Oxidative Stress Induced by Cortisol in Human Platelets
Abstract
1. Introduction
2. Results
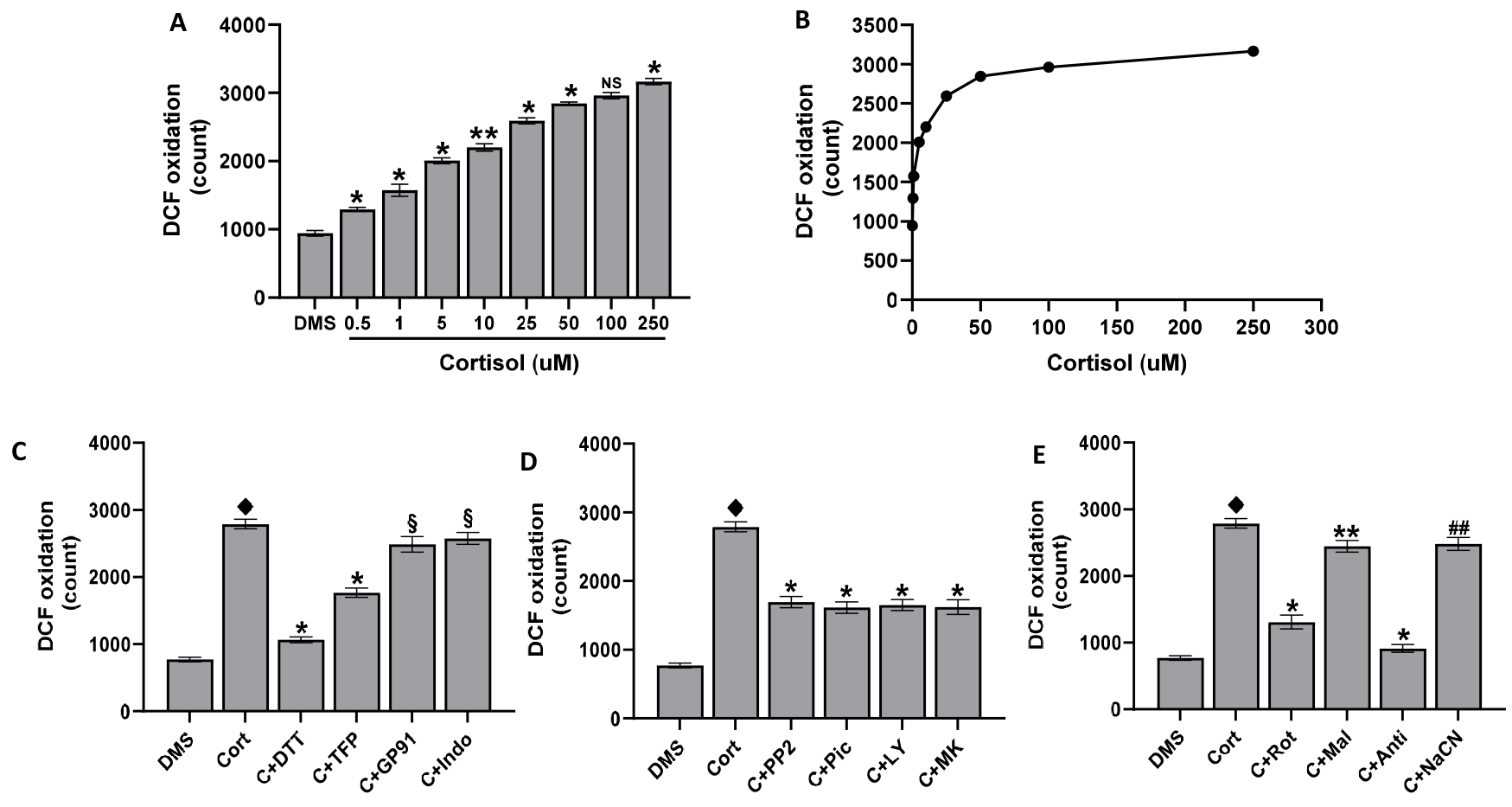
2.1. ROS Production in Platelets Treated with Cortisol
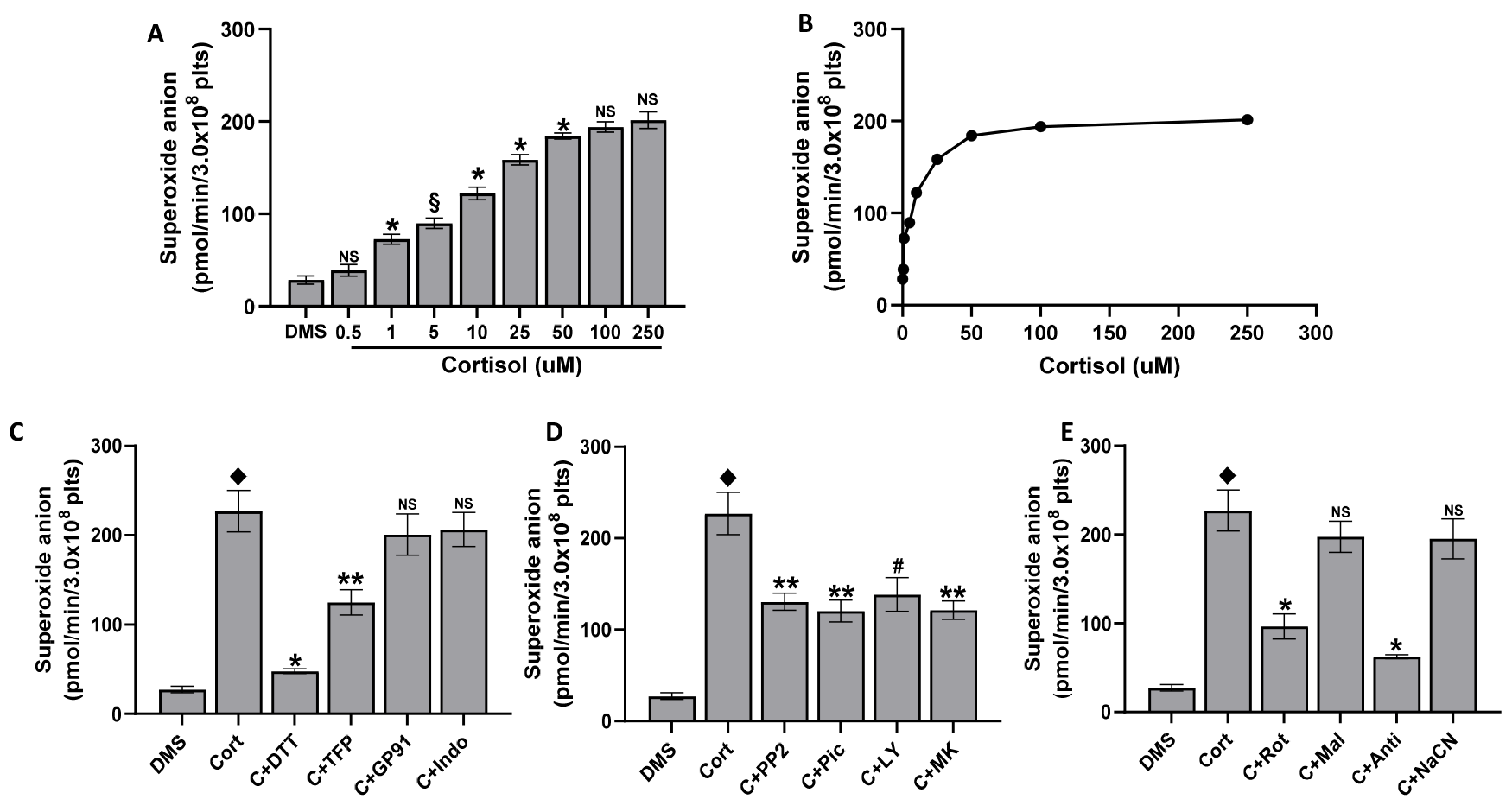
2.2. Superoxide Anion Formation in Platelets Treated with Cortisol
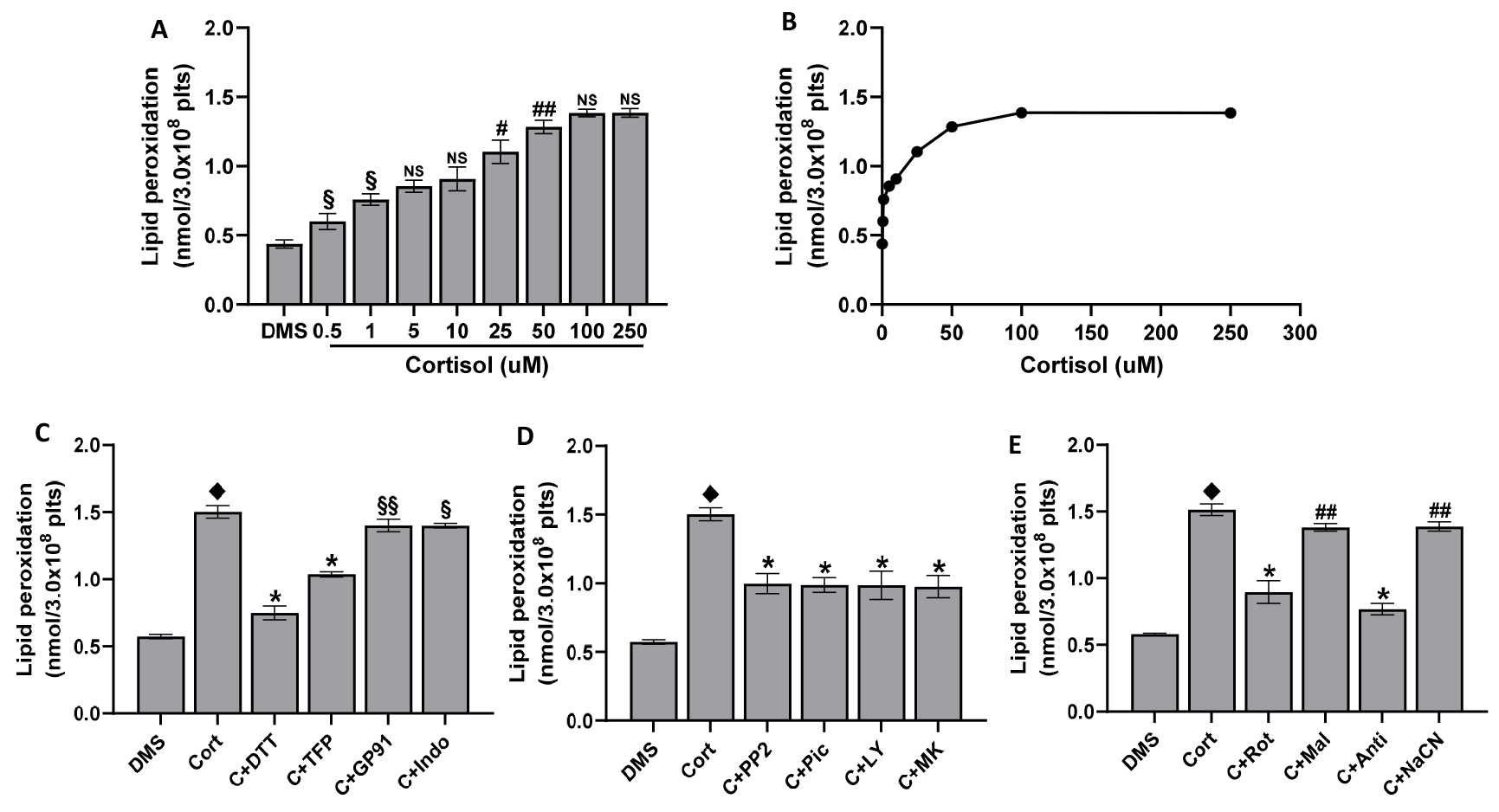
2.3. Lipid Peroxidation Induced by Cortisol
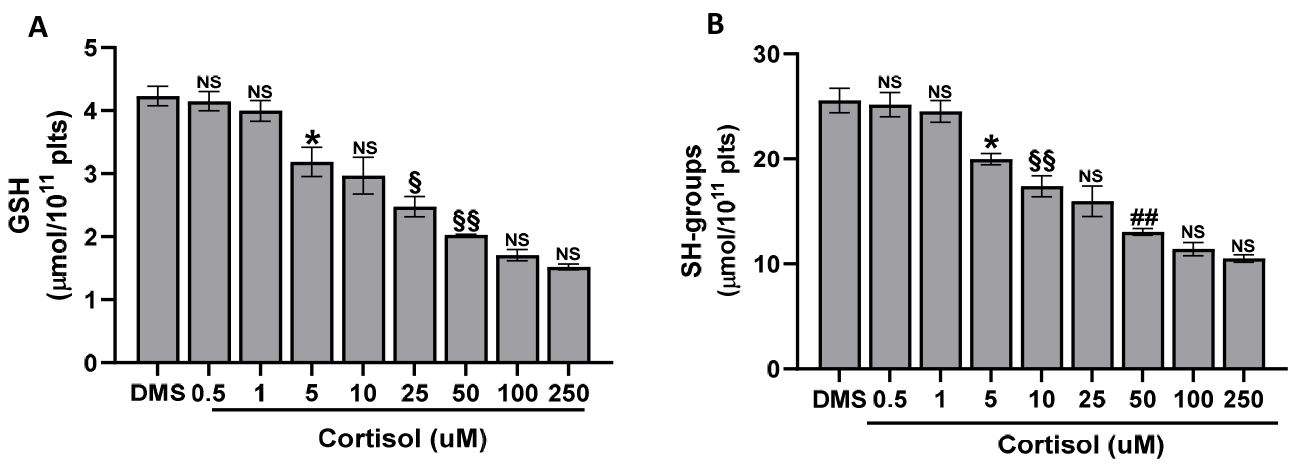
2.4. The Cortisol Effect on GSH and SH-Groups
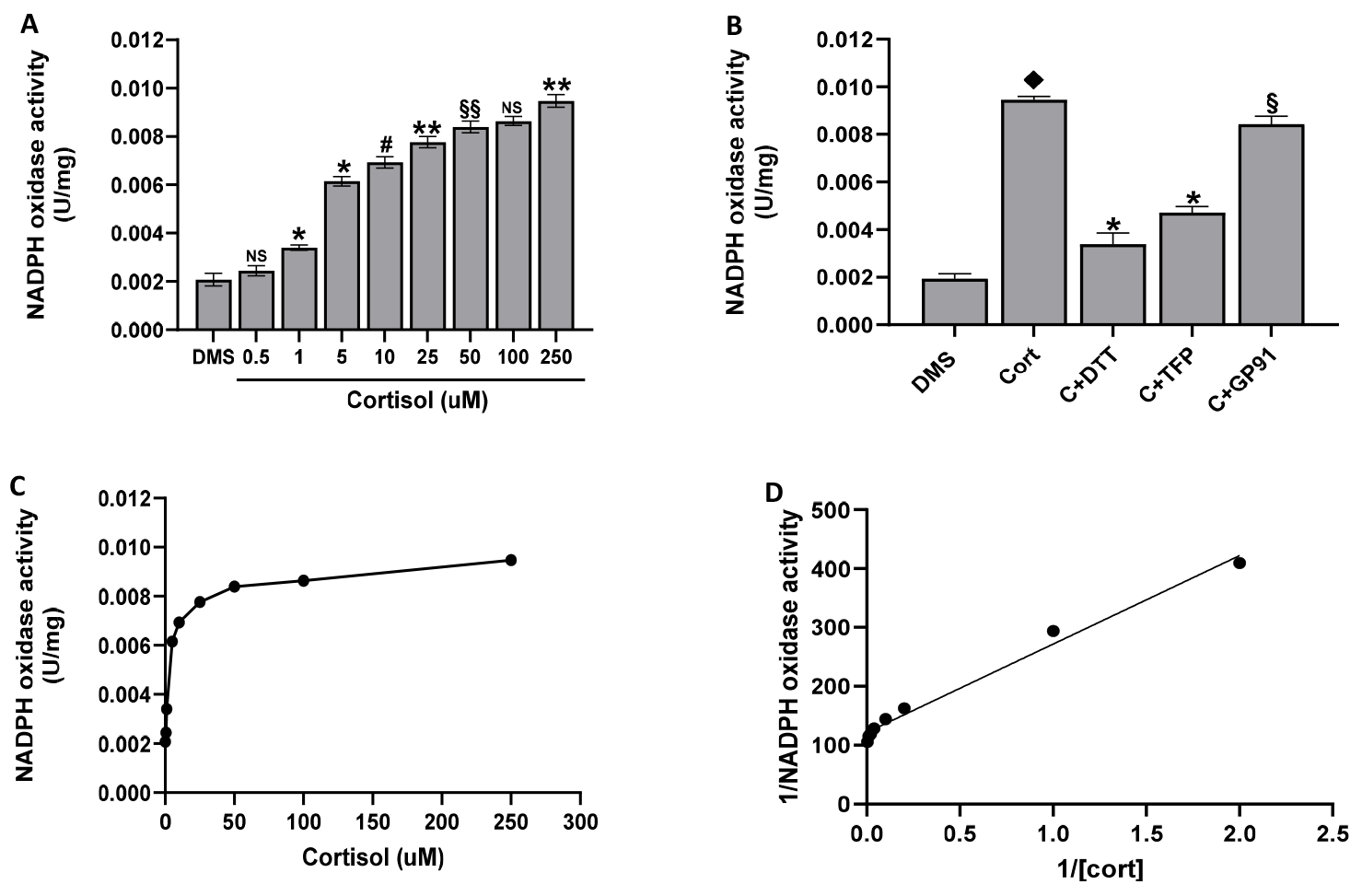
2.5. The Cortisol Effect on NADPH Oxidase Activity
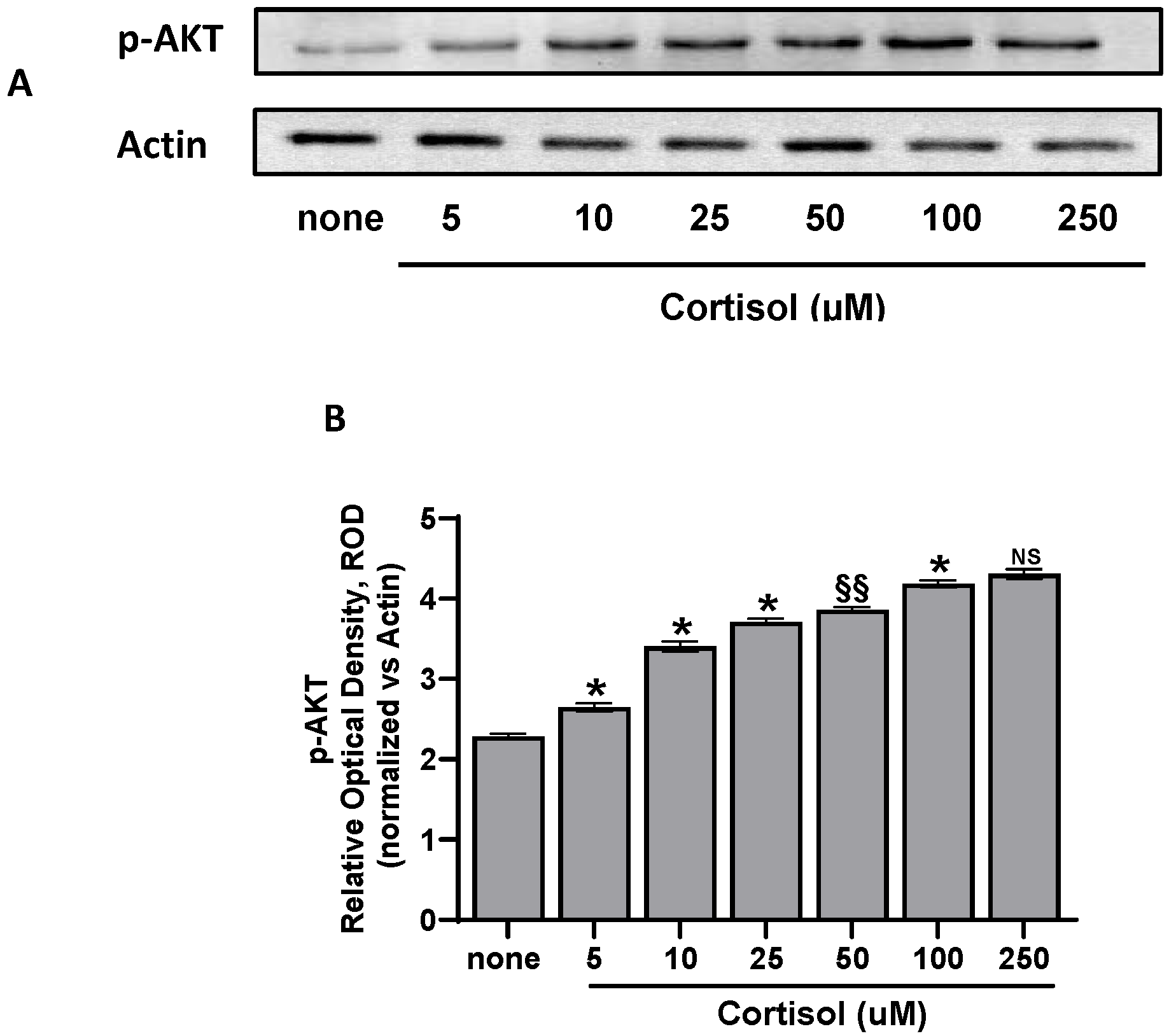
2.6. Western Blotting
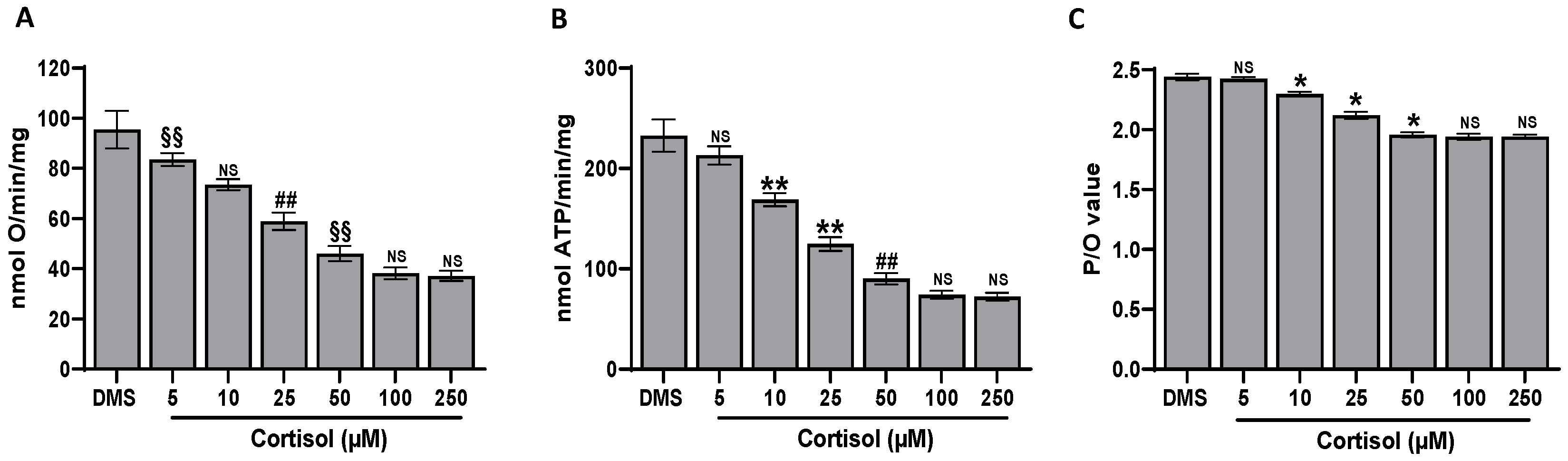
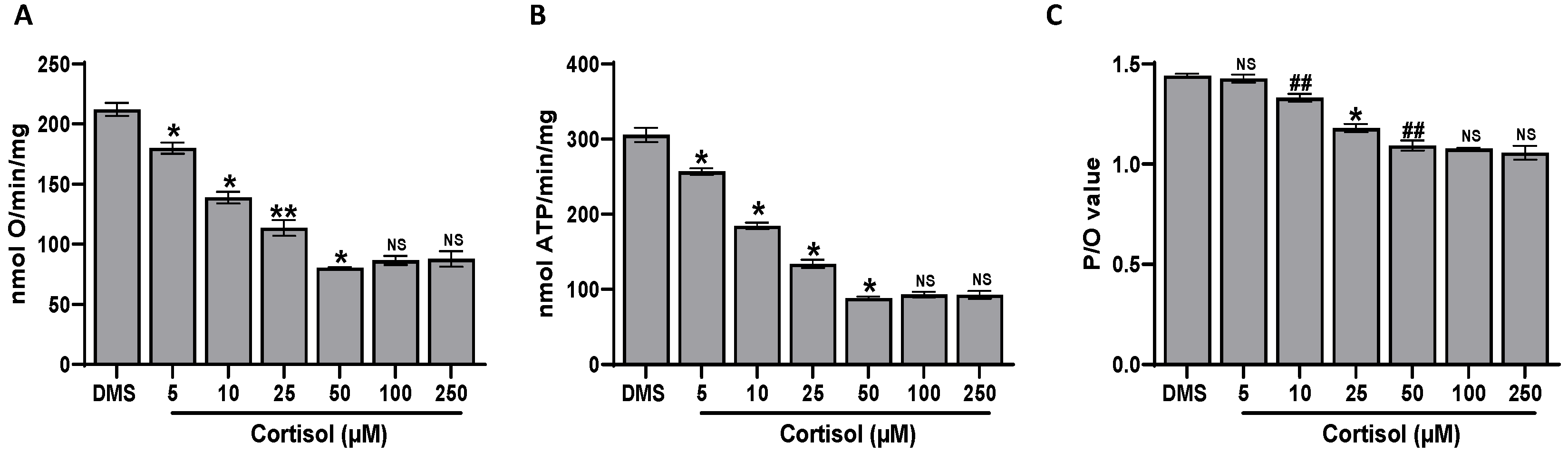
2.7. Effect of Cortisol on Platelet Aerobic Metabolism
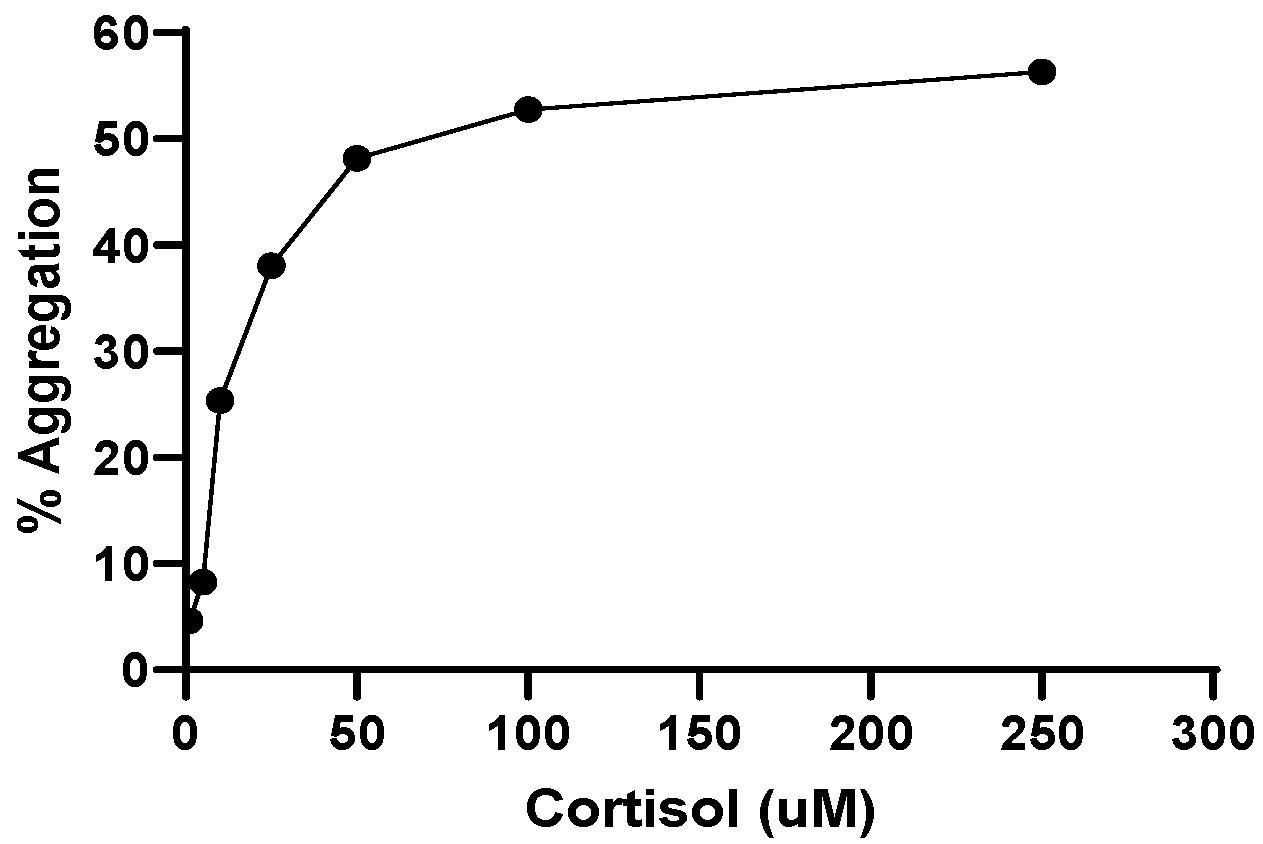
2.8. Effect of Cortisol on Platelet Aggregation
3. Discussion
4. Material and Methods
4.1. Materials
4.2. Blood Collection and Preparative Procedures
4.3. ROS Assay
4.4. Superoxide Anion Assay
4.5. Lipid Peroxidation Measurement
4.6. GSH and Membrane SH-Group Assay
4.7. NADPH Oxidase Activity Assay
4.8. Western Blotting (WB) Analysis
4.9. Oximetric Analysis
4.10. Fo-F1 ATP Synthase Activity Assay
4.11. P/O Ratio Calculation
4.12. Aggregation
4.13. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Oray, M.; Abu Samra, K.; Ebrahimiadib, N.; Meese, H.; Foster, C.S. Long-Term Side Effects of Glucocorticoids. Expert Opin. Drug Saf. 2016, 15, 457–465. [Google Scholar] [CrossRef] [PubMed]
- Światkowska-Stodulska, R.; Sworczak, K. Disorders of Hemostasis in Overt and Subclinical Hypercortisolism. Exp. Clin. Endocrinol. Diabetes 2013, 121, 588–594. [Google Scholar] [CrossRef] [PubMed]
- Świątkowska-Stodulska, R.; Mital, A.; Wiśniewski, P.; Babińska, A.; Skibowska-Bielińska, A.; Sworczak, K. Assessment of Platelet Function in Endogenous Hypercortisolism. Endokrynol. Pol. 2015, 66, 207–213. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Światkowska-Stodulska, R.; Babińska, A.; Sworczak, K. Hypercortisolism and Hemostasis. Pol. Merkur. Lek. 2009, 26, 142–144. [Google Scholar]
