Association between Estrogen Levels and Temporomandibular Disorders: An Updated Systematic Review
Abstract
1. Introduction
2. Methods
3. Results
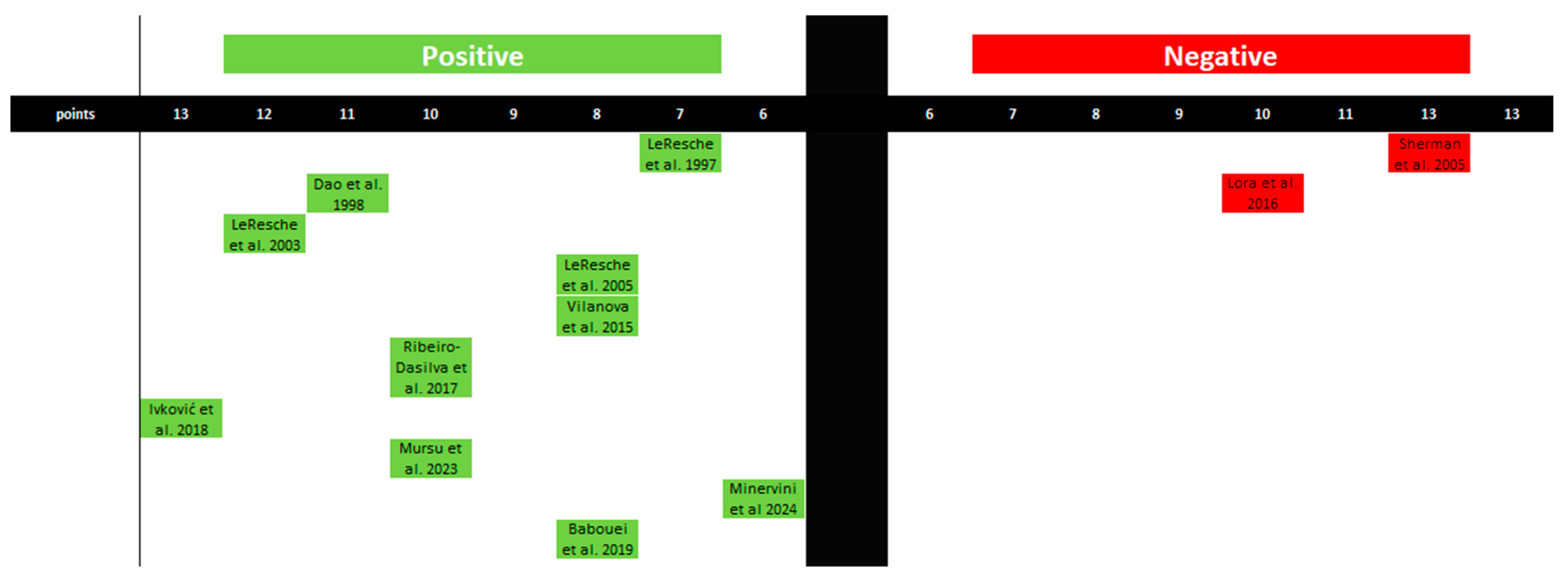
3.1. Presentation and Evaluation of Qualified Studies
3.2. Synthesis of Systematic Reviews
4. Discussion
5. Conclusions
- Estrogen levels are associated with pain modulation in the temporomandibular joint and the entire orofacial region.
- There is insufficient evidence to either confirm or refute the influence of estrogen on the occurrence of TMDs.
