The Role of Protein Kinases in the Suppressive Phenotype of Myeloid-Derived Suppressor Cells
Abstract
1. Introduction
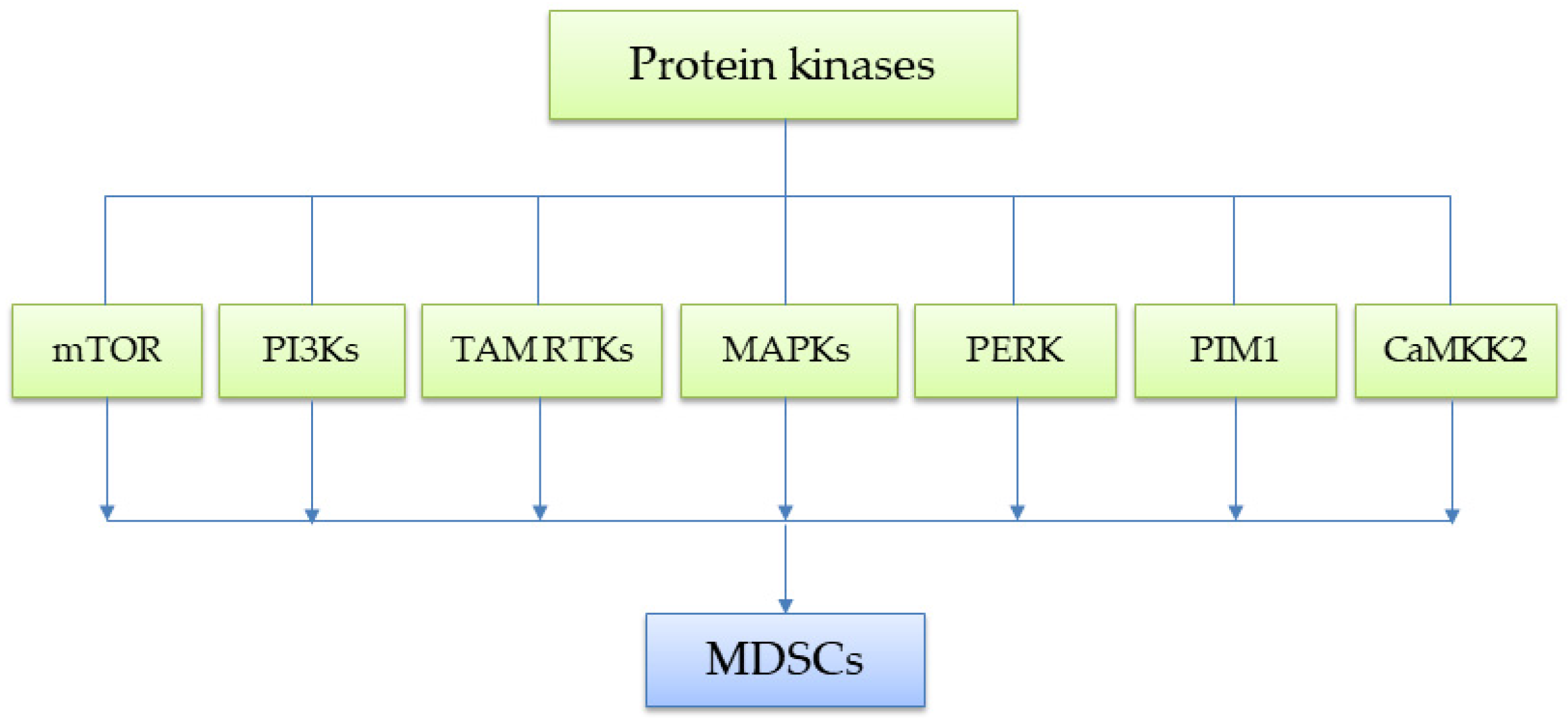
2. Protein Kinases in MDSCs
2.1. mTOR
2.2. PI3Ks
2.3. TAM Receptor Tyrosine Kinase
2.4. MAPKs
3. Other Serine/Threonine Kinases
3.1. PERK
3.2. PIM1
3.3. CaMKK2
4. Conclusions and Prospects
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| AKI | Acute kidney injury |
| AMPK | AMP-activated protein kinase |
| BTK | Bruton’s tyrosine kinase |
| C/EBPβ | CCAAT/enhancer binding protein beta |
| CaMKK2 | Calcium/calmodulin-dependent protein kinase kinase 2 |
| CIH | Con A-induced immune-mediated hepatic injuries |
| DCs | Dendritic cells |
| DSKs | Dual-specificity kinases |
| ER | Endoplasmic reticulum |
| ERKs | Extracellular signal-regulated kinases |
| GAS6 | Growth Arrest-Specific 6 |
| GM-CSF | Granulocyte–macrophage colony-stimulating factor |
| HNSCC | head and neck squamous cell carcinoma |
| HSPCs | hematopoietic stem and progenitor cells |
| ICB | Immune checkpoint blockade |
| IDO | Indoleamine 2,3-dioxygenase |
| IF1 | Inhibitory Factor 1 |
| IFN-α | Interferon-alpha |
| IFNAR1 | Interferon alpha and beta receptor subunit 1 |
| IL-6 | Interleukin-6 |
| iNOS IRF-8 | Inducible nitric oxide synthase Interferon regulatory factor-8 |
| JNK | c-Jun N-terminal kinases |
| MAPKs | Mitogen-activated protein kinases |
| M-CSF | Macrophage colony-stimulating factor |
| mTOR | Mechanistic target of rapamycin |
| NETs | Neutrophil extracellular traps |
| NF-κB | Nuclear factor kappa B |
| 2NBDG | 2-(N-(7-Nitrobenz-2-oxa-1,3-diazol-4-yl)Amino)-2-Deoxyglucose |
| NK | Natural killer |
| NRTKs | Non-receptor tyrosine kinases |
| PERK | PKR-like endoplasmic reticulum (ER) kinase |
| PI3Ks | Phosphoinositide 3-kinases |
| PIH | Picryl chloride |
| PIM1 | Proviral integration site for Moloney murine leukemia virus-1 |
| PIP3 | Phosphatidylinositol-3, 4, 5-triphosphate |
| PKB | Protein Kinase B |
| PROS1 | Protein S |
| PPAR-γ | Peroxisome Proliferator-Activated Receptor gamma |
| PtdSer | Phosphatidylserine |
| ROS | Reactive oxygen species |
| RTKs | Receptor tyrosine kinases |
| STAT3 | Signal transducer and activator of transcription 3 |
| STKs | Serine/threonine kinases |
| TAM RTK | TAM (Tyro3, Axl, Mer) family of receptor tyrosine kinases |
| TAMs | Tumor-associated macrophages |
| TEK | Tyrosine kinase expressed in hepatocellular carcinoma |
| TGF-β | Transforming growth factor-beta |
| TLR7 | Toll-like receptor 7 |
| TKs | Tyrosine kinases |
| TME | Tumor microenvironment |
| UPR | Unfolded protein response |
| VEGF | Vascular endothelial growth factor |
References
- Wang, Y.; Schafer, C.C.; Hough, K.P.; Tousif, S.; Duncan, S.R.; Kearney, J.F.; Ponnazhagan, S.; Hsu, H.-C.; Deshane, J.S. Myeloid-Derived Suppressor Cells Impair B Cell Responses in Lung Cancer through IL-7 and STAT5. J. Immunol. 2018, 201, 278–295. [Google Scholar] [CrossRef] [PubMed]
- Jaufmann, J.; Lelis, F.J.N.; Teschner, A.C.; Fromm, K.; Rieber, N.; Hartl, D.; Beer-Hammer, S. Human Monocytic Myeloid-Derived Suppressor Cells Impair B-Cell Phenotype and Function in Vitro. Eur. J. Immunol. 2019, 50, 33–47. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Li, C.; Liu, T.; Dai, X.; Bazhin, A.V. Myeloid-Derived Suppressor Cells in Tumors: From Mechanisms to Antigen Specificity and Microenvironmental Regulation. Front. Immunol. 2020, 11, 1371. [Google Scholar] [CrossRef] [PubMed]
- Jayakumar, A.; Bothwell, A.L.M. Functional Diversity of Myeloid-Derived Suppressor Cells: The Multitasking Hydra of Cancer. J. Immunol. 2019, 203, 1095–1103. [Google Scholar] [CrossRef] [PubMed]
- Özkan, B.; Lim, H.; Park, S.G. Immunomodulatory Function of Myeloid-Derived Suppressor Cells during B Cell-Mediated Immune Responses. Int. J. Mol. Sci. 2018, 19, 1468. [Google Scholar] [CrossRef] [PubMed]
- Sinha, P.; Clements, V.K.; Bunt, S.K.; Albelda, S.M.; Ostrand-Rosenberg, S. Cross-Talk between Myeloid-Derived Suppressor Cells and Macrophages Subverts Tumor Immunity toward a Type 2 Response. J. Immunol. 2007, 179, 977–983. [Google Scholar] [CrossRef] [PubMed]
- Zhao, T.; Du, H.; Ding, X.; Walls, K.; Yan, C. Activation of MTOR Pathway in Myeloid-Derived Suppressor Cells Stimulates Cancer Cell Proliferation and Metastasis in Lal-/- Mice. Oncogene 2014, 34, 1938–1948. [Google Scholar] [CrossRef] [PubMed]
- Kumar, S.; Wilkes, D.W.; Samuel, N.; Blanco, M.A.; Nayak, A.; Alicea-Torres, K.; Gluck, C.; Sinha, S.; Gabrilovich, D.; Chakrabarti, R. Δnp63-Driven Recruitment of Myeloid-Derived Suppressor Cells Promotes Metastasis in Triple-Negative Breast Cancer. J. Clin. Investig. 2018, 128, 5095–5109. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Ding, Y.; Guo, N.; Wang, S. MDSCs: Key Criminals of Tumor Pre-Metastatic Niche Formation. Front. Immunol. 2019, 10, 172. [Google Scholar] [CrossRef] [PubMed]
