Abstract
Secondary lymphedema is a common complication of lymph node dissection or radiation therapy for cancer treatment. Conventional therapies such as compression sleeve therapy, complete decongestive physiotherapy, and surgical therapies decrease edema; however, they are not curative because they cannot modulate the pathophysiology of lymphedema. Recent advances reveal that the activation and accumulation of CD4+ T cells are key in the development of lymphedema. Based on this pathophysiology, the efficacy of pharmacotherapy (tacrolimus, anti-IL-4/IL-13 antibody, or fingolimod) and cell-based therapy for lymphedema has been demonstrated in animal models and pilot studies. In addition, mesenchymal stem/stromal cells (MSCs) have attracted attention as candidates for cell-based lymphedema therapy because they improve symptoms and decrease edema volume in the long term with no serious adverse effects in pilot studies. Furthermore, MSC transplantation promotes functional lymphatic regeneration and improves the microenvironment in animal models. In this review, we focus on inflammatory cells involved in the pathogenesis of lymphedema and discuss the efficacy and challenges of pharmacotherapy and cell-based therapies for lymphedema.
1. Introduction
Lymphedema is caused by a dysfunction of the lymphatic system, resulting in localized interstitial fluid retention and tissue swelling; it is classified as primary or secondary. Primary lymphedema develops due to inherited hypoplasia/dysplasia or dysfunction of lymphatic vessels because of some intrinsic factors such as genetic mutations in the signaling pathway for vascular endothelial growth factor C (VEGF-C), while secondary lymphedema is caused by a dysfunction of the lymphatic vascular system due to trauma or parasitic infection [1,2,3]. Although the incidence of secondary lymphedema has been declining due to advances in surgery, this iatrogenic disorder has a strong negative impact on physical and mental quality of life (QOL) [4]. Additionally, radiation therapy (RT) increases the risk of lymphedema in the upper and lower limbs; for instance, in breast cancer patients, the risk of lymphedema is five times higher with postoperative RT than with axillary lymph node dissection alone [5]. Patients with lymphedema typically present with symptoms such as altered mechanical properties and sensitivity of the skin, increased susceptibility to systemic and local infections, decreased function of the affected upper or lower limb, and chronic pain and discomfort [3,6]. In addition, patients may have problems with body image and social acceptability and exhibit low self-esteem [6]. The protein-rich fluid accumulated in the interstitial space induces the migration of CD4+ T-helper (Th) cells, low-grade inflammation, remodeling of extracellular matrix, hyperkeratosis, adipose deposition, and fibrosis [6,7,8,9,10,11]. These changes in the edematous limb exacerbate lymphatic dysfunction, resulting in clinical manifestations of lymphedema.
No curative therapy for lymphedema has been established so far. While conservative therapies (such as manual lymphatic drainage, complete decongestive physiotherapy, compression sleeve therapy, exercise, and weight reduction) decrease edema temporarily, they cannot modulate the pathophysiology of lymphedema. Therefore, it is difficult to maintain their therapeutic efficacy over a lifetime [12,13,14,15,16,17]. Surgical interventions such as lymphovenous anastomosis/bypass or vascularized lymph node transfer (VLNT) are effective in early-stage lymphedema; however, they are ineffective in chronic lymphedema with fibrosis due to lymphatic dysfunction in the edematous region [18,19,20,21,22]. Recently, pharmacotherapy and cell-based therapy have been developed to treat lymphedema by promoting lymphangiogenesis, improving lymphatic function, and suppressing fibrosis and inflammatory responses. Several studies focus on the migration and accumulation of CD4+ T cells in the edematous region as a new target to treat lymphedema [23,24,25,26,27,28]. Mesenchymal stem/stromal cells (MSCs) exert anti-inflammatory, anti-fibrosis, antioxidant stress, and immunomodulatory effects and are hence used in studies to establish cell-based therapy to treat wounds [29], inflammatory bowel diseases [30], diabetes mellitus [31], psoriasis [32,33], and graft-versus-host disease [34]; they are useful since they promote lymphangiogenesis in lymphedema animal models [35,36,37,38,39,40,41,42,43,44,45]. In this review, we focused on the inflammatory cells involved in the pathogenesis of lymphedema and discuss the efficacy and challenges of pharmacotherapy and cell-based therapies for lymphedema.
