Multiple Sclerosis: From the Application of Oligoclonal Bands to Novel Potential Biomarkers
Abstract
1. Introduction
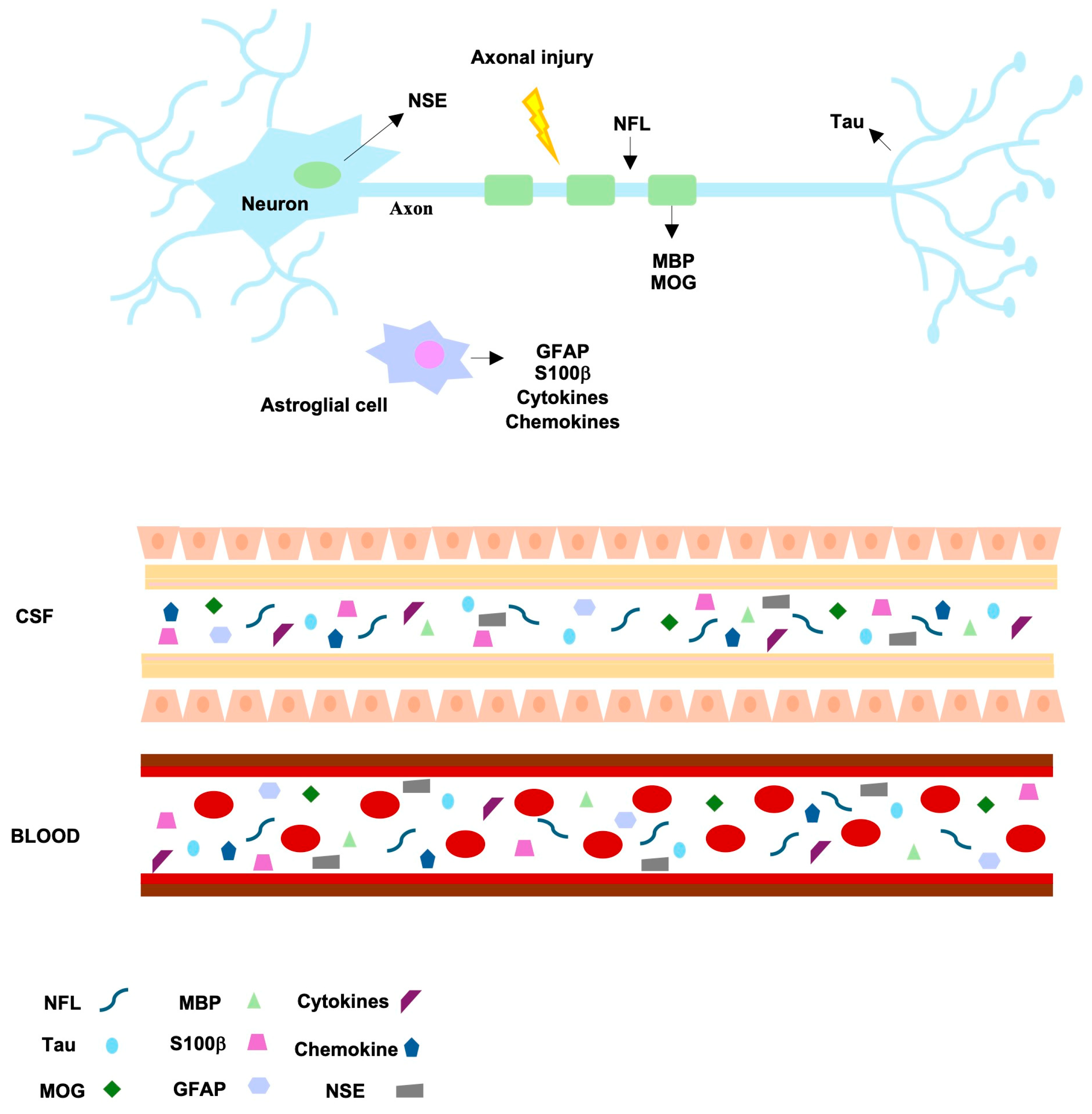
2. Current Biomarkers and Procedures Used in Clinical Setting
2.1. The Application of Oligoclonal Bands, IgG Intrathecal Synthesis, and “Gold Standard” Laboratory Test
2.2. Kappa (and Lambda) Free Light Chains as New Biomarkers for MS Diagnosis
2.3. κFLCs in the CSF of MS Patients and Early Disease Activity
| Parameter/Algorithm Used for κFLC Measurement | Formula |
|---|---|
| CSF κFLC concentration | Absolute concentration |
| κFLC quotient (Q-κFLC) | CSF κFLC/serum κFLC |
| κFLC index | Q κFLC/QAlb |
| * Presslauer’s formula [49] | QLim-FLC = 0.9358 × QAlb0.6687 |
| * Hegen formula [50] | QLim-FLC = 3.1276 × QAlb0.8001 |
| * Reiber’s formula [51] | QLim-FLC = 3.27 (QAlb2 + 33)0.5 − 8.2 × 10−3 |
| * Senel’s formula [52] | QLim-FLC = 14.85 + 2.41 × QAlb |
2.4. κFLC Index: Advantages and Open Issues
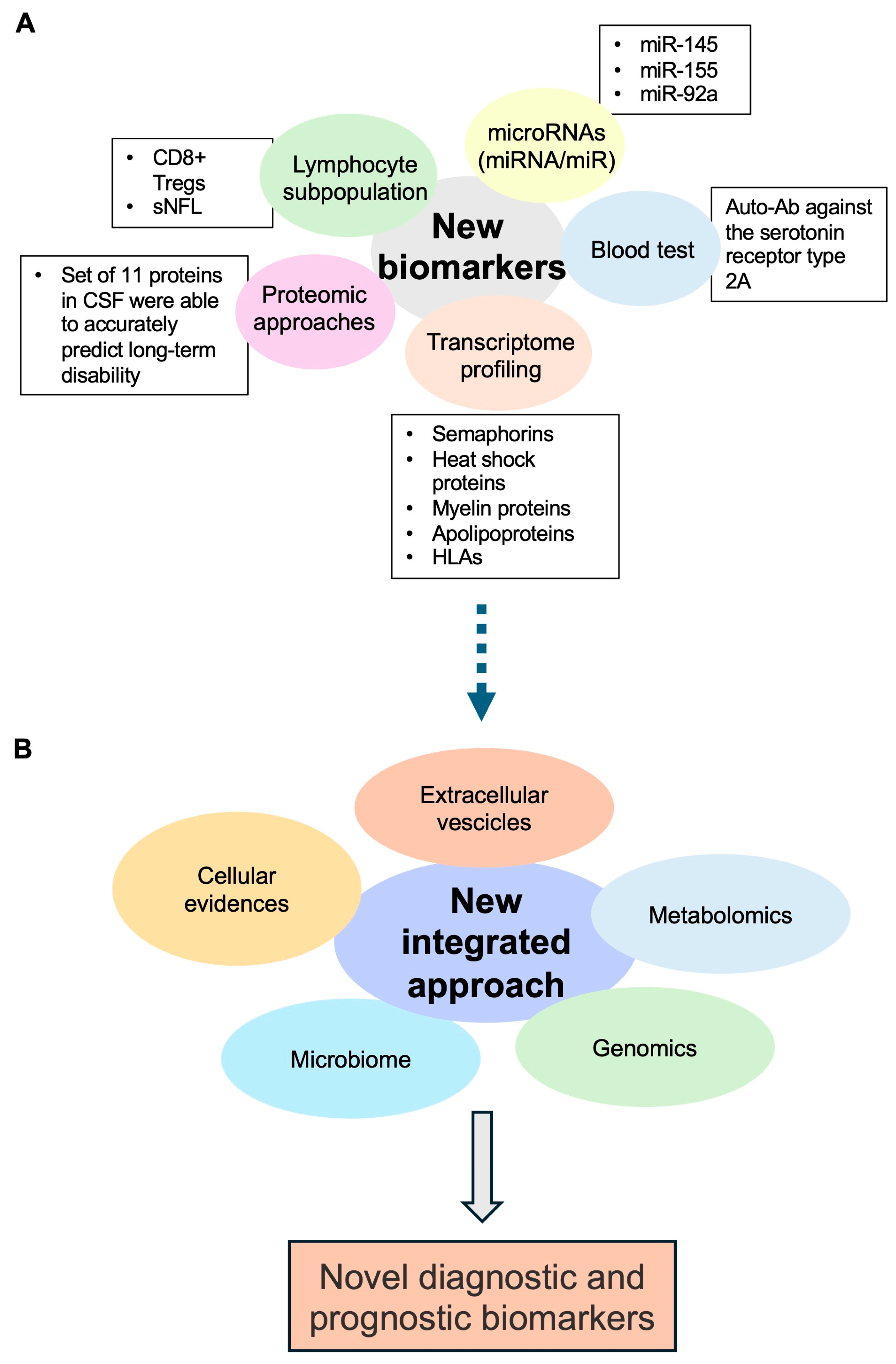
3. Future Perspectives: The Search for Novel Potential Biomarkers
4. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Jakimovski, D.; Bittner, S.; Zivadinov, R.; Morrow, S.A.; Benedict, R.H.; Zipp, F.; Weinstock-Guttman, B. Multiple sclerosis. Lancet 2024, 403, 183–202. [Google Scholar] [CrossRef]
- Maroto-García, J.; Martínez-Escribano, A.; Delgado-Gil, V.; Mañez, M.; Mugueta, C.; Varo, N.; García de la Torre, Á.; Ruiz-Galdón, M. Biochemical biomarkers for multiple sclerosis. Clin. Chim. Acta 2023, 548, 117471. [Google Scholar] [CrossRef] [PubMed]
- Waubant, E.; Lucas, R.; Mowry, E.; Graves, J.; Olsson, T.; Alfredsson, L.; Langer-Gould, A. Environmental and genetic risk factors for MS: An integrated review. Ann. Clin. Transl. Neurol. 2019, 6, 1905–1922. [Google Scholar] [CrossRef]
- Thompson, A.J.; Banwell, B.L.; Barkhof, F.; Carroll, W.M.; Coetzee, T.; Comi, G.; Correale, J.; Fazekas, F.; Filippi, M.; Freedman, M.S.; et al. Diagnosis of multiple sclerosis: 2017 revisions of the McDonald criteria. Lancet Neurol. 2018, 17, 162–173. [Google Scholar] [CrossRef]
- Hauser, S.L.; Cree, B.A.C. Treatment of Multiple Sclerosis: A Review. Am. J. Med. 2020, 133, 1380–1390.e2. [Google Scholar] [CrossRef] [PubMed]
- Giovannoni, G. Disease-modifying treatments for early and advanced multiple sclerosis: A new treatment paradigm. Curr. Opin. Neurol. 2018, 31, 233–243. [Google Scholar] [CrossRef] [PubMed]
- Ontaneda, D.; Tallantyre, E.; Kalincik, T.; Planchon, S.M.; Evangelou, N. Early highly effective versus escalation treatment approaches in relapsing multiple sclerosis. Lancet Neurol. 2019, 18, 973–980. [Google Scholar] [CrossRef]
- Bsteh, G.; Hegen, H.; Dosser, C.; Auer, M.; Berek, K.; Wurth, S.; Zinganell, A.; Di Pauli, F.; Deisenhammer, F.; Berger, T. To treat or not to treat: Sequential individualized treatment evaluation in relapsing multiple sclerosis. Mult. Scler. Relat. Disord. 2020, 39, 101908. [Google Scholar] [CrossRef]
- Freedman, M.S.; Thompson, E.J.; Deisenhammer, F.; Giovannoni, G.; Grimsley, G.; Keir, G.; Ohman, S.; Racke, M.K.; Sharief, M.; Sindic, C.J.; et al. Recommended standard of cerebrospinal fluid analysis in the diagnosis of multiple sclerosis: A consensus statement. Arch. Neurol. 2005, 62, 865–870. [Google Scholar] [CrossRef]
