Decoding Genetic Features and Antimicrobial Susceptibility of Pseudomonas aeruginosa Strains Isolated from Bloodstream Infections
Abstract
1. Introduction
2. Results
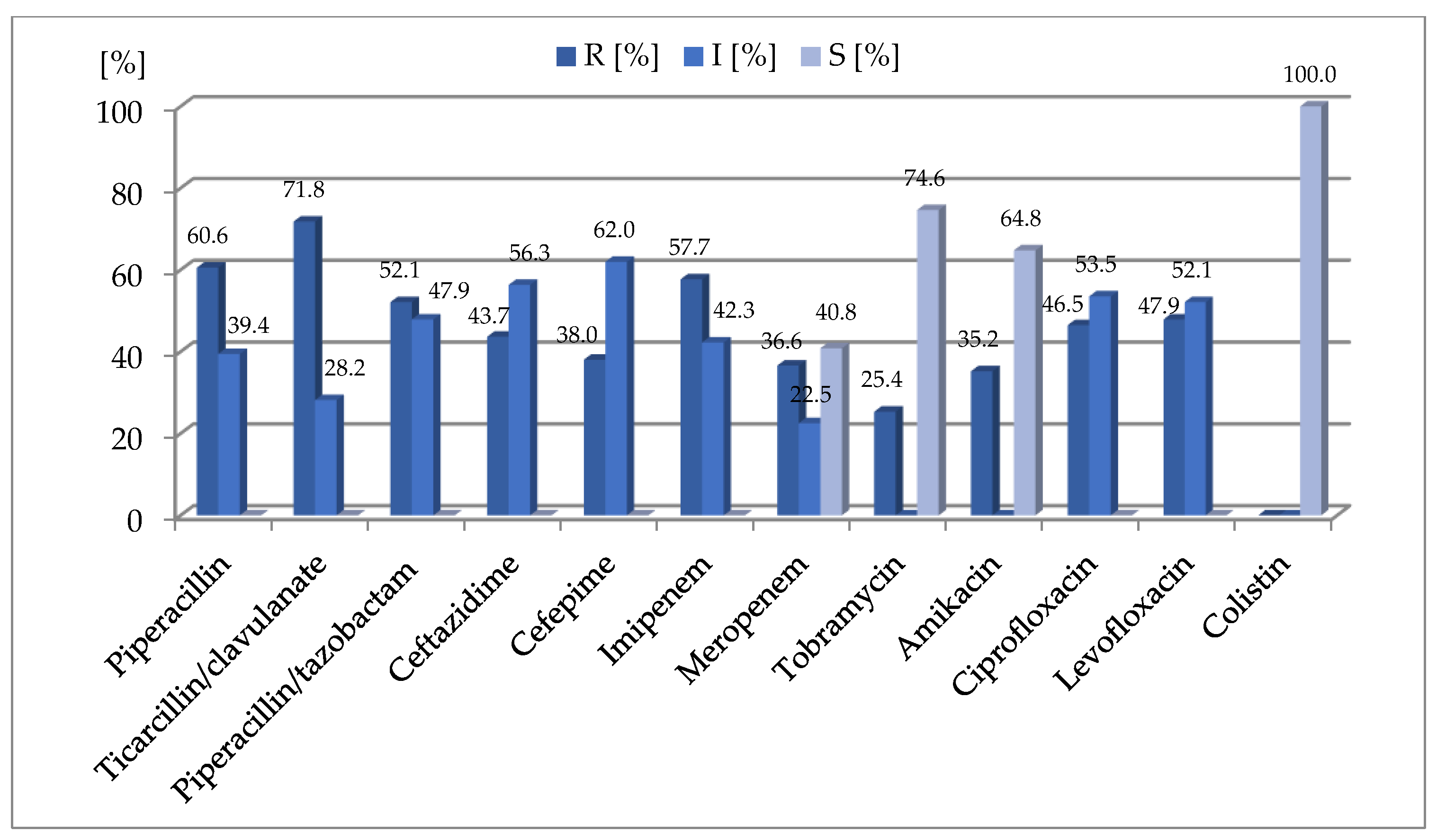
2.1. Antimicrobial Susceptibility of the Strains
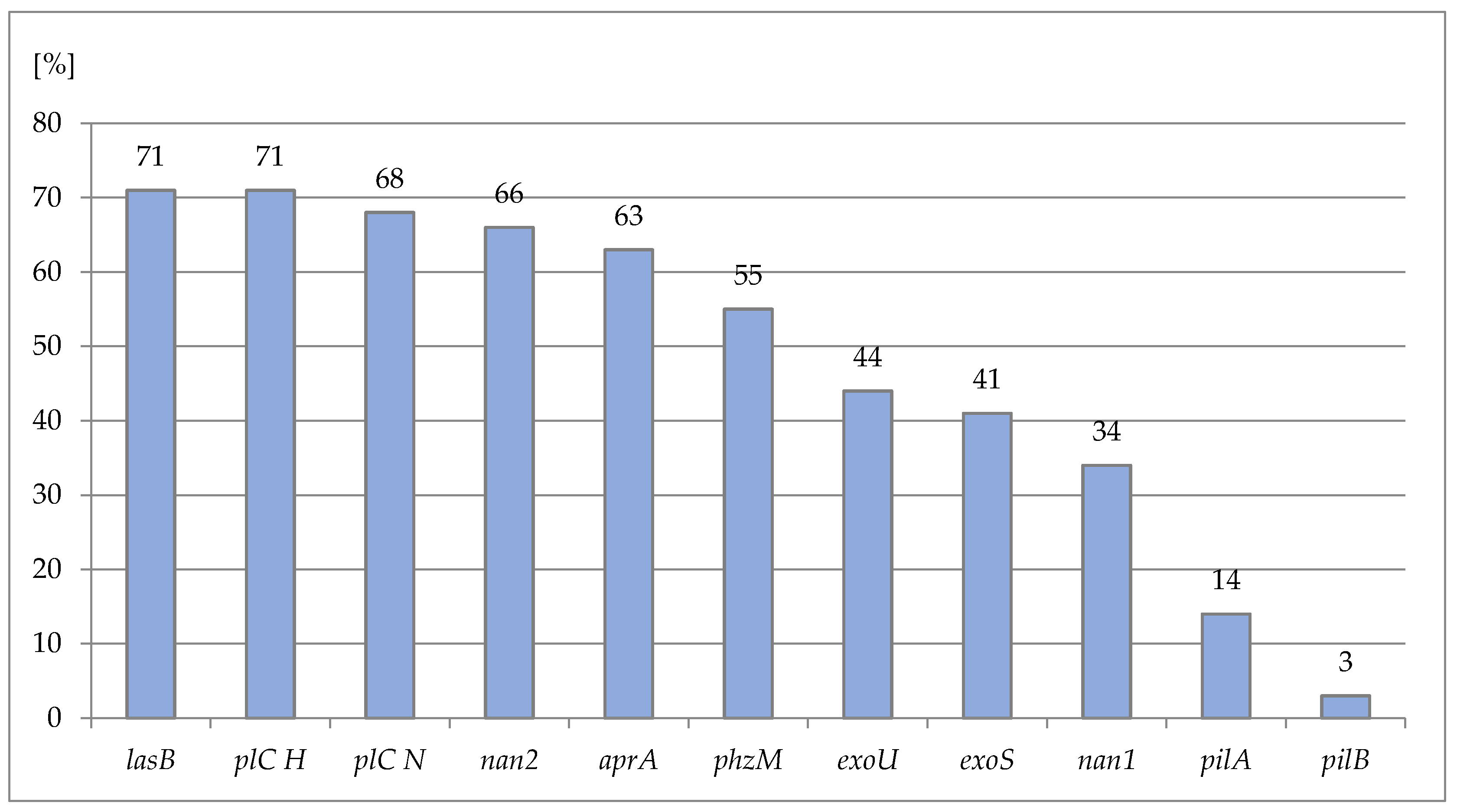
2.2. Prevalence of the Virulence-Factor Genes
2.3. Clinical Data Analysis
2.4. Statistical Analysis
3. Discussion
4. Materials and Methods
4.1. Origin of the Strains, Their Selection Criteria and Clinical Data Analysis
4.2. Antimicrobial Susceptibility Testing
4.3. Bacterial DNA Isolation
4.4. Virulence-Factor Genes Detection
4.5. Statistical Methods
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- de Sousa, T.; Hébraud, M.; Dapkevicius, M.L.N.E.; Maltez, L.; Pereira, J.E.; Capita, R.; Alonso-Calleja, C.; Igrejas, G.; Poeta, P. Genomic and Metabolic Characteristics of the Pathogenicity in Pseudomonas Aeruginosa. Int. J. Mol. Sci. 2021, 22, 12892. [Google Scholar] [CrossRef] [PubMed]
- Reynolds, D.; Kollef, M. The Epidemiology and Pathogenesis and Treatment of Pseudomonas Aeruginosa Infections: An Update. Drugs 2021, 81, 2117–2131. [Google Scholar] [CrossRef] [PubMed]
- Antimicrobial Resistance in the EU/EEA (EARS-Net)—Annual Epidemiological Report for 2019. Available online: https://www.ecdc.europa.eu/en/publications-data/surveillance-antimicrobial-resistance-europe-2019 (accessed on 13 July 2022).