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bordoni, B.; Varacallo, M. Anatomy, Head and Neck, Temporomandibular Joint. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2024. [Google Scholar]
- Zieliński, G.; Pająk-Zielińska, B.; Ginszt, M. A Meta-Analysis of the Global Prevalence of Temporomandibular Disorders. J. Clin. Med. 2024, 13, 1365. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, A.; Hasebe, M.; Hamada, Y. Intra-Articular Pathologies Detected by Magnetic Resonance Imaging in Patients with Temporomandibular Disorders Undergone Successful Non-Surgical Treatments. J. Oral Maxillofac. Surg. Med. Pathol. 2024, 36, 804–809. [Google Scholar] [CrossRef]
- Xie, C.; Lin, M.; Yang, H.; Ren, A. Prevalence of Temporomandibular Disorders and Its Clinical Signs in Chinese Students, 1979–2017: A Systematic Review and Meta-Analysis. Oral Dis. 2019, 25, 1697–1706. [Google Scholar] [CrossRef] [PubMed]
- Minervini, G.; Franco, R.; Marrapodi, M.M.; Fiorillo, L.; Cervino, G.; Cicciù, M. Prevalence of Temporomandibular Disorders in Children and Adolescents Evaluated with Diagnostic Criteria for Temporomandibular Disorders: A Systematic Review with Meta-Analysis. J. Oral Rehabil. 2023, 50, 522–530. [Google Scholar] [CrossRef]
- Melo, V.; Monteiro, L.; Orge, C.; Sales, M.; Melo, J.; Rodrigues, B.; Melo, A. Prevalence of Temporomandibular Disorders in the Brazilian Population: A Systematic Review and Meta-Analysis. Cranio J. Craniomandib. Pract. 2023, 1–8. [Google Scholar] [CrossRef]
- Robinson, J.L.; Johnson, P.M.; Kister, K.; Yin, M.T.; Chen, J.; Wadhwa, S. Estrogen Signaling Impacts Temporomandibular Joint and Periodontal Disease Pathology. Odontology 2020, 108, 153–165. [Google Scholar] [CrossRef]
- Wright, G.J.; Coombs, M.C.; Hepfer, R.G.; Damon, B.J.; Bacro, T.H.; Lecholop, M.K.; Slate, E.H.; Yao, H. Tensile Biomechanical Properties of Human Temporomandibular Joint Disc: Effects of Direction, Region and Sex. J. Biomech. 2016, 49, 3762–3769. [Google Scholar] [CrossRef]
- Wright, G.J.; Coombs, M.C.; Wu, Y.; Damon, B.J.; Bacro, T.H.; Kern, M.J.; Chen, X.; Yao, H. Electrical Conductivity Method to Determine Sexual Dimorphisms in Human Temporomandibular Disc Fixed Charge Density. Ann. Biomed. Eng. 2018, 46, 310–317. [Google Scholar] [CrossRef]
- Hong, S.W.; Lee, J.K.; Kang, J.-H. Skeletal Maturation and Predicted Adult Height in Adolescents with Temporomandibular Joint Osteoarthritis. J. Oral Rehabil. 2019, 46, 541–548. [Google Scholar] [CrossRef]
- Berger, M.; Szalewski, L.; Bakalczuk, M.; Bakalczuk, G.; Bakalczuk, S.; Szkutnik, J. Association between Estrogen Levels and Temporomandibular Disorders: A Systematic Literature Review. Menopause Rev. Menopauzalny 2015, 14, 260–270. [Google Scholar] [CrossRef]
- Bi, R.-Y.; Ding, Y.; Gan, Y.-H. A New Hypothesis of Sex-Differences in Temporomandibular Disorders: Estrogen Enhances Hyperalgesia of Inflamed TMJ through Modulating Voltage-Gated Sodium Channel 1.7 in Trigeminal Ganglion? Med. Hypotheses 2015, 84, 100–103. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, N.; Chen, S.; Wang, W.; Kapila, S. 17β-Estradiol Induces MMP-9 and MMP-13 in TMJ Fibrochondrocytes via Estrogen Receptor α. J. Dent. Res. 2018, 97, 1023–1030. [Google Scholar] [CrossRef] [PubMed]
- Doetzer, A.D.; Almeida, L.E.; de Alcântara Camejo, F.; de Noronha, L.; Olandoski, M.; Trevilatto, P.C. Association of Estrogen Receptor Alpha 1 and TMJ Dysfunction: A Pilot Study. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2021, 131, e89–e94. [Google Scholar] [CrossRef] [PubMed]
- Abubaker, A.O.; Raslan, W.F.; Sotereanos, G.C. Estrogen and Progesterone Receptors in Temporomandibular Joint Discs of Symptomatic and Asymptomatic Persons: A Preliminary Study. J. Oral Maxillofac. Surg. 1993, 51, 1096–1100. [Google Scholar] [CrossRef]
- Marty, M.S.; Carney, E.W.; Rowlands, J.C. Endocrine Disruption: Historical Perspectives and Its Impact on the Future of Toxicology Testing. Toxicol. Sci. 2011, 120, S93–S108. [Google Scholar] [CrossRef]
- Huether, S.; McCance, K. Understanding Pathophysiology, 7th ed.; Mosby: Maryland Heights, MO, USA, 2019; ISBN 978-0-323-67281-8. [Google Scholar]
- Naprotechnologia—Przeliczniki Hormony—Napromed. Available online: https://napromed.pl/naprotechnologia-przeliczniki-hormony.html (accessed on 14 August 2024).
