Exudative versus Nonexudative Age-Related Macular Degeneration: Physiopathology and Treatment Options
Abstract
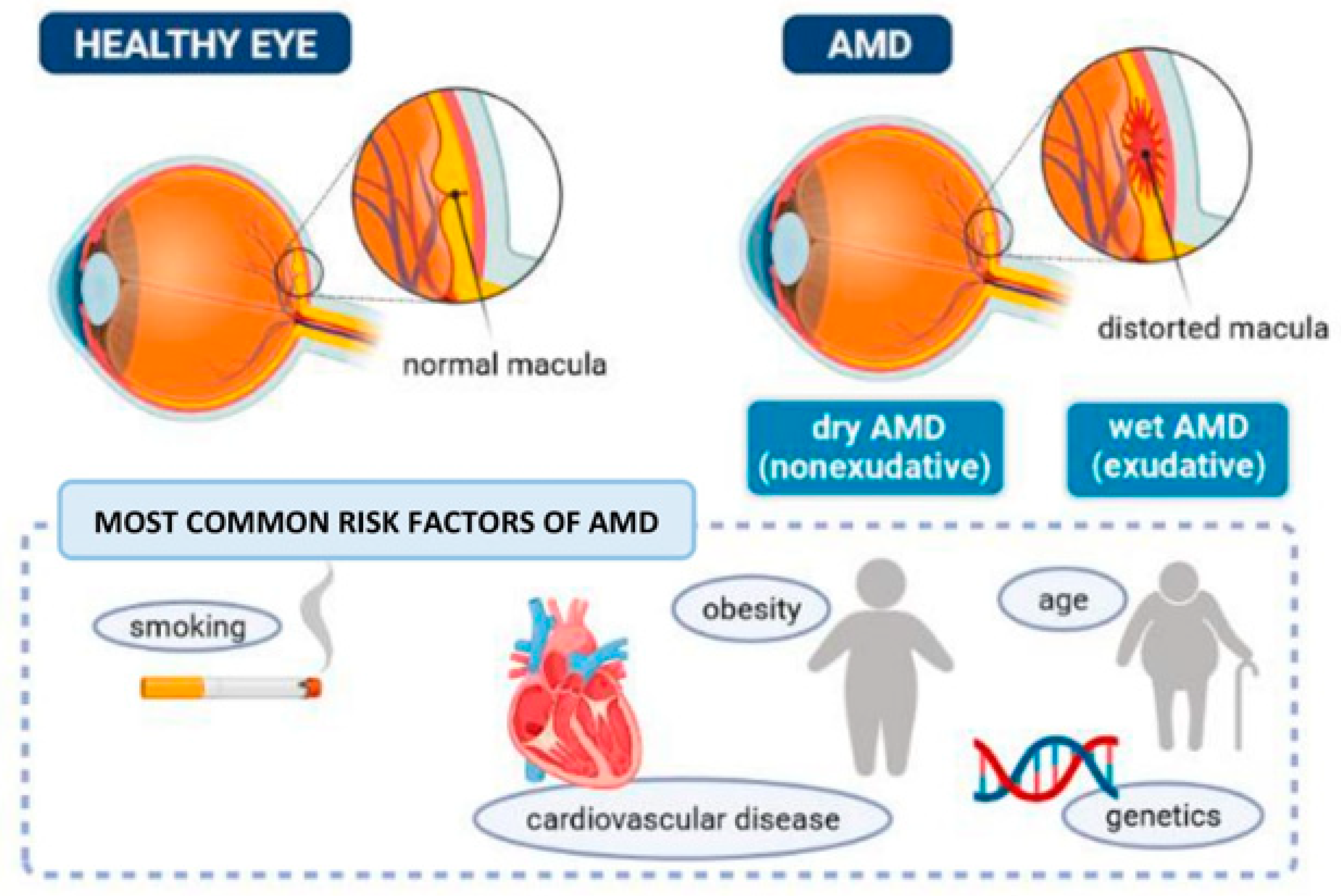
1. Introduction
| Race | Sex | Age | Prevalence | Prognosis | References | |
|---|---|---|---|---|---|---|
| Exudative AMD | Caucasian people are far more likely to have wet AMD and vision loss compared with black people and Hispanics. | Women have an increased risk for AMD when compared with men. | There is a positive correlation between the prevalence and progression of the disease with aging. | In the United States, AMD occurs in 10% of the population aged between 65 and 74 years and in 25% of population with more than 74 years. 10% to 20% of people with nonexudative AMD progress to exudative disease. | The prognosis for exudative AMD is significantly worse when compared with nonexudative AMD. | [29,30,31] |
| Nonexudative AMD | Higher incidence in Caucasian people (especially in patients with light-colored eyes) compared with African Americans. Incidence in Asians is increasing. | Unknown difference between women and men. | The disease prevalence increases in each decade of life. More common in patients older than 70 years. | In the United States: -AMD is the principal cause of blindness in people older than 50 years. -In population older than 60 years the prevalence is greater than 20%. -Late atrophy and CNV have an incidence of 0% in patients with 50 years or less. In patients with 70 years the incidence is 2% and at 80 years the prevalence is 6%. | Better prognosis when compared with wet AMD. People with nonexudative AMD will have steady gradual deterioration of visual acuity. Is usual to have other visual dysfunctions, i.e., loss of contrast sensitivity. | [31,32,33,34] |
2. Age-Related Macular Degeneration Classification Systems
3. Exudative Age-Related Macular Degeneration (Wet AMD)
3.1. Clinical Presentation
3.2. Pharmacological Treatments
| Formulation | Administration | Mechanism of Action | Results | Approval | References | |
|---|---|---|---|---|---|---|
| Aflibercept | Fusion protein | Intravitreal injection, 2 mg monthly or every 2 months | Connection to all forms of VEGF-A | Safety and tolerability with similar visual results than ranibizumab. Aflibercept enhanced vision, i.e., 96%, 95%, and 95% of patients taking injections of 0.5 mg monthly, 2 mg monthly, and 2 mg every 2 months, respectively. | Approved for the first time in November 2011. August 2018 approval of the administration of Aflibercept every 12 weeks after the first 1 year of effective treatment. | [90] |
| Bevacizumab | Humanized full length humanized monoclonal antibody | Infusion, 5 mg/kg every 2 weeks for 2–3 treatments | Off-label VEGF inhibitor | Increase in mean visual acuity and central retinal thickness. Bevacizumab had comparable effectiveness compared with ranibizumab on visual acuity after 1 year of treatment. | FDA has not approved bevacizumab for ocular indications. | [91,92] |
| Brolucizumab | Humanized single-chain antibody fragment (scFv) | Intravitreal injection, 6 mg every month for 3 months, then, some patients were maintained over 2 or 3 months dosing interval | Small molecule with high affinity to all VEGF-A isoforms; inhibition of activation of the receptors of VEGF and consequent avoidance of the ligand-receptor interaction | Compared with aflibercept, showed non inferiority in mean change in best corrected visual acuity in one year. Reduction occurred in central subfield thickness. Few patients had intra-retinal and/or sub-retinal fluid. These fluids are a marker of AMD. | Approved in October 2019. | [93] |
| Pegaptanib sodium | Polyethylene glycol conjugated oligonucleotide | Intravitreal injection of 0.3 mg every 6 weeks | Connection and neutralization of VEGF165 (principal VEGF isomer in CNV) | Safety and efficacy. Risk of severe loss of visual acuity was reduced from 22% in placebo group to 10% in the group treated with pegaptanib sodium. Patients preserved their visual acuity (33%) or increased acuity (23%). | Food and Drug Administration (FDA) approved in 2004. | [94] |
| Ranibizumab | Humanized fragmented monoclonal antibody | 24 monthly intravitreal injections of 0.3 or 0.5 mg | Connection and inhibition of isoforms of VEGF | After 12 months of accompaniment, 95% of patients had enhanced or stable vision in both dosages. The visual acuity increased 24.8% with 0.3 mg and 33.8% with 0.5 mg. These results were maintained for 24 months. | FDA approved in 2006. | [81] |
| Title | EudraCT Number | Medical Condition | Sponsor Name | Start Date |
|---|---|---|---|---|
| Predictability of response of aflibercept treatment for wet age-related macular degeneration under the treat-and-moderate extend regimen (TMER) treatment model | 2015-001394-41 | Wet AMD | Raimo Tuuminen | 2015-06-10 |
| The effect of intravitreal bevacizumab injections in patients with macular oedema caused by AMD, CRVO or DME on the plasticity of nerves studied by visual evoked potentials | 2012-000765-20 | Wet AMD, diabetic macular edema, central retinal vein occlusion | Kuopion yliopistollinen sairaala/silmätautien poliklinikka | 2015-11-27 |
| The effect of intravitreal aflibercept on ocular perfusion—a pilot study | 2016-004608-78 | Wet AMD | Kepler University Hospital, Institute of Ophthalmology | 2017-03-03 |
| Evaluation the pharmacokinetics, safety, tolerability of single intravitreal injection RC28-E in subjects with wet AMD | ClinicalTrials.gov Identifier: NCT03777254 | Wet AMD | RemeGen Co., Ltd. | 2018-12-17 |
| Safety, tolerability and pharmacodynamics of single rising intravitreal and multiple rising intravitreal doses of BI 836880 in patients with wet AMD (open label, non-randomized, uncontrolled) | 2017-001221-40 | Wet AMD | Boehringer Ingelheim Pharma GmbH & Co. KG | 2019-05-06 |
| Zoledronic acid as adjuvant therapy in neovascular age-related macular degeneration (The Z-AMD study): a randomized controlled pilot study | 2019-001492-37 | Wet AMD | Oslo University Hospital | 2019-11-01 |
| Long-term study of ADVM-022 in neovascular AMD | ClinicalTrials.gov Identifier: NCT04645212 | Wet AMD | Adverum Biotechnologies, Inc. | 2020-11-27 |
| RGX-314 gene therapy pharmacodynamic study for neovascular AMD | ClinicalTrials.gov Identifier: NCT04832724 | Wet AMD | Regenxbio Inc. | 2021-02-22 |
| A multicenter, open-label extension study to evaluate the long-term safety and tolerability of faricimab in patients with neovascular age-related macular degeneration | 2020-004523-16 | Neovascular age-related macular degeneration (nAMD) | F. Hoffmann La-Roche Ltd. | 2021-04-12 |
| A phase 3, multicentre, double-masked, randomised study to evaluate the efficacy and safety of intravitreal OPT-302 in combination with aflibercept, compared with aflibercept alone, in participants with wet AMD | 2020-004694-46 | Wet AMD | Opthea Limited | 2021-08-06 |
