The Ultrasonic Directional Tidal Breathing Pattern Sensor: Equitable Design Realization Based on Phase Information
Abstract
1. Introduction
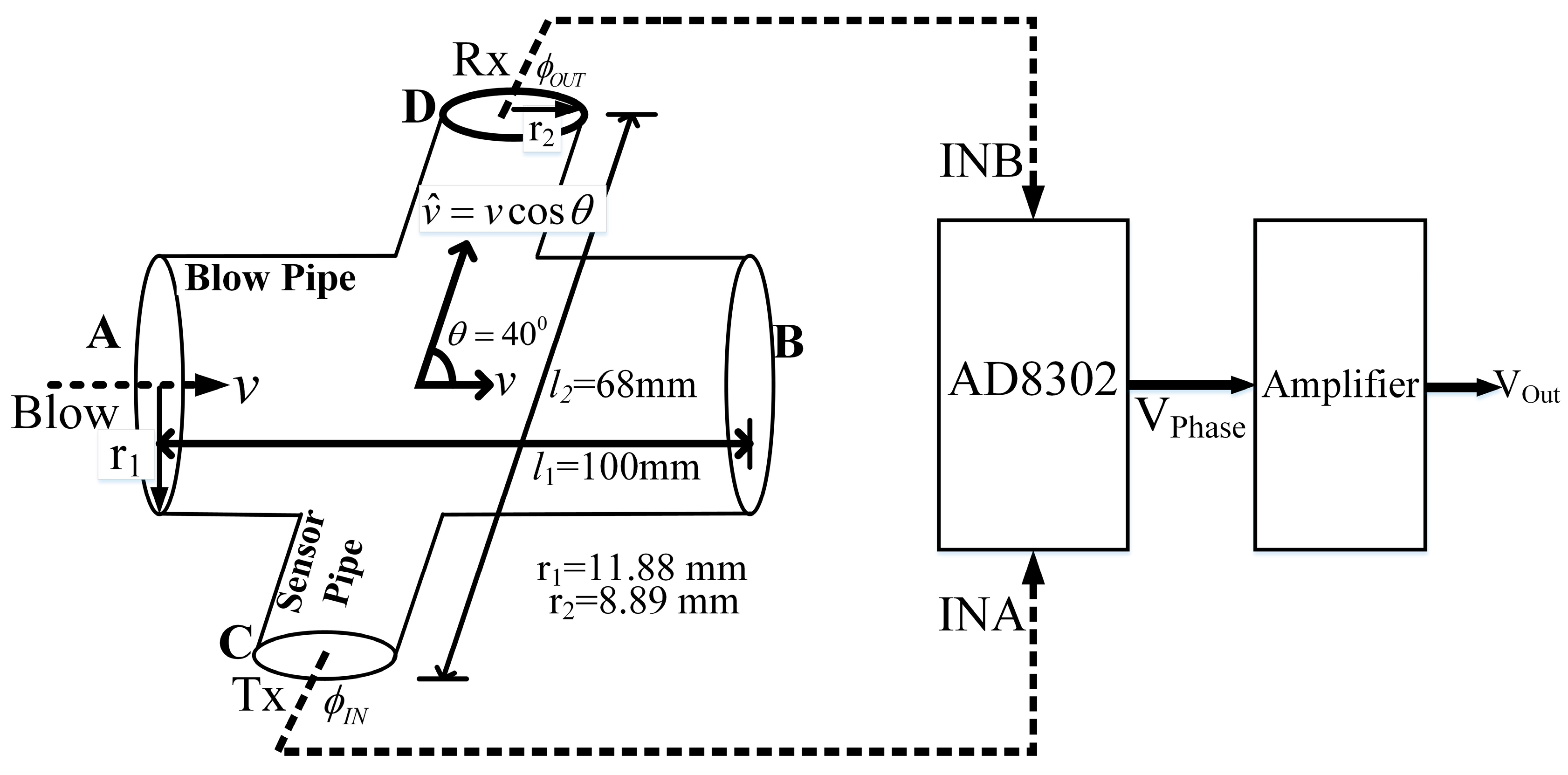
2. Measurement Principle
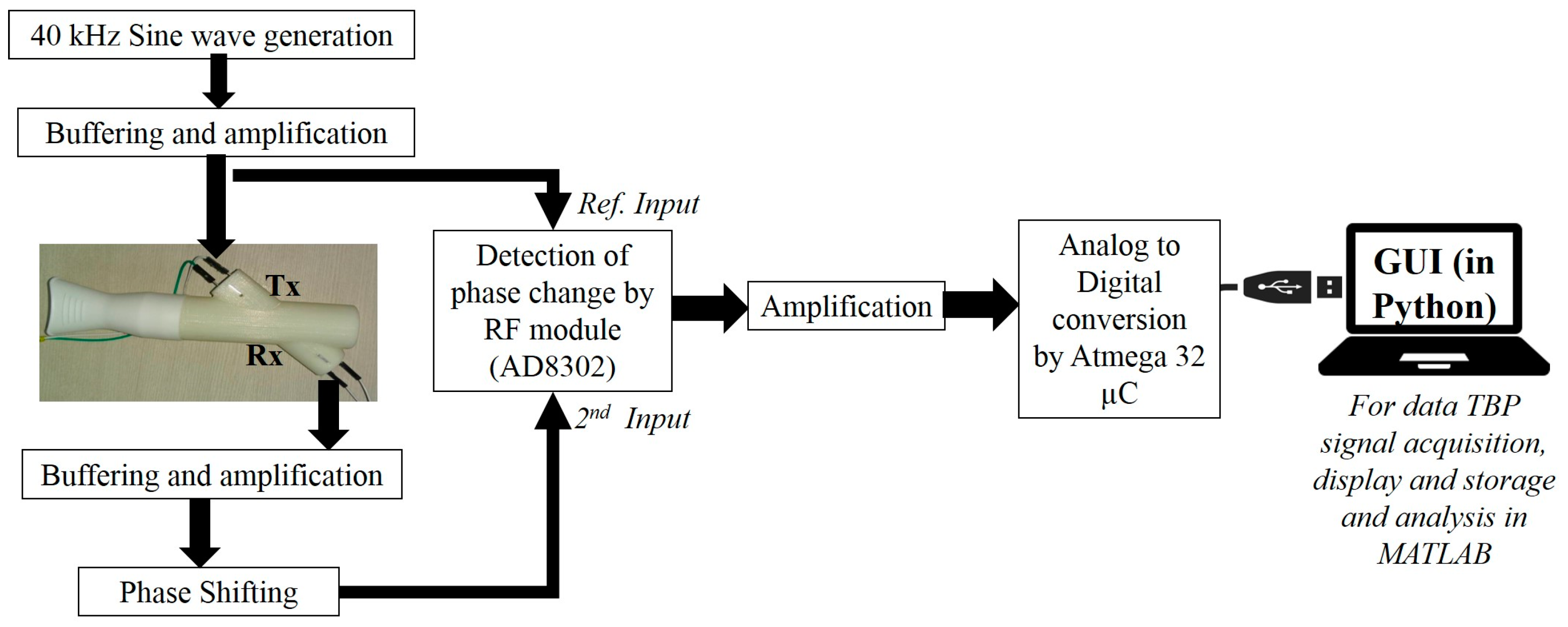
3. System Architecture
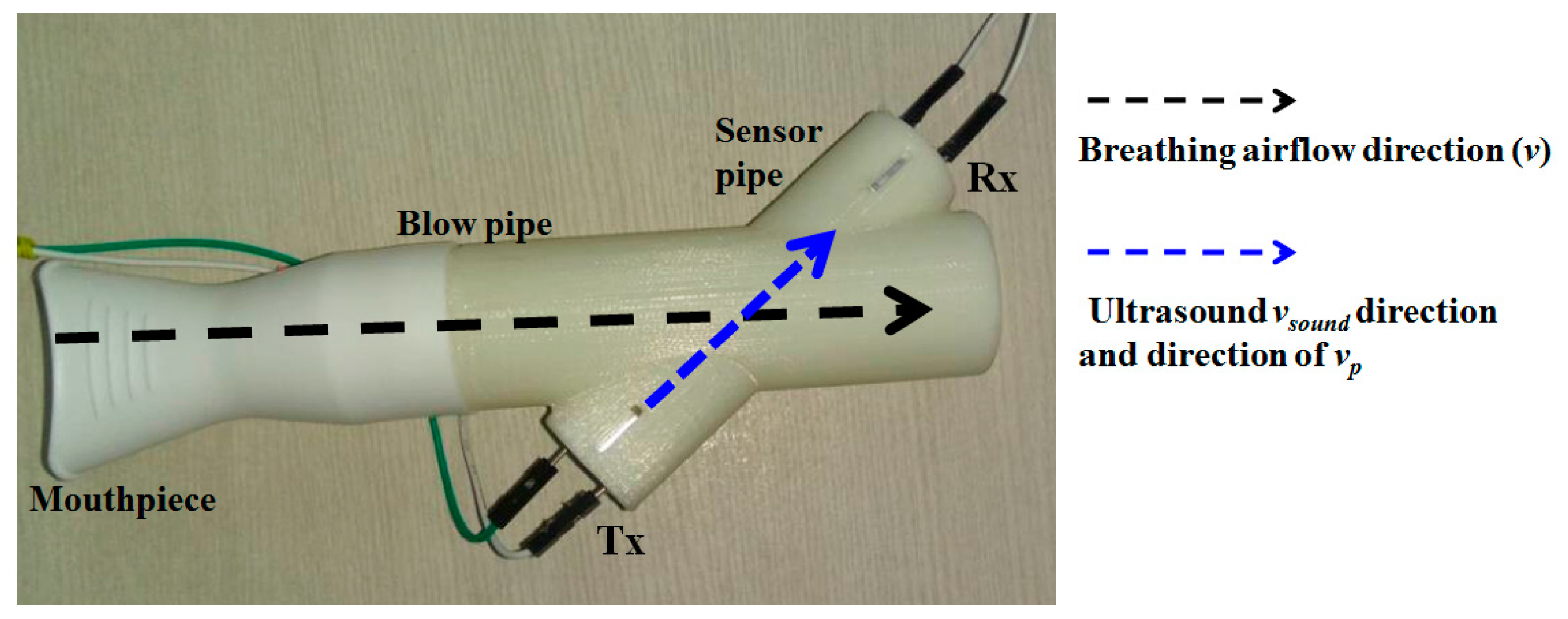
