The Key Role of Lysosomal Protease Cathepsins in Viral Infections
Abstract
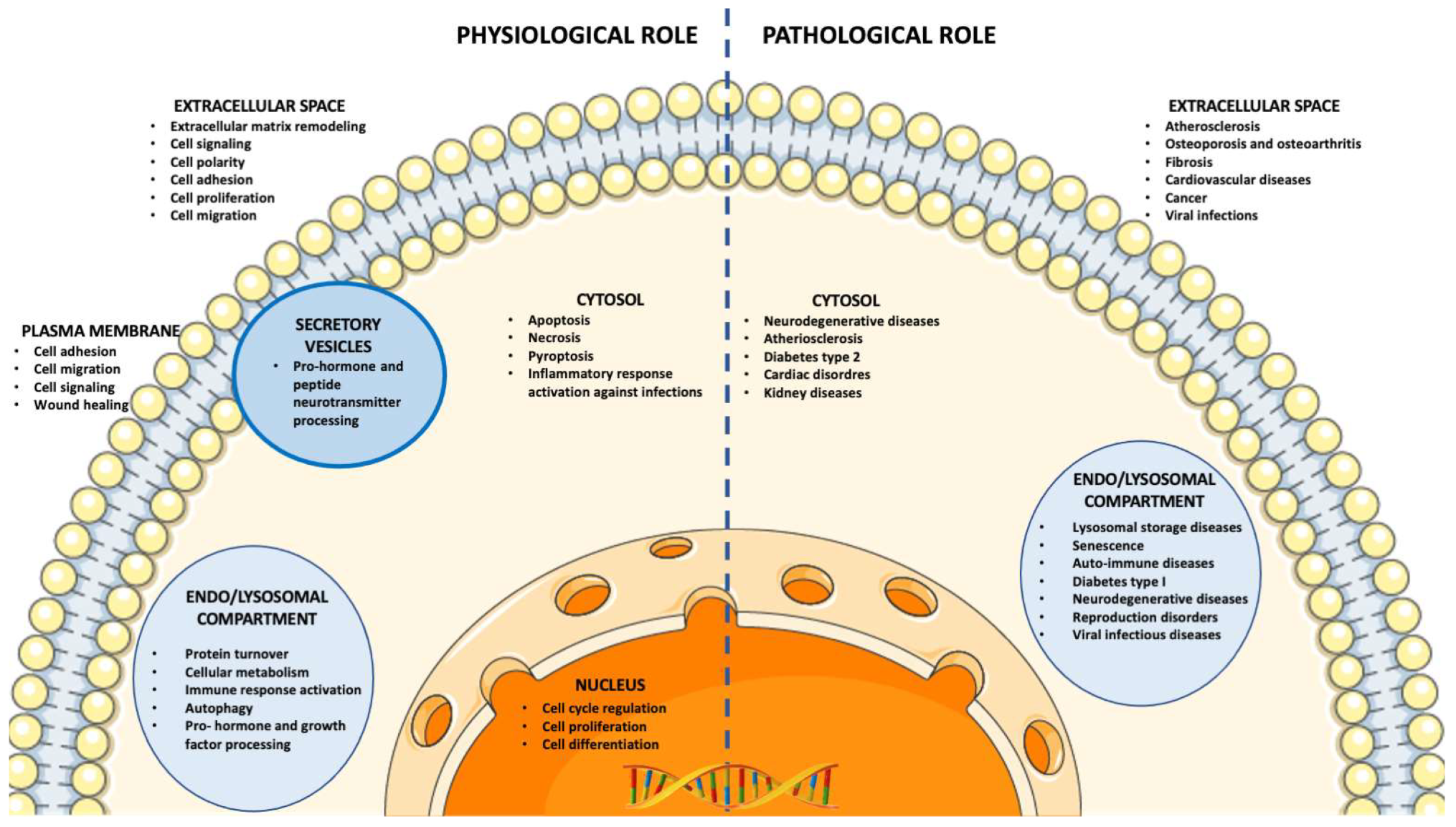
:1. Classification, Synthesis, Cellular Localization, and Physiopathological Roles of Cathepsin
2. Aid of Cathepsins to Viruses in the Host Cell Infection
3. Cathepsins as Potential Targets for Antiviral Therapies
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Schröder, B.A.; Wrocklage, C.; Hasilik, A.; Saftig, P. The proteome of lysosomes. Proteomics 2010, 10, 4053–4076. [Google Scholar] [CrossRef] [PubMed]
- Turk, V.; Stoka, V.; Vasiljeva, O.; Renko, M.; Sun, T.; Turk, B.; Turk, D. Cysteine cathepsins: From structure, function and regulation to new frontiers. Biochim. Biophys. Acta BBA-Proteins Proteom. 2012, 1824, 68–88. [Google Scholar] [CrossRef] [PubMed]
- Patel, S.; Homaei, A.; El-Seedi, H.R.; Akhtar, N. Cathepsins: Proteases that are vital for survival but can also be fatal. Biomed. Pharmacother. 2018, 105, 526–532. [Google Scholar] [CrossRef] [PubMed]
- Rawlings, N.D.; Barrett, A.J.; Finn, R. Twenty years of the MEROPS database of proteolytic enzymes, their substrates and inhibitors. Nucleic Acids Res. 2016, 44, D343–D350. [Google Scholar] [CrossRef]
- Braulke, T.; Bonifacino, J.S. Sorting of lysosomal proteins. Biochim. Biophys. Acta 2009, 1793, 605–614. [Google Scholar] [CrossRef]
- Coutinho, M.F.; Prata, M.J.; Alves, S. A shortcut to the lysosome: The mannose-6-phosphate-independent pathway. Mol. Genet. Metab. 2012, 107, 257–266. [Google Scholar] [CrossRef]
- Verma, S.; Dixit, R.; Pandey, K.C. Cysteine Proteases: Modes of Activation and Future Prospects as Pharmacological Targets. Front. Pharmacol. 2016, 7, 107. [Google Scholar] [CrossRef]
- Yadati, T.; Houben, T.; Bitorina, A.; Shiri-Sverdlov, R. The Ins and Outs of Cathepsins: Physiological Function and Role in Disease Management. Cells 2020, 9, 1679. [Google Scholar] [CrossRef]
- Wittlin, S.; Rosel, J.; Hofmann, F.; Stover, D.R. Mechanisms and kinetics of procathepsin D activation. JBIC J. Biol. Inorg. Chem. 1999, 265, 384–393. [Google Scholar] [CrossRef]
- Vasiljeva, O.; Dolinar, M.; Pungerčar, J.R.; Turk, V.; Turk, B. Recombinant human procathepsin S is capable of autocatalytic processing at neutral pH in the presence of glycosaminoglycans. FEBS Lett. 2005, 579, 1285–1290. [Google Scholar] [CrossRef]
- Pungerčar, J.R.; Caglič, D.; Sajid, M.; Dolinar, M.; Vasiljeva, O.; Požgan, U.; Turk, D.; Bogyo, M.; Turk, V.; Turk, B. Autocatalytic processing of procathepsin B is triggered by proenzyme activity. FEBS J. 2009, 276, 660–668. [Google Scholar] [CrossRef]
- Collette, J.; Bocock, J.P.; Ahn, K.; Chapman, R.L.; Godbold, G.; Yeyeodu, S.; Erickson, A.H. Biosynthesis and Alternate Targeting of the Lysosomal Cysteine Protease Cathepsin L. Int. Rev. Cytol. 2004, 241, 1–51. [Google Scholar] [CrossRef]
- Rojnik, M.; Jevnikar, Z.R.; Doljak, B.; Turk, S.; Zidar, N.; Kos, J. The influence of differential processing of procathepsin H on its aminopeptidase activity, secretion and subcellular localization in human cell lines. Eur. J. Cell Biol. 2012, 91, 757–764. [Google Scholar] [CrossRef]
- Laurent-Matha, V.; Derocq, D.; Prébois, C.; Katunuma, N.; Liaudet-Coopman, E. Processing of Human Cathepsin D Is Independent of Its Catalytic Function and Auto-Activation: Involvement of Cathepsins L and B. J. Biochem. 2006, 139, 363–371. [Google Scholar] [CrossRef]
- Fairhead, M.; Kelly, S.M.; van der Walle, C.F. A heparin binding motif on the pro-domain of human procathepsin L mediates zymogen destabilization and activation. Biochem. Biophys. Res. Commun. 2008, 366, 862–867. [Google Scholar] [CrossRef]
- Caglič, D.; Pungerčar, J.R.; Pejler, G.; Turk, V.; Turk, B. Glycosaminoglycans Facilitate Procathepsin B Activation through Disruption of Propeptide-Mature Enzyme Interactions. J. Biol. Chem. 2007, 282, 33076–33085. [Google Scholar] [CrossRef]
- Bojarski, K.K.; Karczyńska, A.S.; Samsonov, S.A. Role of Glycosaminoglycans in Procathepsin B Maturation: Molecular Mechanism Elucidated by a Computational Study. J. Chem. Inf. Model. 2020, 60, 2247–2256. [Google Scholar] [CrossRef]
- Ricard-Blum, S.; Lisacek, F. Glycosaminoglycanomics: Where we are. Glycoconj. J. 2017, 34, 339–349. [Google Scholar] [CrossRef]
- Kjellén, L.; Lindahl, U. Specificity of glycosaminoglycan–protein interactions. Curr. Opin. Struct. Biol. 2018, 50, 101–108. [Google Scholar] [CrossRef]
- De Pasquale, V.; Pavone, L.M. Heparan sulfate proteoglycans: The sweet side of development turns sour in mucopolysaccharidoses. Biochim. Biophys. Acta (BBA)-Mol. Basis Dis. 2019, 1865, 165539. [Google Scholar] [CrossRef]
- Shi, D.; Sheng, A.; Chi, L. Glycosaminoglycan-Protein Interactions and Their Roles in Human Disease. Front. Mol. Biosci. 2021, 8, 639666. [Google Scholar] [CrossRef]
- Vidak, E.; Javoršek, U.; Vizovišek, M.; Turk, B. Cysteine Cathepsins and Their Extracellular Roles: Shaping the Microenvironment. Cells 2019, 8, 264. [Google Scholar] [CrossRef]
- Dennemärker, J.; Lohmüller, T.; Müller, S.; Aguilar, S.V.; Tobin, D.J.; Peters, C.; Reinheckel, T. Impaired turnover of autophagolysosomes in cathepsin L deficiency. Biol. Chem. 2010, 391, 913–922. [Google Scholar] [CrossRef]
- Müller, S.; Dennemärker, J.; Reinheckel, T. Specific functions of lysosomal proteases in endocytic and autophagic pathways. Biochim. Biophys. Acta (BBA)-Proteins Proteom. 2012, 1824, 34–43. [Google Scholar] [CrossRef]
- Man, S.M.; Kanneganti, T.-D. Regulation of lysosomal dynamics and autophagy by CTSB/cathepsin B. Autophagy 2016, 12, 2504–2505. [Google Scholar] [CrossRef]
- Yang, M.; Liu, J.; Shao, J.; Qin, Y.; Ji, Q.; Zhang, X.; Du, J. Cathepsin S-mediated autophagic flux in tumor-associated macrophages accelerate tumor development by promoting M2 polarization. Mol. Cancer 2014, 13, 43. [Google Scholar] [CrossRef]