| A phase 3 open-label, multicenter, extension study to evaluate the long-term safety and efficacy of pegcetacoplan in subjects with geographic atrophy secondary to age-related macular degeneration | 2020-002931-32 | Geographic atrophy secondary to AMD | Apellis Pharmaceuticals Inc. | 2021-09-17 |
| A study to evaluate the efficacy and safety of intravitreal KSI-301 compared with intravitreal aflibercept in participants with neovascular (wet) age-related macular degeneration (DAYLIGHT) | 2021-000225-27 | Wet AMD | Kodiak Sciences Inc. | 2021-10-26 |
3.3. Combination Therapies
| Techniques | Drug | Results | References |
|---|---|---|---|
| PDT (reduced-fluence) | Bevacizumab |
| [122] |
| PDT (standard-fluence) |
| [123] | |
| Verteporfin PDT | Ranibizumab |
| [124] |
| Stereotactic radiotherapy |
| [125] |
4. Nonexudative Age-Related Macular Degeneration (Dry AMD)
4.1. Clinical Presentation
4.2. Pharmacological Treatments
5. Retinal Imaging Studies Used in Both Wet and Dry AMD
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- De Jong, S.; Gagliardi, G.; Garanto, A.; de Breuk, A.; Lechanteur, Y.T.E.; Katti, S.; van den Heuvel, L.P.; Volokhina, E.B.; den Hollander, A.I. Implications of genetic variation in the complement system in age-related macular degeneration. Prog. Retin. Eye Res. 2021, 84, 100952. [Google Scholar] [CrossRef]
- Stahl, A. The Diagnosis and Treatment of Age-Related Macular Degeneration. Dtsch. Arztebl. Int. 2020, 117, 513–520. [Google Scholar] [CrossRef] [PubMed]
- Xu, X.; Wu, J.; Yu, X.; Tang, Y.; Tang, X.; Shentu, X. Regional differences in the global burden of age-related macular degeneration. BMC Public Health 2020, 20, 410. [Google Scholar] [CrossRef]
- Wong, W.L.; Su, X.; Li, X.; Cheung, C.M.G.; Klein, R.; Cheng, C.-Y.; Wong, T.Y. Global prevalence of age-related macular degeneration and disease burden projection for 2020 and 2040: A systematic review and meta-analysis. Lancet Glob. Health 2014, 2, e106–e116. [Google Scholar] [CrossRef]
- Brandl, C.; Zimmermann, M.E.; Günther, F.; Barth, T.; Olden, M.; Schelter, S.C.; Kronenberg, F.; Loss, J.; Küchenhoff, H.; Helbig, H. On the impact of different approaches to classify age-related macular degeneration: Results from the German AugUR study. Sci. Rep. 2018, 8, 8675. [Google Scholar] [CrossRef]
- Korb, C.A.; Kottler, U.B.; Wolfram, C.; Hoehn, R.; Schulz, A.; Zwiener, I.; Wild, P.S.; Pfeiffer, N.; Mirshahi, A. Prevalence of age-related macular degeneration in a large European cohort: Results from the population-based Gutenberg Health Study. Graefe’s Arch. Clin. Exp. Ophthalmol. 2014, 252, 1403–1411. [Google Scholar] [CrossRef] [PubMed]
- Xu, K.; Gupta, V.; Bae, S.; Sharma, S. Metamorphopsia and vision-related quality of life among patients with age-related macular degeneration. Can. J. Ophthalmol. 2018, 53, 168–172. [Google Scholar] [CrossRef]
- Brody, B.L.; Gamst, A.C.; Williams, R.A.; Smith, A.R.; Lau, P.W.; Dolnak, D.; Rapaport, M.H.; Kaplan, R.M.; Brown, S.I. Depression, visual acuity, comorbidity, and disability associated with age-related macular degeneration. Ophthalmology 2001, 108, 1893–1900. [Google Scholar] [CrossRef]
- Casten, R.J.; Rovner, B.W.; Tasman, W. Age-related macular degeneration and depression: A review of recent research. Curr. Opin. Ophthalmol. 2004, 15, 181–183. [Google Scholar] [CrossRef]
- Coleman, A.L.; Stone, K.; Ewing, S.K.; Nevitt, M.; Cummings, S.; Cauley, J.A.; Ensrud, K.E.; Harris, E.L.; Hochberg, M.C.; Mangione, C.M. Higher risk of multiple falls among elderly women who lose visual acuity. Ophthalmology 2004, 111, 857–862. [Google Scholar] [CrossRef]
- Christen, W.G.; Schaumberg, D.A.; Glynn, R.J.; Buring, J.E. Dietary ω-3 fatty acid and fish intake and incident age-related macular degeneration in women. Arch. Ophthalmol. 2011, 129, 921–929. [Google Scholar] [CrossRef] [PubMed]
- Seddon, J.M.; George, S.; Rosner, B. Cigarette smoking, fish consumption, omega-3 fatty acid intake, and associations with age-related macular degeneration: The US Twin Study of Age-Related Macular Degeneration. Arch. Ophthalmol. 2006, 124, 995–1001. [Google Scholar] [CrossRef] [PubMed]
- Seddon, J.M. Macular degeneration epidemiology: Nature-Nurture, lifestyle factors, genetic risk, and gene-environment interactions—The Weisenfeld Award Lecture. Investig. Ophthalmol. Vis. Sci. 2017, 58, 6513–6528. [Google Scholar] [CrossRef]
- Fleckenstein, M.; Keenan, T.D.L.; Guymer, R.H.; Chakravarthy, U.; Schmitz-Valckenberg, S.; Klaver, C.C.; Wong, W.T.; Chew, E.Y. Age-related macular degeneration. Nat. Rev. Dis. Primers 2021, 7, 31. [Google Scholar] [CrossRef]
- Klein, R.J.; Zeiss, C.; Chew, E.Y.; Tsai, J.Y.; Sackler, R.S.; Haynes, C.; Henning, A.K.; SanGiovanni, J.P.; Mane, S.M.; Mayne, S.T.; et al. Complement factor H polymorphism in age-related macular degeneration. Science 2005, 308, 385–389. [Google Scholar] [CrossRef] [PubMed]
- Maller, J.; George, S.; Purcell, S.; Fagerness, J.; Altshuler, D.; Daly, M.J.; Seddon, J.M. Common variation in three genes, including a noncoding variant in CFH, strongly influences risk of age-related macular degeneration. Nat. Genet. 2006, 38, 1055–1059. [Google Scholar] [CrossRef] [PubMed]
- Spencer, K.L.; Olson, L.M.; Anderson, B.M.; Schnetz-Boutaud, N.; Scott, W.K.; Gallins, P.; Agarwal, A.; Postel, E.A.; Pericak-Vance, M.A.; Haines, J.L. C3 R102G polymorphism increases risk of age-related macular degeneration. Hum. Mol. Genet. 2008, 17, 1821–1824. [Google Scholar] [CrossRef]
- Baas, D.C.; Ho, L.; Ennis, S.; Merriam, J.E.; Tanck, M.W.; Uitterlinden, A.G.; de Jong, P.T.; Cree, A.J.; Griffiths, H.L.; Rivadeneira, F.; et al. The complement component 5 gene and age-related macular degeneration. Ophthalmology 2010, 117, 500–511. [Google Scholar] [CrossRef]
- Gold, B.; Merriam, J.E.; Zernant, J.; Hancox, L.S.; Taiber, A.J.; Gehrs, K.; Cramer, K.; Neel, J.; Bergeron, J.; Barile, G.R. Variation in factor B (BF) and complement component 2 (C2) genes is associated with age-related macular degeneration. Nat. Genet. 2006, 38, 458–462. [Google Scholar] [CrossRef]
- Hageman, G.S.; Anderson, D.H.; Johnson, L.V.; Hancox, L.S.; Taiber, A.J.; Hardisty, L.I.; Hageman, J.L.; Stockman, H.A.; Borchardt, J.D.; Gehrs, K.M. A common haplotype in the complement regulatory gene factor H (HF1/CFH) predisposes individuals to age-related macular degeneration. Proc. Natl. Acad. Sci. USA 2005, 102, 7227–7232. [Google Scholar] [CrossRef]
- Esparza-Gordillo, J.; Soria, J.M.; Buil, A.; Almasy, L.; Blangero, J.; Fontcuberta, J.; De Córdoba, S.R. Genetic and environmental factors influencing the human factor H plasma levels. Immunogenetics 2004, 56, 77–82. [Google Scholar] [CrossRef]
