Dichotomous Effects of Glypican-4 on Cancer Progression and Its Crosstalk with Oncogenes
Abstract
1. Introduction
2. Results
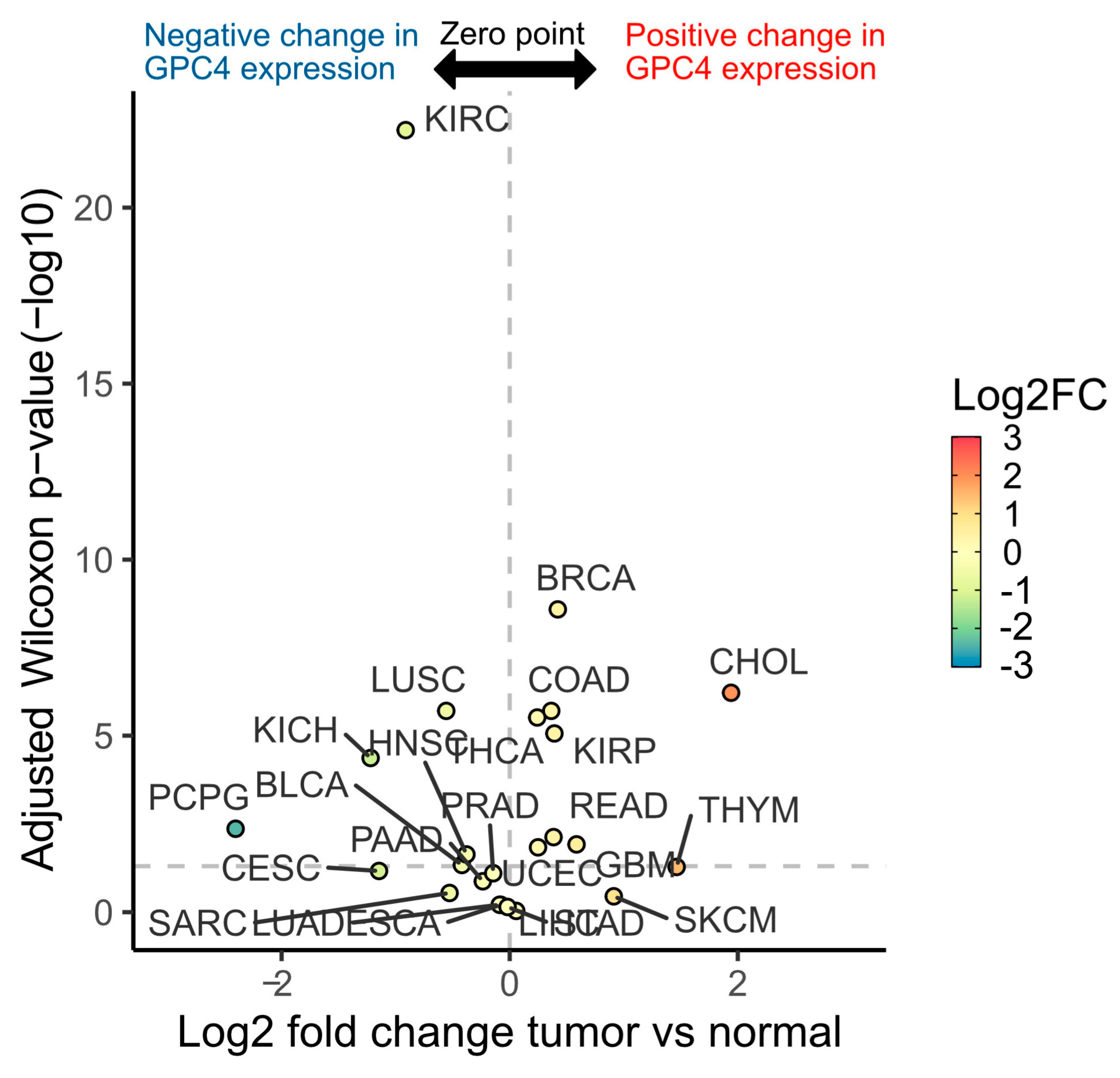
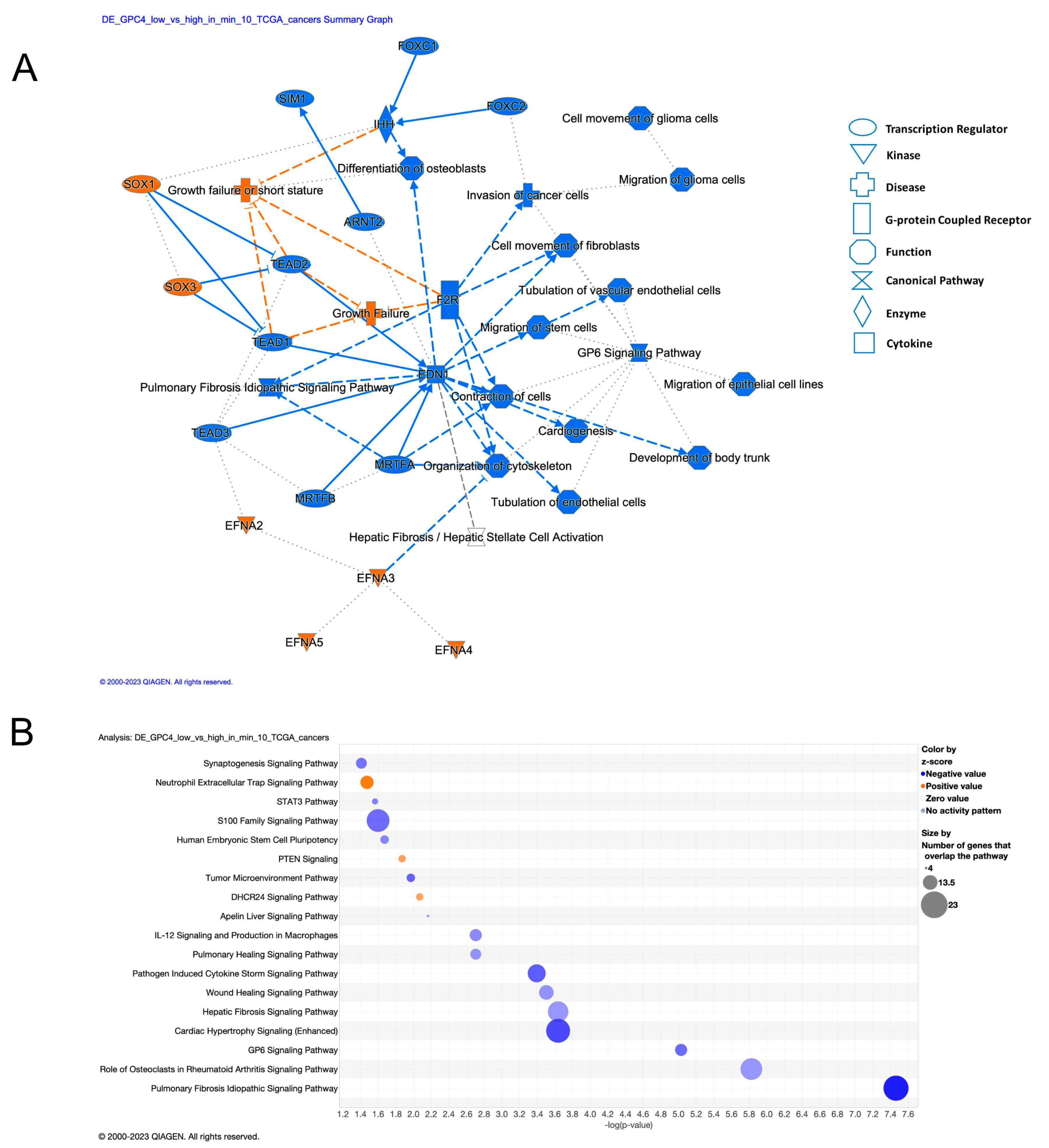
2.1. Wide Range of GPC4 Expression Differences between Normal and Cancer Tissues across TCGA Cancer Types
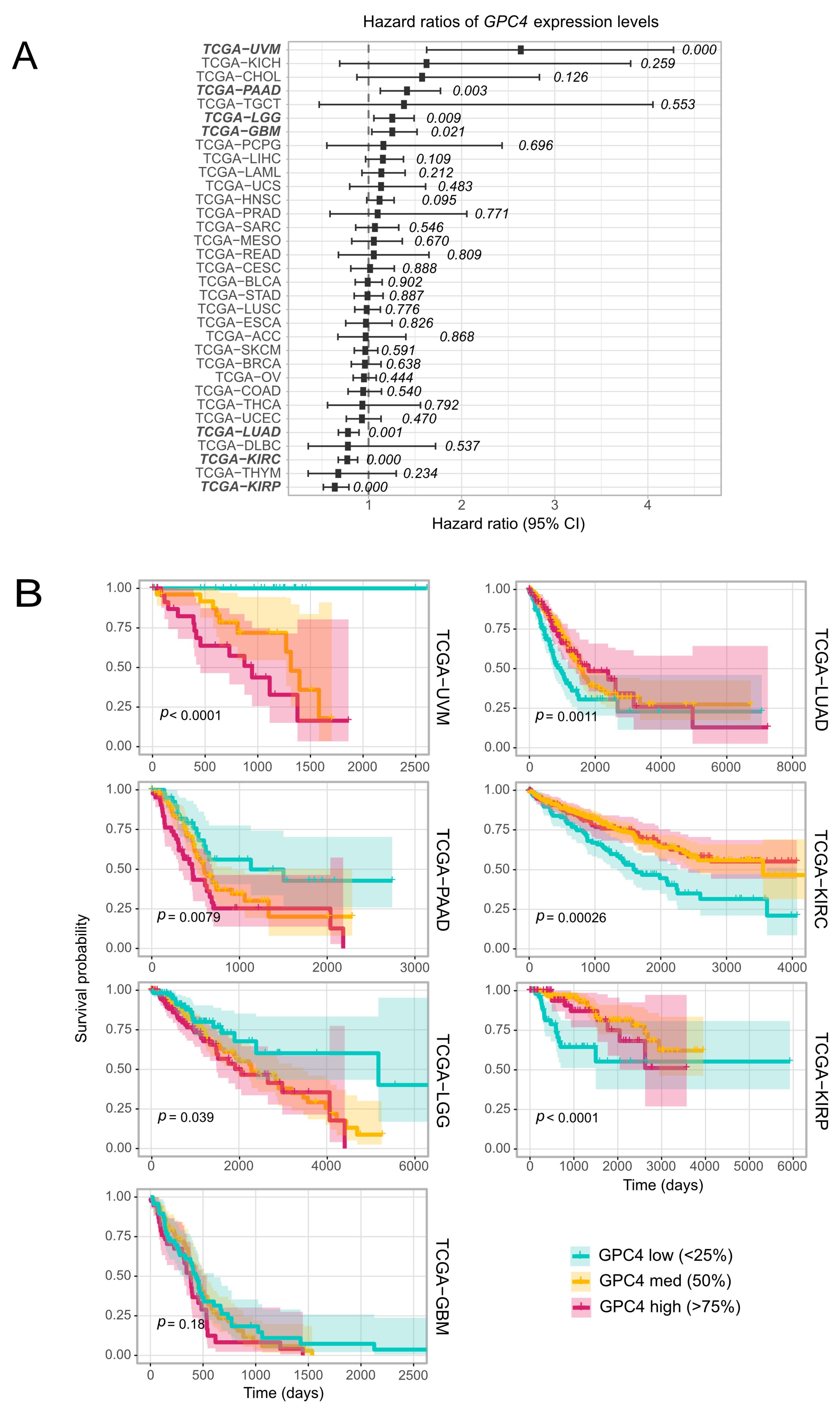
2.2. Cancer Survival Is Associated with GPC4 Expression Levels in a Cancer Type Specific Manner
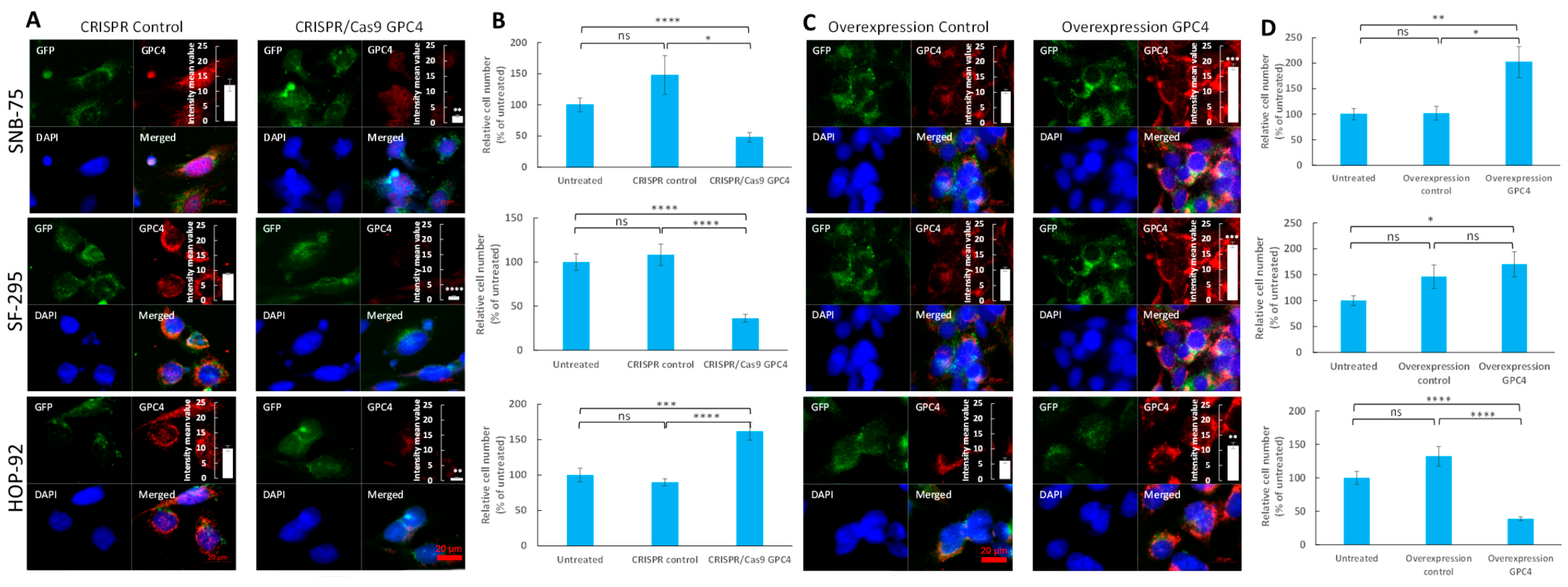
2.3. Suppression of GPC4 Attenuates Proliferation of Glioblastoma and Augments Proliferation of Lung Adenocarcinoma Cells
2.4. Overexpression of GPC4 Augments Proliferation of Glioblastoma and Attenuates Proliferation of Lung Adenocarcinoma Cells
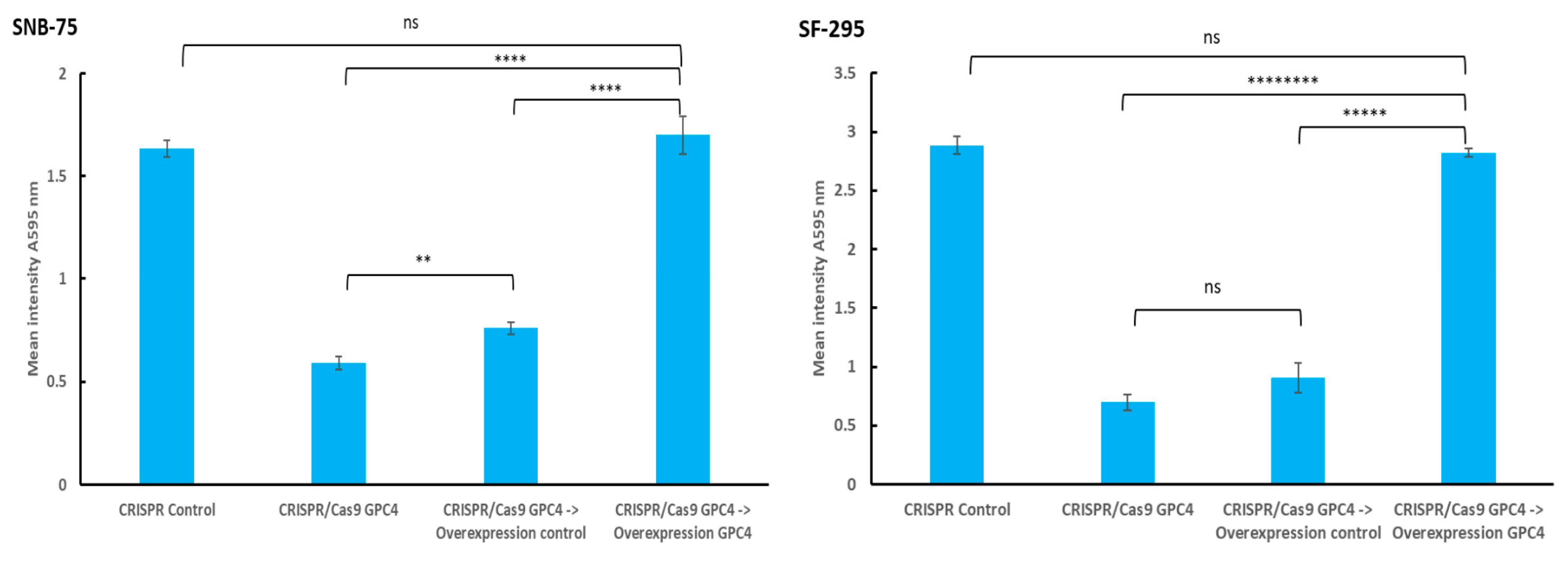
2.5. Overexpression of GPC4 in GPC4-Knockdown Glioblastoma Cells Resulted in Restored Proliferation Rate
2.6. Upregulation of GPC4 Activates Proto-Oncogenes in Glioblastoma but Not in Lung Adenocarcinoma
3. Discussion
4. Materials and Methods
4.1. TCGA Data Pre-Processing
4.2. Univariate Survival Analysis
4.3. Multivariate Cox PH Survival Analysis
4.4. Differential Expression (DE) Analysis
4.5. Pathway Analysis
4.6. Cell Culture
4.7. Transfection of Human GPC4 Targeting CRISPR/Cas9
4.8. Overexpression of GPC4 Using Ectopic Expression of Green Fluorescent Protein-Tagged Gpc4 (GFP-GPC4)
4.9. Fluorescence Imaging
4.10. Slot Blot Assay
4.11. Proliferation Rate Assay Using Crystal Violet
4.12. Statistical Analyses
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Fico, A.; Maina, F.; Dono, R. Fine-tuning of cell signaling by glypicans. Cell. Mol. Life Sci. 2011, 68, 923–929. [Google Scholar] [CrossRef] [PubMed]
- Barkovskaya, A.; Buffone, A., Jr.; Žídek, M.; Weaver, V.M. Proteoglycans as Mediators of Cancer Tissue Mechanics. Front. Cell Dev. Biol. 2020, 8, 569377. [Google Scholar] [CrossRef] [PubMed]
- De Pasquale, V.; Pavone, L.M. Heparan Sulfate Proteoglycan Signaling in Tumor Microenvironment. Int. J. Mol. Sci. 2020, 21, 6588. [Google Scholar] [CrossRef] [PubMed]
- Hassan, N.; Greve, B.; Espinoza-Sánchez, N.A.; Götte, M. Cell surface heparan sulfate proteoglycans as multifunctional integrators of signaling in cancer. Cell Signal. 2021, 77, 109822. [Google Scholar] [CrossRef] [PubMed]
- Kaur, S.P.; Cummings, B.S. Role of glypicans in regulation of the tumor microenvironment and cancer progression. Biochem. Pharmacol. 2019, 168, 108–118. [Google Scholar] [CrossRef] [PubMed]
- Li, N.; Spetz, M.R.; Ho, M. The Role of Glypicans in Cancer Progression and Therapy. J. Histochem. Cytochem. 2020, 68, 841–862. [Google Scholar] [CrossRef] [PubMed]
- Cheng, F.; Chérouvrier Hansson, V.; Georgolopoulos, G.; Mani, K. Attenuation of cancer proliferation by suppression of glypican-1 and its pleiotropic effects in neoplastic behavior. Oncotarget 2023, 14, 219–235. [Google Scholar] [CrossRef] [PubMed]
- Saito, T.; Sugiyama, K.; Hama, S.; Yamasaki, F.; Takayasu, T.; Nosaka, R.; Onishi, S.; Muragaki, Y.; Kawamata, T.; Kurisu, K. High Expression of Glypican-1 Predicts Dissemination and Poor Prognosis in Glioblastomas. World Neurosurg. 2017, 105, 282–288. [Google Scholar] [CrossRef] [PubMed]
