Behavior of Hypertrophied Right Ventricle during the Development of Left Ventricular Failure Due to Myocardial Infarction
Abstract
1. Introduction
2. Development of Right Ventricular Hypertrophy
3. Subcellular Remodeling in the Hypertrophied Right Ventricle
4. β-Adrenoreceptor Mediated Signal Transduction in Right Ventricle
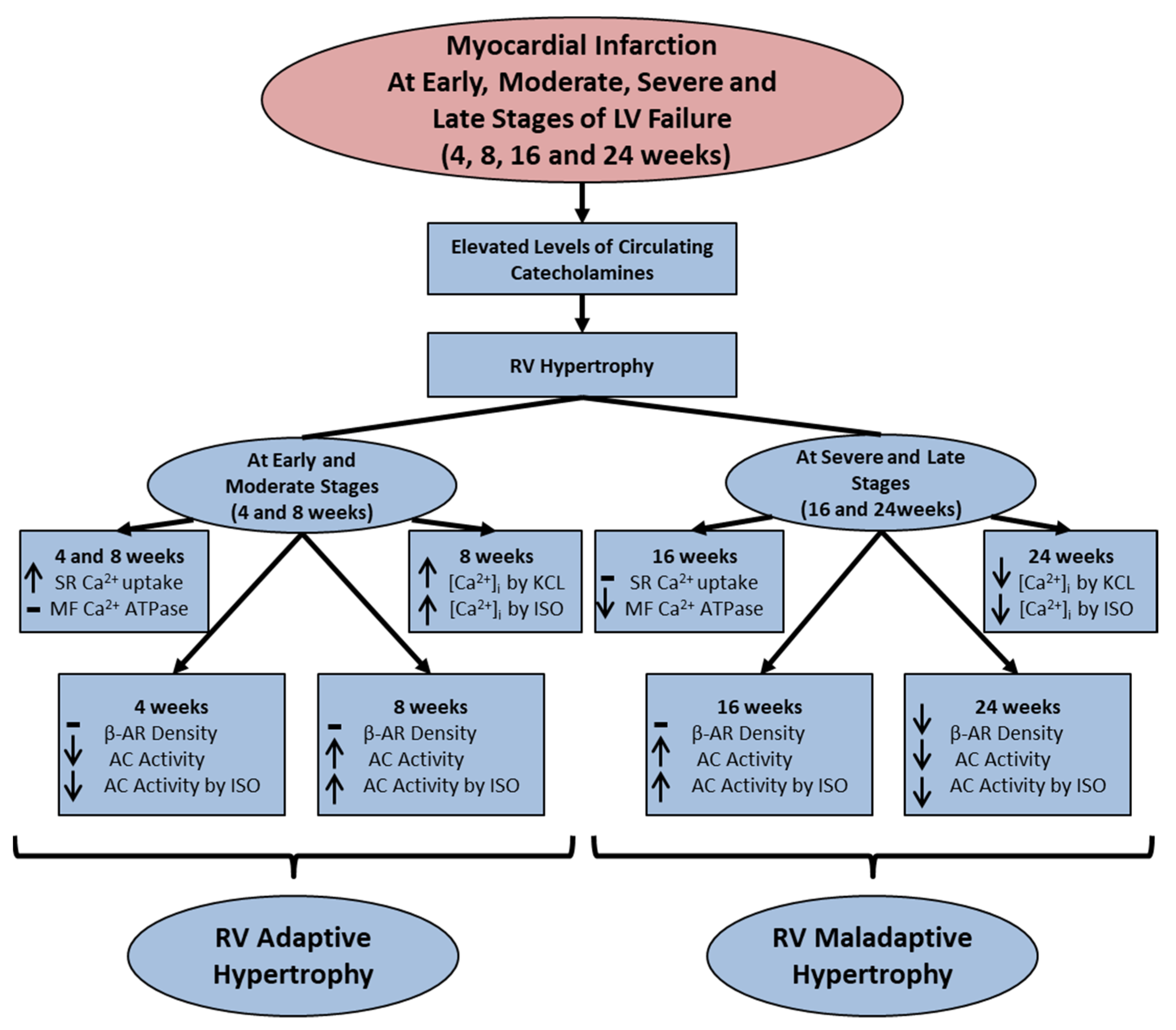
5. Mechanisms of Right Ventricular Remodeling Due to Myocardial Infarction
6. Concluding Remarks
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Parmley, W.W. Pathophysiology and current therapy of congestive heart failure. Am. J. Cardiol. 1989, 13, 771–785. [Google Scholar] [CrossRef]
- Cohen, J.N.; Ferrari, R.; Sharpe, N. Cardiac remodeling—Concepts and clinical implications: A consensus paper from an international form on cardiac remodeling. J. Am. Coll. Cardiol. 2000, 35, 569–582. [Google Scholar] [CrossRef]
- Dhalla, N.S.; Rangi, S.; Babick, A.O.; Zieroth, S.; Elimban, V. Cardiac remodeling and subcellular defects in heart failure due to myocardial infarction and aging. Heart Fail. Rev. 2012, 17, 671–681. [Google Scholar] [CrossRef]
- Packer, M. Neurohormonal interactions and adaptations in congestive heart failure. Circulation 1998, 77, 721–730. [Google Scholar] [CrossRef]
- Mudd, J.O.; Kass, D.A. Tackling heart failure in twenty-first century. Nature 2008, 451, 919–928. [Google Scholar] [CrossRef]
- Zhang, W.; Elimban, V.; Nijjar, M.S.; Gupta, S.K.; Dhalla, N.S. Role of mitogen-activated protein kinase in cardiac hypertrophy and heart failure. Exp. Clin. Cardiol. 2003, 8, 173–183. [Google Scholar]
- Arai, M.; Matsui, H.; Periasamy, M. Sarcoplasmic reticulum gene expression in cardiac hypertrophy and heart failure. Circ. Res. 1994, 74, 555–564. [Google Scholar] [CrossRef]
- Sethi, R.; Saini, H.K.; Guo, X.; Wang, X.; Elimban, V.; Dhalla, N.S. Dependence of changes in β- adrenoreceptor signal transduction on type and stage of cardiac hypertrophy. J. Appl. Physiol. 2007, 102, 978–984. [Google Scholar] [CrossRef]
- Shah, A.K.; Bhullar, S.K.; Elimban, V.; Dhalla, N.S. Oxidative stress as a mechanism for functional alterations in cardiac hypertrophy and heart failure. Antioxidants 2021, 10, 931. [Google Scholar] [CrossRef]
- Dhalla, N.S.; Bhullar, S.K.; Adameova, A.; Mota, K.O.; de Vasconcelos, C.M.L. States of β1- adrenoreceptor signal transduction system in cardiac hypertrophy and heart failure. Res. Cardiovasc. Med. 2023, 24, 264. [Google Scholar] [CrossRef]
- Oldfield, C.J.; Duhamel, J.A.; Dhalla, N.S. Mechanisms for the transition from physiological to pathological cardiac hypertrophy. Can. J. Physiol. Pharmacol. 2020, 98, 74–84. [Google Scholar] [CrossRef]
- Murray, P.A.; Baig, H.; Fishbein, M.E.; Vatner, S.F. Effects of experimental right ventricular and hypertrophy on myocardial blood flow in conscious dogs. J. Clin. Investig. 1997, 64, 421–427. [Google Scholar] [CrossRef]
