DNA Methylation Episignatures in Neurodevelopmental Disorders Associated with Large Structural Copy Number Variants: Clinical Implications
Abstract
1. Introduction
2. The Role of CNVs in Genomic Disorders
3. Clinical Identification of CNVs in Patients with NDDs
4. The Role of Epigenetics in NDDs and Subsequent Episignature Mapping
5. Current Episignature Detection in NDDs
6. The Use of Episignatures in the Diagnosis of NDDs
7. Episignature Development in CNV-Associated Genomic Disorders Provides Insight into Pathological Mechanism
8. Defined Episignatures in Other CNV-Associated Genomic Disorders Provide Rationale to Further Expand Episignature Discovery
9. Combined Detection of CNVs and DNA Methylation Episignatures in a Single Assay
10. Conclusions
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- López-Rivera, J.A.; Pérez-Palma, E.; Symonds, J.; Lindy, A.S.; McKnight, D.A.; Leu, C.; Zuberi, S.; Brunklaus, A.; Møller, R.; Lal, D. A catalogue of new incidence estimates of monogenic neurodevelopmental disorders caused by de novo variants. Brain 2020, 143, 1099–1105. [Google Scholar] [CrossRef] [PubMed]
- Institute of Medicine (US) Committee on Nervous System Disorders in Developing Countries. Neurological, Psychiatric, and Developmental Disorders: Meeting the Challenge in the Developing World; National Academies Press: Washington, DC, USA, 2001.
- Morris-Rosendahl, D.J.; Crocq, M.-A. Neurodevelopmental disorders—The history and future of a diagnostic concept. Dialogues Clin. Neurosci. 2020, 22, 65–72. [Google Scholar] [CrossRef] [PubMed]
- Parenti, I.; Rabaneda, L.G.; Schoen, H.; Novarino, G. Neurodevelopmental Disorders: From Genetics to Functional Pathways. Trends Neurosci. 2020, 43, 608–621. [Google Scholar] [CrossRef] [PubMed]
- Sheridan, E.; Wright, J.; Small, N.; Corry, P.C.; Oddie, S.; Whibley, C.; Petherick, E.S.; Malik, T.; Pawson, N.; McKinney, P.A.; et al. Risk factors for congenital anomaly in a multiethnic birth cohort: An analysis of the Born in Bradford study. Lancet 2013, 382, 1350–1359. [Google Scholar] [CrossRef]
- Pinto, D.; Delaby, E.; Merico, D.; Barbosa, M.; Merikangas, A.; Klei, L.; Thiruvahindrapuram, B.; Xu, X.; Ziman, R.; Wang, Z.; et al. Convergence of Genes and Cellular Pathways Dysregulated in Autism Spectrum Disorders. Am. J. Hum. Genet. 2014, 94, 677–694. [Google Scholar] [CrossRef]
- Miller, D.T.; Adam, M.P.; Aradhya, S.; Biesecker, L.G.; Brothman, A.R.; Carter, N.P.; Church, D.M.; Crolla, J.A.; Eichler, E.E.; Epstein, C.J.; et al. Consensus Statement: Chromosomal Microarray Is a First-Tier Clinical Diagnostic Test for Individuals with Developmental Disabilities or Congenital Anomalies. Am. J. Hum. Genet. 2010, 86, 749–764. [Google Scholar] [CrossRef]
- Silva, M.; De Leeuw, N.; Mann, K.; Schuring-Blom, H.; Morgan, S.; Giardino, D.; Rack, K.; Hastings, R. European guidelines for constitutional cytogenomic analysis. Eur. J. Hum. Genet. 2019, 27, 1–16. [Google Scholar] [CrossRef]
- Shaw-Smith, C.; Redon, R.; Rickman, L.; Rio, M.; Willatt, L.; Fiegler, H.; Firth, H.; Sanlaville, D.; Winter, R.; Colleaux, L.; et al. Microarray based comparative genomic hybridisation (array-CGH) detects submicroscopic chromosomal deletions and duplications in patients with learning disability/mental retardation and dysmorphic features. J. Med. Genet. 2004, 41, 241–248. [Google Scholar] [CrossRef]
- Vissers, L.E.; de Vries, B.B.; Osoegawa, K.; Janssen, I.M.; Feuth, T.; Choy, C.O.; Straatman, H.; van der Vliet, W.; Huys, E.H.; van Rijk, A.; et al. Array-Based Comparative Genomic Hybridization for the Genomewide Detection of Submicroscopic Chromosomal Abnormalities. Am. J. Hum. Genet. 2003, 73, 1261–1270. [Google Scholar] [CrossRef]
- Haraksingh, R.R.; Abyzov, A.; Urban, A.E. Comprehensive performance comparison of high-resolution array platforms for genome-wide Copy Number Variation (CNV) analysis in humans. BMC Genom. 2017, 18, 321. [Google Scholar] [CrossRef]
- McCarroll, S.; Kuruvilla, F.G.; Korn, J.M.; Cawley, S.; Nemesh, J.; Wysoker, A.; Shapero, M.H.; Bakker, P.I.W.D.; Maller, J.; Kirby, A.; et al. Integrated detection and population-genetic analysis of SNPs and copy number variation. Nat. Genet. 2008, 40, 1166–1174. [Google Scholar] [CrossRef] [PubMed]
- Feuk, L.; Carson, A.R.; Scherer, S. Structural variation in the human genome. Nat. Rev. Genet. 2006, 7, 85–97. [Google Scholar] [CrossRef] [PubMed]