- Mandadi, S.; Pulluru, H.; Annie, F. Comparative Outcomes of Combined Corticosteroid and Remdesivir Therapy with Corticosteroid Monotherapy in Ventilated COVID-19 Patients. PLoS ONE 2022, 17, e0264301. [Google Scholar] [CrossRef] [PubMed]
- van Paassen, J.; Vos, J.S.; Hoekstra, E.M.; Neumann, K.M.I.; Boot, P.C.; Arbous, S.M. Corticosteroid Use in COVID-19 Patients: A Systematic Review and Meta-Analysis on Clinical Outcomes. Crit. Care 2020, 24, 696. [Google Scholar] [CrossRef] [PubMed]
- Angelier, F.; Wingfield, J.C. Importance of the Glucocorticoid Stress Response in a Changing World: Theory, Hypotheses and Perspectives. Gen. Comp. Endocrinol. 2013, 190, 118–128. [Google Scholar] [CrossRef] [PubMed]
- Van Zaane, B.; Nur, E.; Squizzato, A.; Dekkers, O.M.; Twickler, M.B.; Fliers, E.; Gerdes, V.E.A.; Büller, H.R.; Brandjes, D.P.M. Hypercoagulable State in Cushing’s Syndrome: A Systematic Review. J. Clin. Endocrinol. Metab. 2009, 94, 2743–2750. [Google Scholar] [CrossRef] [PubMed]
- Stuijver, D.J.F.; Van Zaane, B.; Feelders, R.A.; Debeij, J.; Cannegieter, S.C.; Hermus, A.R.; Van Den Berg, G.; Pereira, A.M.; De Herder, W.W.; Wagenmakers, M.A.E.M.; et al. Incidence of Venous Thromboembolism in Patients with Cushing’s Syndrome: A Multicenter Cohort Study. J. Clin. Endocrinol. Metab. 2011, 96, 3525–3532. [Google Scholar] [CrossRef] [PubMed]
- Whitworth, J.A.; Williamson, P.M.; Mangos, G.; Kelly, J.J. Cardiovascular Consequences of Cortisol Excess. Vasc. Health Risk Manag. 2005, 1, 291–299. [Google Scholar] [CrossRef]
- Bertagna, X.; Guignat, L.; Groussin, L.; Bertherat, J. Cushing’s Disease. Best Pract. Res. Clin. Endocrinol. Metab. 2009, 23, 607–623. [Google Scholar] [CrossRef] [PubMed]
- Graversen, D.; Vestergaard, P.; Stochholm, K.; Gravholt, C.H.; Jørgensen, J.O.L. Mortality in Cushing’s Syndrome: A Systematic Review and Meta-Analysis. Eur. J. Intern. Med. 2012, 23, 278–282. [Google Scholar] [CrossRef] [PubMed]
- Moraes, L.A.; Paul-Clark, M.J.; Rickman, A.; Flower, R.J.; Goulding, N.J.; Perretti, M. Ligand-Specific Glucocorticoid Receptor Activation in Human Platelets. Blood 2005, 106, 4167–4175. [Google Scholar] [CrossRef] [PubMed]