- Sepp, T.; Khan, J.C.; Thurlby, D.A.; Shahid, H.; Clayton, D.G.; Moore, A.T.; Bird, A.C.; Yates, J.R. Complement factor H variant Y402H is a major risk determinant for geographic atrophy and choroidal neovascularization in smokers and nonsmokers. Investig. Ophthalmol. Vis. Sci. 2006, 47, 536–540. [Google Scholar] [CrossRef] [PubMed]
- Knickelbein, J.E.; Chan, C.-C.; Sen, H.N.; Ferris, F.L.; Nussenblatt, R.B. Inflammatory Mechanisms of Age-related Macular Degeneration. Int. Ophthalmol. Clin. 2015, 55, 63–78. [Google Scholar] [CrossRef] [PubMed]
- Cao, S.; Ko, A.; Partanen, M.; Pakzad-Vaezi, K.; Merkur, A.B.; Albiani, D.A.; Kirker, A.W.; Wang, A.; Cui, J.Z.; Forooghian, F.; et al. Relationship between systemic cytokines and complement factor H Y402H polymorphism in patients with dry age-related macular degeneration. Am. J. Ophthalmol. 2013, 156, 1176–1183. [Google Scholar] [CrossRef] [PubMed]
- Jonas, J.B.; Jonas, R.A.; Neumaier, M.; Findeisen, P. Cytokine concentration in aqueous humor of eyes with diabetic macular edema. Retina 2012, 32, 2150–2157. [Google Scholar] [CrossRef]
- Jonas, J.B.; Tao, Y.; Neumaier, M.; Findeisen, P. Cytokine concentration in aqueous humour of eyes with exudative age-related macular degeneration. Acta Ophthalmol. 2012, 90, e381–e388. [Google Scholar] [CrossRef]
- Chen, M.; Xu, H. Parainflammation, chronic inflammation, and age-related macular degeneration. J. Leukoc. Biol. 2015, 98, 713–725. [Google Scholar] [CrossRef]
- Medzhitov, R. Origin and physiological roles of inflammation. Nature 2008, 454, 428–435. [Google Scholar] [CrossRef]
- Armstrong, R.A.; Mousavi, M. Overview of risk factors for age-related macular degeneration (AMD). J. Stem Cells 2015, 10, 171. [Google Scholar]
- Yashkin, A.P.; Hahn, P.; Sloan, F.A. Introducing anti-vascular endothelial growth factor therapies for AMD did not raise risk of myocardial infarction, stroke, and death. Ophthalmology 2016, 123, 2225–2231. [Google Scholar] [CrossRef]
- Lim, L.S.; Mitchell, P.; Seddon, J.M.; Holz, F.G.; Wong, T.Y. Age-related macular degeneration. Lancet 2012, 379, 1728–1738. [Google Scholar] [CrossRef]
- Mitchell, P.; Liew, G.; Gopinath, B.; Wong, T.Y. Age-related macular degeneration. Lancet 2018, 392, 1147–1159. [Google Scholar] [CrossRef]
- Modenese, A.; Gobba, F. Macular degeneration and occupational risk factors: A systematic review. Int. Arch. Occup. Environ. Health 2019, 92, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Colijn, J.M.; Buitendijk, G.H.; Prokofyeva, E.; Alves, D.; Cachulo, M.L.; Khawaja, A.P.; Cougnard-Gregoire, A.; Merle, B.M.; Korb, C.; Erke, M.G. Prevalence of age-related macular degeneration in Europe: The past and the future. Ophthalmology 2017, 124, 1753–1763. [Google Scholar] [CrossRef] [PubMed]
- Jones, M.; Whitton, C.; Tan, A.G.; Holliday, E.G.; Oldmeadow, C.; Flood, V.M.; Sim, X.; Chai, J.-F.; Hamzah, H.; Klein, R.; et al. Exploring Factors Underlying Ethnic Difference in Age-related Macular Degeneration Prevalence. Ophthalmic Epidemiol. 2020, 27, 399–408. [Google Scholar] [CrossRef]
- Al-Zamil, W.M.; Yassin, S.A. Recent developments in age-related macular degeneration: A review. Clin. Interv. Aging 2017, 12, 1313–1330. [Google Scholar] [CrossRef]
- Friedman, D.S.; O’Colmain, B.J.; Munoz, B.; Tomany, S.C.; McCarty, C.; De Jong, P.; Nemesure, B.; Mitchell, P.; Kempen, J. Prevalence of age-related macular degeneration in the United States. Arch. Ophthalmol. 2004, 122, 564–572. [Google Scholar]
- Ratnayake, K.; Payton, J.L.; Lakmal, O.H.; Karunarathne, A. Blue light excited retinal intercepts cellular signaling. Sci. Rep. 2018, 8, 10207. [Google Scholar]
- Bird, A.C.; Bressler, N.M.; Bressler, S.B.; Chisholm, I.H.; Coscas, G.; Davis, M.D.; de Jong, P.T.; Klaver, C.; Klein, B.; Klein, R. An international classification and grading system for age-related maculopathy and age-related macular degeneration. Surv. Ophthalmol. 1995, 39, 367–374. [Google Scholar] [CrossRef]
- Spaide, R.F.; Jaffe, G.J.; Sarraf, D.; Freund, K.B.; Sadda, S.R.; Staurenghi, G.; Waheed, N.K.; Chakravarthy, U.; Rosenfeld, P.J.; Holz, F.G.; et al. Consensus Nomenclature for Reporting Neovascular Age-Related Macular Degeneration Data: Consensus on Neovascular Age-Related Macular Degeneration Nomenclature Study Group. Ophthalmology 2020, 127, 616–636. [Google Scholar] [CrossRef]
- Davis, M.D.; Gangnon, R.E.; Lee, L.-Y.; Hubbard, L.D.; Klein, B.E.K.; Klein, R.; Ferris, F.L.; Bressler, S.B.; Milton, R.C.; Age-Related Eye Disease Study, G. The Age-Related Eye Disease Study severity scale for age-related macular degeneration: AREDS Report No. 17. Arch. Ophthalmol. 2005, 123, 1484–1498. [Google Scholar] [CrossRef]
- Klein, M.L.; Francis, P.J.; Ferris, F.L.; Hamon, S.C.; Clemons, T.E. Risk assessment model for development of advanced age-related macular degeneration. Arch. Ophthalmol. 2011, 129, 1543–1550. [Google Scholar] [CrossRef]
- Bonilha, V.L. Age and disease-related structural changes in the retinal pigment epithelium. Clin. Ophthalmol. 2008, 2, 413–424. [Google Scholar] [CrossRef]
- Farazdaghi, M.K.; Ebrahimi, K.B. Role of the Choroid in Age-related Macular Degeneration: A Current Review. J. Ophthalmic Vis. Res. 2019, 14, 78–87. [Google Scholar] [CrossRef] [PubMed]
- Johnson, L.V.; Leitner, W.P.; Staples, M.K.; Anderson, D.H. Complement activation and inflammatory processes in Drusen formation and age related macular degeneration. Exp. Eye Res. 2001, 73, 887–896. [Google Scholar] [PubMed]
- Funk, M.; Karl, D.; Georgopoulos, M.; Benesch, T.; Sacu, S.; Polak, K.; Zlabinger, G.J.; Schmidt-Erfurth, U. Neovascular age-related macular degeneration: Intraocular cytokines and growth factors and the influence of therapy with ranibizumab. Ophthalmology 2009, 116, 2393–2399. [Google Scholar] [CrossRef] [PubMed]
- Fredriksson, L.; Li, H.; Eriksson, U. The PDGF family: Four gene products form five dimeric isoforms. Cytokine Growth Factor Rev. 2004, 15, 197–204. [Google Scholar] [CrossRef] [PubMed]
- Jo, N.; Mailhos, C.; Ju, M.; Cheung, E.; Bradley, J.; Nishijima, K.; Robinson, G.S.; Adamis, A.P.; Shima, D.T. Inhibition of platelet-derived growth factor B signaling enhances the efficacy of anti-vascular endothelial growth factor therapy in multiple models of ocular neovascularization. Am. J. Pathol. 2006, 168, 2036–2053. [Google Scholar] [CrossRef]
- Cabral, T.; Mello, L.G.M.; Lima, L.H.; Polido, J.; Regatieri, C.V.; Belfort, R.; Mahajan, V.B. Retinal and choroidal angiogenesis: A review of new targets. Int. J. Retin. Vitr. 2017, 3, 31. [Google Scholar] [CrossRef]
- Bergers, G.; Song, S. The role of pericytes in blood-vessel formation and maintenance. Neuro-Oncology 2005, 7, 452–464. [Google Scholar] [CrossRef]
- Yang, S.; Zhao, J.; Sun, X. Resistance to anti-VEGF therapy in neovascular age-related macular degeneration: A comprehensive review. Drug Des. Dev. Ther. 2016, 10, 1857. [Google Scholar]
