The Synergistic Benefit of Combination Strategies Targeting Tumor Cell Polyamine Homeostasis
Abstract
1. Introduction
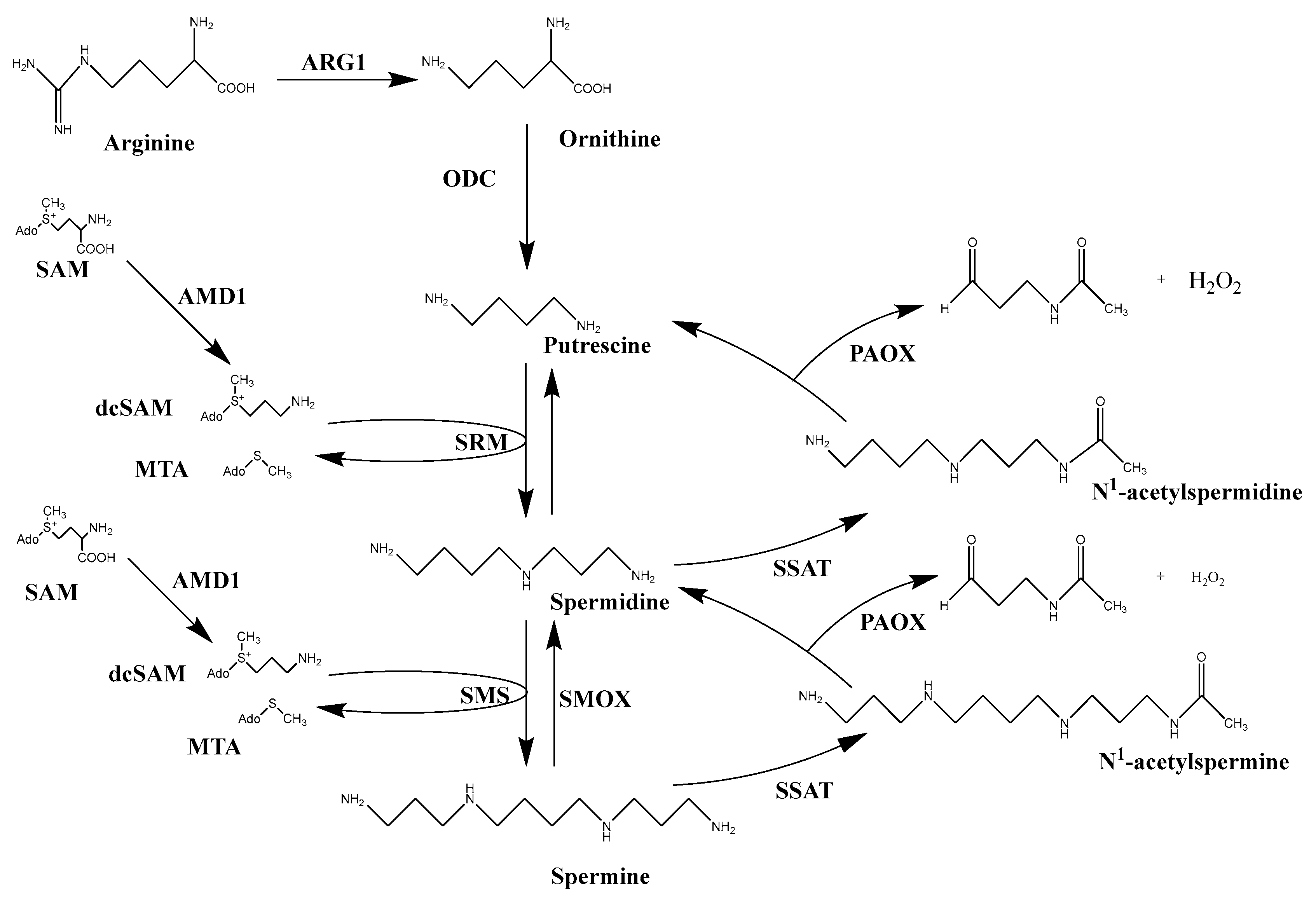
2. Polyamine Transport
3. Polyamine Biosynthesis
4. Polyamine Catabolism
5. Polyamine Function
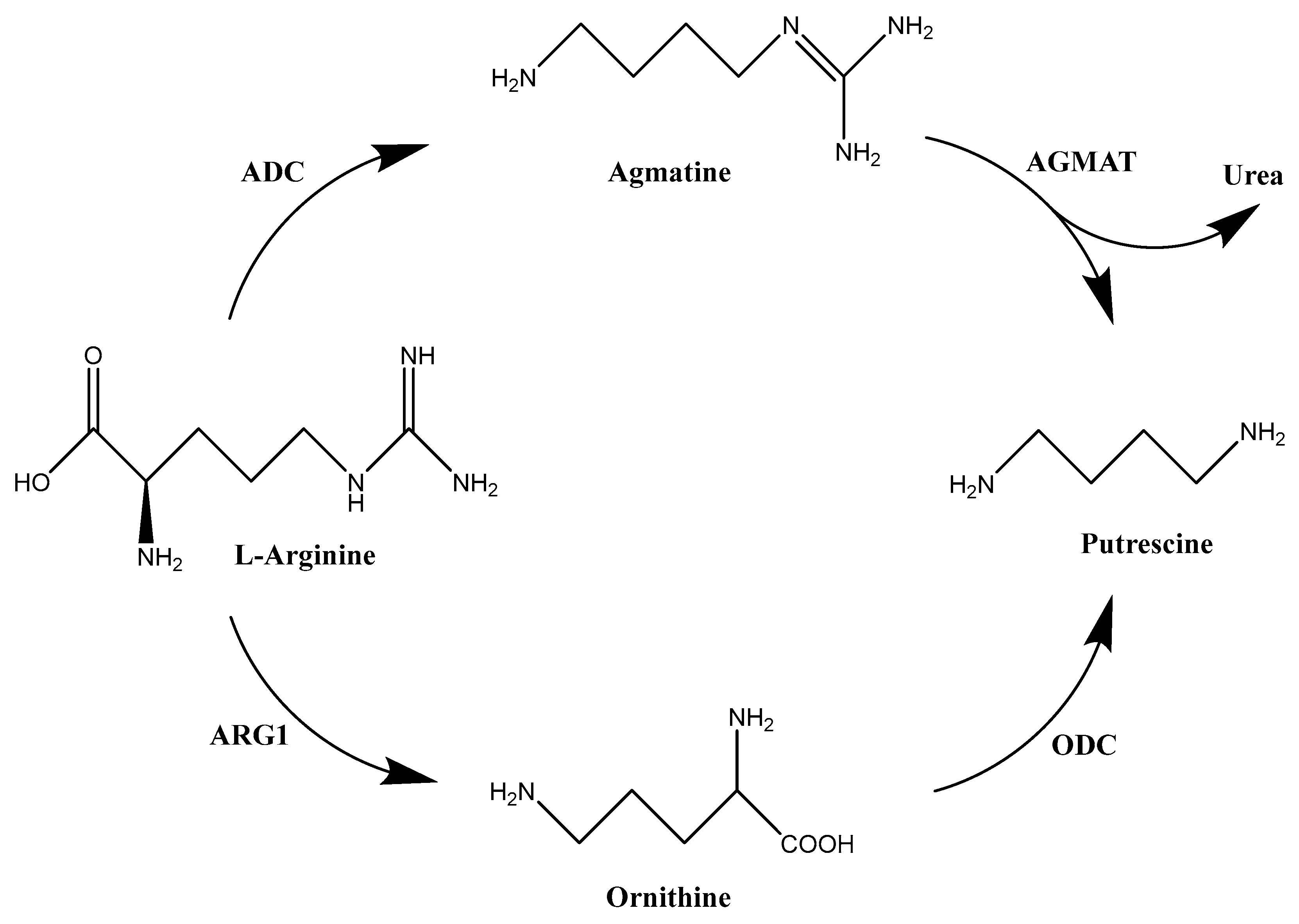
6. Polyamine Deprivation as an Anticancer Strategy: Arginine Deprivation and Agmatine
7. Polyamine Depletion as an Anticancer Strategy: Use of Enzyme Inhibitors
| Name | Structure | Reference |
|---|---|---|
| DFMO (Difluoromethylornithine) | 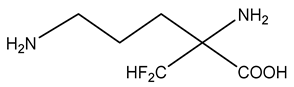 | [92] |
| MGBG (Methylglyoxal (bis)guanylhydrazone) |  | [97] |
| SAM486A (CGP48664) | 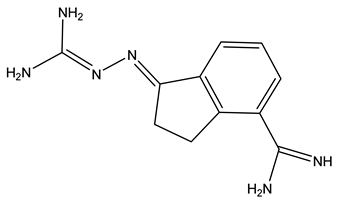 | [100] |
| S-adenosyl-3-thio-1,8-diaminooctane (AdoDATO) | 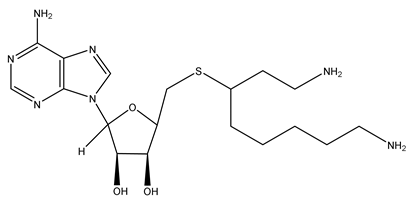 | [104] |
| S-adenosyl-1,12-diamino-3-thio-9-azadodecane (AdoDATAD) | 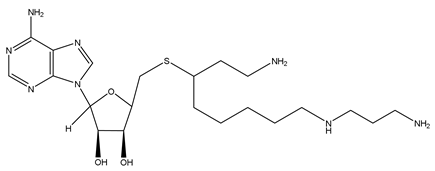 | [105] |
| MDL72527 |  | [109] |
| JNJ-1289 | 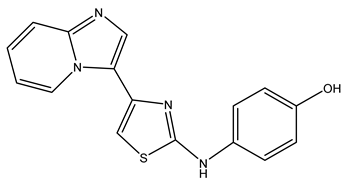 | [111] |
| 2,11-Met2-Spm | 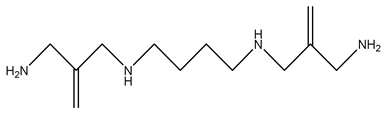 | [113] |
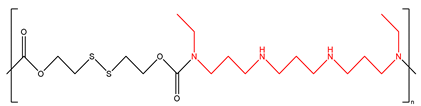
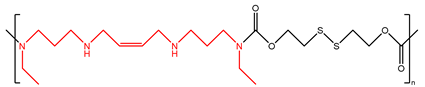
8. Synthetic Polyamine Analogues for Anticancer Treatment
| Name | Structure | Reference |
|---|---|---|
| BENSpm |  | [116] |
| BESpm | 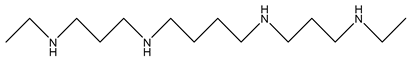 | [117] |
| CPENSpm | 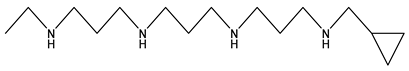 | [122] |
| PENSpm | 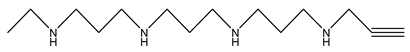 | [122] |
| PG-11047 | 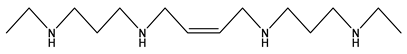 | [125] |
| PG-11093 | 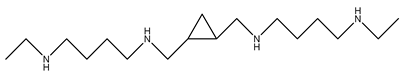 | [126] |
| PG-11144 | 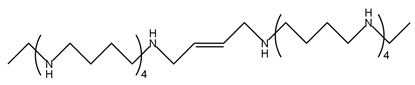 | [132] |
| SBP-101 (ivospemin) | 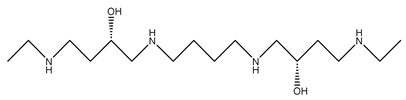 | [140] |
9. Polyamine Transport Inhibitors
10. Synergistic Polyamine Combination Therapeutic Strategies
11. Future Perspectives and Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Benamouzig, R.; Mahé, S.; Luengo, C.; Rautureau, J.; Tomé, D. Fasting and postprandial polyamine concentrations in the human digestive lumen. Am. J. Clin. Nutr. 1997, 65, 766–770. [Google Scholar] [CrossRef]
- Cohen, S.S. A Guide to the Polyamines; Oxford University Press: New York, NY, USA, 1998. [Google Scholar]
- Smirnov, I.V.; Dimitrov, S.I.; Makarov, V.L. Polyamine-DNA Interactions. Condensation of Chromatin and Naked DNA. J. Biomol. Struct. Dyn. 1988, 5, 1149–1161. [Google Scholar] [CrossRef] [PubMed]
- Dever, T.E.; Ivanov, I.P. Roles of polyamines in translation. J. Biol. Chem. 2018, 293, 18719–18729. [Google Scholar] [CrossRef] [PubMed]
- Pegg, A.E. Functions of Polyamines in Mammals. J. Biol. Chem. 2016, 291, 14904–14912. [Google Scholar] [CrossRef]
- Bardócz, S.; Duguid, T.J.; Brown, D.S.; Grant, G.; Pusztai, A.; White, A.; Ralph, A. The importance of dietary polyamines in cell regeneration and growth. Br. J. Nutr. 1995, 73, 819–828. [Google Scholar] [CrossRef] [PubMed]
- Milovic, V. Polyamines in the gut lumen: Bioavailability and biodistribution. Eur. J. Gastroenterol. Hepatol. 2001, 13, 1021–1025. [Google Scholar] [CrossRef]
- Pegg, A.E. Regulation of ornithine decarboxylase. J. Biol. Chem. 2006, 281, 14529–14532. [Google Scholar] [CrossRef] [PubMed]
- Kusano, T.; Berberich, T.; Tateda, C.; Takahashi, Y. Polyamines: Essential factors for growth and survival. Planta 2009, 228, 367–381. [Google Scholar] [CrossRef] [PubMed]
- Zwighaft, Z.; Aviram, R.; Shalev, M.; Rousso-Noori, L.; Kraut-Cohen, J.; Golik, M.; Brandis, A.; Reinke, H.; Aharoni, A.; Kahana, C.; et al. Circadian Clock Control by Polyamine Levels through a Mechanism that Declines with Age. Cell Metab. 2015, 22, 874–885. [Google Scholar] [CrossRef] [PubMed]
- Bello-Fernandez, C.; Packham, G.; Cleveland, J.L. The ornithine decarboxylase gene is a transcriptional target of c-Myc. Proc. Natl. Acad. Sci. USA 1993, 90, 7804–7808. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Dang, C.V. MYC on the Path to Cancer. Cell 2012, 149, 22–35. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Casero, R.A., Jr.; Woster, P.M. Recent Advances in the Development of Polyamine Analogues as Antitumor Agents. J. Med. Chem. 2009, 52, 4551–4573. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Streif, R.R.; Bender, J.F. Phase 1 study of N1–N11-diethylnorspermine (DENSPM) administered TID for 6 days in patients with advanced malignancies. Invest. New Drugs 2001, 19, 29–39. [Google Scholar] [CrossRef] [PubMed]
- Wolff, A.C.; Armstrong, D.K.; Fetting, J.H.; Carducci, M.K.; Riley, C.D.; Bender, J.F.; A Casero, R.; E Davidson, N. A Phase II study of the polyamine analog N1,N11-diethylnorspermine (DENSpm) daily for five days every 21 days in patients with previously treated metastatic breast cancer. Clin. Cancer Res. 2003, 9 Pt 1, 5922–5928. [Google Scholar]
- Casero, R.A., Jr.; Stewart, T.M.; Pegg, A.E. Polyamine metabolism and cancer: Treatments, challenges and opportunities. Nat. Rev. Cancer 2018, 18, 681–695. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Poulin, R.; Casero, R.A.; Soulet, D. Recent advances in the molecular biology of metazoan polyamine transport. Amino Acids 2012, 42, 711–723. [Google Scholar] [CrossRef]
- Soulet, D.; Gagnon, B.; Rivest, S.; Audette, M.; Poulin, R. A Fluorescent Probe of Polyamine Transport Accumulates into Intracellular Acidic Vesicles via a Two-step Mechanism. J. Biol. Chem. 2004, 279, 49355–49366. [Google Scholar] [CrossRef]
- Belting, M.; Persson, S.; Fransson, L.A. Proteoglycan involvement in polyamine uptake. Biochem. J. 1999, 338, 317–323. [Google Scholar] [CrossRef]
- Belting, M.; Mani, K.; Jönsson, M.; Cheng, F.; Sandgren, S.; Jonsson, S.; Ding, K.; Delcros, J.-G.; Fransson, L. Glypican-1 Is a Vehicle for Polyamine Uptake in Mammalian Cells. J. Biol. Chem. 2003, 278, 47181–47189. [Google Scholar] [CrossRef] [PubMed]
- Uemura, T.; Stringer, D.E.; Blohm-Mangone, K.A.; Gerner, E.W. Polyamine transport is mediated by both endocytic and solute carrier transport mechanisms in the gastrointestinal tract. Am. J. Physiol. Liver Physiol. 2010, 299, G517–G522. [Google Scholar] [CrossRef] [PubMed]
- Uemura, T.; Yerushalmi, H.F.; Tsaprailis, G.; Stringer, D.E.; Pastorian, K.E.; Hawel, L.; Byus, C.V.; Gerner, E.W. Identification and Characterization of a Diamine Exporter in Colon Epithelial Cells. J. Biol. Chem. 2008, 283, 26428–26435. [Google Scholar] [CrossRef]
