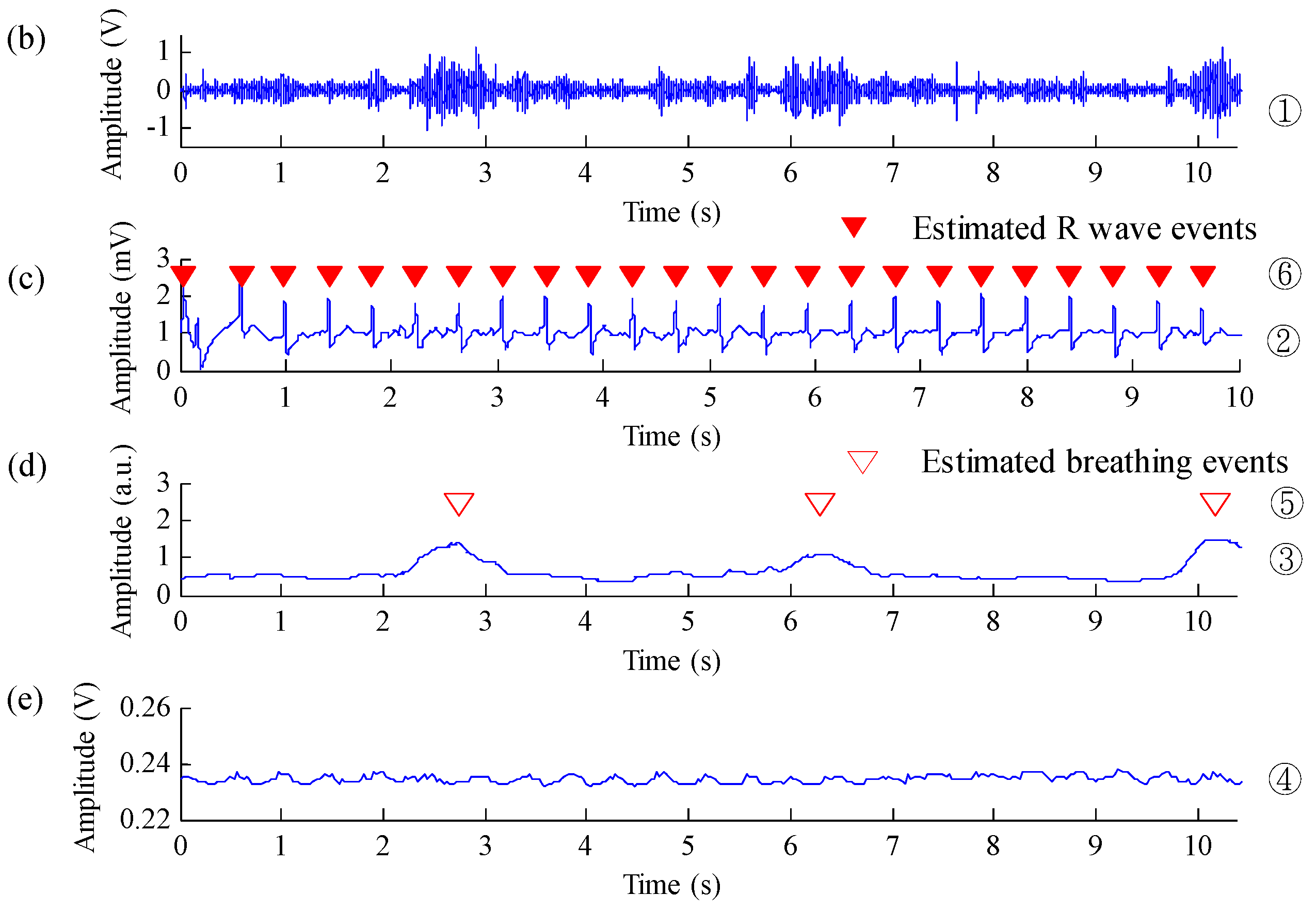
8.1. Performance of the Proposed Algorithm in Detecting Heart and Breathing Rates
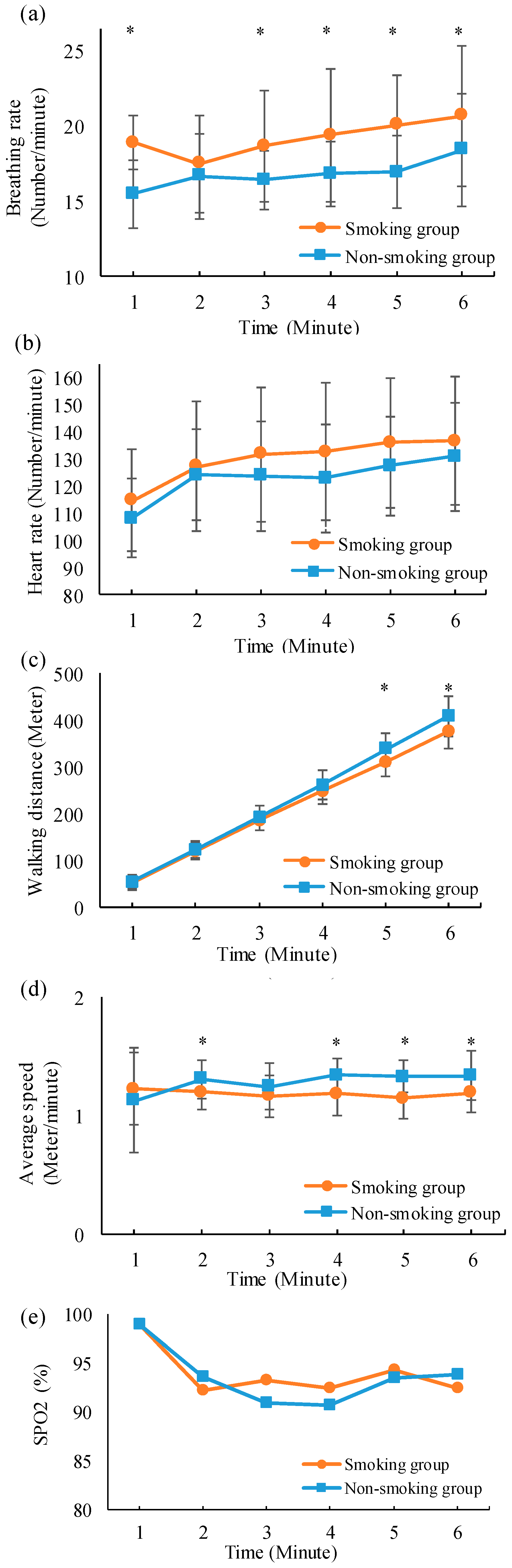
8.2. Differences Between Multiphysiological Parameters of Different Groups During the 6MWT
9. Discussion
10. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Kaymaz, N.; Yıldırım, Ş.; Tekin, M.; Aylanç, H.; Battal, F.; Topaloğlu, N.; Binnetoğlu, F.; Akbal, A. The effects of passive smoking on the six-minute walk test in obese pediatric cases. J. Clin. Res. Pediatr. Endocrinol. 2014, 6, 245–247. [Google Scholar] [CrossRef] [PubMed]
- Van Stel, H.F.; Bogaard, J.M.; Rijssenbeek-Nouwens, L.H.; Colland, V.T. Multivariable assessment of the 6-min walking test in patients with chronic obstructive pulmonary disease. Am. J. Respir. Crit. Care Med. 2001, 163, 1567–1571. [Google Scholar] [CrossRef] [PubMed]
- Solway, S.; Brooks, D.; Lacasse, Y.; Thomas, S. A qualitative systematic overview of the measurement properties of functional walk tests used in the cardiorespiratory domain. Chest 2001, 119, 256–270. [Google Scholar] [CrossRef] [PubMed]
- Hernandes, N.A.; Wouters, E.; Meijer, K.; Annegarn, J.; Pitta, F.; Spruit, M. Reproducibility of 6-minute walking test in patients with COPD. Eur. Respir. J. 2011, 38, 261–267. [Google Scholar] [CrossRef] [PubMed]
- Enright, P.L. The six-minute walk test. Respir. Care 2003, 48, 783–785. [Google Scholar]
- Rasekaba, T.; Lee, A.L.; Naughton, M.T.; Williams, T.J.; Holland, A.E. The six-minute walk test: A useful metric for the cardiopulmonary patient. Intern. Med. J. 2009, 39, 495–501. [Google Scholar] [CrossRef]
- Spruit, M.A.; Pennings, H.-J.; Janssen, P.P.; Does, J.D.; Scroyen, S.; Akkermans, M.A.; Mostert, R.; Wouters, E.F. Extra-pulmonary features in COPD patients entering rehabilitation after stratification for MRC dyspnea grade. Respir. Med. 2007, 101, 2454–2463. [Google Scholar] [CrossRef][Green Version]
- Han, M.K.; Agusti, A.; Calverley, P.M.; Celli, B.R.; Criner, G.; Curtis, J.L.; Fabbri, L.M.; Goldin, J.G.; Jones, P.W.; MacNee, W. Chronic obstructive pulmonary disease phenotypes: The future of COPD. Am. J. Respir. Crit. Care Med. 2010, 182, 598–604. [Google Scholar] [CrossRef]
- Barreiro, E.; Peinado, V.I.; Galdiz, J.B.; Ferrer, E.; Marin-Corral, J.; Sanchez, F.; Gea, J.; Barberà, J.A. Cigarette smoke–induced oxidative stress: A role in chronic obstructive pulmonary disease skeletal muscle dysfunction. Am. J. Respir. Crit. Care Med. 2010, 182, 477–488. [Google Scholar] [CrossRef]