3.1. The 3D printed Flow Pipe
3.2. The Electronic Circuitry
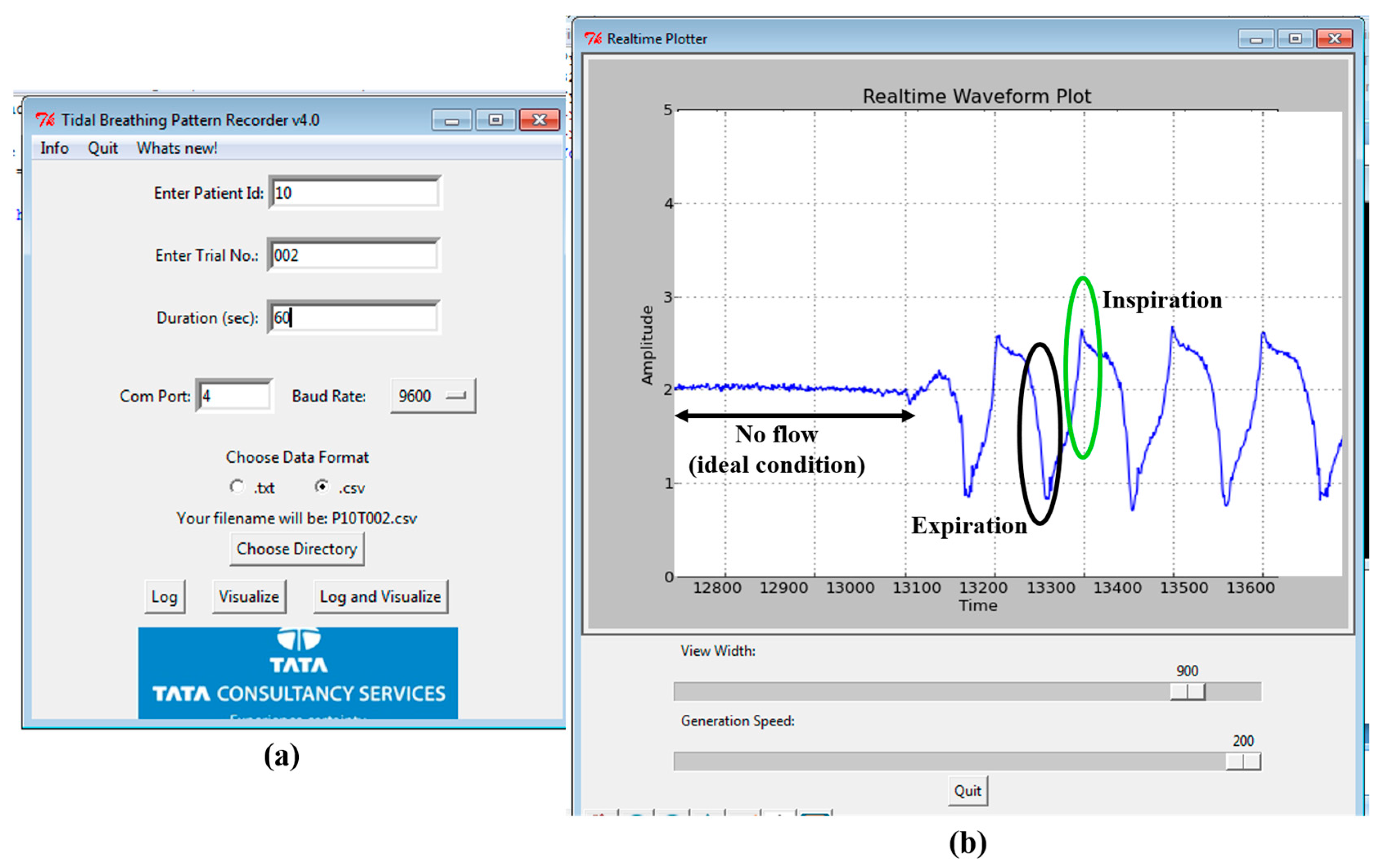
3.3. GUI
4. Tidal Flow Estimation Based on Actual Configuration
4.1. Tidal Velocity, Flow and Volume Computations
4.2. Parametric Evaluation
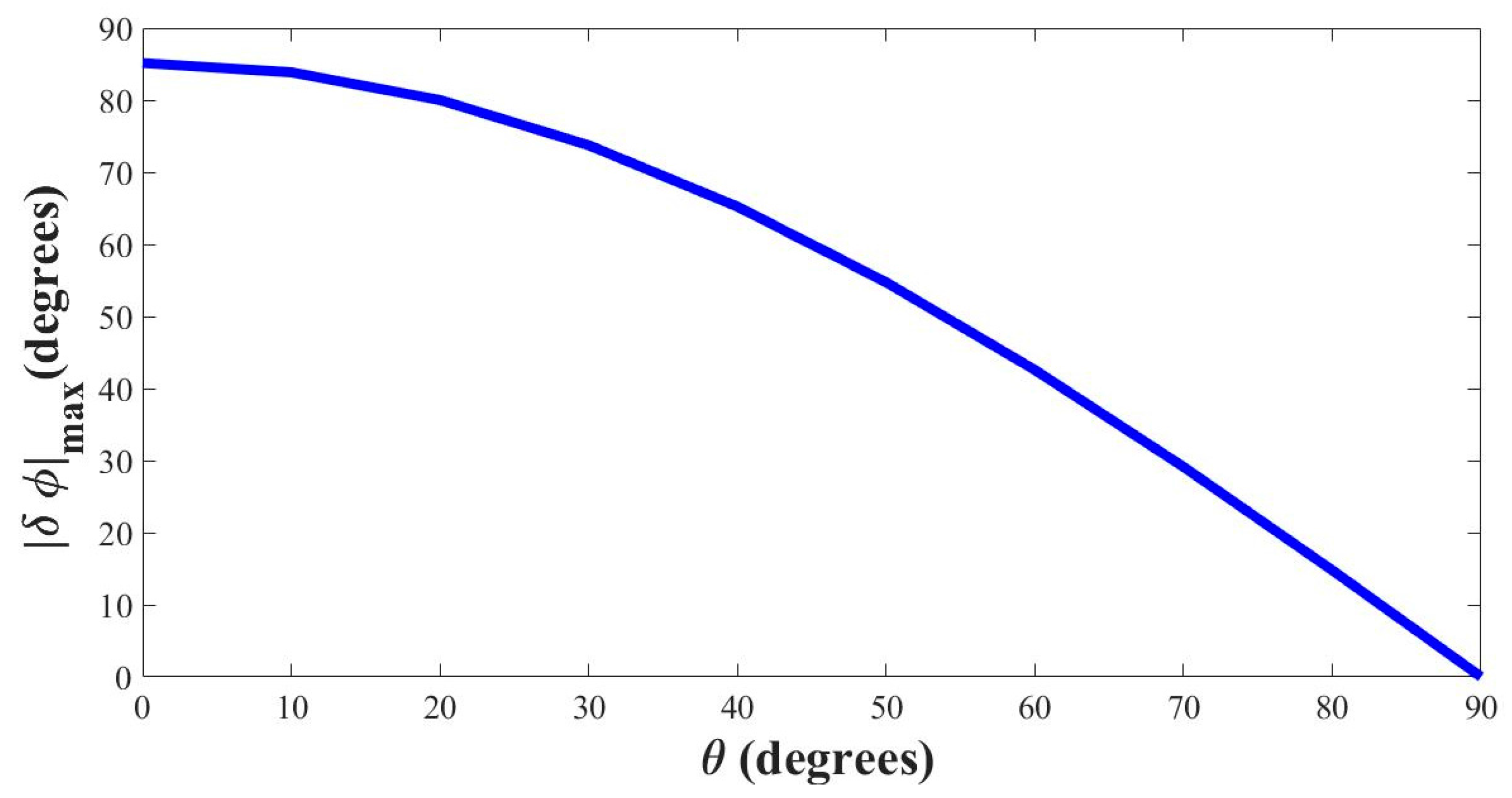
4.3. Selecting the Optimal Angle (θ)