- Cabral, T.; Lima, L.H.; Polido, J.; Duong, J.; Okuda, É.; Oshima, A.; Serracarbassa, P.; Regatieri, C.V.; Belfort, R. Aqueous vascular endothelial growth factor and clinical outcomes correlation after single intravitreal injection of bevacizumab in patients with neovascular age-related macular degeneration. Int. J. Retin. Vitr. 2017, 3, 6. [Google Scholar] [CrossRef] [PubMed]
- Kinnunen, K.; Ylä-Herttuala, S. Vascular endothelial growth factors in retinal and choroidal neovascular diseases. Ann. Med. 2012, 44, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Papadopoulos, N.; Martin, J.; Ruan, Q.; Rafique, A.; Rosconi, M.P.; Shi, E.; Pyles, E.A.; Yancopoulos, G.D.; Stahl, N.; Wiegand, S.J. Binding and neutralization of vascular endothelial growth factor (VEGF) and related ligands by VEGF Trap, ranibizumab and bevacizumab. Angiogenesis 2012, 15, 171–185. [Google Scholar] [CrossRef] [PubMed]
- Anand-Apte, B.; Hollyfield, J. Developmental anatomy of the retinal and choroidal vasculature. In Encyclopedia of the Eye; Academic Press: Cambdridge, MA, USA, 2010. [Google Scholar]
- Marneros, A.G.; Fan, J.; Yokoyama, Y.; Gerber, H.P.; Ferrara, N.; Crouch, R.K.; Olsen, B.R. Vascular endothelial growth factor expression in the retinal pigment epithelium is essential for choriocapillaris development and visual function. Am. J. Pathol. 2005, 167, 1451–1459. [Google Scholar] [CrossRef]
- Marneros, A.G. NLRP3 inflammasome blockade inhibits VEGF-A-induced age-related macular degeneration. Cell Rep. 2013, 4, 945–958. [Google Scholar] [CrossRef]
- Al-Khersan, H.; Hussain, R.M.; Ciulla, T.A.; Dugel, P.U. Innovative therapies for neovascular age-related macular degeneration. Expert Opin. Pharmacother. 2019, 20, 1879–1891. [Google Scholar] [CrossRef]
- Hussain, R.M.; Ciulla, T.A. Emerging vascular endothelial growth factor antagonists to treat neovascular age-related macular degeneration. Expert Opin. Emerg. Drugs 2017, 22, 235–246. [Google Scholar] [CrossRef]
- Zipfel, P.F. Complement and immune defense: From innate immunity to human diseases. Immunol. Lett. 2009, 126, 1–7. [Google Scholar] [CrossRef]
- Maugeri, A.; Barchitta, M.; Mazzone, M.G.; Giuliano, F.; Agodi, A. Complement system and age-related macular degeneration: Implications of gene-environment interaction for preventive and personalized medicine. BioMed Res. Int. 2018, 2018. [Google Scholar] [CrossRef]
- Xu, H.; Chen, M. Targeting the complement system for the management of retinal inflammatory and degenerative diseases. Eur. J. Pharmacol. 2016, 787, 94–104. [Google Scholar] [CrossRef] [PubMed]
- Yeo, N.J.Y.; Chan, E.J.J.; Cheung, C. Choroidal Neovascularization: Mechanisms of Endothelial Dysfunction. Front. Pharmacol. 2019, 10, 1363. [Google Scholar] [CrossRef] [PubMed]
- Wolf, A.; Langmann, T. Anti-VEGF-A/ANG 2 combotherapy limits pathological angiogenesis in the eye: A replication study. EMBO Mol. Med. 2019, 11, e10362. [Google Scholar] [CrossRef]
- Ng, D.S.; Yip, Y.W.; Bakthavatsalam, M.; Chen, L.J.; Ng, T.K.; Lai, T.Y.; Pang, C.P.; Brelén, M.E. Elevated angiopoietin 2 in aqueous of patients with neovascular age related macular degeneration correlates with disease severity at presentation. Sci. Rep. 2017, 7, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Foxton, R.H.; Uhles, S.; Grüner, S.; Revelant, F.; Ullmer, C. Efficacy of simultaneous VEGF-A/ANG-2 neutralization in suppressing spontaneous choroidal neovascularization. EMBO Mol. Med. 2019, 11, e10204. [Google Scholar] [CrossRef]
- Papadopoulos, Z. Recent Developments in the Treatment of Wet Age-related Macular Degeneration. Curr. Med. Sci. 2020, 40, 851–857. [Google Scholar] [CrossRef] [PubMed]
- Sunness, J.S.; Rubin, G.S.; Zuckerbrod, A.; Applegate, C.A. Foveal-sparing scotomas in advanced dry age-related macular degeneration. J. Vis. Impair. Blind. 2008, 102, 600–610. [Google Scholar] [CrossRef]
- Sahay, P.; Singh, S.; Brar, A.S.; Kumar, A. Choroidal Neovascular Membranes. Retin. Med. Surg. Manag. 2018, 168. [Google Scholar]
- Lee, C.S.; Larson, E.B.; Gibbons, L.E.; Lee, A.Y.; McCurry, S.M.; Bowen, J.D.; McCormick, W.C.; Crane, P.K. Associations between recent and established ophthalmic conditions and risk of Alzheimer’s disease. Alzheimer’s Dement. 2019, 15, 34–41. [Google Scholar] [CrossRef]
- Tsai, D.-C.; Chen, S.-J.; Huang, C.-C.; Yuan, M.-K.; Leu, H.-B. Age-related macular degeneration and risk of degenerative dementia among the elderly in Taiwan: A population-based cohort study. Ophthalmology 2015, 122, 2327–2335.e2322. [Google Scholar] [CrossRef]
- Chung, S.-D.; Ho, J.-D.; Hu, C.-C.; Lin, H.-C.; Sheu, J.-J. Increased risk of Parkinson disease following a diagnosis of neovascular age-related macular degeneration: A retrospective cohort study. Am. J. Ophthalmol. 2014, 157, 464–469.e461. [Google Scholar] [CrossRef]
- Marmor, M.F. A brief history of macular grids: From Thomas Reid to Edvard Munch and Marc Amsler. Surv. Ophthalmol. 2000, 44, 343–353. [Google Scholar] [CrossRef]
- Kolar, P. Classification and clinical features of AMD. In Age-Related Macular Degeneration-Etiology, Diagnosis and Management—A Glance at the Future; IntechOpen: London, UK, 2013; pp. 105–132. [Google Scholar]
- Kitagawa, Y.; Shimada, H.; Mori, R.; Tanaka, K.; Yuzawa, M. Intravitreal Tissue Plasminogen Activator, Ranibizumab, and Gas Injection for Submacular Hemorrhage in Polypoidal Choroidal Vasculopathy. Ophthalmology 2016, 123, 1278–1286. [Google Scholar] [CrossRef]
- Yonekawa, Y.; Kim, I.K. Clinical characteristics and current treatment of age-related macular degeneration. Cold Spring Harb. Perspect. Med. 2014, 5, a017178. [Google Scholar] [CrossRef]
- Gujral, G.S.; Agarwal, M.; Mayor, R.; Shroff, D.; Chhablani, J.; Shanmugam, M.P. Clinical profile and management outcomes of traumatic submacular hemorrhage. J. Curr. Ophthalmol. 2019, 31, 411–415. [Google Scholar] [CrossRef] [PubMed]
- Tolentino, M.J.; Husain, D.; Theodosiadis, P.; Gragoudas, E.S.; Connolly, E.; Kahn, J.; Cleland, J.; Adamis, A.P.; Cuthbertson, A.; Miller, J.W. ANgiography of fluoresceinated anti–vascular endothelial growth factor antibody and dextrans in experimental choroidal neovascularization. Arch. Ophthalmol. 2000, 118, 78–84. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Heier, J.S.; Brown, D.M.; Chong, V.; Korobelnik, J.F.; Kaiser, P.K.; Nguyen, Q.D.; Kirchhof, B.; Ho, A.; Ogura, Y.; Yancopoulos, G.D.; et al. Intravitreal aflibercept (VEGF trap-eye) in wet age-related macular degeneration. Ophthalmology 2012, 119, 2537–2548. [Google Scholar] [CrossRef]
- Lotery, A.; Griner, R.; Ferreira, A.; Milnes, F.; Dugel, P. Real-world visual acuity outcomes between ranibizumab and aflibercept in treatment of neovascular AMD in a large US data set. Eye 2017, 31, 1697–1706. [Google Scholar] [CrossRef] [PubMed]
