Epigenetics of Endometrial Cancer: The Role of Chromatin Modifications and Medicolegal Implications
Abstract
1. Introduction
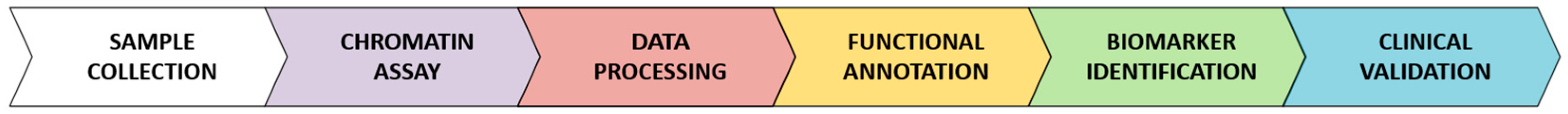
2. Results
2.1. Molecular Bases of Chromatin Modification in Endometrial Cancer
Driver and Passenger Mutations
2.2. Role of DNA Methylation in EC
2.3. Histone Modifications and Chromatin Remodeling in EC
2.4. Using Chromatin Modifications as Diagnostic, Prognostic, and Therapeutic Tools in EC
2.5. Limitations of Identifying EC Biomarkers Using Chromatin Modifications
2.6. Medico-Legal Framework
3. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Concin, N.; Matias-Guiu, X.; Vergote, I.; Cibula, D.; Mirza, M.R.; Marnitz, S.; Ledermann, J.; Bosse, T.; Chargari, C.; Fagotti, A.; et al. ESGO/ESTRO/ESP Guidelines for the Management of Patients with Endometrial Carcinoma. Radiother. Oncol. 2021, 154, 327–353. [Google Scholar] [CrossRef]
- Leone Roberti Maggiore, U.; Khamisy-Farah, R.; Bragazzi, N.L.; Bogani, G.; Martinelli, F.; Lopez, S.; Chiappa, V.; Signorelli, M.; Ditto, A.; Raspagliesi, F. Fertility-Sparing Treatment of Patients with Endometrial Cancer: A Review of the Literature. J. Clin. Med. 2021, 10, 4784. [Google Scholar] [CrossRef]
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef]
- Gullo, G.; Cucinella, G.; Chiantera, V.; Dellino, M.; Cascardi, E.; Török, P.; Herman, T.; Garzon, S.; Uccella, S.; Laganà, A.S. Fertility-Sparing Strategies for Early-Stage Endometrial Cancer: Stepping towards Precision Medicine Based on the Molecular Fingerprint. Int. J. Mol. Sci. 2023, 24, 811. [Google Scholar] [CrossRef]
- Huvila, J.; Pors, J.; Thompson, E.F.; Gilks, C.B. Endometrial Carcinoma: Molecular Subtypes, Precursors and the Role of Pathology in Early Diagnosis. J. Pathol. 2021, 253, 355–365. [Google Scholar] [CrossRef] [PubMed]
- Billone, V.; De Paola, L.; Conti, E.; Borsellino, L.; Kozinszky, Z.; Giampaolino, P.; Suranyi, A.; Della Corte, L.; Andrisani, A.; Cucinella, G.; et al. Sentinel Lymph Node in Endometrial Hyperplasia: State of the Art and Future Perspectives. Cancers 2025, 17, 776. [Google Scholar] [CrossRef] [PubMed]
- Gallo, A.; Catena, U.; Saccone, G.; Di Spiezio Sardo, A. Conservative Surgery in Endometrial Cancer. J. Clin. Med. 2021, 11, 183. [Google Scholar] [CrossRef] [PubMed]
- Cai, Y.; Wang, B.; Xu, W.; Liu, K.; Gao, Y.; Guo, C.; Chen, J.; Kamal, M.A.; Yuan, C. Endometrial Cancer: Genetic, Metabolic Characteristics, Therapeutic Strategies and Nanomedicine. Curr. Med. Chem. 2021, 28, 8755–8781. [Google Scholar] [CrossRef]
- Paola, L.D.; Napoletano, G.; Gullo, G.; Circosta, F.; Vergallo, G.M.; Marinelli, S. The Era of Increasing Cancer Survivorship: Trends in Fertility Preservation, Medico-Legal Implications, and Ethical Challenges. Open Med. 2025, 20, 20251144. [Google Scholar] [CrossRef]
- Centini, G.; Colombi, I.; Ianes, I.; Perelli, F.; Ginetti, A.; Cannoni, A.; Habib, N.; Negre, R.R.; Martire, F.G.; Raimondo, D.; et al. Fertility Sparing in Endometrial Cancer: Where Are We Now? Cancers 2025, 17, 112. [Google Scholar] [CrossRef]
- Ronsini, C.; Romeo, P.; Andreoli, G.; Palmara, V.; Palumbo, M.; Caruso, G.; De Franciscis, P.; Vizzielli, G.; Restaino, S.; Chiantera, V.; et al. Fertility-Sparing Treatments in Endometrial Cancer: A Comprehensive Review on Efficacy, Oncological Outcomes, and Reproductive Potential. Medicina 2025, 61, 471. [Google Scholar] [CrossRef] [PubMed]
- Mutlu, L.; Manavella, D.D.; Gullo, G.; McNamara, B.; Santin, A.D.; Patrizio, P. Endometrial Cancer in Reproductive Age: Fertility-Sparing Approach and Reproductive Outcomes. Cancers 2022, 14, 5187. [Google Scholar] [CrossRef] [PubMed]
- Gullo, G.; Scaglione, M.; Cucinella, G.; Perino, A.; Chiantera, V.; D’Anna, R.; Laganà, A.S.; Buzzaccarini, G. Impact of Assisted Reproduction Techniques on the Neuro-Psycho-Motor Outcome of Newborns: A Critical Appraisal. J. Obstet. Gynaecol. 2022, 42, 2583–2587. [Google Scholar] [CrossRef]
- Medenica, S.; Abazovic, D.; Ljubić, A.; Vukovic, J.; Begovic, A.; Cucinella, G.; Zaami, S.; Gullo, G. The Role of Cell and Gene Therapies in the Treatment of Infertility in Patients with Thyroid Autoimmunity. Int. J. Endocrinol. 2022, 2022, 4842316. [Google Scholar] [CrossRef]
- Prapas, Y.; Ravanos, K.; Petousis, S.; Panagiotidis, Y.; Papatheodorou, A.; Margioula-Siarkou, C.; Iuliano, A.; Gullo, G.; Prapas, N. GnRH Antagonist Administered Twice the Day before hCG Trigger Combined with a Step-down Protocol May Prevent OHSS in IVF/ICSI Antagonist Cycles at Risk for OHSS without Affecting the Reproductive Outcomes: A Prospective Randomized Control Trial. J. Assist. Reprod. Genet. 2017, 34, 1537–1545. [Google Scholar] [CrossRef]