- Rashid, M.H.; Borin, T.F.; Ara, R.; Piranlioglu, R.; Achyut, B.R.; Korkaya, H.; Liu, Y.; Arbab, A.S. Critical Immunosuppressive Effect of MDSC-Derived Exosomes in the Tumor Microenvironment. Oncol. Rep. 2021, 45, 1171–1181. [Google Scholar] [CrossRef] [PubMed]
- Tang, R.; Luo, S.; Liu, H.; Sun, Y.; Liu, M.; Li, L.; Ren, H.; Angele, M.K.; Börner, N.; Yu, K.; et al. Circulating Tumor Microenvironment in Metastasis. Cancer Res. 2025, 85, 1354–1367. [Google Scholar] [CrossRef] [PubMed]
- Bronte, V.; Brandau, S.; Chen, S.H.; Colombo, M.P.; Frey, A.B.; Greten, T.F.; Mandruzzato, S.; Murray, P.J.; Ochoa, A.; Ostrand-Rosenberg, S.; et al. Recommendations for Myeloid-Derived Suppressor Cell Nomenclature and Characterization Standards. Nat. Commun. 2016, 7, 12150. [Google Scholar] [CrossRef] [PubMed]
- Lasser, S.A.; Ozbay Kurt, F.G.; Arkhypov, I.; Utikal, J.; Umansky, V. Myeloid-Derived Suppressor Cells in Cancer and Cancer Therapy. Nat. Rev. Clin. Oncol. 2024, 21, 147–164. [Google Scholar] [CrossRef] [PubMed]
- Hegde, S.; Leader, A.M.; Merad, M. MDSC: Markers, Development, States, and Unaddressed Complexity. Immunity 2021, 54, 875–884. [Google Scholar] [CrossRef] [PubMed]
- Musolino, C.; Allegra, A.; Pioggia, G.; Gangemi, S. Immature Myeloid-Derived Suppressor Cells: A Bridge between Inflammation and Cancer (Review). Oncol. Rep. 2016, 37, 671–683. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Y.; Cao, S. Unraveling the Complexities of Myeloid-Derived Suppressor Cells in Inflammatory Bowel Disease. Int. J. Mol. Sci. 2025, 26, 3291. [Google Scholar] [CrossRef] [PubMed]
- Millrud, C.R.; Bergenfelz, C.; Leandersson, K. On the Origin of Myeloid-Derived Suppressor Cells. Oncotarget 2016, 8, 3649. [Google Scholar] [CrossRef] [PubMed]
- Wu, X.; Zhu, D.; Tian, J.; Tang, X.; Guo, H.; Ma, J.; Xu, H.; Wang, S. Granulocytic Myeloid-Derived Suppressor Cell Exosomal Prostaglandin E2 Ameliorates Collagen-Induced Arthritis by Enhancing IL-10+ B Cells. Front. Immunol. 2020, 11, 588500. [Google Scholar] [CrossRef] [PubMed]
- Barnie, P.A.; Zhang, P.; Lv, H.; Wang, D.; Su, X.; Su, Z.; Xu, H. Myeloid-Derived Suppressor Cells and Myeloid Regulatory Cells in Cancer and Autoimmune Disorders (Review). Exp. Ther. Med. 2017, 13, 378–388. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Lee, J.Y.; Sohn, H.J.; Kim, C.H.; Kim, T.G.; Lee, H.S. Local and Systemic Injections of Human Cord Blood Myeloid-Derived Suppressor Cells to Prevent Graft Rejection in Corneal Transplantation. Biomedicines 2022, 10, 3223. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.; Wu, T.; Zhao, Y. The Roles of Myeloid-Derived Suppressor Cells in Transplantation. Expert Rev. Clin. Immunol. 2014, 10, 1385–1394. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.; Li, J.; Qi, G.; Tu, G.; Yang, C.; Xu, M. Myeloid-Derived Suppressor Cells in Transplantation: The Dawn of Cell Therapy. J. Transl. Med. 2018, 16, 19. [Google Scholar] [CrossRef] [PubMed]
- Saiwai, H.; Kumamaru, H.; Ohkawa, Y.; Kubota, K.; Kobayakawa, K.; Yamada, H.; Yokomizo, T.; Iwamoto, Y.; Okada, S. Ly6C+Ly6G- Myeloid-Derived Suppressor Cells Play a Critical Role in the Resolution of Acute Inflammation and the Subsequent Tissue Repair Process after Spinal Cord Injury. J. Neurochem. 2013, 125, 74–88. [Google Scholar] [CrossRef] [PubMed]
- Grover, A.; Sanseviero, E.; Timosenko, E.; Gabrilovich, D.I. Myeloid-Derived Suppressor Cells: A Propitious Road to Clinic. Cancer Discov. 2021, 11, 2693–2706. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.; Yi, M.; Niu, M.; Mei, Q.; Wu, K. Myeloid-Derived Suppressor Cells: An Emerging Target for Anticancer Immunotherapy. Mol. Cancer 2022, 21, 184. [Google Scholar] [CrossRef] [PubMed]
- Zhang, C.; Sui, Y.; Liu, S.; Yang, M. The Roles of Myeloid-Derived Suppressor Cells in Liver. Dis. Biomed. 2024, 12, 299. [Google Scholar] [CrossRef] [PubMed]
- Manning, G.; Whyte, D.B.; Martinez, R.; Hunter, T.; Sudarsanam, S. The Protein Kinase Complement of the Human. Genome Sci. 2002, 298, 1912–1934. [Google Scholar] [CrossRef] [PubMed]
- Ardito, F.; Giuliani, M.; Perrone, D.; Troiano, G.; Muzio, L. Lo The Crucial Role of Protein Phosphorylation in Cell Signalingand Its Use as Targeted Therapy (Review). Int. J. Mol. Med. 2017, 40, 271–280. [Google Scholar] [CrossRef] [PubMed]
- Good, L.; Benner, B.; Carson, W.E. Bruton’s Tyrosine Kinase: An Emerging Targeted Therapy in Myeloid Cells within the Tumor Microenvironment. Cancer Immunol. Immunother. 2021, 70, 2439–2451. [Google Scholar] [CrossRef] [PubMed]
- Saxton, R.A.; Sabatini, D.M. MTOR Signaling in Growth, Metabolism, and Disease. Cell 2017, 168, 960–976. [Google Scholar] [CrossRef] [PubMed]