- Tang, P.-C.; Lee, C.-C.; Li, C.-W.; Li, M.-C.; Ko, W.-C.; Lee, N.-Y. Time-to-Positivity of Blood Culture: An Independent Prognostic Factor of Monomicrobial Pseudomonas Aeruginosa Bacteremia. J. Microbiol. Immunol. Infect. Wei Mian Yu Gan Ran Za Zhi 2017, 50, 486–493. [Google Scholar] [CrossRef]
- Glen, K.A.; Lamont, I.L. β-Lactam Resistance in Pseudomonas Aeruginosa: Current Status, Future Prospects. Pathogens 2021, 10, 1638. [Google Scholar] [CrossRef] [PubMed]
- Al-Wrafy, F.; Brzozowska, E.; Górska, S.; Gamian, A. Pathogenic Factors of Pseudomonas Aeruginosa—The Role of Biofilm in Pathogenicity and as a Target for Phage Therapy. Postepy Hig. Med. Dosw. Online 2017, 71, 78–91. [Google Scholar] [CrossRef] [PubMed]
- Bogiel, T.; Prażyńska, M.; Kwiecińska-Piróg, J.; Mikucka, A.; Gospodarek-Komkowska, E. Carbapenem-Resistant Pseudomonas Aeruginosa Strains-Distribution of the Essential Enzymatic Virulence Factors Genes. Antibiotics 2020, 10, 8. [Google Scholar] [CrossRef] [PubMed]
- Bogiel, T.; Depka, D.; Rzepka, M.; Kwiecińska-Piróg, J.; Gospodarek-Komkowska, E. Prevalence of the Genes Associated with Biofilm and Toxins Synthesis amongst the Pseudomonas Aeruginosa Clinical Strains. Antibiotics 2021, 10, 241. [Google Scholar] [CrossRef]
- Stover, C.K.; Pham, X.Q.; Erwin, A.L.; Mizoguchi, S.D.; Warrener, P.; Hickey, M.J.; Brinkman, F.S.; Hufnagle, W.O.; Kowalik, D.J.; Lagrou, M.; et al. Complete Genome Sequence of Pseudomonas Aeruginosa PAO1, an Opportunistic Pathogen. Nature 2000, 406, 959–964. [Google Scholar] [CrossRef]
- Vanderwoude, J.; Fleming, D.; Azimi, S.; Trivedi, U.; Rumbaugh, K.P.; Diggle, S.P. The Evolution of Virulence in Pseudomonas Aeruginosa during Chronic Wound Infection. Proc. Biol. Sci. 2020, 287, 20202272. [Google Scholar] [CrossRef]
- Fan, X.; Wu, Y.; Xiao, M.; Xu, Z.-P.; Kudinha, T.; Bazaj, A.; Kong, F.; Xu, Y.-C. Diverse Genetic Background of Multidrug-Resistant Pseudomonas Aeruginosa from Mainland China, and Emergence of an Extensively Drug-Resistant ST292 Clone in Kunming. Sci. Rep. 2016, 6, 26522. [Google Scholar] [CrossRef]
- Kiewitz, C.; Tümmler, B. Sequence Diversity of Pseudomonas Aeruginosa: Impact on Population Structure and Genome Evolution. J. Bacteriol. 2000, 182, 3125–3135. [Google Scholar] [CrossRef] [PubMed]
- Finnan, S.; Morrissey, J.P.; O’Gara, F.; Boyd, E.F. Genome Diversity of Pseudomonas Aeruginosa Isolates from Cystic Fibrosis Patients and the Hospital Environment. J. Clin. Microbiol. 2004, 42, 5783–5792. [Google Scholar] [CrossRef] [PubMed]
- Al Dawodeyah, H.Y.; Obeidat, N.; Abu-Qatouseh, L.F.; Shehabi, A.A. Antimicrobial Resistance and Putative Virulence Genes of Pseudomonas Aeruginosa Isolates from Patients with Respiratory Tract Infection. Germs 2018, 8, 31–40. [Google Scholar] [CrossRef] [PubMed]
- Lanotte, P.; Watt, S.; Mereghetti, L.; Dartiguelongue, N.; Rastegar-Lari, A.; Goudeau, A.; Quentin, R. Genetic Features of Pseudomonas Aeruginosa Isolates from Cystic Fibrosis Patients Compared with Those of Isolates from Other Origins. J. Med. Microbiol. 2004, 53, 73–81. [Google Scholar] [CrossRef]