- Hegen, H.; Arrambide, G.; Gnanapavan, S.; Kaplan, B.; Khalil, M.; Saadeh, R.; Teunissen, C.; Tumani, H.; Villar, L.M.; Willrich, M.A.V.; et al. Cerebrospinal fluid kappa free light chains for the diagnosis of multiple sclerosis: A consensus statement. Mult. Scler. 2023, 29, 182–195. [Google Scholar] [CrossRef]
- Hegen, H.; Zinganell, A.; Auer, M.; Deisenhammer, F. The clinical significance of single or double bands in cerebrospinal fluid isoelectric focusing. A retrospective study and systematic review. PLoS ONE 2019, 14, e0215410. [Google Scholar] [CrossRef] [PubMed]
- Kabat, E.A.; Freedman, D.A. A study of the crystalline albumin, gamma globulin and total protein in the cerebrospinal fluid of 100 cases of multiple sclerosis and in other diseases. Am. J. Med. Sci. 1950, 219, 55–64. [Google Scholar] [CrossRef] [PubMed]
- Jin, H.; Lu, Q.; Gao, F.; Hao, H. Application of oligoclonal bands and other cerebrospinal fluid variables in multiple sclerosis and other neuroimmunological diseases: A narrative review. Ann. Transl. Med. 2023, 11, 282. [Google Scholar] [CrossRef] [PubMed]
- Tourtellotte, W.W.; Parker, J.A. Multiple sclerosis: Correlation between immunoglobulin-G in cerebrospinal fluid and brain. Science 1966, 154, 1044–1045. [Google Scholar] [CrossRef] [PubMed]
- Tourtellotte, W.W.; Parker, J.A. Multiple sclerosis: Brain immunoglobulin-G and albumin. Nature 1967, 214, 683–686. [Google Scholar] [CrossRef] [PubMed]
- Link, H. Oligoclonal immunoglobulin G in multiple sclerosis brains. J. Neurol. Sci. 1972, 16, 103–114. [Google Scholar] [CrossRef] [PubMed]
- Kuhle, J.; Disanto, G.; Dobson, R.; Adiutori, R.; Bianchi, L.; Topping, J.; Bestwick, J.P.; Meier, U.C.; Marta, M.; Dalla Costa, G.; et al. Conversion from clinically isolated syndrome to multiple sclerosis: A large multicentre study. Mult. Scler. 2015, 21, 1013–1024. [Google Scholar] [CrossRef] [PubMed]
- Gastaldi, M.; Zardini, E.; Franciotta, D. An update on the use of cerebrospinal fluid analysis as a diagnostic tool in multiple sclerosis. Expert. Rev. Mol. Diagn. 2017, 17, 31–46. [Google Scholar] [CrossRef]
- Reiber, H.; Felgenhauer, K. Protein transfer at the blood cerebrospinal fluid barrier and the quantitation of the humoral immune response within the central nervous system. Clin. Chim. Acta 1987, 163, 319–328. [Google Scholar] [CrossRef] [PubMed]
- Petzold, A. Intrathecal oligoclonal IgG synthesis in multiple sclerosis. J. Neuroimmunol. 2013, 262, 1–10. [Google Scholar] [CrossRef]
- Reiber, H.; Peter, J.B. Cerebrospinal fluid analysis: Disease-related data patterns and evaluation programs. J. Neurol. Sci. 2001, 184, 101–122. [Google Scholar] [CrossRef]
- Tibbling, G.; Link, H.; Ohman, S. Principles of albumin and IgG analyses in neurological disorders. I. Establishment of reference values. Scand. J. Clin. Lab. Investig. 1977, 37, 385–390. [Google Scholar] [CrossRef] [PubMed]
- Link, H.; Tibbling, G. Principles of albumin and IgG analyses in neurological disorders. III. Evaluation of IgG synthesis within the central nervous system in multiple sclerosis. Scand. J. Clin. Lab. Investig. 1977, 37, 397–401. [Google Scholar] [CrossRef] [PubMed]
- Bonnan, M. Intrathecal IgG synthesis: A resistant and valuable target for future multiple sclerosis treatments. Mult. Scler. Int. 2015, 2015, 296184. [Google Scholar] [CrossRef] [PubMed]
- Auer, M.; Hegen, H.; Zeileis, A.; Deisenhammer, F. Quantitation of intrathecal immunoglobulin synthesis—A new empirical formula. Eur. J. Neurol. 2016, 23, 713–721. [Google Scholar] [CrossRef]