- Van Veen, S.; Martin, S.; Haute, C.V.D.; Benoy, V.; Lyons, J.; Vanhoutte, R.; Kahler, J.P.; Decuypere, J.-P.; Gelders, G.; Lambie, E.; et al. ATP13A2 deficiency disrupts lysosomal polyamine export. Nature 2020, 578, 419–424. [Google Scholar] [CrossRef] [PubMed]
- Sekhar, V.; Andl, T.; Phanstiel, O. ATP13A3 facilitates polyamine transport in human pancreatic cancer cells. Sci. Rep. 2022, 12, 4045. [Google Scholar] [CrossRef]
- Hamouda, N.N.; Haute, C.V.D.; Vanhoutte, R.; Sannerud, R.; Azfar, M.; Mayer, R.; Calabuig, C.; Swinnen, J.V.; Agostinis, P.; Baekelandt, V.; et al. ATP13A3 is a major component of the enigmatic mammalian polyamine transport system. J. Biol. Chem. 2021, 296, 100182. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Van Veen, S.; Kourti, A.; Ausloos, E.; Van Asselberghs, J.; Haute, C.V.D.; Baekelandt, V.; Eggermont, J.; Vangheluwe, P. ATP13A4 Upregulation Drives the Elevated Polyamine Transport System in the Breast Cancer Cell Line MCF7. Biomolecules 2023, 13, 918. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Hiasa, M.; Miyaji, T.; Haruna, Y.; Takeuchi, T.; Harada, Y.; Moriyama, S.; Yamamoto, A.; Omote, H.; Moriyama, Y. Identification of a mammalian vesicular polyamine transporter. Sci. Rep. 2014, 4, 6836. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Fredriksson, R.; Sreedharan, S.; Nordenankar, K.; Alsiö, J.; Lindberg, F.A.; Hutchinson, A.; Eriksson, A.; Roshanbin, S.; Ciuculete, D.M.; Klockars, A.; et al. The polyamine transporter Slc18b1(VPAT) is important for both short and long time memory and for regulation of polyamine content in the brain. PLoS Genet. 2019, 15, e1008455. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Cervelli, M.; Pietropaoli, S.; Signore, F.; Amendola, R.; Mariottini, P. Polyamines metabolism and breast cancer: State of the art and perspectives. Breast Cancer Res. Treat. 2014, 148, 233–248. [Google Scholar] [CrossRef]
- Gilmour, S.K. Polyamines and nonmelanoma skin cancer. Toxicol. Appl. Pharmacol. 2007, 224, 249–256. [Google Scholar] [CrossRef]
- Upp, J.R., Jr.; Saydjari, R.; Townsend, C.M., Jr.; Singh, P.; Barranco, S.C.; Thompson, J.C. Polyamine Levels and Gastrin Receptors in Colon Cancers. Ann. Surg. 1988, 207, 662–669. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Singh, K.; Gobert, A.P.; Coburn, L.A.; Barry, D.P.; Allaman, M.; Asim, M.; Luis, P.B.; Schneider, C.; Milne, G.L.; Boone, H.H.; et al. Dietary Arginine Regulates Severity of Experimental Colitis and Affects the Colonic Microbiome. Front. Cell. Infect. Microbiol. 2019, 9, 66. [Google Scholar] [CrossRef]
- Russell, D.H.; Snyder, S.H. Amine synthesis in regenerating rat liver: extremely rapid turnover of ornithine decarboxylase . Mol. Pharmacol. 1969, 5, 253–262. [Google Scholar]
- Zhao, B.; Butler, A.P. Core promoter involvement in the induction of rat ornithine decarboxylase by phorbol esters. Mol. Carcinog. 2001, 32, 92–99. [Google Scholar] [CrossRef]
- Nowotarski, S.L.; Shantz, L.M. Cytoplasmic accumulation of the RNA-binding protein HuR stabilizes the ornithine decarboxylase transcript in a murine nonmelanoma skin cancer model. J. Biol. Chem. 2010, 285, 31885–31894. [Google Scholar] [CrossRef]
- Shantz, L.M. Transcriptional and translational control of ornithine decarboxylase during Ras transformation. Biochem. J. 2004, 377, 257–264. [Google Scholar] [CrossRef]
- Wallon, U.M.; Persson, L.; Heby, O. Regulation of ornithine decarboxylase during cell growth. Changes in the stability and translatability of the mRNA, and in the turnover of the protein. Mol. Cell. Biochem. 1995, 146, 39–44. [Google Scholar] [CrossRef]
- Moinard, C.; Cynober, L.; Debandt, J. Polyamines: Metabolism and implications in human diseases. Clin. Nutr. 2005, 24, 184–197. [Google Scholar] [CrossRef]
- Zhu, C.; Lang, D.W.; Coffino, P. Antizyme2 Is a Negative Regulator of Ornithine Decarboxylase and Polyamine Transport. J. Biol. Chem. 1999, 274, 26425–26430. [Google Scholar] [CrossRef]
- Ivanov, I.P.; Rohrwasser, A.; Terreros, D.A.; Gesteland, R.F.; Atkins, J.F. Discovery of a spermatogenesis stage-specific ornithine decarboxylase antizyme: Antizyme 3. Proc. Natl. Acad. Sci. USA 2000, 97, 4808–4813. [Google Scholar] [CrossRef]
- Fraser, A.V.; Goodwin, A.C.; Hacker-Prietz, A.; Sugar, E.; Woster, P.M.; Casero, R.A. Knockdown of ornithine decarboxylase antizyme 1 causes loss of uptake regulation leading to increased N 1, N 11-bis(ethyl)norspermine (BENSpm) accumulation and toxicity in NCI H157 lung cancer cells. Amino Acids 2012, 42, 529–538. [Google Scholar] [CrossRef][Green Version]
- Kahana, C. Antizyme and antizyme inhibitor, a regulatory tango. Cell. Mol. Life Sci. 2009, 66, 2479–2488. [Google Scholar] [CrossRef] [PubMed]
- Zhang, M.; Pickart, C.M.; Coffino, P. Determinants of proteasome recognition of ornithine decarboxylase, a ubiquitin-independent substrate. EMBO J. 2003, 22, 1488–1496. [Google Scholar] [CrossRef] [PubMed]
- Bachmann, A.S.; Geerts, D. Polyamine synthesis as a target of MYC oncogenes. J. Biol. Chem. 2018, 293, 18757–18769. [Google Scholar] [CrossRef]
- Wu, H.-Z.; Xiao, J.-Q.; Xiao, S.-S.; Cheng, Y. KRAS: A Promising Therapeutic Target for Cancer Treatment. Curr. Top. Med. Chem. 2019, 19, 2081–2097. [Google Scholar] [CrossRef] [PubMed]
- Morris, S.M. Arginine Metabolism Revisited. J. Nutr. 2016, 146, 2579S–2586S. [Google Scholar] [CrossRef] [PubMed]
- Mistry, S.K.; Burwell, T.J.; Chambers, R.M.; Rudolph-Owen, L.; Spaltmann, F.; Cook, W.J.; Morris, S.M. Cloning of human agmatinase. An alternate path for polyamine synthesis induced in liver by hepatitis B virus. Am. J. Physiol. Liver Physiol. 2002, 282, G375–G381. [Google Scholar] [CrossRef]
- Barua, S.; Kim, J.Y.; Kim, J.Y.; Lee, J.E. Therapeutic Effect of Agmatine on Neurological Disease: Focus on Ion Channels and Receptors. Neurochem. Res. 2019, 44, 735–750. [Google Scholar] [CrossRef] [PubMed]
- Pegg, A.E. S-Adenosylmethionine decarboxylase. Essays Biochem. 2009, 46, 25–46. [Google Scholar]
- Bale, S.; Lopez, M.M.; Makhatadze, G.I.; Fang, Q.; Pegg, A.E.; Ealick, S.E. Structural Basis for Putrescine Activation of Human S-Adenosylmethionine Decarboxylase. Biochemistry 2008, 47, 13404–13417. [Google Scholar] [CrossRef] [PubMed]