- Pino, I.; Gozzini, E.; Radice, D.; Boveri, S.; Iacobone, A.D.; Vidal Urbinati, A.M.; Multinu, F.; Gullo, G.; Cucinella, G.; Franchi, D. Advancing Tailored Treatments: A Predictive Nomogram, Based on Ultrasound and Laboratory Data, for Assessing Nodal Involvement in Endometrial Cancer Patients. J. Clin. Med. 2024, 13, 496. [Google Scholar] [CrossRef]
- Stampoliou, A.; Arapantoni-Dadioti, P.; Pavlakis, K. Epigenetic Mechanisms in Endometrial Cancer. J. BUON 2016, 21, 301–306. [Google Scholar]
- Inoue, F.; Sone, K.; Toyohara, Y.; Takahashi, Y.; Kukita, A.; Hara, A.; Taguchi, A.; Tanikawa, M.; Tsuruga, T.; Osuga, Y. Targeting Epigenetic Regulators for Endometrial Cancer Therapy: Its Molecular Biology and Potential Clinical Applications. Int. J. Mol. Sci. 2021, 22, 2305. [Google Scholar] [CrossRef]
- Farkas, S.A.; Sorbe, B.G.; Nilsson, T.K. Epigenetic Changes as Prognostic Predictors in Endometrial Carcinomas. Epigenetics 2017, 12, 19–26. [Google Scholar] [CrossRef] [PubMed]
- Chandrashekhar, P.; Minooei, F.; Arreguin, W.; Masigol, M.; Steinbach-Rankins, J.M. Perspectives on Existing and Novel Alternative Intravaginal Probiotic Delivery Methods in the Context of Bacterial Vaginosis Infection. AAPS J. 2021, 23, 66. [Google Scholar] [CrossRef]
- Balla, B.; Illés, A.; Tobiás, B.; Pikó, H.; Beke, A.; Sipos, M.; Lakatos, P.; Kósa, J.P. The Role of the Vaginal and Endometrial Microbiomes in Infertility and Their Impact on Pregnancy Outcomes in Light of Recent Literature. Int. J. Mol. Sci. 2024, 25, 13227. [Google Scholar] [CrossRef]
- Bernabeu, A.; Lledo, B.; Díaz, M.C.; Lozano, F.M.; Ruiz, V.; Fuentes, A.; Lopez-Pineda, A.; Moliner, B.; Castillo, J.C.; Ortiz, J.A.; et al. Effect of the Vaginal Microbiome on the Pregnancy Rate in Women Receiving Assisted Reproductive Treatment. J. Assist. Reprod. Genet. 2019, 36, 2111–2119. [Google Scholar] [CrossRef] [PubMed]
- Gullo, G.; Satullo, M.; Billone, V.; De Paola, L.; Petousis, S.; Kotlik, Y.; Margioula-Siarkou, C.; Perino, A.; Cucinella, G. The Role of the Genital Tract Microbiome in Human Fertility: A Literature Review. J. Clin. Med. 2025, 14, 2923. [Google Scholar] [CrossRef]
- Gambioli, R.; Forte, G.; Aragona, C.; Bevilacqua, A.; Bizzarri, M.; Unfer, V. The Use of D-Chiro-Inositol in Clinical Practice. Eur. Rev. Med. Pharmacol. Sci. 2021, 25, 438–446. [Google Scholar] [CrossRef] [PubMed]
- Olcha, P.; Winiarska-Mieczan, A.; Kwiecień, M.; Nowakowski, Ł.; Miturski, A.; Semczuk, A.; Kiczorowska, B.; Gałczyński, K. Antioxidative, Anti-Inflammatory, Anti-Obesogenic, and Antidiabetic Properties of Tea Polyphenols-The Positive Impact of Regular Tea Consumption as an Element of Prophylaxis and Pharmacotherapy Support in Endometrial Cancer. Int. J. Mol. Sci. 2022, 23, 6703. [Google Scholar] [CrossRef]
- Liu, D.; Liu, X. Polyphenols as microRNA Modulator in Endometrial Cancer: Implications for Apoptosis Induction. Mol. Genet. Genomics 2025, 300, 34. [Google Scholar] [CrossRef]
- Desai, S.A.; Patel, V.P.; Bhosle, K.P.; Nagare, S.D.; Thombare, K.C. The Tumor Microenvironment: Shaping Cancer Progression and Treatment Response. J. Chemother. 2025, 37, 15–44. [Google Scholar] [CrossRef] [PubMed]
- Kay, E.J.; Zanivan, S. The Tumor Microenvironment Is an Ecosystem Sustained by Metabolic Interactions. Cell Rep. 2025, 44, 115432. [Google Scholar] [CrossRef]
- Wang, Y.; Zhou, H.; Ju, S.; Dong, X.; Zheng, C. The Solid Tumor Microenvironment and Related Targeting Strategies: A Concise Review. Front. Immunol. 2025, 16, 1563858. [Google Scholar] [CrossRef]
- Chen, M.; Linstra, R.; van Vugt, M.A.T.M. Genomic Instability, Inflammatory Signaling and Response to Cancer Immunotherapy. Biochim. Biophys. Acta Rev. Cancer 2022, 1877, 188661. [Google Scholar] [CrossRef]
- Hosea, R.; Hillary, S.; Naqvi, S.; Wu, S.; Kasim, V. The Two Sides of Chromosomal Instability: Drivers and Brakes in Cancer. Signal Transduct. Target. Ther. 2024, 9, 75. [Google Scholar] [CrossRef]
- Aparisi, F.; Amado-Labrador, H.; Calabuig-Fariñas, S.; Torres, S.; Herreros-Pomares, A. Passenger Mutations in Cancer Evolution. Cancer Rep. Rev. 2019, 3, 1–8. [Google Scholar] [CrossRef]
- McFarland, C.D.; Yaglom, J.A.; Wojtkowiak, J.W.; Scott, J.G.; Morse, D.L.; Sherman, M.Y.; Mirny, L.A. The Damaging Effect of Passenger Mutations on Cancer Progression. Cancer Res. 2017, 77, 4763–4772. [Google Scholar] [CrossRef]
- Kumar, S.; Warrell, J.; Li, S.; McGillivray, P.D.; Meyerson, W.; Salichos, L.; Harmanci, A.; Martinez-Fundichely, A.; Chan, C.W.Y.; Nielsen, M.M.; et al. Passenger Mutations in More Than 2,500 Cancer Genomes: Overall Molecular Functional Impact and Consequences. Cell 2020, 180, 915–927.e16. [Google Scholar] [CrossRef] [PubMed]