- Zhou, C.Y.; Dong, Y.P.; Sun, X.; Sui, X.; Zhu, H.; Zhao, Y.Q.; Zhang, Y.Y.; Mason, C.; Zhu, Q.; Han, S.X. High levels of serum glypican-1 indicate poor prognosis in pancreatic ductal adenocarcinoma. Cancer Med. 2018, 7, 5525–5533. [Google Scholar] [CrossRef] [PubMed]
- Sabanathan, D.; Lund, M.E.; Campbell, D.H.; Walsh, B.J.; Gurney, H. Radioimmunotherapy for solid tumors: Spotlight on Glypican-1 as a radioimmunotherapy target. Ther. Adv. Med. Oncol. 2021, 13, 17588359211022918. [Google Scholar] [CrossRef] [PubMed]
- Chen, G.; Luo, D.; Zhong, N.; Li, D.; Zheng, J.; Liao, H.; Li, Z.; Lin, X.; Chen, Q.; Zhang, C.; et al. GPC2 Is a Potential Diagnostic, Immunological, and Prognostic Biomarker in Pan-Cancer. Front. Immunol. 2022, 13, 857308. [Google Scholar] [CrossRef]
- Shimizu, Y.; Suzuki, T.; Yoshikawa, T.; Endo, I.; Nakatsura, T. Next-Generation Cancer Immunotherapy Targeting Glypican-3. Front. Oncol. 2019, 9, 248. [Google Scholar] [CrossRef] [PubMed]
- Guo, L.; Wang, J.; Zhang, T.; Yang, Y. Glypican-5 is a tumor suppressor in non-small cell lung cancer cells. Biochem. Biophys. Res. 2016, 6, 108–112. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Wang, S.; Qiu, M.; Xia, W.; Xu, Y.; Mao, Q.; Wang, J.; Dong, G.; Xu, L.; Yang, X.; Yin, R. Glypican-5 suppresses Epithelial-Mesenchymal Transition of the lung adenocarcinoma by competitively binding to Wnt3a. Oncotarget 2016, 7, 79736–79746. [Google Scholar] [CrossRef] [PubMed]
- Sun, Y.; Xu, K.; He, M.; Fan, G.; Lu, H. Overexpression of Glypican 5 (GPC5) inhibits prostate cancer cell proliferation and invasion via suppressing Sp1-mediated EMT and activation of Wnt/beta-catenin signaling. Oncol. Res. 2018, 26, 565–572. [Google Scholar] [CrossRef] [PubMed]
- Yuan, Q.; Zhang, Y.; Li, J.; Cao, G.; Yang, W. High expression of microRNA-4295 contributes to cell proliferation and invasion of pancreatic ductal adenocarcinoma by the down-regulation of Glypican-5. Biochem. Biophys. Res. Commun. 2018, 497, 73–79. [Google Scholar] [CrossRef] [PubMed]
- Hong, X.; Zhang, Z.; Pan, L.; Ma, W.; Zhai, X.; Gu, C.; Zhang, Y.; Bi, X.; Huang, W.; Pei, H.; et al. MicroRNA-301b promotes the proliferation and invasion of glioma cells through enhancing activation of Wnt/β-catenin signaling via targeting Glypican-5. Eur. J. Pharmacol. 2019, 854, 39–47. [Google Scholar] [CrossRef]
- Li, Y.; Miao, L.; Cai, H.; Ding, J.; Xiao, Y.; Yang, J.; Zhang, D. The overexpression of glypican-5 promotes cancer cell migration and is associated with shorter overall survival in non-small cell lung cancer. Oncol. Lett. 2013, 6, 1565–1572. [Google Scholar] [CrossRef]
- Zhang, C.; Zhang, S.; Zhang, D.; Zhang, Z.; Xu, Y.; Liu, S. A lung cancer gene GPC5 could also be crucial in breast cancer. Mol. Genet. Metab. 2011, 103, 104–105. [Google Scholar] [CrossRef] [PubMed]