- De Oca, M.M.; Loeb, E.; Torres, S.H.; De Sanctis, J.; Hernández, N.; Tálamo, C. Peripheral muscle alterations in non-COPD smokers. Chest 2008, 133, 13–18. [Google Scholar] [CrossRef]
- Cielen, N.; Maes, K.; Heulens, N.; Troosters, T.; Carmeliet, G.; Janssens, W.; Gayan, R.G.N. Interaction between physical activity and smoking on lung, muscle, and bone in mice. Am. J. Respir. Cell Mol. Biol. 2016, 54, 674–682. [Google Scholar] [CrossRef] [PubMed]
- Brown, J.; Votto, J.; Thrall, R.; Campbell, H.M.; Stockdale, W.R.; Bandyopadhyay, T.; ZuWallack, R. Functional Status and Survival Following Pulmonary Rehabilitation. J. Cardiopulm. Rehabil. Prev. 2001, 21, 53–57. [Google Scholar] [CrossRef]
- Decramer, M.; Gosselink, R.; Troosters, T.; Verschueren, M.; Evers, G. Muscle weakness is related to utilization of health care resources in COPD patients. Eur. Respir. J. 1997, 10, 417–423. [Google Scholar] [CrossRef] [PubMed]
- Hassett, D.J.; Borchers, M.T.; Panos, R.J. Chronic obstructive pulmonary disease (COPD): Evaluation from clinical, immunological and bacterial pathogenesis perspectives. J. Microbiol. 2014, 52, 211–226. [Google Scholar] [CrossRef] [PubMed]
- Pinto-Plata, V.; Cote, C.; Cabral, H.; Taylor, J.; Celli, B. The 6-min walk distance: Change over time and value as a predictor of survival in severe COPD. Eur. Respir. J. 2004, 23, 28–33. [Google Scholar] [CrossRef]
- Troosters, T.; Vilaro, J.; Rabinovich, R.; Casas, A.; Barbera, J.; Rodriguez, R.R.; Roca, J. Physiological responses to the 6-min walk test in patients with chronic obstructive pulmonary disease. Eur. Respir. J. 2002, 20, 564–569. [Google Scholar] [CrossRef]
- Redelmeier, D.A.; Bayoumi, A.M.; Goldstein, R.S.; Guyatt, G.H. Interpreting small differences in functional status: The Six Minute Walk test in chronic lung disease patients. Am. J. Respir. Cell Mol. Biol. 1997, 155, 1278–1282. [Google Scholar] [CrossRef]
- Cote, C.G.; Pinto-Plata, V.; Kasprzyk, K.; Dordelly, L.J.; Celli, B.R. The 6-min walk distance, peak oxygen uptake, and mortality in COPD. Chest 2007, 132, 1778–1785. [Google Scholar] [CrossRef]
- Jehn, M.; Schmidt-Trucksäess, A.; Schuster, T.; Hanssen, H.; Weis, M.; Halle, M.; Koehler, F. Accelerometer-based quantification of 6-minute walk test performance in patients with chronic heart failure: Applicability in telemedicine. J. Card. Fail. 2009, 15, 334–340. [Google Scholar] [CrossRef]