- Boufidou, F.; Vakrakou, A.G.; Anagnostouli, M.; Patas, K.; Paraskevas, G.; Chatzipanagiotou, S.; Stefanis, L.; Evangelopoulos, M.E. An Updated Evaluation of Intrathecal IgG Synthesis Markers in Relation to Oligoclonal Bands. Diagnostics 2023, 13, 389. [Google Scholar] [CrossRef] [PubMed]
- Ferraro, D.; Simone, A.M.; Bedin, R.; Galli, V.; Vitetta, F.; Federzoni, L.; D’Amico, R.; Merelli, E.; Nichelli, P.F.; Sola, P. Cerebrospinal fluid oligoclonal IgM bands predict early conversion to clinically definite multiple sclerosis in patients with clinically isolated syndrome. J. Neuroimmunol. 2013, 257, 76–81. [Google Scholar] [CrossRef] [PubMed]
- Fonderico, M.; Biagioli, T.; Lanzilao, L.; Bellinvia, A.; Fratangelo, R.; Pastò, L.; Prestipino, E.; Razzolini, L.; Tudisco, L.; Ginestroni, A.; et al. Prognostic role of intrathecal IgM synthesis in multiple sclerosis: Results from a clinical series. Mult. Scler. 2021, 27, 198–207. [Google Scholar] [CrossRef] [PubMed]
- Nakano, T.; Matsui, M.; Inoue, I.; Awata, T.; Katayama, S.; Murakoshi, T. Free immunoglobulin light chain: Its biology and implications in diseases. Clin. Chim. Acta 2011, 412, 843–849. [Google Scholar] [CrossRef] [PubMed]
- Brebner, J.A.; Stockley, R.A. Polyclonal free light chains: A biomarker of inflammatory disease or treatment target? F1000 Med. Rep. 2013, 5, 4. [Google Scholar] [CrossRef]
- Goffette, S.; Schluep, M.; Henry, H.; Duprez, T.; Sindic, C.J. Detection of oligoclonal free kappa chains in the absence of oligoclonal IgG in the CSF of patients with suspected multiple sclerosis. J. Neurol. Neurosurg. Psychiatry 2004, 75, 308–310. [Google Scholar] [CrossRef] [PubMed]
- Jenner, E. Serum free light chains in clinical laboratory diagnostics. Clin. Chim. Acta 2014, 427, 15–20. [Google Scholar] [CrossRef] [PubMed]
- Stendahl-Brodin, L.; Link, H. Relation between benign course of multiple sclerosis and low-grade humoral immune response in cerebrospinal fluid. J. Neurol. Neurosurg. Psychiatry 1980, 43, 102–105. [Google Scholar] [CrossRef] [PubMed]
- Konen, F.F.; Schwenkenbecher, P.; Jendretzky, K.F.; Gingele, S.; Sühs, K.W.; Tumani, H.; Süße, M.; Skripuletz, T. The Increasing Role of Kappa Free Light Chains in the Diagnosis of Multiple Sclerosis. Cells 2021, 10, 3056. [Google Scholar] [CrossRef] [PubMed]
- Zeman, D.; Kušnierová, P.; Švagera, Z.; Všianský, F.; Byrtusová, M.; Hradílek, P.; Kurková, B.; Zapletalová, O.; Bartoš, V. Assessment of Intrathecal Free Light Chain Synthesis: Comparison of Different Quantitative Methods with the Detection of Oligoclonal Free Light Chains by Isoelectric Focusing and Affinity-Mediated Immunoblotting. PLoS ONE 2016, 11, e0166556. [Google Scholar] [CrossRef] [PubMed]
- Süße, M.; Hannich, M.; Petersmann, A.; Zylla, S.; Pietzner, M.; Nauck, M.; Dressel, A. Kappa free light chains in cerebrospinal fluid to identify patients with oligoclonal bands. Eur. J. Neurol. 2018, 25, 1134–1139. [Google Scholar] [CrossRef] [PubMed]
- Makshakov, G.; Nazarov, V.; Kochetova, O.; Surkova, E.; Lapin, S.; Evdoshenko, E. Diagnostic and Prognostic Value of the Cerebrospinal Fluid Concentration of Immunoglobulin Free Light Chains in Clinically Isolated Syndrome with Conversion to Multiple Sclerosis. PLoS ONE 2015, 10, e0143375. [Google Scholar] [CrossRef] [PubMed]
- Bayart, J.L.; Muls, N.; van Pesch, V. Free Kappa light chains in neuroinflammatory disorders: Complement rather than substitute? Acta Neurol. Scand. 2018, 138, 352–358. [Google Scholar] [CrossRef] [PubMed]