- Karapetsas, A.; Giannakakis, A.; Dangaj, D.; Lanitis, E.; Kynigopoulos, S.; Lambropoulou, M.; Tanyi, J.L.; Galanis, A.; Kakolyris, S.; Trypsianis, G.; et al. Overexpression of GPC6 and TMEM132D in early stage ovarian cancer correlates with CD8+ T-lymphocyte infiltration and increased patient survival. Biomed. Res. Int. 2015, 2015, 712438. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Li, M.; Shats, I.; Krahn, J.M.; Flake, G.P.; Umbach, D.M.; Li, X.; Li, L. Glypican 6 is a putative biomarker for metastatic progression of cutaneous melanoma. PLoS ONE 2019, 14, e0218067. [Google Scholar] [CrossRef]
- Cao, J.; Ma, J.; Sun, L.; Li, J.; Qin, T.; Zhou, C.; Cheng, L.; Chen, K.; Qian, W.; Duan, W.; et al. Targeting glypican-4 overcomes 5-FU resistance and attenuates stem cell-like properties via suppression of Wnt/beta-catenin pathway in pancreatic cancer cells. J. Cell. Biochem. 2018, 119, 9498–9512. [Google Scholar] [CrossRef] [PubMed]
- Munir, J.; Van Ngu, T.; Na Ayudthaya, P.D.; Ryu, S. Downregulation of glypican-4 facilitates breast cancer progression by inducing cell migration and proliferation. Biochem. Biophys. Res. Commun. 2020, 526, 91–97. [Google Scholar] [CrossRef] [PubMed]
- Muendlein, A.; Heinzle, C.; Brandtner, E.M.; Leiherer, A.; Drexel, H.; Dechow, T.; Decker, T. Circulating Glypican-4 Is a Predictor of 24-Month Overall Survival in Metastatic Breast Cancer. Oncol. Res. Treat. 2023, 46, 151–156. [Google Scholar] [CrossRef] [PubMed]
- Muendlein, A.; Severgnini, L.; Decker, T.; Heinzle, C.; Leiherer, A.; Geiger, K.; Drexel, H.; Winder, T.; Reimann, P.; Mayer, F.; et al. Circulating syndecan-1 and glypican-4 predict 12-month survival in metastatic colorectal cancer patients. Front. Oncol. 2022, 12, 1045995. [Google Scholar] [CrossRef] [PubMed]
- Legier, T.; Rattier, D.; Llewellyn, J.; Vannier, T.; Sorre, B.; Maina, F.; Dono, R. Epithelial disruption drives mesendoderm differentiation in human pluripotent stem cells by enabling TGF-β protein sensing. Nat. Commun. 2023, 14, 349. [Google Scholar] [CrossRef] [PubMed]
- He, S.; Li, W.; Wang, G.; Wang, X.; Fan, W.; Zhang, Z.; Li, N.; Hou, S. FTO-mediated m6A modification alleviates autoimmune uveitis by regulating microglia phenotypes via the GPC4/TLR4/NF-κB signaling axis. Genes. Dis. 2022, 10, 2179–2193. [Google Scholar] [CrossRef] [PubMed]
- Hu, B.; Rodriguez, J.J.; Kakkerla Balaraju, A.; Gao, Y.; Nguyen, N.T.; Steen, H.; Suhaib, S.; Chen, S.; Lin, F. Glypican 4 mediates Wnt transport between germ layers via signaling filopodia. J. Cell Biol. 2021, 220, e202009082. [Google Scholar] [CrossRef] [PubMed]
- Shi, W.; Filmus, J. Glypican-6 and Glypican-4 stimulate embryonic stomach growth by regulating Hedgehog and noncanonical Wnt signaling. Dev. Dyn. 2022, 251, 2015–2028. [Google Scholar] [CrossRef]
- Maddala, R.; Eldawy, C.; Bachman, W.; Soderblom, E.J.; Rao, P.V. Glypican-4 regulated actin cytoskeletal reorganization in glucocorticoid treated trabecular meshwork cells and involvement of Wnt/PCP signaling. J. Cell. Physiol. 2023, 238, 631–646. [Google Scholar] [CrossRef] [PubMed]
- Hu, B.; Gao, Y.; Davies, L.; Woo, S.; Topczewski, J.; Jessen, J.R.; Lin, F. Glypican 4 and Mmp14 interact in regulating the migration of anterior endodermal cells by limiting extracellular matrix deposition. Development 2018, 145, dev163303. [Google Scholar] [CrossRef] [PubMed]