- Bárány, I.; Berenguer, E.; Solís, M.-T.; Pérez-Pérez, Y.; Santamaria, M.E.; Crespo, J.L.; Risueño, M.C.; Díaz, I.; Testillano, P.S. Autophagy is activated and involved in cell death with participation of cathepsins during stress-induced microspore embryogenesis in barley. J. Exp. Bot. 2018, 69, 1387–1402. [Google Scholar] [CrossRef]
- Winckler, B.; Faundez, V.; Maday, S.; Cai, Q.; Almeida, C.G.; Zhang, H. The Endolysosomal System and Proteostasis: From Development to Degeneration. J. Neurosci. 2018, 38, 9364–9374. [Google Scholar] [CrossRef]
- Andres-Alonso, M.; Kreutz, M.R.; Karpova, A. Autophagy and the endolysosomal system in presynaptic function. Cell Mol. Life Sci. 2020, 78, 2621–2639. [Google Scholar] [CrossRef]
- Hsu, A.; Podvin, S.; Hook, V. Lysosomal Cathepsin Protease Gene Expression Profiles in the Human Brain During Normal Development. J. Mol. Neurosci. 2018, 65, 420–431. [Google Scholar] [CrossRef]
- Authier, F.; Kouach, M.; Briand, G. Endosomal proteolysis of insulin-like growth factor-I at its C-terminal D-domain by cathepsin B. FEBS Lett. 2005, 579, 4309–4316. [Google Scholar] [CrossRef] [PubMed]
- Palesch, D.; Wagner, J.; Meid, A.; Molenda, N.; Sienczyk, M.; Burkhardt, J.; Münch, J.; Prokop, L.; Stevanovic, S.; Westhoff, M.-A.; et al. Cathepsin G-mediated proteolytic degradation of MHC class I molecules to facilitate immune detection of human glioblastoma cells. Cancer Immunol. Immunother. 2016, 65, 283–291. [Google Scholar] [CrossRef] [PubMed]
- Yan, X.; Wu, Z.; Wang, B.; Yu, T.; Hu, Y.; Wang, S.; Deng, C.; Zhao, B.; Nakanishi, H.; Zhang, X. Involvement of Cathepsins in Innate and Adaptive Immune Responses in Periodontitis. Evid.-Based Complement. Altern. Med. 2020, 2020, 4517587. [Google Scholar] [CrossRef] [PubMed]
- Nanut, M.P.; Fonović, U.P.; Jakoš, T.; Kos, J. The Role of Cysteine Peptidases in Hematopoietic Stem Cell Differentiation and Modulation of Immune System Function. Front. Immunol. 2021, 12, 680279. [Google Scholar] [CrossRef] [PubMed]
- Campden, R.I.; Zhang, Y. The role of lysosomal cysteine cathepsins in NLRP3 inflammasome activation. Arch. Biochem. Biophys. 2019, 670, 32–42. [Google Scholar] [CrossRef] [PubMed]
- Creasy, B.M.; McCoy, K.L. Cytokines regulate cysteine cathepsins during TLR responses. Cell. Immunol. 2011, 267, 56–66. [Google Scholar] [CrossRef] [PubMed]
- Ketterer, S.; Gomez-Auli, A.; Hillebrand, L.E.; Petrera, A.; Ketscher, A.; Reinheckel, T. Inherited diseases caused by mutations in cathepsin protease genes. FEBS J. 2017, 284, 1437–1454. [Google Scholar] [CrossRef] [PubMed]
- Timur, Z.K.; Demir, S.A.; Seyrantepe, V. Lysosomal Cathepsin a Plays a Significant Role in the Processing of Endogenous Bioactive Peptides. Front. Mol. Biosci. 2016, 3, 68. [Google Scholar] [CrossRef]
- De Pasquale, V.; Moles, A.; Pavone, L.M. Cathepsins in the Pathophysiology of Mucopolysaccharidoses: New Perspectives for Therapy. Cells 2020, 9, 979. [Google Scholar] [CrossRef]
- Afinogenova, Y.; Ruan, J.; Yang, R.; Kleytman, N.; Pastores, G.; Lischuk, A.; Mistry, P.K. Aberrant progranulin, YKL-40, cathepsin D and cathepsin S in Gaucher disease. Mol. Genet. Metab. 2019, 128, 62–67. [Google Scholar] [CrossRef]
- Hook, V.; Funkelstein, L.; Wegrzyn, J.; Bark, S.; Kindy, M.; Hook, G. Cysteine Cathepsins in the secretory vesicle produce active peptides: Cathepsin L generates peptide neurotransmitters and cathepsin B produces beta-amyloid of Alzheimer’s disease. Biochim. Biophys. Acta (BBA)-Proteins Proteom. 2012, 1824, 89–104. [Google Scholar] [CrossRef]
- Hook, V.; Yoon, M.; Mosier, C.; Ito, G.; Podvin, S.; Head, B.P.; Rissman, R.; O’Donoghue, A.J.; Hook, G. Cathepsin B in neurodegeneration of Alzheimer’s disease, traumatic brain injury, and related brain disorders. Biochim. Biophys. Acta (BBA)-Proteins Proteom. 2020, 1868, 140428. [Google Scholar] [CrossRef]
- Drobny, A.; Huarcaya, S.P.; Dobert, J.; Kluge, A.; Bunk, J.; Schlothauer, T.; Zunke, F. The role of lysosomal cathepsins in neurodegeneration: Mechanistic insights, diagnostic potential and therapeutic approaches. Biochim. Biophys. Acta Mol. Cell Res. 2022, 1869, 119243. [Google Scholar] [CrossRef]
- Hsing, L.C.; Kirk, E.A.; McMillen, T.S.; Hsiao, S.-H.; Caldwell, M.; Houston, B.; Rudensky, A.Y.; LeBoeuf, R.C. Roles for cathepsins S, L, and B in insulitis and diabetes in the NOD mouse. J. Autoimmun. 2010, 34, 96–104. [Google Scholar] [CrossRef]
- Oberle, C.; Huai, J.; Reinheckel, T.; Tacke, M.; Rassner, M.; Ekert, P.; Buellesbach, J.; Borner, C. Lysosomal membrane permeabilization and cathepsin release is a Bax/Bak-dependent, amplifying event of apoptosis in fibroblasts and monocytes. Cell Death Differ. 2010, 17, 1167–1178. [Google Scholar] [CrossRef]
- Stoka, V.; Turk, V.; Turk, B. Lysosomal cysteine cathepsins: Signaling pathways in apoptosis. Biol. Chem. 2007, 388, 555–560. [Google Scholar] [CrossRef]
- Kavčič, N.; Butinar, M.; Sobotič, B.; Česen, M.H.; Petelin, A.; Bojić, L.; Bergant, T.Z.; Bratovš, A.; Reinheckel, T.; Turk, B. Intracellular cathepsin C levels determine sensitivity of cells to leucyl-leucine methyl ester-triggered apoptosis. FEBS J. 2020, 287, 5148–5166. [Google Scholar] [CrossRef]
- Stoka, V.; Turk, V.; Turk, B. Lysosomal cathepsins and their regulation in aging and neurodegeneration. Ageing Res. Rev. 2016, 32, 22–37. [Google Scholar] [CrossRef]
- Lowry, J.R.; Klegeris, A. Emerging roles of microglial cathepsins in neurodegenerative disease. Brain Res. Bull. 2018, 139, 144–156. [Google Scholar] [CrossRef]
- Ding, L.; Houben, T.; Oligschlaeger, Y.; Bitorina, A.V.; Verwer, B.J.; Tushuizen, M.E.; Shiri-Sverdlov, R. Plasma Cathepsin D Activity Rather Than Levels Correlates with Metabolic Parameters of Type 2 Diabetes in Male Individuals. Front. Endocrinol. 2020, 11, 575070. [Google Scholar] [CrossRef]