- Worringham, C.; Rojek, A.; Stewart, I. Development and feasibility of a smartphone, ECG and GPS based system for remotely monitoring exercise in cardiac rehabilitation. PLoS ONE 2011, 6, 669–675. [Google Scholar] [CrossRef]
- Juen, J.; Cheng, Q.; Schatz, B. A natural walking monitor for pulmonary patients using mobile phones. IEEE J. Biomed. Health Inform. 2015, 19, 1399–1405. [Google Scholar] [CrossRef] [PubMed]
- Capela, N.A.; Lemaire, E.D.; Baddour, N. Novel algorithm for a smartphone-based 6-minute walk test application: Algorithm, application development, and evaluation. J. Neuroeng. Rehabil. 2015, 12, 19–25. [Google Scholar] [CrossRef] [PubMed]
- Creber, R.M.M.; Hickey, K.T.; Maurer, M.S. Gerontechnologies for older patients with heart failure: What is the role of smartphones, tablets, and remote monitoring devices in improving symptom monitoring and self-care management. Curr. Cardiovasc. Risk Rep. 2016, 10, 30–38. [Google Scholar] [CrossRef] [PubMed]
- Andreoni, G.; Mazzola, M.; Perego, P.; Standoli, C.E.; Manzoni, S.; Piccini, L.; Molteni, F. Wearable monitoring devices for assistive technology: Case studies in post-polio syndrome. Sensors 2014, 14, 2012–2027. [Google Scholar] [CrossRef] [PubMed]
- Miramontes, R.; Aquino, R.; Flores, A.; Rodríguez, G.; Anguiano, R.; Ríos, A.; Edwards, A. PlaIMoS: A remote mobile healthcare platform to monitor cardiovascular and respiratory variables. Sensors 2017, 17, 176. [Google Scholar] [CrossRef]
- Taffoni, F.; Rivera, D.; La Camera, A.; Nicolò, A.; Velasco, J.R.; Massaroni, C. A wearable system for real-time continuous monitoring of physical activity. J. Healthc. Eng. 2018, 2018, 1878354. [Google Scholar] [CrossRef]
- Klum, M.; Leib, F.; Oberschelp, C.; Martens, D.; Pielmus, A.G.; Tigges, T.; Penzel, T.; Orglmeister, R. Wearable Multimodal Stethoscope Patch for Wireless Biosignal Acquisition and Long-Term Auscultation. In Proceedings of the EMBC 2019, Berlin, Germany, 23–27 July 2019; pp. 5781–5785. [Google Scholar]
- NAudio. Available online: http://github.com/naudio/NAudio (accessed on 13 September 2019).
- Li, S.H.; Lin, B.S.; Tsai, C.H.; Yang, C.T.; Lin, B.S. Design of wearable breathing sound monitoring system for real-time wheeze detection. Sensors 2017, 17, 171. [Google Scholar] [CrossRef]
- Hadjileontiadis, L.J.; Rekanos, I.T. Detection of explosive lung and bowel sounds by means of fractal dimension. IEEE Signal Process. Lett. 2003, 10, 311–314. [Google Scholar] [CrossRef]
- Chen, C.T.; Wang, L.Y.; Wang, Y.L.; Lin, B.-S. Quantitative real-time assessment for feeding skill of preterm infants. J. Med. Syst. 2017, 41, 95–104. [Google Scholar] [CrossRef]