2. Pathophysiology of Secondary Lymphedema
In most regions of the body, lymph flows against a hydrostatic pressure gradient created by extrinsic and intrinsic pump forces arising from the surrounding skeletal muscle and/or lymphatic collecting vessel network [46]. In lymphedema, fluid stasis is caused by lymphatic pump dysfunction due to contractile dysfunction, chronic inflammation, fibrosis, abnormal lymphangiogenesis, barrier dysfunction, or valve defects [46,47]. The protein-rich fluid that accumulates triggers an inflammatory response and exacerbates lymphedema. Although details of the mechanisms remain unclear, the activation of dendritic cells (DCs) and subsequent activation of CD4+ T cells, especially Th2 cell maturation, have been hypothesized as key factors in the inflammatory response (Figure 1) [11,48].
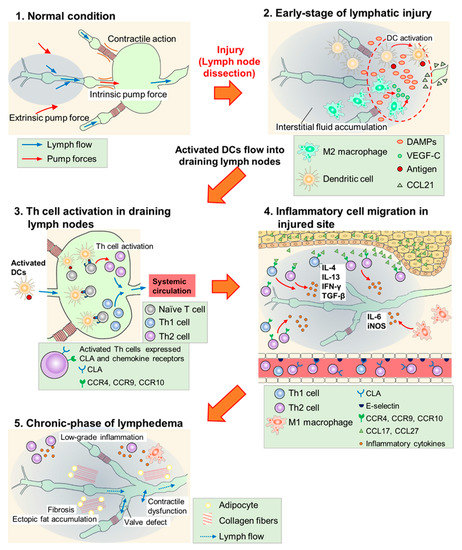
Figure 1.
Scheme of lymphedema development after lymph node dissection. (1) In normal conditions, lymph flow is generated due to intrinsic pump force by a lymphatic collecting vessel network and extrinsic pump force by surrounding skeletal muscles. (2) In the early phase of lymphatic injury, damage-associated molecular patterns (DAMPs) are released from injured cells and these molecules promote lymphangiogenesis. M2 macrophages secrete vascular endothelial growth factor C (VEGF-C) and serve as lymphatic endothelial cell (LEC) progenitors. Dendritic cells (DCs) are activated at the injured site, and invade into lymphatic vessels along the concentration gradient of the C–C chemokine ligand (CCL) 21 secreted by LECs. (3) Activated DCs flow into draining lymph nodes and activate helper T (Th) cells. Expressions of cutaneous leukocyte antigen (CLA), C–C chemokine receptor (CCR) 4, CCR9, and CCR10 are increased at the surface of activated Th cells. These cells enter systemic circulation. (4) Activated Th cells, guided by adhesion molecules and CCLs, infiltrate the injured site and secrete inflammatory cytokines. M1 macrophages also accumulate at the injured site and cause inflammatory responses. (5) Low-grade inflammatory responses, fibrosis, adipose deposition, and unfunctional lymphangiogenesis (valve defect and contractile dysfunction) occur in the chronic phase of lymphedema. These responses impair lymphatic function and exacerbate lymphedema.
In the early phase (~6 weeks) of lymphatic injury, endogenous danger signals such as high mobility group box 1 (HMGB1) and heat-shock protein 70 are expressed in endothelial cells, adipocytes, and other stromal cells at the injury site [11,26]. These proteins promote lymphangiogenesis via toll-like receptor signaling and the blockade of HMGB1 activity with glycyrrhizin inhibited inflammatory lymphangiogenesis in the mouse tail lymphedema model [11,26,49,50]. Furthermore, macrophages are recruited, and they accumulate in the lymphedematous region, especially in the early phase [51,52], while M2 macrophages secrete VEGF-C to promote superficial lymphangiogenesis [53]. Shimizu et al. reported that bone marrow-derived M2 macrophages may serve as lymphatic endothelial cell (LEC)-progenitors after adipose-derived regenerative cell (ADRC) treatment in mouse tail lymphedema models [38]. Therefore, innate immune responses may promote lymphangiogenesis and suppress the development of lymphedema in the early phase of lymphatic injury.