- Liu, L.; Chen, B.; Zhang, X.; Tan, L.; Wang, D.W. Increased Cathepsin D Correlates with Clinical Parameters in Newly Diagnosed Type 2 Diabetes. Dis. Mark. 2017, 2017, 5286408. [Google Scholar] [CrossRef]
- Cocchiaro, P.; De Pasquale, V.; Della Morte, R.; Tafuri, S.; Avallone, L.; Pizard, A.; Moles, A.; Pavone, L.M. The Multifaceted Role of the Lysosomal Protease Cathepsins in Kidney Disease. Front. Cell Dev. Biol. 2017, 5, 114. [Google Scholar] [CrossRef]
- Cocchiaro, P.; Fox, C.; Tregidgo, N.W.; Howarth, R.; Wood, K.M.; Situmorang, G.; Pavone, L.M.; Sheerin, N.S.; Moles, A. Lysosomal protease cathepsin D; a new driver of apoptosis during acute kidney injury. Sci. Rep. 2016, 6, 27112. [Google Scholar] [CrossRef]
- Xu, M.; Yang, L.; Rong, J.-G.; Ni, Y.; Gu, W.-W.; Luo, Y.; Ishidoh, K.; Katunuma, N.; Li, Z.-S.; Zhang, H.-L. Inhibition of cysteine cathepsin B and L activation in astrocytes contributes to neuroprotection against cerebral ischemia via blocking the tBid-mitochondrial apoptotic signaling pathway. Glia 2014, 62, 855–880. [Google Scholar] [CrossRef]
- Xu, W.; Yu, C.; Piao, L.; Inoue, A.; Wang, H.; Meng, X.; Li, X.; Cui, L.; Umegaki, H.; Shi, G.-P.; et al. Cathepsin S-Mediated Negative Regulation of Wnt5a/SC35 Activation Contributes to Ischemia-Induced Neovascularization in Aged Mice. Circ. J. 2019, 83, 2537–2546. [Google Scholar] [CrossRef]
- Peng, K.; Liu, H.; Yan, B.; Meng, X.; Song, S.; Ji, F.; Xia, Z. Inhibition of cathepsin S attenuates myocardial ischemia/reperfusion injury by suppressing inflammation and apoptosis. J. Cell. Physiol. 2021, 236, 1309–1320. [Google Scholar] [CrossRef]
- Soond, S.M.; Kozhevnikova, M.V.; Frolova, A.S.; Savvateeva, L.V.; Plotnikov, E.Y.; Townsend, P.A.; Han, Y.-P.; Zamyatnin, A.A. Lost or Forgotten: The nuclear cathepsin protein isoforms in cancer. Cancer Lett. 2019, 462, 43–50. [Google Scholar] [CrossRef]
- Manou, D.; Caon, I.; Bouris, P.; Triantaphyllidou, I.-E.; Giaroni, C.; Passi, A.; Karamanos, N.K.; Vigetti, D.; Theocharis, A.D. The Complex Interplay Between Extracellular Matrix and Cells in Tissues. Methods Mol. Biol. 2019, 1952, 1–20. [Google Scholar] [CrossRef]
- Vizovišek, M.; Fonović, M.; Turk, B. Cysteine cathepsins in extracellular matrix remodeling: Extracellular matrix degradation and beyond. Matrix Biol. 2019, 75–76, 141–159. [Google Scholar] [CrossRef]
- Brix, K. Host Cell Proteases: Cathepsins. In Activation of Viruses by Host Proteases; Springer: Cham, Switzerland, 2018; pp. 249–276. [Google Scholar] [CrossRef]
- Maginnis, M.S. Virus-Receptor Interactions: The Key to Cellular Invasion. J. Mol. Biol. 2018, 430, 2590–2611. [Google Scholar] [CrossRef]
- Grove, J.; Marsh, M. The cell biology of receptor-mediated virus entry. J. Cell Biol. 2011, 195, 1071–1082. [Google Scholar] [CrossRef] [PubMed]
- Schornberg, K.; Matsuyama, S.; Kabsch, K.; Delos, S.; Bouton, A.; White, J. Role of Endosomal Cathepsins in Entry Mediated by the Ebola Virus Glycoprotein. J. Virol. 2006, 80, 4174–4178. [Google Scholar] [CrossRef] [PubMed]
- Kaletsky, R.L.; Simmons, G.; Bates, P. Proteolysis of the Ebola Virus Glycoproteins Enhances Virus Binding and Infectivity. J. Virol. 2007, 81, 13378–13384. [Google Scholar] [CrossRef] [PubMed]
- Yamaoka, S.; Ebihara, H. Pathogenicity and Virulence of Ebolaviruses with Species- and Variant-specificity. Virulence 2021, 12, 885–901. [Google Scholar] [CrossRef] [PubMed]
- Fels, J.M.; Bortz, R.H.; Alkutkar, T.; Mittler, E.; Jangra, R.K.; Spence, J.S.; Chandran, K. A Glycoprotein Mutation That Emerged during the 2013–2016 Ebola Virus Epidemic Alters Proteolysis and Accelerates Membrane Fusion. mBio 2021, 12, e03616-20. [Google Scholar] [CrossRef] [PubMed]
- Dabydeen, S.A.; Meneses, P.I. The role of NH4Cl and cysteine proteases in Human Papillomavirus type 16 infection. Virol. J. 2009, 6, 109–112. [Google Scholar] [CrossRef] [PubMed]
- Calton, C.M.; Schlegel, A.; Chapman, J.A.; Campos, S. Human papillomavirus type 16 does not require cathepsin L or B for infection. J. Gen. Virol. 2013, 94, 1865–1869. [Google Scholar] [CrossRef]
- Cerqueira, C.; Ventayol, P.S.; Vogeley, C.; Schelhaas, M. Kallikrein-8 Proteolytically Processes Human Papillomaviruses in the Extracellular Space to Facilitate Entry into Host Cells. J. Virol. 2015, 89, 7038–7052. [Google Scholar] [CrossRef]
- Ebert, D.H.; Deussing, J.; Peters, C.; Dermody, T.S. Cathepsin L and Cathepsin B Mediate Reovirus Disassembly in Murine Fibroblast Cells. J. Biol. Chem. 2002, 277, 24609–24617. [Google Scholar] [CrossRef]
- Golden, J.W.; Bahe, J.A.; Lucas, W.T.; Nibert, M.L.; Schiff, L.A. Cathepsin S Supports Acid-independent Infection by Some Reoviruses. J. Biol. Chem. 2004, 279, 8547–8557. [Google Scholar] [CrossRef]
- Mainou, B.A. The Orchestra of Reovirus Cell Entry. Curr. Clin. Microbiol. Rep. 2017, 4, 142–149. [Google Scholar] [CrossRef]
- Huang, I.-C.; Bosch, B.J.; Li, F.; Li, W.; Lee, K.H.; Ghiran, S.; Vasilieva, N.; Dermody, T.S.; Harrison, S.C.; Dormitzer, P.R.; et al. SARS Coronavirus, but Not Human Coronavirus NL63, Utilizes Cathepsin L to Infect ACE2-expressing Cells. J. Biol. Chem. 2006, 281, 3198–3203. [Google Scholar] [CrossRef]
- Pišlar, A.; Mitrović, A.; Sabotič, J.; Fonović, U.P.; Nanut, M.P.; Jakoš, T.; Senjor, E.; Kos, J. The role of cysteine peptidases in coronavirus cell entry and replication: The therapeutic potential of cathepsin inhibitors. PLoS Pathog. 2020, 16, e1009013. [Google Scholar] [CrossRef]
- Millet, J.K.; Whittaker, G.R. Host cell proteases: Critical determinants of coronavirus tropism and pathogenesis. Virus Res. 2015, 202, 120–134. [Google Scholar] [CrossRef]
- Li, F. Structure, Function, and Evolution of Coronavirus Spike Proteins. Annu. Rev. Virol. 2016, 3, 237–261. [Google Scholar] [CrossRef]