- Bellés, A.; Bueno, J.; Rojo-Bezares, B.; Torres, C.; Javier Castillo, F.; Sáenz, Y.; Seral, C. Characterisation of VIM-2-Producing Pseudomonas Aeruginosa Isolates from Lower Tract Respiratory Infections in a Spanish Hospital. Eur. J. Clin. Microbiol. Infect. Dis. Off. Publ. Eur. Soc. Clin. Microbiol. 2018, 37, 1847–1856. [Google Scholar] [CrossRef]
- Di Martino, P.; Gagnière, H.; Berry, H.; Bret, L. Antibiotic Resistance and Virulence Properties of Pseudomonas Aeruginosa Strains from Mechanically Ventilated Patients with Pneumonia in Intensive Care Units: Comparison with Imipenem-Resistant Extra-Respiratory Tract Isolates from Uninfected Patients. Microbes Infect. 2002, 4, 613–620. [Google Scholar] [CrossRef]
- Faraji, F.; Mahzounieh, M.; Ebrahimi, A.; Fallah, F.; Teymournejad, O.; Lajevardi, B. Molecular Detection of Virulence Genes in Pseudomonas Aeruginosa Isolated from Children with Cystic Fibrosis and Burn Wounds in Iran. Microb. Pathog. 2016, 99, 1–4. [Google Scholar] [CrossRef]
- Tingpej, P.; Smith, L.; Rose, B.; Zhu, H.; Conibear, T.; Al Nassafi, K.; Manos, J.; Elkins, M.; Bye, P.; Willcox, M.; et al. Phenotypic Characterization of Clonal and Nonclonal Pseudomonas Aeruginosa Strains Isolated from Lungs of Adults with Cystic Fibrosis. J. Clin. Microbiol. 2007, 45, 1697–1704. [Google Scholar] [CrossRef]
- Pobiega, M.; Maciag, J.; Pomorska-Wesolowska, M.; Chmielarczyk, A.; Romaniszyn, D.; Ziolkowski, G.; Heczko, P.B.; Wojkowska-Mach, J.; Bulanda, M. Urinary Tract Infections Caused by Pseudomonas Aeruginosa among Children in Southern Poland: Virulence Factors and Antibiotic Resistance. J. Pediatr. Urol. 2016, 12, 36.e1–36.e6. [Google Scholar] [CrossRef]
- Pobiega, M.; Maciąg, J.; Chmielarczyk, A.; Romaniszyn, D.; Pomorska-Wesolowska, M.; Ziolkowski, G.; Heczko, P.B.; Bulanda, M.; Wojkowska-Mach, J. Molecular Characterization of Carbapenem-Resistant Pseudomonas Aeruginosa Strains Isolated from Patients with Urinary Tract Infections in Southern Poland. Diagn. Microbiol. Infect. Dis. 2015, 83, 295–297. [Google Scholar] [CrossRef]
- Sabharwal, N.; Dhall, S.; Chhibber, S.; Harjai, K. Molecular Detection of Virulence Genes as Markers in Pseudomonas Aeruginosa Isolated from Urinary Tract Infections. Int. J. Mol. Epidemiol. Genet. 2014, 5, 125–134. [Google Scholar]
- Mitov, I.; Strateva, T.; Markova, B. Prevalence of Virulence Genes among Bulgarian Nosocomial and Cystic Fibrosis Isolates of Pseudomonas Aeruginosa. Braz. J. Microbiol. Publ. Braz. Soc. Microbiol. 2010, 41, 588–595. [Google Scholar] [CrossRef] [PubMed]
- Strateva, T.; Petrova, G.; Perenovska, P.; Mitov, I. Bulgarian Cystic Fibrosis Pseudomonas Aeruginosa Isolates: Antimicrobial Susceptibility and Neuraminidase-Encoding Gene Distribution. J. Med. Microbiol. 2009, 58, 690–692. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Lloyd, M.G.; Vossler, J.L.; Nomura, C.T.; Moffat, J.F. Blocking RpoN Reduces Virulence of Pseudomonas Aeruginosa Isolated from Cystic Fibrosis Patients and Increases Antibiotic Sensitivity in a Laboratory Strain. Sci. Rep. 2019, 9, 6677. [Google Scholar] [CrossRef] [PubMed]