- Anckaert, E.; Jank, A.; Petzold, J.; Rohsmann, F.; Paris, R.; Renggli, M.; Schönfeld, K.; Schiettecatte, J.; Kriner, M. Extensive Monitoring of the Natural Menstrual Cycle Using the Serum Biomarkers Estradiol, Luteinizing Hormone and Progesterone. Pract. Lab. Med. 2021, 25, e00211. [Google Scholar] [CrossRef]
- Gajewski, K. Estrogeny. Available online: http://www.mp.pl/social/article/171848 (accessed on 8 August 2024).
- Bręborowicz, G.H.; Rechberger, T. (Eds.) Ginekologia; Położnictwo i ginekologia; Wydanie I, 6 Dodruk.; PZWL: Wydawnictwo Naukowe PWN: Warszawa, Poland, 2022; ISBN 978-83-200-6248-9. [Google Scholar]
- Zieliński, G.; Gawda, P. Surface Electromyography in Dentistry—Past, Present and Future. J. Clin. Med. 2024, 13, 1328. [Google Scholar] [CrossRef]
- Zieliński, G.; Pająk, A.; Wójcicki, M. Global Prevalence of Sleep Bruxism and Awake Bruxism in Pediatric and Adult Populations: A Systematic Review and Meta-Analysis. J. Clin. Med. 2024, 13, 4259. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Zieliński, G.; Pająk-Zielińska, B. Association between Estrogen Levels and Temporomandibular Disorders: An Updated Systematic Review. OSF 2024. [Google Scholar] [CrossRef]
- Brown, D. A Review of the PubMed PICO Tool: Using Evidence-Based Practice in Health Education. Health Promot. Pract. 2020, 21, 496–498. [Google Scholar] [CrossRef] [PubMed]
- Chang, V.K.O.; Thambar, S. TMJ Pain as a Presentation of Metastatic Breast Cancer to the Right Mandibular Condyle. BMJ Case Rep. 2021, 14, e241601. [Google Scholar] [CrossRef] [PubMed]
- Almubarak, H.; Alzahrani, F.; Mohammed, K.; Meer, Z. Prevalence of Temporomandibular Disorders (TMDs) in Relation to Estrogen Levels among Females in Aseer Region, Saudi Arabia. Ann. Trop. Med. Public Health 2020, 23, 227298424. [Google Scholar] [CrossRef]
- Higgins, J.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A.; Cochrane Collaboration (Eds.) Cochrane Handbook for Systematic Reviews of Interventions, 2nd ed.; Cochrane Book Series; Wiley Blackwell: Hoboken, NJ, USA; Chichester, UK, 2019; ISBN 978-1-119-53662-8. [Google Scholar]
- Whiting, P.F.; Rutjes, A.W.S.; Westwood, M.E.; Mallett, S.; Deeks, J.J.; Reitsma, J.B.; Leeflang, M.M.G.; Sterne, J.A.C.; Bossuyt, P.M.M. QUADAS-2 Group QUADAS-2: A Revised Tool for the Quality Assessment of Diagnostic Accuracy Studies. Ann. Intern. Med. 2011, 155, 529–536. [Google Scholar] [CrossRef]
- Schiffman, E.; Ohrbach, R.; Truelove, E.; Look, J.; Anderson, G.; Goulet, J.-P.; List, T.; Svensson, P.; Gonzalez, Y.; Lobbezoo, F.; et al. Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) for Clinical and Research Applications: Recommendations of the International RDC/TMD Consortium Network* and Orofacial Pain Special Interest Group†. J. Oral Facial Pain Headache 2014, 28, 6–27. [Google Scholar] [CrossRef]
- Patil, S.; Yadav, N.; Mousa, M.; Alzwiri, A.; Kassab, M.; Sahu, R.; Chuggani, S. Role of Female Reproductive Hormones Estrogen and Progesterone in Temporomandibular Disorder in Female Patients. J. Oral Res. Rev. 2015, 7, 41. [Google Scholar] [CrossRef]
- Ivković, N.; Racic, M.; Lecic, R.; Bozovic, D.; Kulic, M. Relationship between Symptoms of Temporomandibular Disorders and Estrogen Levels in Women With Different Menstrual Status. J. Oral Facial Pain Headache 2018, 32, 151–158. [Google Scholar] [CrossRef]