- Rosenfeld, P.J.; Brown, D.M.; Heier, J.S.; Boyer, D.S.; Kaiser, P.K.; Chung, C.Y.; Kim, R.Y. Ranibizumab for neovascular age-related macular degeneration. N. Engl. J. Med. 2006, 355, 1419–1431. [Google Scholar] [CrossRef]
- Martin, D.F.; Maguire, M.G.; Fine, S.L.; Ying, G.-s.; Jaffe, G.J.; Grunwald, J.E.; Toth, C.; Redford, M.; Ferris, F.L., 3rd. Comparison of Age-related Macular Degeneration Treatments Trials (CATT) Research Group. Ranibizumab and bevacizumab for treatment of neovascular age-related macular degeneration: Two-year results. Ophthalmology 2012, 119, 1388–1398. [Google Scholar] [CrossRef]
- Fileta, J.B.; Scott, I.U.; Flynn Jr, H.W. Meta-analysis of infectious endophthalmitis after intravitreal injection of anti-vascular endothelial growth factor agents. Ophthalmic Surg. Lasers Imaging Retin. 2014, 45, 143–149. [Google Scholar] [CrossRef]
- Gragoudas, E.S.; Adamis, A.P.; Cunningham, E.T., Jr.; Feinsod, M.; Guyer, D.R. Pegaptanib for neovascular age-related macular degeneration. N. Engl. J. Med. 2004, 351, 2805–2816. [Google Scholar] [CrossRef] [PubMed]
- Wirfs, M.J. The APRN and PA’s Complete Guide to Prescribing Drug Therapy 2022; Springer Publishing Company: Cham, Switzerland, 2021. [Google Scholar]
- Sharma, A.; Kumar, N.; Bandello, F.; Loewenstein, A.; Kuppermann, B.D. Need of education on biosimilars amongst ophthalmologists: Combating the nocebo effect. Eye 2020, 34, 1006–1007. [Google Scholar] [CrossRef]
- Sharma, A.; Kumar, N.; Kuppermann, B.D.; Bandello, F.; Loewenstein, A. Understanding biosimilars and its regulatory aspects across the globe: An ophthalmology perspective. Br. J. Ophthalmol. 2020, 104, 2–7. [Google Scholar] [CrossRef]
- Arepalli, S.; Kaiser, P.K. Pipeline therapies for neovascular age related macular degeneration. Int. J. Retin. Vitr. 2021, 7, 55. [Google Scholar] [CrossRef] [PubMed]
- Sharma, A.; Reddy, P.; Kuppermann, B.D.; Bandello, F.; Lowenstein, A. Biosimilars in ophthalmology: “Is there a big change on the horizon?”. Clin. Ophthalmol. 2018, 12, 2137. [Google Scholar] [CrossRef] [PubMed]
- Dixon, J.A.; Oliver, S.C.; Olson, J.L.; Mandava, N. VEGF Trap-Eye for the treatment of neovascular age-related macular degeneration. Expert Opin. Investig. Drugs 2009, 18, 1573–1580. [Google Scholar] [CrossRef]
- Michels, S.; Rosenfeld, P.J.; Puliafito, C.A.; Marcus, E.N.; Venkatraman, A.S. Systemic bevacizumab (Avastin) therapy for neovascular age-related macular degeneration: Twelve-week results of an uncontrolled open-label clinical study. Ophthalmology 2005, 112, 1035–1047.e1039. [Google Scholar] [CrossRef]
- Martin, D.F.; Maguire, M.G.; Ying, G.; Grunwald, J.E.; Fine, S.L.; Jaffe, G.J. Ranibizumab and bevacizumab for neovascular age-related macular degeneration. N. Engl. J. Med. 2011, 364, 1897–1908. [Google Scholar]
- Dugel, P.U.; Koh, A.; Ogura, Y.; Jaffe, G.J.; Schmidt-Erfurth, U.; Brown, D.M.; Gomes, A.V.; Warburton, J.; Weichselberger, A.; Holz, F.G. HAWK and HARRIER: Phase 3, multicenter, randomized, double-masked trials of brolucizumab for neovascular age-related macular degeneration. Ophthalmology 2020, 127, 72–84. [Google Scholar] [CrossRef]
- Gragoudas, E.; Adamis, A.; Cunningham Jr, E.; Feinsod, M.; Guyer, D. VEGF inhibition study in ocular neovascularization clinical trial group. N. Engl. J. Med. 2004, 351, 2805–2816. [Google Scholar] [CrossRef] [PubMed]
- Jaffe, G.J.; Ciulla, T.A.; Ciardella, A.P.; Devin, F.; Dugel, P.U.; Eandi, C.M.; Masonson, H.; Monés, J.; Pearlman, J.A.; Quaranta-El Maftouhi, M. Dual antagonism of PDGF and VEGF in neovascular age-related macular degeneration: A phase IIb, multicenter, randomized controlled trial. Ophthalmology 2017, 124, 224–234. [Google Scholar] [CrossRef] [PubMed]
- Dunn, E.N.; Sheth, V.S.; Hariprasad, S.M. An overview of the fovista and rinucumab trials and the fate of anti-PDGF medications. Ophthalmic Surg. Lasers Imaging Retin. 2017, 48, 100–104. [Google Scholar] [CrossRef] [PubMed]
- Jackson, T.L.; Boyer, D.; Brown, D.M.; Chaudhry, N.; Elman, M.; Liang, C.; O’Shaughnessy, D.; Parsons, E.C.; Patel, S.; Slakter, J.S. Oral tyrosine kinase inhibitor for neovascular age-related macular degeneration: A phase 1 dose-escalation study. JAMA Ophthalmol. 2017, 135, 761–767. [Google Scholar] [CrossRef]
- Cohen, M.N.; O’Shaughnessy, D.; Fisher, K.; Cerami, J.; Awh, C.C.; Salazar, D.E.; Rosenfeld, P.; Heier, J.S. APEX: A phase II randomised clinical trial evaluating the safety and preliminary efficacy of oral X-82 to treat exudative age-related macular degeneration. Br. J. Ophthalmol. 2021, 105, 716–722. [Google Scholar] [CrossRef]
- Pechan, P.; Rubin, H.; Lukason, M.; Ardinger, J.; DuFresne, E.; Hauswirth, W.; Wadsworth, S.; Scaria, A. Novel anti-VEGF chimeric molecules delivered by AAV vectors for inhibition of retinal neovascularization. Gene Ther. 2009, 16, 10–16. [Google Scholar] [CrossRef]
- Heier, J.S.; Kherani, S.; Desai, S.; Dugel, P.; Kaushal, S.; Cheng, S.H.; Delacono, C.; Purvis, A.; Richards, S.; Le-Halpere, A. Intravitreous injection of AAV2-sFLT01 in patients with advanced neovascular age-related macular degeneration: A phase 1, open-label trial. Lancet 2017, 390, 50–61. [Google Scholar] [CrossRef]
- Constable, I.J.; Lai, C.-M.; Magno, A.L.; French, M.A.; Barone, S.B.; Schwartz, S.D.; Blumenkranz, M.S.; Degli-Esposti, M.A.; Rakoczy, E.P. Gene therapy in neovascular age-related macular degeneration: Three-year follow-up of a phase 1 randomized dose escalation trial. Am. J. Ophthalmol. 2017, 177, 150–158. [Google Scholar] [CrossRef]
- Rakoczy, E.P.; Lai, C.-M.; Magno, A.L.; Wikstrom, M.E.; French, M.A.; Pierce, C.M.; Schwartz, S.D.; Blumenkranz, M.S.; Chalberg, T.W.; Degli-Esposti, M.A. Gene therapy with recombinant adeno-associated vectors for neovascular age-related macular degeneration: 1 year follow-up of a phase 1 randomised clinical trial. Lancet 2015, 386, 2395–2403. [Google Scholar] [CrossRef]
- Constable, I.J.; Pierce, C.M.; Lai, C.-M.; Magno, A.L.; Degli-Esposti, M.A.; French, M.A.; McAllister, I.L.; Butler, S.; Barone, S.B.; Schwartz, S.D. Phase 2a randomized clinical trial: Safety and post hoc analysis of subretinal rAAV. sFLT-1 for wet age-related macular degeneration. EBioMedicine 2016, 14, 168–175. [Google Scholar] [CrossRef]
- Campochiaro, P.A.; Lauer, A.K.; Sohn, E.H.; Mir, T.A.; Naylor, S.; Anderton, M.C.; Kelleher, M.; Harrop, R.; Ellis, S.; Mitrophanous, K.A. Lentiviral vector gene transfer of endostatin/angiostatin for macular degeneration (GEM) study. Hum. Gene Ther. 2017, 28, 99–111. [Google Scholar] [CrossRef] [PubMed]
- Haddad, W.M.; Coscas, G.; Soubrane, G. Eligibility for treatment and angiographic features at the early stage of exudative age related macular degeneration. Br. J. Ophthalmol. 2002, 86, 663–669. [Google Scholar] [CrossRef] [PubMed]