- Weichhart, T.; Hengstschläger, M.; Linke, M. Regulation of Innate Immune Cell Function by MTOR. Nat. Rev. Immunol. 2015, 15, 599–614. [Google Scholar] [CrossRef] [PubMed]
- Karmaus, P.W.F.; Herrada, A.A.; Guy, C.; Neale, G.; Dhungana, Y.; Long, L.; Vogel, P.; Avila, J.; Clish, C.B.; Chi, H. Critical Roles of MTORC1 Signaling and Metabolic Reprogramming for M-CSF-Mediated Myelopoiesis. J. Exp. Med. 2017, 214, 2629–2647. [Google Scholar] [CrossRef] [PubMed]
- Wu, T.; Zhao, Y.; Wang, H.; Li, Y.; Shao, L.; Wang, R.; Lu, J.; Yang, Z.; Wang, J.; Zhao, Y. MTOR Masters Monocytic Myeloid-Derived Suppressor Cells in Mice with Allografts or Tumors. Sci. Rep. 2016, 6, 35230. [Google Scholar] [CrossRef] [PubMed]
- Deng, Y.; Yang, J.; Luo, F.; Qian, J.; Liu, R.; Zhang, D.; Yu, H.; Chu, Y. MTOR-Mediated Glycolysis Contributes to the Enhanced Suppressive Function of Murine Tumor-Infiltrating Monocytic Myeloid-Derived Suppressor Cells. Cancer Immunol. Immunother. 2018, 67, 1355–1364. [Google Scholar] [CrossRef] [PubMed]
- Dos, D.S.; Ali, S.M.; Kim, D.H.; Guertin, D.A.; Latek, R.R.; Erdjument-Bromage, H.; Tempst, P.; Sabatini, D.M. Rictor, a Novel Binding Partner of MTOR, Defines a Rapamycin-Insensitive and Raptor-Independent Pathway That Regulates the Cytoskeleton. Curr. Biol. 2004, 14, 1296–1302. [Google Scholar] [CrossRef]
- Shi, G.; Li, D.; Zhang, D.; Xu, Y.; Pan, Y.; Lu, L.; Li, J.; Xia, X.; Dou, H.; Hou, Y. IRF-8/MiR-451a Regulates M-MDSC Differentiation via the AMPK/MTOR Signal Pathway during Lupus Development. Cell Death Discov. 2021, 7, 179. [Google Scholar] [CrossRef] [PubMed]
- Marigo, I.; Bosio, E.; Solito, S.; Mesa, C.; Fernandez, A.; Dolcetti, L.; Ugel, S.; Sonda, N.; Bicciato, S.; Falisi, E.; et al. Tumor-Induced Tolerance and Immune Suppression Depend on the C/EBPβ Transcription Factor. Immunity 2010, 32, 790–802. [Google Scholar] [CrossRef] [PubMed]
- Paschall, A.V.; Zhang, R.; Qi, C.-F.; Bardhan, K.; Peng, L.; Lu, G.; Yang, J.; Merad, M.; McGaha, T.; Zhou, G.; et al. IFN Regulatory Factor 8 Represses GM-CSF Expression in T Cells To Affect Myeloid Cell Lineage Differentiation. J. Immunol. 2015, 194, 2369–2379. [Google Scholar] [CrossRef] [PubMed]
- Waight, J.D.; Netherby, C.; Hensen, M.L.; Miller, A.; Hu, Q.; Liu, S.; Bogner, P.N.; Farren, M.R.; Lee, K.P.; Liu, K.; et al. Myeloid-Derived Suppressor Cell Development Is Regulated by a STAT/IRF-8 Axis. J. Clin. Investig. 2013, 123, 4464–4478. [Google Scholar] [CrossRef] [PubMed]
- Moorman, H.R.; Reategui, Y.; Poschel, D.B.; Liu, K. IRF8: Mechanism of Action and Health Implications. Cells 2022, 11, 2630. [Google Scholar] [CrossRef] [PubMed]
- Cui, Y.; Chen, J.; Zhang, Z.; Shi, H.; Sun, W.; Yi, Q. The Role of AMPK in Macrophage Metabolism, Function and Polarisation. J. Transl. Med. 2023, 21, 892. [Google Scholar] [CrossRef] [PubMed]
- Salminen, A.; Kauppinen, A.; Kaarniranta, K. AMPK Activation Inhibits the Functions of Myeloid-Derived Suppressor Cells (MDSC): Impact on Cancer and Aging. J. Mol. Med. 2019, 97, 1049–1064. [Google Scholar] [CrossRef] [PubMed]
- Qin, G.; Lian, J.; Huang, L.; Zhao, Q.; Liu, S.; Zhang, Z.; Chen, X.; Yue, D.; Li, L.; Li, F.; et al. Metformin Blocks Myeloid-Derived Suppressor Cell Accumulation through AMPK-DACH1-CXCL1 Axis. OncoImmunology 2018, 7, e1442167. [Google Scholar] [CrossRef] [PubMed]
- Trillo-Tinoco, J.; Sierra, R.A.; Mohamed, E.; Cao, Y.; de Mingo-Pulido, A.; Gilvary, D.L.; Anadon, C.M.; Costich, T.L.; Wei, S.; Flores, E.R.; et al. AMPK Alpha-1 Intrinsically Regulates the Function and Differentiation of Tumor Myeloid-Derived Suppressor Cells. Cancer Res. 2019, 79, 5034–5047. [Google Scholar] [CrossRef] [PubMed]
- Rong, Y.; Yuan, C.H.; Qu, Z.; Zhou, H.; Guan, Q.; Yang, N.; Leng, X.H.; Bu, L.; Wu, K.; Wang, F.B. Doxorubicin Resistant Cancer Cells Activate Myeloid-Derived Suppressor Cells by Releasing PGE2. Sci. Rep. 2016, 6, 23824. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Zhang, Z.; Bi, Y.; Fu, Z.; Gong, P.; Li, Y.; Yu, Q.; Jia, A.; Wang, J.; Xue, L.; et al. MTOR Signaling Disruption from Myeloid-Derived Suppressive Cells Protects against Immune-Mediated Hepatic Injury through the HIF1α-Dependent Glycolytic Pathway. J. Leukoc. Biol. 2016, 6, 23824. [Google Scholar] [CrossRef] [PubMed]
- Zhang, C.; Wang, S.; Li, J.; Zhang, W.; Zheng, L.; Yang, C.; Zhu, T.; Rong, R. The Mtor Signal Regulates Myeloid-Derived Suppressor Cells Differentiation and Immunosuppressive Function in Acute Kidney Injury. Cell Death Dis. 2017, 8, e2695. [Google Scholar] [CrossRef] [PubMed]
- Martina, M.N.; Noel, S.; Bandapalle, S.; Hamad, A.R.A.; Rabb, H. T Lymphocytes and Acute Kidney Injury: Update. Nephron Clin. Pract. 2014, 127, 51–55. [Google Scholar] [CrossRef] [PubMed]