- Hagihara, K.; Watanabe, K.; Chun, J.; Yamaguchi, Y. Glypican-4 is an FGF2-binding heparan sulfate proteoglycan expressed in neural precursor cells. Dev. Dyn. 2000, 219, 353–567. [Google Scholar] [CrossRef] [PubMed]
- Galli, A.; Roure, A.; Zeller, R.; Dono, R. Glypican 4 modulates FGF signalling and regulates dorsoventral forebrain patterning in Xenopus embryos. Development 2003, 130, 4919–4929. [Google Scholar] [CrossRef] [PubMed]
- Ma, K.G.; Hu, H.B.; Zhou, J.S.; Ji, C.; Yan, Q.S.; Peng, S.M.; Ren, L.D.; Yang, B.N.; Xiao, X.L.; Ma, Y.B.; et al. Neuronal Glypican 4 promotes mossy fiber sprouting through the mTOR pathway after pilocarpine-induced status epilepticus in mice. Exp. Neurol. 2022, 347, 113918. [Google Scholar] [CrossRef] [PubMed]
- Ko, J.S.; Pramanik, G.; Um, J.W.; Shim, J.S.; Lee, D.; Kim, K.H.; Chung, G.Y.; Condomitti, G.; Kim, H.M.; Kim, H.; et al. PTPσ functions as a presynaptic receptor for the glypican-4/LRRTM4 complex and is essential for excitatory synaptic transmission. Proc. Natl. Acad. Sci. USA 2015, 112, 1874–1879. [Google Scholar] [CrossRef] [PubMed]
- Kamimura, K.; Maeda, N. Glypicans and Heparan Sulfate in Synaptic Development, Neural Plasticity, and Neurological Disorders. Front. Neural Circuits 2021, 15, 595596. [Google Scholar] [CrossRef] [PubMed]
- Hashemi, M.; Etemad, S.; Rezaei, S.; Ziaolhagh, S.; Rajabi, R.; Rahmanian, P.; Abdi, S.; Koohpar, Z.K.; Rafiei, R.; Raei, B.; et al. Progress in targeting PTEN/PI3K/Akt axis in glioblastoma therapy: Revisiting molecular interactions. Biomed. Pharmacother. 2023, 158, 114204. [Google Scholar] [CrossRef] [PubMed]
- Sirhan, Z.; Alojair, R.; Thyagarajan, A.; Sahu, R.P. Therapeutic Implications of PTEN in Non-Small Cell Lung Cancer. Pharmaceutics 2023, 15, 2090. [Google Scholar] [CrossRef] [PubMed]
- Aiello, N.M.; Stanger, B.Z. Echoes of the embryo: Using the developmental biology toolkit to study cancer. Dis. Model. Mech. 2016, 9, 105–114. [Google Scholar] [CrossRef] [PubMed]
- Chandel, S.S.; Mishra, A.; Dubey, G.; Singh, R.P.; Singh, M.; Agarwal, M.; Chawra, H.S.; Kukreti, N. Unravelling the role of long non-coding RNAs in modulating the Hedgehog pathway in cancer. Pathol. Res. Pract. 2024, 254, 155156. [Google Scholar] [CrossRef] [PubMed]
- Iwadate, Y. Epithelial-mesenchymal transition in glioblastoma progression. Oncol. Lett. 2016, 11, 1615–1620. [Google Scholar] [CrossRef] [PubMed]
- Grillo, P.K.; Győrffy, B.; Götte, M. Prognostic impact of the glypican family of heparan sulfate proteoglycans on the survival of breast cancer patients. J. Cancer Res. Clin. Oncol. 2021, 147, 1937–1955. [Google Scholar] [CrossRef] [PubMed]
- Farrugia, B.L.; Melrose, J. The Glycosaminoglycan Side Chains and Modular Core Proteins of Heparan Sulphate Proteoglycans and the Varied Ways They Provide Tissue Protection by Regulating Physiological Processes and Cellular Behaviour. Int. J. Mol. Sci. 2023, 24, 14101. [Google Scholar] [CrossRef] [PubMed]
- Song, K. Current Development Status of Cytokines for Cancer Immunotherapy. Biomol. Ther. 2024, 32, 13–24. [Google Scholar] [CrossRef] [PubMed]