- Group, M.P.S. Five-year follow-up of fellow eyes of patients with age-related macular degeneration and unilateral extrafoveal choroidal neovascularization. Arch. Ophthalmol. 1993, 111, 1189–1199. [Google Scholar]
- Freund, K.B.; Yannuzzi, L.A.; Sorenson, J.A. Age-related macular degeneration and choroidal neovascularization. Am. J. Ophthalmol. 1993, 115, 786–791. [Google Scholar] [CrossRef]
- Moisseiev, J.; Alhalel, A.; Masuri, R.; Treister, G. The impact of the macular photocoagulation study results on the treatment of exudative age-related macular degeneration. Arch. Ophthalmol. 1995, 113, 185–189. [Google Scholar] [CrossRef]
- Nishijima, K.; Takahashi, M.; Akita, J.; Katsuta, H.; Tanemura, M.; Aikawa, H.; Mandai, M.; Takagi, H.; Kiryu, J.; Honda, Y. Laser photocoagulation of indocyanine green angiographically identified feeder vessels to idiopathic polypoidal choroidal vasculopathy. Am. J. Ophthalmol. 2004, 137, 770–773. [Google Scholar] [CrossRef]
- Chabbar, I.; Serghini, L.; Boulanouar, A.; Berraho, A. Exudative Age-Related Macular Degeneration: A Case Report and Review of the Literature. Saudi J. Med. Pharm. Sci. 2020, 6, 466–469. [Google Scholar] [CrossRef]
- Aveline, B.; Hasan, T.; Redmond, R.W. Photophysical and photosensitizing properties of benzoporphyrin derivative monoacid ring A (BPD-MA). Photochem. Photobiol. 1994, 59, 328–335. [Google Scholar] [CrossRef] [PubMed]
- Breukink, M.B.; Downes, S.M.; Querques, G.; van Dijk, E.H.C.; den Hollander, A.I.; Blanco-Garavito, R.; Keunen, J.E.E.; Souied, E.H.; MacLaren, R.E.; Hoyng, C.B.; et al. Comparing half-dose photodynamic therapy with high-density subthreshold micropulse laser treatment in patients with chronic central serous chorioretinopathy (the PLACE trial): Study protocol for a randomized controlled trial. Trials 2015, 16, 419. [Google Scholar] [CrossRef]
- Lai, T.Y.Y.; Wong, R.L.M.; Chan, W.-M. Long-Term Outcome of Half-Dose Verteporfin Photodynamic Therapy for the Treatment of Central Serous Chorioretinopathy (An American Ophthalmological Society Thesis). Trans. Am. Ophthalmol. Soc. 2015, 113, T8. [Google Scholar]
- Blumenkranz, M.S.; Bressler, N.M.; Bressler, S.B.; Donati, G.; Fish, G.E.; Haynes, A.L.; Lewis, H.; Miller, J.W.; Monés, J.M.; Potter, M.J.; et al. Verteporfin therapy for subfoveal choroidal neovascularization in age-related macular degeneration: Three-year results of an open-label extension of 2 randomized clinical trials—TAP Report no. 5. Arch. Ophthalmol. 2002, 120, 1307–1314. [Google Scholar]
- Bradley, J.; Ju, M.; Robinson, G.S. Combination therapy for the treatment of ocular neovascularization. Angiogenesis 2007, 10, 141–148. [Google Scholar] [CrossRef] [PubMed]
- Augustin, A.J.; Puls, S.; Offermann, I. Triple therapy for choroidal neovascularization due to age-related macular degeneration: Verteporfin PDT, bevacizumab, and dexamethasone. Retina 2007, 27, 133–140. [Google Scholar] [PubMed]
- Schmidt-Erfurth, U.; Schlötzer-Schrehard, U.; Cursiefen, C.; Michels, S.; Beckendorf, A.; Naumann, G.O. Influence of photodynamic therapy on expression of vascular endothelial growth factor (VEGF), VEGF receptor 3, and pigment epithelium–derived factor. Investig. Ophthalmol. Vis. Sci. 2003, 44, 4473–4480. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.; Wang, B.; Cui, W.; Fang, S. Efficacy of ranibizumab combined with photodynamic therapy on wet age-related macular degeneration. Exp. Med. 2020, 19, 3691–3697. [Google Scholar] [CrossRef]
- Yamashiro, K.; Oishi, A.; Hata, M.; Takahashi, A.; Tsujikawa, A. Visual acuity outcomes of anti-VEGF treatment for neovascular age-related macular degeneration in clinical trials. Jpn. J. Ophthalmol. 2021, 65, 741–760. [Google Scholar] [CrossRef]
- Ye, L.; Jiaqi, Z.; Jianchao, W.; Zhaohui, F.; Liang, Y.; Xiaohui, Z. Comparative efficacy and safety of anti-vascular endothelial growth factor regimens for neovascular age-related macular degeneration: Systematic review and Bayesian network meta-analysis. Ther. Adv. Chronic Dis. 2020, 11. [Google Scholar] [CrossRef]
- Hawkins, B.S.; Bressler, N.M.; Miskala, P.H.; Bressler, S.B.; Holekamp, N.M.; Marsh, M.J.; Redford, M.; Schwartz, S.D.; Sternberg, P., Jr.; Thomas, M.A. Surgery for subfoveal choroidal neovascularization in age-related macular degeneration: Ophthalmic findings: SST report no. 11. Ophthalmology 2004, 111, 1967–1980. [Google Scholar]
- Costagliola, C.; Romano, M.R.; Rinaldi, M.; Dell’Omo, R.; Chiosi, F.; Menzione, M.; Semeraro, F. Low fluence rate photodynamic therapy combined with intravitreal bevacizumab for neovascular age-related macular degeneration. Br. J. Ophthalmol. 2010, 94, 180–184. [Google Scholar] [CrossRef]
- Lim, J.Y.; Lee, S.Y.; Kim, J.G.; Lee, J.Y.; Chung, H.; Yoon, Y.H. Intravitreal bevacizumab alone versus in combination with photodynamic therapy for the treatment of neovascular maculopathy in patients aged 50 years or older: 1-year results of a prospective clinical study. Acta Ophthalmol. 2012, 90, 61–67. [Google Scholar] [CrossRef]
- Larsen, M.; Schmidt-Erfurth, U.; Lanzetta, P.; Wolf, S.; Simader, C.; Tokaji, E.; Pilz, S.; Weisberger, A.; Group, M.B.S. Verteporfin plus ranibizumab for choroidal neovascularization in age-related macular degeneration: Twelve-month MONT BLANC study results. Ophthalmology 2012, 119, 992–1000. [Google Scholar] [PubMed]
- Jackson, T.L.; Chakravarthy, U.; Kaiser, P.K.; Slakter, J.S.; Jan, E.; Bandello, F.; O’Shaughnessy, D.; Gertner, M.E.; Danielson, L.; Moshfeghi, D.M. Stereotactic radiotherapy for neovascular age-related macular degeneration: 52-week safety and efficacy results of the INTREPID study. Ophthalmology 2013, 120, 1893–1900. [Google Scholar] [CrossRef]
- Michalska-Małecka, K.; Kabiesz, A.; Nowak, M.; Śpiewak, D. Age related macular degeneration—Challenge for future: Pathogenesis and new perspectives for the treatment. Eur. Geriatr. Med. 2015, 6, 69–75. [Google Scholar] [CrossRef]
- García-Layana, A.; Cabrera-López, F.; García-Arumí, J.; Arias-Barquet, L.; Ruiz-Moreno, J.M. Early and intermediate age-related macular degeneration: Update and clinical review. Clin. Interv. Aging 2017, 12, 1579–1587. [Google Scholar] [CrossRef] [PubMed]
- Clemons, T.E.; Rankin, M.W.; McBee, W.L. Cognitive impairment in the age-related eye disease study: AREDS report no. 16. Arch. Ophthalmol. 2006, 124, 537–543. [Google Scholar] [PubMed]
- Group, A.R.; Chew, E.Y.; Clemons, T.; SanGiovanni, J.P.; Danis, R.; Domalpally, A.; McBee, W.; Sperduto, R.; Ferris, F.L. The Age-Related Eye Disease Study 2 (AREDS2): Study design and baseline characteristics (AREDS2 report number 1). Ophthalmology 2012, 119, 2282–2289. [Google Scholar] [CrossRef]
- Cserhalmi, M.; Papp, A.; Brandus, B.; Uzonyi, B.; Józsi, M. Regulation of regulators: Role of the complement factor H-related proteins. Semin. Immunol. 2019, 45, 101341. [Google Scholar] [CrossRef]