- Daves, M.; Piccin, A.; Roccaforte, V.; Lippi, G. Comparison of Freelite and N-Latex serum free light chain assays: A critical review. Biochem. Med. 2021, 31, 030701. [Google Scholar] [CrossRef]
- Bradwell, A.R.; Carr-Smith, H.D.; Mead, G.P.; Tang, L.X.; Showell, P.J.; Drayson, M.T.; Drew, R. Highly sensitive, automated immunoassay for immunoglobulin free light chains in serum and urine. Clin. Chem. 2001, 47, 673–680. [Google Scholar] [CrossRef]
- DeCarli, C.; Menegus, M.A.; Rudick, R.A. Free light chains in multiple sclerosis and infections of the CNS. Neurology 1987, 37, 1334–1338. [Google Scholar] [CrossRef] [PubMed]
- Ferraro, D.; Trovati, A.; Bedin, R.; Natali, P.; Franciotta, D.; Santangelo, M.; Camera, V.; Vitetta, F.; Varani, M.; Trenti, T.; et al. Cerebrospinal fluid kappa and lambda free light chains in oligoclonal band-negative patients with suspected multiple sclerosis. Eur. J. Neurol. 2020, 27, 461–467. [Google Scholar] [CrossRef] [PubMed]
- Leurs, C.E.; Twaalfhoven, H.; Lissenberg-Witte, B.I.; van Pesch, V.; Dujmovic, I.; Drulovic, J.; Castellazzi, M.; Bellini, T.; Pugliatti, M.; Kuhle, J.; et al. Kappa free light chains is a valid tool in the diagnostics of MS: A large multicenter study. Mult. Scler. 2020, 26, 912–923. [Google Scholar] [CrossRef] [PubMed]
- Duranti, F.; Pieri, M.; Centonze, D.; Buttari, F.; Bernardini, S.; Dessi, M. Determination of κFLC and κ Index in cerebrospinal fluid: A valid alternative to assess intrathecal immunoglobulin synthesis. J. Neuroimmunol. 2013, 263, 116–120. [Google Scholar] [CrossRef]
- Hegen, H.; Walde, J.; Berek, K.; Arrambide, G.; Gnanapavan, S.; Kaplan, B.; Khalil, M.; Saadeh, R.; Teunissen, C.; Tumani, H.; et al. Cerebrospinal fluid kappa free light chains for the diagnosis of multiple sclerosis: A systematic review and meta-analysis. Mult. Scler. 2023, 29, 169–181. [Google Scholar] [CrossRef] [PubMed]
- Gaetani, L.; Di Carlo, M.; Brachelente, G.; Valletta, F.; Eusebi, P.; Mancini, A.; Gentili, L.; Borrelli, A.; Calabresi, P.; Sarchielli, P.; et al. Cerebrospinal fluid free light chains compared to oligoclonal bands as biomarkers in multiple sclerosis. J. Neuroimmunol. 2020, 339, 577108. [Google Scholar] [CrossRef] [PubMed]
- Hegen, H.; Walde, J.; Milosavljevic, D.; Aboulenein-Djamshidian, F.; Senel, M.; Tumani, H.; Deisenhammer, F.; Presslauer, S. Free light chains in the cerebrospinal fluid. Comparison of different methods to determine intrathecal synthesis. Clin. Chem. Lab. Med. 2019, 57, 1574–1586. [Google Scholar] [CrossRef] [PubMed]
- Cutellè, C.; Balducci, C.; Cereda, D.; Fusco, M.L.; Iacobucci, D.; Perugini, J.; Pirro, F.; Brivio, R.; Bernasconi, D.P.; Ferrarese, C.; et al. K index utility as diagnostic and prognostic biomarker in the assessment of patients with suspected Multiple Sclerosis. J. Neuroimmunol. 2022, 373, 577992. [Google Scholar] [CrossRef] [PubMed]
- Presslauer, S.; Milosavljevic, D.; Huebl, W.; Parigger, S.; Schneider-Koch, G.; Bruecke, T. Kappa free light chains: Diagnostic and prognostic relevance in MS and CIS. PLoS ONE 2014, 9, e89945. [Google Scholar] [CrossRef] [PubMed]
- Hegen, H.; Milosavljevic, D.; Schnabl, C.; Manowiecka, A.; Walde, J.; Deisenhammer, F.; Presslauer, S. Cerebrospinal fluid free light chains as diagnostic biomarker in neuroborreliosis. Clin. Chem. Lab. Med. 2018, 56, 1383–1391. [Google Scholar] [CrossRef]