- Wang, Y.L.; Kuo, H.C.; Wang, L.Y.; Ko, M.J.; Lin, B.-S. Design of wireless multi-parameter monitoring system for oral feeding of premature infants. Med. Biol. Eng. Comput. 2016, 54, 1061–1069. [Google Scholar] [CrossRef]
- Lin, B.S.; Wu, P.J.; Chen, C.Y. 2D/3D-display auto-adjustment switch system. IEEE J. Biomed. Health Inform. 2018, 22, 799–805. [Google Scholar] [CrossRef] [PubMed]
- Sheu, M.J.; Lin, P.Y.; Chen, J.Y.; Lee, C.C.; Lin, B.-S. Higher-order-statistics-based fractal dimension for noisy bowel sound detection. IEEE Signal Process. Lett. 2015, 22, 789–793. [Google Scholar] [CrossRef]
- Katz, M.J. Fractals and the analysis of waveforms. Comput. Biol. Med. 1988, 18, 145–156. [Google Scholar] [CrossRef]
- Lin, B.S.; Chou, W.; Wang, H.Y.; Huang, Y.J.; Pan, J.S. Development of novel non-contact electrodes for mobile electrocardiogram monitoring system. IEEE J. Transl. Eng. Health Med. 2013, 1, 2700108. [Google Scholar] [PubMed]
- Kästle, S.; Noller, F.; Falk, S.; Bukta, A.; Mayer, E.; Miller, D. A new family of sensors for pulse oximetry. Hewlett Packard J. 1997, 48, 39–47. [Google Scholar]
- Nitzan, M.; Noach, S.; Tobal, E.; Adar, Y.; Miller, Y.; Shalom, E.; Engelberg, S. Calibration-free pulse oximetry based on two wavelengths in the infrared—A preliminary study. Sensors 2014, 14, 7420–7434. [Google Scholar] [CrossRef]
- Arzeno, N.M.; Deng, Z.D.; Poon, C.S. Analysis of first-derivative based QRS detection algorithms. IEEE Trans. Biomed. Eng. 2008, 55, 478–484. [Google Scholar] [CrossRef]
- Clarke, J.; Shelton, J.; Venning, G.; Hamer, J.; Taylor, S. The rhythm of the normal human heart. Lancet 1976, 308, 508–512. [Google Scholar] [CrossRef]
- Stubán, N.; Masatsugu, N. Non-invasive calibration method for pulse oximeters. Period. Polytech. Electr. Eng. 2008, 52, 91–94. [Google Scholar] [CrossRef]
- Borg, G. ATS statement: Guidelines for the six-minute walk test. Am. J. Respir. Crit. Care Med. 2002, 166, 111–117. [Google Scholar]
- Farkhooy, A. Lung Function in Relation to Exercise Capacity in Health and Disease. Ph.D. Thesis, Acta Universitatis, Upsaliensis, Sweden, 2017. [Google Scholar]
- Iwamoto, H.; Yokoyama, A.; Kitahara, Y.; Ishikawa, N.; Haruta, Y.; Yamane, K.; Hattori, N.; Hara, H.; Kohno, N. Airflow limitation in smokers is associated with subclinical atherosclerosis. Am. J. Respir. Crit. Care Med. 2009, 179, 35–40. [Google Scholar] [CrossRef] [PubMed]



| Estimated Breathing Events | ||||
|---|---|---|---|---|
