Special Issue “The Angiotensin in Human Health and Diseases”
Funding
Conflicts of Interest
List of Contributions
- 1.
- Zhang, B.; Liu, Z.; Chang, Y.; Lv, R.; Guo, H.; Qiang, P.; Shimosawa, T.; Xu, Q.; Yang, F. Aldosterone-Induced Transformation of Vascular Smooth Muscle Cells into Macrophage-like Cells Participates in Inflammatory Vascular Lesions. Int. J. Mol. Sci. 2025, 26, 3345.
- 2.
- Forster, P.; Wysocki, J.; Abedini, Y.; Müller, T.; Ye, M.; Ferrario, C.M.; Batlle, D. Aminopeptidase A Effect on Angiotensin Peptides and Their Blood Pressure Action. Int. J. Mol. Sci. 2025, 26, 6990.
- 3.
- Kamiyama, M.; Iijima, K.; Okuzawa, R.; Kawata, R.; Kimura, A.; Shinohara, Y.; Shimada, A.; Yamanaka, M.; Youda, A.; Iwamoto, T. Augmented Intrarenal and Urinary Angiotensinogen in Diabetic Nephropathy: The Role of Isoflavones. Int. J. Mol. Sci. 2025, 26, 1443.
- 4.
- Mkhize, B.C.; Mosili, P.; Ngubane, P.S.; Sibiya, N.H.; Khathi, A. Increased Plasma Levels of ACE and Ang II in Prediabetes May Contribute to Adipose Tissue Dysfunction. Int. J. Mol. Sci. 2025, 26, 5517.
- 5.
- McGrath, M.S.; Wentworth, B.J. The Renin-Angiotensin System in Liver Disease. Int. J. Mol. Sci. 2024, 25, 5807.
- 6.
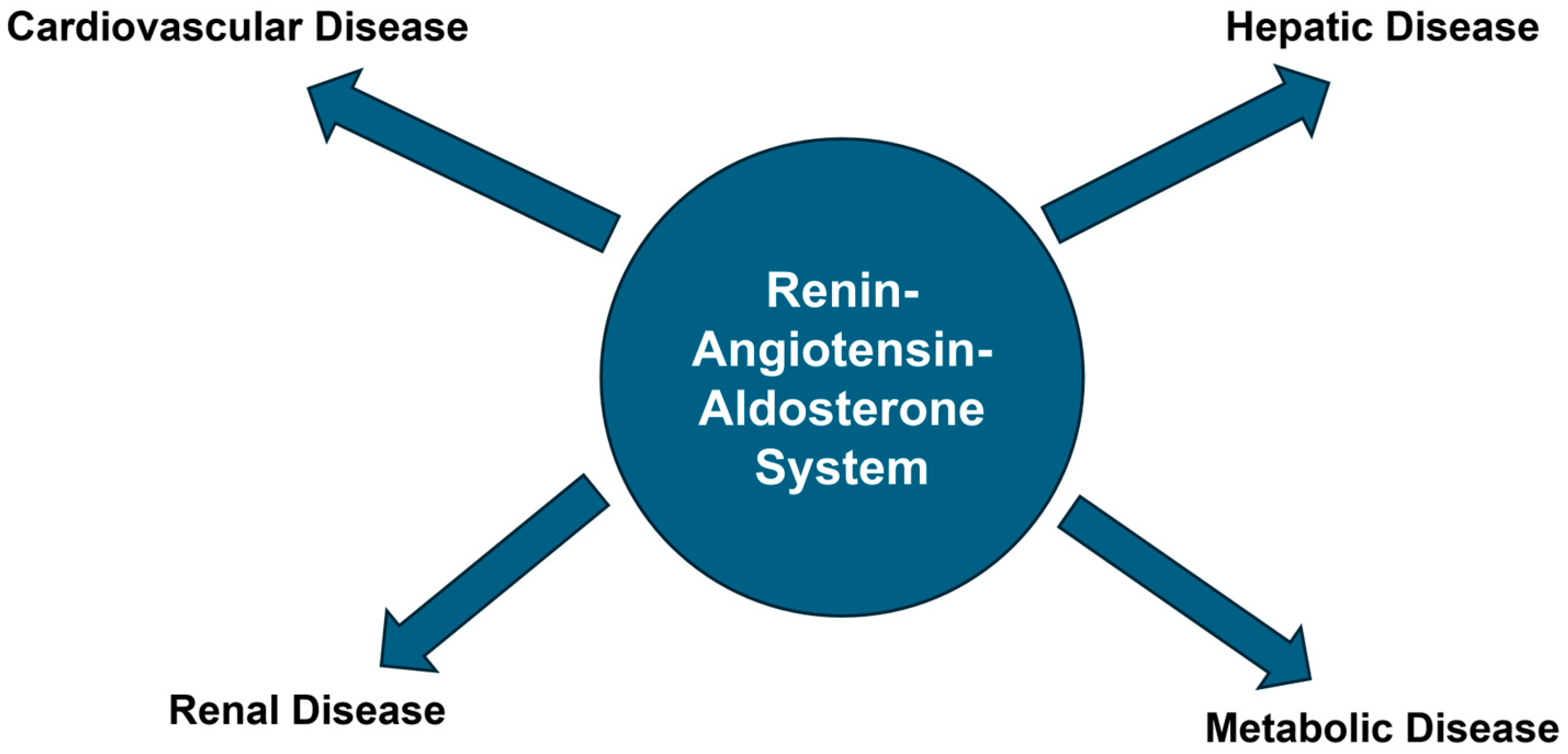
- Tain, Y.L.; Hsu, C.N. The Renin-Angiotensin System and Cardiovascular-Kidney-Metabolic Syndrome: Focus on Early-Life Programming. Int. J. Mol. Sci. 2024, 25, 3298.