- Yuan, M.; Xie, Q.; Shen, P.; Yang, C. Do Sex Hormone Imbalances Contribute to Idiopathic Condylar Resorption? Int. J. Oral Maxillofac. Surg. 2021, 50, 1244–1248. [Google Scholar] [CrossRef] [PubMed]
- Yazici, H.; Taskin, M.I.; Guney, G.; Hismiogullari, A.A.; Arslan, E.; Tulaci, K.G. The Novel Relationship between Polycystic Ovary Syndrome and Temporomandibular Joint Disorders. J. Stomatol. Oral Maxillofac. Surg. 2021, 122, 544–548. [Google Scholar] [CrossRef]
- Vilanova, L.S.; Gonçalves, T.M.; Meirelles, L.; Garcia, R.C. Hormonal Fluctuations Intensify Temporomandibular Disorder Pain without Impairing Masticatory Function. Int. J. Prosthodont. 2015, 28, 72–74. [Google Scholar] [CrossRef]
- Lora, V.R.M.M.; Canales, G.D.l.T.; Gonçalves, L.M.; Meloto, C.B.; Barbosa, C.M.R. Prevalence of Temporomandibular Disorders in Postmenopausal Women and Relationship with Pain and HRT. Braz. Oral Res. 2016, 30, e100. [Google Scholar] [CrossRef] [PubMed]
- Ribeiro-Dasilva, M.C.; Fillingim, R.B.; Wallet, S.M. Estrogen-Induced Monocytic Response Correlates with TMD Pain: A Case Control Study. J. Dent. Res. 2017, 96, 285–291. [Google Scholar] [CrossRef] [PubMed]
- Babouei, M.; Farzin, M.; Vejdani, M.; Moayedi, I.; Ka, K.N.R.T.U.; Russia, K. Evaluating the Prevalence of Temporomandibular Joint Abnormalities in Postmenopausal Women. Rev. Latinoam. Hipertens. 2019, 14, 518–524. [Google Scholar]
- Fichera, G.; Polizzi, A.; Scapellato, S.; Palazzo, G.; Indelicato, F. Craniomandibular Disorders in Pregnant Women: An Epidemiological Survey. J. Funct. Morphol. Kinesiol. 2020, 5, 36. [Google Scholar] [CrossRef]
- Jedynak, B.; Jaworska-Zaremba, M.; Grzechocińska, B.; Chmurska, M.; Janicka, J.; Kostrzewa-Janicka, J. TMD in Females with Menstrual Disorders. Int. J. Environ. Res. Public. Health 2021, 18, 7263. [Google Scholar] [CrossRef]
- Mursu, E.; Yu, J.; Karjalainen, E.; Savukoski, S.; Niinimäki, M.; Näpänkangas, R.; Pesonen, P.; Pirttiniemi, P.; Raustia, A. Association of Climacterium with Temporomandibular Disorders at the Age of 46 Years—A Cross-Sectional Study. Acta Odontol. Scand. 2023, 81, 319–324. [Google Scholar] [CrossRef]
- Minervini, G.; Marrapodi, M.M.; La Verde, M.; Meto, A.; Siurkel, Y.; Ronsivalle, V.; Cicciù, M. Pregnancy Related Factors and Temporomandibular Disorders Evaluated through the Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) Axis II: A Cross Sectional Study. BMC Oral Health 2024, 24, 226. [Google Scholar] [CrossRef]
- LeResche, L.; Saunders, K.; Von Korff, M.R.; Barlow, W.; Dworkin, S.F. Use of Exogenous Hormones and Risk of Temporomandibular Disorder Pain. Pain 1997, 69, 153–160. [Google Scholar] [CrossRef]
- LeResche, L.; Mancl, L.; Sherman, J.J.; Gandara, B.; Dworkin, S.F. Changes in Temporomandibular Pain and Other Symptoms across the Menstrual Cycle. Pain 2003, 106, 253–261. [Google Scholar] [CrossRef]
- LeResche, L.; Sherman, J.J.; Huggins, K.; Saunders, K.; Mancl, L.A.; Lentz, G.; Dworkin, S.F. Musculoskeletal Orofacial Pain and Other Signs and Symptoms of Temporomandibular Disorders during Pregnancy: A Prospective Study. J. Orofac. Pain 2005, 19, 193–201. [Google Scholar]