- Shlafer, M.; Gelband, H.; Sung, R.J.; Palmer, R.F.; Bassett, A.L. Time-dependent alterations of myocardial microsomal yield and calcium accumulation in experimentally-induced right ventricular hypertrophy and failure. J. Mol. Cell. Cardiol. 1978, 10, 395–407. [Google Scholar] [CrossRef]
- Bassett, A.L.; Gelband, H. Chronic partial occlusion of the pulmonary artery in cats: Changes in ventricular action potential configuration during early hypertrophy. Circ. Res. 1973, 32, 15–26. [Google Scholar] [CrossRef] [PubMed]
- Limas, C.J.; Spier, S.S.; Kahlon, J. Enhanced calcium transport by sarcoplasmic reticulum in mild cardiac hypertrophy. J. Mol. Cell. Cardiol. 1980, 12, 1103–1116. [Google Scholar] [CrossRef] [PubMed]
- Dhalla, N.S.; Alto, L.E.; Heyliger, C.E.; Pierce, G.N.; Panagia, V.; Singal, P.K. Sarcoplasmic reticular Ca2+-pump adaptation in cardiac hypertrophy due to pressure overload in pigs. Eur. Heart J. 1984, 5, 323–328. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Ren, B.; Liu, S.; Sentex, E.; Tappia, P.S.; Dhalla, N.S. Characterization of cardiac hypertrophy and heart failure due to volume overload in the rat. J. Appl. Physiol. 2003, 94, 752–763. [Google Scholar] [CrossRef]
- Wang, X.; Sentex, E.; Chapman, D.; Dhalla, N.S. Alterations of adenylyl cyclase and G proteins in aortocaval shunt-induced heart failure. Am. J. Physiol. Heart Circ. Physiol. 2004, 287, 118–125. [Google Scholar] [CrossRef] [PubMed]
- Sentex, E.; Wang, X.; Liu, X.; Lukas, A.; Dhalla, N.S. Expression of protein kinase C isoforms in cardiac hypertrophy and heart failure due to volume overload. Can. J. Physiol. Pharmacol. 2006, 84, 227–238. [Google Scholar] [CrossRef] [PubMed]
- Bloomfield, R.A.; Lauson, H.D.; Cournand, A.; Breed, E.S.; Richards, D.W. Recording of right heart pressures in normal subjects and in patients with chronic pulmonary disease and various types of cardio-circulatory disease. J. Clin. Investig. 1946, 25, 639–664. [Google Scholar] [CrossRef] [PubMed]
- Parmley, W.W. Pathophysiology of congestive heart failure. Am. J. Cardiol. 1985, 55, 9A–14A. [Google Scholar] [CrossRef] [PubMed]
- Dhalla, N.S.; Sulakhe, P.V.; Lee, S.L.; Singal, P.K.; Varley, K.G.; Yates, J.C. Subcellular Ca2+ transport in different areas of dog heart. Can. J. Physiol. Pharmacol. 1980, 58, 360–367. [Google Scholar] [CrossRef] [PubMed]
- DeFelice, A.; Frering, R.; Horan, P. Time course of hemodynamic changes in rats with healed severe myocardial infarction. Am. J. Physiol. 1989, 257, H289–H296. [Google Scholar] [CrossRef] [PubMed]
- Pfeffer, J.M.; Pfeffer, M.A.; Fletcher, P.J.; Braunwald, E. Progressive ventricular remodeling in rat with myocardial infarction. Am. J. Physiol. 1991, 260, H1406–H1414. [Google Scholar] [CrossRef] [PubMed]
- Anversa, P.; Beghi, C.; Kikkawa, Y.; Olivetti, G. Myocardial response to infarction in the rat. Morphometric measurement of infarct size and myocyte cellular hypertrophy. Am. J. Pathol. 1985, 118, 484–492. [Google Scholar] [PubMed]
- Anversa, P.; Beghi, C.; Kikkawa, Y.; Olivetti, G. Myocardial infarction in rats. Infarct size, myocyte hypertrophy, and capillary growth. Circ. Res. 1986, 58, 26–37. [Google Scholar] [CrossRef]