- Zhan, X.; Larson, D.E.; Wang, C.; Koboldt, D.C.; Sergeev, Y.V.; Fulton, R.S.; Fulton, L.L.; Fronick, C.C.; Branham, K.E.; Bragg-Gresham, J.; et al. Identification of a rare coding variant in complement 3 associated with age-related macular degeneration. Nat. Genet. 2013, 45, 1375–1379. [Google Scholar] [CrossRef]
- Helgason, H.; Sulem, P.; Duvvari, M.R.; Luo, H.; Thorleifsson, G.; Stefansson, H.; Jonsdottir, I.; Masson, G.; Gudbjartsson, D.F.; Walters, G.B.; et al. A rare nonsynonymous sequence variant in C3 is associated with high risk of age-related macular degeneration. Nat. Genet. 2013, 45, 1371–1374. [Google Scholar] [CrossRef]
- Tarallo, V.; Hirano, Y.; Gelfand, B.D.; Dridi, S.; Kerur, N.; Kim, Y.; Cho, W.G.; Kaneko, H.; Fowler, B.J.; Bogdanovich, S.; et al. DICER1 loss and Alu RNA induce age-related macular degeneration via the NLRP3 inflammasome and MyD88. Cell 2012, 149, 847–859. [Google Scholar] [CrossRef]
- Kaneko, H.; Dridi, S.; Tarallo, V.; Gelfand, B.D.; Fowler, B.J.; Cho, W.G.; Kleinman, M.E.; Ponicsan, S.L.; Hauswirth, W.W.; Chiodo, V.A.; et al. DICER1 deficit induces Alu RNA toxicity in age-related macular degeneration. Nature 2011, 471, 325–330. [Google Scholar] [CrossRef] [PubMed]
- Thomas, C.J.; Mirza, R.G.; Gill, M.K. Age-Related Macular Degeneration. Med. Clin. N. Am. 2021, 105, 473–491. [Google Scholar] [CrossRef]
- Mallias, I.; Mylova, P.; Tassiopoulou, A. Fundus autofluorescence and multicolour imaging comparison in assessing disease severity in patients suffering from geographic atrophy. A case series analysis. Ophthalmol. J. 2017, 2, 69–78. [Google Scholar] [CrossRef][Green Version]
- Apte, R.S. Age-Related Macular Degeneration. N. Engl. J. Med. 2021, 385, 539–547. [Google Scholar] [CrossRef] [PubMed]
- Sura, A.A.; Chen, L.; Messinger, J.D.; Swain, T.A.; McGwin, G., Jr.; Freund, K.B.; Curcio, C.A. Measuring the Contributions of Basal Laminar Deposit and Bruch’s Membrane in Age-Related Macular Degeneration. Investig. Ophthalmol. Vis. Sci. 2020, 61, 19. [Google Scholar] [CrossRef]
- Holz, F.G.; Sadda, S.R.; Busbee, B.; Chew, E.Y.; Mitchell, P.; Tufail, A.; Brittain, C.; Ferrara, D.; Gray, S.; Honigberg, L. Efficacy and safety of lampalizumab for geographic atrophy due to age-related macular degeneration: Chroma and Spectri phase 3 randomized clinical trials. JAMA Ophthalmol. 2018, 136, 666–677. [Google Scholar] [CrossRef] [PubMed]
- Yehoshua, Z.; de Amorim Garcia Filho, C.A.; Nunes, R.P.; Gregori, G.; Penha, F.M.; Moshfeghi, A.A.; Zhang, K.; Sadda, S.; Feuer, W.; Rosenfeld, P.J. Systemic complement inhibition with eculizumab for geographic atrophy in age-related macular degeneration: The COMPLETE study. Ophthalmology 2014, 121, 693–701. [Google Scholar] [CrossRef]
- Yaspan, B.L.; Williams, D.F.; Holz, F.G.; Regillo, C.D.; Li, Z.; Dressen, A.; van Lookeren Campagne, M.; Le, K.N.; Graham, R.R.; Beres, T. Targeting factor D of the alternative complement pathway reduces geographic atrophy progression secondary to age-related macular degeneration. Sci. Transl. Med. 2017, 9, eaaf1443. [Google Scholar] [CrossRef]
- Jaffe, G.J.; Schmitz-Valckenberg, S.; Boyer, D.; Heier, J.; Wolf-Schnurrbusch, U.; Staurenghi, G.; Schmidt-Erfurth, U.; Holz, F.G. Randomized trial to evaluate tandospirone in geographic atrophy secondary to age-related macular degeneration: The GATE study. Am. J. Ophthalmol. 2015, 160, 1226–1234. [Google Scholar] [CrossRef]
- Evans, J.R.; Lawrenson, J.G. Antioxidant vitamin and mineral supplements for preventing age-related macular degeneration. Cochrane Database Syst. Rev. 2017, 7. [Google Scholar] [CrossRef]
- Blodi, B.A. Nutritional supplements in the prevention of age-related macular degeneration. Insight 2004, 29, 15–16. [Google Scholar] [PubMed]
- Dashti, N.; McGwin, G.; Owsley, C.; Curcio, C.A. Plasma apolipoproteins and risk for age related maculopathy. Br. J. Ophthalmol. 2006, 90, 1028–1033. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Mukhtar, S.; Ambati, B.K. The value of nutritional supplements in treating Age-Related Macular Degeneration: A review of the literature. Int. Ophthalmol. 2019, 39, 2975–2983. [Google Scholar] [CrossRef] [PubMed]
- SanGiovanni, J.P.; Chew, E.Y. The role of omega-3 long-chain polyunsaturated fatty acids in health and disease of the retina. Prog. Retin. Eye Res. 2005, 24, 87–138. [Google Scholar] [CrossRef]
- Age-Related Eye Disease Study Research Group. A randomized, placebo-controlled, clinical trial of high-dose supplementation with vitamins C and E, beta carotene, and zinc for age-related macular degeneration and vision loss: AREDS report no. 8. Arch. Ophthalmol. 2001, 119, 1417–1436. [Google Scholar] [CrossRef]
- Gorusupudi, A.; Nelson, K.; Bernstein, P.S. The age-related eye disease 2 study: Micronutrients in the treatment of macular degeneration. Adv. Nutr. 2017, 8, 40–53. [Google Scholar] [CrossRef]
- Awh, C.C.; Hawken, S.; Zanke, B.W. Treatment response to antioxidants and zinc based on CFH and ARMS2 genetic risk allele number in the Age-Related Eye Disease Study. Ophthalmology 2015, 122, 162–169. [Google Scholar] [CrossRef]
- Di Carlo, E.; Augustin, A.J. Prevention of the Onset of Age-Related Macular Degeneration. J. Clin. Med. 2021, 10, 3297. [Google Scholar] [CrossRef]
- Nunes, S.; Alves, D.; Barreto, P.; Raimundo, M.; da Luz Cachulo, M.; Farinha, C.; Laíns, I.; Rodrigues, J.; Almeida, C.; Ribeiro, L. Adherence to a Mediterranean diet and its association with age-related macular degeneration. The Coimbra Eye Study–Report 4. Nutrition 2018, 51, 6–12. [Google Scholar] [CrossRef]
- Bartlett, H.; Eperjesi, F. Age-related macular degeneration and nutritional supplementation: A review of randomised controlled trials. Ophthalmic Physiol. Opt. 2003, 23, 383–399. [Google Scholar] [CrossRef]
- Eter, N.; Krohne, T.U.; Holz, F.G. New pharmacologic approaches to therapy for age-related macular degeneration. BioDrugs 2006, 20, 167–179. [Google Scholar] [CrossRef]
- Ghasemi, M.; Alizadeh, E.; Saei Arezoumand, K.; Fallahi Motlagh, B.; Zarghami, N. Ciliary neurotrophic factor (CNTF) delivery to retina: An overview of current research advancements. Artif. Cells Nanomed. Biotechnol. 2018, 46, 1694–1707. [Google Scholar] [CrossRef] [PubMed]
- Keane, P.A.; Sim, D.A.; Sadda, S.R. Advances in imaging in age-related macular degeneration. Curr. Ophthalmol. Rep. 2013, 1, 1–11. [Google Scholar] [CrossRef][Green Version]
- Gess, A.J.; Fung, A.E.; Rodriguez, J.G. Imaging in neovascular age-related macular degeneration. Semin. Ophthalmol. 2011, 26, 225–233. [Google Scholar] [CrossRef]
- Talks, S.J.; Aftab, A.M.; Ashfaq, I.; Soomro, T. The role of new imaging methods in managing age-related macular degeneration. Asia-Pac. J. Ophthalmol. 2017, 6, 498–507. [Google Scholar]