- Berntsson, P.S.; Alm, K.; Oredsson, S.M. Half-Lives of Ornithine Decarboxylase and S-Adenosylmethionine Decarboxylase Activities during the Cell Cycle of Chinese Hamster Ovary Cells. Biochem. Biophys. Res. Commun. 1999, 263, 13–16. [Google Scholar] [CrossRef]
- Zabala-Letona, A.; Arruabarrena-Aristorena, A.; Martín-Martín, N.; Fernandez-Ruiz, S.; Sutherland, J.D.; Clasquin, M.; Tomas-Cortazar, J.; Jimenez, J.; Torres, I.; Quang, P.; et al. mTORC1-dependent AMD1 regulation sustains polyamine metabolism in prostate cancer. Nature 2017, 547, 109–113, Erratum in Nature 2018, 554, 554. https://doi.org/10.1038/nature25470. [Google Scholar] [CrossRef] [PubMed]
- Wahlfors, J.; Alhonen, L.; Kauppinen, L.; Hyvönen, T.; Jänne, J.; Eloranta, T.O. Human Spermidine Synthase: Cloning and Primary Structure. DNA Cell Biol. 1990, 9, 103–110. [Google Scholar] [CrossRef] [PubMed]
- Korhonen, V.-P.; Halmekytö, M.; Kauppinen, L.; Myöhänen, S.; Wahlfors, J.; Keinänen, T.; Hyvönen, T.; Alhonen, L.; Eloranta, T.; Jänne, J. Molecular Cloning of a cDNA Encoding Human Spermine Synthase. DNA Cell Biol. 1995, 14, 841–847. [Google Scholar] [CrossRef] [PubMed]
- Ikeguchi, Y.; Bewley, M.C.; Pegg, A.E. Aminopropyltransferases: Function, Structure and Genetics. J. Biochem. 2006, 139, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Dante, R.; Anaud, M.; Niveleau, A. Effects of 5′deoxy-5′-methylthioadenosine on the metabolism of S-adenosylmethionine. Biochem. Biophys. Res. Commun. 1983, 114, 214–221. [Google Scholar] [CrossRef] [PubMed]
- Della Ragione, F.; Russo, G.; Oliva, A.; Mastropietro, S.; Mancini, A.; Borrelli, A.; A Casero, R.; Iolascon, A.; Zappia, V. 5′-Deoxy-5′-methylthioadenosine phosphorylase and p16INK4 deficiency in multiple tumor cell lines. Oncogene 1995, 10, 827–833. [Google Scholar] [PubMed]
- Casero, R.A., Jr.; Pegg, A.E. Spermidine/spermine N1-acetyltransferase—The turning point in polyamine metabolism. FASEB J. 1993, 7, 653–661. [Google Scholar] [CrossRef] [PubMed]
- Wu, T.; Yankovskaya, V.; McIntire, W.S. Cloning, Sequencing, and Heterologous Expression of the Murine Peroxisomal Flavoprotein, N1-Acetylated Polyamine Oxidase. J. Biol. Chem. 2003, 278, 20514–20525. [Google Scholar] [CrossRef]
- Vujcic, S.; Liang, P.; Diegelman, P.; Kramer, D.L.; Porter, C.W. Genomic identification and biochemical characterization of the mammalian polyamine oxidase involved in polyamine back-conversion. Biochem. J. 2003, 370, 19–28. [Google Scholar] [CrossRef]
- Wang, Y.; Devereux, W.; Woster, P.M.; Stewart, T.M.; Hacker, A.; A Casero, R. Cloning and characterization of a human polyamine oxidase that is inducible by polyamine analogue exposure. Cancer Res. 2001, 61, 5370–5373. [Google Scholar]
- Wang, Y.; Murray-Stewart, T.; Devereux, W.; Hacker, A.; Frydman, B.; Woster, P.M.; Casero, R.A., Jr. Properties of purified recombinant human polyamine oxidase, PAOh1/SMO. Biochem. Biophys. Res. Commun. 2003, 304, 605–611. [Google Scholar] [CrossRef] [PubMed]
- Kashiwagi, K.; Igarashi, K. Molecular Characteristics of Toxicity of Acrolein Produced from Spermine. Biomolecules 2023, 13, 298. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Murray-Stewart, T.; Wang, Y.; Goodwin, A.; Hacker, A.; Meeker, A.; Casero, R.A., Jr. Nuclear localization of human spermine oxidase isoforms—Possible implications in drug response and disease etiology. FEBS J. 2008, 275, 2795–2806. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
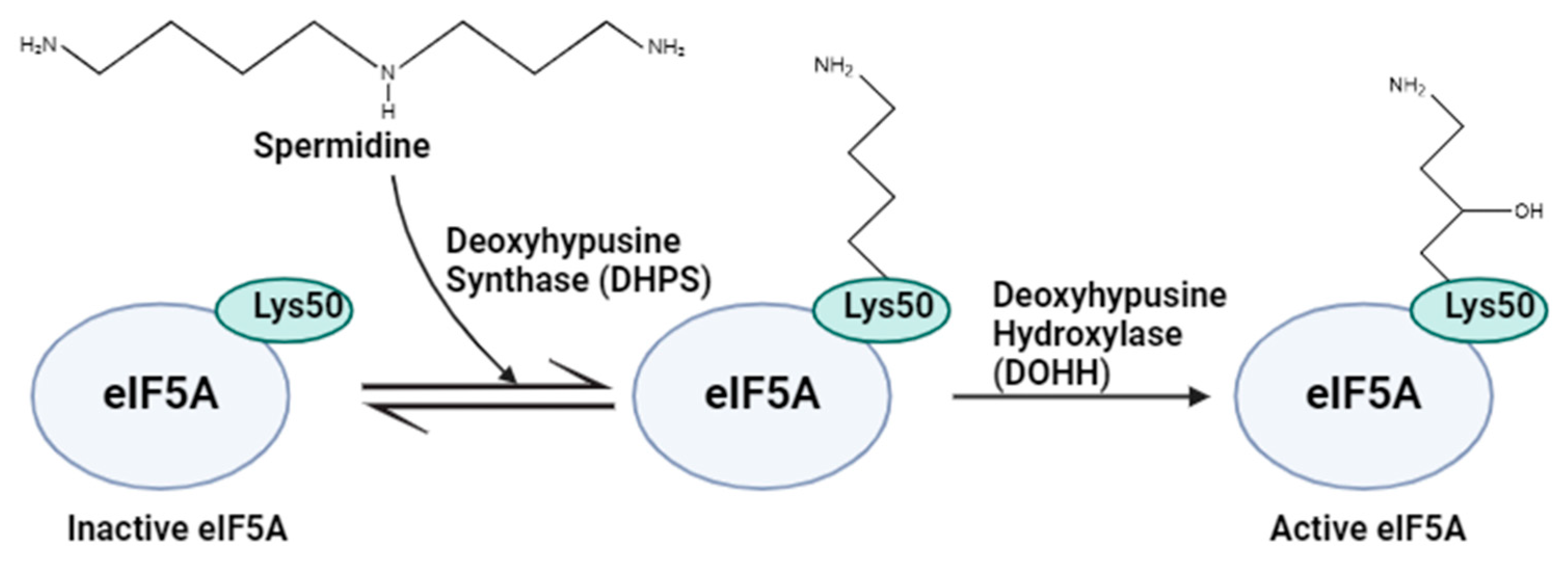
- Cooper, H.L.; Park, M.H.; Folk, J. Posttranslational formation of hypusine in a single major protein occurs generally in growing cells and is associated with activation of lymphocyte growth. Cell 1982, 29, 791–797. [Google Scholar] [CrossRef] [PubMed]
- Park, M.H.; Wolff, E.C.; E Folk, J. Hypusine: Its post-translational formation in eukaryotic initiation factor 5A and its potential role in cellular regulation. Biofactors 1993, 4, 95–104. [Google Scholar] [PubMed]
- Gutierrez, E.; Shin, B.-S.; Woolstenhulme, C.J.; Kim, J.-R.; Saini, P.; Buskirk, A.R.; Dever, T.E. eIF5A Promotes Translation of Polyproline Motifs. Mol. Cell 2013, 51, 35–45. [Google Scholar] [CrossRef]
- Pálfi, P.; Bakacsy, L.; Kovács, H.; Szepesi, Á. Hypusination, a Metabolic Posttranslational Modification of eIF5A in Plants during Development and Environmental Stress Responses. Plants 2021, 10, 1261. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Reinberg, D. Transcription regulation by histone methylation: Interplay between different covalent modifications of the core histone tails. Genes Dev. 2001, 15, 2343–2360. [Google Scholar] [CrossRef] [PubMed]
- Frostesjö, L.; Holm, I.; Grahn, B.; Page, A.W.; Bestor, T.H.; Heby, O. Interference with DNA Methyltransferase Activity and Genome Methylation during F9 Teratocarcinoma Stem Cell Differentiation Induced by Polyamine Depletion. J. Biol. Chem. 1997, 272, 4359–4366. [Google Scholar] [CrossRef]
- Yamamoto, D.; Shima, K.; Matsuo, K.; Nishioka, T.; Chen, C.Y.; Hu, G.-F.; Sasaki, A.; Tsuji, T. Ornithine Decarboxylase Antizyme Induces Hypomethylation of Genome DNA and Histone H3 Lysine 9 Dimethylation (H3K9me2) in Human Oral Cancer Cell Line. PLoS ONE 2010, 5, e12554. [Google Scholar] [CrossRef]
- Fukui, T.; Soda, K.; Takao, K.; Rikiyama, T. Extracellular Spermine Activates DNA Methyltransferase 3A and 3B. Int. J. Mol. Sci. 2019, 20, 1254. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Feun, L.; You, M.; Wu, C.J.; Kuo, M.T.; Wangpaichitr, M.; Spector, S.; Savaraj, N. Arginine Deprivation as a Targeted Therapy for Cancer. Curr. Pharm. Des. 2008, 14, 1049–1057. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Buga, G.M.; Wei, L.H.; Bauer, P.M.; Fukuto, J.M.; Ignarro, L.J. NG-hydroxy-l-arginine and nitric oxide inhibit Caco-2 tumor cell proliferation by distinct mechanisms. Am. J. Physiol. Integr. Comp. Physiol. 1998, 275, R1256–R1264. [Google Scholar] [CrossRef] [PubMed]
- Bauer, P.M.; Buga, G.M.; Fukuto, J.M.; Pegg, A.E.; Ignarro, L.J. Nitric Oxide Inhibits Ornithine Decarboxylase viaS-Nitrosylation of Cysteine 360 in the Active Site of the Enzyme. J. Biol. Chem. 2001, 276, 34458–34464. [Google Scholar] [CrossRef] [PubMed]