- Porta, C.; Paglino, C.; Mosca, A. Targeting PI3K/Akt/MTOR Signaling in Cancer. Front. Oncol. 2014, 4, 64. [Google Scholar] [CrossRef] [PubMed]
- Xie, S.; Chen, M.; Yan, B.; He, X.; Chen, X.; Li, D. Identification of a Role for the PI3K/AKT/MTOR Signaling Pathway in Innate Immune Cells. PLoS ONE 2014, 9, e94496. [Google Scholar] [CrossRef] [PubMed]
- Mafi, S.; Mansoori, B.; Taeb, S.; Sadeghi, H.; Abbasi, R.; Cho, W.C.; Rostamzadeh, D. MTOR-Mediated Regulation of Immune Responses in Cancer and Tumor Microenvironment. Front. Immunol. 2022, 12, 774103. [Google Scholar] [CrossRef] [PubMed]
- Weichhart, T.; Säemann, M.D. The PI3K/Akt/MTOR Pathway in Innate Immune Cells: Emerging Therapeutic Applications. Ann. Rheum. Dis. 2008, 67, iii70–iii74. [Google Scholar] [CrossRef] [PubMed]
- Sun, Y.; Han, X.; Shang, C.; Wang, Y.; Xu, B.; Jiang, S.; Mo, Y.; Wang, D.; Ke, Y.; Zeng, X. The Downregulation of Type I IFN Signaling in G-MDSCs under Tumor Conditions Promotes Their Development towards an Immunosuppressive Phenotype. Cell Death Dis. 2022, 13, 36. [Google Scholar] [CrossRef] [PubMed]
- Ribechini, E.; Hutchinson, J.A.; Hergovits, S.; Heuer, M.; Lucas, J.; Schleicher, U.; Garrote, A.L.J.; Potter, S.J.; Riquelme, P.; Brackmann, H.; et al. Novel GM-CSF Signals via IFN-GR/IRF-1 and AKT/MTOR License Monocytes for Suppressor Function. Blood Adv. 2017, 1, 947–960. [Google Scholar] [CrossRef] [PubMed]
- Jiang, X.; Wu, A.; Yan, J.; Chen, J.; Wen, Y.; Wu, H.; Yan, N.; Yang, Z.; Liu, F.; Li, P. Eleutheroside A Inhibits PI3K/AKT1/MTOR-Mediated Glycolysis in MDSCs to Alleviate Their Immunosuppressive Function in Gastric Cancer. Int. Immunol. 2025, 159, 114907. [Google Scholar] [CrossRef] [PubMed]
- Rößner, S.; Voigtländer, C.; Wiethe, C.; Hänig, J.; Seifarth, C.; Lutz, M.B. Myeloid Dendritic Cell Precursors Generated from Bone Marrow Suppress T Cell Responses via Cell Contact and Nitric Oxide Production in Vitro. Eur. J. Immunol. 2005, 35, 3533–3544. [Google Scholar] [CrossRef] [PubMed]
- Dolcetti, L.; Peranzoni, E.; Ugel, S.; Marigo, I.; Gomez, A.F.; Mesa, C.; Geilich, M.; Winkels, G.; Traggiai, E.; Casati, A.; et al. Hierarchy of Immunosuppressive Strength among Myeloid-Derived Suppressor Cell Subsets Is Determined by GM-CSF. Eur. J. Immunol. 2010, 40, 22–35. [Google Scholar] [CrossRef] [PubMed]
- Kumar, A.; Taghi Khani, A.; Sanchez Ortiz, A.; Swaminathan, S. GM-CSF: A Double-Edged Sword in Cancer Immunotherapy. Front. Immunol. 2022, 13, 901277. [Google Scholar] [CrossRef] [PubMed]
- Sun, L.; Rautela, J.; Delconte, R.B.; Souza-Fonseca-Guimaraes, F.; Carrington, E.M.; Schenk, R.L.; Herold, M.J.; Huntington, N.D.; Lew, A.M.; Xu, Y.; et al. GM-CSF Quantity Has a Selective Effect on Granulocytic vs. Monocytic Myeloid Development and Function. Front. Immunol. 2018, 9, 1922. [Google Scholar] [CrossRef] [PubMed]
- Gabrilovich, D.I.; Ostrand-Rosenberg, S.; Bronte, V. Coordinated Regulation of Myeloid Cells by Tumours. Nat. Rev. Immunol. 2012, 12, 253–268. [Google Scholar] [CrossRef] [PubMed]
- Hallowell, R.W.; Collins, S.L.; Craig, J.M.; Zhang, Y.; Oh, M.; Illei, P.B.; Chan-Li, Y.; Vigeland, C.L.; Mitzner, W.; Scott, A.L.; et al. MTORC2 Signalling Regulates M2 Macrophage Differentiation in Response to Helminth Infection and Adaptive Thermogenesis. Nat. Commun. 2017, 8, 14208. [Google Scholar] [CrossRef] [PubMed]
- Huang, S.C.C.; Smith, A.M.; Everts, B.; Colonna, M.; Pearce, E.L.; Schilling, J.D.; Pearce, E.J. Metabolic Reprogramming Mediated by the MTORC2-IRF4 Signaling Axis Is Essential for Macrophage Alternative Activation. Immunity 2016, 45, 817–830. [Google Scholar] [CrossRef] [PubMed]
- Raïch-Regué, D.; Fabian, K.P.; Watson, A.R.; Fecek, R.J.; Storkus, W.J.; Thomson, A.W. Intratumoral Delivery of MTORC2-Deficient Dendritic Cells Inhibits B16 Melanoma Growth by Promoting CD8+ Effector T Cell Responses. OncoImmunology 2016, 5, e1146841. [Google Scholar] [CrossRef] [PubMed]
- Hawkins, P.T.; Stephens, L.R. PI3K Signalling in Inflammation. Biochim. Biophys. Acta Mol. Cell Biol. Lipids 2015, 1851, 882–897. [Google Scholar] [CrossRef] [PubMed]
- Fruman, D.A.; Chiu, H.; Hopkins, B.D.; Bagrodia, S.; Cantley, L.C.; Abraham, R.T. The PI3K Pathway in Human Disease. Cell 2017, 170, 605–635. [Google Scholar] [CrossRef] [PubMed]
- van Wigcheren, G.F.; Cuenca-Escalona, J.; Stelloo, S.; Brake, J.; Peeters, E.; Horrevorts, S.K.; Frölich, S.; Ramos-Tomillero, I.; Wesseling-Rozendaal, Y.; van Herpen, C.M.L.; et al. Myeloid-Derived Suppressor Cells and Tolerogenic Dendritic Cells Are Distinctively Induced by PI3K and Wnt Signaling Pathways. J. Biol. Chem. 2023, 299, 105276. [Google Scholar] [CrossRef] [PubMed]
- Gato-Cañas, M.; de Morentin, X.M.; Blanco-Luquin, I.; Fernandez-Irigoyen, J.; Zudaire, I.; Liechtenstein, T.; Arasanz, H.; Lozano, T.; Casares, N.; Chaikuad, A.; et al. A Core of Kinase-Regulated Interactomes Defines the Neoplastic MDSC Lineage. Oncotarget 2015, 6, 27160–27175. [Google Scholar] [CrossRef] [PubMed]