- Unsworth, A.J.; Flora, G.D.; Gibbins, J.M. Non-Genomic Effects of Nuclear Receptors: Insights from the Anucleate Platelet. Cardiovasc. Res. 2018, 114, 645–655. [Google Scholar] [CrossRef] [PubMed]
- Casella, S.; Giudice, E.; Giannetto, C.; Marafioti, S.; Piccione, G. Effects of Hydrocortisone and Aminophylline on the Aggregation of Equine Platelets in Vitro. J. Vet. Sci. 2011, 12, 215–219. [Google Scholar] [CrossRef] [PubMed]
- Van Giezen, J.J.J.; Brakkee, J.G.P.; Dreteler, G.H.; Bouma, B.N.; Jansen, J.W.C.M. Dexamethasone Affects Platelet Aggregation and Fibrinolytic Activity in Rats at Different Doses Which Is Reflected by Their Effect on Arterial Thrombosis. Blood Coagul. Fibrinolysis 1994, 5, 249–255. [Google Scholar] [CrossRef] [PubMed]
- Glass, F.L.; Lippton, H.L. Kadovitz Effects of Methylprednisolone and Hydrocortisone on Aggregation of Rabbit Platelets Induced by Arachidonic Acid and Other Aggregating Substances. Thromb. Haemost. 1981, 46, 676–679. [Google Scholar] [PubMed]
- Casonato, A.; Pontara, E.; Boscaro, M.; Sonino, N.; Sartorello, F.; Ferasin, S.; Girolami, A. Abnormalities of von Willebrand Factor Are Also Part of the Prothrombotic State of Cushing’s Syndrome. Blood Coagul. Fibrinolysis 1999, 10, 145–151. [Google Scholar] [CrossRef] [PubMed]
- Karolczak, K.; Konieczna, L.; Soltysik, B.; Kostka, T.; Witas, P.J.; Kostanek, J.; Baczek, T.; Watala, C. Plasma Concentration of Cortisol Negatively Associates with Platelet Reactivity in Older Subjects. Int. J. Mol. Sci. 2022, 24, 717. [Google Scholar] [CrossRef] [PubMed]
- Larosa, V.; Remacle, C. Insights into the Respiratory Chain and Oxidative Stress. Biosci. Rep. 2018, 38, BSR20171492. [Google Scholar] [CrossRef] [PubMed]
- Panday, A.; Sahoo, M.K.; Osorio, D.; Batra, S. NADPH Oxidases: An Overview from Structure to Innate Immunity-Associated Pathologies. Cell. Mol. Immunol. 2015, 12, 5–23. [Google Scholar] [CrossRef] [PubMed]