- Levy, B.; Burnside, R.D. Are all chromosome microarrays the same? What clinicians need to know. Prenat. Diagn. 2019, 39, 157–164. [Google Scholar] [CrossRef] [PubMed]
- D’Amours, G.; Langlois, M.; Mathonnet, G.; Fetni, R.; Nizard, S.; Srour, M.; Tihy, F.; Phillips, M.S.; Michaud, J.L.; Lemyre, E. SNP arrays: Comparing diagnostic yields for four platforms in children with developmental delay. BMC Med. Genom. 2014, 7, 70. [Google Scholar] [CrossRef][Green Version]
- Zhang, Y.; Haraksingh, R.; Grubert, F.; Abyzov, A.; Gerstein, M.; Weissman, S.; Urban, A.E. Child Development and Structural Variation in the Human Genome. Child Dev. 2013, 84, 34–48. [Google Scholar] [CrossRef] [PubMed]
- Tuzun, E.; Sharp, A.J.; Bailey, J.A.; Kaul, R.; Morrison, V.A.; Pertz, L.M.; Haugen, E.; Hayden, H.S.; Albertson, D.G.; Pinkel, D.; et al. Fine-scale structural variation of the human genome. Nat. Genet. 2005, 37, 727–732. [Google Scholar] [CrossRef]
- Liu, J.; Zhou, Y.; Liu, S.; Song, X.; Yang, X.Z.; Fan, Y.; Chen, W.; Akdemir, Z.C.; Yan, Z.; Zuo, Y.; et al. The coexistence of copy number variations (CNVs) and single nucleotide polymorphisms (SNPs) at a locus can result in distorted calculations of the significance in associating SNPs to disease. Hum. Genet. 2018, 137, 553–567. [Google Scholar] [CrossRef]
- Akhtar, M.S.; Ashino, R.; Oota, H.; Ishida, H.; Niimura, Y.; Touhara, K.; Melin, A.D.; Kawamura, S. Genetic variation of olfactory receptor gene family in a Japanese population. Anthr. Sci. 2022, 211024. [Google Scholar] [CrossRef]
- Lee, J.A.; Lupski, J.R. Genomic Rearrangements and Gene Copy-Number Alterations as a Cause of Nervous System Disorders. Neuron 2006, 52, 103–121. [Google Scholar] [CrossRef]
- Cooper, G.M.; Coe, B.P.; Girirajan, S.; Rosenfeld, J.A.; Vu, T.H.; Baker, C.; Williams, C.; Stalker, H.; Hamid, R.; Hannig, V.; et al. A Copy Number Variation Morbidity Map of Developmental Delay. Nat. Genet. 2011, 43, 838–846. [Google Scholar] [CrossRef]
- Le Gouard, N.R.; Jacquinet, A.; Ruaud, L.; Deleersnyder, H.; Ageorges, F.; Gallard, J.; Lacombe, D.; Odent, S.; Mikaty, M.; Manouvrier-Hanu, S.; et al. Smith-Magenis syndrome: Clinical and behavioral characteristics in a large retrospective cohort. Clin. Genet. 2021, 99, 519–528. [Google Scholar] [CrossRef] [PubMed]
- Eichler, E.E. Recent duplication, domain accretion and the dynamic mutation of the human genome. Trends Genet. 2001, 17, 661–669. [Google Scholar] [CrossRef]
- Sharp, A.J.; Cheng, Z.; Eichler, E.E. Structural Variation of the Human Genome. Annu. Rev. Genom. Hum. Genet. 2006, 7, 407–442. [Google Scholar] [CrossRef] [PubMed]
- Liu, P.; Lacaria, M.; Zhang, F.; Withers, M.; Hastings, P.; Lupski, J.R. Frequency of Nonallelic Homologous Recombination Is Correlated with Length of Homology: Evidence that Ectopic Synapsis Precedes Ectopic Crossing-Over. Am. J. Hum. Genet. 2011, 89, 580–588. [Google Scholar] [CrossRef] [PubMed]
- Smajlagić, D.; Lavrichenko, K.; Berland, S.; Helgeland, Ø.; Knudsen, G.P.; Vaudel, M.; Haavik, J.; Knappskog, P.M.; Njølstad, P.R.; Houge, G.; et al. Population prevalence and inheritance pattern of recurrent CNVs associated with neurodevelopmental disorders in 12,252 newborns and their parents. Eur. J. Hum. Genet. 2021, 29, 205–215. [Google Scholar] [CrossRef]
- Tatton-Brown, K.; Douglas, J.; Coleman, K.; Baujat, G.; Chandler, K.; Clarke, A.; Collins, A.; Davies, S.; Faravelli, F.; Firth, H.; et al. Multiple mechanisms are implicated in the generation of 5q35 microdeletions in Sotos syndrome. J. Med. Genet. 2005, 42, 307–313. [Google Scholar] [CrossRef]
- Goldenberg, P. An Update on Common Chromosome Microdeletion and Microduplication Syndromes. Pediatr. Ann. 2018, 47, e198–e203. [Google Scholar] [CrossRef]
- Bernardini, L.; Alesi, V.; Loddo, S.; Novelli, A.; Bottillo, I.; Battaglia, A.; Digilio, M.C.; Zampino, G.; Ertel, A.; Fortina, P.; et al. High-resolution SNP arrays in mental retardation diagnostics: How much do we gain? Eur. J. Hum. Genet. 2010, 18, 178–185. [Google Scholar] [CrossRef]
- De Ligt, J.; Willemsen, M.H.; Van Bon, B.W.; Kleefstra, T.; Yntema, H.G.; Kroes, T.; Vulto-van Silfhout, A.T.; Koolen, D.A.; De Vries, P.; Gilissen, C.; et al. Diagnostic Exome Sequencing in Persons with Severe Intellectual Disability. N. Engl. J. Med. 2012, 367, 1921–1929. [Google Scholar] [CrossRef]
- Lemke, J.R.; Riesch, E.; Scheurenbrand, T.; Schubach, M.; Wilhelm, C.; Steiner, I.; Hansen, J.; Courage, C.; Gallati, S.; Bürki, S.; et al. Targeted next generation sequencing as a diagnostic tool in epileptic disorders. Epilepsia 2012, 53, 1387–1398. [Google Scholar] [CrossRef]