- Rostami, S.; Farajzadeh Sheikh, A.; Shoja, S.; Farahani, A.; Tabatabaiefar, M.A.; Jolodar, A.; Sheikhi, R. Investigating of Four Main Carbapenem-Resistance Mechanisms in High-Level Carbapenem Resistant Pseudomonas Aeruginosa Isolated from Burn Patients. J. Chin. Med. Assoc. JCMA 2018, 81, 127–132. [Google Scholar] [CrossRef]
- Wolska, K.; Szweda, P. Genetic Features of Clinical Pseudomonas Aeruginosa Strains. Pol. J. Microbiol. 2009, 58, 255–260. [Google Scholar]
- Alverdy, J.; Holbrook, C.; Rocha, F.; Seiden, L.; Wu, R.L.; Musch, M.; Chang, E.; Ohman, D.; Suh, S. Gut-Derived Sepsis Occurs When the Right Pathogen with the Right Virulence Genes Meets the Right Host: Evidence for in Vivo Virulence Expression in Pseudomonas Aeruginosa. Ann. Surg. 2000, 232, 480–489. [Google Scholar] [CrossRef]
- Leonov, V.V.; Bulatov, I.A.; Mironov, A.Y. The increasing and expression of virulence factors of opportunistic microorganisms in blood serum under various alternatives of iron homeostasis. Klin. Lab. Diagn. 2016, 61, 498–501. [Google Scholar]
- Yoon, E.-J.; Kim, D.; Lee, H.; Lee, H.S.; Shin, J.H.; Park, Y.S.; Kim, Y.A.; Shin, J.H.; Shin, K.S.; Uh, Y.; et al. Mortality Dynamics of Pseudomonas Aeruginosa Bloodstream Infections and the Influence of Defective OprD on Mortality: Prospective Observational Study. J. Antimicrob. Chemother. 2019, 74, 2774–2783. [Google Scholar] [CrossRef]
- Rossi Gonçalves, I.; Dantas, R.C.C.; Ferreira, M.L.; da Fonseca Batistão, D.W.; Gontijo-Filho, P.P.; Ribas, R.M. Carbapenem-Resistant Pseudomonas Aeruginosa: Association with Virulence Genes and Biofilm Formation. Braz. J. Microbiol. Publ. Braz. Soc. Microbiol. 2017, 48, 211–217. [Google Scholar] [CrossRef]
- Cho, H.H.; Kwon, K.C.; Kim, S.; Koo, S.H. Correlation between Virulence Genotype and Fluoroquinolone Resistance in Carbapenem-Resistant Pseudomonas Aeruginosa. Ann. Lab. Med. 2014, 34, 286–292. [Google Scholar] [CrossRef] [PubMed]
- Peña, C.; Cabot, G.; Gómez-Zorrilla, S.; Zamorano, L.; Ocampo-Sosa, A.; Murillas, J.; Almirante, B.; Pomar, V.; Aguilar, M.; Granados, A.; et al. Influence of Virulence Genotype and Resistance Profile in the Mortality of Pseudomonas Aeruginosa Bloodstream Infections. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2015, 60, 539–548. [Google Scholar] [CrossRef] [PubMed]
- Dehbashi, S.; Tahmasebi, H.; Arabestani, M.R. Association between Beta-Lactam Antibiotic Resistance and Virulence Factors in AmpC Producing Clinical Strains of P. Aeruginosa. Osong Public Health Res. Perspect. 2018, 9, 325–333. [Google Scholar] [CrossRef]
- Ellappan, K.; Belgode Narasimha, H.; Kumar, S. Coexistence of Multidrug Resistance Mechanisms and Virulence Genes in Carbapenem-Resistant Pseudomonas Aeruginosa Strains from a Tertiary Care Hospital in South India. J. Glob. Antimicrob. Resist. 2018, 12, 37–43. [Google Scholar] [CrossRef]
- El-Mahdy, R.; El-Kannishy, G. Virulence Factors Of Carbapenem-Resistant Pseudomonas Aeruginosa In Hospital-Acquired Infections In Mansoura, Egypt. Infect. Drug Resist. 2019, 12, 3455–3461. [Google Scholar] [CrossRef] [PubMed]