In this early phase, DCs accumulate in the injured skin and activate acquired immunity [25]. The expression of C–C chemokine receptor (CCR) type 7 increases on the surface of activated DCs, which migrate according to the concentration gradient of C-C chemokine ligand (CCL) type 21 secreted by LECs. Furthermore, after reaching the lymphatic vessels, activated DCs invade them using intercellular adhesion molecule 1 and/or vascular cell adhesion molecule 1 and flow into the draining lymph nodes [54,55,56,57,58]. In lymph nodes, naïve CD4+ T cells are activated by DCs, and increase the expression of cutaneous leukocyte antigen (CLA), CCR4, CCR9, and CCR10. Furthermore, after entering the bloodstream, activated CD4+ T cells infiltrate the edematous region using adhesion molecules such as E-selectin (a CLA ligand) and migrate toward chemokine ligands for CCR4 (CCL17) and CCR 10 (CCL27). The expression of these adhesion molecules and chemokines increases in the vasculature and keratinocytes of lymphedematous tissue, respectively [25,59,60,61,62,63]. Subsequently, inflammatory cytokines such as interferon (IFN)-γ, interleukin (IL)-4, IL-13, and transforming growth factor (TGF)-β (secreted from the activated CD4+ T cells) promote infiltration of the inflammatory cells, exacerbate fibrosis by collagen deposition, and directly inhibit lymphangiogenesis by suppressing the proliferation, differentiation, and migration of LECs [10,24,64,65,66,67,68,69,70]. Therefore, the activation of CD4+ T cells through antigen presentation by DCs is the key process in the development and exacerbation of lymphedema. This hypothesis is supported by studies using the mouse tail lymphedema models, in which CD4 knockout mice were less likely to develop lymphedema [25] and the depletion of regulatory T cells (Tregs) exacerbated lymphedema [23].
M1 macrophages also infiltrate the lymphedematous region and exacerbate lymphedema by inducing adipose deposition and chronic inflammation via IL-6 [71,72]. In addition, M1 macrophages strongly express inducible nitric oxide synthase (iNOS) and disturb nitric oxide homeostasis maintained by endothelial nitric oxide synthase (eNOS), resulting in attenuated lymphatic vessel pumping [25,73]. These reports suggest that the innate immune system, especially M1 macrophages, is involved in aggravating lymphedema as an inflammatory reaction in the chronic phase.
3. Pharmacotherapy for Lymphedema
Doxycycline, ketoprofen, ubenimex, selenium, synbiotic supplement, tacrolimus, anti-IL-4/IL-13 antibody, fingolimod, and TGF-β inhibitors have been studied for their suppression of inflammatory and oxidative stress. The reported pharmacological mechanisms of these agents are summarized in Figure 2.
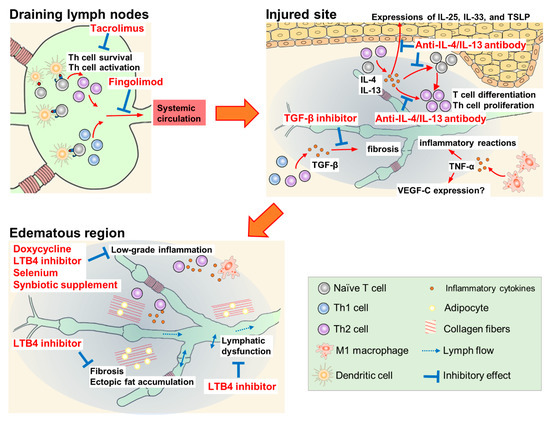
Figure 2.
Pharmacological mechanisms of therapeutic agents for lymphedema.
3.1. Doxycycline
Doxycycline, a tetracycline antibiotic, is an anti-Wolbachia drug used for filarial lymphedema. Mand et al. reported that a 6-week course of doxycycline at 200 mg/day improved mild to moderate lymphedema for two years, independent of ongoing filarial infection [74]. The efficacy of doxycycline is probably due to its non-antibiotic effects such as the direct inhibition of inflammation and angiogenesis [75].