- Schwarze, K.; Buchanan, J.; Taylor, J.C.; Wordsworth, S. Are whole-exome and whole-genome sequencing approaches cost-effective? A systematic review of the literature. Genet. Med. 2018, 20, 1122–1130. [Google Scholar] [CrossRef] [PubMed]
- Sikkema-Raddatz, B.; Johansson, L.F.; de Boer, E.N.; Almomani, R.; Boven, L.G.; van den Berg, M.P.; van Spaendonck-Zwarts, K.Y.; van Tintelen, J.P.; Sijmons, R.H.; Jongbloed, J.D.H.; et al. Targeted Next-Generation Sequencing can Replace Sanger Sequencing in Clinical Diagnostics. Hum. Mutat. 2013, 34, 1035–1042. [Google Scholar] [CrossRef] [PubMed]
- Fraiman, Y.S.; Wojcik, M.H. The influence of social determinants of health on the genetic diagnostic odyssey: Who remains undiagnosed, why, and to what effect? Pediatr. Res. 2021, 89, 295–300. [Google Scholar] [CrossRef]
- Michaels-Igbokwe, C.; McInnes, B.; MacDonald, K.V.; Currie, G.R.; Omar, F.; Shewchuk, B.; Bernier, F.P.; Marshall, D.A. (Un)standardized testing: The diagnostic odyssey of children with rare genetic disorders in Alberta, Canada. Genet. Med. 2021, 23, 272–279. [Google Scholar] [CrossRef] [PubMed]
- Thevenon, J.; Duffourd, Y.; Masurel-Paulet, A.; Lefebvre, M.; Feillet, F.; El Chehadeh-Djebbar, S.; St-Onge, J.; Steinmetz, A.; Huet, F.; Chouchane, M.; et al. Diagnostic odyssey in severe neurodevelopmental disorders: Toward clinical whole-exome sequencing as a first-line diagnostic test. Clin. Genet. 2016, 89, 700–707. [Google Scholar] [CrossRef]
- Schenkel, L.C.; Schwartz, C.; Skinner, C.; Rodenhiser, D.I.; Ainsworth, P.J.; Pare, G.; Sadikovic, B. Clinical Validation of Fragile X Syndrome Screening by DNA Methylation Array. J. Mol. Diagn. 2016, 18, 834–841. [Google Scholar] [CrossRef]
- Coffee, B.; Ikeda, M.; Budimirovic, D.B.; Hjelm, L.N.; Kaufmann, W.E.; Warren, S.T. Mosaic FMR1 Deletion Causes Fragile X Syndrome and Can Lead to Molecular Misdiagnosis. Am. J. Med. Genet. Part A 2008, 146A, 1358–1367. [Google Scholar] [CrossRef] [PubMed]
- van Nimwegen, K.; Schieving, J.; Willemsen, M.; Veltman, J.; van der Burg, S.; van der Wilt, G.; Grutters, J. The diagnostic pathway in complex paediatric neurology: A cost analysis. Eur. J. Paediatr. Neurol. 2015, 19, 233–239. [Google Scholar] [CrossRef]
- Copeland, H.; Kivuva, E.; Firth, H.V.; Wright, C.F. Systematic assessment of outcomes following a genetic diagnosis identified through a large-scale research study into developmental disorders. Genet. Med. 2021, 23, 1058–1064. [Google Scholar] [CrossRef]
- Kleinendorst, L.; Heuvel, L.M.V.D.; Henneman, L.; Van Haelst, M.M. Who ever heard of 16p11.2 deletion syndrome? Parents’ perspectives on a susceptibility copy number variation syndrome. Eur. J. Hum. Genet. 2020, 28, 1196–1204. [Google Scholar] [CrossRef]
- Savatt, J.M.; Myers, S.M. Genetic Testing in Neurodevelopmental Disorders. Front. Pediatr. 2021, 9, 526779. [Google Scholar] [CrossRef] [PubMed]
- Levy, M.A.; McConkey, H.; Kerkhof, J.; Barat-Houari, M.; Bargiacchi, S.; Biamino, E.; Bralo, M.P.; Cappuccio, G.; Ciolfi, A.; Clarke, A.; et al. Novel diagnostic DNA methylation episignatures expand and refine the epigenetic landscapes of Mendelian disorders. Hum. Genet. Genom. Adv. 2021, 3, 100075. [Google Scholar] [CrossRef] [PubMed]
- Aref-Eshghi, E.; Kerkhof, J.; Pedro, V.P.; Barat-Houari, M.; Ruiz-Pallares, N.; Andrau, J.-C.; Lacombe, D.; Van-Gils, J.; Fergelot, P.; Dubourg, C.; et al. Evaluation of DNA Methylation Episignatures for Diagnosis and Phenotype Correlations in 42 Mendelian Neurodevelopmental Disorders. Am. J. Hum. Genet. 2020, 106, 356–370. [Google Scholar] [CrossRef]
- Sadikovic, B.; Levy, M.A.; Kerkhof, J.; Aref-Eshghi, E.; Schenkel, L.; Stuart, A.; McConkey, H.; Henneman, P.; Venema, A.; Schwartz, C.E.; et al. Clinical epigenomics: Genome-wide DNA methylation analysis for the diagnosis of Mendelian disorders. Genet. Med. 2021, 23, 1065–1074. [Google Scholar] [CrossRef] [PubMed]
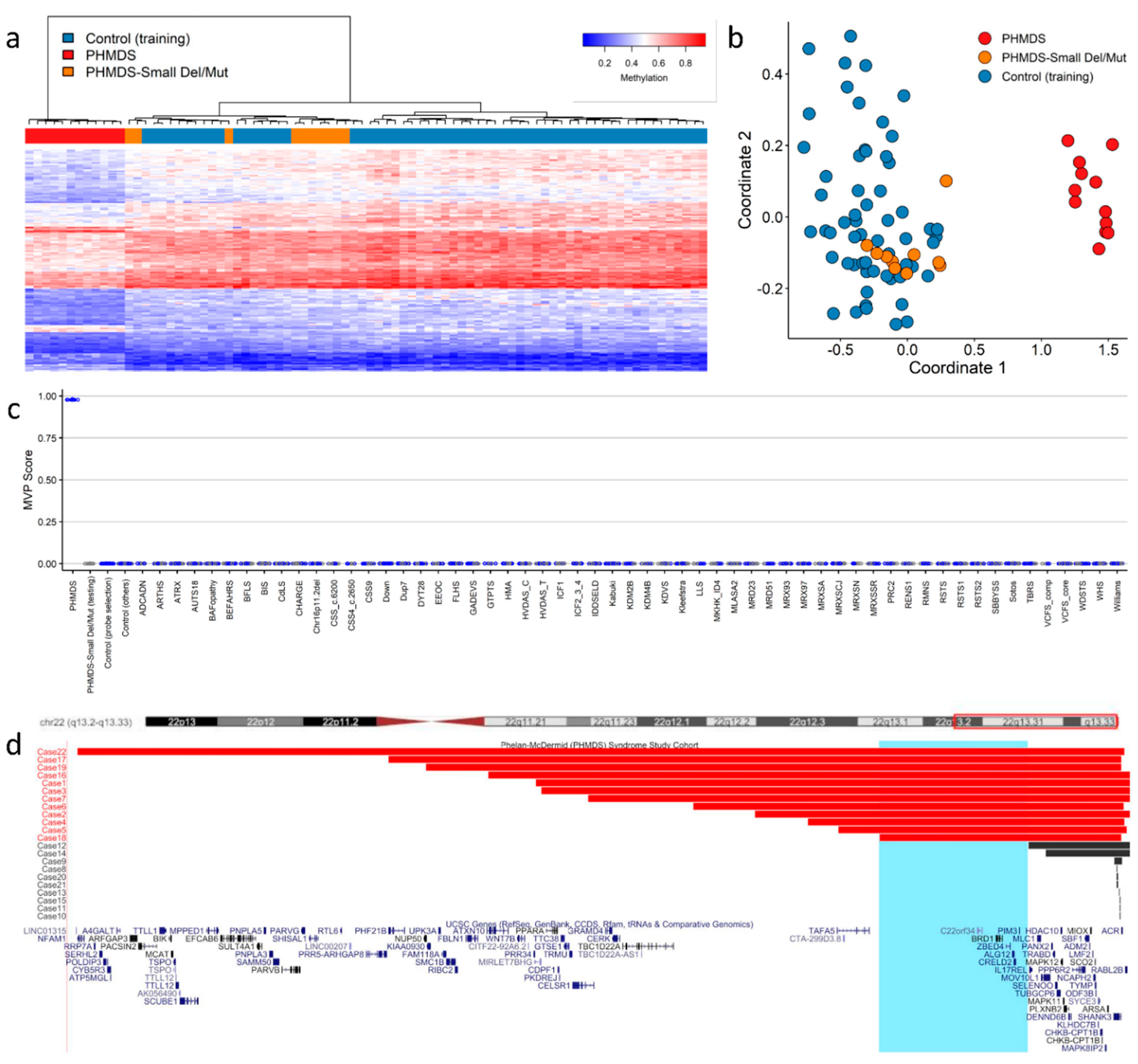
- Schenkel, L.C.; Aref-Eshghi, E.; Rooney, K.; Kerkhof, J.; Levy, M.A.; McConkey, H.; Rogers, R.C.; Phelan, K.; Sarasua, S.M.; Jain, L.; et al. DNA methylation epi-signature is associated with two molecularly and phenotypically distinct clinical subtypes of Phelan-McDermid syndrome. Clin. Epigenetics 2021, 13, 2. [Google Scholar] [CrossRef]