- Kaneda, M.M.; Messer, K.S.; Ralainirina, N.; Li, H.; Leem, C.J.; Gorjestani, S.; Woo, G.; Nguyen, A.V.; Figueiredo, C.C.; Foubert, P.; et al. Erratum: Corrigendum: PI3Kγ Is a Molecular Switch That Controls Immune Suppression. Nature 2016, 542, 124. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.; Xia, X.; Mao, L.; Wang, S. The CCAAT/Enhancer-Binding Protein Family: Its Roles in MDSC Expansion and Function. Front. Immunol. 2019, 10, 1804. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.-W.; Tseng, H.-P.; Chen, L.-C.; Chen, B.-K.; Chang, W.-C. Functional Cooperation of Simian Virus 40 Promoter Factor 1 and CCAAT/Enhancer-Binding Protein β and δ in Lipopolysaccharide-Induced Gene Activation of IL-10 in Mouse Macrophages. J. Immunol. 2003, 171, 821–828. [Google Scholar] [CrossRef] [PubMed]
- Qi, H.; Li, Y.; Liu, X.; Jiang, Y.; Li, Z.; Xu, X.; Zhang, H.; Hu, X. Tim-3 Regulates the Immunosuppressive Function of Decidual MDSCs via the FynSTAT3-C/EBPβ Pathway during Toxoplasma Gondii Infection. PLoS Pathog. 2023, 19, e1011329. [Google Scholar] [CrossRef] [PubMed]
- Davis, R.J.; Moore, E.C.; Clavijo, P.E.; Friedman, J.; Cash, H.; Chen, Z.; Silvin, C.; Van Waes, C.; Allen, C. Anti-PD-L1 Efficacy Can Be Enhanced by Inhibition of Myeloid-Derived Suppressor Cells with a Selective Inhibitor of PI3Kd/G. Cancer Res. 2017, 77, 2607–2619. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, S.; Abu-Eid, R.; Shrimali, R.; Webb, M.; Verma, V.; Doroodchi, A.; Berrong, Z.; Samara, R.; Rodriguez, P.C.; Mkrtichyan, M.; et al. Differential PI3Kδ Signaling in CD4+ T-Cell Subsets Enables Selective Targeting of t Regulatory Cells to Enhance Cancer Immunotherapy. Cancer Res. 2017, 77, 1892–1904. [Google Scholar] [CrossRef] [PubMed]
- Ali, K.; Soond, D.R.; Piñeiro, R.; Hagemann, T.; Pearce, W.; Lim, E.L.; Bouabe, H.; Scudamore, C.L.; Hancox, T.; Maecker, H.; et al. Inactivation of PI(3)K P110δ Breaks Regulatory T-Cell-Mediated Immune Tolerance to Cancer. Nature 2014, 510, 407–411. [Google Scholar] [CrossRef] [PubMed]
- Lauder, S.N.; Smart, K.; Bart, V.M.T.; Pires, A.; Scott, J.; Milutinovic, S.; Godkin, A.; Vanhaesebroeck, B.; Gallimore, A. Treg-Driven Tumour Control by PI3Kδ Inhibition Limits Myeloid-Derived Suppressor Cell Expansion. Br. J. Cancer 2022, 127, 1595–1602. [Google Scholar] [CrossRef] [PubMed]
- Rothlin, C.V.; Carrera-Silva, E.A.; Bosurgi, L.; Ghosh, S. TAM Receptor Signaling in Immune Homeostasis. Annu. Rev. Immunol. 2015, 33, 355–391. [Google Scholar] [CrossRef] [PubMed]
- Triantafyllou, E.; Pop, O.T.; Possamai, L.A.; Wilhelm, A.; Liaskou, E.; Singanayagam, A.; Bernsmeier, C.; Khamri, W.; Petts, G.; Dargue, R.; et al. MerTK Expressing Hepatic Macrophages Promote the Resolution of Inflammation in Acute Liver Failure. Gut 2018, 67, 333–347. [Google Scholar] [CrossRef] [PubMed]
- Su, Y.T.; Butler, M.; Zhang, M.; Zhang, W.; Song, H.; Hwang, L.; Tran, A.D.; Bash, R.E.; Schorzman, A.N.; Pang, Y.; et al. MerTK Inhibition Decreases Immune Suppressive Glioblastoma-Associated Macrophages and Neoangiogenesis in Glioblastoma Microenvironment. Neuro-Oncol. Adv. 2020, 2, vdaa065. [Google Scholar] [CrossRef] [PubMed]
- Leroy, V.; Jr, G.R.U.; Sharma, A.K.; Leroy, V.; Kollareth, D.J.M.; Tu, Z.; Valisno, J.A.C.; Woolet-stockton, M.; Saha, B.; Emtiazjoo, A.M.; et al. Resolution of Ischemia/Reperfusion Injury after Lung Transplant MerTK-Dependent Efferocytosis by Monocytic-MDSCs Mediates Resolution of Ischemia/Reperfusion Injury after Lung Transplant. JCI Insight 2024, 9, e179876. [Google Scholar] [CrossRef] [PubMed]
- Holtzhausen, A.; Harris, W.; Ubil, E.; Hunter, D.M.; Zhao, J.; Zhang, Y.; Zhang, D.; Liu, Q.; Wang, X.; Graham, D.K.; et al. TAM Family Receptor Kinase Inhibition Reverses MDSC-Mediated Suppression and Augments Anti–PD-1 Therapy in Melanoma. Cancer Immunol. Res. 2019, 7, 1672–1686. [Google Scholar] [CrossRef] [PubMed]
- Graham, D.K.; Deryckere, D.; Davies, K.D.; Earp, H.S. The TAM Family: Phosphatidylserine-Sensing Receptor Tyrosine Kinases Gone Awry in Cancer. Nat. Rev. Cancer 2014, 14, 769–785. [Google Scholar] [CrossRef] [PubMed]
- Wei, Z.; Liu, H.T. MAPK Signal Pathways in the Regulation of Cell Proliferation in Mammalian Cells. Cell Res. 2002, 12, 9–18. [Google Scholar] [CrossRef] [PubMed]
- Kim, E.K.; Choi, E.J. Pathological Roles of MAPK Signaling Pathways in Human Diseases. Biochim. Biophys. Acta Mol. Cell Biol. Lipids 2010, 1802, 396–405. [Google Scholar] [CrossRef] [PubMed]
- Geest, C.R.; Coffer, P.J. MAPK Signaling Pathways in the Regulation of Hematopoiesis. J. Leukoc. Biol. 2009, 86, 237–250. [Google Scholar] [CrossRef] [PubMed]