- Sánchez-Diener, I.; Zamorano, L.; Peña, C.; Ocampo-Sosa, A.; Cabot, G.; Gómez-Zorrilla, S.; Almirante, B.; Aguilar, M.; Granados, A.; Calbo, E.; et al. Weighting the Impact of Virulence on the Outcome of Pseudomonas Aeruginosa Bloodstream Infections. Clin. Microbiol. Infect. Off. Publ. Eur. Soc. Clin. Microbiol. Infect. Dis. 2020, 26, 351–357. [Google Scholar] [CrossRef]
- McCarthy, K.L.; Wailan, A.M.; Jennison, A.V.; Kidd, T.J.; Paterson, D.L.P. Aeruginosa Blood Stream Infection Isolates: A “Full House” of Virulence Genes in Isolates Associated with Rapid Patient Death and Patient Survival. Microb. Pathog. 2018, 119, 81–85. [Google Scholar] [CrossRef]
- Boontham, P.; Robins, A.; Chandran, P.; Pritchard, D.; Cámara, M.; Williams, P.; Chuthapisith, S.; McKechnie, A.; Rowlands, B.J.; Eremin, O. Significant Immunomodulatory Effects of Pseudomonas Aeruginosa Quorum-Sensing Signal Molecules: Possible Link in Human Sepsis. Clin. Sci. Lond. Engl. 1979 2008, 115, 343–351. [Google Scholar] [CrossRef]
- Alonso, B.; Fernández-Barat, L.; Di Domenico, E.G.; Marín, M.; Cercenado, E.; Merino, I.; de Pablos, M.; Muñoz, P.; Guembe, M. Characterization of the Virulence of Pseudomonas Aeruginosa Strains Causing Ventilator-Associated Pneumonia. BMC Infect. Dis. 2020, 20, 909. [Google Scholar] [CrossRef]
- Murugan, N.; Malathi, J.; Umashankar, V.; Madhavan, H.N. Draft Genome Sequence of BlaVeb-1, Blaoxa-10 Producing Multi-Drug Resistant (MDR) Pseudomonas Aeruginosa Strain VRFPA09 Recovered from Bloodstream Infection. Braz. J. Microbiol. Publ. Braz. Soc. Microbiol. 2015, 46, 639–640. [Google Scholar] [CrossRef]
- Segata, N.; Ballarini, A.; Jousson, O. Genome Sequence of Pseudomonas Aeruginosa PA45, a Highly Virulent Strain Isolated from a Patient with Bloodstream Infection. Genome Announc. 2013, 1, e00289-13. [Google Scholar] [CrossRef] [PubMed]
- Gupte, A.; Jyot, J.; Ravi, M.; Ramphal, R. High Pyocyanin Production and Non-Motility of Pseudomonas Aeruginosa Isolates Are Correlated with Septic Shock or Death in Bacteremic Patients. PLoS ONE 2021, 16, e0253259. [Google Scholar] [CrossRef] [PubMed]
- Sharifi, H.; Pouladfar, G.; Shakibaie, M.R.; Pourabbas, B.; Mardaneh, J.; Mansouri, S. Prevalence of β-Lactamase Genes, Class 1 Integrons, Major Virulence Factors and Clonal Relationships of Multidrug-Resistant Pseudomonas Aeruginosa Isolated from Hospitalized Patients in Southeast of Iran. Iran. J. Basic Med. Sci. 2019, 22, 806–812. [Google Scholar] [CrossRef] [PubMed]
- Fuse, K.; Fujimura, S.; Kikuchi, T.; Gomi, K.; Iida, Y.; Nukiwa, T.; Watanabe, A. Reduction of Virulence Factor Pyocyanin Production in Multidrug-Resistant Pseudomonas Aeruginosa. J. Infect. Chemother. Off. J. Jpn. Soc. Chemother. 2013, 19, 82–88. [Google Scholar] [CrossRef]
- Javanmardi, F.; Emami, A.; Pirbonyeh, N.; Keshavarzi, A.; Rajaee, M. A Systematic Review and Meta-Analysis on Exo-Toxins Prevalence in Hospital Acquired Pseudomonas Aeruginosa Isolates. Infect. Genet. Evol. J. Mol. Epidemiol. Evol. Genet. Infect. Dis. 2019, 75, 104037. [Google Scholar] [CrossRef]
- Khodayary, R.; Nikokar, I.; Mobayen, M.R.; Afrasiabi, F.; Araghian, A.; Elmi, A.; Moradzadeh, M. High Incidence of Type III Secretion System Associated Virulence Factors (Exoenzymes) in Pseudomonas Aeruginosa Isolated from Iranian Burn Patients. BMC Res. Notes 2019, 12, 28. [Google Scholar] [CrossRef]