3.2. Leukotriene B4 Inhibitors (Ketoprofen, Ubenimex)
Ketoprofen is a non-steroidal anti-inflammatory drug. The efficacy of ketoprofen has been demonstrated in a mouse tail lymphedema model and patients with lymphedema. In a mouse lymphedema model, the subcutaneous injection of ketoprofen decreased tail volume and suppressed histological changes such as epidermal thickening and neutrophil infiltration, while increasing the expression of tumor necrosis factor-α (TNF-α). In contrast, pegsunercept, a modified soluble form of TNF-α receptor R1, increased tail volume, histologically exacerbated the disease, and reduced TNF-α expression. The expression of VEGF-C in this model showed a correlation with TNF-α expression, suggesting that ketoprofen could induce TNF-α-dependent VEGF-C expression followed by lymphangiogenesis [76]. In a clinical study, patients with lymphedema received 75 mg oral ketoprofen three times daily for four months [77]. This treatment significantly improved the histopathology scores (dermal thickness, collagen thickness, intercellular mucin deposits, and perivascular inflammation); however, the volume of the limbs and content of the extracellular fluid were not affected. The mechanism of action of ketoprofen in lymphedema is the inhibition of 5-lipoxygenase activity, which produces leukotriene B4 (LTB4), rather than the inhibition of cyclooxygenase activity [77,78]. In a mouse tail lymphedema model, the intraperitoneal injection of ubenimex (2 mg/kg), a leukotriene A4 hydrolase inhibitor, improved lymphatic collecting vessel pumping, but did not affect the tail volume and leukocyte population in draining lymph nodes [79]. However, the long-term administration of ketoprofen may be inappropriate because of side effects such as acute kidney injury and gastric ulcer due to the non-selective inhibition of physiological cyclooxygenase activity. In contrast, ubenimex inhibits the production of LTB4 selectively. Therefore, ubenimex may be more suitable than ketoprofen for long-term treatment.
3.3. Selenium
The oral and intravenous administration of sodium selenite is effective in the treatment of lymphedema associated with breast cancer and head and neck cancer. In these patients, selenium decreased edema volume and improved the clinical stage of lymphedema. The antioxidant properties of selenium contribute to its efficacy in lymphedema; however, the experimental evidence is unclear [80,81,82]. In a recent study, the intravenous administration of sodium selenite improved lymphoedema and elevated the serum levels of corticosterone, LTB4 dimethylamide (endogenous LTB4 antagonist), and prostaglandin E3 in breast cancer-related lymphedema patients [83]. Elevated levels of these anti-inflammatory substances may be a factor in the therapeutic efficacy of selenium.
3.4. Synbiotic Supplements
Synbiotic supplements, dietary supplements combining probiotics and prebiotics, reduce inflammatory markers such as C-reactive protein (CRP) and TNF-α [84]. In overweight and obese patients with breast cancer-related lymphedema, a 10-week combination of low-calorie diet and synbiotic supplementation resulted in significant reductions in edema volume, serum leptin, and serum inflammatory marker levels (high-sensitivity CRP, IL-1β and TNF-α). However, after adjusting for baseline edema volume, inflammatory marker levels, and body mass index, only serum leptin and TNF-α levels were found to be significantly lower in the synbiotic supplementation group than in the low-calorie diet and placebo capsule group [85]. Although the same research group has reported antioxidant effects and improvement in QOL score with the same dietary combination, the efficacy of synbiotic supplementation for lymphedema has not yet been determined [86,87].