5. Tidal Breathing Analysis
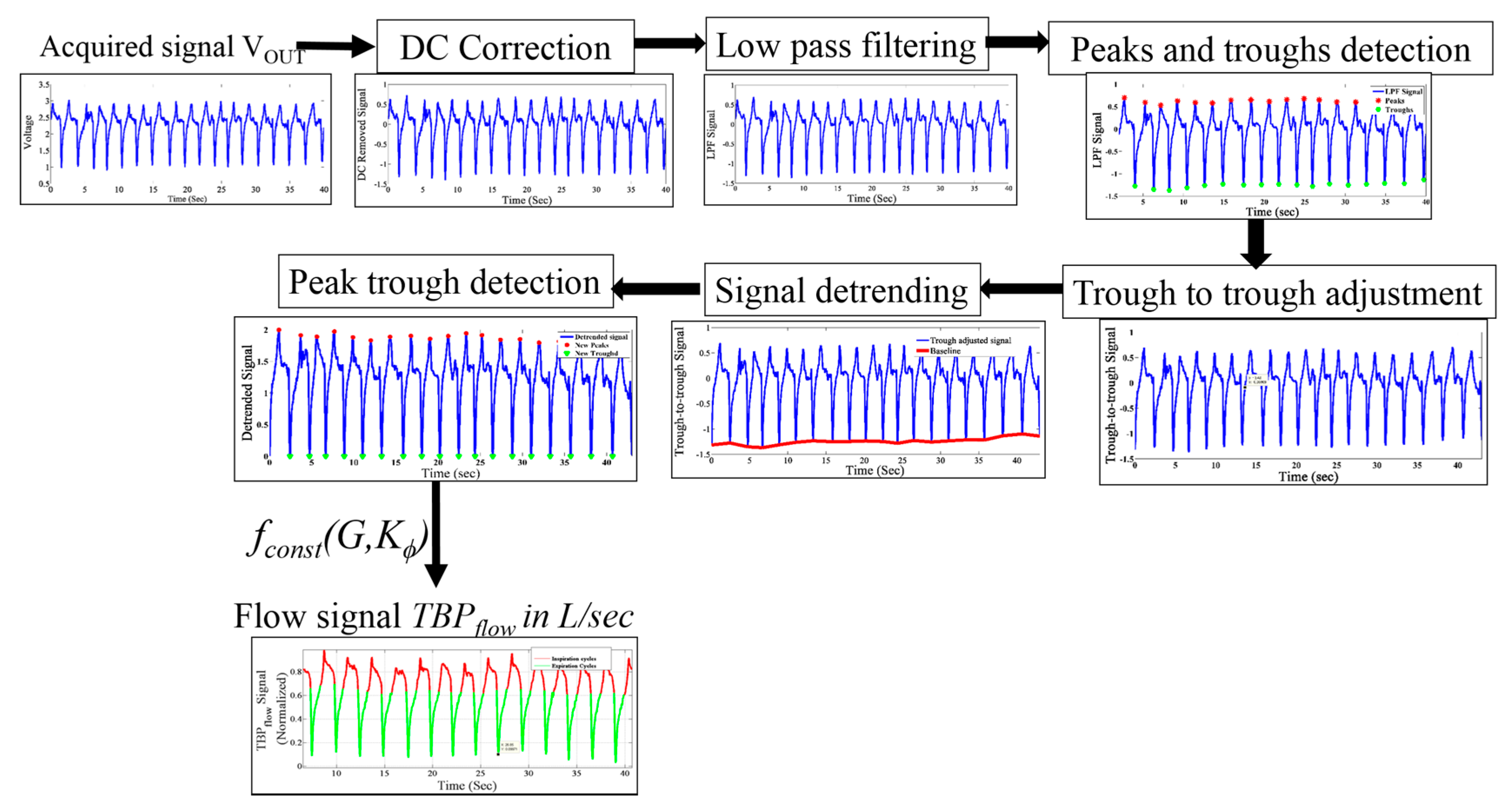
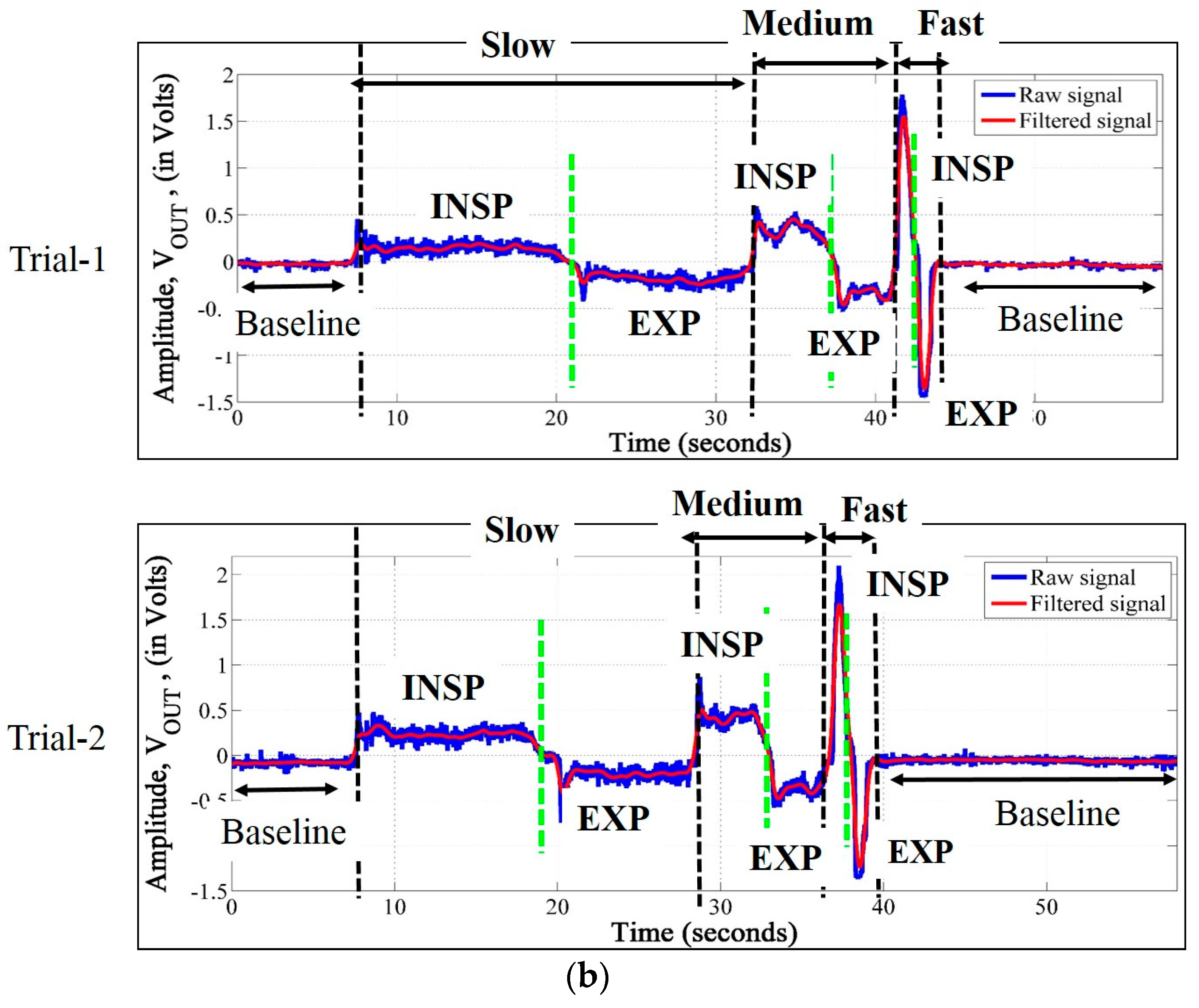
5.1. Preprocessing
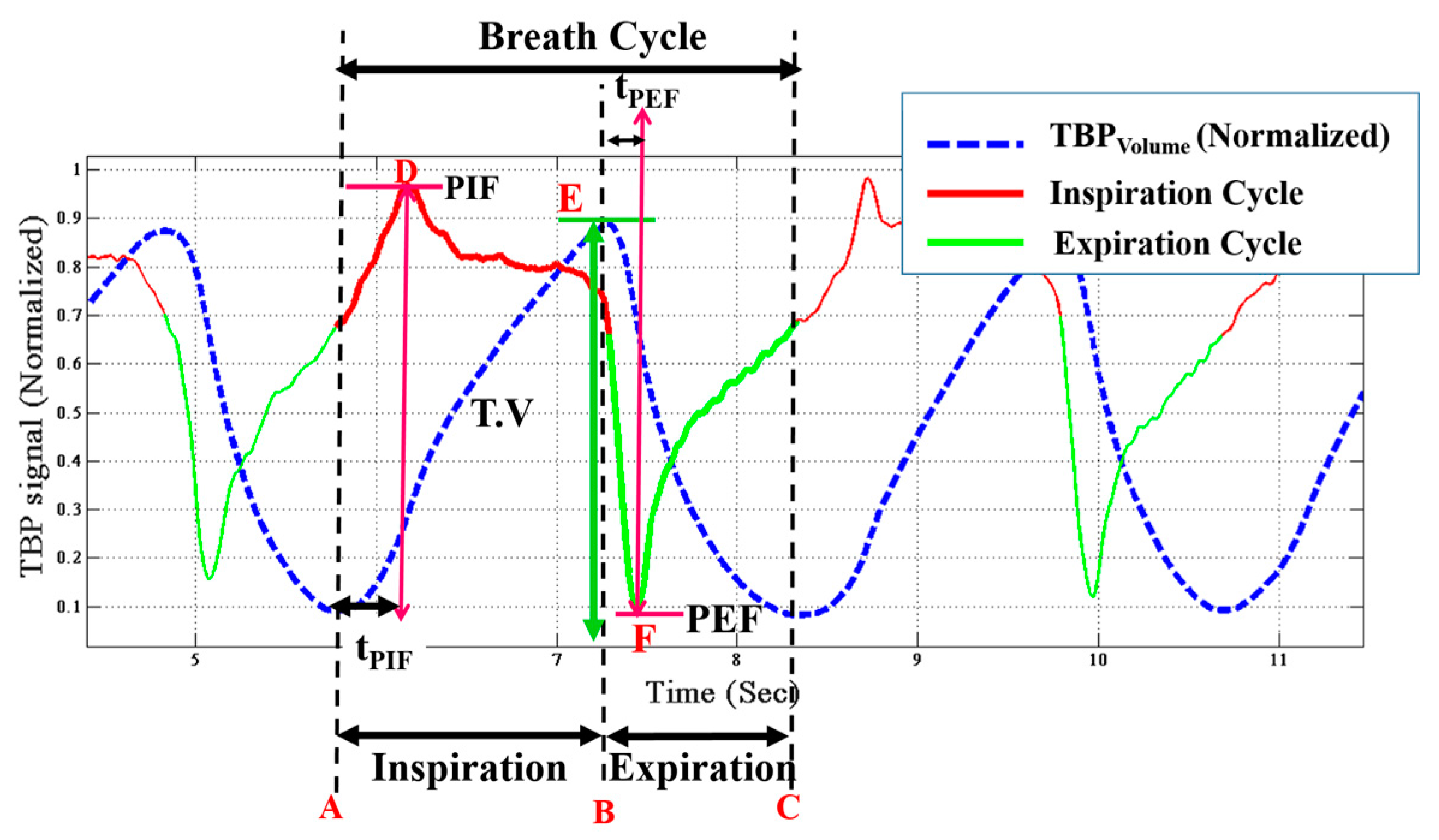
5.2. Tidal Breathing Signal Parameters
- Inspiratory time (TI) is the time elapsed from onset (A) to the end (B) of inspiration. It is given in seconds.