References
- Carey, R.M.; Siragy, H.M. Newly recognized components of the renin-angiotensin system: Potential roles in cardiovascular and renal regulation. Endocr. Rev. 2003, 24, 261–271. [Google Scholar] [CrossRef] [PubMed]
- Jankowski, P.; Safar, M.E.; Benetos, A. Pleiotropic effects of drugs inhibiting the renin-angiotensin-aldosterone system. Curr. Pharm. Des. 2009, 15, 571–584. [Google Scholar] [CrossRef] [PubMed]
- Cantero-Navarro, E.; Fernández-Fernández, B.; Ramos, A.M.; Rayego-Mateos, S.; Rodrigues-Diez, R.R.; Sánchez-Niño, M.D.; Sanz, A.B.; Ruiz-Ortega, M.; Ortiz, A. Renin-angiotensin system and inflammation update. Mol. Cell. Endocrinol. 2021, 529, 111254. [Google Scholar] [CrossRef] [PubMed]
- Jia, G.; Aroor, A.R.; Hill, M.A.; Sowers, J.R. Role of Renin-Angiotensin-Aldosterone System Activation in Promoting Cardiovascular Fibrosis and Stiffness. Hypertension 2018, 72, 537–548. [Google Scholar] [CrossRef] [PubMed]
- Sebastian, S.A.; Padda, I.; Johal, G. Cardiovascular-Kidney-Metabolic (CKM) syndrome: A state-of-the-art review. Curr. Probl. Cardiol. 2024, 49, 102344. [Google Scholar] [CrossRef] [PubMed]
- Brasier, A.R.; Recinos, A., 3rd; Eledrisi, M.S. Vascular inflammation and the renin-angiotensin system. Arter. Thromb. Vasc. Biol. 2002, 22, 1257–1266. [Google Scholar] [CrossRef] [PubMed]
- Thethi, T.; Kamiyama, M.; Kobori, H. The link between the renin-angiotensin-aldosterone system and renal injury in obesity and the metabolic syndrome. Curr. Hypertens Rep. 2012, 14, 160–169. [Google Scholar] [CrossRef] [PubMed]
- Mkhize, B.C.; Mosili, P.; Ngubane, P.S.; Sibiya, N.H.; Khathi, A. Diet-induced prediabetes: Effects on the activity of the renin-angiotensin-aldosterone system in selected organs. J. Diabetes Investig. 2022, 13, 768–780. [Google Scholar] [CrossRef] [PubMed]
- Padmanabhan, S.; Dominiczak, A.F. Genomics of hypertension: The road to precision medicine. Nat. Rev. Cardiol. 2021, 18, 235–250. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Siragy, H.M. Special Issue “The Angiotensin in Human Health and Diseases”. Int. J. Mol. Sci. 2025, 26, 11940. https://doi.org/10.3390/ijms262411940
Siragy HM. Special Issue “The Angiotensin in Human Health and Diseases”. International Journal of Molecular Sciences. 2025; 26(24):11940. https://doi.org/10.3390/ijms262411940
Chicago/Turabian StyleSiragy, Helmy M. 2025. "Special Issue “The Angiotensin in Human Health and Diseases”" International Journal of Molecular Sciences 26, no. 24: 11940. https://doi.org/10.3390/ijms262411940
APA StyleSiragy, H. M. (2025). Special Issue “The Angiotensin in Human Health and Diseases”. International Journal of Molecular Sciences, 26(24), 11940. https://doi.org/10.3390/ijms262411940