- Singh, R.; Pervin, S.; Karimi, A.; Cederbaum, S.; Chaudhuri, G. Arginase activity in human breast cancer cell lines: N(omega)-hydroxy-L-arginine selectively inhibits cell proliferation and induces apoptosis in MDA-MB-468 cells. Cancer Res. 2000, 60, 3305–3312. [Google Scholar] [PubMed]
- Chang, C.I.; Liao, J.C.; Kuo, L. Macrophage arginase promotes tumor cell growth and suppresses nitric oxide-mediated tumor cytotoxicity. Cancer Res. 2001, 61, 1100–1106. [Google Scholar] [PubMed]
- Erbas, H.; Bal, O.; Cakir, E. Effect of Rosuvastatin on Arginase Enzyme Activity and Polyamine Production in Experimental Breast Cancer. Balk. Med. J. 2015, 32, 89–95. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Locke, M.; Ghazaly, E.; Freitas, M.O.; Mitsinga, M.; Lattanzio, L.; Nigro, C.L.; Nagano, A.; Wang, J.; Chelala, C.; Szlosarek, P.; et al. Inhibition of the Polyamine Synthesis Pathway Is Synthetically Lethal with Loss of Argininosuccinate Synthase 1. Cell Rep. 2016, 16, 1604–1613. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ramos-Molina, B.; Lambertos, A.; Peñafiel, R. Antizyme Inhibitors in Polyamine Metabolism and Beyond: Physiopathological Implications. Med. Sci. 2018, 6, 89. [Google Scholar] [CrossRef] [PubMed]
- Piletz, J.E.; Chikkala, D.N.; Ernsberger, P. Comparison of the properties of agmatine and endogenous clonidine-displacing substanceat imidazoline and a-2 adrenergic receptors. J. Pharmacol. Exp. Ther. 1995, 272, 581–587. [Google Scholar]
- Cabella, C.; Gardini, G.; Corpillo, D.; Testore, G.; Bedino, S.; Solinas, S.P.; Cravanzola, C.; Vargiu, C.; Grillo, M.A.; Colombatto, S. Transport and metabolism of agmatine in rat hepatocyte cultures. Eur. J. Biochem. 2001, 268, 940–947. [Google Scholar] [CrossRef] [PubMed]
- Vargiu, C.; Cabella, C.; Belliardo, S.; Cravanzola, C.; Grillo, M.A.; Colombatto, S. Agmatine modulates polyamine content in hepatocytes by inducing spermidine/spermine acetyltransferase. Eur. J. Biochem. 1999, 259, 933–938. [Google Scholar] [CrossRef]
- Ishizuka, S.; Cunard, R.; Poucell-Hatton, S.; Wead, L.; Lortie, M.; Thomson, S.C.; Gabbai, F.B.; Satriano, J.; Blantz, R.C. Agmatine Inhibits Cell Proliferation and Improves Renal Function in Anti—Thy-1 Glomerulonephritis. J. Am. Soc. Nephrol. 2000, 11, 2256–2264. [Google Scholar] [CrossRef]
- Isome, M.; Lortie, M.J.; Murakami, Y.; Parisi, E.; Matsufuji, S.; Satriano, J. The antiproliferative effects of agmatine correlate with the rate of cellular proliferation. Am. J. Physiol. Physiol. 2007, 293, C705–C711. [Google Scholar] [CrossRef] [PubMed]
- Molderings, G.J.; Kribben, B.; Heinen, A.; Schröder, D.; Brüss, M.; Göthert, M. Intestinal tumor and agmatine (decarboxylated arginine). Cancer 2004, 101, 858–868. [Google Scholar] [CrossRef] [PubMed]
- Wolf, C.; Brüss, M.; Hänisch, B.; Göthert, M.; von Kügelgen, I.; Molderings, G.J. Molecular Basis for the Antiproliferative Effect of Agmatine in Tumor Cells of Colonic, Hepatic, and Neuronal Origin. Mol. Pharmacol. 2007, 71, 276–283. [Google Scholar] [CrossRef] [PubMed]
- Mayeur, C.; Veuillet, G.; Michaud, M.; Raul, F.; Blottière, H.M.; Blachier, F. Effects of agmatine accumulation in human colon carcinoma cells on polyamine metabolism, DNA synthesis and the cell cycle. Biochim. Biophys. Acta 2005, 1745, 111–123. [Google Scholar] [CrossRef] [PubMed]
- Wei, X.; Chow, H.-Y.; Chong, H.-C.; Leung, S.-L.; Ho, M.-K.; Lee, M.-Y.; Leung, Y.-C. Arginine Is a Novel Drug Target for Arginine Decarboxylase in Human Colorectal Cancer Cells. Int. J. Mol. Sci. 2023, 24, 13741. [Google Scholar] [CrossRef] [PubMed]
- Levêque, J.; Foucher, F.; Bansard, J.-Y.; Havouis, R.; Grall, J.-Y.; Moulinoux, J.-P. Polyamine profiles in tumor, normal tissue of the homologous breast, blood, and urine of breast cancer sufferers. Breast Cancer Res. Treat. 2000, 60, 99–105. [Google Scholar] [CrossRef]
- Gerner, E.W.; Meyskens, F.L., Jr. Polyamines and cancer: Old molecules, new understanding. Nat. Rev. Cancer 2004, 4, 781–792. [Google Scholar] [CrossRef]
- Metcalf, B.W.; Bey, P.; Danzin, C.; Jung, M.J.; Casara, P.; Vevert, J.P. Catalytic irreversible inhibition of mammalian ornithine decarboxylase (E.C.4.1.1.17) by substrate and product analogs. J. Am. Chem. Soc. 1978, 100, 2551–2553. [Google Scholar] [CrossRef]
- Poulin, R.; Lu, L.; Ackermann, B.; Bey, P.; E Pegg, A. Mechanism of the irreversible inactivation of mouse ornithine decarboxylase by alpha-difluoromethylornithine. Characterization of sequences at the inhibitor and coenzyme binding sites. J. Biol. Chem. 1992, 267, 150–158. [Google Scholar] [CrossRef] [PubMed]
- Seidenfeld, J. Effects of difluoromethylornithine on proliferation, polyamine content and plating efficiency of cultured human carcinoma cells. Cancer Chemother. Pharmacol. 1985, 15, 196–202. [Google Scholar] [CrossRef]
- Oesterheld, J.; Ferguson, W.; Kraveka, J.M.; Bergendahl, G.; Clinch, T.; Lorenzi, E.; Berry, D.; Wada, R.K.; Isakoff, M.S.; Eslin, D.E.; et al. Eflornithine as Postimmunotherapy Maintenance in High-Risk Neuroblastoma: Externally Controlled, Propensity Score–Matched Survival Outcome Comparisons. J. Clin. Oncol. 2024, 42, 90–102. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Duke, E.S.; Bradford, D.; Sinha, A.K.; Mishra-Kalyani, P.S.; Lerro, C.C.; Rivera, D.; Wearne, E.; Miller, C.P.; Leighton, J.; Sabit, H.; et al. US Food and Drug Administration Approval Summary: Eflornithine for High-Risk Neuroblastoma After Prior Multiagent, Multimodality Therapy. J. Clin. Oncol. 2024, JCO2400546. [Google Scholar] [CrossRef] [PubMed]
- Williams-Ashman, H.G.; Schenone, A. Methyl glyoxal bis(guanylhydrazone) as a potent inhibitor of mammalian and yeast S-adenosylmethionine decayboxylase. Biochem. Biophys. Res. Commun. 1972, 46, 288–295. [Google Scholar] [CrossRef] [PubMed]
- Williams-Ashman, H.; Seidenfeld, J. Aspects of the biochemical pharmacology of methyl glyoxal bis(guanylhydrazone). Biochem. Pharmacol. 1986, 35, 1217–1225. [Google Scholar] [CrossRef] [PubMed]
- Pleshkewych, A.; Kramer, D.L.; Kelly, E.; Porter, C.W. Independence of drug action on mitochondria and polyamines in L1210 leukemia cells treated with methylglyoxal-bis(guanylhydrazone). Cancer Res. 1980, 40, 4533–4540. [Google Scholar]