- Reiber, H.; Zeman, D.; Kušnierová, P.; Mundwiler, E.; Bernasconi, L. Diagnostic relevance of free light chains in cerebrospinal fluid—The hyperbolic reference range for reliable data interpretation in quotient diagrams. Clin. Chim. Acta 2019, 497, 153–162. [Google Scholar] [CrossRef] [PubMed]
- Senel, M.; Mojib-Yezdani, F.; Braisch, U.; Bachhuber, F.; Lewerenz, J.; Ludolph, A.C.; Otto, M.; Tumani, H. CSF Free Light Chains as a Marker of Intrathecal Immunoglobulin Synthesis in Multiple Sclerosis: A Blood-CSF Barrier Related Evaluation in a Large Cohort. Front. Immunol. 2019, 10, 641. [Google Scholar] [CrossRef] [PubMed]
- Presslauer, S.; Milosavljevic, D.; Huebl, W.; Aboulenein-Djamshidian, F.; Krugluger, W.; Deisenhammer, F.; Senel, M.; Tumani, H.; Hegen, H. Validation of kappa free light chains as a diagnostic biomarker in multiple sclerosis and clinically isolated syndrome: A multicenter study. Mult. Scler. 2016, 22, 502–510. [Google Scholar] [CrossRef] [PubMed]
- Gurtner, K.M.; Shosha, E.; Bryant, S.C.; Andreguetto, B.D.; Murray, D.L.; Pittock, S.J.; Willrich, M.A.V. CSF free light chain identification of demyelinating disease: Comparison with oligoclonal banding and other CSF indexes. Clin. Chem. Lab. Med. 2018, 56, 1071–1080. [Google Scholar] [CrossRef] [PubMed]
- Berek, K.; Bsteh, G.; Auer, M.; Di Pauli, F.; Grams, A.; Milosavljevic, D.; Poskaite, P.; Schnabl, C.; Wurth, S.; Zinganell, A.; et al. Kappa-Free Light Chains in CSF Predict Early Multiple Sclerosis Disease Activity. Neurol. Neuroimmunol. Neuroinflamm. 2021, 8, e1005. [Google Scholar] [CrossRef] [PubMed]
- Salavisa, M.; Paixão, P.; Ladeira, A.F.; Mendes, A.; Correia, A.S.; Viana, J.F.; Viana-Baptista, M. Prognostic value of kappa free light chains determination in first-ever multiple sclerosis relapse. J. Neuroimmunol. 2020, 347, 577355. [Google Scholar] [CrossRef] [PubMed]
- Alves Martins, D.; Lopes, J.; Martins da Silva, A.; Morais, C.I.; Vasconcelos, J.; Lima, I.; Carneiro, C.; Neves, E. Kappa free light chains: Diagnostic performance in multiple sclerosis and utility in a clinical laboratory. Clin. Chim. Acta 2022, 528, 56–64. [Google Scholar] [CrossRef]
- Teunissen, C.; Menge, T.; Altintas, A.; Álvarez-Cermeño, J.C.; Bertolotto, A.; Berven, F.S.; Brundin, L.; Comabella, M.; Degn, M.; Deisenhammer, F.; et al. Consensus definitions and application guidelines for control groups in cerebrospinal fluid biomarker studies in multiple sclerosis. Mult. Scler. 2013, 19, 1802–1809. [Google Scholar] [CrossRef]
- Passerini, G.; Dalla Costa, G.; Sangalli, F.; Moiola, L.; Colombo, B.; Locatelli, M.; Comi, G.; Furlan, R.; Martinelli, V. Free Light Chains and Intrathecal B Cells Activity in Multiple Sclerosis: A Prospective Study and Meta-Analysis. Mult. Scler. Int. 2016, 2016, 2303857. [Google Scholar] [CrossRef]
- Emersic, A.; Anadolli, V.; Krsnik, M.; Rot, U. Intrathecal immunoglobulin synthesis: The potential value of an adjunct test. Clin. Chim. Acta 2019, 489, 109–116. [Google Scholar] [CrossRef]
- Sanz Diaz, C.T.; de Las Heras Flórez, S.; Carretero Perez, M.; Hernández Pérez, M.Á.; Martín García, V. Evaluation of Kappa Index as a Tool in the Diagnosis of Multiple Sclerosis: Implementation in Routine Screening Procedure. Front. Neurol. 2021, 12, 676527. [Google Scholar] [CrossRef] [PubMed]
- Rosenstein, I.; Rasch, S.; Axelsson, M.; Novakova, L.; Blennow, K.; Zetterberg, H.; Lycke, J. Kappa free light chain index as a diagnostic biomarker in multiple sclerosis: A real-world investigation. J. Neurochem. 2021, 159, 618–628. [Google Scholar] [CrossRef] [PubMed]