- Futreal, P.A.; Coin, L.; Marshall, M.; Down, T.; Hubbard, T.; Wooster, R.; Rahman, N.; Stratton, M.R. A Census of Human Cancer Genes. Nat. Rev. Cancer 2004, 4, 177–183. [Google Scholar] [CrossRef] [PubMed]
- Parsons, D.W.; Jones, S.; Zhang, X.; Lin, J.C.-H.; Leary, R.J.; Angenendt, P.; Mankoo, P.; Carter, H.; Siu, I.-M.; Gallia, G.L.; et al. An Integrated Genomic Analysis of Human Glioblastoma Multiforme. Science 2008, 321, 1807–1812. [Google Scholar] [CrossRef] [PubMed]
- Lawrence, M.S.; Stojanov, P.; Mermel, C.H.; Robinson, J.T.; Garraway, L.A.; Golub, T.R.; Meyerson, M.; Gabriel, S.B.; Lander, E.S.; Getz, G. Discovery and Saturation Analysis of Cancer Genes across 21 Tumour Types. Nature 2014, 505, 495–501. [Google Scholar] [CrossRef]
- Watanabe, T.; Nanamiya, H.; Kojima, M.; Nomura, S.; Furukawa, S.; Soeda, S.; Tanaka, D.; Isogai, T.; Imai, J.-I.; Watanabe, S.; et al. Clinical Relevance of Oncogenic Driver Mutations Identified in Endometrial Carcinoma. Transl. Oncol. 2021, 14, 101010. [Google Scholar] [CrossRef]
- Cancer Genome Atlas Research Network; Kandoth, C.; Schultz, N.; Cherniack, A.D.; Akbani, R.; Liu, Y.; Shen, H.; Robertson, A.G.; Pashtan, I.; Shen, R.; et al. Integrated Genomic Characterization of Endometrial Carcinoma. Nature 2013, 497, 67–73. [Google Scholar] [CrossRef]
- Bailey, M.H.; Tokheim, C.; Porta-Pardo, E.; Sengupta, S.; Bertrand, D.; Weerasinghe, A.; Colaprico, A.; Wendl, M.C.; Kim, J.; Reardon, B.; et al. Comprehensive Characterization of Cancer Driver Genes and Mutations. Cell 2018, 173, 371–385.e18. [Google Scholar] [CrossRef]
- Stan, A.; Bosart, K.; Kaur, M.; Vo, M.; Escorcia, W.; Yoder, R.J.; Bouley, R.A.; Petreaca, R.C. Detection of Driver Mutations and Genomic Signatures in Endometrial Cancers Using Artificial Intelligence Algorithms. PLoS ONE 2024, 19, e0299114. [Google Scholar] [CrossRef]
- Schübeler, D. Function and Information Content of DNA Methylation. Nature 2015, 517, 321–326. [Google Scholar] [CrossRef] [PubMed]
- Xiong, Y.; Dowdy, S.C.; Xue, A.; Shujuan, J.; Eberhardt, N.L.; Podratz, K.C.; Jiang, S.-W. Opposite Alterations of DNA Methyltransferase Gene Expression in Endometrioid and Serous Endometrial Cancers. Gynecol. Oncol. 2005, 96, 601–609. [Google Scholar] [CrossRef] [PubMed]
- Liao, X.; Siu, M.K.-Y.; Chan, K.Y.-K.; Wong, E.S.-Y.; Ngan, H.Y.-S.; Chan, Q.K.-Y.; Li, A.S.-M.; Khoo, U.-S.; Cheung, A.N.-Y. Hypermethylation of RAS Effector Related Genes and DNA Methyltransferase 1 Expression in Endometrial Carcinogenesis. Int. J. Cancer 2008, 123, 296–302. [Google Scholar] [CrossRef] [PubMed]
- Edwards, J.R.; O’Donnell, A.H.; Rollins, R.A.; Peckham, H.E.; Lee, C.; Milekic, M.H.; Chanrion, B.; Fu, Y.; Su, T.; Hibshoosh, H.; et al. Chromatin and Sequence Features That Define the Fine and Gross Structure of Genomic Methylation Patterns. Genome Res. 2010, 20, 972–980. [Google Scholar] [CrossRef]
- Ma, X.; Gao, X. Epigenetic Modifications and Carcinogenesis of Human Endometrial Cancer. Austin. J. Clin. Pathol. 2014, 1, 1014. [Google Scholar]
- Visnovsky, J.; Fiolka, R.; Kudela, E.; Slavik, P.; Krkoska, M.; Lasabová, Z.; Danko, J. Hypermethylation of Selected Genes in Endometrial Carcinogenesis. Neuro Endocrinol. Lett. 2013, 34, 675–680. [Google Scholar]
- Pan, Y.; Liu, G.; Zhou, F.; Su, B.; Li, Y. DNA Methylation Profiles in Cancer Diagnosis and Therapeutics. Clin. Exp. Med. 2018, 18, 1–14. [Google Scholar] [CrossRef]
- Lakshminarasimhan, R.; Liang, G. The Role of DNA Methylation in Cancer. Adv. Exp. Med. Biol. 2016, 945, 151–172. [Google Scholar] [CrossRef]
- Nishiyama, A.; Nakanishi, M. Navigating the DNA Methylation Landscape of Cancer. Trends Genet. 2021, 37, 1012–1027. [Google Scholar] [CrossRef]
- Wong, Y.F.; Chung, T.K.; Cheung, T.H.; Nobori, T.; Yu, A.L.; Yu, J.; Batova, A.; Lai, K.W.; Chang, A.M. Methylation of p16INK4A in Primary Gynecologic Malignancy. Cancer Lett. 1999, 136, 231–235. [Google Scholar] [CrossRef] [PubMed]
- Whitcomb, B.P.; Mutch, D.G.; Herzog, T.J.; Rader, J.S.; Gibb, R.K.; Goodfellow, P.J. Frequent HOXA11 and THBS2 Promoter Methylation, and a Methylator Phenotype in Endometrial Adenocarcinoma. Clin. Cancer Res. 2003, 9, 2277–2287. [Google Scholar]
- Kang, S.; Kim, J.W.; Kang, G.H.; Lee, S.; Park, N.H.; Song, Y.S.; Park, S.Y.; Kang, S.B.; Lee, H.P. Comparison of DNA Hypermethylation Patterns in Different Types of Uterine Cancer: Cervical Squamous Cell Carcinoma, Cervical Adenocarcinoma and Endometrial Adenocarcinoma. Int. J. Cancer 2006, 118, 2168–2171. [Google Scholar] [CrossRef]