- Regenass, U.; Mett, H.; Stanek, J.; Mueller, M.; Kramer, D.; Porter, C.W. CGP 48664, a new S-adenosylmethionine decarboxylase inhibitor with broad spectrum antiproliferative and antitumor activity. Cancer Res. 1994, 54, 3210–3217. [Google Scholar]
- Siu, L.L.; Rowinsky, E.K.; A Hammond, L.; Weiss, G.R.; Hidalgo, M.; Clark, G.M.; Moczygemba, J.; Choi, L.; Linnartz, R.; Barbet, N.C.; et al. A phase I and pharmacokinetic study of SAM486A, a novel polyamine biosynthesis inhibitor, administered on a daily-times-five every-three-week schedule in patients with Advanced solid malignancies. Clin. Cancer Res. 2002, 8, 2157–2166. [Google Scholar]
- Pless, M.; Belhadj, K.; Menssen, H.D.; Kern, W.; Coiffier, B.; Wolf, J.; Herrmann, R.; Thiel, E.; Bootle, D.; Sklenar, I.; et al. Clinical efficacy, tolerability, and safety of SAM486A, a novel polyamine biosynthesis inhibitor, in patients with relapsed or refractory non-Hodgkin’s lymphoma: Results from a phase II multicenter study. Clin. Cancer Res. 2004, 10, 1299–1305. [Google Scholar] [CrossRef]
- Van Zuylen, L.; Bridgewater, J.; Sparreboom, A.; Eskens, F.A.L.M.; de Bruijn, P.; Sklenar, I.; Planting, A.S.T.; Choi, L.; Bootle, D.; Mueller, C.; et al. Phase I and Pharmacokinetic Study of the Polyamine Synthesis Inhibitor SAM486A in Combination with 5-Fluorouracil/ Leucovorin in Metastatic Colorectal Cancer. Clin. Cancer Res. 2004, 10, 1949–1955. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Tang, K.-C.; Pegg, A.E.; Coward, J.K. Specific and potent inhibition of spermidine synthase by the transition-state analog, S-adenosyl-3-thio-1,8-diaminooctane. Biochem. Biophys. Res. Commun. 1980, 96, 1371–1377. [Google Scholar] [CrossRef]
- Woster, P.M.; Black, A.Y.; Duff, K.J.; Coward, J.K.; Pegg, A.E. Synthesis and biological evaluation of S-adenosyl-1,12-diamino-3-thio-9-azadodecane, a multisubstrate adduct inhibitor of spermine synthase. J. Med. Chem. 1989, 32, 1300–1307. [Google Scholar] [CrossRef]
- Chaturvedi, R.; de Sablet, T.; Asim, M.; Piazuelo, M.B.; Barry, D.P.; Verriere, T.G.; Sierra, J.C.; Hardbower, D.M.; Delgado, A.G.; Schneider, B.G.; et al. Increased Helicobacter pylori-associated gastric cancer risk in the Andean region of Colombia is mediated by spermine oxidase. Oncogene 2015, 34, 3429–3440. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Goodwin, A.C.; Jadallah, S.; Toubaji, A.; Lecksell, K.; Hicks, J.L.; Kowalski, J.; Bova, G.S.; De Marzo, A.M.; Netto, G.J.; Casero, R.A., Jr. Increased spermine oxidase expression in human prostate cancer and prostatic intraepithelial neoplasia tissues. Prostate 2008, 68, 766–772. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Goodwin, A.C.; Destefano Shields, C.E.; Wu, S.; Huso, D.L.; Wu, X.; Murray-Stewart, T.R.; Hacker-Prietz, A.; Rabizadeh, S.; Woster, P.M.; Sears, C.L.; et al. Polyamine catabolism contributes to enterotoxigenic Bacteroides fragilis-induced colon tumorigenesis. Proc. Natl. Acad. Sci. USA 2011, 108, 15354–15359. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Bey, P.; Bolkenius, F.N.; Seiler, N.; Casara, P. N-(2,3-Butadienyl)-1,4-butanediamine derivatives: Potent irreversible inactivators of mammalian polyamine oxidase. J. Med. Chem. 1985, 28, 1–2. [Google Scholar] [CrossRef] [PubMed]
- Seiler, N.; Duranton, B.; Raul, F. The polyamine oxidase inactivator MDL 72527. Prog. Drug Res. 2002, 59, 1–40. [Google Scholar] [PubMed]
- Diaz, E.; Adhikary, S.; Tepper, A.W.J.W.; Riley, D.; Ortiz-Meoz, R.; Krosky, D.; Buyck, C.; Lamenca, C.M.; Llaveria, J.; Fang, L.; et al. Structure of human spermine oxidase in complex with a highly selective allosteric inhibitor. Commun. Biol. 2022, 5, 787. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Furbish, A.B.; Alford, A.S.; Burger, P.; Peterson, Y.K.; Murray-Stewart, T.; Casero, R.A.; Woster, P.M. Identification and Characterization of Novel Small-Molecule SMOX Inhibitors. Med. Sci. 2022, 10, 47. [Google Scholar] [CrossRef] [PubMed]
- Dunston, T.T.; Khomutov, M.A.; Gabelli, S.B.; Stewart, T.M.; Foley, J.R.; Kochetkov, S.N.; Khomutov, A.R.; Casero, R.A., Jr. Identification of a Novel Substrate-Derived Spermine Oxidase Inhibitor. Acta Naturae 2020, 12, 140–144. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.-C.; Chi, Y.-J.; Yu, Y.-S.; Liu, J.-L.; Su, R.-W.; Ma, X.-H.; Shan, C.-H.; Yang, Z.-M. Polyamines Are Essential in Embryo Implantation: Expression and Function of Polyamine-Related Genes in Mouse Uterus during Peri-Implantation Period. Endocrinology 2008, 149, 2325–2332. [Google Scholar] [CrossRef]
- Porter, C.W.; Bergeron, R.J. Regulation of polyamine biosynthetic activity by spermidine and spermine analogs—A novel antiproliferative strategy. Adv. Exp. Med. Biol. 1988, 250, 677–690. [Google Scholar] [PubMed]
- Casero, R.A., Jr.; Woster, P.M. Terminally alkylated polyamine analogs as chemotherapeutic agents. J. Med. Chem. 2001, 441, 1–26. [Google Scholar] [CrossRef]
- Casero, R.A., Jr.; Woster, P.M. The role of polyamine catabolism in polyamine analogue-induced programmed cell death. Proc. Natl. Acad. Sci. USA 1997, 94, 11557–11562. [Google Scholar]
- Gabrielson, E.W.; Pegg, A.E.; Casero, R.A., Jr. The induction of spermidine/spermine N1-acetyltransferase (SSAT) is a common event in the response of human primary non-small cell lung carcinomas to exposure to the new antitumor polyamine analogue N1, N11-bis(ethyl)norspermine. Clin. Cancer Res. 1999, 5, 1638–1641. [Google Scholar]
- Bernacki, R.J.; Bergeron, R.J.; Porter, C.W. Antitumor activity of N,N′-bis(ethyl)spermine homologues against human MALME-3 melanoma xenografts. Cancer Res. 1992, 52, 2424–2430. [Google Scholar]
- Hahm, H.A.; Ettinger, D.S.; Bowling, K.; Hoker, B.; Chen, T.L.; Zabelina, Y.; Casero, R.A., Jr. Phase I study of N(1),N(11)-diethylnorspermine in patients with non-small cell lung cancer. Clin. Cancer Res. 2002, 8, 684–690. [Google Scholar]
- Creaven, P.J.; Perez, R.; Pendyala, L.; Meropol, N.J.; Loewen, G.; Levine, E.; Berghorn, E.; Raghavan, D. Unusual central nervous system toxicity in a phase I study of N1N11diethylnorspermine in patients with advanced malignancy. Investig. New Drugs 1997, 15, 227–234. [Google Scholar] [CrossRef] [PubMed]