- Ferraro, D.; Bedin, R.; Natali, P.; Franciotta, D.; Smolik, K.; Santangelo, M.; Immovilli, P.; Camera, V.; Vitetta, F.; Gastaldi, M.; et al. Kappa Index Versus CSF Oligoclonal Bands in Predicting Multiple Sclerosis and Infectious/Inflammatory CNS Disorders. Diagnostics 2020, 10, 856. [Google Scholar] [CrossRef] [PubMed]
- Christiansen, M.; Gjelstrup, M.C.; Stilund, M.; Christensen, T.; Petersen, T.; Jon Møller, H. Cerebrospinal fluid free kappa light chains and kappa index perform equal to oligoclonal bands in the diagnosis of multiple sclerosis. Clin. Chem. Lab. Med. 2018, 57, 210–220. [Google Scholar] [CrossRef]
- Presslauer, S.; Milosavljevic, D.; Brücke, T.; Bayer, P.; Hübl, W. Elevated levels of kappa free light chains in CSF support the diagnosis of multiple sclerosis. J. Neurol. 2008, 255, 1508–1514. [Google Scholar] [CrossRef] [PubMed]
- Valencia-Vera, E.; Martinez-Escribano Garcia-Ripoll, A.; Enguix, A.; Abalos-Garcia, C.; Segovia-Cuevas, M.J. Application of κ free light chains in cerebrospinal fluid as a biomarker in multiple sclerosis diagnosis: Development of a diagnosis algorithm. Clin. Chem. Lab. Med. 2018, 56, 609–613. [Google Scholar] [CrossRef] [PubMed]
- Marlas, M.; Bost, C.; Dorcet, G.; Delourme, A.; Biotti, D.; Ciron, J.; Renaudineau, Y.; Puissant-Lubrano, B. Kappa-index: Real-life evaluation of a new tool for multiple sclerosis diagnosis. Clin. Immunol. 2022, 241, 109066. [Google Scholar] [CrossRef] [PubMed]
- Menéndez-Valladares, P.; García-Sánchez, M.I.; Cuadri Benítez, P.; Lucas, M.; Adorna Martínez, M.; Carranco Galán, V.; García De Veas Silva, J.L.; Bermudo Guitarte, C.; Izquierdo Ayuso, G. Free kappa light chains in cerebrospinal fluid as a biomarker to assess risk conversion to multiple sclerosis. Mult. Scler. J. Exp. Transl. Clin. 2015, 1, 2055217315620935. [Google Scholar] [CrossRef] [PubMed]
- Paul, A.; Comabella, M.; Gandhi, R. Biomarkers in Multiple Sclerosis. Cold Spring Harb. Perspect. Med. 2019, 9, a029058. [Google Scholar] [CrossRef]
- Yang, J.; Hamade, M.; Wu, Q.; Wang, Q.; Axtell, R.; Giri, S.; Mao-Draayer, Y. Current and Future Biomarkers in Multiple Sclerosis. Int. J. Mol. Sci. 2022, 23, 5877. [Google Scholar] [CrossRef]
- Kim, J.S. Protein biomarkers in multiple sclerosis. Encephalitis 2023, 3, 54–63. [Google Scholar] [CrossRef] [PubMed]
- Bridel, C.; van Wieringen, W.N.; Zetterberg, H.; Tijms, B.M.; Teunissen, C.E.; the NFL Group; Alvarez-Cermeño, J.C.; Andreasson, U.; Axelsson, M.; Bäckström, D.C.; et al. Diagnostic Value of Cerebrospinal Fluid Neurofilament Light Protein in Neurology: A Systematic Review and Meta-analysis. JAMA Neurol. 2019, 76, 1035–1048. [Google Scholar] [CrossRef] [PubMed]
- Bittner, S.; Oh, J.; Havrdová, E.K.; Tintoré, M.; Zipp, F. The potential of serum neurofilament as biomarker for multiple sclerosis. Brain 2021, 144, 2954–2963. [Google Scholar] [CrossRef] [PubMed]
- Benkert, P.; Meier, S.; Schaedelin, S.; Manouchehrinia, A.; Yaldizli, Ö.; Maceski, A.; Oechtering, J.; Achtnichts, L.; Conen, D.; Derfuss, T.; et al. Serum neurofilament light chain for individual prognostication of disease activity in people with multiple sclerosis: A retrospective modelling and validation study. Lancet Neurol. 2022, 21, 246–257. [Google Scholar] [CrossRef] [PubMed]