- Hartenian, E.; Nandakumar, D.; Lari, A.; Ly, M.; Tucker, J.M.; Glaunsinger, B.A. The molecular virology of coronaviruses. J. Biol. Chem. 2020, 295, 12910–12934. [Google Scholar] [CrossRef]
- Park, J.-E.; Li, K.; Barlan, A.; Fehr, A.R.; Perlman, S.; McCray, P.B.; Gallagher, T. Proteolytic processing of Middle East respiratory syndrome coronavirus spikes expands virus tropism. Proc. Natl. Acad. Sci. USA 2016, 113, 12262–12267. [Google Scholar] [CrossRef]
- Kleine-Weber, H.; Elzayat, M.T.; Hoffmann, M.; Pöhlmann, S. Functional analysis of potential cleavage sites in the MERS-coronavirus spike protein. Sci. Rep. 2018, 8, 16597. [Google Scholar] [CrossRef]
- Shang, J.; Wan, Y.; Luo, C.; Ye, G.; Geng, Q.; Auerbach, A.; Li, F. Cell entry mechanisms of SARS-CoV-2. Proc. Natl. Acad. Sci. USA 2020, 117, 11727–11734. [Google Scholar] [CrossRef]
- Jaimes., J.; Millet, J.; Whittaker, G. Proteolytic Cleavage of the SARS-CoV-2 Spike Protein and the Role of the Novel S1/S2 Site. SSRN 2020, 3581359, preprintUpdate in iScience 2020, 23, 101212. [Google Scholar] [CrossRef]
- Hoffmann, M.; Kleine-Weber, H.; Schroeder, S.; Krüger, N.; Herrler, T.; Erichsen, S.; Schiergens, T.S.; Herrler, G.; Wu, N.-H.; Nitsche, A.; et al. SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically Proven Protease Inhibitor. Cell 2020, 181, 271–280.e8. [Google Scholar] [CrossRef]
- Seyran, M.; Takayama, K.; Uversky, V.N.; Lundstrom, K.; Palù, G.; Sherchan, S.P.; Attrish, D.; Rezaei, N.; Aljabali, A.A.A.; Ghosh, S.; et al. The structural basis of accelerated host cell entry by SARS-CoV-2. FEBS J. 2021, 288, 5010–5020. [Google Scholar] [CrossRef]
- Zhao, M.-M.; Yang, W.-L.; Yang, F.-Y.; Zhang, L.; Huang, W.-J.; Hou, W.; Fan, C.-F.; Jin, R.-H.; Feng, Y.-M.; Wang, Y.-C.; et al. Cathepsin L plays a key role in SARS-CoV-2 infection in humans and humanized mice and is a promising target for new drug development. Signal Transduct. Target. Ther. 2021, 6, 134. [Google Scholar] [CrossRef]
- Bollavaram, K.; Leeman, T.H.; Lee, M.W.; Kulkarni, A.; Upshaw, S.G.; Yang, J.; Song, H.; Platt, M.O. Multiple sites on SARS-CoV-2 spike protein are susceptible to proteolysis by cathepsins B, K, L, S, and V. Protein Sci. 2021, 30, 1131–1143. [Google Scholar] [CrossRef]
- Edinger, T.O.; Pohl, M.; Yángüez, E.; Stertz, S. Cathepsin W Is Required for Escape of Influenza A Virus from Late Endosomes. mBio 2015, 6, e00297-15. [Google Scholar] [CrossRef]
- Pager, C.T.; Dutch, R.E. Cathepsin L Is Involved in Proteolytic Processing of the Hendra Virus Fusion Protein. J. Virol. 2005, 79, 12714–12720. [Google Scholar] [CrossRef]
- Diederich, S.; Sauerhering, L.; Weis, M.; Altmeppen, H.; Schaschke, N.; Reinheckel, T.; Erbar, S.; Maisner, A. Activation of the Nipah Virus Fusion Protein in MDCK Cells Is Mediated by Cathepsin B within the Endosome-Recycling Compartment. J. Virol. 2012, 86, 3736–3745. [Google Scholar] [CrossRef]
- Hadigal, S.; Koganti, R.; Yadavalli, T.; Agelidis, A.; Suryawanshi, R.; Shukla, D. Heparanase-Regulated Syndecan-1 Shedding Facilitates Herpes Simplex Virus 1 Egress. J. Virol. 2020, 94, e01672–e01719. [Google Scholar] [CrossRef] [PubMed]
- Agelidis, A.; Shukla, D. Heparanase, Heparan Sulfate and Viral Infection. Adv. Exp. Med. Biol. 2019, 1221, 759–770. [Google Scholar] [CrossRef]
- Vlodavsky, I.; Ilan, N.; Sanderson, R.D. Forty Years of Basic and Translational Heparanase Research. Adv. Exp. Med. Biol. 2020, 1221, 3–59. [Google Scholar] [CrossRef] [PubMed]
- Vlodavsky, I.; Barash, U.; Nguyen, H.M.; Yang, S.-M.; Ilan, N. Biology of the Heparanase-Heparan Sulfate Axis and Its Role in Disease Pathogenesis. Semin. Thromb. Hemost. 2021, 47, 240–253. [Google Scholar] [CrossRef]
- Mayfosh, A.J.; Nguyen, T.K.; Hulett, M.D. The Heparanase Regulatory Network in Health and Disease. Int. J. Mol. Sci. 2021, 22, 11096. [Google Scholar] [CrossRef]
- De Pasquale, V.; Quiccione, M.; Tafuri, S.; Avallone, L.; Pavone, L. Heparan Sulfate Proteoglycans in Viral Infection and Treatment: A Special Focus on SARS-CoV-2. Int. J. Mol. Sci. 2021, 22, 6574. [Google Scholar] [CrossRef]
- Abboud-Jarrous, G.; Atzmon, R.; Peretz, T.; Palermo, C.; Gadea, B.B.; Joyce, J.A.; Vlodavsky, I. Cathepsin L Is Responsible for Processing and Activation of Proheparanase through Multiple Cleavages of a Linker Segment. J. Biol. Chem. 2008, 283, 18167–18176. [Google Scholar] [CrossRef]
- Iozzo, R.V.; Schaefer, L. Proteoglycan form and function: A comprehensive nomenclature of proteoglycans. Matrix Biol. 2015, 42, 11–55. [Google Scholar] [CrossRef]
- Khanna, M.; Parish, C.R. Heparanase: Historical Aspects and Future Perspectives. Adv. Exp. Med. Biol. 2020, 1221, 71–96. [Google Scholar] [CrossRef]
- Billings, P.C.; Pacifici, M. Interactions of signaling proteins, growth factors and other proteins with heparan sulfate: Mechanisms and mysteries. Connect. Tissue Res. 2015, 56, 272–280. [Google Scholar] [CrossRef]
- Cagno, V.; Tseligka, E.D.; Jones, S.T.; Tapparel, C. Heparan sulfate proteoglycans and viral attachment: True receptors or adaptation bias? Viruses 2019, 11, 596. [Google Scholar] [CrossRef]
- Clausen, T.M.; Sandoval, D.R.; Spliid, C.B.; Pihl, J.; Perrett, H.R.; Painter, C.D.; Narayanan, A.; Majowicz, S.A.; Kwong, E.M.; McVicar, R.N.; et al. SARS-CoV-2 Infection Depends on Cellular Heparan Sulfate and ACE2. Cell 2020, 183, 1043–1057.e15. [Google Scholar] [CrossRef]
- Zhang, Q.; Chen, C.Z.; Swaroop, M.; Xu, M.; Wang, L.; Lee, J.; Wang, A.Q.; Pradhan, M.; Hagen, N.; Chen, L.; et al. Heparan sulfate assists SARS-CoV-2 in cell entry and can be targeted by approved drugs in vitro. Cell Discov. 2020, 6, 80. [Google Scholar] [CrossRef]