- Berger, S.L.; Kouzarides, T.; Shiekhattar, R.; Shilatifard, A. An operational definition of epigenetics. Genes Dev. 2009, 23, 781–783. [Google Scholar] [CrossRef] [PubMed]
- Deans, C.; Maggert, K.A. What Do You Mean, “Epigenetic”? Genetics 2015, 199, 887–896. [Google Scholar] [CrossRef]
- Gibney, E.R.; Nolan, C.M. Epigenetics and gene expression. Heredity 2010, 105, 4–13. [Google Scholar] [CrossRef]
- Li, E.; Zhang, Y. DNA Methylation in Mammals. Cold Spring Harb. Perspect. Biol. 2014, 6, a019133. [Google Scholar] [CrossRef]
- Miller, J.L.; Grant, P.A. The Role of DNA Methylation and Histone Modifications in Transcriptional Regulation in Humans. In Epigenetics: Development and Disease; Kundu, T.K., Ed.; Springer: Dordrecht, The Netherlands, 2013; pp. 289–317. [Google Scholar] [CrossRef]
- Jones, P.A. Functions of DNA methylation: Islands, start sites, gene bodies and beyond. Nat. Rev. Genet. 2012, 13, 484–492. [Google Scholar] [CrossRef]
- Aref-Eshghi, E.; Schenkel, L.C.; Lin, H.; Skinner, C.; Ainsworth, P.; Paré, G.; Rodenhiser, D.; Schwartz, C.; Sadikovic, B. The defining DNA methylation signature of Kabuki syndrome enables functional assessment of genetic variants of unknown clinical significance. Epigenetics 2017, 12, 923–933. [Google Scholar] [CrossRef] [PubMed]
- Schenkel, L.C.; Aref-Eshghi, E.; Skinner, C.; Ainsworth, P.; Lin, H.; Paré, G.; Rodenhiser, D.I.; Schwartz, C.; Sadikovic, B. Peripheral blood epi-signature of Claes-Jensen syndrome enables sensitive and specific identification of patients and healthy carriers with pathogenic mutations in KDM5C. Clin. Epigenetics 2018, 10, 21. [Google Scholar] [CrossRef] [PubMed]
- Kernohan, K.D.; Schenkel, L.C.; Huang, L.; Smith, A.; Pare, G.; Ainsworth, P.; Care4Rare Canada Consortium; Boycott, K.M.; Warman-Chardon, J.; Sadikovic, B. Identification of a methylation profile for DNMT1-associated autosomal dominant cerebellar ataxia, deafness, and narcolepsy. Clin. Epigenetics 2016, 8, 91. [Google Scholar] [CrossRef] [PubMed]
- Klein, C.J.; Bird, T.; Ertekin-Taner, N.; Lincoln, S.; Hjorth, R.; Wu, Y.; Kwok, J.; Mer, G.; Dyck, P.J.; Nicholson, G.A. DNMT1 mutation hot spot causes varied phenotypes of HSAN1 with dementia and hearing loss Background: Mutations in DNA methyltransferase 1 (DNMT1) have been identified in 2 autosomal. Neurology 2013, 80, 824–828. [Google Scholar] [CrossRef]
- Klein, C.J.; Botuyan, M.; Wu, Y.; Ward, C.J.; Nicholson, G.A.; Hammans, S.; Hojo, K.; Yamanishi, H.; Adam, R.; Wallace, D.C.; et al. Mutations in DNMT1 cause hereditary sensory neuropathy with dementia and hearing loss. Nat. Genet. 2011, 43, 595–600. [Google Scholar] [CrossRef]
- Tatton-Brown, K.; Childhood Overgrowth Consortium; Seal, S.; Ruark, E.; Harmer, J.; Ramsay, E.; Duarte, S.D.V.; Zachariou, A.; Hanks, S.; O’Brien, E.; et al. Mutations in the DNA methyltransferase gene DNMT3A cause an overgrowth syndrome with intellectual disability. Nat. Genet. 2014, 46, 385–388. [Google Scholar] [CrossRef]
- Jin, B.; Tao, Q.; Peng, J.; Soo, H.M.; Wu, W.; Ying, J.; Fields, C.R.; Delmas, A.I.; Liu, X.; Qiu, J.; et al. DNA methyltransferase 3B (DNMT3B) mutations in ICF syndrome lead to altered epigenetic modifications and aberrant expression of genes regulating development, neurogenesis and immune function. Hum. Mol. Genet. 2008, 17, 690–709. [Google Scholar] [CrossRef]
- Levy, M.A.; Beck, D.B.; Metcalfe, K.; Douzgou, S.; Sithambaram, S.; Cottrell, T.; Ansar, M.; Kerkhof, J.; Mignot, C.; Nougues, M.-C.; et al. Deficiency of TET3 leads to a genome-wide DNA hypermethylation episignature in human whole blood. NPJ Genom. Med. 2021, 6, 92. [Google Scholar] [CrossRef]
- Beck, D.B.; Petracovici, A.; He, C.; Moore, H.W.; Louie, R.J.; Ansar, M.; Douzgou, S.; Sithambaram, S.; Cottrell, T.; Santos-Cortez, R.L.P.; et al. Delineation of a Human Mendelian Disorder of the DNA Demethylation Machinery: TET3 Deficiency. Am. J. Hum. Genet. 2020, 106, 234–245. [Google Scholar] [CrossRef]
- Hood, R.L.; Schenkel, L.C.; Nikkel, S.M.; Ainsworth, P.J.; Pare, G.; Boycott, K.M.; Bulman, D.E.; Sadikovic, B. The defining DNA methylation signature of Floating-Harbor Syndrome. Sci. Rep. 2016, 6, 38803. [Google Scholar] [CrossRef]
- Schenkel, L.C.; Kernohan, K.D.; McBride, A.; Reina, D.; Hodge, A.; Ainsworth, P.J.; Rodenhiser, D.I.; Pare, G.; Bérubé, N.G.; Skinner, C.; et al. Identification of epigenetic signature associated with alpha thalassemia/mental retardation X-linked syndrome. Epigenet. Chromatin 2017, 10, 10. [Google Scholar] [CrossRef] [PubMed]