- Dao, T.T.; Knight, K.; Ton-That, V. Modulation of Myofascial Pain by the Reproductive Hormones: A Preliminary Report. J. Prosthet. Dent. 1998, 79, 663–670. [Google Scholar] [CrossRef] [PubMed]
- Hatch, J.P.; Rugh, J.D.; Sakai, S.; Saunders, M.J. Is Use of Exogenous Estrogen Associated with Temporomandibular Signs and Symptoms? J. Am. Dent. Assoc. 1939 2001, 132, 319–326. [Google Scholar] [CrossRef] [PubMed]
- Sherman, J.J.; LeResche, L.; Mancl, L.A.; Huggins, K.; Sage, J.C.; Dworkin, S.F. Cyclic Effects on Experimental Pain Response in Women with Temporomandibular Disorders. J. Orofac. Pain 2005, 19, 133–143. [Google Scholar]
- Nekora-Azak, A.; Evlioglu, G.; Ceyhan, A.; Keskin, H.; Berkman, S.; Issever, H. Estrogen Replacement Therapy among Postmenopausal Women and Its Effects on Signs and Symptoms of Temporomandibular Disorders. Cranio J. Craniomandib. Pract. 2008, 26, 211–215. [Google Scholar] [CrossRef]
- Landi, N.; Manfredini, D.; Lombardi, I.; Casarosa, E.; Bosco, M. 17-Beta-Estradiol and Progesterone Serum Levels in Temporomandibular Disorder Patients. Minerva Stomatol. 2004, 53, 651–660. [Google Scholar]
- Landi, N.; Lombardi, I.; Manfredini, D.; Casarosa, E.; Biondi, K.; Gabbanini, M.; Bosco, M. Sexual Hormone Serum Levels and Temporomandibular Disorders. A Preliminary Study. Gynecol. Endocrinol. Off. J. Int. Soc. Gynecol. Endocrinol. 2005, 20, 99–103. [Google Scholar] [CrossRef]
- Zhang, X.; Rahman, M.; Bereiter, D.A. Estrogen Status and Trigeminal Ganglion Responses to Jaw Movement. J. Dent. Res. 2022, 101, 1075–1081. [Google Scholar] [CrossRef]
- Hornung, R.S.; Benton, W.L.; Tongkhuya, S.; Uphouse, L.; Kramer, P.R.; Averitt, D.L. Progesterone and Allopregnanolone Rapidly Attenuate Estrogen-Associated Mechanical Allodynia in Rats with Persistent Temporomandibular Joint Inflammation. Front. Integr. Neurosci. 2020, 14, 26. [Google Scholar] [CrossRef]
- Kroeff, G.P.H.; de Castro, J.M.; Braga, H.B.; Bosco, T.D.; de Oliveira, T.C.; de Sousa Morais, I.T.; Medeiros, L.F.; Caumo, W.; Stein, D.J.; Torres, I.L.S. Hormone Replacement Therapy Did Not Alleviate Temporomandibular Joint Inflammatory Pain in Ovariectomized Rats. Odontology 2024. [Google Scholar] [CrossRef]
- Chen, Q.; Zhang, W.; Sadana, N.; Chen, X. Estrogen Receptors in Pain Modulation: Cellular Signaling. Biol. Sex Differ. 2021, 12, 22. [Google Scholar] [CrossRef]
- Robinson, J.L.; Cass, K.; Aronson, R.; Choi, T.; Xu, M.; Buttenbaum, R.; Drissi, H.; Lu, H.H.; Chen, J.; Wadhwa, S. Sex Differences in the Estrogen-Dependent Regulation of Temporomandibular Joint Remodeling in Altered Loading. Osteoarthr. Cartil. 2017, 25, 533–543. [Google Scholar] [CrossRef] [PubMed]
- Xue, X.-T.; Zhang, T.; Cui, S.-J.; He, D.-Q.; Wang, X.-D.; Yang, R.-L.; Liu, D.-W.; Liu, Y.; Gan, Y.-H.; Kou, X.-X.; et al. Sexual Dimorphism of Estrogen-Sensitized Synoviocytes Contributes to Gender Difference in Temporomandibular Joint Osteoarthritis. Oral Dis. 2018, 24, 1503–1513. [Google Scholar] [CrossRef] [PubMed]
- Zhao, H.; Liu, S.; Ma, C.; Ma, S.; Chen, G.; Yuan, L.; Chen, L.; Zhao, H. Estrogen-Related Receptor γ Induces Angiogenesis and Extracellular Matrix Degradation of Temporomandibular Joint Osteoarthritis in Rats. Front. Pharmacol. 2019, 10, 1290. [Google Scholar] [CrossRef] [PubMed]