- Hadigal, S.R.; Agelidis, A.M.; Karasneh, G.A.; Antoine, T.E.; Yakoub, A.M.; Ramani, V.C.; Djalilian, A.R.; Sanderson, R.D.; Shukla, D. Heparanase is a host enzyme required for herpes simplex virus-1 release from cells. Nat. Commun. 2015, 6, 6985. [Google Scholar] [CrossRef]
- Hopkins, J.; Yadavalli, T.; Agelidis, A.M.; Shukla, D. Host Enzymes Heparanase and Cathepsin L Promote Herpes Simplex Virus 2 Release from Cells. J. Virol. 2018, 92, e01179-18. [Google Scholar] [CrossRef]
- Guo, C.; Zhu, Z.; Guo, Y.; Wang, X.; Yu, P.; Xiao, S.; Chen, Y.; Cao, Y.; Liu, X. Heparanase Upregulation Contributes to Porcine Reproductive and Respiratory Syndrome Virus Release. J. Virol. 2017, 91, e00625-17. [Google Scholar] [CrossRef]
- Puerta-Guardo, H.; Glasner, D.; Harris, E. Dengue Virus NS1 Disrupts the Endothelial Glycocalyx, Leading to Hyperpermeability. PLoS Pathog. 2016, 12, e1005738. [Google Scholar] [CrossRef]
- Thakkar, N.; Yadavalli, T.; Jaishankar, D.; Shukla, D. Emerging Roles of Heparanase in Viral Pathogenesis. Pathogens 2017, 6, 43. [Google Scholar] [CrossRef]
- Surviladze, Z.; Sterkand, R.T.; Ozbun, M.A. Interaction of human papillomavirus type 16 particles with heparan sulfate and syndecan-1 molecules in the keratinocyte extracellular matrix plays an active role in infection. J. Gen. Virol. 2015, 96, 2232–2241. [Google Scholar] [CrossRef]
- Tao, Y.; Wang, Z.; Zhou, Y. Expression of heparanase in kidney of rats with respiratory syncytial virus nephropathy and its relationship with proteinurina. Sichuan Da Xue Xue Bao Yi Xue Ban 2014, 45, 212–215. (In Chinese) [Google Scholar]
- Barth, H.; Schnober, E.K.; Zhang, F.; Linhardt, R.J.; Depla, E.; Boson, B.; Cosset, F.-L.; Patel, A.H.; Blum, H.E.; Baumert, T.F. Viral and Cellular Determinants of the Hepatitis C Virus Envelope-Heparan SulfateInteraction. J. Virol. 2006, 80, 10579–10590. [Google Scholar] [CrossRef]
- Buijsers, B.; Yanginlar, C.; de Nooijer, A.; Grondman, I.; Maciej-Hulme, M.L.; Jonkman, I.; Janssen, N.A.F.; Rother, N.; de Graaf, M.; Pickkers, P.; et al. Increased Plasma Heparanase Activity in COVID-19 Patients. Front. Immunol. 2020, 11, 575047. [Google Scholar] [CrossRef]
- Koganti, R.; Suryawanshi, R.; Shukla, D. Heparanase, cell signaling, and viral infections. Cell Mol. Life Sci. 2020, 77, 5059–5077. [Google Scholar] [CrossRef] [PubMed]
- Kinaneh, S.; Khamaysi, I.; Karram, T.; Hamoud, S. Heparanase as a potential player in SARS-CoV-2 infection and induced coagulopathy. Biosci. Rep. 2021, 41, BSR20210290. [Google Scholar] [CrossRef] [PubMed]
- Rudensky, A.; Beers, C. Lysosomal Cysteine Proteases and Antigen Presentation. Ernst. Scher. Res. Found Workshop 2006, 56, 81–95. [Google Scholar] [CrossRef]
- Kopitar-Jerala, N. The Role of Cysteine Proteinases and their Inhibitors in the Host-Pathogen Cross Talk. Curr. Protein Pept. Sci. 2012, 13, 767–775. [Google Scholar] [CrossRef] [PubMed]
- Manoury, B. Proteases: Essential Actors in Processing Antigens and Intracellular Toll-Like Receptors. Front. Immunol. 2013, 4, 299. [Google Scholar] [CrossRef]
- Jakoš, T.; Pišlar, A.; Jewett, A.; Kos, J. Cysteine Cathepsins in Tumor-Associated Immune Cells. Front. Immunol. 2019, 10, 2037. [Google Scholar] [CrossRef]
- Mielcarska, M.B.; Bossowska-Nowicka, M.; Toka, F.N. Cell Surface Expression of Endosomal Toll-Like Receptors—A Necessity or a Superfluous Duplication? Front. Immunol. 2021, 11, 620972. [Google Scholar] [CrossRef]
- Foronjy, R.F.; Taggart, C.; Dabo, A.J.; Weldon, S.; Cummins, N.; Geraghty, P. Type-I interferons induce lung protease responses following respiratory syncytial virus infection via RIG-I-like receptors. Mucosal Immunol. 2015, 8, 161–175. [Google Scholar] [CrossRef]
- Embgenbroich, M.; Burgdorf, S. Current Concepts of Antigen Cross-Presentation. Front. Immunol. 2018, 9, 1643. [Google Scholar] [CrossRef]
- Strumillo, S.T.; Kartavykh, D.; de Carvalho, F.F., Jr.; Cruz, N.C.; de Souza Teodoro, A.C.; Sobhie Diaz, R.; Curcio, M.F. Host-virus interaction and viral evasion. Cell Biol. Int. 2021, 45, 1124–1147. [Google Scholar] [CrossRef]
- Bossowska-Nowicka, M.; Mielcarska, M.B.; Romaniewicz, M.; Kaczmarek, M.M.; Gregorczyk-Zboroch, K.P.; Struzik, J.; Grodzik, M.; Gieryńska, M.M.; Toka, F.N.; Szulc-Dąbrowska, L. Ectromelia virus suppresses expression of cathepsins and cystatins in conventional dendritic cells to efficiently execute the replication process. BMC Microbiol. 2019, 19, 92. [Google Scholar] [CrossRef]
- Harman, A.N.; Kraus, M.; Bye, C.R.; Byth, K.; Turville, S.G.; Tang, O.; Mercier, S.K.; Nasr, N.; Stern, J.L.; Slobedman, B.; et al. HIV-1-infected dendritic cells show 2 phases of gene expression changes, with lysosomal enzyme activity decreased during the second phase. Blood 2009, 114, 85–94. [Google Scholar] [CrossRef]
- Burster, T.; Giffon, T.; Dahl, M.E.; Björck, P.; Bogyo, M.; Weber, E.; Mahmood, K.; Lewis, D.B.; Mellins, E.D. Influenza A virus elevates active cathepsin B in primary murine DC. Int. Immunol. 2007, 19, 645–655. [Google Scholar] [CrossRef]
- Coleman, M.D.; Ha, S.D.; Haeryfar, S.M.; Barr, S.D.; Kim, S.O. Cathepsin B Plays a Key Role in Optimal Production of the Influenza A- Virus. J. Virol. Antivir. Res. 2018, 7, 1–20. [Google Scholar] [CrossRef]
- Kim, H.; Mazumdar, B.; Bose, S.K.; Meyer, K.; Di Bisceglie, A.M.; Hoft, D.F.; Ray, R. Hepatitis C Virus-Mediated Inhibition of Cathepsin S Increases Invariant-Chain Expression on Hepatocyte Surface. J. Virol. 2012, 86, 9919–9928. [Google Scholar] [CrossRef]
- Hu, W.; Yen, Y.-T.; Singh, S.; Kao, C.-L.; Wu-Hsieh, B.A. SARS-CoV Regulates Immune Function-Related Gene Expression in Human Monocytic Cells. Viral Immunol. 2012, 25, 277–288. [Google Scholar] [CrossRef]
- Crow, M.S.; Lum, K.K.; Sheng, X.; Song, B.; Cristea, I.M. Diverse mechanisms evolved by DNA viruses to inhibit early host defenses. Crit. Rev. Biochem. Mol. Biol. 2016, 51, 452–481. [Google Scholar] [CrossRef]