- Wiseman, H.; Halliwell, B. Damage to DNA by Reactive Oxygen and Nitrogen Species: Role in Inflammatory Disease and Progression to Cancer. Biochem. J. 1996, 313, 17–29. [Google Scholar] [CrossRef] [PubMed]
- Eisen, J.A.; Hanawalt, P.C. A Phylogenomic Study of DNA Repair Genes, Proteins, and Processes. Mutat. Res.-DNA Repair 1999, 435, 171–213. [Google Scholar] [CrossRef] [PubMed]
- Olinski, R.; Gackowski, D.; Foksinski, M.; Rozalski, R.; Roszkowski, K.; Jaruga, P. Oxidative DNA Damage: Assessment of the Role in Carcinogenesis, Atherosclerosis, and Acquired Immunodeficiency Syndrome. Free Radic. Biol. Med. 2002, 33, 192–200. [Google Scholar] [CrossRef] [PubMed]
- Roos, W.P.; Kaina, B. DNA Damage-Induced Cell Death by Apoptosis. Trends Mol. Med. 2006, 12, 440–450. [Google Scholar] [CrossRef] [PubMed]
- Holmström, K.M.; Finkel, T. Cellular Mechanisms and Physiological Consequences of Redox-Dependent Signalling. Nat. Rev. Mol. Cell Biol. 2014, 15, 411–421. [Google Scholar] [CrossRef] [PubMed]
- Finkel, T. Signal Transduction by Reactive Oxygen Species. J. Cell Biol. 2011, 194, 7–15. [Google Scholar] [CrossRef] [PubMed]
- Hansson, G.K.; Libby, P.; Tabas, I. Inflammation and Plaque Vulnerability. J. Intern. Med. 2015, 278, 483–493. [Google Scholar] [CrossRef] [PubMed]
- Förstermann, U.; Xia, N.; Li, H. Roles of Vascular Oxidative Stress and Nitric Oxide in the Pathogenesis of Atherosclerosis. Circ. Res. 2017, 120, 713–735. [Google Scholar] [CrossRef] [PubMed]
- Maritim, A.C.; Sanders, R.A.; Watkins, J.B. Diabetes, Oxidative Stress, and Antioxidants: A Review. J. Biochem. Mol. Toxicol. 2003, 17, 24–38. [Google Scholar] [CrossRef]
- Chen, X.; Guo, C.; Kong, J. Oxidative Stress in Neurodegenerative Diseases. Neural Regen. Res. 2012, 7, 376–385. [Google Scholar] [CrossRef] [PubMed]
- Haigis, M.C.; Yankner, B.A. The Aging Stress Response. Mol. Cell 2010, 40, 333–344. [Google Scholar] [CrossRef] [PubMed]
- Bae, Y.S.; Oh, H.; Rhee, S.G.; Yoo, Y. Do Regulation of Reactive Oxygen Species Generation in Cell Signaling. Mol. Cells 2011, 32, 491–509. [Google Scholar] [CrossRef] [PubMed]