- Ye, T.; Sun, D.; Mu, T.; Chu, Y.; Miao, H.; Zhang, M.; Yang, H.; Liu, Q.; Lu, L.; Xing, X.; et al. Differential Effects of High-Physiological Oestrogen on the Degeneration of Mandibular Condylar Cartilage and Subchondral Bone. Bone 2018, 111, 9–22. [Google Scholar] [CrossRef]
- Abdrabuh, A.; Baljon, K.; Alyami, Y. Impact of Estrogen Therapy on Temporomandibular Joints of Rats: Histological and Hormone Analytical Study. Saudi Dent. J. 2021, 33, 608–613. [Google Scholar] [CrossRef]
- Mortazavi, N.; Tabatabaei, A.H.; Mohammadi, M.; Rajabi, A. Is Bruxism Associated with Temporomandibular Joint Disorders? A Systematic Review and Meta-Analysis. Evid. Based Dent. 2023, 24, 144. [Google Scholar] [CrossRef]
- Goulet, J.P.; Lund, J.P.; Montplaisir, J.Y.; Lavigne, G.J. Daily clenching, nocturnal bruxism, and stress and their association with TMD symptoms. J. Orofac. Pain 1993, 7, 120. [Google Scholar]
- Wetselaar, P.; Vermaire, E.J.H.; Lobbezoo, F.; Schuller, A.A. The prevalence of awake bruxism and sleep bruxism in the Dutch adult population. J. Oral Rehabilitation 2019, 46, 617–623. [Google Scholar] [CrossRef]



| Inclusion | Exclusion | |
|---|---|---|
| Population | ||
| Women of various ages suffering from TMDs. | Men of various ages suffering from TMDs. | |
| Intervention | ||
| Estrogen levels, e.g., endogenous estrogen levels, estrogen supplementation, hormone replacement therapy. | ||
| Comparison | ||
| Control group: women with normal estrogen levels, no estrogen supplementation, placebo, or no TMDs. | ||
| Outcome | ||
| Impact on the severity of TMDs symptoms, e.g., pain, limited mobility, sounds during movement in the joint (clicking), overall quality of life. | ||
| Study Design | ||
|
| Number of People and Group Information | Estrogen Levels | Measurement Unit in Researches | Converted Units ng/L | ||
|---|---|---|---|---|---|
| Patil et al. [32] | Severe cases of TMDs | 59 | 444.20 | pg/mL | 444.20 |
| Moderate cases of TMDs | 66 | 264.50 | 264.50 | ||
| Mild cases of TMDs | 75 | 199.80 | 199.80 | ||
| Total | 200 | 302.10 | 302.10 | ||
| Ivković et al. [33] | Normally cycling women | TMDs n–28 (56%) Total n–50 | 0.10 | ng/mL | 100 |
| Pregnant women | TMDs n–23 (51%) Total n–45 | 14.67 | 14,670 | ||
| Women in surgical menopause | TMDs n–13 (43%) Total n–30 | 0.02 | 20 | ||
| Yuan et al. [34] | Idiopathic condylar resorption | 80 | 36.93 | pg/mL | 36.93 |
| Disc displacement | 259 | 34.36 | 34.36 | ||
| Yazici et al. [35] | Control group | TMDs n–2 (7%) Total n–30 | 44.3 | ng/mL | 44,300 |
| Polycystic ovary syndrome | TMDs n–23 (51%) Total n–45 | 47.6 | 47,600 | ||
| Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Total | |
|---|---|---|---|---|---|---|---|---|
| Patil et al. 2015 [32] | 2 | 0 | 1 | 1 | 1 | 2 | 2 | 9 |
| Vilanova et al. 2015 [36] | 1 | 2 | 1 | 0 | 2 | 1 | 1 | 8 |
| Lora et al. 2016 [37] | 2 | 2 | 1 | 0 | 2 | 1 | 2 | 10 |
| Ribeiro-Dasilva et al. 2017 [38] | 1 | 2 | 1 | 0 | 2 | 2 | 2 | 10 |
| Ivković et al. 2018 [33] | 2 | 2 | 1 | 2 | 2 | 2 | 2 | 13 |
| Babouei et al. 2019 [39] | 1 | 2 | 1 | 0 | 2 | 1 | 1 | 8 |
| Fichera et al. 2020 [40] | 2 | 2 | 1 | 0 | 1 | 1 | 2 | 9 |
| Yuan et al. 2021 [34] | 2 | 0 | 2 | 1 | 1 | 2 | 2 | 10 |
| Yazici et al. 2021 [35] | 1 | 2 | 1 | 0 | 2 | 2 | 2 | 10 |
| Jedynak et al. 2021 [41] | 2 | 2 | 1 | 0 | 2 | 2 | 2 | 11 |