- Beasley, K.L.; Cristy, S.A.; Elmassry, M.M.; Dzvova, N.; Colmer-Hamood, J.A.; Hamood, A.N. During Bacteremia, Pseudomonas Aeruginosa PAO1 Adapts by Altering the Expression of Numerous Virulence Genes Including Those Involved in Quorum Sensing. PLoS ONE 2020, 15, e0240351. [Google Scholar] [CrossRef]
- Kruczek, C.; Kottapalli, K.R.; Dissanaike, S.; Dzvova, N.; Griswold, J.A.; Colmer-Hamood, J.A.; Hamood, A.N. Major Transcriptome Changes Accompany the Growth of Pseudomonas Aeruginosa in Blood from Patients with Severe Thermal Injuries. PLoS ONE 2016, 11, e0149229. [Google Scholar] [CrossRef]
- Elmassry, M.M.; Mudaliar, N.S.; Kottapalli, K.R.; Dissanaike, S.; Griswold, J.A.; San Francisco, M.J.; Colmer-Hamood, J.A.; Hamood, A.N. Pseudomonas Aeruginosa Alters Its Transcriptome Related to Carbon Metabolism and Virulence as a Possible Survival Strategy in Blood from Trauma Patients. mSystems 2019, 4, e00312–e00318. [Google Scholar] [CrossRef]
- Golpayegani, A.; Nodehi, R.N.; Rezaei, F.; Alimohammadi, M.; Douraghi, M. Real-Time Polymerase Chain Reaction Assays for Rapid Detection and Virulence Evaluation of the Environmental Pseudomonas Aeruginosa Isolates. Mol. Biol. Rep. 2019, 46, 4049–4061. [Google Scholar] [CrossRef]
- Ajayi, T.; Allmond, L.R.; Sawa, T.; Wiener-Kronish, J.P. Single-Nucleotide-Polymorphism Mapping of the Pseudomonas Aeruginosa Type III Secretion Toxins for Development of a Diagnostic Multiplex PCR System. J. Clin. Microbiol. 2003, 41, 3526–3531. [Google Scholar] [CrossRef] [PubMed]
| lasB | plC H | plC N | nan2 | aprA | phzM | exoU | exoS | nan1 | pilA | pilB | Genotype Number | Number of Strains (n = 71) | Percentage of Strains (%) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| + | + | + | + | + | + | + | + | + | + | - | I | 2 | 2.8 |
| + | + | + | + | + | + | + | + | + | - | - | II | 2 | 2.8 |
| + | + | + | + | + | + | + | + | - | - | - | III | 4 | 5.6 |
| + | + | + | + | + | + | + | - | + | + | - | IV | 5 | 7.0 |
| + | + | + | + | + | + | + | - | + | - | - | V | 5 | 7.0 |
| + | + | + | + | + | + | + | - | - | + | + | VI | 1 | 1.4 |
| + | + | + | + | + | + | + | - | - | - | - | VII | 10 | 14.1 |
| + | + | + | + | + | + | - | + | + | + | - | VIII | 1 | 1.4 |
| + | + | + | + | + | + | - | + | + | - | - | IX | 13 | 18.3 |
| + | + | + | + | + | + | - | + | - | - | - | X | 6 | 8.5 |
| + | + | + | + | + | - | + | + | - | - | - | XI | 1 | 1.4 |
| + | + | + | + | + | - | + | - | - | - | + | XII | 1 | 1.4 |
| + | + | + | + | + | - | + | - | - | - | - | XIII | 4 | 5.6 |
| + | + | + | + | + | - | - | + | + | - | - | XIV | 3 | 4.2 |
| + | + | + | + | + | - | - | + | - | + | - | XV | 1 | 1.4 |
| + | + | + | + | + | - | - | + | - | - | - | XVI | 1 | 1.4 |
| + | + | + | + | - | + | + | + | + | + | - | XVII | 1 | 1.4 |
| + | + | + | + | - | + | + | + | + | - | - | XVIII | 1 | 1.4 |
| + | + | + | + | - | + | - | + | - | + | + | XIX | 1 | 1.4 |
| + | + | + | + | - | - | + | + | - | - | - | XX | 1 | 1.4 |
| + | + | + | - | + | + | + | - | - | - | - | XXI | 1 | 1.4 |