- Expiratory time (TE) is the time taken to expire, i.e., the time elapsed between the onset (B) to the end (C) of expiration.
- Breathing rate (BR) is the number of breaths cycles per minute (BPM) is computed by the following equation,
- Duty cycle (DCy) is given by the equation,
- Peak inspiratory flow (PIF) is the maximal flow rate attained during every inspiratory cycle. It is obtained from the TBPflow signal. In Figure 8 the point D corresponds to PIF.
- Peak expiratory flow (PEF) is the minima in the TBPflow signal during every expiratory cycle, i.e., the maximal flow attained during expiration. It refers to point F in the Figure 8.
- Time to peak inspiratory flow (tPIF) is the time taken to reach the maximum flow rate during inspiration from its onset, i.e., the time taken to reach D from A.
- Time to peak expiratory flow (tPEF) is the time elapsed from to onset of expiration (E) till PEF is attained.
- Tidal volume (T.V) is represented in terms of inspiratory and expiratory tidal volume. Inspiratory (TVins) and expiratory tidal volume (TVexp) are the total volume of air inspired and exhaled respectively. TVins refers to the area under the curve between point A and B and TVexp is that between the point B and C in the TBPflow signal. TVins is the same as the tidal volume (T.V). During restful tidal breathing is the TVins (i.e., T.V) is around 500 mL, however, it can vary largely during stimulated tidal breathing [52], as in this current study.
- Inspiratory (vins) and expiratory (vexp) velocity are the velocities during inhalation and exhalation, respectively.
6. Experiments and Results
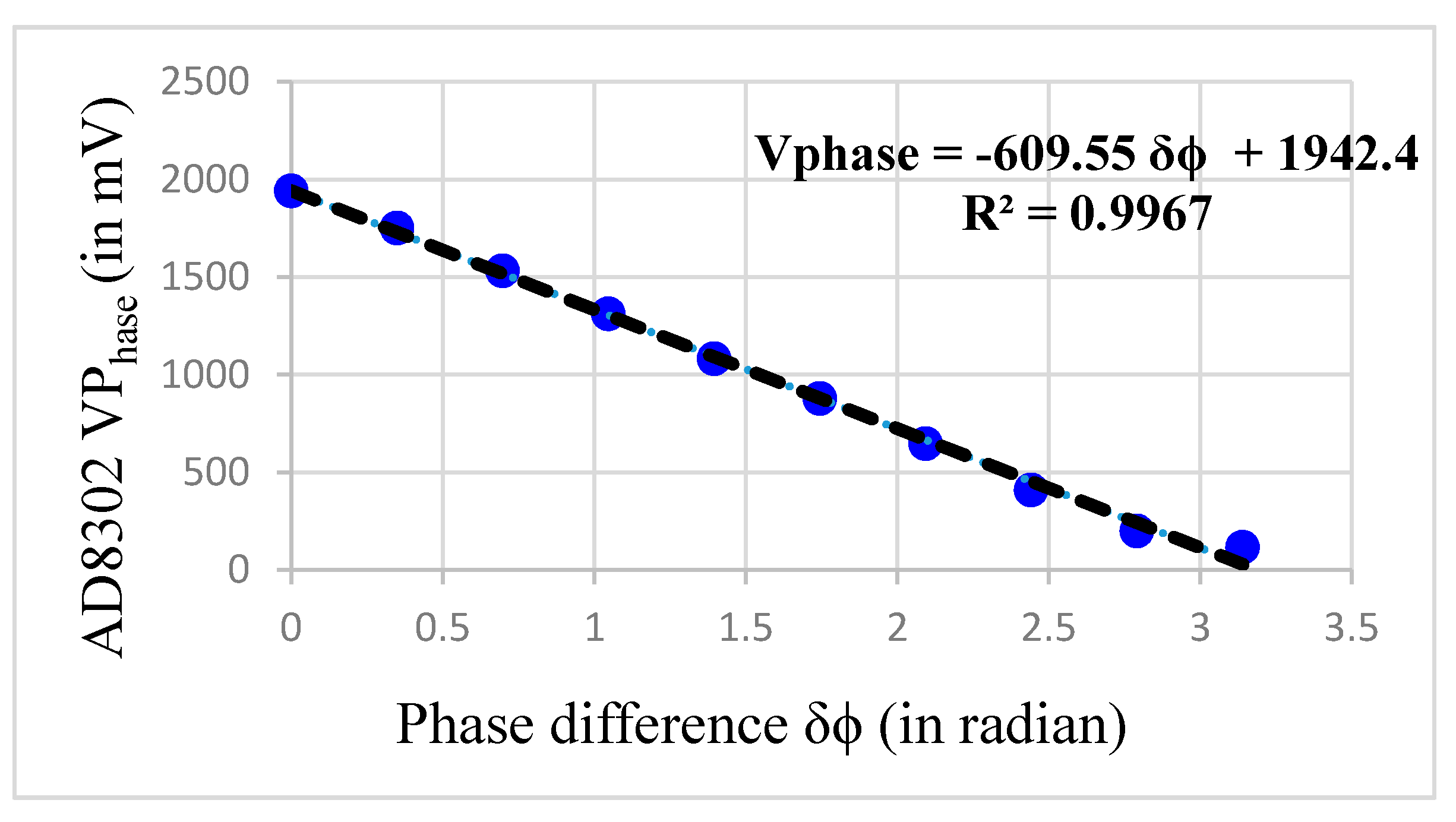
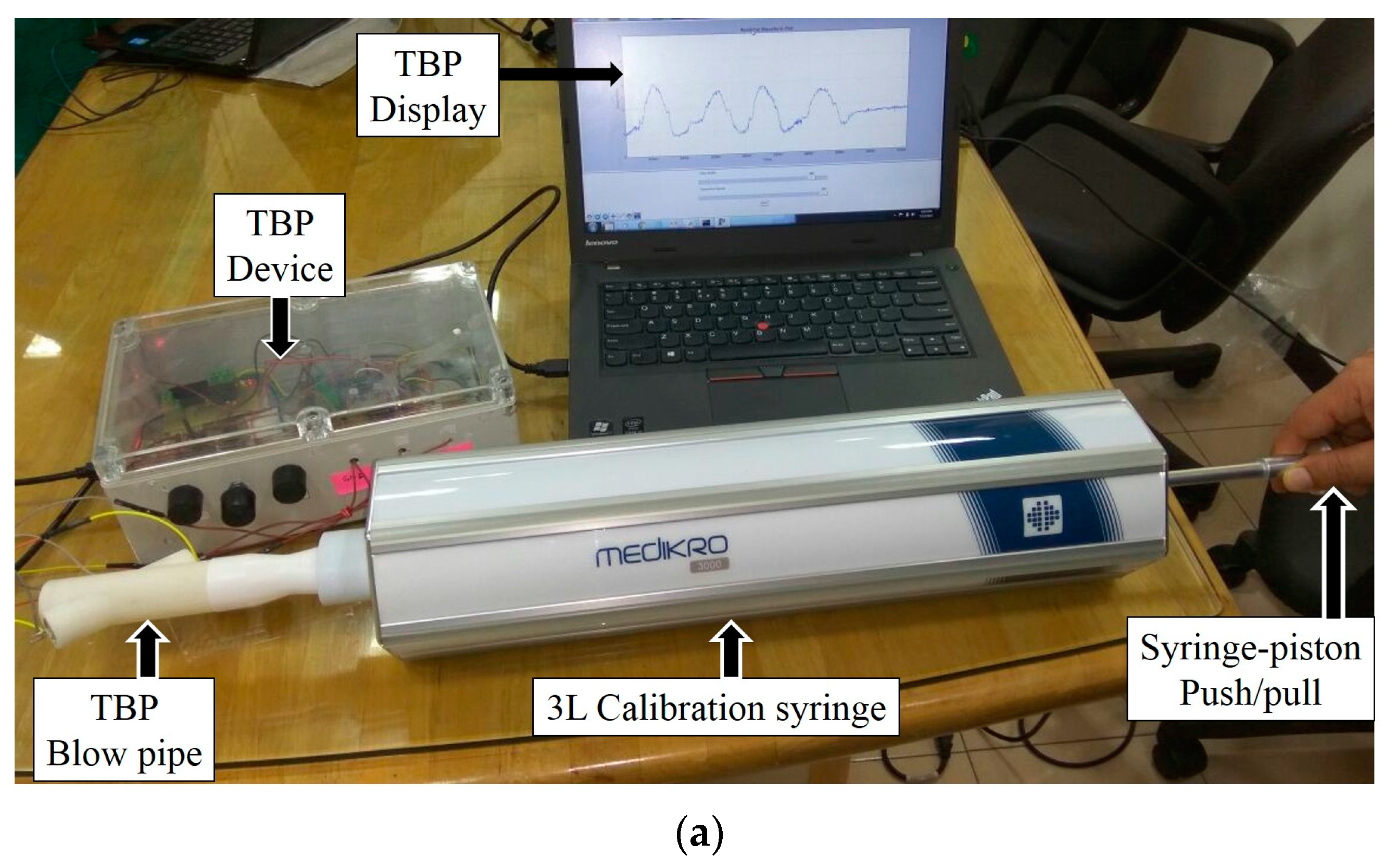
6.1. System Calibration
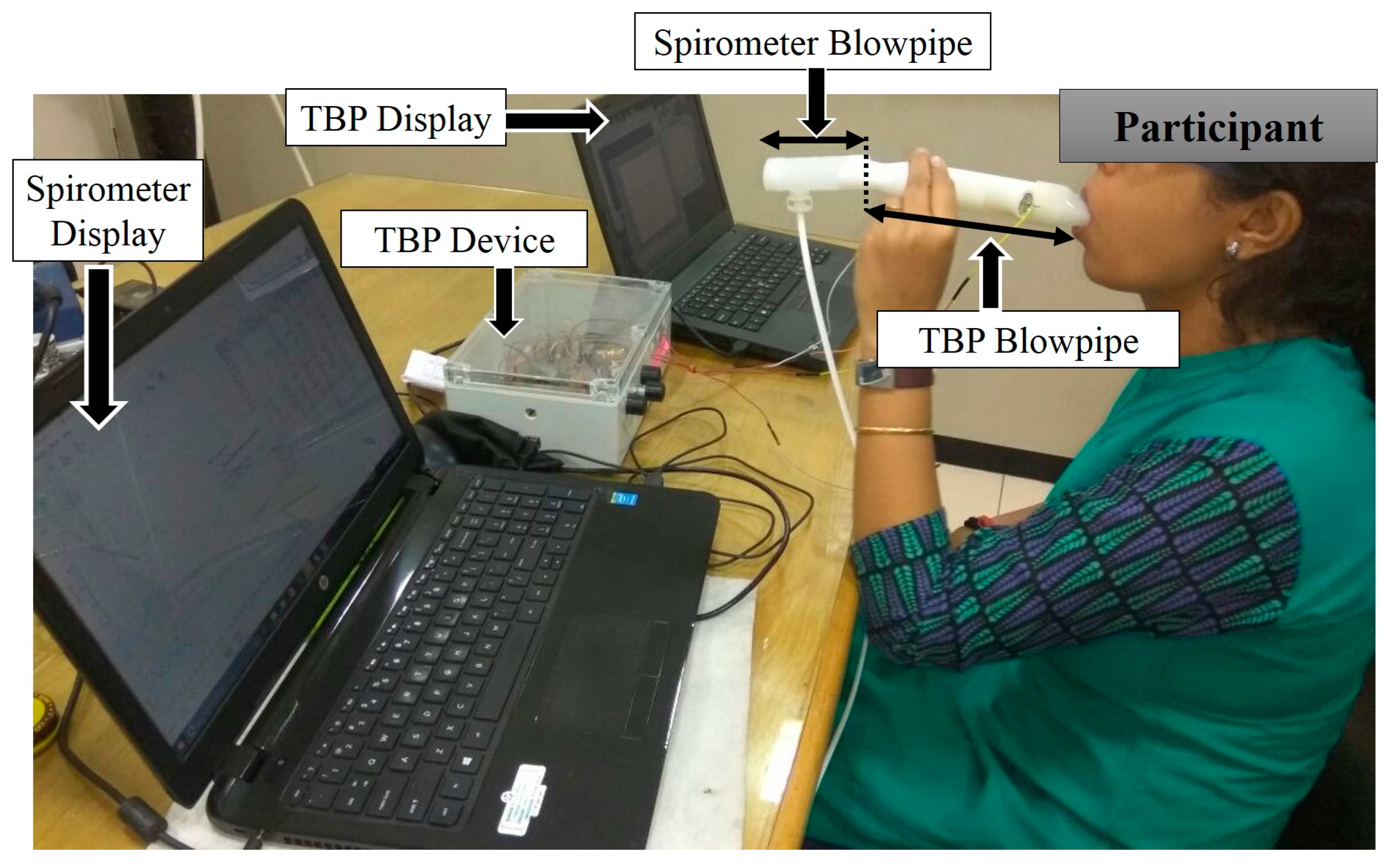
6.2. System Validation using Standard Spirometer
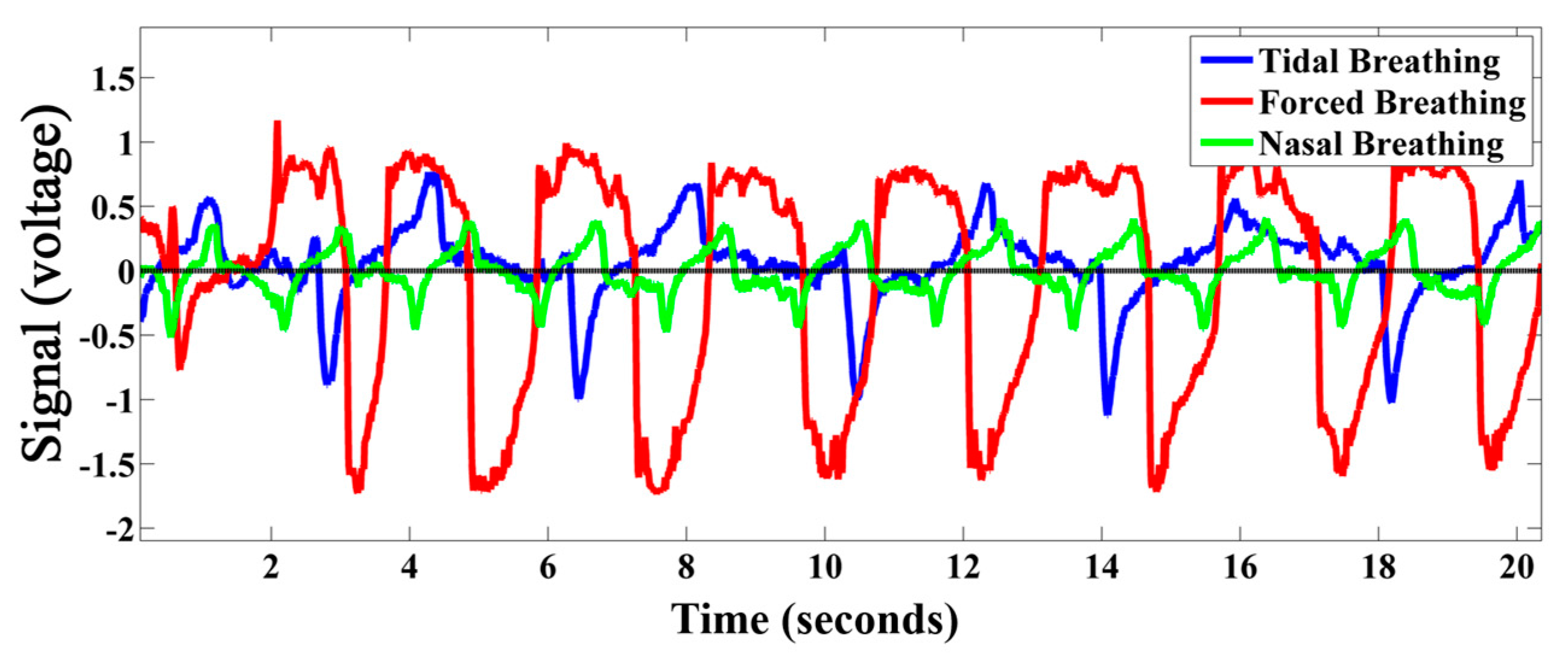
6.3. TBP Data Acquisition
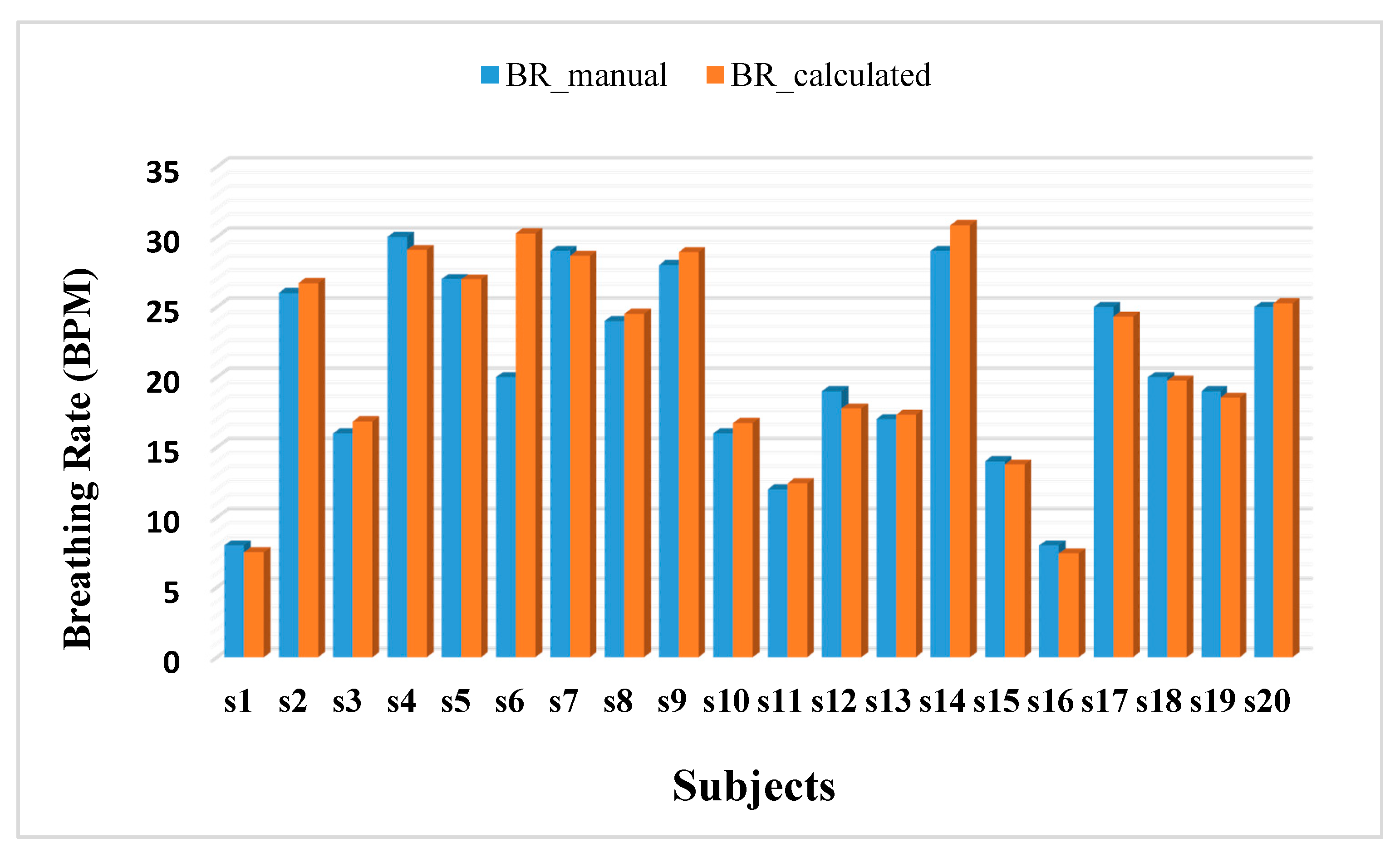
6.4. Experimental Results and Discussion
6.4.1. Computing Tidal Breathing Parameters
6.4.2. Comparison with Existing Relevant Works
7. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Chen, J.C.; Mannino, D.M. Worldwide epidemiology of chronic obstructive pulmonary disease. Curr. Opin. Pulm. Med. 1999, 5, 93. [Google Scholar] [CrossRef] [PubMed]
- Salvi, S.S.; Barnes, P.J. Chronic obstructive pulmonary disease in non-smokers. Lancet 2009, 374, 733–743. [Google Scholar] [CrossRef]
- Bhome, A.B. COPD in India: Iceberg or volcano. J. Thorac. Dis. 2012, 4, 298–309. [Google Scholar] [PubMed]
- Top Ten Causes of Death. Available online: http://www.who.int/mediacentre/factsheets/fs310/en/index3.html (accessed on 21 July 2017).