- Aref-Eshghi, E.; Bend, E.G.; Hood, R.L.; Schenkel, L.C.; Carere, D.A.; Chakrabarti, R.; Nagamani, S.C.S.; Cheung, S.W.; Campeau, P.M.; Prasad, C.; et al. BAFopathies’ DNA methylation epi-signatures demonstrate diagnostic utility and functional continuum of Coffin–Siris and Nicolaides–Baraitser syndromes. Nat. Commun. 2018, 9, 4885. [Google Scholar] [CrossRef] [PubMed]
- Wieczorek, D.; Bögershausen, N.; Beleggia, F.; Steiner-Haldenstätt, S.; Pohl, E.; Li, Y.; Milz, E.; Martin, M.; Thiele, H.; Altmüller, J.; et al. A comprehensive molecular study on Coffin–Siris and Nicolaides–Baraitser syndromes identifies a broad molecular and clinical spectrum converging on altered chromatin remodeling. Hum. Mol. Genet. 2013, 22, 5121–5135. [Google Scholar] [CrossRef] [PubMed]
- Cappuccio, G.; Sayou, C.; Tanno, P.L.; Tisserant, E.; Bruel, A.L.; Kennani, S.E.; Sá, J.; Low, K.J.; Dias, C.; Havlovicová, M.; et al. De novo SMARCA2 variants clustered outside the helicase domain cause a new recognizable syndrome with intellectual disability and blepharophimosis distinct from Nicolaides–Baraitser syndrome. Genet. Med. 2020, 22, 1838–1850. [Google Scholar] [CrossRef]
- Bend, E.G.; Aref-Eshghi, E.; Everman, D.B.; Rogers, R.C.; Cathey, S.S.; Prijoles, E.J.; Lyons, M.J.; Davis, H.; Clarkson, K.; Gripp, K.W.; et al. Gene domain-specific DNA methylation episignatures highlight distinct molecular entities of ADNP syndrome. Clin. Epigenet. 2019, 11, 64. [Google Scholar] [CrossRef]
- Breen, M.S.; Garg, P.; Tang, L.; Mendonca, D.; Levy, T.; Barbosa, M.; Arnett, A.B.; Kurtz-Nelson, E.; Agolini, E.; Battaglia, A.; et al. Episignatures Stratifying Helsmoortel-Van Der Aa Syndrome Show Modest Correlation with Phenotype. Am. J. Hum. Genet. 2020, 107, 555–563. [Google Scholar] [CrossRef]
- Tolmacheva, E.N.; Kashevarova, A.A.; Nazarenko, L.P.; Minaycheva, L.I.; Skryabin, N.A.; Lopatkina, M.E.; Nikitina, T.V.; Sazhenova, E.A.; Belyaeva, E.O.; Fonova, E.A.; et al. Delineation of Clinical Manifestations of the Inherited Xq24 Microdeletion Segregating with sXCI in Mothers: Two Novel Cases with Distinct Phenotypes Ranging from UBE2A Deficiency Syndrome to Recurrent Pregnancy Loss. Cytogenet. Genome Res. 2020, 160, 245–254. [Google Scholar] [CrossRef]
- Wojcik, F.; Dann, G.P.; Beh, L.Y.; Debelouchina, G.T.; Hofmann, R.; Muir, T.W. Functional crosstalk between histone H2B ubiquitylation and H2A modifications and variants. Nat. Commun. 2018, 9, 1394. [Google Scholar] [CrossRef]
- Selmi, C.; Feghali-Bostwick, C.A.; Lleo, A.; Lombardi, S.A.; De Santis, M.; Cavaciocchi, F.; Zammataro, L.; Mitchell, M.M.; LaSalle, J.M.; Medsger, T.; et al. X chromosome gene methylation in peripheral lymphocytes from monozygotic twins discordant for scleroderma. Clin. Exp. Immunol. 2012, 169, 253–262. [Google Scholar] [CrossRef]
- Aref-Eshghi, E.; Bend, E.G.; Colaiacovo, S.; Caudle, M.; Chakrabarti, R.; Napier, M.; Brick, L.; Brady, L.; Carere, D.A.; Levy, M.A.; et al. Diagnostic Utility of Genome-wide DNA Methylation Testing in Genetically Unsolved Individuals with Suspected Hereditary Conditions. Am. J. Hum. Genet. 2019, 104, 685–700. [Google Scholar] [CrossRef]
- Alisch, R.S.; Barwick, B.G.; Chopra, P.; Myrick, L.K.; Satten, G.A.; Conneely, K.N.; Warren, S.T. Age-associated DNA methylation in pediatric populations. Genome Res. 2012, 22, 623–632. [Google Scholar] [CrossRef] [PubMed]
- Houseman, E.A.; Accomando, W.P.; Koestler, D.C.; Christensen, B.C.; Marsit, C.J.; Nelson, H.H.; Wiencke, J.K.; Kelsey, K.T. DNA methylation arrays as surrogate measures of cell mixture distribution. BMC Bioinform. 2012, 13, 86. [Google Scholar] [CrossRef] [PubMed]
- Jaffe, A.; Murakami, P.; Lee, H.; Leek, J.; Fallin, M.D.; Feinberg, A.; Irizarry, R.A. Bump hunting to identify differentially methylated regions in epigenetic epidemiology studies. Int. J. Epidemiol. 2012, 41, 200–209. [Google Scholar] [CrossRef] [PubMed]
- Aref-Eshghi, E.; Schenkel, L.C.; Lin, H.; Skinner, C.; Ainsworth, P.; Paré, G.; Siu, V.; Rodenhiser, D.; Schwartz, C.; Sadikovic, B. Clinical Validation of a Genome-Wide DNA Methylation Assay for Molecular Diagnosis of Imprinting Disorders. J. Mol. Diagn. 2017, 19, 848–856. [Google Scholar] [CrossRef]
- Aref-Eshghi, E.; Rodenhiser, D.I.; Schenkel, L.C.; Lin, H.; Skinner, C.; Ainsworth, P.; Paré, G.; Hood, R.L.; Bulman, D.E.; Kernohan, K.D.; et al. Genomic DNA Methylation Signatures Enable Concurrent Diagnosis and Clinical Genetic Variant Classification in Neurodevelopmental Syndromes. Am. J. Hum. Genet. 2018, 102, 156–174. [Google Scholar] [CrossRef]