| + | + | + | - | - | - | + | + | - | - | - | XXII | 1 | 1.4 |
| + | + | + | - | - | - | + | - | - | - | - | XXIII | 1 | 1.4 |
| + | + | + | - | - | - | - | + | - | - | - | XXIV | 1 | 1.4 |
| + | + | - | + | + | + | + | + | + | + | - | XXV | 1 | 1.4 |
| + | + | - | + | + | + | + | - | - | + | - | XXVI | 1 | 1.4 |
| + | + | - | - | - | - | + | - | - | - | - | XXVII | 1 | 1.4 |
| Virulence Factor Detected | Gene/PCR Primer Name | Manufacturer | Primer Sequence 5′→3′ | Tm (°C) | Annealing Temperature (°C) | Amplicon Size (bp) |
|---|---|---|---|---|---|---|
| Exotoxin U | exoU F | Sigma | CCGTTGTGGTGCCGTTGAAG | 55.9 | 64 | 134 |
| exoU R | CCAGATGTTCACCGACTCGC | 55.9 | ||||
| Exoenzyme S | exoS F | Integrated DNA Technologies | CTTGAAGGGACTCGACAAGG | 55.2 | 53 | 504 |
| exoS R | TTCAGGTCCGCGTAGTGAAT | 56.2 | ||||
| Phospholipase C (non-hemolytic) | plC N F | GTTATCGCAACCAGCCCTAC | 55.9 | 53 | 466 | |
| plC N R | AGGTCGAACACCTGGAACAC | 57.2 | ||||
| Phospholipase C (hemolytic) | plC H F | GAAGCCATGGGCTACTTCAA | 55.1 | 52 | 307 | |
| plC H R | AGAGTGACGAGGAGCGGTAG | 58.2 | ||||
| Elastase B | lasB F | Genomed | GGAATGAACGAAGCGTTCTC | 51.8 | 50 | 300 |
| lasB R | GGTCCAGTAGTAGCGGTTGG | 55.9 | ||||
| Phenazine methyltransferase | phzM F | ATGGAGAGCGGGATCGACAG | 55.9 | 54 | 875 | |
| phzM R | ATGCGGGTTTCCATCGGCAG | 55.9 | ||||
| Pilin A | pilA F | ACAGCATCCAACTGAGCG | 50.3 | 59 | 1675 | |
| pilA R | TTGACTTCCTCCAGGCTG | 50.3 | ||||
| Pilin B | pilB F | TCGAACTGATGATCGTGG | 48.0 | 54 | 408 | |
| pilB R | CTTTCGGAGTGAACATCG | 48.0 | ||||
| Neuraminidase 1 | nan1 F | AGGATGAATACTTATTTTGAT | 42.6 | 47 | 1316 | |
| nan1 R | TCACTAAATCCATCTCTGACCCGATA | 56.4 | ||||
| Neuraminidase 2 | nan2 F | GTTTTGCTGATGCTGGTTCA | 51.1 | 50 | 1161 | |
| nan2 R | TGTCCAGCAATTCTCTTGC | 49.7 | ||||
| Alkaline protease | aprA F | TGTCCAGCAATTCTCTTGC | 48.9 | 50 | 1017 | |
| aprA R | CGTTTTCCACGGTGACC | 49.5 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bogiel, T.; Depka, D.; Rzepka, M.; Mikucka, A. Decoding Genetic Features and Antimicrobial Susceptibility of Pseudomonas aeruginosa Strains Isolated from Bloodstream Infections. Int. J. Mol. Sci. 2022, 23, 9208. https://doi.org/10.3390/ijms23169208
Bogiel T, Depka D, Rzepka M, Mikucka A. Decoding Genetic Features and Antimicrobial Susceptibility of Pseudomonas aeruginosa Strains Isolated from Bloodstream Infections. International Journal of Molecular Sciences. 2022; 23(16):9208. https://doi.org/10.3390/ijms23169208
Chicago/Turabian StyleBogiel, Tomasz, Dagmara Depka, Mateusz Rzepka, and Agnieszka Mikucka. 2022. "Decoding Genetic Features and Antimicrobial Susceptibility of Pseudomonas aeruginosa Strains Isolated from Bloodstream Infections" International Journal of Molecular Sciences 23, no. 16: 9208. https://doi.org/10.3390/ijms23169208
APA StyleBogiel, T., Depka, D., Rzepka, M., & Mikucka, A. (2022). Decoding Genetic Features and Antimicrobial Susceptibility of Pseudomonas aeruginosa Strains Isolated from Bloodstream Infections. International Journal of Molecular Sciences, 23(16), 9208. https://doi.org/10.3390/ijms23169208