3.5. CD4+ T Cell Suppressants (Tacrolimus, Anti-IL-4/IL-13 Antibodies, Fingolimod)
Treatment with tacrolimus ointment and anti-IL-4/IL-13 antibodies has been shown to suppress the activation and differentiation of CD4+ T cells [24,27,28]. Tacrolimus ointment is used to treat cutaneous inflammatory diseases such as atopic dermatitis. In CD4+ T cells, tacrolimus binds to FK-506-binding protein 12, and the complex inhibits the phosphatase activity of calcineurin, thereby reducing the transcription of IL-2 [88]. CD4+ T cells cannot survive in the presence of tacrolimus because optimal autocrine IL-2 signaling is essential to limit the apoptosis of effector CD4+ T cells and to sustain their transition to and persistence as memory cells [89]. The local administration of tacrolimus in a mouse model with tail lymphedema showed protective and therapeutic efficacy by reducing soft tissue thickness, suppressing inflammatory cell infiltration and inflammatory cytokine expression, and increasing the formation of lymphatic-collecting vessels at the injured site. Furthermore, the recovery of lymphatic functions by tacrolimus, including lymphatic pumping, was observed in a popliteal lymph node dissection model [24].
The inhibition of Th2 differentiation with IL-4- or IL-13-neutralizing antibodies prevents the initiation and progression of lymphedema by inhibiting tissue fibrosis and improving lymphatic function in another mouse tail lymphedema model [27]. Additionally, a report detailed the efficacy of monthly intravenous QBX258 infusion, a combination of two monoclonal antibodies neutralizing IL-4 and IL-13, in eight patients with breast cancer-related lymphedema [28]. Four infusions of QBX258 reduced histological epidermal thickness and suppressed keratinocyte proliferation, type III collagen deposition, mast cell infiltration, and Th2-inducible epithelial-derived cytokine (IL-33, IL-25, and thymic stromal lymphopoietin) expression. QBX258 also improved skin stiffness and patient QOL scores immediately after treatment; however, these improvements returned to baseline four months after the treatment was discontinued. Furthermore, treatment with QBX258 did not decrease the limb volume [28].
Fingolimod (FTY720), a modulator of the sphingosine-1-phosphate receptor, suppresses the emigration of lymphocytes from lymph nodes. In a mouse model with popliteal lymph node dissection, the administration of fingolimod (dissolved in drinking water) from the day of surgery increased CD4+ T cells in inguinal lymph nodes, but decreased them in the skin of the hindlimb [25]. In another mouse tail lymphedema model, fingolimod suppressed the increase in edema volume and fibroadipose thickness from 1 to 6 weeks after lymphatic dissection [25].
3.6. TGF-β Inhibitors (Anti-TGF-β Antibody, Vactosertib, LY-364947)
TGF-β is one of the key mediators in tissue fibrosis; it inhibits functional lymphatic regeneration in the lymphedematous region. The inhibition of TGF-β signaling by monoclonal antibodies or small-molecule drug EW-7197 (vactosertib, an inhibitor of TGF-β receptor type 1) enhanced lymphangiogenesis and lymphatic function by inhibiting fibrosis in a mouse tail lymphedema model [10,90]. Furthermore, LY-364947, a selective inhibitor of TGF-β receptor type 1, markedly suppressed tissue fibrosis and improved lymphatic dysfunction, which was induced by irradiation (with 15 Gy radiation) on the mouse tail [91].
4. Cell-Based Therapy for Lymphedema
4.1. Animal Studies
Cell-based therapies have been studied using lymphedema animal models, as shown in Table 1. In these studies, MSCs derived from bone marrow or adipose tissue were commonly used; until around 2010, the primary mechanism of cell-based therapy using MSCs was attributed to their multipotency in differentiating directly into LECs and promoting lymphangiogenesis [35,36,37,43]. Hwang et al. constructed a mouse hindlimb lymphedema model by circumferential incision and electrocautery of the lymph vessels in the thigh. On the day of surgery, PKH-26-labeled human adipose-derived MSCs (ASCs) were injected subcutaneously, and VEGF-C hydrogel sheets were sutured to the site of the injured lymphatic vessels. As a result, the footpad thickness of the affected limbs was significantly reduced, and the number of vessels with lymphatic vessel endothelial hyaluronan receptor 1 (LYVE-1) was significantly increased on day 28 after the operation. Furthermore, the co-localization of LYVE-1 and PKH-26 was observed around the lymphatic vessels in the combination of human ASCs and VEGF-C hydrogel, but not in human ASCs alone, indicating that transplanted ASCs combined with VFGF-C hydrogel could differentiate into LECs in vivo under specific conditions [36]. In addition, Dai et al. established a mouse hindlimb lymphedema model by circumferentially incising the thigh and removing inguinal lymph nodes following two rounds of 2.25 Gy radiation. Six weeks after the surgery, podoplanin-positive ASCs derived from green fluorescent protein (GFP)-transgenic mice were injected into the lymphedematous skin. Two weeks after implantation, co-localization of GFP and LYVE-1 was detected only in the lymphatic vessels of the podoplanin-positive ASCs transplantation group, and not in the podoplanin-negative and unsorted ASCs transplantation groups [43]. However, the ASCs used in the study may be adipose-derived stromal vascular fraction (SVF) and the cell population of their podoplanin-positive ASCs may be LEC-progenitor cells contained in the SVF.