- Yu, J.; Li, H.; Zhang, Z.; Lin, W.; Wei, X.; Shao, B. Targeting the MDSCs of Tumors In Situ With Inhibitors of the MAPK Signaling Pathway to Promote Tumor Regression. Front. Oncol. 2021, 11, 647312. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.J.; Oh, J.Y. Mesenchymal Stem/Stromal Cells Induce Myeloid-Derived Suppressor Cells in the Bone Marrow via the Activation of the c-Jun N-Terminal Kinase Signaling Pathway. Int. J. Mol. Sci. 2024, 25, 1119. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.J.; Ko, J.H.; Kim, H.J.; Jeong, H.J.; Oh, J.Y. Mesenchymal Stromal Cells Induce Distinct Myeloid-Derived Suppressor Cells in Inflammation. JCI Insight 2020, 5, e136059. [Google Scholar] [CrossRef] [PubMed]
- Alicea-Torres, K.; Sanseviero, E.; Gui, J.; Chen, J.; Veglia, F.; Yu, Q.; Donthireddy, L.; Kossenkov, A.; Lin, C.; Fu, S.; et al. Immune Suppressive Activity of Myeloid-Derived Suppressor Cells in Cancer Requires Inactivation of the Type I Interferon Pathway. Nat. Commun. 2021, 12, 1717. [Google Scholar] [CrossRef] [PubMed]
- Johnson, J.L.; Yaron, T.M.; Huntsman, E.M.; Kerelsky, A.; Song, J.; Regev, A.; Lin, T.Y.; Liberatore, K.; Cizin, D.M.; Cohen, B.M.; et al. An Atlas of Substrate Specificities for the Human Serine/Threonine Kinome. Nature 2023, 613, 759–766. [Google Scholar] [CrossRef] [PubMed]
- Maenhout, S.K.; Thielemans, K.; Aerts, J.L. Location, Location, Location: Functional and Phenotypic Heterogeneity between Tumor-Infiltrating and Non-Infiltrating Myeloid-Derived Suppressor Cells. OncoImmunology 2014, 3, e956579. [Google Scholar] [CrossRef] [PubMed]
- Kumar, V.; Patel, S.; Tcyganov, E.; Gabrilovich, D.I. The Nature of Myeloid-Derived Suppressor Cells in the Tumor Microenvironment. Trends Immunol. 2016, 37, 208–220. [Google Scholar] [CrossRef] [PubMed]
- Lou, X.; Gao, D.; Yang, L.; Wang, Y.; Hou, Y. Endoplasmic Reticulum Stress Mediates the Myeloid-Derived Immune Suppression Associated with Cancer and Infectious Disease. J. Transl. Med. 2023, 21, 1. [Google Scholar] [CrossRef] [PubMed]
- Mohamed, E.; Sierra, R.A.; Trillo-Tinoco, J.; Cao, Y.; Innamarato, P.; Payne, K.K.; de Mingo Pulido, A.; Mandula, J.; Zhang, S.; Thevenot, P.; et al. The Unfolded Protein Response Mediator PERK Governs Myeloid Cell-Driven Immunosuppression in Tumors through Inhibition of STING Signaling. Immunity 2020, 52, 668–682.e7. [Google Scholar] [CrossRef] [PubMed]
- Liu, Z.; Lv, Y.; Zhao, N.; Guan, G.; Wang, J. Protein Kinase R-like ER Kinase and Its Role in Endoplasmic Reticulum Stress-Decided Cell Fate. Cell Death Dis. 2015, 6, e1822. [Google Scholar] [CrossRef] [PubMed]
- He, F.; Ru, X.; Wen, T. NRF2, a Transcription Factor for Stress Response and Beyond. Int. J. Mol. Sci. 2020, 21, 4777. [Google Scholar] [CrossRef] [PubMed]
- Beury, D.W.; Carter, K.A.; Nelson, C.; Sinha, P.; Hanson, E.; Nyandjo, M.; Fitzgerald, P.J.; Majeed, A.; Wali, N.; Ostrand-Rosenberg, S. Myeloid-Derived Suppressor Cell Survival and Function Are Regulated by the Transcription Factor Nrf2. J. Immunol. 2016, 196, 3470–3478. [Google Scholar] [CrossRef] [PubMed]
- Ohl, K.; Fragoulis, A.; Klemm, P.; Baumeister, J.; Klock, W.; Verjans, E.; Böll, S.; Möllmann, J.; Lehrke, M.; Costa, I.; et al. Nrf2 Is a Central Regulator of Metabolic Reprogramming of Myeloid-Derived Suppressor Cells in Steady State and Sepsis. Front. Immunol. 2018, 9, 1552. [Google Scholar] [CrossRef] [PubMed]
- Regazzi, R.; Widmann, C. Fatty Acid Metabolism Regulates Cell Survival in Specific Niches. Curr. Opin. Lipidol. 2017, 28, 284–285. [Google Scholar] [CrossRef] [PubMed]
- Xin, G.; Chen, Y.; Topchyan, P.; Kasmani, M.Y.; Burns, R.; Volberding, P.J.; Wu, X.; Cohn, A.; Chen, Y.; Lin, C.W.; et al. Targeting PIM1-Mediated Metabolism in Myeloid Suppressor Cells to Treat Cancer. Cancer Immunol. Res. 2021, 9, 454–469. [Google Scholar] [CrossRef] [PubMed]
- Choudhury, R.; Bahadi, C.K.; Ray, I.P.; Dash, P.; Pattanaik, I.; Mishra, S.; Mohapatra, S.R.; Patnaik, S.; Nikhil, K. PIM1 Kinase and Its Diverse Substrate in Solid Tumors. Cell Commun. Signal. 2024, 22, 529. [Google Scholar] [CrossRef] [PubMed]
- Clements, A.N.; Warfel, N.A. Targeting PIM Kinases to Improve the Efficacy of Immunotherapy. Cells 2022, 11, 3007. [Google Scholar] [CrossRef] [PubMed]
- Volberding, P.J.; Xin, G.; Kasmani, M.Y.; Khatun, A.; Brown, A.K.; Nguyen, C.; Stancill, J.S.; Martinez, E.; Corbett, J.A.; Cui, W. Suppressive Neutrophils Require PIM1 for Metabolic Fitness and Survival during Chronic Viral Infection. Cell Rep. 2021, 35, 109160. [Google Scholar] [CrossRef] [PubMed]
- Liu, S.; Zhang, H.; Li, Y.; Zhang, Y.; Bian, Y.; Zeng, Y.; Yao, X.; Wan, J.; Chen, X.; Li, J.; et al. S100A4 Enhances Protumor Macrophage Polarization by Control of PPAR-Î 3-Dependent Induction of Fatty Acid Oxidation. J. Immunother. Cancer 2021, 9, e002548. [Google Scholar] [CrossRef] [PubMed]