- Fletcher, P.J.; Pfeffer, J.M.; Pfeffer, M.A.; Braunwald, E. Left ventricular diastolic pressure-volume relations in rats with healed myocardial infarction. Effects on systolic function. Circ. Res. 1981, 49, 618–626. [Google Scholar] [CrossRef]
- Pfeffer, M.A.; Pfeffer, J.M.; Fishbein, M.C.; Fletcher, P.J.; Spadaro, J.; Kloner, R.A.; Braunwald, E. Myocardial infarct size and ventricular function in rats. Circ. Res. 1979, 44, 503–512. [Google Scholar] [CrossRef]
- Dixon, I.M.; Lee, S.L.; Dhalla, N.S. Nitrendipine binding in congestive heart failure due to myocardial infarction. Circ. Res. 1990, 66, 782–788. [Google Scholar] [CrossRef] [PubMed]
- Homcy, C.M.; Vatner, S.F.; Vatner, D.E. β-Adrenoreceptor receptor regulation in the heart in pathophysiologic states: Abnormal adrenergic responsiveness in cardiac disease. Annu. Rev. Physiol. 1991, 53, 137–159. [Google Scholar] [CrossRef] [PubMed]
- Sethi, R.; Elimban, V.; Chapman, D.; Dixon, I.M.; Dhalla, N.S. Differential alterations in left and right ventricular G-proteins in congestive heart failure due to myocardial infarction. J. Mol. Cell. Cardiol. 1998, 30, 2153–2163. [Google Scholar] [CrossRef]
- Sethi, R.; Saini, H.K.; Wang, X.; Elimban, V.; Babick, A.; Dhalla, N.S. Differential changes in beta-adrenoceptor signal transduction in left and right ventricles of infarcted rats. Can. J. Physiol. Pharmacol. 2006, 84, 747–754. [Google Scholar] [CrossRef]
- Anversa, P.; Loud, A.V.; Levicky, V.; Guideri, G. Left ventricular failure induced by myocardial infarction. I. Myocyte hypertrophy. Am. J. Physiol. 1985, 248, 876–882. [Google Scholar] [CrossRef]
- Wang, J.; Liu, X.; Sentex, E.; Takeda, N.; Dhalla, N.S. Increased expression of protein kinase C isoforms in heart failure due to myocardial infarction. Am. J. Physiol. Heart Circ. Physiol. 2003, 284, H2277–H2287. [Google Scholar]
- Meij, J.T.; Panagia, V.; Mesaeli, N.; Peachell, J.L.; Afzal, N.; Dhalla, N.S. Identification of changes in cardiac phospholipase C activity in congestive heart failure. J. Mol. Cell. Cardiol. 1997, 29, 237–246. [Google Scholar] [CrossRef]
- Ganguly, P.K.; Dhalla, K.S.; Shao, Q.; Beamish, R.E.; Dhalla, N.S. Differential changes in sympathetic activity in left and right ventricles in congestive heart failure after myocardial infarction. Am. Heart J. 1997, 133, 340–405. [Google Scholar] [CrossRef]
- Afzal, N.; Dhalla, N.S. Differential changes in left and right ventricular SR calcium transport in congestive heart failure. Am. J. Physiol. 1992, 262, 868–874. [Google Scholar] [CrossRef]
- Malhotra, A.; Penpargkul, S.; Schaible, T.; Scheuer, J. Contractile proteins and sarcoplasmic reticulum in physiologic cardiac hypertrophy. Am. J. Physiol. 1981, 241, H263–H267. [Google Scholar] [CrossRef] [PubMed]
- Panagia, V.; Pierce, G.N.; Dhalla, K.S.; Ganguly, P.K.; Beamish, R.E.; Dhalla, N.S. Adaptive changes in subcellular calcium transport during catecholamine-induced cardiomyopathy. J. Mol. Cell. Cardiol. 1985, 17, 411–420. [Google Scholar] [CrossRef] [PubMed]