- Jakubczyk, K.; Dec, K.; Kałduńska, J.; Kawczuga, D.; Kochman, J.; Janda, K. Reactive Oxygen Species—Sources, Functions, Oxidative Damage. Pol. Merkur. Lek. 2020, 48, 124–127. [Google Scholar]
- Sies, H.; Jones, D.P. Oxidative Stress: Introduction. In Oxidative Stress: Oxidant and Antioxidants; Academic Press: San Diego, CA, USA, 1991; pp. 15–22. [Google Scholar]
- Sies, H.; Jones, D.P. Reactive Oxygen Species (ROS) as Pleiotropic Physiological Signalling Agents. Nat. Rev. Mol. Cell Biol. 2020, 21, 363–383. [Google Scholar] [CrossRef] [PubMed]
- Schieber, M.; Chandel, N.S. ROS Function in Redox Signaling and Oxidative Stress. Curr. Biol. 2014, 24, R453–R462. [Google Scholar] [CrossRef] [PubMed]
- Yana, M.H.; Wang, X.; Zhu, X. Mitochondrial Defects and Oxidative Stress in Alzheimer Disease and Parkinson Disease. Free Radic. Biol. Med. 2013, 62, 90–101. [Google Scholar] [CrossRef] [PubMed]
- Lee, R.; Margaritis, M.; Channon, M.K.; Antoniades, C. Evaluating Oxidative Stress in Human Cardiovascular Disease: Methodological Aspects and Considerations. Curr. Med. Chem. 2012, 19, 2504–2520. [Google Scholar] [CrossRef]
- Morrow, J.D. Quantification of Isoprostanes as Indices of Oxidant Stress and the Risk of Atherosclerosis in Humans. Arterioscler. Thromb. Vasc. Biol. 2005, 25, 279–286. [Google Scholar] [CrossRef] [PubMed]
- Karamouzis, I.; Berardelli, R.; D’Angelo, V.; Fussotto, B.; Zichi, C.; Giordano, R.; Settanni, F.; Maccario, M.; Ghigo, E.; Arvat, E. Enhanced Oxidative Stress and Platelet Activation in Patients with Cushing’s Syndrome. Clin. Endocrinol. 2015, 82, 517–524. [Google Scholar] [CrossRef] [PubMed]
- Brown, D.I.; Griendling, K.K. Regulation of Signal Transduction by Reactive Oxygen Species in the Cardiovascular System. Circ. Res. 2015, 116, 531–549. [Google Scholar] [CrossRef] [PubMed]
- Leoncini, G.; Maresca, M.; Colao, C. Oxidative Metabolism of Human Platelets. Biochem. Int. 1991, 25, 647–655. [Google Scholar] [PubMed]
- Maresca, M.; Colao, C.; Leoncini, G. Generation of Hydrogen Peroxide in Resting and Activated Platelets. Cell Biochem. Funct. 1992, 10, 79–85. [Google Scholar] [CrossRef] [PubMed]