- Casero, R.A.; Mank, A.R.; Saab, N.H.; Wu, R.; Dyer, W.J.; Woster, P.M. Growth and biochemical effects of unsymmetrically substituted polyamine analogues in human lung tumor cells 1. Cancer Chemother. Pharmacol. 1995, 36, 69–74. [Google Scholar] [CrossRef] [PubMed]
- Varghese, S.; Senanayake, T.; Murray-Stewart, T.; Doering, K.; Fraser, A.; Casero, R.A.; Woster, P.M. Polyaminohydroxamic Acids and Polyaminobenzamides as Isoform Selective Histone Deacetylase Inhibitors. J. Med. Chem. 2008, 51, 2447–2456. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Leary, A.; Le Tourneau, C.; Varga, A.; Sablin, M.-P.; Gomez-Roca, C.; Guilbaud, N.; Petain, A.; Pavlyuk, M.; Delord, J.-P. Phase I dose-escalation study of F14512, a polyamine-vectorized topoisomerase II inhibitor, in patients with platinum-refractory or resistant ovarian cancer. Investig. New Drugs 2019, 37, 693–701. [Google Scholar] [CrossRef] [PubMed]
- Thibault, B.; Clement, E.; Zorza, G.; Meignan, S.; Delord, J.-P.; Couderc, B.; Bailly, C.; Narducci, F.; Vandenberghe, I.; Kruczynski, A.; et al. F14512, a polyamine-vectorized inhibitor of topoisomerase II, exhibits a marked anti-tumor activity in ovarian cancer. Cancer Lett. 2016, 370, 10–18. [Google Scholar] [CrossRef] [PubMed]
- Hacker, A.; Marton, L.J.; Sobolewski, M.; Casero, R.A. In vitro and in vivo effects of the conformationally restricted polyamine analogue CGC-11047 on small cell and non-small cell lung cancer cells. Cancer Chemother. Pharmacol. 2008, 63, 45–53. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Carew, J.S.; Nawrocki, S.T.; Reddy, V.K.; Bush, D.; Rehg, J.E.; Goodwin, A.; Houghton, J.A.; Casero, R.A.; Marton, L.J.; Cleveland, J.L. The Novel Polyamine Analogue CGC-11093 Enhances the Antimyeloma Activity of Bortezomib. Cancer Res. 2008, 68, 4783–4790. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kuo, W.-L.; Das, D.; Ziyad, S.; Bhattacharya, S.; Gibb, W.J.; Heiser, L.M.; Sadanandam, A.; Fontenay, G.V.; Hu, Z.; Wang, N.J.; et al. A systems analysis of the chemosensitivity of breast cancer cells to the polyamine analogue PG-11047. BMC Med. 2009, 7, 77. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- A Ignatenko, N.; Yerushalmi, H.F.; Pandey, R.; Kachel, K.L.; E Stringer, D.; Marton, L.J.; Gerner, E.W. Gene expression analysis of HCT116 colon tumor-derived cells treated with the polyamine analog PG-11047. Cancer Genom. Proteom. 2009, 6, 161–175. [Google Scholar] [PubMed] [PubMed Central]
- Dredge, K.; Kink, J.A.; Johnson, R.M.; Bytheway, I.; Marton, L.J. The polyamine analog PG11047 potentiates the antitumor activity of cisplatin and bevacizumab in preclinical models of lung and prostate cancer. Cancer Chemother. Pharmacol. 2009, 65, 191–195. [Google Scholar] [CrossRef] [PubMed]
- Murray Stewart, T.; Desai, A.A.; Fitzgerald, M.L.; Marton, L.J.; Casero, R.A., Jr. A phase I dose-escalation study of the polyamine analog PG-11047 in patients with advanced solid tumors. Cancer Chemother. Pharmacol. 2020, 85, 1089–1096. [Google Scholar] [CrossRef]
- Valasinas, A.; Reddy, V.K.; Blokhin, A.V.; Basu, H.S.; Bhattacharya, S.; Sarkar, A.; Marton, L.J.; Frydman, B. Long-chain polyamines (oligoamines) exhibit strong cytotoxicities against human prostate cancer cells. Bioorganic Med. Chem. 2003, 11, 4121–4131. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.; Hager, E.R.; Phillips, D.L.; Dunn, V.R.; Hacker, A.; Frydman, B.; A Kink, J.; Valasinas, A.L.; Reddy, V.K.; Marton, L.J.; et al. A novel polyamine analog inhibits growth and induces apoptosis in human breast cancer cells. Clin. Cancer Res. 2003, 9, 2769–2777. [Google Scholar] [PubMed] [PubMed Central]
- Huang, Y.; Stewart, T.M.; Wu, Y.; Baylin, S.B.; Marton, L.J.; Perkins, B.; Jones, R.J.; Woster, P.M.; Casero, R.A. Novel Oligoamine Analogues Inhibit Lysine-Specific Demethylase 1 and Induce Reexpression of Epigenetically Silenced Genes. Clin. Cancer Res. 2009, 15, 7217–7228. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Shi, Y.; Lan, F.; Matson, C.; Mulligan, P.; Whetstine, J.R.; Cole, P.A.; Casero, R.A.; Shi, Y. Histone Demethylation Mediated by the Nuclear Amine Oxidase Homolog LSD1. Cell 2004, 119, 941–953. [Google Scholar] [CrossRef] [PubMed]
- Schulte, J.H.; Lim, S.; Schramm, A.; Friedrichs, N.; Koster, J.; Versteeg, R.; Ora, I.; Pajtler, K.; Klein-Hitpass, L.; Kuhfittig-Kulle, S.; et al. Lysine-Specific Demethylase 1 Is Strongly Expressed in Poorly Differentiated Neuroblastoma: Implications for Therapy. Cancer Res. 2009, 69, 2065–2071. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.; Greene, E.; Murray-Stewart, T.; Goodwin, A.; Baylin, S.; Woster, P.; Casero, R., Jr. Inhibition of lysine-specific demethylase 1 by polyamine analogues results in reexpression of aberrantly silenced genes. Proc. Natl. Acad. Sci. USA 2007, 104, 8023–8028. [Google Scholar] [CrossRef]
- Lee, M.G.; Wynder, C.; Schmidt, D.M.; McCafferty, D.G.; Shiekhattar, R. Histone H3 Lysine 4 Demethylation Is a Target of Nonselective Antidepressive Medications. Chem. Biol. 2006, 13, 563–567. [Google Scholar] [CrossRef]
- Culhane, J.C.; Szewczuk, L.M.; Liu, X.; Da, G.; Marmorstein, R.; Cole, P.A. A Mechanism-Based Inactivator for Histone Demethylase LSD1. J. Am. Chem. Soc. 2006, 128, 4536–4537. [Google Scholar] [CrossRef]
- Bergeron, R.J.; Müller, R.; Bussenius, J.; McManis, J.S.; Merriman, R.L.; Smith, R.E.; Yao, H.; Weimar, W.R. Synthesis and Evaluation of Hydroxylated Polyamine Analogues as Antiproliferatives. J. Med. Chem. 2000, 43, 224–235. [Google Scholar] [CrossRef]
- Panbela Therapeutics. Phase 1A/1B Dose Escalation and Expansion Study of SBP-101 in Combination with Nab-Paclitaxel and Gemcitabine in Subjects with Previously Untreated Metastatic Pancreatic Ductal Adenocarcinoma. ClinicalTrials.gov identifier: NCT03412799. Available online: https://clinicaltrials.gov/study/NCT03412799?tab=history&a=10 (accessed on 20 May 2024).
- Panbela Therapeutics. A Randomized, Double-Blind, Placebo-Controlled Study of Nab-Paclitaxel and Gemcitabine with or without SBP-101 in Subjects Previously Untreated for Metastatic Pancreatic Ductal Adenocarcinoma. NCT05254171. Available online: https://clinicaltrials.gov/ct2/show/NCT05254171 (accessed on 23 August 2023).