- Zimmer, H.G.; Martius, P.A.; Marschner, G. Myocardial infarction in rats: Effects of metabolic and pharmacologic interventions. Basic. Res. Cardiol. 1989, 84, 332–343. [Google Scholar] [CrossRef] [PubMed]
- Fletcher, P.J.; Pfeffer, J.M.; Pfeffer, M.A.; Braunwald, E. Effects of hypertension on cardiac performance in rats with myocardial infarction. Am. J. Cardiol. 1982, 50, 488–496. [Google Scholar] [CrossRef]
- Wang, J.; Liu, X.; Ren, B.; Rupp, H.; Takeda, N.; Dhalla, N.S. Modification of myosin gene expression by imidapril in failing heart due to myocardial infarction. J. Mol. Cell. Cardiol. 2002, 34, 847–857. [Google Scholar] [CrossRef]
- Geenen, D.L.; Malhotra, A.; Scheuer, J. Regional variation in rat cardiac myosin isoenzymes and ATPase activity after infarction. Am. J. Physiol. 1989, 256, H745–H750. [Google Scholar] [CrossRef]
- Shimada, T.; Yoshiyama, M.; Takeuchi, K.; Omura, T.; Takemoto, Y.; Kim, S.; Iwao, H.; Yoshikawa, J. Long acting calcium antagonist amlodipine prevents left ventricular remodeling after myocardial infarction in rats. Cardiovasc. Res. 1998, 37, 618–626. [Google Scholar] [CrossRef]
- Wang, J.; Guo, X.; Dhalla, N.S. Modification of myosin protein and gene expression in failing hearts due to myocardial infarction by enalapril or losartan. Biochim. Biophys. Acta 2004, 1690, 177–184. [Google Scholar] [CrossRef][Green Version]
- Sethi, R.; Dhalla, K.S.; Beamish, R.E.; Dhalla, N.S. Differential changes in left and right ventricular adenylyl cyclase activities in congestive heart failure. Am. J. Physiol. 1997, 272, 884–893. [Google Scholar] [CrossRef]
- Reiss, K.; Capasso, J.M.; Huang, H.E.; Meggs, L.G.; Li, P.; Anversa, P. ANG II receptors, c-myc, and c-jun in myocytes after myocardial infarction and ventricular failure. Am. J. Physiol. 1993, 264, H760–H769. [Google Scholar] [CrossRef] [PubMed]
- Anversa, P.; Sonnenblick, E.H. Ischemic cardiomyopathy: Pathophysiologic mechanisms. Prog. Cardiovasc. Dis. 1990, 33, 49–70. [Google Scholar] [CrossRef] [PubMed]
- Capasso, J.M.; Li, P.; Zhang, X.; Anversa, P. Heterogeneity of ventricular remodeling after acute myocardial infarction in rats. Am. J. Physiol. 1992, 262, H486–H495. [Google Scholar] [CrossRef] [PubMed]
- Meggs, L.G.; Tillotson, J.; Huang, H.; Sonnenblick, E.H.; Capasso, J.M.; Anversa, P. Noncoordinate regulation of α1 adrenoreceptor coupling and reexpression of α skeletal actin in myocardial infarction-induced left ventricular failure in rats. J. Clin. Investig. 1990, 86, 1451–1458. [Google Scholar] [CrossRef] [PubMed]
- Holmgren, S.; Abrahamsson, T.; Almgren, O.; Eriksson, B.M. Effect of ischaemic on the adrenergic neurons of the rat heart: A fluorescence histochemical and biochemical study. Cardiovasc. Res. 1981, 15, 680–689. [Google Scholar] [CrossRef]
- Mathes, P.; Gudbjarnason, S. Changes in norepinephrine stores in the canine heart following experimental myocardial infarction. Am. Heart J. 1971, 81, 211–219. [Google Scholar] [CrossRef]