- Giuliano, P.; La Rosa, G.; Capozzi, S.; Cassano, E.; Damiano, S.; Habetswallner, F.; Iodice, R.; Marra, M.; Pavone, L.M.; Quarantelli, M.; et al. A Blood Test for the Diagnosis of Multiple Sclerosis. Int. J. Mol. Sci. 2024, 25, 1696. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.C.; Yang, X.; Miao, L.; Liu, Z.G.; Li, W.; Zhao, Z.X.; Sun, X.J.; Jiang, G.X.; Chen, S.D.; Cheng, Q. Serum level of interleukin-6 in Chinese patients with multiple sclerosis. J. Neuroimmunol. 2012, 249, 109–111. [Google Scholar] [CrossRef] [PubMed]
- Schneider, R.; Mohebiany, A.N.; Ifergan, I.; Beauseigle, D.; Duquette, P.; Prat, A.; Arbour, N. B cell-derived IL-15 enhances CD8 T cell cytotoxicity and is increased in multiple sclerosis patients. J. Immunol. 2011, 187, 4119–4128. [Google Scholar] [CrossRef]
- Kowarik, M.C.; Cepok, S.; Sellner, J.; Grummel, V.; Weber, M.S.; Korn, T.; Berthele, A.; Hemmer, B. CXCL13 is the major determinant for B cell recruitment to the CSF during neuroinflammation. J. Neuroinflamm. 2012, 9, 93. [Google Scholar] [CrossRef] [PubMed]
- Mouzaki, A.; Rodi, M.; Dimisianos, N.; Emmanuil, A.; Kalavrizioti, D.; Lagoudaki, R.; Grigoriadis, N.C.; Papathanasopoulos, P. Immune Parameters That Distinguish Multiple Sclerosis Patients from Patients with Other Neurological Disorders at Presentation. PLoS ONE 2015, 10, e0135434, Erratum in: PLoS ONE 2016, 11, e0151411. [Google Scholar] [CrossRef]
- Dobson, R.; Miller, R.F.; Palmer, H.E.; Feldmann, M.; Thompson, E.J.; Thompson, A.J.; Miller, D.H.; Giovannoni, G. Increased urinary free immunoglobulin light chain excretion in patients with multiple sclerosis. J. Neuroimmunol. 2010, 220, 99–103. [Google Scholar] [CrossRef]
- Lotan, I.; Ganelin-Cohen, E.; Tartakovsky, E.; Khasminsky, V.; Hellmann, M.A.; Steiner, I.; Ben-Zvi, I.; Livneh, A.; Golderman, S.; Kaplan, B. Saliva immunoglobulin free light chain analysis for monitoring disease activity and response to treatment in multiple sclerosis. Mult. Scler. Relat. Disord. 2020, 44, 102339. [Google Scholar] [CrossRef]
- Król-Grzymała, A.; Sienkiewicz-Szłapka, E.; Fiedorowicz, E.; Rozmus, D.; Cieślińska, A.; Grzybowski, A. Tear Biomarkers in Alzheimer’s and Parkinson’s Diseases, and Multiple Sclerosis: Implications for Diagnosis (Systematic Review). Int. J. Mol. Sci. 2022, 23, 10123. [Google Scholar] [CrossRef]
- Casamassimi, A.; Federico, A.; Rienzo, M.; Esposito, S.; Ciccodicola, A. Transcriptome Profiling in Human Diseases: New Advances and Perspectives. Int. J. Mol. Sci. 2017, 18, 1652. [Google Scholar] [CrossRef]
- Husseini, L.; Geladaris, A.; Weber, M.S. Toward identifying key mechanisms of progression in multiple sclerosis. Trends Neurosci. 2024, 47, 58–70. [Google Scholar] [CrossRef]
- Elkjaer, M.L.; Röttger, R.; Baumbach, J.; Illes, Z. A Systematic Review of Tissue and Single Cell Transcriptome/Proteome Studies of the Brain in Multiple Sclerosis. Front. Immunol. 2022, 13, 761225. [Google Scholar] [CrossRef] [PubMed]
- Chiricosta, L.; Blando, S.; D’Angiolini, S.; Gugliandolo, A.; Mazzon, E. A Comprehensive Exploration of the Transcriptomic Landscape in Multiple Sclerosis: A Systematic Review. Int. J. Mol. Sci. 2023, 24, 1448. [Google Scholar] [CrossRef]
- Schafflick, D.; Xu, C.A.; Hartlehnert, M.; Cole, M.; Schulte-Mecklenbeck, A.; Lautwein, T.; Wolbert, J.; Heming, M.; Meuth, S.G.; Kuhlmann, T.; et al. Integrated single cell analysis of blood and cerebrospinal fluid leukocytes in multiple sclerosis. Nat. Commun. 2020, 11, 247. [Google Scholar] [CrossRef]