Table 1.
Cell-based therapies in animal models of lymphedema.
However, the engraftment and direct differentiation of MSCs into LECs may only be marginally effective. The differentiation of ASCs into LECs after transplantation has not been confirmed because SVF or ASCs derived from GFP-transgenic mice cannot survive long term [38,40,43]. Recent studies have focused on paracrine functions that exert anti- inflammatory, anti-fibrosis, and immunomodulatory effects. In animal studies, the therapeutic effects of MSCs increased the lymphatic vessel density (by secreting lymphangiogenic factors such as VEGF-C) [35,36,37,38,39,40,41,42,43,44], restored lymphatic vessel function (by promoting the regeneration of lymphatic collecting vessels and lymphatic pumping) [35,41,42,45], promoted wound healing [39,42], and improved the tissue microenvironment (by anti-fibrotic and anti-inflammatory effects) [38,39,44].
MSC-based therapies combined with biomaterial scaffolds such as Matrigel® [42] and BioBridge® [45] or surgical therapy (VLNT) [41] exhibit efficient regeneration of the functional lymphatic system. These combinational therapies are expected to have a more synergistic effect on lymphedema than individual therapy.
In addition to MSCs, LECs and Tregs have been considered candidate cell populations for lymphedema therapy [23,92,93]. Both LEC-like cells differentiated from mouse muscle-derived stem cells and human LECs promote functional lymphangiogenesis by lymphography [92,93]. Although human LECs did not survive in F344/N rnu/rnu nude rats for more than 22 days after local injection, this treatment resulted in reduced skin thickness and the regeneration of rat-derived lymph vessels. These results suggest that transplanted LECs not only integrate in regenerated lymphatic vessels, but also promote the secretory function of resident cells [93]. Gousopoulos et al. evaluated the efficacy of Tregs (CD4+, CD25+ T cells) transplantation (intravenous injection) using a mouse tail lymphedema model. The results showed the suppression of tail volume increase, inflammatory cell (CD45+ cells, CD206+ cells, and CD68+ cells) infiltration, Tgfb1, Tnfa, and Il10 mRNA expression and fibrotic tissue deposition, and restored lymphatic vessel dilation and lymphatic flow. Therefore, the transplantation of Treg that suppresses Th1/Th2 immune responses has the potential to be a novel therapeutic strategy [23]. The systemic expansion of Tregs by intraperitoneal injection with IL-2/anti-IL-2 monoclonal antibody complexes (IL2-c) was effective for lymphedema to the same degree as adoptive Treg transplantation [23]. However, IL2-c therapy may not be clinically suitable due to the potential side effects of effector T cell activation. Although it has not been confirmed whether MSCs transplantation could induce Tregs in lymphedema models, the expansion of Tregs by MSCs has been examined in in vitro and in vivo studies [94,95]. Therefore, the induction of Tregs may contribute to the therapeutic efficacy of MSCs transplantation in lymphedema.