| Real Breathing Events | + | – | Total | |
| + | 3073 (TP) | 347 (TN) | 3420 | |
| – | 112 (FP) | 0 (FN) | 112 | |
| Total | 3185 | 347 | 3532 | |
| Estimated R Waves | ||||
|---|---|---|---|---|
| Real R Waves | + | – | Total | |
| + | 22742 (TP) | 0 (TN) | 22742 | |
| – | 0 (FP) | 0 (FN) | 0 | |
| Total | 22742 | 0 | 22742 | |
| Andreoni et al. [24] | Miramontes et al. [25] | Taffoni et al. [26] | Proposed System | |
|---|---|---|---|---|
| Physiological Parameters | ECG, ICG, and Lower-Limb Acceleration | ECG, SpO2, Skin Temperature, Fall Detection, Breathing Rate and Skin Response | Breathing Rate, Heart Rate, Body Movement, Walking Step | SpO2, ECG, Breathing Sound, Breathing Rate, and Walking Information |
| Measurement Under Motion | Yes | No | Yes | Yes |
| Sensors | Triaxial Accelerometer, ECG Electrodes | ECG Electrodes, PPG Sensor, Triaxial Accelerometer, Temperature Sensor, Airflow Sensor, and Galvanic Sensor | PPG Sensor, SDP Sensor, IMU (Accelerometers, Gyroscopes, and Magnetometers) | ECG Electrodes, PPG Sensor, RFID Sensor, and Stethoscope |
| Power Supply | Battery | Battery | Battery | Battery |
| Size (cm3) | 11.7 × 7 × 2.3 | - | - | 6 × 6 × 2 |
| Transmission Mode | Bluetooth | Wireless Sensor Network | Bluetooth | Bluetooth |
| Applications | 6MWT | Cardiopulmonary Function Monitoring | Cardiopulmonary Function Monitoring | 6MWT, Cardiopulmonary Function Monitoring |
| Disadvantages | Influence of Motion on Measurement Gait Information | Higher Cost Transmission Architecture, Limited Range of Activities. | Influence of Motion On Heart Rate Estimation | Requirement of RFID Placement |
| Monitor Breathing Sound Under Walking | No | No | No | Yes |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lin, B.-S.; Jhang, R.-J.; Lin, B.-S. Wearable Cardiopulmonary Function Evaluation System for Six-Minute Walking Test. Sensors 2019, 19, 4656. https://doi.org/10.3390/s19214656
Lin B-S, Jhang R-J, Lin B-S. Wearable Cardiopulmonary Function Evaluation System for Six-Minute Walking Test. Sensors. 2019; 19(21):4656. https://doi.org/10.3390/s19214656
Chicago/Turabian StyleLin, Bor-Shing, Ruei-Jie Jhang, and Bor-Shyh Lin. 2019. "Wearable Cardiopulmonary Function Evaluation System for Six-Minute Walking Test" Sensors 19, no. 21: 4656. https://doi.org/10.3390/s19214656
APA StyleLin, B.-S., Jhang, R.-J., & Lin, B.-S. (2019). Wearable Cardiopulmonary Function Evaluation System for Six-Minute Walking Test. Sensors, 19(21), 4656. https://doi.org/10.3390/s19214656