- Ahlers, C.; Götzinger, E.; Pircher, M.; Golbaz, I.; Prager, F.; Schütze, C.; Baumann, B.; Hitzenberger, C.K.; Schmidt-Erfurth, U. Imaging of the retinal pigment epithelium in age-related macular degeneration using polarization-sensitive optical coherence tomography. Investig. Ophthalmol. Vis. Sci. 2010, 51, 2149–2157. [Google Scholar] [CrossRef]
- Pircher, M.; Götzinger, E.; Findl, O.; Michels, S.; Geitzenauer, W.; Leydolt, C.; Schmidt-Erfurth, U.; Hitzenberger, C.K. Human macula investigated in vivo with polarization-sensitive optical coherence tomography. Investig. Ophthalmol. Vis. Sci. 2006, 47, 5487–5494. [Google Scholar] [CrossRef]
- Karampelas, M.; Sim, D.A.; Keane, P.A.; Papastefanou, V.P.; Sadda, S.R.; Tufail, A.; Dowler, J. Evaluation of retinal pigment epithelium–Bruch’s membrane complex thickness in dry age-related macular degeneration using optical coherence tomography. Br. J. Ophthalmol. 2013, 97, 1256–1261. [Google Scholar] [CrossRef]
- Ueda-Arakawa, N.; Ooto, S.; Tsujikawa, A.; Yamashiro, K.; Oishi, A.; Yoshimura, N. Sensitivity and specificity of detecting reticular pseudodrusen in multimodal imaging in Japanese patients. Retina 2013, 33, 490–497. [Google Scholar] [CrossRef]
- Cicinelli, M.V.; Rabiolo, A.; Sacconi, R.; Carnevali, A.; Querques, L.; Bandello, F.; Querques, G. Optical coherence tomography angiography in dry age-related macular degeneration. Surv. Ophthalmol. 2018, 63, 236–244. [Google Scholar] [CrossRef]
- Toto, L.; Borrelli, E.; Di Antonio, L.; Carpineto, P.; Mastropasqua, R. Retinal vascular plexuses’ changes in dry age-related macular degeneration, evaluated by means of optical coherence tomography angiography. Retina 2016, 36, 1566–1572. [Google Scholar] [CrossRef] [PubMed]
- Fleckenstein, M.; Schmitz-Valckenberg, S.; Adrion, C.; Krämer, I.; Eter, N.; Helb, H.M.; Brinkmann, C.K.; Issa, P.C.; Mansmann, U.; Holz, F.G. Tracking progression with spectral-domain optical coherence tomography in geographic atrophy caused by age-related macular degeneration. Investig. Ophthalmol. Vis. Sci. 2010, 51, 3846–3852. [Google Scholar] [CrossRef] [PubMed]
- Fleckenstein, M.; Schmitz-Valckenberg, S.; Martens, C.; Kosanetzky, S.; Brinkmann, C.K.; Hageman, G.S.; Holz, F.G. Fundus autofluorescence and spectral-domain optical coherence tomography characteristics in a rapidly progressing form of geographic atrophy. Investig. Ophthalmol. Vis. Sci. 2011, 52, 3761–3766. [Google Scholar] [CrossRef] [PubMed]
- Zweifel, S.A.; Engelbert, M.; Laud, K.; Margolis, R.; Spaide, R.F.; Freund, K.B. Outer retinal tubulation: A novel optical coherence tomography finding. Arch. Ophthalmol. 2009, 127, 1596–1602. [Google Scholar] [CrossRef]
- Victor, A.A. The Role of Imaging in Age-Related Macular Degeneration. In Visual Impairment and Blindness—What We Know and What We Have to Know; IntechOpen: London, UK, 2019. [Google Scholar]
- Göbel, A.P.; Fleckenstein, M.; Schmitz-Valckenberg, S.; Brinkmann, C.K.; Holz, F.G. Imaging geographic atrophy in age-related macular degeneration. Ophthalmologica 2011, 226, 182–190. [Google Scholar] [CrossRef]
- Abdelsalam, A.; Del Priore, L.; Zarbin, M.A. Drusen in age-related macular degeneration: Pathogenesis, natural course, and laser photocoagulation–induced regression. Surv. Ophthalmol. 1999, 44, 1–29. [Google Scholar] [CrossRef]
- Mokwa, N.F.; Ristau, T.; Keane, P.A.; Kirchhof, B.; Sadda, S.R.; Liakopoulos, S. Grading of age-related macular degeneration: Comparison between color fundus photography, fluorescein angiography, and spectral domain optical coherence tomography. J. Ophthalmol. 2013, 2013. [Google Scholar] [CrossRef]
- Ly, A.; Nivison-Smith, L.; Zangerl, B.; Assaad, N.; Kalloniatis, M. Advanced imaging for the diagnosis of age-related macular degeneration: A case vignettes study. Clin. Exp. Optom. 2018, 101, 243–254. [Google Scholar] [CrossRef]
- Ly, A.; Nivison-Smith, L.; Assaad, N.; Kalloniatis, M. Fundus autofluorescence in age-related macular degeneration. Optom. Vis. Sci. 2017, 94, 246. [Google Scholar] [CrossRef]
- Batoglu, F.; Demirel, S.; Özmert, E.; Oguz, Y.G.; Özyol, P. Autofluorescence patterns as a predictive factor for neovascularization. Optom. Vis. Sci. 2014, 91, 950–955. [Google Scholar] [CrossRef] [PubMed]
- Cachulo, L.; Silva, R.; Fonseca, P.; Pires, I.; Carvajal-Gonzalez, S.; Bernardes, R.; Cunha-Vaz, J.G. Early markers of choroidal neovascularization in the fellow eye of patients with unilateral exudative age-related macular degeneration. Ophthalmologica 2011, 225, 144–149. [Google Scholar] [CrossRef] [PubMed]
- Kellner, U.; Kellner, S.; Weinitz, S. Fundus autofluorescence (488 NM) and near-infrared autofluorescence (787 NM) visualize different retinal pigment epithelium alterations in patients with age-related macular degeneration. Retina 2010, 30, 6–15. [Google Scholar] [CrossRef] [PubMed]
- Savastano, M.C.; Rispoli, M.; Lumbroso, B.; Di Antonio, L.; Mastropasqua, L.; Virgili, G.; Savastano, A.; Bacherini, D.; Rizzo, S. Fluorescein angiography versus optical coherence tomography angiography: FA vs OCTA Italian Study. Eur. J. Ophthalmol. 2021, 31, 514–520. [Google Scholar] [CrossRef] [PubMed]
- Kwan, A.S.; Barry, C.; McAllister, I.L.; Constable, I. Fluorescein angiography and adverse drug reactions revisited: The Lions Eye experience. Clin. Exp. Ophthalmol. 2006, 34, 33–38. [Google Scholar] [CrossRef]
- Yannuzzi, L.A. Indocyanine green angiography: A perspective on use in the clinical setting. Am. J. Ophthalmol. 2011, 151, 745–751.e741. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fernandes, A.R.; Zielińska, A.; Sanchez-Lopez, E.; dos Santos, T.; Garcia, M.L.; Silva, A.M.; Karczewski, J.; Souto, E.B. Exudative versus Nonexudative Age-Related Macular Degeneration: Physiopathology and Treatment Options. Int. J. Mol. Sci. 2022, 23, 2592. https://doi.org/10.3390/ijms23052592
Fernandes AR, Zielińska A, Sanchez-Lopez E, dos Santos T, Garcia ML, Silva AM, Karczewski J, Souto EB. Exudative versus Nonexudative Age-Related Macular Degeneration: Physiopathology and Treatment Options. International Journal of Molecular Sciences. 2022; 23(5):2592. https://doi.org/10.3390/ijms23052592
Chicago/Turabian StyleFernandes, Ana Rita, Aleksandra Zielińska, Elena Sanchez-Lopez, Tiago dos Santos, Maria Luisa Garcia, Amelia M. Silva, Jacek Karczewski, and Eliana B. Souto. 2022. "Exudative versus Nonexudative Age-Related Macular Degeneration: Physiopathology and Treatment Options" International Journal of Molecular Sciences 23, no. 5: 2592. https://doi.org/10.3390/ijms23052592
APA StyleFernandes, A. R., Zielińska, A., Sanchez-Lopez, E., dos Santos, T., Garcia, M. L., Silva, A. M., Karczewski, J., & Souto, E. B. (2022). Exudative versus Nonexudative Age-Related Macular Degeneration: Physiopathology and Treatment Options. International Journal of Molecular Sciences, 23(5), 2592. https://doi.org/10.3390/ijms23052592