- Holbert, C.E.; Foley, J.R.; Stewart, T.M.; Casero, R.A. Expanded Potential of the Polyamine Analogue SBP-101 (Diethyl Dihydroxyhomospermine) as a Modulator of Polyamine Metabolism and Cancer Therapeutic. Int. J. Mol. Sci. 2022, 23, 6798. [Google Scholar] [CrossRef]
- Holbert, C.E.; Stewart, T.M.; Simpson, J.K.; Walker, M.J.; Casero, R.A. Abstract 5488: The potential of spermine analogue SBP-101 (diethyl dihydroxyhomospermine) as a polyamine metabolism modulator in ovarian cancer. Cancer Res. 2022, 82, 5488. [Google Scholar] [CrossRef]
- Muth, A.; Madan, M.; Archer, J.J.; Ocampo, N.; Rodriguez, L.; Phanstiel, O. Polyamine Transport Inhibitors: Design, Synthesis, and Combination Therapies with Difluoromethylornithine. J. Med. Chem. 2014, 57, 348–363. [Google Scholar] [CrossRef]
- Burns, M.R.; Carlson, C.L.; Vanderwerf, S.M.; Ziemer, J.R.; Weeks, R.S.; Cai, F.; Webb, H.K.; Graminski, G.F. Amino Acid/Spermine Conjugates: Polyamine Amides as Potent Spermidine Uptake Inhibitors. J. Med. Chem. 2001, 44, 3632–3644. [Google Scholar] [CrossRef]
- Burns, M.R.; Graminski, G.F.; Weeks, R.S.; Chen, Y.; O’brien, T.G. Lipophilic Lysine−Spermine Conjugates Are Potent Polyamine Transport Inhibitors for Use in Combination with a Polyamine Biosynthesis Inhibitor. J. Med. Chem. 2009, 52, 1983–1993. [Google Scholar] [CrossRef]
- Holbert, C.E.; Dunworth, M.; Foley, J.R.; Dunston, T.T.; Stewart, T.M.; Casero, R.A. Autophagy induction by exogenous polyamines is an artifact of bovine serum amine oxidase activity in culture serum. J. Biol. Chem. 2020, 295, 9061–9068. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Muth, A.; Kamel, J.; Kaur, N.; Shicora, A.C.; Ayene, I.S.; Gilmour, S.K.; Phanstiel, O. Development of Polyamine Transport Ligands with Improved Metabolic Stability and Selectivity against Specific Human Cancers. J. Med. Chem. 2013, 56, 5819–5828. [Google Scholar] [CrossRef]
- Dobrovolskaite, A.; Gardner, R.A.; Delcros, J.G.; Phanstiel, O., IV. Development of Polyamine Lassos as Polyamine Transport Inhibitors. ACS Med. Chem. Lett. 2022, 132, 319–326. [Google Scholar] [CrossRef]
- Beiu, C.; Giurcaneanu, C.; Grumezescu, A.M.; Holban, A.M.; Popa, L.G.; Mihai, M.M. Nanosystems for Improved Targeted Therapies in Melanoma. J. Clin. Med. 2020, 9, 318. [Google Scholar] [CrossRef] [PubMed]
- Bumcrot, D.; Manoharan, M.; Koteliansky, V.; Sah, D.W.Y. RNAi therapeutics: A potential new class of pharmaceutical drugs. Nat. Chem. Biol. 2006, 2, 711–719. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Liu, J.; Guo, B. RNA-based therapeutics for colorectal cancer: Updates and future directions. Pharmacol. Res. 2020, 152, 104550. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Gupta, E.D.; Pachauri, M.; Ghosh, P.C.; Rajam, M.V. Targeting polyamine biosynthetic pathway through RNAi causes the abrogation of MCF 7 breast cancer cell line. Tumor Biol. 2016, 37, 1159–1171. [Google Scholar] [CrossRef] [PubMed]
- Xu, C.-X.; Yan, Y.-F.; Yang, Y.-P.; Liu, B.; Xin, J.-X.; Chen, S.-M.; Wang, W.; Jiang, C.-Y.; Lu, Z.-X.; Liu, X.-X. Downregulation of ornithine decarboxylase by pcDNA-ODCr inhibits gastric cancer cell growth in vitro. Mol. Biol. Rep. 2011, 38, 949–955. [Google Scholar] [CrossRef] [PubMed]
- Chi, W.; Song, X.; Jiang, C.; Liu, X.; Li, W.; Wang, X. Lentiviral Vector-Mediated Downregulation of Ornithine Decarboxylase Inhibits Tumor Cell Growth in vitro and in vivo. Tumor Biol. 2006, 27, 243–251. [Google Scholar] [CrossRef] [PubMed]
- Cui, P.-F.; Xing, L.; Qiao, J.-B.; Zhang, J.-L.; He, Y.-J.; Zhang, M.; Lyu, J.-Y.; Luo, C.-Q.; Jin, L.; Jiang, H.-L. Polyamine metabolism-based dual functional gene delivery system to synergistically inhibit the proliferation of cancer. Int. J. Pharm. 2016, 506, 79–86. [Google Scholar] [CrossRef] [PubMed]
- Yathindranath, V.; Safa, N.; Sajesh, B.V.; Schwinghamer, K.; Vanan, M.I.; Bux, R.; Sitar, D.S.; Pitz, M.; Siahaan, T.J.; Miller, D.W. Spermidine/Spermine N1-Acetyltransferase 1 (SAT1)—A Potential Gene Target for Selective Sensitization of Glioblastoma Cells Using an Ionizable Lipid Nanoparticle to Deliver siRNA. Cancers 2022, 14, 5179. [Google Scholar] [CrossRef] [PubMed]
- Dong, Y.; Zhu, Y.; Li, J.; Zhou, Q.-H.; Wu, C.; Oupický, D. Synthesis of Bisethylnorspermine Lipid Prodrug as Gene Delivery Vector Targeting Polyamine Metabolism in Breast Cancer. Mol. Pharm. 2012, 9, 1654–1664. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Murray-Stewart, T.; Ferrari, E.; Xie, Y.; Yu, F.; Marton, L.J.; Oupicky, D.; Casero, R.A. Biochemical evaluation of the anticancer potential of the polyamine-based nanocarrier Nano11047. PLoS ONE 2017, 12, e0175917. [Google Scholar] [CrossRef] [PubMed]
- Chang, T.-C.; Wentzel, E.A.; Kent, O.A.; Ramachandran, K.; Mullendore, M.; Lee, K.H.; Feldmann, G.; Yamakuchi, M.; Ferlito, M.; Lowenstein, C.J.; et al. Transactivation of miR-34a by p53 Broadly Influences Gene Expression and Promotes Apoptosis. Mol. Cell 2007, 26, 745–752. [Google Scholar] [CrossRef]
- Xie, Y.; Murray-Stewart, T.; Wang, Y.; Yu, F.; Li, J.; Marton, L.J.; Casero, R.A.; Oupický, D. Self-immolative nanoparticles for simultaneous delivery of microRNA and targeting of polyamine metabolism in combination cancer therapy. J. Control. Release 2017, 246, 110–119. [Google Scholar] [CrossRef]
- Holbert, C.E.; Foley, J.R.; Yu, A.; Stewart, T.M.; Phanstiel, O.; Oupicky, D.; Casero, R.A. Polyamine-Based Nanostructures Share Polyamine Transport Mechanisms with Native Polyamines and Their Analogues: Significance for Polyamine-Targeted Therapy. Med. Sci. 2022, 10, 44. [Google Scholar] [CrossRef]
- Lu, B.; Wang, L.; Ran, X.; Tang, H.; Cao, D. Recent Advances in Fluorescent Methods for Polyamine Detection and the Polyamine Suppressing Strategy in Tumor Treatment. Biosensors 2022, 12, 633. [Google Scholar] [CrossRef] [PubMed]
- Raj, K.P.; A Zell, J.; Rock, C.L.; E McLaren, C.; Zoumas-Morse, C.; Gerner, E.W.; Meyskens, F.L. Role of dietary polyamines in a phase III clinical trial of difluoromethylornithine (DFMO) and sulindac for prevention of sporadic colorectal adenomas. Br. J. Cancer 2013, 108, 512–518. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Sarhan, S.; Knodgen, B.; Seiler, N. The gastrointestinal tract as polyamine source for tumor growth. Anticancer. Res. 1989, 9, 215–223. [Google Scholar]
- Gamble, L.D.; Purgato, S.; Murray, J.; Xiao, L.; Yu, D.M.T.; Hanssen, K.M.; Giorgi, F.M.; Carter, D.R.; Gifford, A.J.; Valli, E.; et al. Inhibition of polyamine synthesis and uptake reduces tumor progression and prolongs survival in mouse models of neuroblastoma. Sci. Transl. Med. 2019, 11, eaau1099. [Google Scholar] [CrossRef] [PubMed]
- Samal, K.; Zhao, P.; Kendzicky, A.; Yco, L.P.; McClung, H.; Gerner, E.; Burns, M.; Bachmann, A.S.; Sholler, G. AMXT-1501, a novel polyamine transport inhibitor, synergizes with DFMO in inhibiting neuroblastoma cell proliferation by targeting both ornithine decarboxylase and polyamine transport. Int. J. Cancer 2013, 133, 1323–1333. [Google Scholar] [CrossRef] [PubMed]
- Gitto, S.B.; Pandey, V.; Oyer, J.L.; Copik, A.J.; Hogan, F.C.; Phanstiel, O.; Altomare, D.A. Difluoromethylornithine Combined with a Polyamine Transport Inhibitor Is Effective against Gemcitabine Resistant Pancreatic Cancer. Mol. Pharm. 2018, 15, 369–376. [Google Scholar] [CrossRef]
- Skorupski, K.A.; O’Brien, T.G.; Guerrero, T.; Rodriguez, C.O.; Burns, M.R. Phase I/II clinical trial of 2-difluoromethyl-ornithine (DFMO) and a novel polyamine transport inhibitor (MQT 1426) for feline oral squamous cell carcinoma*. Vet.-Comp. Oncol. 2011, 9, 275–282. [Google Scholar] [CrossRef] [PubMed]
- A Chan, T. Nonsteroidal anti-inflammatory drugs, apoptosis, and colon-cancer chemoprevention. Lancet Oncol. 2002, 3, 166–174. [Google Scholar] [CrossRef]
- Verdoodt, F.; Dehlendorff, C.; Friis, S.; Kjaer, S.K. Non-aspirin NSAID use and ovarian cancer mortality. Gynecol. Oncol. 2018, 150, 331–337. [Google Scholar] [CrossRef]
- López-Contreras, F.; Muñoz-Uribe, M.; Pérez-Laines, J.; Ascencio-Leal, L.; Rivera-Dictter, A.; Martin-Martin, A.; Burgos, R.A.; Alarcon, P.; López-Muñoz, R. Searching for Drug Synergy Against Cancer Through Polyamine Metabolism Impairment: Insight into the Metabolic Effect of Indomethacin on Lung Cancer Cells. Front. Pharmacol. 2020, 10, 1670. [Google Scholar] [CrossRef]
- Babbar, N.; Ignatenko, N.A.; Casero, R.A.; Gerner, E.W. Cyclooxygenase-independent Induction of Apoptosis by Sulindac Sulfone Is Mediated by Polyamines in Colon Cancer. J. Biol. Chem. 2003, 278, 47762–47775. [Google Scholar] [CrossRef] [PubMed]
- Babbar, N.; Gerner, E.W.; Casero, R.A. Induction of spermidine/spermine N1-acetyltransferase (SSAT) by aspirin in Caco-2 colon cancer cells. Biochem. J. 2006, 394, 317–324. [Google Scholar] [CrossRef] [PubMed]