- Praticò, D.; Iuliano, L.; Pulcinelli, F.M.; Bonavita, M.S.; Gazzaniga, P.P.; Violi, F. Hydrogen Peroxide Triggers Activation of Human Platelets Selectively Exposed to Nonaggregating Concentrations of Arachidonic Acid and Collagen. J. Lab. Clin. Med. 1992, 119, 364–370. [Google Scholar] [PubMed]
- Leo, R.; Praticò, D.; Iuliano, L.; Pulcinelli, F.M.; Ghiselli, A.; Pignatelli, P.; Colavita, A.R.; FitzGerald, G.A.; Violi, F. Platelet Activation by Superoxide Anion and Hydroxyl Radicals Intrinsically Generated by Platelets That Had Undergone Anoxia and Then Reoxygenated. Circulation 1997, 95, 885–891. [Google Scholar] [CrossRef] [PubMed]
- Krötz, F.; Sohn, H.Y.; Gloe, T.; Zahler, S.; Riexinger, T.; Schiele, T.M.; Becker, B.F.; Theisen, K.; Klauss, V.; Pohl, U. NAD(P)H Oxidase-Dependent Platelet Superoxide Anion Release Increases Platelet Recruitment. Blood 2002, 100, 917–924. [Google Scholar] [CrossRef] [PubMed]
- Dayal, S.; Wilson, K.M.; Motto, D.G.; Miller, F.J.; Chauhan, A.K.; Lentz, S.R. Hydrogen Peroxide Promotes Aging-Related Platelet Hyperactivation and Thrombosis. Circulation 2013, 127, 1308–1316. [Google Scholar] [CrossRef] [PubMed]
- Gianni, D.; Taulet, N.; Zhang, H.; DerMardirossian, C.; Kister, J.; Martinez, L.; Roush, W.R.; Brown, S.J.; Bokoch, G.M.; Rosen, H. A Novel and Specific NADPH Oxidase-1 (Nox1) Small-Molecule Inhibitor Blocks the Formation of Functional Invadopodia in Human Colon Cancer Cells. ACS Chem. Biol. 2010, 5, 981–993. [Google Scholar] [CrossRef] [PubMed]
- Cangemi, R.; Pignatelli, P.; Carnevale, R.; Bartimoccia, S.; Nocella, C.; Falcone, M.; Taliani, G.; Violi, F.; Battaglia, S.; Bertazzoni, G.; et al. Low-Grade Endotoxemia, Gut Permeability and Platelet Activation in Community-Acquired Pneumonia. J. Infect. 2016, 73, 107–114. [Google Scholar] [CrossRef] [PubMed]
- Ravera, S.; Signorello, M.G.; Bartolucci, M.; Ferrando, S.; Manni, L.; Caicci, F.; Calzia, D.; Panfoli, I.; Morelli, A.; Leoncini, G. Extramitochondrial Energy Production in Platelets. Biol. Cell 2018, 110, 97–108. [Google Scholar] [CrossRef]