- Chronic Respiratory Diseases. Available online: http://www.who.int/gard/publications/chronic_respiratory_diseases.pdf (accessed on 21 July 2017).
- Sciurba, F.C. Physiologic similarities and differences between COPD and asthma. Chest 2004, 126, 117S–124S. [Google Scholar] [CrossRef]
- Schlegelmilch, R.M.; Kramme, R. Pulmonary function testing. In Springer Handbook of Medical Technology; Springer: Berlin/Heidelberg, Germany, 2011; pp. 95–117. [Google Scholar]
- Ruppel, G.L.; Enright, P.L. Pulmonary function testing. Respir. Care 2012, 57, 165–175. [Google Scholar] [CrossRef] [PubMed]
- Calonge, N.; Petitti, D.B.; DeWitt, T.G.; Gordis, L.; Dietrich, A.J.; Gregory, K.D.; Harris, R.P.; Isham, G.J.; LeFevre, M.L.; Leipzig, R.; et al. Screening for chronic obstructive pulmonary disease using spirometry. Ann. Intern. Med. 2008, 148, 529–534. [Google Scholar]
- Hamouda, A.; Manck, O.; Hafiane, M.L.; Bouguechal, N.E. An Enhanced Technique for Ultrasonic Flow Metering Featuring Very Low Jitter and Offset. Sensors 2016, 16, 1008. [Google Scholar] [CrossRef] [PubMed]
- Rhoades, J.N. Basic Pulmonary Function Testing, 1997. Available online: http://asthma.about.com/library/weekly/aa091597.htm (accessed on 21 July 2017).
- Pellegrino, R.; Viegi, G.; Brusasco, V.; Crapo, R.O.; Burgos, F.; Casaburi, R.E.A.; Coates, A.; Van Der Grinten, C.P.M.; Gustafsson, P.; Hankinson, J.; et al. Interpretative strategies for lung function tests. Eur. Respir. J. 2005, 26, 948–968. [Google Scholar] [CrossRef] [PubMed]
- Williams, E.M.; Powell, T.; Eriksen, M.; Neill, P.; Colasanti, R. A pilot study quantifying the shape of tidal breathing waveforms using centroids in health and COPD. J. Clin. Monit. Comput. 2014, 28, 67–74. [Google Scholar] [CrossRef] [PubMed]
- Van der Ent, C.K.; Brackel, H.J.; Van der Laag, J.; Bogaard, J.M. Tidal breathing analysis as a measure of airway obstruction in children three years of age and older. Am. J. Respir. Crit. Care Med. 1996, 153, 1253–1258. [Google Scholar] [CrossRef] [PubMed]
- Morris, M.J.; Lane, D.J. Tidal expiratory flow patterns in airflow obstruction. Thorax 1981, 36, 135–142. [Google Scholar] [CrossRef] [PubMed]
- Frey, U.; Silverman, M.; Suki, B. Analysis of the harmonic content of the tidal flow waveforms in infants. J. Appl. Physiol. 2001, 91, 1687–1693. [Google Scholar] [PubMed]
- Seppä, V.P.; Pelkonen, A.S.; Kotaniemi-Syrjänen, A.; Mäkelä, M.J.; Viik, J.; Malmberg, L.P. Tidal breathing flow measurement in awake young children by using impedance pneumography. J. Appl. Physiol. 2013, 115, 1725–1731. [Google Scholar]
- Bates, J.H.; Schmalisch, G.; Filbrun, D.; Stocks, J. Tidal breath analysis for infant pulmonary function testing. ERS/ATS task force on standards for infant respiratory function testing. European respiratory society/American thoracic society. Eur. Respir. J. 2000, 16, 1180–1192. [Google Scholar] [CrossRef] [PubMed]