| Mursu et al. 2023 [42] | 2 | 2 | 1 | 0 | 2 | 1 | 2 | 10 |
| Minervini et al. 2024 [43] | 1 | 0 | 1 | 0 | 1 | 1 | 2 | 6 |
| Author | Conclusion | Evaluation | Summary of Estrogen’s Effect on TMDs |
|---|---|---|---|
| LeResche et al., 1997 [44] * | “These results suggest that female reproductive hormones may play an etiologic role in orofacial pain”. | 7 | Positive |
| Dao et al., 1998 [47] * | “(…)Evidence supporting the link between estrogen, nitric oxide, and inflammatory processes is presented”. | 11 | Positive |
| Hatch et al., 2001 [48] * | “Estrogen replacement therapy does not place women at increased risk of developing TMDs”. | 8 | Negative |
| LeResche et al., 2003 [45] * | “These results suggest that TMD pain in women is highest at times of lowest estrogen, but rapid estrogen change may also be associated with increased pain”. | 12 | Positive |
| Landi et al., 2004 [51] * | “The results of this study suggest that high serum estrogens levels might be implicated in the physiopathology of temporomandibular joint disorders, since subjects with these pathologies showed significantly higher serum levels with respect to a group of healthy controls”. | 10 | Positive |
| LeResche et al., 2005 [46] * | “Musculoskeletal orofacial pain and related symptoms appear to improve over the course of pregnancy. This improvement occurs in the presence of increased joint laxity and is not paralleled by improvements in psychological distress. Thus, it was concluded that the improvement in pain is most likely associated with the dramatic hormonal changes occurring during pregnancy”. | 8 | Positive |
| Landi et al., 2005 [52] * | “Considering the multifactorial etiology of TMD and the hypothesis that some joint tissues (e.g., bone, cartilage, collagen, proteins) could be a target for sexual hormones, these data suggest that high serum estrogen levels might be implicated in the physiopathology of TMD”. | 11 | Positive |
| Sherman et al., 2005 [49] * | “Phase-related differences in experimental pain response were not strong and were more often found for experimental stimuli with greater clinical relevance (ie, palpation pain) compared with an ischemic pain task”. | 12 | Negative |
| Nekora-Azak et al., 2008 [50] * | “There was no significant difference found in the signs and symptoms of TMD between postmenopausal women using hormone therapy and those not using postmenopausal hormones. There was no association between the use of postmenopausal hormones and the signs and symptoms of TMD in this study”. | 8 | Negative |
| Patil et al., 2015 [32] | “Increasing serum levels of estrogen and progesterone with increasing grade of severity of TMD suggest a role of these hormones as etiological factors for TMD”. | 9 | Positive |
| Vilanova et al., 2015 [36] | “Hormonal fluctuations intensify pain in women with symptomatic TMD without impairing mastication”. | 8 | Positive |
| Lora et al., 2016 [37] | “There was a similar percentage of TMD and non TMD patients; moreover, the use of exogenous hormones was no associated with TMD, suggesting that there is no influence on the pain threshold”. | 10 | Negative |