- Tokumitsu, H.; Sakagami, H. Molecular Mechanisms Underlying Ca2+/Calmodulin-Dependent Protein Kinase Kinase Signal Transduction. Int. J. Mol. Sci. 2022, 23, 11025. [Google Scholar] [CrossRef] [PubMed]
- Teng, E.C.; Racioppi, L.; Means, A.R. A Cell-Intrinsic Role for CaMKK2 in Granulocyte Lineage Commitment and Differentiation. J. Leukoc. Biol. 2011, 90, 897–909. [Google Scholar] [CrossRef] [PubMed]
- Racioppi, L.; Lento, W.; Huang, W.; Arvai, S.; Doan, P.L.; Harris, J.R.; Marcon, F.; Nakaya, H.I.; Liu, Y.; Chao, N. Calcium/Calmodulin-Dependent Kinase Kinase 2 Regulates Hematopoietic Stem and Progenitor Cell Regeneration. Cell Death Dis. 2017, 8, e3076. [Google Scholar] [CrossRef] [PubMed]
- Huang, W.; Liu, Y.; Luz, A.; Berrong, M.; Meyer, J.N.; Zou, Y.; Swann, E.; Sundaramoorthy, P.; Kang, Y.; Jauhari, S.; et al. Calcium/Calmodulin Dependent Protein Kinase Kinase 2 Regulates the Expansion of Tumor-Induced Myeloid-Derived Suppressor Cells. Front. Immunol. 2021, 12, 754083. [Google Scholar] [CrossRef] [PubMed]
- Najar, M.A.; Rex, D.A.B.; Modi, P.K.; Agarwal, N.; Dagamajalu, S.; Karthikkeyan, G.; Vijayakumar, M.; Chatterjee, A.; Sankar, U.; Prasad, T.S.K. A Complete Map of the Calcium/Calmodulin-Dependent Protein Kinase Kinase 2 (CAMKK2) Signaling Pathway. J. Cell Commun. Signal. 2020, 15, 283–290. [Google Scholar] [CrossRef] [PubMed]
- Tomaszewski, W.H.; Waibl-Polania, J.; Chakraborty, M.; Perera, J.; Ratiu, J.; Miggelbrink, A.; McDonnell, D.P.; Khasraw, M.; Ashley, D.M.; Fecci, P.E.; et al. Neuronal CaMKK2 Promotes Immunosuppression and Checkpoint Blockade Resistance in Glioblastoma. Nat. Commun. 2022, 13, 6483. [Google Scholar] [CrossRef] [PubMed]
- Condamine, T.; Gabrilovich, D.I. Molecular Mechanisms Regulating Myeloid-Derived Suppressor Cell Differentiation and Function. Trends Immunol. 2011, 32, 19–25. [Google Scholar] [CrossRef] [PubMed]
- Racioppi, L.; Noeldner, P.K.; Lin, F.; Arvai, S.; Means, A.R. Calcium/Calmodulin-Dependent Protein Kinase Kinase 2 Regulates Macrophage-Mediated Inflammatory Responses. J. Biol. Chem. 2012, 287, 11579–11591. [Google Scholar] [CrossRef] [PubMed]
- Grant, S.K. Therapeutic Protein Kinase Inhibitors. Cell. Mol. Life Sci. 2009, 66, 1163–1177. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Yang, P.L.; Gray, N.S. Targeting Cancer with Small Molecule Kinase Inhibitors. Nat. Rev. Cancer 2009, 9, 28–39. [Google Scholar] [CrossRef] [PubMed]
- Zaky, M.Y.; John, J.; Vashisht, M.; Singh, P.; Al-Hatamleh, M.A.I.; Siddoway, K.; Chen, Z.; Wang, J.H. Targeting Myeloid Cells in Head and Neck Squamous Cell Carcinoma: A Kinase Inhibitor Library Screening Approach. Int. J. Mol. Sci. 2024, 25, 12277. [Google Scholar] [CrossRef] [PubMed]
- Gross, S.; Rahal, R.; Stransky, N.; Lengauer, C.; Hoeflich, K.P. Targeting Cancer with Kinase Inhibitors. J. Clin. Investig. 2015, 125, 1780–1789. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.; Akbar, S.M.F.; Abe, M.; Hiasa, Y.; Onji, M. Immunosuppressive Functions of Hepatic Myeloid-Derived Suppressor Cells of Normal Mice and in a Murine Model of Chronic Hepatitis B Virus. Clin. Exp. Immunol. 2011, 166, 134–142. [Google Scholar] [CrossRef] [PubMed]
- Fiocchi, C. What Is “Physiological” Intestinal Inflammation and How Does It Differ from “Pathological” Inflammation? Inflamm. Bowel Dis. 2008, 14, S77–S78. [Google Scholar] [CrossRef] [PubMed]
- Whitmarsh, A.J.; Davis, R.J. Regulation of Transcription Factor Function by Phosphorylation. Cell. Mol. Life Sci. 2000, 57, 1172–1183. [Google Scholar] [CrossRef] [PubMed]
- Waitkus, M.S.; Chandrasekharan, U.M.; Willard, B.; Tee, T.L.; Hsieh, J.K.; Przybycin, C.G.; Rini, B.I.; DiCorleto, P.E. Signal Integration and Gene Induction by a Functionally Distinct STAT3 Phosphoform. Mol. Cell. Biol. 2014, 34, 1800–1811. [Google Scholar] [CrossRef] [PubMed]
- Huang, G.; Yan, H.; Ye, S.; Tong, C.; Ying, Q.L. STAT3 Phosphorylation at Tyrosine 705 and Serine 727 Differentially Regulates Mouse Esc Fates. Stem Cells 2013, 32, 1149–1160. [Google Scholar] [CrossRef] [PubMed]
- Berkley, K.; Zalejski, J.; Sharma, A. Targeting STAT3 for Cancer Therapy: Focusing on Y705, S727, or Dual Inhibition? Cancers 2025, 17, 755. [Google Scholar] [CrossRef] [PubMed]
- Hazan-Halevy, I.; Harris, D.; Liu, Z.; Liu, J.; Li, P.; Chen, X.; Shanker, S.; Ferrajoli, A.; Keating, M.J.; Estrov, Z. STAT3 Is Constitutively Phosphorylated on Serine 727 Residues, Binds DNA, and Activates Transcription in CLL Cells. Blood 2010, 115, 2852–2863. [Google Scholar] [CrossRef] [PubMed]
| Protein Kinases | Models | Species | MDSC Phenotype | Transcription Factors | Roles | Pharmacological Inhibitors | Ref. |
|---|---|---|---|---|---|---|---|