- Zelis, R.; Clemson, B.; Baily, R.; Davis, D. Regulation of tissue noradrenaline in the rat myocardial infarction model of chronic heart failure. Cardiovasc. Res. 1992, 26, 933–938. [Google Scholar] [CrossRef]
- Dhalla, N.S.; Dzurba, A.; Pierce, G.N.; Tregaskis, M.G.; Panagia, V.; Beamish, R.E. Membrane changes in myocardium during catecholamine-induced pathological hypertrophy. Persp. Cadiovasc. Res. 1969, 7, 527–534. [Google Scholar]
- Moser, D.K. Pathophysiology of heart failure update: The role of neurohumoral activation in the progression of heart failure. AACN Adv. Crit. Care 1998, 9, 157–171. [Google Scholar] [CrossRef]
- Ramachandra, C.J.A.; Cong, S.; Chan, X.; Yap, E.P.; Yu, F.; Hausenloy, D.J. Oxidative stress in cardiac hypertrophy: From molecular mechanisms to novel therapeutic targets. Free Rad. Biol. Med. 2021, 166, 297–312. [Google Scholar] [CrossRef]
- Neri, M.; Fineschi, V.; Di Paolo, M.; Pomara, C.; Riezzo, I.; Turillazzi, E.; Cerretani, D. Cardiac oxidative stress and inflammatory cytokines response after myocardial infarction. Curr. Vasc. Pharmacol. 2015, 13, 26–36. [Google Scholar] [CrossRef] [PubMed]
- Llucià-Valldeperas, A.; de Man, F.S.; Bogaard, H.J. Adaptation and maladaptation of the right ventricle in pulmonary vascular diseases. Clin. Chest. Med. 2021, 42, 179–194. [Google Scholar] [CrossRef] [PubMed]
- Keen, J.; Prisco, S.Z.; Prins, K.W. Sex differences in right ventricular dysfunction: Insights from the bench to bedside. Front. Physiol. 2021, 11, 623129. [Google Scholar] [CrossRef] [PubMed]
- Bourantas, C.V.; Loh, H.P.; Bragadeesh, T.; Rigby, A.S.; Lukaschuk, E.I.; Garg, S.; Tweddel, A.C.; Alamgir, F.M.; Nikitin, N.P.; Clark, A.L.; et al. Relationship between right ventricular volumes measured by cardiac magnetic resonance imaging and prognosis in patients with chronic heart failure. Eur. J. Heart Fail. 2021, 13, 52–60. [Google Scholar] [CrossRef] [PubMed]
- Kawut, S.M.; Pinder, D.; Al-Naamani, N.; McCormick, A.; Palevsky, H.I.; Fritz, J.; Smith, K.A.; Mazurek, J.A.; Doyle, M.F.; MacLean, M.R.; et al. Fulvestrant for the Treatment of pulmonary arterial hypertension. Ann. Am. Thoracic Soc. 2019, 16, 1456–1459. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Sellés, M.; Muñoa, M.D.; Martínez, E.; Fernández, M.A.; García, E. The influence of sex on right ventricular dysfunction in patients with severely depressed left ventricular ejection fraction. Eur. J. Heart Fail. 2006, 8, 400–403. [Google Scholar] [CrossRef] [PubMed]
- Melenovsky, V.; Hwang, S.J.; Lin, G.; Redfield, M.M.; Borlaug, B.A. Right heart dysfunction in heart failure with preserved ejection fraction. Eur. Heart J. 2014, 35, 3452–3462. [Google Scholar] [CrossRef]
- Mohammed, S.F.; Hussain, I.; AbouEzzeddine, O.F.; Takahama, H.; Kwon, S.H.; Forfia, P.; Roger, V.L.; Redfield, M.M. Right ventricular function in heart failure with preserved ejection fraction: A community-based study. Circulation 2014, 130, 2310–2320. [Google Scholar] [CrossRef]