- Yeh, K.-T.; Yang, M.-Y.; Liu, T.-C.; Chen, J.-C.; Chan, W.-L.; Lin, S.-F.; Chang, J.-G. Abnormal Expression of Period 1 (PER1) in Endometrial Carcinoma. J. Pathol. 2005, 206, 111–120. [Google Scholar] [CrossRef]
- Gurin, C.C.; Federici, M.G.; Kang, L.; Boyd, J. Causes and Consequences of Microsatellite Instability in Endometrial Carcinoma. Cancer Res. 1999, 59, 462–466. [Google Scholar]
- Salvesen, H.B.; MacDonald, N.; Ryan, A.; Jacobs, I.J.; Lynch, E.D.; Akslen, L.A.; Das, S. PTEN Methylation Is Associated with Advanced Stage and Microsatellite Instability in Endometrial Carcinoma. Int. J. Cancer 2001, 91, 22–26. [Google Scholar] [CrossRef]
- Shibata, D.; Mori, Y.; Cai, K.; Zhang, L.; Yin, J.; Elahi, A.; Hamelin, R.; Wong, Y.F.; Lo, W.K.; Chung, T.K.H.; et al. RAB32 Hypermethylation and Microsatellite Instability in Gastric and Endometrial Adenocarcinomas. Int. J. Cancer 2006, 119, 801–806. [Google Scholar] [CrossRef]
- Yamaguchi, S.; Asanoma, K.; Takao, T.; Kato, K.; Wake, N. Homeobox Gene HOPX Is Epigenetically Silenced in Human Uterine Endometrial Cancer and Suppresses Estrogen-Stimulated Proliferation of Cancer Cells by Inhibiting Serum Response Factor. Int. J. Cancer 2009, 124, 2577–2588. [Google Scholar] [CrossRef]
- Zighelboim, I.; Goodfellow, P.J.; Schmidt, A.P.; Walls, K.C.; Mallon, M.A.; Mutch, D.G.; Yan, P.S.; Huang, T.H.-M.; Powell, M.A. Differential Methylation Hybridization Array of Endometrial Cancers Reveals Two Novel Cancer-Specific Methylation Markers. Clin. Cancer Res. 2007, 13, 2882–2889. [Google Scholar] [CrossRef] [PubMed]
- Zysman, M.; Saka, A.; Millar, A.; Knight, J.; Chapman, W.; Bapat, B. Methylation of Adenomatous Polyposis Coli in Endometrial Cancer Occurs More Frequently in Tumors with Microsatellite Instability Phenotype. Cancer Res. 2002, 62, 3663–3666. [Google Scholar] [PubMed]
- Risinger, J.I.; Maxwell, G.L.; Chandramouli, G.V.R.; Aprelikova, O.; Litzi, T.; Umar, A.; Berchuck, A.; Barrett, J.C. Gene Expression Profiling of Microsatellite Unstable and Microsatellite Stable Endometrial Cancers Indicates Distinct Pathways of Aberrant Signaling. Cancer Res. 2005, 65, 5031–5037. [Google Scholar] [CrossRef]
- Balch, C.; Matei, D.E.; Huang, T.H.-M.; Nephew, K.P. Role of Epigenomics in Ovarian and Endometrial Cancers. Epigenomics 2010, 2, 419–447. [Google Scholar] [CrossRef]
- Xu, T.; Ding, H.; Chen, J.; Lei, J.; Zhao, M.; Ji, B.; Chen, Y.; Qin, S.; Gao, Q. Research Progress of DNA Methylation in Endometrial Cancer. Biomolecules 2022, 12, 938. [Google Scholar] [CrossRef]
- Powell, M.A.; Mutch, D.G.; Rader, J.S.; Herzog, T.J.; Huang, T.H.-M.; Goodfellow, P.J. Ribosomal DNA Methylation in Patients with Endometrial Carcinoma: An Independent Prognostic Marker. Cancer 2002, 94, 2941–2952. [Google Scholar] [CrossRef]
- Shahid, Z.; Simpson, B.; Miao, K.H.; Singh, G. Genetics, Histone Code. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2025. [Google Scholar]
- Audia, J.E.; Campbell, R.M. Histone Modifications and Cancer. Cold Spring Harb. Perspect. Biol. 2016, 8, a019521. [Google Scholar] [CrossRef]
- McBrian, M.A.; Behbahan, I.S.; Ferrari, R.; Su, T.; Huang, T.-W.; Li, K.; Hong, C.S.; Christofk, H.R.; Vogelauer, M.; Seligson, D.B.; et al. Histone Acetylation Regulates Intracellular pH. Mol. Cell 2013, 49, 310–321. [Google Scholar] [CrossRef]
- Bartosch, C.; Lopes, J.M.; Jerónimo, C. Epigenetics in Endometrial Carcinogenesis—Part 2: Histone Modifications, Chromatin Remodeling and Noncoding RNAs. Epigenomics 2017, 9, 873–892. [Google Scholar] [CrossRef]
- Szwarc, M.M.; Kommagani, R.; Lessey, B.A.; Lydon, J.P. The P160/Steroid Receptor Coactivator Family: Potent Arbiters of Uterine Physiology and Dysfunction. Biol. Reprod. 2014, 91, 122. [Google Scholar] [CrossRef] [PubMed]
- Huang, J.; Qiao, B.; Yuan, Y.; Xie, Y.; Xia, X.; Li, F.; Wang, L. PRMT3 and CARM1: Emerging Epigenetic Targets in Cancer. J. Cell. Mol. Med. 2025, 29, e70386. [Google Scholar] [CrossRef] [PubMed]
- Prabhu, K.S.; Kuttikrishnan, S.; Ahmad, N.; Habeeba, U.; Mariyam, Z.; Suleman, M.; Bhat, A.A.; Uddin, S. H2AX: A Key Player in DNA Damage Response and a Promising Target for Cancer Therapy. Biomed. Pharmacother. 2024, 175, 116663. [Google Scholar] [CrossRef] [PubMed]
- Brunner, A.H.; Hinterholzer, S.; Riss, P.; Heinze, G.; Weiss, K.; Brustmann, H. Expression of γ-H2AX in Endometrial Carcinomas: An Immunohistochemical Study with P53. Gynecol. Oncol. 2011, 121, 206–211. [Google Scholar] [CrossRef]
- Auguste, A.; Genestie, C.; De Bruyn, M.; Adam, J.; Le Formal, A.; Drusch, F.; Pautier, P.; Crosbie, E.J.; MacKay, H.; Kitchener, H.C.; et al. Refinement of High-Risk Endometrial Cancer Classification Using DNA Damage Response Biomarkers: A TransPORTEC Initiative. Mod. Pathol. 2018, 31, 1851–1861. [Google Scholar] [CrossRef]