- Van der Ent, C.K.; Brackel, H.J.; Mulder, P.; Bogaard, J.M. Improvement of tidal breathing pattern analysis in children with asthma by on-line automatic data processing. Eur. Respir. J. 1996, 9, 1306–1313. [Google Scholar] [CrossRef] [PubMed]
- Olden, C.; Symes, E.; Seddon, P. Measuring tidal breathing parameters using a volumetric vest in neonates with and without lung disease. Pediatr. Pulmonol. 2010, 45, 1070–1075. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, M.; Foitzik, B.; Wauer, R.R.; Winkler, F.; Schmalisch, G. Comparative investigations of algorithms for the detection of breaths in newborns with disturbed respiratory signals. Comput. Biomed. Res. 1998, 31, 413–425. [Google Scholar] [CrossRef] [PubMed]
- Stocks, J.; Dezateux, C.A.; Jackson, E.A.; Hoo, A.F.; Costeloe, K.L.; Wade, A.M. Analysis of tidal breathing parameters in infancy: How variable is TPTEF: TE? Am. J. Respir. Crit. Care Med. 1994, 150, 1347–1354. [Google Scholar] [CrossRef] [PubMed]
- Hudgel, D.W.; Martin, R.J.; Johnson, B.A.; Hill, P.A. Mechanics of the respiratory system and breathing pattern during sleep in normal humans. J. Appl. Physiol. 1984, 56, 133–137. [Google Scholar] [PubMed]
- Ranganathan, S.C.; Goetz, I.; Hoo, A.F.; Lum, S.; Castle, R.; Stocks, J. Assessment of tidal breathing parameters in infants with cystic fibrosis. Eur. Respir. J. 2003, 22, 761–766. [Google Scholar] [CrossRef] [PubMed]
- Palmer, J.; Julian, A.; Oscar, M. Tidal breathing analysis. Neo Rev. 2004, 5, e186–e193. [Google Scholar] [CrossRef]
- Fekr, A. R.; Radecka, R.; Zilic, Z. Design and evaluation of an intelligent remote tidal volume variability monitoring system in e-health applications. IEEE J. Biomed. Health Inform. 2015, 19, 1532–1548. [Google Scholar] [CrossRef] [PubMed]
- Araujo, G.A.L.; Freire, R.C.S.; Silva, J.F.; Oliveira, A.; Jaguaribe, E.F. Breathing Flow Measurement with Constant Temperature Hotwire Anemometer for Forced Oscillations Technique. In Proceedings of the 21st IEEE Instrumentation and Measurement Technology Conference, Como, Italy, 18–20 May 2004; pp. 730–733. [Google Scholar]
- Bai, Y.W.; Li, W.T.; Chen, Y.W. Design and implementation of an embedded monitor system for detection of a patient’s breath by double Webcams. In Proceedings of the 2010 IEEE International Workshop on Medical Measurements and Applications Proceedings (MeMeA), Ottawa, ON, Canada, 30 April–1 May 2010; pp. 93–98. [Google Scholar]
- McWilliams, J. Review of Air Flow Measurement Techniques; Lawrence Berkeley National Laboratory: Berkeley, CA, USA, 2002.