- Duca, F.; Zotter-Tufaro, C.; Kammerlander, A.A.; Aschauer, S.; Binder, C.; Mascherbauer, J.; Bonderman, D. Gender-related differences in heart failure with preserved ejection fraction. Sci. Rep. 2018, 8, 1080. [Google Scholar] [CrossRef] [PubMed]

| Parameters | Control | Early Stage | Moderate Stage | Severe Stage | Late Stage |
|---|---|---|---|---|---|
| (4 Weeks MI) | (8 Weeks MI) | (16 Weeks MI) | (24 Weeks MI) | ||
| Scar wt (g): | |||||
| ND | 0.361 ± 0.061 | 0.371 ± 0.082 | 0.351 ± 0.061 | 0.350 ± 0.052 * | |
| Viable Left Ventricle wt (g): | |||||
| 0.805 ± 0.086 | 0.794 ± 0.092 | 1.273 ± 0.172 * | 1.475 ± 0.103 * | 1.548 ± 0.149 * | |
| Right Ventricle wt (g): | |||||
| 0.235 ± 0.033 | 0.331 ± 0.027 * | 0.392 ± 0.041 * | 0.427 ± 0.047 * | 0.546 ± 0.026 * | |
| Ascites (mL): | |||||
| ND | 3.4 ± 1.1 * | 6.2 ± 1.9 * | 12.0 ± 0.2 * | 13.2 ± 1.4 * | |
| Left Ventricle Systolic Pressure (mmHg): | |||||
| 125 ± 5.2 | 131 ± 6.1 | 121 ± 2.8 | 93 ± 4.1 * | 84 ± 3.9 * | |
| Left Ventricle Diastolic Pressure (mmHg): | |||||
| 2.1 ± 0.1 | 11.5 ± 2.2 * | 12.0 ± 1.3 * | 15 ± 0.7 * | 20 ± 4.3 * | |
| Left Ventricle + dP/dt (mmHg/s): | |||||
| 5986 ± 197 | 4691 ± 172 * | 4691 ± 172 * | 3645 ± 330 * | 3608 ± 218 * | |
| Left Ventricle − dP/dt (mmHg/s): | |||||
| 5184 ± 272 | 3507 ± 197 * | 382 ± 214 * | 3152 ± 284 * | 3314 ± 168 * | |
| Parameters | Pre-Failure Stage | Early Failure Stage | Moderate Failure Stage | |||
|---|---|---|---|---|---|---|
| Sham | (2 Weeks MI) | Sham | (4 Weeks MI) | Sham | (8 Weeks MI) | |
| Right ventricle wt (g) | ||||||
| 163 ± 5.2 | 216 ± 17.2 * | 172 ± 12.6 | 306 ± 33.1 * | 278 ± 17.1 | 600 ± 19.8 * | |
| Ca2+-dependent PKC activity (pmol 32P/min/mg protein) | ||||||
| 126 ± 4.7 | 156 ± 15.3 * | 98.7 ± 6.8 | 132 ± 13.4 * | 93.5 ± 6.4 | 184 ± 14 * | |
| Ca2+-independent PKC activity (pmol 32P/min/mg protein) | ||||||
| 118 ± 4.9 | 146 ± 8.9 * | 106 ± 2.6 | 137 ± 4.7 * | 70.5 ± 5.2 | 238 ± 18.5 * | |
| Parameters | Sham | Moderate Failure Stage (8 Weeks MI) |
|---|---|---|
| A. Protein kinase C (% of control): | ||
| PKC-α | 100 | 138 ± 11 * |
| PKC-β | 100 | 145 ± 16 * |
| PKC-ℇ | 100 | 126 ± 5 * |
| PKC-ꞔ | 100 | 108 ± 3 |
| B. Protein kinase A | ||
| PKA content (% of control): | 100 | |
| PKA activity (pmol 32P/min/mg protein): | 3600 ± 356 | 3580 ± 375 |
| Parameters | Moderate Failure Stage | Severe Failure Stage | ||
| Control | (8 Weeks MI) | Control | (16 Weeks MI) | |
| A. PLC activity (nmol IP3/min/mg protein): | 4.35 ± 0.64 | 4.23 ± 0.37 | 5.42 ± 0.60 | 3.7 ± 0.58 * |
| B. Kinetic parameters | ||||
| Vmax (nmol IP3/min/mg protein): | 35.5 ± 4.2 | 36.9 ± 5.4 | 37.7 ± 3.1 | 40.1 ± 7.0 |
| Km (μM PIP2): | 123 ± 11 | 138 ± 6 | 118 ± 3 | 193 ± 7 * |
| Parameters | Control | Early Failure | Moderate Failure | Severe Failure |
|---|---|---|---|---|
| (4 Weeks MI) | (8 Weeks MI) | (8 Weeks MI) | ||
| A. Calcium uptake (nmol Ca2+/min/mg protein) | 29 ± 1.9 | 42 ± 1.6 * | 35 ± 1.3* | 25 ± 0.9 |
| B. Kinetic parameters | ||||