- Allgöwer, C.; Kretz, A.L.; von Karstedt, S.; Wittau, M.; Henne-Bruns, D.; Lemke, J. Friend or Foe: S100 Proteins in Cancer. Cancers 2020, 12, 2037. [Google Scholar] [CrossRef] [PubMed]
- Yue, T.; Zheng, X.; Dou, Y.; Zheng, X.; Sun, R.; Tian, Z.; Wei, H. Interleukin 12 shows a better curative effect on lung cancer than paclitaxel and cisplatin doublet chemotherapy. BMC Cancer 2016, 16, 665. [Google Scholar] [CrossRef] [PubMed]
- Filmus, J. Glypicans, 35 years later. Proteoglycan Res. 2023, 1, e5. [Google Scholar] [CrossRef]
- Pellegrini, L.; Burke, D.; von Delft, F.; Mulloy, B.; Blundell, T.L. Crystal structure of fibroblast growth factor receptor ectodomain bound to ligand and heparin. Nature 2000, 407, 1029–1034. [Google Scholar] [CrossRef] [PubMed]
- Ding, K.; Lopez-Burks, M.; Sánchez-Duran, J.A.; Korc, M.; Lander, A.D. Growth factor-induced shedding of syndecan-1 confers glypican-1 dependence on mitogenic responses of cancer cells. J. Cell Biol. 2005, 171, 729–738. [Google Scholar] [CrossRef] [PubMed]
- Li, S.; Zhang, N.; Liu, S.; Zhang, H.; Liu, J.; Qi, Y.; Zhang, Q.; Lim, X. ITGA5 Is a Novel Oncogenic Biomarker and Correlates with Tumor Immune Microenvironment in Gliomas. Front. Oncol. 2022, 12, 844144. [Google Scholar] [CrossRef] [PubMed]
- Colaprico, A.; Silva, T.C.; Olsen, C.; Garofano, L.; Cava, C.; Garolini, D.; Sabedot, T.S.; Malta, T.M.; Pagnotta, S.M.; Castiglioni, I.; et al. TCGAbiolinks: An R/Bioconductor package for integrative analysis of TCGA data. Nucleic Acids Res. 2016, 44, e71. [Google Scholar] [CrossRef] [PubMed]
- Silva, T.C.; Colaprico, A.; Olsen, C.; D’Angelo, F.; Bontempi, G.; Ceccarelli, M.; Noushmehr, H. TCGA Workflow: Analyze cancer genomics and epigenomics data using Bioconductor packages. F1000Research 2016, 5, 1542. [Google Scholar] [CrossRef] [PubMed]
- Mounir, M.; Lucchetta, M.; Silva, T.C.; Olsen, C.; Bontempi, G.; Chen, X.; Noushmehr, H.; Colaprico, A.; Papaleo, E. New functionalities in the TCGAbiolinks package for the study and integration of cancer data from GDC and GTEx. PLoS Comput. Biol. 2019, 15, e1006701. [Google Scholar] [CrossRef] [PubMed]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2023; Available online: https://www.r-project.org/ (accessed on 6 December 2023).
- Therneau, T. A Package for Survival Analysis in R. R Package Version 3.5-7. 2023. Available online: https://CRAN.R-project.org/package=survival (accessed on 6 December 2023).
- Kassambara, A.; Kosinski, M.; Biecek, P. Survminer: Drawing Survival Curves Using ‘ggplot2’. R Package Version 0.4.8. 2020. Available online: https://CRAN.R-project.org/package=survminer (accessed on 6 December 2023).
- Love, M.I.; Huber, W.; Anders, S. Moderated estimation of fold change and dispersion for RNA-seq data with DESeq2. Genome Biol. 2014, 15, 550. [Google Scholar] [CrossRef] [PubMed]
- Krämer, A.; Green, J.; Pollard, J., Jr.; Tugendreich, S. Causal analysis approaches in Ingenuity Pathway Analysis. Bioinformatics 2014, 30, 523–530. [Google Scholar] [CrossRef] [PubMed]