- Rosenfeld, B.A.; Faraday, N.; Campbell, D.; Dise, K.; Bell, W.; Goldschmidt, P. Hemostatic Effects of Stress Hormone Infusion. Anesthesiology 1994, 81, 1116–1126. [Google Scholar] [CrossRef]
- Jilma, B.; Cvitko, T.; Winter-Fabry, A.; Petroczi, K.; Quehenberger, P.; Blann, A.D. High Dose Dexamethasone Increases Circulating P-Selectin and von Willebrand Factor Levels in Healthy Men. Thromb. Haemost. 2005, 94, 797–801. [Google Scholar] [CrossRef]
- Liverani, E.; Banerjee, S.; Roberts, W.; Naseem, K.M.; Perretti, M. Prednisolone Exerts Exquisite Inhibitory Properties on Platelet Functions. Biochem. Pharmacol. 2012, 83, 1364–1373. [Google Scholar] [CrossRef] [PubMed]
- Delaney, M.K.; Kim, K.; Estevez, B.; Xu, Z.; Stojanovic-Terpo, A.; Shen, B.; Ushio-Fukai, M.; Cho, J.; Du, X. Differential Roles of the NADPH-Oxidase 1 and 2 in Platelet Activation and Thrombosis. Arterioscler. Thromb. Vasc. Biol. 2016, 36, 846–854. [Google Scholar] [CrossRef] [PubMed]
- Sonkar, V.K.; Kumar, R.; Jensen, M.; Wagner, B.A.; Sharathkumar, A.A.; Miller, F.J.; Fasano, M.B.; Lentz, S.R.; Buettner, G.R.; Dayal, S. Nox2 NADPH Oxidase Is Dispensable for Platelet Activation or Arterial Thrombosis in Mice. Blood Adv. 2019, 3, 1272–1284. [Google Scholar] [CrossRef] [PubMed]
- Vara, D.; Campanella, M.; Pula, G. The Novel NOX Inhibitor 2-Acetylphenothiazine Impairs Collagen-Dependent Thrombus Formation in a GPVI-Dependent Manner. Br. J. Pharmacol. 2013, 168, 212. [Google Scholar] [CrossRef]
- Signorello, M.G.; Leoncini, G. The Molecular Mechanisms Involved in Lectin-Induced Human Platelet Aggregation. Biol. Chem. 2017, 398, 1335–1346. [Google Scholar] [CrossRef] [PubMed]
- Henderson, L.M.; Chappell, J.B. NADPH Oxidase of Neutrophils. Biochim. Biophys. Acta-Bioenerg. 1996, 1273, 87–107. [Google Scholar] [CrossRef] [PubMed]
- Senis, Y.A.; Mazharian, A.; Mori, J. Src Family Kinases: At the Forefront of Platelet Activation. Blood 2014, 124, 2013–2024. [Google Scholar] [CrossRef] [PubMed]