| Vmax (nmol/min/mg protein): | 30 ± 1.5 | 45 ± 0.9 * | 37 ± 1.3 * | 25 ± 1.2 |
| Km (μM Ca2+): | 0.61 ± 0.04 | 0.52 ± 0.06 | 0.52 ± 0.09 | 0.58 ± 0.05 |
| Parameters | Control | Early Failure | Moderate Failure | Severe Failure |
|---|---|---|---|---|
| (4 Weeks MI) | (8 Weeks MI) | (16 Weeks MI) | ||
| A. Myofibrillar Ca2+-stimulated ATPase activity (μmolPi/h/mg protein): | ||||
| 8.9 ± 035 | 8.1 ± 0.33 | 8.0 ± 0.38 | 7.3 ± 0.23 * | |
| B. Myosin protein and isozyme expression at 8 weeks MI | ||||
| Protein content (% of control): | 95 ± 2.4 | |||
| Myosin isozymes (% of total) | ||||
| Decrease in myosin α: | 57 ± 5 * | |||
| Increase in myosin β: | 43 ± 4 * | |||
| C. Myosin mRNA expression (at 8 weeks MI) | ||||
| Decrease in myosin α mRNA (% of control) | 45 ± 5 * | |||
| Increase in myosin β mRNA (% of control) | 40 ± 5 * | |||
| Parameters | Moderate Failure Stage | Late Failure Stage | ||
|---|---|---|---|---|
| Control | (8 Weeks MI) | Control | (24 Weeks MI) | |
| A. Basal | ||||
| [Ca2+]i (nmol/L): | 83 ± 7.1 | 82 ± 5.2 | 82 ± 6.4 | 87 ± 5.3 |
| B. KCL-induced increase | ||||
| [Ca2+]i (nmol/L): | 52 ± 3.4 | 78 ± 4.9 * | 56 ± 2.8 | 38 ± 1.7 * |
| C. Isoproterenol-induced increase | ||||
| [Ca2+]i (nmol/L): | 33 ± 4.8 | 48 ± 5.6 * | 36 ± 3.1 | 24 ± 2.2 * |
| Parameters | Moderate Failure Stage | Late Failure Stage | ||
|---|---|---|---|---|
| Control | (8 Weeks MI) | Control | (24 Weeks MI) | |
| A. β-adrenoreceptors | ||||
| Bmax (f mol/mg protein) | 54 ± 3.7 | 58 ± 4.1 | 51 ± 2.9 | 36 ± 2.7 * |
| Kd (p mol) | 49 ± 6.4 | 55 ± 5.2 | 54 ± 6.0 | 49 ± 4.6 |
| B. Adenylyl cyclase activity (pmol cyclic AMP/10 min/mg protein) | ||||
| Basal: | 121 ± 8.9 | 152 ± 7.6 * | 123 ± 6.8 | 65 ± 4.2 * |
| Isoproterenol: | 327 ± 18.5 | 486 ± 29.7 * | 290 ± 18.5 | 113 ± 8.6 * |
| Parameters | Control | Early Failure Stage (4 Week MI) | Moderate Failure Stage (8 Weeks MI) | Severe Failure Stage (16 Weeks MI) |
|---|---|---|---|---|
| A. β1-Adrenoreceptors | ||||
| Bmax (f mol/mg protein): | 24 ± 2.3 | 29 ± 3.1 | 28 ± 3.1 | 27 ± 3.2 |
| Kd (pM): | 48 ± 3.3 | 49 ± 3.4 | 49 ± 4.0 | 49 ± 4.1 |
| B. β2-Adrenoreceptors | ||||
| Bmax (f mol/mg protein): | 8 ± 1.9 | 7 ± 1.1 | 9 ± 2.0 | 10 ± 1.8 |
| Kd (pM): | 13 ± 1.2 | 14 ± 1.0 | 11 ± 1.3 | 12 ± 1.4 |
| C. Adenylyl cyclase activity (pmol cyclic AMP/10 min/mg protein) | ||||
| Isoproterenol | 402 ± 35 | 258 ± 21 * | 640 ± 42 * | 648 ± 45 * |
| Parameters | Control | Early Failure Stage (4 Weeks MI) | Moderate Failure Stage (8 Weeks MI) | Severe Failure Stage (16 Weeks MI) |
|---|---|---|---|---|
| Adenylyl cyclase activity (pmol cyclic AMP/10 min/mg protein): | ||||
| Basal | 114 ± 15 | 66 ± 8 * | 156 ± 8 * | 163 ± 10* |
| NaF (5 mM) | 570 ± 54 | 244 ± 36 * | 936 ± 76 * | 720 ± 31 * |
| Foskolin (100 μM) | 353 ± 23 | 183 ± 22 * | 624 ± 45 * | 484 ± 12 * |
| Gpp (NH)p (30 μM) | 300 ± 16 | 171 ± 12 * | 445 ± 21 * | 455 ± 9 * |
| Parameters | Control | Early Failure Stage (4 Weeks MI) | Moderate Failure Stage (8 Weeks MI) | Severe Failure Stage (16 Weeks MI) |