- Krzyzewska, I.M.; Maas, S.M.; Henneman, P.; Lip, K.V.D.; Venema, A.; Baranano, K.; Chassevent, A.; Aref-Eshghi, E.; Van Essen, A.J.; Fukuda, T.; et al. A genome-wide DNA methylation signature for SETD1B-related syndrome. Clin. Epigenet. 2019, 11, 156. [Google Scholar] [CrossRef]
- De Rubeis, S.; Siper, P.M.; Durkin, A.; Weissman, J.; Muratet, F.; Halpern, D.; Trelles, M.D.P.; Frank, Y.; Lozano, R.; Wang, A.T.; et al. Delineation of the genetic and clinical spectrum of Phelan-McDermid syndrome caused by SHANK3 point mutations. Mol. Autism 2018, 9, 31. [Google Scholar] [CrossRef]
- Sarasua, S.M.; Dwivedi, A.; Boccuto, L.; Chen, C.-F.; Sharp, J.L.; Rollins, J.D.; Collins, J.S.; Rogers, R.C.; Phelan, K.; DuPont, B.R. 22q13.2q13.32 genomic regions associated with severity of speech delay, developmental delay, and physical features in Phelan–McDermid syndrome. Genet. Med. 2014, 16, 318–328. [Google Scholar] [CrossRef]
- Wilson, H.L.; Crolla, J.A.; Walker, D.; Artifoni, L.; Dallapiccola, B.; Takano, T.; Vasudevan, P.; Huang, S.; Maloney, V.; Yobb, T.; et al. Interstitial 22q13 deletions: Genes other than SHANK3 have major effects on cognitive and language development. Eur. J. Hum. Genet. 2008, 16, 1301–1310. [Google Scholar] [CrossRef]
- Kent, W.J.; Sugnet, C.W.; Furey, T.S.; Roskin, K.M.; Pringle, T.H.; Zahler, A.M.; Haussler, D. The Human Genome Browser at UCSC. Genome Res. 2002, 12, 996–1006. [Google Scholar] [CrossRef]
- Strong, E.; Butcher, D.T.; Singhania, R.; Mervis, C.B.; Morris, C.A.; De Carvalho, D.; Weksberg, R.; Osborne, L.R. Symmetrical Dose-Dependent DNA-Methylation Profiles in Children with Deletion or Duplication of 7q11.23. Am. J. Hum. Genet. 2015, 97, 216–227. [Google Scholar] [CrossRef] [PubMed]
- Siu, M.T.; Butcher, D.T.; Turinsky, A.L.; Cytrynbaum, C.; Stavropoulos, D.J.; Walker, S.; Caluseriu, O.; Carter, M.; Lou, Y.; Nicolson, R.; et al. Functional DNA methylation signatures for autism spectrum disorder genomic risk loci: 16p11.2 deletions and CHD8 variants. Clin. Epigenetics 2019, 11, 103. [Google Scholar] [CrossRef] [PubMed]
- Rooney, K.; Levy, M.A.; Haghshenas, S.; Kerkhof, J.; Rogaia, D.; Tedesco, M.G.; Imperatore, V.; Mencarelli, A.; Squeo, G.M.; Di Venere, E.; et al. Identification of a DNA Methylation Episignature in the 22q11.2 Deletion Syndrome. Int. J. Mol. Sci. 2021, 22, 8611. [Google Scholar] [CrossRef] [PubMed]
- Van Gils, J.; Magdinier, F.; Fergelot, P.; Lacombe, D. Rubinstein-Taybi Syndrome: A Model of Epigenetic Disorder. Genes 2021, 12, 968. [Google Scholar] [CrossRef] [PubMed]
- Choufani, S.; Cytrynbaum, C.; Chung, B.H.Y.; Turinsky, A.L.; Grafodatskaya, D.; Chen, Y.A.; Cohen, A.S.A.; Dupuis, L.; Butcher, D.T.; Siu, M.T.; et al. NSD1 mutations generate a genome-wide DNA methylation signature. Nat. Commun. 2015, 6, 10207. [Google Scholar] [CrossRef]
- Singh, H.R.; Nardozza, A.P.; Möller, I.R.; Knobloch, G.; Kistemaker, H.A.V.; Hassler, M.; Harrer, N.; Blessing, C.; Eustermann, S.; Kotthoff, C.; et al. A Poly-ADP-Ribose Trigger Releases the Auto-Inhibition of a Chromatin Remodeling Oncogene. Mol. Cell 2017, 68, 860–871. [Google Scholar] [CrossRef]
- Cho, S.; Kim, H.-S.; Zeiger, M.A.; Umbricht, C.B.; Cope, L.M. Measuring DNA Copy Number Variation Using High-Density Methylation Microarrays. J. Comput. Biol. 2019, 26, 295–304. [Google Scholar] [CrossRef]
- Feber, A.; Guilhamon, P.; Lechner, M.; Fenton, T.; Wilson, G.A.; Thirlwell, C.; Morris, T.J.; Flanagan, A.M.; Teschendorff, A.E.; Kelly, J.D.; et al. Using high-density DNA methylation arrays to profile copy number alterations. Genome Biol. 2014, 15, R30. [Google Scholar] [CrossRef]
- Tian, Y.; Morris, T.J.; Webster, A.P.; Yang, Z.; Beck, S.; Feber, A.; Teschendorff, A.E. ChAMP: Updated methylation analysis pipeline for Illumina BeadChips. Bioinformatics 2017, 33, 3982–3984. [Google Scholar] [CrossRef]
- Morris, T.J.; Butcher, L.M.; Feber, A.; Teschendorff, A.E.; Chakravarthy, A.R.; Wojdacz, T.K.; Beck, S. ChAMP: 450k Chip Analysis Methylation Pipeline. Bioinformatics 2014, 30, 428–430. [Google Scholar] [CrossRef]
- Papillon-Cavanagh, S.; Fortin, J.-P.; De Jay, N. CopyNumber 450k: An R Package for CNV Inference Using Illumina 450k DNA Methylation Assay. 2013. Available online: http://rdrr.io/github/spapillon/CopyNumber450k/ (accessed on 15 May 2022).