- Chen, E.Y.; Tan, C.M.; Kou, Y.; Duan, Q.; Wang, Z.; Meirelles, G.V.; Clark, N.R.; Ma’ayan, A. Enrichr: Interactive and collaborative HTML5 gene list enrichment analysis tool. BMC Bioinform. 2013, 14, 128. [Google Scholar] [CrossRef] [PubMed]
- Persson, A.; Tykesson, E.; Westergren-Thorsson, G.; Malmström, A.; Ellervik, U.; Mani, K. Xyloside-primed Chondroitin Sulfate/Dermatan Sulfate from Breast Carcinoma Cells with a Defined Disaccharide Composition Has Cytotoxic Effects in vitro. J. Biol. Chem. 2016, 291, 14871–14882. [Google Scholar] [CrossRef]

| Ingenuity Canonical Pathways | −log (p-Value) | z-Score | Ratio | Gene Names | p-Value | Adj. p-Value |
|---|---|---|---|---|---|---|
| S100 Family Signaling Pathway | 2.62 | −2.83683 | 0.0272 | CACNA1C, CACNA1H, EDNRA, EDNRB, FGFR1, FZD1, IGHG1, LGR5, MMP13, MMP7, NTRK2, PLA2G2A, PTH1R, RYR2, S100A2, S100A8, S100A9, S1PR3, SMAD9, TGFB2, WNT6 | 0.00239 | 0.02515 |
| Neutrophil Extracellular Trap Signaling Pathway | 2.43 | 3.050851 | 0.0326 | COL10A1, COL11A1, COL12A1, COL1A1, COL21A1, COL25A1, COL26A1, COL2A1, COL6A3, COL8A1, COL8A2, IGHG1, PLA2G2A | 0.003715 | 0.03352 |
| Myelination Signaling Pathway | 2.24 | −1.50756 | 0.0336 | ARHGAP6, BMP5, FGFR1, FZD1, HES5, ITGB3, NTRK2, PDGFRA, SMAD9, SOX8, WNT6 | 0.005754 | 0.04962 |
| Synaptogenesis Signaling Pathway | 2.36 | −2.7136 | 0.0349 | ADCY2, CADM1, CDH11, CDH6, CPLX2, EPHA3, EPHA7, NTRK2, RELN, THBS1, THBS4 | 0.004365 | 0.03849 |
| RAR Activation | 3.49 | −1.5 | 0.0373 | ADCY2, ADH1B, COL10A1, COL1A1, CRABP1, DKK2, FABP5, FGF10, MMP13, PDE1C, PDE3A, PDE5A, PRDM16, RBP4, RHOV, TGFB2 | 0.000324 | 0.00502 |
| Sperm Motility | 2.51 | 0.0389 | CACNA1H, DDR2, EPHA3, FGFR1, NTRK2, PDE1C, PDGFRA, PLA2G2A, PRKG1, ROR1 | 0.00309 | 0.03074 | |
| Cardiac Hypertrophy Signaling (Enhanced) | 5.16 | −3.44124 | 0.0406 | ADCY2, CACNA1C, EDNRA, EDNRB, FGF10, FGFR1, FZD1, GHR, IL17RD, ITGA8, ITGA9, ITGB3, MYOCD, PDE1C, PDE3A, PDE5A, PLN, PRKG1, RYR2, TGFB2, TNFRSF11B, WNT6 | 0.000007 | 0.00022 |
| RHOGDI Signaling | 2.45 | 1.341641 | 0.0409 | ACTG2, ARHGAP6, CDH11, CDH6, ITGA8, ITGA9, ITGB3, MYH11, RHOV | 0.003548 | 0.03352 |
| Activin Inhibin Signaling Pathway | 2.49 | −1.66667 | 0.0415 | CCN2, COL10A1, COL1A1, COL2A1, IGHG1, MMP7, SMAD9, TGFB2, TNFRSF11B | 0.003236 | 0.03138 |
| Axonal Guidance Signaling | 5.59 | 0.0431 | ADAM33, BMP5, CXCL12, DPYSL5, EPHA3, EPHA7, FZD1, ITGA8, ITGA9, ITGB3, MMP13, MMP7, NTN1, NTN4, NTRK2, SDC2, SEMA3D, SEMA3E, SLIT2, SLIT3, UNC5A, WNT6 | 0.000003 | 0.0001 | |
| Gustation Pathway | 2.7 | −1 | 0.0446 | ABCC9, ADCY2, CACNA1C, CACNA1H, KCNJ8, KCNN2, LPL, PDE3A, SCN7A | 0.001995 | 0.02150 |
| Human Embryonic Stem Cell Pluripotency | 2.72 | −2.33333 | 0.0448 | BMP5, FGFR1, FZD1, NR0B1, NTRK2, PDGFRA, SMAD9, TGFB2, WNT6 | 0.001905 | 0.02112 |
| Hepatic Fibrosis Signaling Pathway | 5.15 | −2 | 0.0449 | CACNA1C, CCN2, COL10A1, COL1A1, COL2A1, EDNRA, FGFR1, FZD1, ITGA8, ITGA9, ITGB3, MMP13, MYLK3, PDGFRA, RHOV, TF, TGFB2, TNFRSF11B, WNT6 | 0.000007 | 0.00023 |
| Pathogen-Induced Cytokine Storm Signaling Pathway | 4.77 | −3.15296 | 0.0458 | COL10A1, COL11A1, COL12A1, COL1A1, COL21A1, COL25A1, COL26A1, COL2A1, COL6A3, COL8A1, COL8A2, CXCL12, CXCL5, CXCL6, RYR2, TGFB2, TNFRSF11B | 0.000017 | 0.00041 |