- Burgess, W.A.; Ellenbecker, M.J.; Treitman, R.D. Airflow Measurement Techniques. In Ventilation for Control of the Work Environment, 2nd ed.; John Willey and Sons: New York, NY, USA, 2004; pp. 43–89. [Google Scholar]
- Heldt, G.P.; Ward, R.J. Evaluation of Ultrasound-Based Sensor to Monitor Respiratory and Non respiratory Movement and Timing in Infants. IEEE Trans. Biomed. Eng. 2016, 63, 619–629. [Google Scholar] [CrossRef] [PubMed]
- Lázaro, J.; Alcaine, A.; Romero, D.; Gil, E.; Laguna, P.; Pueyo, E.; Bailón, R. Electrocardiogram derived respiratory rate from QRS slopes and R-wave angle. Ann. Biomed. Eng. 2014, 42, 2072–2083. [Google Scholar] [CrossRef] [PubMed]
- Fouzas, S.; Priftis, K.N.; Anthracopoulos, M.B. Pulse oximetry in pediatric practice. Pediatrics 2011, 128, 740–752. [Google Scholar] [CrossRef] [PubMed]
- Que, C.L.; Kolmaga, C.; Durand, L.G.; Kelly, S.M.; Macklem, P.T. Phonospirometry for noninvasive measurement of ventilation: Methodology and preliminary results. J. Appl. Physiol. 2002, 93, 1515–1526. [Google Scholar] [CrossRef] [PubMed]
- Seppa, V.P.; Viik, J.; Hyttinen, J. Assessment of pulmonary flow using impedance pneumography. IEEE Trans. Biomed. Eng. 2010, 57, 2277–2285. [Google Scholar] [CrossRef] [PubMed]
- Dei, D.; Grazzini, G.; Luzi, G.; Pieraccini, M.; Atzeni, C.; Boncinelli, S.; Camiciottoli, G.; Castellani, W.; Marsili, M.; Lo Dico, J. Non-contact detection of breathing using a microwave sensor. Sensors 2009, 9, 2574–2585. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.S.; Pathirana, P.N.; Steinfort, C.L.; Caelli, T. Monitoring and Analysis of Respiratory Patterns Using Microwave Doppler Radar. IEEE J. Trans. Eng. Health Med. 2014, 2, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Ciobotariu, R.; Rotariu, C.; Adochiei, F.; Costin, H. Wireless breathing system for long term telemonitoring of respiratory activity. In Proceedings of the IEEE 7th International Symposium Advanced Topics in Electrical Engineering (ATEE), Bucharest, Romania, 12–14 May 2011; pp. 1–4. [Google Scholar]
- Lowne, D.R.; Tarler, M. Designing a Low-Cost Mattress sensor for Automated Body Position Classification. In Proceedings of the IEEE 27th Annual International Conference Engineering in Medicine and Biology Society, Shanghai, China, 1–4 September 2005; pp. 6437–6440. [Google Scholar]
- Nepal, K.; Biegeleisen, E.; Ning, T. Apnea detection and respiration rate estimation through parametric modelling. In Proceedings of the IEEE 28th Annual Northeast Bioengineering Conference, Philadelphia, PA, USA, 21–21 April 2002; pp. 277–278. [Google Scholar]
- Thap, T.; Chung, H.; Jeong, C.; Hwang, K.E.; Kim, H.R.; Yoon, K.H.; Lee, J. High-Resolution Time-Frequency Spectrum-Based Lung Function Test from a Smartphone Microphone. Sensors 2016, 16, 1305. [Google Scholar] [CrossRef] [PubMed]
- Tadi, M.J.; Koivisto, T.; Pänkäälä, M.; Paasio, A. Accelerometer-based method for extracting respiratory and cardiac gating information for dual gating during nuclear medicine imaging. J. Biomed. Imaging 2014, 2014, 6. [Google Scholar]
- Knobloch, J. The Effect of Regular Peak Flow Meter Utilisation on Asthma Self-Management. Bachelor’s Thesis, Charles Darwin University, Casaurina, Australia, 2013. [Google Scholar]
- Raine, A.B.; Aslam, N.; Underwood, C.P.; Danaher, S. Development of an ultrasonic airflow measurement device for ducted air. Sensors 2015, 15, 10705–10722. [Google Scholar] [CrossRef] [PubMed]
- Gupta, J.K.; Lin, C.H.; Chen, Q. Characterizing exhaled airflow from breathing and talking. Indoor Air 2010, 1, 31–39. [Google Scholar] [CrossRef] [PubMed]
- Medina, C.; Segura, J.C.; De la Torre, A. Ultrasound indoor positioning system based on a low-power wireless sensor network providing sub-centimeter accuracy. Sensors 2013, 13, 3501–3526. [Google Scholar] [CrossRef] [PubMed]
- AD8302. Available online: http://www.analog.com/en/products/rf-microwave/rf-power-detectors/non-rms-responding-detector/ad8302.html#product-overview (accessed on 21 July 2017).
- AD8302 Datasheet. Available online: http://www.analog.com/media/en/technical-documentation/data-sheets/AD8302.pdf (accessed on 21 July 2017).
- Khasnobish, A.; Rakshit, R.; Sinharay, A.; Chakravarty, T. Phase-gain IC based novel design of tidal breathing pattern sensor for pulmonary disease diagnostics: Demo abstract. In Proceedings of the 16th ACM/IEEE International Conference on Information Processing in Sensor Networks, Pittsburgh, PA, USA, 18–20 April 2017; pp. 273–274. [Google Scholar]
- Medikro Calibration Syringe. Available online: http://www.medikro.com/products/accessories/medikro-calibration-syringe (accessed on 21 July 2017).
- Medikro Nano Spirometer. Available online: http://www.medikro.com/products/spirometers/medikro-nano-spirometer (accessed on 21 July 2017).
- Benchetrit, G. Breathing pattern in humans: Diversity and individuality. Respir. Physiol. 2000, 122, 123–129. [Google Scholar] [CrossRef]
- World Medical Association. World Medical Association Declaration of Helsinki: Ethical principles for medical research involving human subjects. J Postgrad. Med. 2013, 310, 2191–2194. [Google Scholar]
- Elcner, J.; Jedelsky, J.; Lizal, F.; Jicha, M. Velocity profiles in idealized model of human respiratory tract. EPJ Web Conf. 2013, 45, 01025–01029. [Google Scholar] [CrossRef]
- Reyes, B.; Reljin, N.; Kong, Y.; Nam, Y.; Chon, K. Tidal volume and instantaneous respiration rate estimation using a smartphone camera. IEEE J. Biomed. Health Inform. 2017, 21, 764–777. [Google Scholar] [CrossRef] [PubMed]
- Tang, J.W.; Nicolle, A.D.; Klettner, C.A.; Pantelic, J.; Wang, L.; Suhaimi, A.B.; Tan, A.Y.; Ong, G.W.; Su, R.; Sekhar, C.; et al. Airflow dynamics of human jets: Sneezing and breathing-potential sources of infectious aerosols. PLoS ONE 2013, 8, e59970. [Google Scholar] [CrossRef] [PubMed]
| Flow Rates | Slow | Medium | Fast | |||
|---|---|---|---|---|---|---|
| INSP | EXP | INSP | EXP | INSP | EXP | |
| AUC | 1.48 | 1.32 | 1.23 | 1.11 | 1.17 | 1.09 |
| Flow Rate | during Inspiration | during Expiration |
|---|---|---|
| Slow | 4.57 | 5.12 |
| Medium | 5.51 | 6.09 |