- Kumar, R.; Li, D.-Q.; Müller, S.; Knapp, S. Epigenomic Regulation of Oncogenesis by Chromatin Remodeling. Oncogene 2016, 35, 4423–4436. [Google Scholar] [CrossRef]
- Gullo, G.; Carlomagno, G.; Unfer, V.; D’Anna, R. Myo-Inositol: From Induction of Ovulation to Menopausal Disorder Management. Minerva Ginecol. 2015, 67, 485–486. [Google Scholar] [PubMed]
- Pasta, V.; Gullo, G.; Giuliani, A.; Harrath, A.H.; Alwasel, S.H.; Tartaglia, F.; Cucina, A.; Bizzarri, M. An Association of Boswellia, Betaine and Myo-Inositol (Eumastós) in the Treatment of Mammographic Breast Density: A Randomized, Double-Blind Study. Eur. Rev. Med. Pharmacol. Sci. 2015, 19, 4419–4426. [Google Scholar]
- Li, M.; Xia, Z.; Wang, R.; Xi, M.; Hou, M. Unveiling DNA Methylation: Early Diagnosis, Risk Assessment, and Therapy for Endometrial Cancer. Front. Oncol. 2024, 14, 1455255. [Google Scholar] [CrossRef]
- Zheng, H.; Yu, C.; Yang, L.; Zhou, F.; Liu, A. Research Progress of DNA Methylation Markers for Endometrial Carcinoma Diagnosis. J. Cancer 2025, 16, 812–820. [Google Scholar] [CrossRef] [PubMed]
- Sonar, S.; Nyahatkar, S.; Kalele, K.; Adhikari, M.D. Role of DNA Methylation in Cancer Development and Its Clinical Applications. Clin. Transl. Discov. 2024, 4, e279. [Google Scholar] [CrossRef]
- Asaturova, A.; Zaretsky, A.; Rogozhina, A.; Tregubova, A.; Badlaeva, A. Advancements in Minimally Invasive Techniques and Biomarkers for the Early Detection of Endometrial Cancer: A Comprehensive Review of Novel Diagnostic Approaches and Clinical Implications. J. Clin. Med. 2024, 13, 7538. [Google Scholar] [CrossRef]
- Ran, R.; Wang, M.; Miao, J.W. The Accuracy of DNA Methylation Detection in Endometrial Cancer Screening: A Systematic Review and Meta-Analysis. Int. J. Gynaecol. Obstet. 2025, 169, 557–566. [Google Scholar] [CrossRef]
- Zglejc-Waszak, K.; Jozwik, M.; Thoene, M.; Wojtkiewicz, J. Role of Receptor for Advanced Glycation End-Products in Endometrial Cancer: A Review. Cancers 2024, 16, 3192. [Google Scholar] [CrossRef]
- Pasanen, A.; Loukovaara, M.; Bützow, R. Clinicopathological Significance of Deficient DNA Mismatch Repair and MLH1 Promoter Methylation in Endometrioid Endometrial Carcinoma. Mod. Pathol. 2020, 33, 1443–1452. [Google Scholar] [CrossRef] [PubMed]
- Post, C.C.B.; Stelloo, E.; Smit, V.T.H.B.M.; Ruano, D.; Tops, C.M.; Vermij, L.; Rutten, T.A.; Jürgenliemk-Schulz, I.M.; Lutgens, L.C.H.W.; Jobsen, J.J.; et al. Prevalence and Prognosis of Lynch Syndrome and Sporadic Mismatch Repair Deficiency in Endometrial Cancer. J. Natl. Cancer Inst. 2021, 113, 1212–1220. [Google Scholar] [CrossRef]
- Borden, L.E.; Locklear, T.M.; Grider, D.J.; Osborne, J.L.; Saks, E.J.; Valea, F.A.; Iglesias, D.A. Endometrial Cancer Characteristics and Risk of Recurrence. Am. J. Clin. Pathol. 2022, 157, 90–97. [Google Scholar] [CrossRef]
- Saito, T.; Nishimura, M.; Yamasaki, H.; Kudo, R. Hypermethylation in Promoter Region of E-Cadherin Gene Is Associated with Tumor Dedifferention and Myometrial Invasion in Endometrial Carcinoma. Cancer 2003, 97, 1002–1009. [Google Scholar] [CrossRef]
- Dong, R.; Pu, H.; Wang, Y.; Yu, J.; Lian, K.; Mao, C. TESTIN Was Commonly Hypermethylated and Involved in the Epithelial-Mesenchymal Transition of Endometrial Cancer. APMIS 2015, 123, 394–400. [Google Scholar] [CrossRef]
- Ying, J.; Xu, T.; Wang, Q.; Ye, J.; Lyu, J. Exploration of DNA Methylation Markers for Diagnosis and Prognosis of Patients with Endometrial Cancer. Epigenetics 2018, 13, 490–504. [Google Scholar] [CrossRef]
- Huo, X.; Sun, H.; Cao, D.; Yang, J.; Peng, P.; Yu, M.; Shen, K. Identification of Prognosis Markers for Endometrial Cancer by Integrated Analysis of DNA Methylation and RNA-Seq Data. Sci. Rep. 2019, 9, 9924. [Google Scholar] [CrossRef] [PubMed]
- Cui, Z.-J.; Zhou, X.-H.; Zhang, H.-Y. DNA Methylation Module Network-Based Prognosis and Molecular Typing of Cancer. Genes 2019, 10, 571. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Yin, F.; Fan, Y.; Cheng, Y.; Dong, Y.; Zhou, J.; Wang, Z.; Li, X.; Wang, J. Establishment and Validation of a Prognostic Nomogram Based on a Novel Five-DNA Methylation Signature for Survival in Endometrial Cancer Patients. Cancer Med. 2021, 10, 693–708. [Google Scholar] [CrossRef]
- Shang, C.; Li, Y.; Wu, Z.; Han, Q.; Zhu, Y.; He, T.; Guo, H. The Prognostic Value of DNA Methylation, Post-Translational Modifications and Correlated with Immune Infiltrates in Gynecologic Cancers. Pharmgenomics Pers. Med. 2021, 14, 39–53. [Google Scholar] [CrossRef]