- Li, D.; Wu, M. Pattern recognition receptors in health and diseases. Signal Transduct. Target. Ther. 2021, 6, 291. [Google Scholar] [CrossRef]
- Rex, D.A.B.; Prasad, T.S.K.; Kandasamy, R.K. Revisiting Regulated Cell Death Responses in Viral Infections. Int. J. Mol. Sci. 2022, 23, 7023. [Google Scholar] [CrossRef]
- Fay, E.J.; Aron, S.L.; Macchietto, M.G.; Markman, M.W.; Esser-Nobis, K.; Gale, M.; Shen, S.; Langlois, R.A. Cell type- and replication stage-specific influenza virus responses in vivo. PLoS Pathog. 2020, 16, e1008760. [Google Scholar] [CrossRef]
- Malik, G.; Zhou, Y. Innate Immune Sensing of Influenza A Virus. Viruses 2020, 12, 755. [Google Scholar] [CrossRef]
- Lamotte, L.-A.; Tafforeau, L. How Influenza A Virus NS1 Deals with the Ubiquitin System to Evade Innate Immunity. Viruses 2021, 13, 2309. [Google Scholar] [CrossRef]
- Ma, J.; Sun, Q.; Mi, R.; Zhang, H. Avian influenza A virus H5N1 causes autophagy-mediated cell death through suppression of mTOR signaling. J. Genet. Genom. 2011, 38, 533–537. [Google Scholar] [CrossRef]
- Gannagé, M.; Dormann, D.; Albrecht, R.; Dengjel, J.; Torossi, T.; Rämer, P.C.; Lee, M.; Strowig, T.; Arrey, F.; Conenello, G.; et al. Matrix Protein 2 of Influenza A Virus Blocks Autophagosome Fusion with Lysosomes. Cell Host Microbe 2009, 6, 367–380. [Google Scholar] [CrossRef]
- Beale, R.; Wise, H.; Stuart, A.; Ravenhill, B.J.; Digard, P.; Randow, F. A LC3-Interacting Motif in the Influenza A Virus M2 Protein Is Required to Subvert Autophagy and Maintain Virion Stability. Cell Host Microbe 2014, 15, 239–247. [Google Scholar] [CrossRef]
- Galluzzi, L.; Brenner, C.; Morselli, E.; Touat, Z.; Kroemer, G. Viral Control of Mitochondrial Apoptosis. PLoS Pathog. 2008, 4, e1000018. [Google Scholar] [CrossRef]
- Liu, B.; Fang, M.; Hu, Y.; Huang, B.; Li, N.; Chang, C.; Huang, R.; Xu, X.; Yang, Z.; Chen, Z.; et al. Hepatitis B virus X protein inhibits autophagic degradation by impairing lysosomal maturation. Autophagy 2014, 10, 416–430. [Google Scholar] [CrossRef]
- Furman, L.M.; Maaty, W.S.; Petersen, L.K.; Ettayebi, K.; Hardy, M.E.; Bothner, B. Cysteine protease activation and apoptosis in Murine norovirus infection. Virol. J. 2009, 6, 139. [Google Scholar] [CrossRef]
- Morchang, A.; Panaampon, J.; Suttitheptumrong, A.; Yasamut, U.; Noisakran, S.; Yenchitsomanus, P.-T.; Limjindaporn, T. Role of cathepsin B in dengue virus-mediated apoptosis. Biochem. Biophys. Res. Commun. 2013, 438, 20–25. [Google Scholar] [CrossRef]
- Wang, Y.; Jia, L.; Shen, J.; Wang, Y.; Fu, Z.; Su, S.-A.; Cai, Z.; Wang, J.-A.; Xiang, M. Cathepsin B aggravates coxsackievirus B3-induced myocarditis through activating the inflammasome and promoting pyroptosis. PLoS Pathog. 2018, 14, e1006872. [Google Scholar] [CrossRef]
- Fung, S.-Y.; Yuen, K.-S.; Ye, Z.-W.; Chan, C.-P.; Jin, D.-Y. A tug-of-war between severe acute respiratory syndrome coronavirus 2 and host antiviral defence: Lessons from other pathogenic viruses. Emerg. Microbes Infect. 2020, 9, 558–570. [Google Scholar] [CrossRef]
- Xiong, Y.; Liu, Y.; Cao, L.; Wang, D.; Guo, M.; Jiang, A.; Guo, D.; Hu, W.; Yang, J.; Tang, Z.; et al. Transcriptomic characteristics of bronchoalveolar lavage fluid and peripheral blood mononuclear cells in COVID-19 patients. Emerg. Microbes Infect. 2020, 9, 761–770. [Google Scholar] [CrossRef] [PubMed]
- Andoniou, C.E.; Fleming, P.; Sutton, V.R.; Trapani, J.A.; Degli-Esposti, M.A. Cathepsin C limits acute viral infection independently of NK cell and CD8+ T-cell cytolytic function. Immunol. Cell Biol. 2010, 89, 540–548. [Google Scholar] [CrossRef] [PubMed]
- Rawlings, N.D.; Barrett, A.J.; Thomas, P.D.; Huang, X.; Bateman, A.; Finn, R.D. The MEROPS database of proteolytic enzymes, their substrates and inhibitors in 2017 and a comparison with peptidases in the PANTHER database. Nucleic Acids Res. 2018, 46, D624–D632. [Google Scholar] [CrossRef] [PubMed]
- Liu, T.; Luo, S.; Libby, P.; Shi, G.-P. Cathepsin L-selective inhibitors: A potentially promising treatment for COVID-19 patients. Pharmacol. Ther. 2020, 213, 107587. [Google Scholar] [CrossRef]
- Zhou, Y.; Vedantham, P.; Lu, K.; Agudelo, J.; Carrion, R., Jr.; Nunneley, J.W.; Barnard, D.; Pöhlmann, S.; McKerrow, J.H.; Renslo, A.R.; et al. Protease inhibitors targeting coronavirus and filovirus entry. Antivir. Res. 2015, 116, 76–84. [Google Scholar] [CrossRef]
- Baranov, M.; Bianchi, F.; Schirmacher, A.; van Aart, M.A.; Maassen, S.; Muntjewerff, E.M.; Dingjan, I.; ter Beest, M.; Verdoes, M.; Keyser, S.G.; et al. The Phosphoinositide Kinase PIKfyve Promotes Cathepsin-S-Mediated Major Histocompatibility Complex Class II Antigen Presentation. iScience 2018, 11, 160–177. [Google Scholar] [CrossRef]
- Riva, L.; Yuan, S.; Yin, X.; Martin-Sancho, L.; Matsunaga, N.; Pache, L.; Burgstaller-Muehlbacher, S.; De Jesus, P.D.; Teriete, P.; Hull, M.V.; et al. Discovery of SARS-CoV-2 antiviral drugs through large-scale compound repurposing. Nat. Cell Biol. 2020, 586, 113–119. [Google Scholar] [CrossRef]
- Kreutzberger, A.J.B.; Sanyal, A.; Ojha, R.; Pyle, J.D.; Vapalahti, O.; Balistreri, G.; Kirchhausen, T. Synergistic Block of SARS-CoV-2 Infection by Combined Drug Inhibition of the Host Entry Factors PIKfyve Kinase and TMPRSS2 Protease. J. Virol. 2021, 95, e0097521. [Google Scholar] [CrossRef]
- Baranov, M.V.; Bianchi, F.; van den Bogaart, G. The PIKfyve Inhibitor Apilimod: A Double-Edged Sword against COVID-19. Cells 2020, 10, 30. [Google Scholar] [CrossRef]
- Gnirß, K.; Kühl, A.; Karsten, C.; Glowacka, I.; Bertram, S.; Kaup, F.; Hofmann, H.; Pöhlmann, S. Cathepsins B and L activate Ebola but not Marburg virus glycoproteins for efficient entry into cell lines and macrophages independent of TMPRSS2 expression. Virology 2012, 424, 3–10. [Google Scholar] [CrossRef]