|---|---|---|---|---|
| A. Adenylyl cyclase activity (pmol cyclic AMP/10 min/mg protein): | ||||
| Basal | 148 ± 9.5 | 120 ± 8.6 * | 184 ± 11.2 * | 186 ± 10.7 * |
| Pertussis toxin | 214 ± 12.9 | 278 ± 15.6 * | 218 ± 12.8 | 206 ± 10.9 |
| B. ADP ribosylation | ||||
| Pertussis toxin catalyzed (% control): | 100 | 162 ± 12 * | 111 ± 10 | 107 ± 7 |
| C. G-protein content | ||||
| Giα protein (% control) | 100 | 172 ± 28 * | 94 ± 9 | 107 ± 7 |
| Parameters | Control | Early Failure Stage (4 Weeks MI) | Moderate Failure Stage (8 Weeks MI) | Severe Failure Stage (16 Weeks MI) |
|---|---|---|---|---|
| A. Adenylyl cyclase activity (pmol/cyclic AMP/10 min/mg protein): | ||||
| Basal | 148 ± 7.6 | 115 ± 5.8 * | 208 ± 17.9 * | 200 ± 14.5 * |
| Cholera Toxin | 292 ± 15.8 | 240 ± 8.9 * | 486 ± 23.7 * | 478 ± 26.2 * |
| B. ADP ribosylation | ||||
| Cholera toxin catalyzed at | ||||
| 45 KD (% control) | 100 | 98 ± 8 | 148 ± 12 * | 137 ± 12 * |
| 52 KD (% control) | 100 | 97 ± 10 | 144 ± 10 * | 129 ± 12 |
| C. G-protein content | ||||
| Gs protein 45 KD (% of control) | 100 | 105 ± 10 | 300 ± 14 * | 213 ± 22 * |
| Gs protein 52 KD (% of control) | 100 | 101 ± 9 | 208 ± 10 * | 152 ± 10 * |
| Parameters | Control | Early Failure Stage (4 Weeks MI) | Moderate Failure Stage (8 Weeks MI) |
|---|---|---|---|
| Plasma norepinephrine (pg/mL): | 920 ± 160 | 1076 ± 143 | 1820 ± 208 * |
| Plasma epinephrine (pg/mL): | 846 ± 209 | 1868 ± 165 * | 1680 ± 248 * |
| Right ventricle norepinephrine (ng/g) | 224 ± 12 | 208 ± 17 | 265 ± 20 * |
| Right ventricle Epinephrine (ng/g) | 18 ± 3.2 | 38 ± 2.6 * | 42 ± 3.8 * |
| Norepinephrine Turnover (Kh−1) | 0.12 ± 0.008 | ND | 0.13 ± 0.01 |
| Initial radioactivity (DPM) | 3940 ± 180 | ND | 7264 ± 235 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dhalla, N.S.; Mota, K.O.; de Vasconcelos, C.M.L.; Adameova, A. Behavior of Hypertrophied Right Ventricle during the Development of Left Ventricular Failure Due to Myocardial Infarction. Int. J. Mol. Sci. 2024, 25, 2610. https://doi.org/10.3390/ijms25052610
Dhalla NS, Mota KO, de Vasconcelos CML, Adameova A. Behavior of Hypertrophied Right Ventricle during the Development of Left Ventricular Failure Due to Myocardial Infarction. International Journal of Molecular Sciences. 2024; 25(5):2610. https://doi.org/10.3390/ijms25052610
Chicago/Turabian StyleDhalla, Naranjan S., Karina Oliveira Mota, Carla Maria Lins de Vasconcelos, and Adriana Adameova. 2024. "Behavior of Hypertrophied Right Ventricle during the Development of Left Ventricular Failure Due to Myocardial Infarction" International Journal of Molecular Sciences 25, no. 5: 2610. https://doi.org/10.3390/ijms25052610
APA StyleDhalla, N. S., Mota, K. O., de Vasconcelos, C. M. L., & Adameova, A. (2024). Behavior of Hypertrophied Right Ventricle during the Development of Left Ventricular Failure Due to Myocardial Infarction. International Journal of Molecular Sciences, 25(5), 2610. https://doi.org/10.3390/ijms25052610