| Clathrin-mediated Endocytosis Signaling | 3.2 | 0.0481 | ACTG2, ALB, AMPH, APOA2, APOC3, FGF10, ITGB3, RBP4, S100A8, TF | 0.000631 | 0.00844 | |
| Acute Phase Response Signaling | 2.97 | −1 | 0.0486 | ALB, APOA2, APOH, C4A/C4B, CRABP1, LBP, RBP4, TF, TNFRSF11B | 0.001072 | 0.01299 |
| IL-12 Signaling and Production in Macrophages | 3.97 | −2.3094 | 0.0511 | ALB, APOA2, APOC3, COL10A1, COL1A1, COL2A1, DDR2, IGHG1, RBP4, S100A8, TGFB2, THBS1 | 0.000107 | 0.00198 |
| STAT3 Pathway | 2.57 | −2.44949 | 0.0519 | FGFR1, GHR, HGF, IL17RD, NTRK2, PDGFRA, TGFB2 | 0.002692 | 0.02748 |
| Tumor Microenvironment Pathway | 3.07 | −3 | 0.0503 | COL1A1, CXCL12, FGF10, HGF, ITGB3, MMP13, MMP7, TGFB2, TNC | 0.000851 | 0.01065 |
| PTEN Signaling | 2.93 | 2.236068 | 0.053 | FGFR1, GHR, ITGA8, ITGA9, ITGB3, NTRK2, PDGFRA, PREX2 | 0.001175 | 0.01340 |
| Semaphorin Neuronal Repulsive Signaling Pathway | 2.95 | 0.377964 | 0.0533 | DPYSL3, DPYSL5, ITGA8, ITGA9, ITGB3, PRKG1, SEMA3E, VCAN | 0.001122 | 0.01319 |
| Pulmonary Healing Signaling Pathway | 3.99 | −2.11058 | 0.0553 | CXCL12, FGF10, FGFR1, FZD1, MMP13, MMP7, SMAD9, TGFB2, THBS1, TNFRSF11B, WNT6 | 0.000102 | 0.00198 |
| Wound Healing Signaling Pathway | 4.95 | −2.13809 | 0.0556 | COL10A1, COL11A1, COL12A1, COL1A1, COL21A1, COL25A1, COL26A1, COL2A1, COL6A3, COL8A1, COL8A2, KRT16, TGFB2, TNFRSF11B | 0.000011 | 0.00031 |
| Role of Osteoblasts, Osteoclasts, and Chondrocytes in Rheumatoid Arthritis | 4.75 | 0.057 | BMP5, COL1A1, DKK2, FRZB, FZD1, ITGB3, MMP13, SFRP4, SFRP5, SMAD9, TNFRSF11B, WIF1, WNT6 | 0.000018 | 0.00041 | |
| WNT/β-catenin Signaling | 3.81 | 0.632456 | 0.0575 | DKK2, FRZB, FZD1, MMP7, SFRP4, SFRP5, SOX8, TGFB2, WIF1, WNT6 | 0.000155 | 0.00261 |
| DHCR24 Signaling Pathway | 3.2 | 2.12132 | 0.0584 | ALB, APOA2, APOC3, APOH, C4A/C4B, RBP4, TF, VTN | 0.000631 | 0.00844 |
| Cellular Effects of Sildenafil (Viagra) | 3.63 | 0.06 | ACTG2, ADCY2, CACNA1C, KCNN2, MYH11, PDE1C, PDE3A, PDE5A, PRKG1 | 0.000234 | 0.00379 | |
| Role of Osteoblasts in Rheumatoid Arthritis Signaling Pathway | 5.8 | −0.7746 | 0.0615 | COL1A1, CTSE, CXCL12, DKK2, FRZB, FZD1, MMP13, MMP7, SFRP4, SFRP5, SMAD9, TGFB2, TNFRSF11B, WIF1, WNT6 | 0.000002 | 0.0001 |
| Role of Osteoclasts in Rheumatoid Arthritis Signaling Pathway | 7.94 | −2.06474 | 0.0649 | ADAM33, COL10A1, COL11A1, COL12A1, COL1A1, COL21A1, COL25A1, COL26A1, COL2A1, COL6A3, COL8A1, COL8A2, FRZB, ITGB3, MMP13, MMP7, RHOV, SFRP4, SFRP5, TNFRSF11B | 0.00000001 | 0.0000015 |
| White Adipose Tissue Browning Pathway | 3.9 | −1.66667 | 0.0652 | ADCY2, CACNA1C, CACNA1H, FGFR1, FNDC5, PRDM16, PRKG1, RUNX1T1, VGF | 0.000125893 | 0.00222 |
| Caveolar-mediated Endocytosis Signaling | 2.43 | 0.0667 | ACTG2, ALB, ITGA8, ITGA9, ITGB3 | 0.003715352 | 0.03352 | |
| Osteoarthritis Pathway | 6.72 | −0.33333 | 0.0678 | COL10A1, COL2A1, DDR2, FGFR1, FRZB, FZD1, ITGA8, ITGA9, ITGB3, MMP13, PTH1R, RBP4, S100A8, S100A9, S1PR3, SMAD9 | 0.0000002 | 0.000009 |
| Microautophagy Signaling Pathway | 4.86 | 0.0688 | COL10A1, COL11A1, COL12A1, COL1A1, COL21A1, COL25A1, COL26A1, COL2A1, COL6A3, COL8A1, COL8A2 | 0.000014 | 0.00036 | |