- Liu, J.; Ji, C.; Wang, Y.; Zhang, C.; Zhu, H. Identification of Methylation-Driven Genes Prognosis Signature and Immune Microenvironment in Uterus Corpus Endometrial Cancer. Cancer Cell Int. 2021, 21, 365. [Google Scholar] [CrossRef] [PubMed]
- Cao, L.; Ma, X.; Rong, P.; Zhang, J.; Yang, M.; Wang, W. Comprehensive Analysis of DNA Methylation and Transcriptome to Identify PD-1-Negative Prognostic Methylated Signature in Endometrial Carcinoma. Dis. Markers 2022, 2022, 3085289. [Google Scholar] [CrossRef]
- Meijuan, C.; Meng, X.; Fang, L.; Qian, W. Synaptotagmin-like Protein 1 Is a Potential Diagnostic and Prognostic Biomarker in Endometrial Cancer Based on Bioinformatics and Experiments. J. Ovarian Res. 2023, 16, 16. [Google Scholar] [CrossRef] [PubMed]
- Janzen, D.M.; Rosales, M.A.; Paik, D.Y.; Lee, D.S.; Smith, D.A.; Witte, O.N.; Iruela-Arispe, M.L.; Memarzadeh, S. Progesterone Receptor Signaling in the Microenvironment of Endometrial Cancer Influences Its Response to Hormonal Therapy. Cancer Res. 2013, 73, 4697–4710. [Google Scholar] [CrossRef] [PubMed]
- Pu, H.; Wen, X.; Luo, D.; Guo, Z. Regulation of Progesterone Receptor Expression in Endometriosis, Endometrial Cancer, and Breast Cancer by Estrogen, Polymorphisms, Transcription Factors, Epigenetic Alterations, and Ubiquitin-Proteasome System. J. Steroid Biochem. Mol. Biol. 2023, 227, 106199. [Google Scholar] [CrossRef]
- Bartosch, C.; Monteiro-Reis, S.; Vieira, R.; Pereira, A.; Rodrigues, M.; Jerónimo, C.; Lopes, J.M. Endometrial Endometrioid Carcinoma Metastases Show Decreased ER-Alpha and PR-A Expression Compared to Matched Primary Tumors. PLoS ONE 2015, 10, e0134969. [Google Scholar] [CrossRef]
- Sasaki, M.; Dharia, A.; Oh, B.R.; Tanaka, Y.; Fujimoto, S.; Dahiya, R. Progesterone Receptor B Gene Inactivation and CpG Hypermethylation in Human Uterine Endometrial Cancer. Cancer Res. 2001, 61, 97–102. [Google Scholar]
- Sasaki, M.; Kaneuchi, M.; Fujimoto, S.; Tanaka, Y.; Dahiya, R. Hypermethylation Can Selectively Silence Multiple Promoters of Steroid Receptors in Cancers. Mol. Cell. Endocrinol. 2003, 202, 201–207. [Google Scholar] [CrossRef]
- Jones, A.; Teschendorff, A.E.; Li, Q.; Hayward, J.D.; Kannan, A.; Mould, T.; West, J.; Zikan, M.; Cibula, D.; Fiegl, H.; et al. Role of DNA Methylation and Epigenetic Silencing of HAND2 in Endometrial Cancer Development. PLoS Med. 2013, 10, e1001551. [Google Scholar] [CrossRef]
- Yanokura, M.; Banno, K.; Kawaguchi, M.; Hirao, N.; Hirasawa, A.; Susumu, N.; Tsukazaki, K.; Aoki, D. Relationship of Aberrant DNA Hypermethylation of CHFR with Sensitivity to Taxanes in Endometrial Cancer. Oncol. Rep. 2007, 17, 41–48. [Google Scholar] [CrossRef]
- Wang, X.; Yang, Y.; Xu, C.; Xiao, L.; Shen, H.; Zhang, X.; Li, T.; Li, X. CHFR Suppression by Hypermethylation Sensitizes Endometrial Cancer Cells to Paclitaxel. Int. J. Gynecol. Cancer 2011, 21, 996–1003. [Google Scholar] [CrossRef] [PubMed]
- Zhou, J.-W.; Tang, J.-J.; Sun, W.; Wang, H. PGK1 Facilities Cisplatin Chemoresistance by Triggering HSP90/ERK Pathway Mediated DNA Repair and Methylation in Endometrial Endometrioid Adenocarcinoma. Mol. Med. 2019, 25, 11. [Google Scholar] [CrossRef]
- Fialkova, V.; Vidomanova, E.; Balharek, T.; Marcinek, J.; Kudela, E.; Hanysova, S.; Visnovsky, J.; Dobrota, D.; Hatok, J. DNA Methylation as Mechanism of Apoptotic Resistance Development in Endometrial Cancer Patients. Gen. Physiol. Biophys. 2017, 36, 521–529. [Google Scholar] [CrossRef]
- Huang, Y.; Tang, M.; Hu, Z.; Cai, B.; Chen, G.; Jiang, L.; Xia, Y.; Guan, P.; Li, X.; Mao, Z.; et al. SMYD3 Promotes Endometrial Cancer through Epigenetic Regulation of LIG4/XRCC4/XLF Complex in Non-Homologous End Joining Repair. Oncogenesis 2024, 13, 3. [Google Scholar] [CrossRef] [PubMed]
- Jamaluddin, M.F.B.; Ko, Y.-A.; Ghosh, A.; Syed, S.M.; Ius, Y.; O’Sullivan, R.; Netherton, J.K.; Baker, M.A.; Nahar, P.; Jaaback, K.; et al. Proteomic and Functional Characterization of Intra-Tumor Heterogeneity in Human Endometrial Cancer. Cell Rep. Med. 2022, 3, 100738. [Google Scholar] [CrossRef] [PubMed]
- Boldu-Fernández, S.; Lliberos, C.; Simon, C.; Mas, A. Mapping Human Uterine Disorders Through Single-Cell Transcriptomics. Cells 2025, 14, 156. [Google Scholar] [CrossRef]
- Richards, R.; Patel, J.; Stevenson, K.; Harbison, S. Evaluation of Massively Parallel Sequencing for Forensic DNA Methylation Profiling. Electrophoresis 2018, 39, 2798–2805. [Google Scholar] [CrossRef]
- Montanari Vergallo, G.; Zaami, S. Guidelines and Best Practices: Remarks on the Gelli-Bianco Law. Clin. Ter. 2018, 169, e82–e85. [Google Scholar] [CrossRef]
- Gazzetta Ufficiale. Available online: https://www.gazzettaufficiale.it/eli/id/2017/03/17/17G00041/s (accessed on 11 June 2025).