| Ribeiro-Dasilva et al., 2017 [38] | “These data suggest that an estrogen-induced hyperinflammatory phenotype in women with TMD may at least in part contribute to heightened clinical pain, perhaps via central sensitization”. | 10 | Positive |
| Ivković et al., 2018 [33] | “TMD signs and symptoms may be modulated and sustained by estrogen levels. (…) Regulating the level and variations of estrogen across the hormonal cycle could be a promising approach for the treatment of TMD” | 13 | Positive |
| Babouei et al., 2019 [39] | “In the results of this study, it was found that the indices of pain in (TMJ, decuple masseter muscles and on mandibular movements) in women are most severe when estrogen levels are at a minimum; it was also found that decreased estrogen secretion in postmenopausal phase (…) caused increased inflammation and reduced development and progress of TMJ tissue components which is the reason for increased incidence and severity of all five symptoms of TMD based on the Helkimo’s clinical index (…)”. | 8 | Positive |
| Fichera et al., 2020 [40] | “Female subjects in pregnancy status could be more susceptible to TMD due to a physiological increment of estrogenic hormones levels. However, further studies are needed to better understand the role of TMD during pregnancy”. | 9 | Positive |
| Yuan et al., 2021 [34] | “(…) there were no differences in serum E2 levels or the levels of other sex hormones between female ICR and DD patients”. | 10 | Negative |
| Yazici et al., 2021 [35] | “In the comparison of estrogen levels, no significant difference was found between groups. -Information from the results section”. | 10 | Negative |
| Jedynak et al., 2021 [41] | “(…) In women with TMD symptoms, their medical history should be extended to include the diagnosis of female hormone disorders”. | 11 | Positive |
| Mursu et al., 2023 [42] | “In conclusion, among females at the age of 46 years, climacterium seems to be associated with TMD by increasing pain on palpation in TMJs and subjective symptoms and clinical signs indicating degenerative changes in TMJs when using DC/TMD”. | 10 | Positive |
| Minervini et al., 2024 [43] | “In conclusion, our study identified significant associations between psychosomatic and psychological symptoms with variables like age and pregnancy trimester in pregnant women”. | 6 | Positive |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zieliński, G.; Pająk-Zielińska, B. Association between Estrogen Levels and Temporomandibular Disorders: An Updated Systematic Review. Int. J. Mol. Sci. 2024, 25, 9867. https://doi.org/10.3390/ijms25189867
Zieliński G, Pająk-Zielińska B. Association between Estrogen Levels and Temporomandibular Disorders: An Updated Systematic Review. International Journal of Molecular Sciences. 2024; 25(18):9867. https://doi.org/10.3390/ijms25189867
Chicago/Turabian StyleZieliński, Grzegorz, and Beata Pająk-Zielińska. 2024. "Association between Estrogen Levels and Temporomandibular Disorders: An Updated Systematic Review" International Journal of Molecular Sciences 25, no. 18: 9867. https://doi.org/10.3390/ijms25189867
APA StyleZieliński, G., & Pająk-Zielińska, B. (2024). Association between Estrogen Levels and Temporomandibular Disorders: An Updated Systematic Review. International Journal of Molecular Sciences, 25(18), 9867. https://doi.org/10.3390/ijms25189867