- Gill, A.J.; Schorr, E.M.; Gadani, S.P.; Calabresi, P.A. Emerging imaging and liquid biomarkers in multiple sclerosis. Eur. J. Immunol. 2023, 53, e2250228. [Google Scholar] [CrossRef]
- Doghish, A.S.; Elazazy, O.; Mohamed, H.H.; Mansour, R.M.; Ghanem, A.; Faraag, A.H.I.; Elballal, M.S.; Elrebehy, M.A.; Elesawy, A.E.; Abdel Mageed, S.S.; et al. The role of miRNAs in multiple sclerosis pathogenesis, diagnosis, and therapeutic resistance. Pathol. Res. Pract. 2023, 251, 154880. [Google Scholar] [CrossRef]
- Sandi, D.; Kokas, Z.; Biernacki, T.; Bencsik, K.; Klivényi, P.; Vécsei, L. Proteomics in Multiple Sclerosis: The Perspective of the Clinician. Int. J. Mol. Sci. 2022, 23, 5162. [Google Scholar] [CrossRef]
- Åkesson, J.; Hojjati, S.; Hellberg, S.; Raffetseder, J.; Khademi, M.; Rynkowski, R.; Kockum, I.; Altafini, C.; Lubovac-Pilav, Z.; Mellergård, J.; et al. Proteomics reveal biomarkers for diagnosis, disease activity and long-term disability outcomes in multiple sclerosis. Nat. Commun. 2023, 14, 6903. [Google Scholar] [CrossRef] [PubMed]
- Benallegue, N.; Nicol, B.; Lasselin, J.; Bézie, S.; Flippe, L.; Regue, H.; Vimond, N.; Remy, S.; Garcia, A.; Le Frère, F.; et al. Patients With Severe Multiple Sclerosis Exhibit Functionally Altered CD8+ Regulatory T Cells. Neurol. Neuroimmunol. Neuroinflamm. 2022, 9, e200016. [Google Scholar] [CrossRef] [PubMed]
- Brune-Ingebretsen, S.; Høgestøl, E.A.; de Rosbo, N.K.; Berg-Hansen, P.; Brunborg, C.; Blennow, K.; Zetterberg, H.; Paul, F.; Uccelli, A.; Villoslada, P.; et al. Immune cell subpopulations and serum neurofilament light chain are associated with increased risk of disease worsening in multiple sclerosis. J. Neuroimmunol. 2023, 382, 578175. [Google Scholar] [CrossRef] [PubMed]
- Miteva, D.; Vasilev, G.V.; Velikova, T. Role of Specific Autoantibodies in Neurodegenerative Diseases: Pathogenic Antibodies or Promising Biomarkers for Diagnosis. Antibodies 2023, 12, 81. [Google Scholar] [CrossRef] [PubMed]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Maglio, G.; D’Agostino, M.; Caronte, F.P.; Pezone, L.; Casamassimi, A.; Rienzo, M.; Di Zazzo, E.; Nappo, C.; Medici, N.; Molinari, A.M.; et al. Multiple Sclerosis: From the Application of Oligoclonal Bands to Novel Potential Biomarkers. Int. J. Mol. Sci. 2024, 25, 5412. https://doi.org/10.3390/ijms25105412
Maglio G, D’Agostino M, Caronte FP, Pezone L, Casamassimi A, Rienzo M, Di Zazzo E, Nappo C, Medici N, Molinari AM, et al. Multiple Sclerosis: From the Application of Oligoclonal Bands to Novel Potential Biomarkers. International Journal of Molecular Sciences. 2024; 25(10):5412. https://doi.org/10.3390/ijms25105412
Chicago/Turabian StyleMaglio, Grazia, Marina D’Agostino, Francesco Pio Caronte, Luciano Pezone, Amelia Casamassimi, Monica Rienzo, Erika Di Zazzo, Carmela Nappo, Nicola Medici, Anna Maria Molinari, and et al. 2024. "Multiple Sclerosis: From the Application of Oligoclonal Bands to Novel Potential Biomarkers" International Journal of Molecular Sciences 25, no. 10: 5412. https://doi.org/10.3390/ijms25105412
APA StyleMaglio, G., D’Agostino, M., Caronte, F. P., Pezone, L., Casamassimi, A., Rienzo, M., Di Zazzo, E., Nappo, C., Medici, N., Molinari, A. M., & Abbondanza, C. (2024). Multiple Sclerosis: From the Application of Oligoclonal Bands to Novel Potential Biomarkers. International Journal of Molecular Sciences, 25(10), 5412. https://doi.org/10.3390/ijms25105412