| High | 5.78 | 6.20 |
| Mean | 5.29 | 5.80 |
| PEF (L/s) | PIF (L/s) | |||||
|---|---|---|---|---|---|---|
| Subjects | Spirometer | TBPR | % Error | Spirometer | TBPR | % Error |
| 1 | 0.97 | 1.1 | 13.40 | 1.13 | 1.3 | 15.04 |
| 2 | 0.8 | 0.67 | 16.25 | 0.71 | 0.6 | 15.49 |
| 3 | 2.21 | 2.2 | 0.45 | 1.7 | 1.5 | 11.76 |
| 4 | 1.85 | 2.13 | 15.13 | 1.57 | 1.7 | 8.28 |
| 5 | 1.78 | 2.01 | 12.92 | 1.7 | 1.5 | 11.76 |
| Sub | BR (BPM) | TI (s) | TE (s) | DCy | PIF (L/s) | tPIF (s) | PEF (L/s) | tPEF (s) | VTins (L) | VTexp (L) | vINSP (m/s) | vEXP (m/s) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 7.51 (0.72) | 3.93 (0.19) | 3.59 (0.20) | 0.49 (0.03) | 1.03 (0.05) | 1.38 (0.15) | 1.60 (0.16) | 0.85 (0.09) | 2.75 (0.27) | 2.59 (0.16) | 2.33 (0.11) | 3.49 (0.12) |
| 2 | 26.7 (1.11) | 1.19 (0.17) | 1.07 (0.08) | 0.51 (0.04) | 0.82 (0.04) | 0.53 (0.02) | 0.98 (0.16) | 0.58 (0.16) | 0.61 (0.07) | 0.64 (0.10) | 1.84 (0.11) | 2.21 (0.31) |
| 3 | 16.84 (1.01) | 1.83 (0.03) | 1.68 (0.15) | 0.50 (0.04) | 1.41 (0.01) | 0.92 (0.05) | 1.73 (0.03) | 0.65 (0.02) | 1.70 (0.03) | 1.82 (0.05) | 3.19 (0.01) | 4.1 (0.04) |
| 4 | 29.06 (0.91) | 1.04 (0.11) | 0.98 (0.06) | 0.51 (0.03) | 0.92 (0.05) | 0.52 (0.03) | 1.04 (0.01) | 0.47 (0.01) | 0.63 (0.01) | 0.64 (0.01) | 2.08 (0.13) | 2.35 (0.01) |
| 5 | 26.96 (1.5) | 1.06 (0.08) | 1.01 (0.05) | 0.51 (0.01) | 1.7 (0.05) | 0.53 (0.06) | 1.37 (0.01) | 0.48 (0.01) | 0.88 (0.04) | 0.89 (0.04) | 3.12 (0.13) | 3.86 (0.01) |
| 6 | 30.24 (0.87) | 1.04 (0.06) | 0.97 (0.02) | 0.51 (0.01) | 1.06 (0.01) | 0.52 (0.01) | 1.21 (0.01) | 0.47 (0.01) | 0.72 (0.04) | 0.74 (0.03) | 2.75 (0.01) | 3.31 (0.06) |
| 7 | 28.64 (2.77) | 1.18 (0.08) | 1.10 (0.08) | 0.52 (0.01) | 1.38 (0.04) | 0.58 (0.02) | 1.57 (0.06) | 0.53 (0.01) | 1.06 (0.04) | 1.11 (0.02) | 3.11 (0.11) | 3.59 (0.13) |
| 8 | 24.51 (3.9) | 1.57 (0.23) | 1.37 (0.15) | 0.53 (0.01) | 1.44 (0.01) | 0.71 (0.12) | 1.75 (0.06) | 0.65 (0.04) | 1.49 (0.13) | 1.45 (0.10) | 3.26 (0.04) | 3.98 (0.15) |
| 9 | 28.90 (1.95) | 1.15 (0.13) | 1.05 (0.05) | 0.52 (0.02) | 1.25 (0.03) | 0.58 (0.01) | 1.47 (0.09) | 0.50 (0.01) | 0.95 (0.05) | 0.99 (0.10) | 2.82 (0.07) | 3.34 (0.29) |
| 10 | 16.73 (0.34) | 2..02 (0.02) | 1.66 (0.08) | 0.56 (0.02) | 1.63 (0.07) | 0.88 (0.06) | 2.27 (0.04) | 0.69 (0.01) | 2.26 (0.04) | 2.23 (0.04) | 3.82 (0.16) | 5.12 (0.09) |
| 11 | 12.42 (0.61) | 2.82 (0.21) | 1.92 (0.12) | 0.56 (0.04) | 1.43 (0.03) | 1.03 (0.27) | 2.07 (0.13) | 0.89 (0.10) | 2.10 (0.11) | 2.13 (0.02) | 3.23 (0.04) | 4.68 (0.03) |
| 12 | 17.76 (1.05) | 1.81 (0.10) | 1.53 (0.07) | 0.52 (0.02) | 1.34 (0.17) | 0.70 (0.02) | 1.56 (0.01) | 0.86 (0.16) | 1.48 (0.04) | 1.32 (0.17) | 3.02 (0.38) | 3.54 (0.21) |
| 13 | 17.31 (0.41) | 1.89 (0.14) | 1.60 (0.07) | 0.54 (0.02) | 1.46 (0.05) | 0.94 (0.11) | 1.94 (0.06) | 0.66 (0.05) | 1.80 (0.09) | 1.90 (0.11) | 3.29 (0.11) | 4.58 (0.11) |
| 14 | 30.84 (1.58) | 0.97 (0.15) | 0.93 (0.06) | 0.51 (0.01) | 0.96 (0.16) | 0.49 (0.53) | 1.06 (0.27) | 0.43 (1.09) | 0.60 (0.03) | 0.62 (0.02) | 2.17 (0.27) | 2.34 (0.49) |
| 15 | 13.76 (0.88) | 2.46 (0.17) | 1.86 (0.16) | 0.54 (0.01) | 1.37 (0.05) | 1.01 (0.20) | 1.99 (0.22) | 0.80 (0.01) | 2.15 (0.21) | 2.22 (0.27) | 3.09 (0.12) | 4.51 (0.51) |
| 16 | 7.42 (0.64) | 4.15 (0.36) | 3.47 (0.21) | 0.57 (0.01) | 1.29 (0.04) | 1.26 (0.21) | 2.12 (0.06) | 0.83 (0.02) | 3.30 (0.05) | 3.39 (0.01) | 2.92 (0.06) | 5.08 (0.04) |
| 17 | 24.30 (3.12) | 1.42 (0.21) | 1.40 (0.18) | 0.50 (0.03) | 1.65 (0.06) | 0.75 (0.08) | 1.73 (0.07) | 0.59 (0.02) | 1.54 (0.05) | 1.60 (0.05) | 3.73 (0.12) | 3.99 (0.16) |
| 18 | 19.75 (0.42) | 1.64 (0.04) | 1.36 (0.01) | 0.56 (0.01) | 1.12 (0.09) | 0.76 (0.07) | 1.60 (0.34) | 0.64 (0.02) | 1.21 (0.11) | 1.37 (0.16) | 2.54 (0.21) | 3.67 (0.76) |
| 19 | 18.53 (0.89) | 1.82 (0.03) | 1.48 (0.03) | 0.55 (0.02) | 1.32 (0.07) | 0.75 (0.09) | 1.79 (0.03) | 0.66 (0.01) | 1.66 (0.05) | 1.65 (0.01) | 2.97 (0.15) | 4.23 (0.04) |
| 20 | 25.26 (1.62) | 1.29 (0.05) | 1.18 (0.06) | 0.51 (0.02) | 1.22 (0.13) | 0.68 (0.04) | 1.35 (0.19) | 0.53 (0.01) | 0.03 (0.11) | 1.01 (0.09) | 2..74 (0.18) | 3.05 (0.38) |
| Approaches | BR (BPM) | TI (s) | TE (s) | DCy | PIF (L/s) | tPIF (s) | PEF (L/s) | tPEF (s) | VTins (L) | VTexp (L) | vins (m/s) | vexp (m/s) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| TBPR | 7–30 | 1.81 ± 0.18 | 1.56 ± 0.17 | 0.53 ± 0.02 | 1.27 ± 0.23 | 0.77 ± 0.41 | 1.62 ± 0.32 | 0.69 ± 0.14 | 1.49 ± 0.74 | 1.51 ± 0.74 | 2.86 ± 0.52 | 3.76 ± 0.68 |
| [13] N = 24 | - | 1.9 ± 0.5 | 2.7 ± 0.7 | 0.41 ± 0.2 | 0.83 ± 0.4 | 0.8 ± 0.2 | 0.64 ± 0.2 | 1 ± 0.4 | 0.98 ± 0.18 | - | - | |
| [52] (review) | 6 to 31 | - | - | - | - | - | - | - | 0.45–1.6 | - | - | |
| [54] (simulation) | - | - | - | - | - | - | - | - | - | 0.79–3.16 | - | |
| [23] N = 16 | 14 ± 0.4 | 1.82 ± 0.13 | 2.37 ± 0.12 | - | - | - | - | - | 0.77 ± 0.11 | - | - | |
| [55] N = 15 | 11–35 | - | - | - | - | - | - | - | 0.3–3 | - | - | |
| [56] N = 20 | - | - | - | - | - | - | - | - | - | 4.7 1.4 (nasal) | ||
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sinharay, A.; Rakshit, R.; Khasnobish, A.; Chakravarty, T.; Ghosh, D.; Pal, A. The Ultrasonic Directional Tidal Breathing Pattern Sensor: Equitable Design Realization Based on Phase Information. Sensors 2017, 17, 1853. https://doi.org/10.3390/s17081853
Sinharay A, Rakshit R, Khasnobish A, Chakravarty T, Ghosh D, Pal A. The Ultrasonic Directional Tidal Breathing Pattern Sensor: Equitable Design Realization Based on Phase Information. Sensors. 2017; 17(8):1853. https://doi.org/10.3390/s17081853
Chicago/Turabian StyleSinharay, Arijit, Raj Rakshit, Anwesha Khasnobish, Tapas Chakravarty, Deb Ghosh, and Arpan Pal. 2017. "The Ultrasonic Directional Tidal Breathing Pattern Sensor: Equitable Design Realization Based on Phase Information" Sensors 17, no. 8: 1853. https://doi.org/10.3390/s17081853
APA StyleSinharay, A., Rakshit, R., Khasnobish, A., Chakravarty, T., Ghosh, D., & Pal, A. (2017). The Ultrasonic Directional Tidal Breathing Pattern Sensor: Equitable Design Realization Based on Phase Information. Sensors, 17(8), 1853. https://doi.org/10.3390/s17081853