- Cucinella, G.; Gullo, G.; Catania, E.; Perino, A.; Billone, V.; Marinelli, S.; Napoletano, G.; Zaami, S. Stem Cells and Infertility: A Review of Clinical Applications and Legal Frameworks. J. Pers. Med. 2024, 14, 135. [Google Scholar] [CrossRef]
- Martines, V.; Magnaldi, S.; Fazio, N.D.; Volonnino, G.; Marinelli, E.; Paola, L.D. Enhancing Patient Safety and Delineate Professional Responsibility in Radiological Procedures Involving Contrast Medium Administration. Clin. Ter. 2025, 176, 42–46. [Google Scholar] [CrossRef]
- Zaami, S.; Melcarne, R.; Patrone, R.; Gullo, G.; Negro, F.; Napoletano, G.; Monti, M.; Aceti, V.; Panarese, A.; Borcea, M.C.; et al. Oncofertility and Reproductive Counseling in Patients with Breast Cancer: A Retrospective Study. J. Clin. Med. 2022, 11, 1311. [Google Scholar] [CrossRef]
- Brasil, S.; Neves, C.J.; Rijoff, T.; Falcão, M.; Valadão, G.; Videira, P.A.; Dos Reis Ferreira, V. Artificial Intelligence in Epigenetic Studies: Shedding Light on Rare Diseases. Front. Mol. Biosci. 2021, 8, 648012. [Google Scholar] [CrossRef]
- Marinelli, S.; De Paola, L.; Stark, M.; Montanari Vergallo, G. Artificial Intelligence in the Service of Medicine: Current Solutions and Future Perspectives, Opportunities, and Challenges. Clin. Ter. 2025, 176, 77–82. [Google Scholar] [CrossRef]
- Tahir, M.; Norouzi, M.; Khan, S.S.; Davie, J.R.; Yamanaka, S.; Ashraf, A. Artificial Intelligence and Deep Learning Algorithms for Epigenetic Sequence Analysis: A Review for Epigeneticists and AI Experts. Comput. Biol. Med. 2024, 183, 109302. [Google Scholar] [CrossRef]
- Pammi, M.; Aghaeepour, N.; Neu, J. Multiomics, Artificial Intelligence, and Precision Medicine in Perinatology. Pediatr. Res. 2023, 93, 308–315. [Google Scholar] [CrossRef] [PubMed]
- Ribatti, D. Epigenetics and Its Ethical Implications. Crit. Rev. Eukaryot. Gene Expr. 2021, 31, 23–27. [Google Scholar] [CrossRef] [PubMed]
- Grunau, C.; Le Luyer, J.; Laporte, M.; Joly, D. The Epigenetics Dilemma. Genes 2019, 11, 23. [Google Scholar] [CrossRef]
- Dupras, C.; Knoppers, T.; Palmour, N.; Beauchamp, E.; Liosi, S.; Siebert, R.; Berner, A.M.; Beck, S.; Charest, I.; Joly, Y. Researcher Perspectives on Ethics Considerations in Epigenetics: An International Survey. Clin. Epigenetics 2022, 14, 110. [Google Scholar] [CrossRef]
- Park, H.L. Epigenetic Biomarkers for Environmental Exposures and Personalized Breast Cancer Prevention. Int. J. Environ. Res. Public Health 2020, 17, 1181. [Google Scholar] [CrossRef]
- Cerdeña, J.P. Epigenetic Citizenship and Political Claims-Making: The Ethics of Molecularizing Structural Racism. Biosocieties 2022, 18, 632–655. [Google Scholar] [CrossRef] [PubMed]
- Sasaki-Honda, M.; Akatsuka, K.; Sawai, T. Is Epigenome Editing Non-Inheritable? Implications for Ethics and the Regulation of Human Applications. Stem Cell Rep. 2023, 18, 2005–2009. [Google Scholar] [CrossRef]
- Ethics and Governance of Artificial Intelligence for Health. Available online: https://www.who.int/publications-detail-redirect/9789240029200 (accessed on 19 March 2024).