| mTORC1 | Murine tumor model, allogeneic transplant model | M | M-MDSC | NA | Rapamycin treatment or genetic deletion of mTORC1 decreased number of M-MDSCs and immunosuppressive function through inhibiting glycolysis. | Rapamycin | [33] |
| mTORC1 | Murine tumor model | M | M-MDSC | NA | Rapamycin treatment decreased glycolysis and reduced the suppressive activities of M- MDSCs. | Rapamycin | [34] |
| mTORC1/mTORC2 | Murine model of Pristane-induced lupus | M | M-MDSC | IRF-8 | Metformin and mTOR inhibitors (rapamycin and NK128) decreased the percentage of M-MDSCs; adoptive transfer of metformin-treated M-MDSCs attenuated the disease symptoms. | Metformin, Rapamycin, NK128 | [36] |
| mTORC1 | Murine models of hepatic injury (CIH and PIH) | M | MDSC | HIF-1α | Rapamycin treatment potentiated the immunosuppressive function of MDSCs and mTORC1-deficient MDSCs exerted protective effects against immune-mediated hepatic injury and improved survival. | Rapamycin | [46] |
| mTORC1 | Murine model of acute kidney injury | M | G-MDSC, M-MDSC | Rnux1 | Rapamycin-treated MDSCs limited T-cell infiltration and significantly improved renal function; mTOR inhibition redirected MDSC differentiation towards the CD11b+Ly6G+Ly6Clow G-MDSC subset and enhanced their immunosuppressive activity. | Rapamycin | [47] |
| PI3Ks | HNSCC patient samples | H | M-MDSC | FOXO | PI3K inhibition reversed the immature phenotype to a more mature phenotype. T-cell suppression was rescued when co-cultured with PI3K-inhibited M-MDSCs. | Wortmanin, LY294002 | [66] |
| PI3K-AkT | In vitro tumor infiltrating MDSC model | M | MDSC | NA | Akt inhibition led to the death of MDSCs. | X | [67] |
| PI3K δ/γ | Murine tumor models of head and neck cancers | M | G-MDSC | NA | IPI-145 treatment of G-MDSCs reduced suppressive ability and decreased Arg1 and Nos2 transcript levels but did not induce cell death. | IPI-145 | [72] |
| MERTK | Murine model of lung transplantation | M | M-MDSC | NA | M-MDSCs with activated MERTK effectively facilitated the resolution of inflammation in ischemia/reperfusion injury by clearing the apoptotic neutrophils at injury sites, while M-MDSCs derived from MERTK−/− mice failed to exhibit an immunosuppressive effect. | NA | [79] |
| TAM RTKs | Murine model of melanoma | M | MDSC | STAT3 | The spleen MDSCs from Mertk−/−, Axl−/−, and Tyro3−/− mice showed decreased expressions of suppressive mediators such as arginase-1, iNOS TGF-β, IDO, and ROS, and the functional assay was consistent with these results. | NA | [80] |
| ERK1/2 and JNK | LL2 tumor model | M | G-MDSC, M-MDSC | NA | Inhibition of ERK1/2 and JNK with SCH772984 and SP600125, respectively, increased apoptosis of both MDSC populations. | SCH772984 and SP600125 | [84] |
| JNK | In vitro model | M | M-MDSC | NA | Pharmacological inhibition of JNK resulted in a failed induction of MDSC molecular features under MSC stimulation. | SP600125 | [87] |
| p38 | Murine tumor models, cancer patient samples | M, H | G-MDSC | IFNAR1 | Activation of p38 was required for the suppressive functions of G-MDSC. | LY2228820 | [88] |
| PERK | Murine tumor models, cancer patient materials | M, H | MDSC | NRF2 | PERK inhibition in MDSCs reduced immunosuppressive activity along with increased expressions of anti-tumor cytokines. | GSK-2606414, AMG-44 | [93] |
| PIM1 | Bilateral tumor model | M | G-MDSCs | PPAR-γ, p-Ser727-STAT3 | Required MDSCs’ immunosuppressive activities, caused ICB resistance. | AZD1208 | [99] |
| CaMKK2 | Lymphoma tumor model | M | MDSCs | NA | Deletion of Camkk2 induced terminal differentiation of MDSCs and reduced tumor growth. | STO-609 | [107] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kali, A.; Abdolla, N.; Perfilyeva, Y.V.; Ostapchuk, Y.O.; Tleulieva, R. The Role of Protein Kinases in the Suppressive Phenotype of Myeloid-Derived Suppressor Cells. Int. J. Mol. Sci. 2025, 26, 6936. https://doi.org/10.3390/ijms26146936
Kali A, Abdolla N, Perfilyeva YV, Ostapchuk YO, Tleulieva R. The Role of Protein Kinases in the Suppressive Phenotype of Myeloid-Derived Suppressor Cells. International Journal of Molecular Sciences. 2025; 26(14):6936. https://doi.org/10.3390/ijms26146936
Chicago/Turabian StyleKali, Aikyn, Nurshat Abdolla, Yuliya V. Perfilyeva, Yekaterina O. Ostapchuk, and Raikhan Tleulieva. 2025. "The Role of Protein Kinases in the Suppressive Phenotype of Myeloid-Derived Suppressor Cells" International Journal of Molecular Sciences 26, no. 14: 6936. https://doi.org/10.3390/ijms26146936
APA StyleKali, A., Abdolla, N., Perfilyeva, Y. V., Ostapchuk, Y. O., & Tleulieva, R. (2025). The Role of Protein Kinases in the Suppressive Phenotype of Myeloid-Derived Suppressor Cells. International Journal of Molecular Sciences, 26(14), 6936. https://doi.org/10.3390/ijms26146936