- Tharappel, A.M.; Samrat, S.K.; Li, Z.; Li, H. Targeting Crucial Host Factors of SARS-CoV-2. ACS Infect. Dis. 2020, 6, 2844–2865. [Google Scholar] [CrossRef]
- Björck, L.; Grubb, A.; Kjellén, L. Cystatin C, a human proteinase inhibitor, blocks replication of herpes simplex virus. J. Virol. 1990, 64, 941–943. [Google Scholar] [CrossRef]
- Xiang, R.; Yu, Z.; Wang, Y.; Wang, L.; Huo, S.; Li, Y.; Liang, R.; Hao, Q.; Ying, T.; Gao, Y.; et al. Recent advances in developing small-molecule inhibitors against SARS-CoV-2. Acta Pharm. Sin. B 2022, 12, 1591–1623. [Google Scholar] [CrossRef]
- Estoppey, D.; Lee, C.M.; Janoschke, M.; Lee, B.H.; Wan, K.F.; Dong, H.; Mathys, P.; Filipuzzi, I.; Schuhmann, T.; Riedl, R.; et al. The Natural Product Cavinafungin Selectively Interferes with Zika and Dengue Virus Replication by Inhibition of the Host Signal Peptidase. Cell Rep. 2017, 19, 451–460. [Google Scholar] [CrossRef]
- Zhang, X.; Liu, Q.; Zhang, N.; Li, Q.; Liu, Z.; Li, Y.; Gao, L.; Wang, Y.; Deng, H.; Song, D. Discovery and evolution of aloperine derivatives as novel anti-filovirus agents through targeting entry stage. Eur. J. Med. Chem. 2018, 149, 45–55. [Google Scholar] [CrossRef]
- Dana, D.; Pathak, S.K. A Review of Small Molecule Inhibitors and Functional Probes of Human Cathepsin L. Molecules 2020, 25, 698. [Google Scholar] [CrossRef]
- Mayer, A.; Guerrero, A.; Rodríguez, A.; Taglialatela-Scafati, O.; Nakamura, F.; Fusetani, N. Marine Pharmacology in 2016–2017: Marine Compounds with Antibacterial, Antidiabetic, Antifungal, Anti-Inflammatory, Antiprotozoal, Antituberculosis and Antiviral Activities; Affecting the Immune and Nervous Systems, and Other Miscellaneous Mechanisms of Action. Mar. Drugs 2021, 19, 49. [Google Scholar] [CrossRef]
- Christy, M.P.; Uekusa, Y.; Gerwick, L.; Gerwick, W.H. Natural Products with Potential to Treat RNA Virus Pathogens Including SARS-CoV-2. J. Nat. Prod. 2020, 84, 161–182. [Google Scholar] [CrossRef]
- Vidal-Albalat, A.; González, F.V. Natural Products as Cathepsin Inhibitors. Stud. Nat. Prod. Chem. 2016, 50, 179–213. [Google Scholar] [CrossRef]
- Ebert, D.H.; Wetzel, J.D.; Brumbaugh, D.E.; Chance, S.R.; Stobie, L.E.; Baer, G.S.; Dermody, T.S. Adaptation of Reovirus to Growth in the Presence of Protease Inhibitor E64 Segregates with a Mutation in the Carboxy Terminus of Viral Outer-Capsid Protein sigma3. J. Virol. 2001, 75, 3197–3206. [Google Scholar] [CrossRef]
- Pillaiyar, T.; Meenakshisundaram, S.; Manickam, M. Recent discovery and development of inhibitors targeting coronaviruses. Drug Discov. Today 2020, 25, 668–688. [Google Scholar] [CrossRef]
- Miller, B.; Friedman, A.J.; Choi, H.; Hogan, J.; McCammon, J.A.; Hook, V.; Gerwick, W.H. The Marine Cyanobacterial Metabolite Gallinamide a Is a Potent and Selective Inhibitor of Human Cathepsin L. J. Nat. Prod. 2013, 77, 92–99. [Google Scholar] [CrossRef]
- Fusetani, N.; Fujita, M.; Nakao, Y.; Matsunaga, S.; van Soest, R.W. Tokaramide A, a new cathepsin B inhibitor from the marine sponge Theonella aff. mirabilis. Bioorg. Med. Chem. Lett. 1999, 9, 3397–3402. [Google Scholar] [CrossRef]
- Nakao, Y.; Fujita, M.; Warabi, K.; Matsunaga, A.S.; Fusetani, N. Miraziridine A, a Novel Cysteine Protease Inhibitor from the Marine Sponge Theonella aff. mirabilis. J. Am. Chem. Soc. 2000, 122, 10462–10463. [Google Scholar] [CrossRef]
- Ashhurst, A.S.; Tang, A.H.; Fajtová, P.; Yoon, M.C.; Aggarwal, A.; Bedding, M.J.; Stoye, A.; Beretta, L.; Pwee, D.; Drelich, A.; et al. Potent Anti-SARS-CoV-2 Activity by the Natural Product Gallinamide A and Analogues via Inhibition of Cathepsin L. J. Med. Chem. 2022, 65, 2956–2970. [Google Scholar] [CrossRef]
- Dang, Z.; Zhu, L.; Lai, W.; Bogerd, H.; Lee, K.-H.; Huang, L.; Chen, C.-H. Aloperine and Its Derivatives as a New Class of HIV-1 Entry Inhibitors. ACS Med. Chem. Lett. 2016, 7, 240–244. [Google Scholar] [CrossRef]
- Lv, X.-Q.; Zou, L.-L.; Tan, J.-L.; Li, H.; Li, J.-R.; Liu, N.-N.; Dong, B.; Song, D.-Q.; Peng, Z.-G. Aloperine inhibits hepatitis C virus entry into cells by disturbing internalisation from endocytosis to the membrane fusion process. Eur. J. Pharmacol. 2020, 883, 173323. [Google Scholar] [CrossRef]
- Dang, Z.; Jung, K.; Zhu, L.; Lai, W.; Xie, H.; Lee, K.-H.; Huang, L.; Chen, C.-H. Identification and Synthesis of Quinolizidines with Anti-Influenza A Virus Activity. ACS Med. Chem. Lett. 2014, 5, 942–946. [Google Scholar] [CrossRef]
- Agbowuro, A.A.; Huston, W.M.; Gamble, A.B.; Tyndall, J.D.A. Proteases and protease inhibitors in infectious diseases. Med. Res. Rev. 2018, 38, 1295–1331. [Google Scholar] [CrossRef]
| Cathepsin | MW * (kDa) | Cellular Localization | Enzymatic Activity | Interacting Virus | Mechanism of Action |
|---|---|---|---|---|---|
| Serine cathepsins | |||||
| A | 54 | Endo/lysosome | Endopeptidase, Carboxypeptidase | SARS-CoV | Antigen processing downregulation [126] |
| G | 29 | Endo/lysosome Extracellular space | Endopeptidase | Respiratory syncytial virus | Activation of pattern recognition receptors and immune response hijacking [118] |
| Aspartate cathepsins | |||||
| D | 45 | Endo/lysosome Cytosol Extracellular space | Endopeptidase | Hepatitis B | Autophagy impairment [137] |
| E | 43 | Endo/lysosome | Endopeptidase | Respiratory syncytial virus | Activation of pattern recognition receptors and immune response hijacking [118] |
| Cysteine cathepsins | |||||
| B | 38 | Endo/lysosome Cytosol Nucleus Plasma membrane Extracellular space | Endopeptidase, Carboxypeptidase | Ebola | Processing of viral glycoprotein prior to fusion with the cell membrane [63,64,65] |
| Human papilloma virus type 16 | Binding, internalization and trafficking at the plasma membrane, in the endolysosome, or vesicles [67,69] | ||||