- Santaló, J.; Berdasco, M. Ethical Implications of Epigenetics in the Era of Personalized Medicine. Clin. Epigenetics 2022, 14, 44. [Google Scholar] [CrossRef]
- Gulìa, C.; Signore, F.; Gaffi, M.; Gigli, S.; Votino, R.; Nucciotti, R.; Bertacca, L.; Zaami, S.; Baffa, A.; Santini, E.; et al. Y RNA: An Overview of Their Role as Potential Biomarkers and Molecular Targets in Human Cancers. Cancers 2020, 12, 1238. [Google Scholar] [CrossRef]
- Del Savio, L.; Loi, M.; Stupka, E. Epigenetics and Future Generations. Bioethics 2015, 29, 580–587. [Google Scholar] [CrossRef]
- Gupta, M.K.; Peng, H.; Li, Y.; Xu, C.-J. The Role of DNA Methylation in Personalized Medicine for Immune-Related Diseases. Pharmacol. Ther. 2023, 250, 108508. [Google Scholar] [CrossRef]
- Chiapperino, L. Epigenetics: Ethics, Politics, Biosociality. Br. Med. Bull. 2018, 128, 49–60. [Google Scholar] [CrossRef]
- Northrup, G.M. Tarasoff: Duty to Protect (Not Warn)-Response to a Tale of Two States. Psychiatry 2005, 2, 53. [Google Scholar]
- Dupras, C.; Saulnier, K.M.; Joly, Y. Epigenetics, Ethics, Law and Society: A Multidisciplinary Review of Descriptive, Instrumental, Dialectical and Reflexive Analyses. Soc. Stud. Sci. 2019, 49, 785–810. [Google Scholar] [CrossRef] [PubMed]
- Retis-Resendiz, A.M.; González-García, I.N.; León-Juárez, M.; Camacho-Arroyo, I.; Cerbón, M.; Vázquez-Martínez, E.R. The Role of Epigenetic Mechanisms in the Regulation of Gene Expression in the Cyclical Endometrium. Clin. Epigenetics 2021, 13, 116. [Google Scholar] [CrossRef] [PubMed]
- Piergentili, R.; Sechi, S.; De Paola, L.; Zaami, S.; Marinelli, E. Building a Hand-Curated ceRNET for Endometrial Cancer, Striving for Clinical as Well as Medicolegal Soundness: A Systematic Review. Noncoding RNA 2025, 11, 34. [Google Scholar] [CrossRef] [PubMed]


| Gene Name | Pathway |
|---|---|
| AJUBA | chromatin other |
| ARID1A* | chromatin SWI/SNF complex |
| ARID2 | chromatin SWI/SNF complex |
| ARID5B* | chromatin histone modifiers |
| ASXL1 | chromatin other |
| ASXL2 | chromatin other |
| ATF7IP* | chromatin other |
| ATRX | chromatin SWI/SNF complex |
| BCOR* | chromatin other |
| BRD7 | chromatin SWI/SNF complex |
| CHD3 | chromatin other |
| CHD4* | chromatin other |
| CHD8* | chromatin other |
| CREBBP | chromatin histone modifiers |
| CTCF* | chromatin other |
| DNMT3A | epigenetic DNA modifiers |
| EP300* | chromatin histone modifiers |
| H3F3A | chromatin other |
| H3F3C | chromatin other |
| HIST1H1E | chromatin other |
| KANSL1* | chromatin histone modifiers |
| KDM5C | chromatin histone modifiers |
| KDM6A | histone modification |
| KMT2A | chromatin histone modifiers |
| KMT2B* | chromatin histone modifiers |
| KMT2C* | chromatin histone modifiers |
| KMT2D | chromatin histone modifiers |
| MEN1 | chromatin histone modifiers |
| NCOR1 | chromatin histone modifiers |
| NIPBL | chromatin other |
| NPM1 | chromatin other |
| NSD1 | chromatin histone modifiers |
| PBRM1* | chromatin SWI/SNF complex |
| PPP6C | histone modification |
| SETD2 | histone modification |
| SIN3A* | chromatin histone modifiers |
| SMARCA1 | chromatin SWI/SNF complex |
| SMARCA4 | chromatin SWI/SNF complex |
| SMARCB1 | chromatin SWI/SNF complex |
| WHSC1 | chromatin histone modifiers |
| ZMYM3 | chromatin histone modifiers |
| Type | Action | Examples * |
|---|---|---|
| Writers | Addition of chemical groups to DNA or histones | DNMT, HAT, KMT, PRMT |
| Readers | Modification recognition and modifiers recruiting | Chromo/bromo-domains |
| Erasers | Removal of chemical groups from DNA or histones | HDAC, KDM |
| Gene | Function | Clinical Relevance in EC |
|---|---|---|
| ARID1A | Component of SWI/SNF complex; chromatin remodeling | Frequently mutated; associated with poor prognosis |
| SMARCA4 | ATPase subunit of SWI/SNF complex | Loss linked to dedifferentiated tumors |
| CHD4 | Part of NuRD complex; transcriptional repression | Mutations associated with microsatellite instability |
| EZH2 | Histone methyltransferase; H3K27me3 writer | Overexpression linked to aggressive tumor behavior |
| KMT2D | Histone methyltransferase; H3K4 methylation | Mutations observed in endometrioid subtypes |
| Assay Type | Description | Use | Limitations |
|---|---|---|---|
| ChIP-seq | Chromatin immunoprecipitation followed by sequencing | Identifies DNA regions bound by specific proteins | Requires high-quality antibodies; low resolution; poor reproducibility; not suitable for FFPE samples |
| ATAC-seq | Assay for transposase-accessible chromatin using sequencing | Measures chromatin accessibility | Sensitive to sample quality; limited in FFPE; limited resolution in complex tissues |
| DNase-seq | DNase I hypersensitive site sequencing | Maps DNase I hypersensitive sites | Requires large input material; complex protocol; fresh tissue; low throughput |
| MNase-seq | Micrococcal nuclease digestion followed by sequencing | Profiles nucleosome positioning | Bias toward accessible regions; digestion variability; complex data interpretation |
| Hi-C | Measures the frequency at which two DNA fragments physically associate in 3D space through crosslinking | Captures 3D chromatin interactions | High cost; complex data interpretation |
| CUT&RUN | Antibody-targeted controlled cleavage by micrococcal nuclease followed by massive parallel DNA sequencing | Analyzes DNA/protein interactions | Emerging method; limited clinical validation |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Piergentili, R.; Marinelli, E.; De Paola, L.; Cucinella, G.; Billone, V.; Zaami, S.; Gullo, G. Epigenetics of Endometrial Cancer: The Role of Chromatin Modifications and Medicolegal Implications. Int. J. Mol. Sci. 2025, 26, 7306. https://doi.org/10.3390/ijms26157306
Piergentili R, Marinelli E, De Paola L, Cucinella G, Billone V, Zaami S, Gullo G. Epigenetics of Endometrial Cancer: The Role of Chromatin Modifications and Medicolegal Implications. International Journal of Molecular Sciences. 2025; 26(15):7306. https://doi.org/10.3390/ijms26157306
Chicago/Turabian StylePiergentili, Roberto, Enrico Marinelli, Lina De Paola, Gaspare Cucinella, Valentina Billone, Simona Zaami, and Giuseppe Gullo. 2025. "Epigenetics of Endometrial Cancer: The Role of Chromatin Modifications and Medicolegal Implications" International Journal of Molecular Sciences 26, no. 15: 7306. https://doi.org/10.3390/ijms26157306
APA StylePiergentili, R., Marinelli, E., De Paola, L., Cucinella, G., Billone, V., Zaami, S., & Gullo, G. (2025). Epigenetics of Endometrial Cancer: The Role of Chromatin Modifications and Medicolegal Implications. International Journal of Molecular Sciences, 26(15), 7306. https://doi.org/10.3390/ijms26157306