| Pulmonary Fibrosis Idiopathic Signaling Pathway | 9.75 | −4.26401 | 0.0706 | ACTG2, CCN2, COL10A1, COL11A1, COL12A1, COL1A1, COL21A1, COL25A1, COL26A1, COL2A1, COL6A3, COL8A1, COL8A2, CXCL12, EDNRA, FGFR1, FZD1, MMP13, MMP7, PDGFRA, TGFB2, THBS1, WNT6 | 0.0000000002 | 0.00000003 |
| Maturity Onset Diabetes of Young (MODY) Signaling | 3.12 | 0.0759 | ABCC9, APOA2, APOC3, APOH, CACNA1C, KCNJ8 | 0.000759 | 0.00981 | |
| FXR/RXR Activation | 5.01 | 0.0794 | ALB, APOA2, APOC3, APOH, C4A/C4B, FABP6, LPL, RBP4, TF, VTN | 0.00001 | 0.00029 | |
| Netrin Signaling | 3.33 | −0.8165 | 0.0833 | CACNA1C, CACNA1H, NTN1, PRKG1, RYR2, UNC5A | 0.000467735 | 0.00687 |
| Dilated Cardiomyopathy Signaling Pathway | 6.78 | −1.26491 | 0.0867 | ABCC9, ACTG2, ADCY2, CACNA1C, CACNA1H, CNN1, DES, MYH11, PDE3A, PLN, RYR2, SGCD, TNNC1 | 0.0000002 | 0.000009 |
| GP6 Signaling Pathway | 6.72 | −2.88675 | 0.0945 | COL10A1, COL11A1, COL12A1, COL1A1, COL21A1, COL25A1, COL26A1, COL2A1, COL6A3, COL8A1, COL8A2, ITGB3 | 0.0000002 | 0.000009 |
| LXR/RXR Activation | 6.87 | 1.507557 | 0.0976 | ALB, APOA2, APOC3, APOH, C4A/C4B, LBP, LPL, RBP4, S100A8, TF, TNFRSF11B, VTN | 0.0000001 | 0.000009 |
| Atherosclerosis Signaling | 7.4 | 0.0977 | ALB, ALOX12B, APOA2, APOC3, COL10A1, COL1A1, COL2A1, CXCL12, LPL, MMP13, PLA2G2A, RBP4, S100A8 | 0.00000004 | 0.000004 | |
| Hepatic Fibrosis/Hepatic Stellate Cell Activation | 13.5 | 0.113 | CCN2, COL10A1, COL11A1, COL12A1, COL1A1, COL21A1, COL25A1, COL26A1, COL2A1, COL6A3, COL8A1, COL8A2, EDNRA, EDNRB, FGFR1, HGF, LBP, MMP13, MYH11, PDGFRA, TGFB2, TNFRSF11B | 0.00000000000003 | 0.00000000001 | |
| Intrinsic Prothrombin Activation Pathway | 4.66 | −0.8165 | 0.143 | COL10A1, COL1A1, COL2A1, F12, F5, KLK10 | 0.00002 | 0.00047 |
| Apelin Liver Signaling Pathway | 3.32 | −2 | 0.148 | COL10A1, COL1A1, COL2A1, EDN3 | 0.000478 | 0.00688 |
| Role of IL-17A in Psoriasis | 4.5 | 0 | 0.286 | CXCL5, CXCL6, S100A8, S100A9 | 0.00003 | 0.00065 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chérouvrier Hansson, V.; Cheng, F.; Georgolopoulos, G.; Mani, K. Dichotomous Effects of Glypican-4 on Cancer Progression and Its Crosstalk with Oncogenes. Int. J. Mol. Sci. 2024, 25, 3945. https://doi.org/10.3390/ijms25073945
Chérouvrier Hansson V, Cheng F, Georgolopoulos G, Mani K. Dichotomous Effects of Glypican-4 on Cancer Progression and Its Crosstalk with Oncogenes. International Journal of Molecular Sciences. 2024; 25(7):3945. https://doi.org/10.3390/ijms25073945
Chicago/Turabian StyleChérouvrier Hansson, Victor, Fang Cheng, Grigorios Georgolopoulos, and Katrin Mani. 2024. "Dichotomous Effects of Glypican-4 on Cancer Progression and Its Crosstalk with Oncogenes" International Journal of Molecular Sciences 25, no. 7: 3945. https://doi.org/10.3390/ijms25073945
APA StyleChérouvrier Hansson, V., Cheng, F., Georgolopoulos, G., & Mani, K. (2024). Dichotomous Effects of Glypican-4 on Cancer Progression and Its Crosstalk with Oncogenes. International Journal of Molecular Sciences, 25(7), 3945. https://doi.org/10.3390/ijms25073945