- Wolfe, M. Future trends in the development of safer nonsteroidal anti-inflammatory drugs. Am. J. Med. 1998, 105, 44S–52S. [Google Scholar] [CrossRef] [PubMed]
- Williams, J.L.; Borgo, S.; Hasan, I.; Castillo, E.; Traganos, F.; Rigas, B. Nitric oxide-releasing nonsteroidal anti-inflammatory drugs (NSAIDs) alter the kinetics of human colon cancer cell lines more effectively than traditional NSAIDs: Implications for colon cancer chemoprevention. Cancer Res. 2001, 61, 3285–3289. [Google Scholar] [PubMed]
- Madka, V.; Patlolla, J.M.R.; Venkatachalam, K.; Zhang, Y.; Pathuri, G.; Stratton, N.; Lightfoot, S.; Janakiram, N.B.; Mohammed, A.; Rao, C.V. Chemoprevention of Colon Cancer by DFMO, Sulindac, and NO-Sulindac Administered Individually or in Combinations in F344 Rats. Cancers 2023, 15, 4001. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Hogarty, M.D.; Ziegler, D.S.; Franson, A.; Chi, Y.-Y.; Tsao-Wei, D.; Liu, K.; Vemu, R.; Gerner, E.W.; Bruckheimer, E.; Shamirian, A.; et al. Phase 1 study of high-dose DFMO, celecoxib, cyclophosphamide and topotecan for patients with relapsed neuroblastoma: A New Approaches to Neuroblastoma Therapy trial. Br. J. Cancer 2024, 130, 788–797. [Google Scholar] [CrossRef] [PubMed]
- Evageliou, N.F.; Haber, M.; Vu, A.; Laetsch, T.W.; Murray, J.; Gamble, L.D.; Cheng, N.C.; Liu, K.; Reese, M.; Corrigan, K.A.; et al. Polyamine Antagonist Therapies Inhibit Neuroblastoma Initiation and Progression. Clin. Cancer Res. 2016, 22, 4391–4404. [Google Scholar] [CrossRef] [PubMed]
- Nigro, N.D.; Bull, A.W.; Boyd, M.E. Inhibition of Intestinal Carcinogenesis in Rats: Effect of Difluoromethylornithine with Piroxicam or Fish Oil2. J. Natl. Cancer Inst. 1986, 77, 1309–1313. [Google Scholar] [CrossRef]
- Abou-el-Ela, S.H.; Prasse, K.W.; Farrell, R.L.; Carroll, R.W.; Wade, A.E.; Bunce, O.R. Effects of dl-2-difluoromethylornithine and indomethacin on mammary tumor promotion in rats fed high n-3 and/or n-6 fat diets. Cancer Res. 1989, 49, 1434–1440. [Google Scholar]
- Li, H.; Schut, H.A.; Conran, P.; Kramer, P.M.; Lubet, R.A.; Steele, V.E.; Hawk, E.E.; Kelloff, G.J.; Pereira, M.A. Prevention by aspirin and its combination with α-difluoromethylornithine of azoxymethane-induced tumors, aberrant crypt foci and prostaglandin E2 levels in rat colon. Carcinogenesis 1999, 20, 425–430. [Google Scholar] [CrossRef]
- Pledgie-Tracy, A.; Billam, M.; Hacker, A.; Sobolewski, M.D.; Woster, P.M.; Zhang, Z.; Casero, R.A.; Davidson, N.E. The role of the polyamine catabolic enzymes SSAT and SMO in the synergistic effects of standard chemotherapeutic agents with a polyamine analogue in human breast cancer cell lines. Cancer Chemother. Pharmacol. 2010, 65, 1067–1081. [Google Scholar] [CrossRef] [PubMed]
- Stewart, T.M.; Von Hoff, D.; Fitzgerald, M.; Marton, L.J.; Becerra, C.H.R.; Boyd, T.E.; Conkling, P.R.; Garbo, L.E.; Jotte, R.M.; Richards, D.A.; et al. A Phase Ib multicenter, dose-escalation study of the polyamine analogue PG-11047 in combination with gemcitabine, docetaxel, bevacizumab, erlotinib, cisplatin, 5-fluorouracil, or sunitinib in patients with advanced solid tumors or lymphoma. Cancer Chemother. Pharmacol. 2021, 87, 135–144. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Stone, M.L.; Chiappinelli, K.B.; Li, H.; Murphy, L.M.; Travers, M.E.; Topper, M.J.; Mathios, D.; Lim, M.; Shih, I.-M.; Wang, T.-L.; et al. Epigenetic therapy activates type I interferon signaling in murine ovarian cancer to reduce immunosuppression and tumor burden. Proc. Natl. Acad. Sci. USA 2017, 114, E10981–E10990. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Tsai, H.-C.; Li, H.; Van Neste, L.; Cai, Y.; Robert, C.; Rassool, F.V.; Shin, J.J.; Harbom, K.M.; Beaty, R.; Pappou, E.; et al. Transient Low Doses of DNA-Demethylating Agents Exert Durable Antitumor Effects on Hematological and Epithelial Tumor Cells. Cancer Cell 2012, 21, 430–446. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Travers, M.; Dunworth, M.; Holbert, C.E.; Wiehagen, K.R.; Bachman, K.E.; Foley, J.R.; Stone, M.L.; Baylin, S.B.; Casero, R.A.; Zahnow, C.A. DFMO and 5-Azacytidine Increase M1 Macrophages in the Tumor Microenvironment of Murine Ovarian Cancer. Cancer Res. 2019, 79, 3445–3454. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Hayes, C.S.; Shicora, A.C.; Keough, M.P.; Snook, A.E.; Burns, M.R.; Gilmour, S.K. Polyamine-Blocking Therapy Reverses Immunosuppression in the Tumor Microenvironment. Cancer Immunol. Res. 2014, 2, 274–285. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Alexander, E.T.; Minton, A.; Peters, M.C.; Phanstiel, O., IV; Gilmour, S.K. A novel polyamine blockade therapy activates an anti-tumor immune response. Oncotarget 2017, 8, 84140–84152. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ye, C.; Geng, Z.; Dominguez, D.; Chen, S.; Fan, J.; Qin, L.; Long, A.; Zhang, Y.; Kuzel, T.M.; Zhang, B. Targeting Ornithine Decarboxylase by α-Difluoromethylornithine Inhibits Tumor Growth by Impairing Myeloid-Derived Suppressor Cells. J. Immunol. 2016, 196, 915–923. [Google Scholar] [CrossRef]
- Dryja, P.; Fisher, C.; Woster, P.M.; Bartee, E. Inhibition of Polyamine Biosynthesis Using Difluoromethylornithine Acts as a Potent Immune Modulator and Displays Therapeutic Synergy With PD-1-blockade. J. Immunother. 2021, 44, 283–291. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Tanaka, Y. Effect of Polyamines on Two Types of Reaction of Purified PoIy(ADP-Ribose) Polymerase1. J. Biochem. 1982, 91, 2029–2037. [Google Scholar] [CrossRef]
- El Naggar, O.; Doyle, B.; Mariner, K.; Gilmour, S.K. Difluoromethylornithine (DFMO) Enhances the Cytotoxicity of PARP Inhibition in Ovarian Cancer Cells. Med. Sci. 2022, 10, 28. [Google Scholar] [CrossRef]
- Tummala, R.; Diegelman, P.; Hector, S.; Kramer, D.L.; Clark, K.; Zagst, P.; Fetterly, G.; Porter, C.W.; Pendyala, L. Combination effects of platinum drugs and N 1, N 11 diethylnorspermine on spermidine/spermine N 1-acetyltransferase, polyamines and growth inhibition in A2780 human ovarian carcinoma cells and their oxaliplatin and cisplatin-resistant variants. Cancer Chemother. Pharmacol. 2011, 67, 401–414. [Google Scholar] [CrossRef]
- Hector, S.; Porter, C.W.; Kramer, D.L.; Clark, K.; Prey, J.; Kisiel, N.; Diegelman, P.; Chen, Y.; Pendyala, L. Polyamine catabolism in platinum drug action: Interactions between oxaliplatin and the polyamine analogue N1,N11-diethylnorspermine at the level of spermidine/spermine N1-acetyltransferase. Mol. Cancer Ther. 2004, 3, 813–822. [Google Scholar] [CrossRef]
- Marverti, G.; Ligabue, A.; Guerrieri, D.; Paglietti, G.; Piras, S.; Costi, M.P.; Farina, D.; Frassineti, C.; Monti, M.G.; Moruzzi, M.S. Spermidine/spermine N1-acetyltranferase modulation by novel folate cycle inhibitors in cisplatin-sensitive and -resistant human ovarian cancer cell lines. Gynecol. Oncol. 2010, 117, 202–210. [Google Scholar] [CrossRef]
- Holbert, C.E.; Foley, J.R.; Casero, R.A.; Stewart, T.M. The Polyamine Analogue Ivospemin Increases Chemotherapeutic Efficacy in Murine Ovarian Cancer. Biomedicines 2024, 12, 1157. [Google Scholar] [CrossRef]
- Takahashi, Y.; Sakaguchi, K.; Horio, H.; Hiramatsu, K.; Moriya, S.; Takahashi, K.; Kawakita, M. Urinary N1, N12-diacetylspermine is a non-invasive marker for the diagnosis and prognosis of non-small-cell lung cancer. Br. J. Cancer 2015, 113, 1493–1501. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Niemi, R.J.; Roine, A.N.; Häkkinen, M.R.; Kumpulainen, P.S.; Keinänen, T.A.; Vepsäläinen, J.J.; Lehtimäki, T.; Oksala, N.K.; Mäenpää, J.U. Urinary Polyamines as Biomarkers for Ovarian Cancer. Int. J. Gynecol. Cancer 2017, 27, 1360–1366. [Google Scholar] [CrossRef] [PubMed]
| Name | Structure | Reference |
|---|---|---|
| Trimer44NMe | 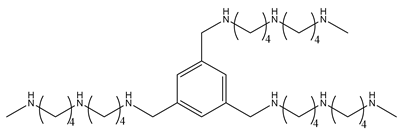 | [145] |
| AMXT1501 | 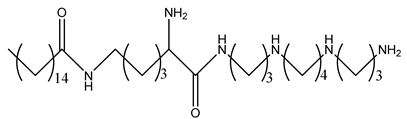 | [146] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, T.-A.; Stewart, T.M.; Casero, R.A., Jr. The Synergistic Benefit of Combination Strategies Targeting Tumor Cell Polyamine Homeostasis. Int. J. Mol. Sci. 2024, 25, 8173. https://doi.org/10.3390/ijms25158173
Liu T-A, Stewart TM, Casero RA Jr. The Synergistic Benefit of Combination Strategies Targeting Tumor Cell Polyamine Homeostasis. International Journal of Molecular Sciences. 2024; 25(15):8173. https://doi.org/10.3390/ijms25158173
Chicago/Turabian StyleLiu, Ting-Ann, Tracy Murray Stewart, and Robert A. Casero, Jr. 2024. "The Synergistic Benefit of Combination Strategies Targeting Tumor Cell Polyamine Homeostasis" International Journal of Molecular Sciences 25, no. 15: 8173. https://doi.org/10.3390/ijms25158173
APA StyleLiu, T.-A., Stewart, T. M., & Casero, R. A., Jr. (2024). The Synergistic Benefit of Combination Strategies Targeting Tumor Cell Polyamine Homeostasis. International Journal of Molecular Sciences, 25(15), 8173. https://doi.org/10.3390/ijms25158173