- Montano, C.; Britton, J.F.; Harris, J.R.; Kerkhof, J.; Barnes, B.T.; Lee, J.A.; Sadikovic, B.; Sobreira, N.; Fahrner, J.A. Genome-wide DNA methylation profiling confirms a case of low-level mosaic Kabuki syndrome 1. Am. J. Med. Genet. Part A 2022, 188, 2217–2225. [Google Scholar] [CrossRef] [PubMed]
| Syndrome | Episignature Abbreviation | Underlying Gene(s) or Region | OMIM |
|---|---|---|---|
| Alpha-thalassemia mental retardation syndrome | ATRX | ATRX | 301040 |
| Angelman syndrome | Angelman | UBE3A | 105830 |
| Arboleda–Tham syndrome | ARTHS | KAT6A | 616268 |
| Autism, susceptibility to, 18 | AUTS18 | CHD8 | 615032 |
| Beck–Fahrner syndrome | BEFAHRS | TET3 | 618798 |
| Beckwith–Wiedemann syndrome | BWS | Chr11p15 (ICR1, KCNQ1OT1, CDKN1C) | 130650 |
| Blepharophimosis intellectual disability SMARCA2 syndrome | BIS | SMARCA2 | 619293 |
| Börjeson–Forssman–Lehmann syndrome | BFLS | PHF6 | 301900 |
| Cerebellar ataxia, deafness, and narcolepsy, autosomal dominant | ADCADN | DNMT1 | 604121 |
| CHARGE syndrome | CHARGE | CHD7 | 214800 |
| Chr16p11.2 deletion syndrome | Chr16p11.2del | Chr16p11.2 deletion | 611913 |
| Coffin–Siris syndrome-1, 2 (CSS1,2) | CSS_c.6200 | ARID1A; ARID1B | 135900; 614607 |
| Coffin–Siris 1–4 (CSS1–4) and Nicolaides–Baraitser syndrome (NCBRS) | BAFopathy | ARID1B; ARID1A; SMARCB1; SMARCA4; SMARCA2 | 135900; 614607; 614608; 614609; 601358 |
| Coffin–Siris syndrome-4 (CSS4) | CSS_c.2656 | SMARCA4 | 614609 |
| Coffin–Siris syndrome-9 (CSS9) | CSS9 | SOX11 | 615866 |
| Cohen–Gibson syndrome; Weaver syndrome | PRC2 | EED; EZH2 | 617561; 277590 |
| Cornelia de Lange syndromes 1–4 | CdLS | NIPBL; SMC1A; SMC3; RAD21 | 122470; 300590; 610759; 614701 |
| Down syndrome | Down | Chr21 trisomy | 190685 |
| Dystonia-28, childhood onset | DYT28 | KMT2B | 617284 |
| Epileptic encephalopathy, childhood onset | EEOC | CHD2 | 615369 |
| Floating-Harbour syndrome | FLHS | SRCAP | 136140 |
| Fragile X syndrome | FXS | FMR1 | 300624 |
| Gabriele de Vries syndrome | GADEVS | YY1 | 617557 |
| Genitopatellar syndrome (see also Ohdo syndrome, SBBYSS variant) | GTPTS | KAT6B | 606170 |
| Helsmoortel–Van der Aa syndrome (ADNP syndrome (Central)) | HVDAS_C | ADNP | 615873 |
| Helsmoortel–Van der Aa syndrome (ADNP syndrome (Terminal)) | HVDAS_T | ADNP | 615873 |
| Hunter–McAlpine craniosynostosis syndrome | HMA | Chr5q35-qter duplication | 601379 |
| Immunodeficiency, centromeric instability, facial anomalies syndrome 1 (ICF1) | ICF_1 | DNMT3B | 242860 |
| Immunodeficiency, centromeric instability, facial anomalies syndrome 2,3,4 (ICF2,3,4) | ICF_2_3_4 | ZBTB24; CDCA7; HELLS | 614069; 616910; 616911 |
| Intellectual developmental disorder-65 | KDM4B | KDM4B | 619320 |
| Intellectual developmental disorder with seizures and language delay | IDDSELD | SETD1B | 619000 |
| Intellectual developmental disorder, X-linked 93 | MRX93 | BRWD3 | 300659 |
| Intellectual developmental disorder, X-linked 97 | MRX97 | ZNF711 | 300803 |
| Intellectual developmental disorder, X-linked, Snyder–Robinson type | MRXSSR | SMS | 309583 |
| Intellectual developmental disorder, X-linked, syndromic, Armfield type | MRXSA | FAM50A | 300261 |
| Intellectual developmental disorder, X-linked, syndromic, Claes-Jensen type | MRXSCJ | KDM5C | 300534 |
| Intellectual developmental disorder, X-linked syndromic, Nascimento-type | MRXSN | UBE2A | 300860 |
| Kabuki syndromes 1, 2 | Kabuki | KMT2D; KDM6A | 147920; 300867 |
| Kagami–Ogatta syndrome | KOS | Chr14q32 | 608149 |
| KDM2B-related syndrome | KDM2B | KDM2B | unofficial |
| Kleefstra syndrome 1 | Kleefstra | EHMT1 | 610253 |
| Koolen de Vries syndrome | KDVS | KANSL1 | 610443 |
| Luscan–Lumish syndrome | LLS | SETD2 | 616831 |
| Menke–Hennekam syndrome-1, 2 | MKHK_ID4 | CREBBP; EP300 | 618332; 618333 |
| Mental retardation, autosomal dominant 23 | MRD23 | SETD5 | 615761 |
| Mental retardation, autosomal dominant 51 | MRD51 | KMT5B | 617788 |
| Mental retardation, FRA12A type | DIP2B | DIP2B | 136630 |
| Myopathy, lactic acidosis, and sideroblastic anemia-2 | MLASA2 | YARS2 | 613561 |
| Ohdo syndrome, SBBYSS variant | SBBYSS | KAT6B | 603736 |
| Phelan–McDermid syndrome | PHMDS | Chr22q13.3 deletion | 606232 |
| Prader–Willi syndrome | PWS | Chr15q11 (SNRPN, NDN) | 176270 |
| Rahman syndrome | RMNS | HIST1H1E | 617537 |
| Renpenning syndrome | RENS1 | PQBP1 | 309500 |
| Rubinstein–Taybi syndrome 1 | RSTS1 | CREBBP | 180849 |
| Rubinstein–Taybi syndrome-1, 2 | RSTS | CREBBP; EP300 | 180849; 613684 |
| Rubinstein–Taybi syndrome-2 | RSTS2 | EP300 | 613684 |
| Silver–Russell syndrome 1 | SRS1 | Chr11p15.5 | 180860 |