- Leoncini, G.; Maresca, M.; Colao, C.; Piana, A.; Armani, U. Increased Hydrogen Peroxide Formation in Platelets of Patients Affected with Essential Thrombocythaemia (ET). Blood Coagul. Fibrinolysis 1992, 3, 271–277. [Google Scholar] [CrossRef] [PubMed]
- Olas, B.; Kontek, B.; Malinowska, P.; Żuchowski, J.; Stochmal, A. Hippophae Rhamnoides L. Fruits Reduce the Oxidative Stress in Human Blood Platelets and Plasma. Oxid. Med. Cell. Longev. 2016, 2016, 4692486. [Google Scholar] [CrossRef] [PubMed]
- Tietze, F. Enzymic Method for Quantitative Determination of Nanogram Amounts of Total and Oxidized Glutathione: Applications to Mammalian Blood and Other Tissues. Anal. Biochem. 1969, 27, 502–522. [Google Scholar] [CrossRef] [PubMed]
- Lowry, O.H.; Rosebrough, N.J.; Farr, A.L.; Randall, R.J. Protein Measurement with the Folin Phenol Reagent. J. Biol. Chem. 1951, 193, 265–275. [Google Scholar] [CrossRef] [PubMed]
- Harlow, E.; Lane, D. Bradford Assay. Cold Spring Harb. Protoc. 2006, pdb.prot4644. [Google Scholar] [CrossRef] [PubMed]
- Hinkle, P.C. P/O Ratios of Mitochondrial Oxidative Phosphorylation. Biochim. Biophys. Acta 2005, 1706, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Born, G.V. Aggregation of Blood Platelets by Adenosine Diphosphate and Its Reversal. Nature 1962, 194, 927–929. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Signorello, M.G.; Ravera, S.; Leoncini, G. Oxidative Stress Induced by Cortisol in Human Platelets. Int. J. Mol. Sci. 2024, 25, 3776. https://doi.org/10.3390/ijms25073776
Signorello MG, Ravera S, Leoncini G. Oxidative Stress Induced by Cortisol in Human Platelets. International Journal of Molecular Sciences. 2024; 25(7):3776. https://doi.org/10.3390/ijms25073776
Chicago/Turabian StyleSignorello, Maria Grazia, Silvia Ravera, and Giuliana Leoncini. 2024. "Oxidative Stress Induced by Cortisol in Human Platelets" International Journal of Molecular Sciences 25, no. 7: 3776. https://doi.org/10.3390/ijms25073776
APA StyleSignorello, M. G., Ravera, S., & Leoncini, G. (2024). Oxidative Stress Induced by Cortisol in Human Platelets. International Journal of Molecular Sciences, 25(7), 3776. https://doi.org/10.3390/ijms25073776