| Reoviruses | Disassembly of the viral particles in the late endosomes [70,71,72] | ||||
| SARS-CoV and SARS-CoV-2 | Activation of S protein for entry by endocytosis [74,75,80,81,85] | ||||
| Nipah | Processing viral fusion protein [88] | ||||
| Ectromelia | Immune response impairment and replication induction [121] | ||||
| Human immunodeficiency virus type 1 | Decreased antigen processing and presentation, replication [122] | ||||
| Influenza A | Impaired MHC II antigen processing [123] | ||||
| Respiratory syncytial virus | Activation of pattern recognition receptors and immune response hijacking [118] | ||||
| Noroviruses | Activation of apoptosis and replication induction [138] | ||||
| Dengue | Apoptosis activation [139] | ||||
| >Coxsackievirus B3 | Inflammasome activation, pyroptosis [140] | ||||
| C | 52 | Endo/lysosome Cytosol | Endopeptidase | Human immunodeficiency virus type 1 | Decreased antigen processing and presentation, replication [122] |
| Respiratory syncytial virus | Activation of pattern recognition receptors and immune response hijacking [118] | ||||
| Cytomegalovirus | Inhibition of viral replication [143] | ||||
| H | 37 | Endo/lysosome Nucleus | Endopeptidase, Aminopeptidase | SARS-CoV | Antigen processing downregulation [126] |
| Respiratory syncytial virus | Activation of pattern recognition receptors and immune response hijacking [118] | ||||
| K | 37 | Endo/lysosome Nucleus Extracellular space | Endopeptidase | SARS-CoV-2 | Protein S processing [85] |
| Respiratory syncytial virus | Activation of pattern recognition receptors and immune response hijacking [118] | ||||
| L | 38 | Endo/lysosome Cytosol Nucleus Plasma membrane Secretory vesicles Extracellular space | Endopeptidase | Ebola | Processing of viral glycoprotein prior to fusion with the cell membrane [63,64,65,66] |
| Human papilloma virus type 16 | Binding, internalization and trafficking at the plasma membrane, in the endolysosome, or vesicles [67,69] | ||||
| Reoviruses | Disassembly of the viral particles in the late endosomes [70,71,72] | ||||
| SARS-CoV, MERS-CoV and SARS-CoV-2 | Activation of S protein for entry by either fusion or endocytosis [73,74,75,78,79,80,81,82,83,84,85]; apoptosis activation facilitating viral dissemination [141,142] | ||||
| Hendra | Processing of the viral fusion protein [87] | ||||
| Herpes Simplex Virus -1 and -2 | Heparanase up-regulation, viral egress [89,95,102,103] | ||||
| Dengue | Heparanase up-regulation, viral egress [105,106] | ||||
| Ectromelia | Immune response escape, replication [121] | ||||
| Respiratory syncytial virus | Activation of pattern recognition receptors and immune response hijacking [118] | ||||
| S | 37 | Endo/lysosome Cytosol Nucleus Plasma membrane Extracellular space | Endopeptidase | Reoviruses | Disassembly of the viral particles in the late endosomes [71] |
| SARS-CoV-2 | Protein S processing [85] | ||||
| Ectromelia | Immune response escape, replication [121] | ||||
| Human immunodeficiency virus type 1 | Decreased antigen processing and presentation, replication [122] | ||||
| Hepatitis C | Impairment of MHC II maturation [125] | ||||
| SARS-CoV | Antigen processing downregulation [126] | ||||
| Respiratory syncytial virus | Activation of pattern recognition receptors and immune response hijacking [118] | ||||
| Dengue | Activation of apoptosis [139] | ||||
| V | 37 | Endo/lysosome Secretory vesicles Extracellular space | Endopeptidase | SARS-CoV-2 | Protein S processing [85] |
| W | 42 | Endo/lysosome Extracellular space | Endopeptidase | Influenza A | Escape from late endosomes [86] |
| Respiratory syncytial virus | Activation of pattern recognition receptors and immune response hijacking [118] | ||||
| Z | 34 | Endo/lysosome Cytosol | Endopeptidase | Human immunodeficiency virus type 1 | Decreased antigen processing and presentation, replication [122] |
| Respiratory syncytial virus | Activation of pattern recognition receptors and immune response hijacking [118] | ||||
| Target | Inhibitor | Virus(es) | Reference(s) |
|---|---|---|---|
| Cysteine cathepsins | K11777 | EBOV, Paramyxoviruses, CoVs | [146] |
| Apilimod | SARS-CoV-2 | [147,148,149] | |
| Cathepsins B and/or L | MDL 28170 | EBOV, SARS-CoV-1, SARS-CoV-2 | [148,151,152] |
| Z LVG CHN2 | HSV MERS and SARS-CoV-2 | [153] [148,154] | |
| Gallinamide A | SARS-CoV-2 | [166] | |
| Aloperine | EBOV HIV-1 HCV IAV | [156] [167] [168] [169] | |
| E-64 | Reoviruses RSV MERS and SARS-CoV-2 | [161] [118] [162] | |
| Cathepsin K | ONO 5334 | SARS-CoV-2 | [148] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Scarcella, M.; d’Angelo, D.; Ciampa, M.; Tafuri, S.; Avallone, L.; Pavone, L.M.; De Pasquale, V. The Key Role of Lysosomal Protease Cathepsins in Viral Infections. Int. J. Mol. Sci. 2022, 23, 9089. https://doi.org/10.3390/ijms23169089
Scarcella M, d’Angelo D, Ciampa M, Tafuri S, Avallone L, Pavone LM, De Pasquale V. The Key Role of Lysosomal Protease Cathepsins in Viral Infections. International Journal of Molecular Sciences. 2022; 23(16):9089. https://doi.org/10.3390/ijms23169089
Chicago/Turabian StyleScarcella, Melania, Danila d’Angelo, Mariangela Ciampa, Simona Tafuri, Luigi Avallone, Luigi Michele Pavone, and Valeria De Pasquale. 2022. "The Key Role of Lysosomal Protease Cathepsins in Viral Infections" International Journal of Molecular Sciences 23, no. 16: 9089. https://doi.org/10.3390/ijms23169089
APA StyleScarcella, M., d’Angelo, D., Ciampa, M., Tafuri, S., Avallone, L., Pavone, L. M., & De Pasquale, V. (2022). The Key Role of Lysosomal Protease Cathepsins in Viral Infections. International Journal of Molecular Sciences, 23(16), 9089. https://doi.org/10.3390/ijms23169089