| Silver–Russell syndrome 2 | SRS2 | Chr7p11.2 | 618905 |
| Sotos syndrome 1 | Sotos | NSD1 | 117550 |
| Tatton–Brown–Rahman syndrome | TBRS | DNMT3A | 615879 |
| Temple syndrome | Temple | Chr14q32 | 616222 |
| Velocardiofacial syndrome | VCFS | Chr22q11.2 deletion | 192430 |
| Wiedemann–Steiner syndrome | WDSTS | KMT2A | 605130 |
| Williams–Beuren deletion syndrome (Chr7q11.23 deletion syndrome) | Williams | Chr7q11.23 deletion | 194050 |
| Williams–Beuren duplication syndrome (Chr7q11.23 duplication syndrome) | Dup7 | Chr7q11.23 duplication | 609757 |
| Wolf–Hirschhorn syndrome | WHS | Chr4p16.13 deletion | 194190 |
| Syndrome | Chromosome Region | Candidate Gene | Genes in Region with Epigenetic Function |
|---|---|---|---|
| 1p36 Deletion/Duplication | 1p36 | - | ICMT, CHD5, TP73, PMRD16, SKI, NOC2L |
| 1q21.1 Deletion/Duplication | 1q21.1 | - | CHD1L |
| 1q43q44 Deletion | 1q43q44 | - | HNRNPU, DESI2, ZBTB18, AKT3 |
| 2q11.2 Deletion/Duplication | 2q11.2 | - | KANSL3, ARID5A |
| 2q13 Deletion/Duplication | 2q13 | - | MIR4435-2HG |
| 2q37 Deletion | 2q37 | - | HDAC4, D2HGDH, ING5, HDLBP, PASK |
| 3q29 Deletion/Duplication | 3q29 | - | PAK2, RNF168 |
| 4p16.3 Deletion (Wolf–Hirschhorn)/4p16.3 Duplication | 4p16.3 | NSD2 | NSD2, CTBP1, SLBP, CTBP1, PCGF3 |
| 5p15 Deletion (Cri du Chat)/5p15 Duplication | 5p15 | - | ATPSCKMT, MTRR, NSUN2, LPCAT1, BRD9 |
| 5q35 Deletion (Sotos)/5q35 Duplication (Hunter–McAlpine) | 5q35 | NSD1 | NSD1, UIMC1 |
| 7q11.23 Deletion (Williams–Beuren)/7q11.23 Duplication | 7q11.23 | - | METTL27, BUD23, BCL7B, BAZ1B |
| 8p23.1 Deletion/Duplication | 8p23.1 | - | TNKS |
| 9q34 Deletion (Kleefstra)/9q34 Duplication | 9q34 | EHMT1 | EHMT1 |
| 10q22.3q23.2 Deletion/Duplication | 10q22.3q23.2 | - | WAPL, DYDC1, MAT1A |
| 11p11.2 Deletion (Potocki–Shaffer)/11p11.2 Duplication | 11p11.2 | - | PHF21A, CD82, ALKBH3 |
| 11q13.2q13.4 Deletion | 11q13.2q13.4 | - | KMT5B |
| 15q11.2 Deletion (non-imprinting region) | 15q11.2 | - | - |
| 15q11q13 Deletion (Prader–Willi/Angelman)/15q11q13 Duplication | 15q11q13 | - | HERC2 |
| 15q13.3 Deletion/Duplication | 15q13.3 | - | OTUD7A, KLF13 |
| 15q24 (BP0-BP1) Deletion/Duplication | 15q24 | - | - |
| 15q24 (BP2-BP3) Deletion | 15q24 | - | SIN3A, COMMD4 |
| 15q25.2 Deletion | 15q25.2 | - | HDGFL3, BNC1 |
| 16p13.3 Deletion (Rubinstein–Taybi)/16p13.3 Duplication | 16p13.3 | CREBBP | CREBBP |
| 16p13.11 Deletion/16p13.11 Duplication | 16p13.11 | - | NDE1 |
| 16p11.2 Distal Deletion/Duplication | 16p11.2 | - | SH2B1 |
| 16p11.2 Deletion/Duplication | 16p11.2 | - | PPP4C, HIRIP3, PAGR1, INO80E |
| 17p13.3 Deletion (Miller–Dieker)/17p13.3 Duplication | 17p13.3 | - | HIC1, SMYD4, MYO1C |
| 17p11.2 Deletion (Smith–Magenis)/17p11.2 Duplication (Potocki–Lupski) | 17p11.2 | RAI1 | ALKBH5, RAI1, PEMT |
| 17q11.2 Deletion/Duplication | 17q11.2 | - | SUZ12 |
| 17q12 Deletion/Duplication | 17q12 | - | HNF1B, TADA2A, AATF, PIGW |
| 17q21.31 Deletion (Koolen–de Vries)/17q21.31 Duplication | 17q21.31 | KANSL1 | KANSL1 |
| 22q11.2 Tetrasomy/Triplication (Cat eye syndrome) | 22q11.2 | - | CECR2, ADA2 |
| 22q11.2 Deletion (DiGeorge/Velocardiofacial)/22q11.2 Duplication | 22q11.2 | - | THAP7, TRMT2A, COMT, HIRA |
| 22q11.2 recurrent region distal type I (D-E/F) Deletion/Duplication | 22q11.2 | - | TOP3B, PPM1F |
| 22q13.3 Deletion (Phelan–McDermid) | 22q13.3 | SHANK3 | BRD1 |
| Xp11.22 Duplication (MRX17) | Xp11.22 | - | HUWE1, HSD17B10, SMC1A |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rooney, K.; Sadikovic, B. DNA Methylation Episignatures in Neurodevelopmental Disorders Associated with Large Structural Copy Number Variants: Clinical Implications. Int. J. Mol. Sci. 2022, 23, 7862. https://doi.org/10.3390/ijms23147862
Rooney K, Sadikovic B. DNA Methylation Episignatures in Neurodevelopmental Disorders Associated with Large Structural Copy Number Variants: Clinical Implications. International Journal of Molecular Sciences. 2022; 23(14):7862. https://doi.org/10.3390/ijms23147862
Chicago/Turabian StyleRooney, Kathleen, and Bekim Sadikovic. 2022. "DNA Methylation Episignatures in Neurodevelopmental Disorders Associated with Large Structural Copy Number Variants: Clinical Implications" International Journal of Molecular Sciences 23, no. 14: 7862. https://doi.org/10.3390/ijms23147862
APA StyleRooney, K., & Sadikovic, B. (2022). DNA Methylation Episignatures in Neurodevelopmental Disorders Associated with Large Structural Copy Number Variants: Clinical Implications. International Journal of Molecular Sciences, 23(14), 7862. https://doi.org/10.3390/ijms23147862