4.2. Clinical Studies
Somatic stem cell-based therapy for lymphedema in humans has been reported by five research groups (Table 2). The therapeutic efficacy of autologous transplantation was evaluated with bone marrow-derived MSCs or ADRCs for patients with breast cancer-related lymphedema [97,98,99,100,101] and with bone marrow-derived mononuclear cells and peripheral blood hematopoietic stem cells for patients with primary lower limb lymphedema [102,103]. The volume of the edematous limb decreased with cell-based therapy in four groups, while subjective symptoms including heaviness, tension, pain, sensitivity, and mobility of the affected limb and total QOL scores improved in all groups; these effects continued throughout the 4-year follow-up [101]. At the 4-year follow-up after ADRC transplantation, six of the ten patients had reduced the use of conservative lymphedema therapy, and no serious adverse events were observed in the patients [101]. While minor adverse events such as bruising, pain, itching, reduced sensation, and slight irregularity of the skin surface were observed at the donor site, these resolved spontaneously up to 6 months after transplantation [99]. Thus, somatic stem cell-based therapy is a new therapeutic strategy for improving subjective and objective symptoms of lymphedema and for decreasing the bothersome conservative therapy in the long term. Further analyses underlying the therapeutic mechanisms in clinical settings are desirable.

Table 2.
Cell-based therapies in patients with lymphedema.
5. Discussion
Anti-inflammatory pharmacotherapy and cell-based therapy are new therapeutic strategies for improving lymphedema symptoms by promoting functional lymphangiogenesis and improving the microenvironment of the edematous region. However, there has been little evidence for their usefulness in lymphedema therapy. Some animal studies and clinical pilot studies have shown that these therapies could improve the subjective symptoms, but not the volume or appearance of lymphedema. In this review, we focus on the inflammatory cells involved in the pathogenesis of lymphedema, and discuss the clinical usefulness of pharmacotherapy and cell-based therapies for lymphedema.
Since it is difficult to reflect the pathophysiology of secondary lymphedema in animal models because of its occurrence in the chronic state, many animal models have been established to evaluate the new therapeutic strategy for lymphedema. The rodent tail lymphedema model is commonly used to evaluate the therapeutic strategies for secondary lymphedema because this model closely mimics the progression of human lymphedema, including fibrosis, fat deposition, and the infiltration of immune cells [104]. However, it is questionable whether rodent tail lymphedema mimics the pathophysiology of lymphedema in human limbs because the tail of rodents has no lymph nodes and is anatomically and physiologically different from human limbs [104,105]. The mouse hindlimb lymphedema model is also used as an animal model of lymphedema. This model is created by a combination of surgery and irradiation, and closely represents the chronic lymphedematous state in humans. When lymphedema is induced by surgery alone, the edema might resolve spontaneously. Thus, irradiation is often necessary to create the chronic lymphedema model. However, the dose and timing of irradiation are not standardized, and the degree of edema varies widely among studies [104]. Although animal lymphedema models such as rabbit, sheep, dog, pig, and monkey have also been used to study chronic or clinically-relevant lymphedema, the numbers of these studies are limited [104]. Therefore, the establishment of a common animal model that reflects the pathophysiology of human lymphedema is necessary to develop new therapeutic strategies.
Doxycycline, selenium, and synbiotic supplements have been reported to improve lymphedema symptoms to some extent. However, their efficacies for decreasing edema volume and improving the clinical stage of lymphedema are not remarkable. Furthermore, their therapeutic mechanisms for lymphedema have not been elucidated. Compared to these agents, the therapeutic mechanisms of immunosuppressive agents such as tacrolimus, IL-4/IL-13-neutralizing antibodies, and fingolimod have been elucidated. Although these immunosuppressive agents improve the lymphedema symptoms, the symptoms may return to baseline after the treatment is discontinued. Therefore, patients with lymphedema require lifelong treatment to maintain their QOL. However, long-term treatment with immunosuppressive agents such as fingolimod and IL-4/IL-13-neutralizing antibodies may be a risk factor for infection (e.g., cellulitis) [28]. Further evidence of the long-term safety and duration of immunosuppressive therapies is necessary to treat lymphedema in clinical settings. Collectively, we consider that pharmacotherapies with these agents cannot be recommended actively for lymphedema at present.
MSCs exhibit immunomodulatory effects [106], and Jørgensen et al. suggested that ADRC transplantation could alleviate the incidence of cellulitis in patients with breast cancer-related lymphedema during a 4-year follow-up period [101]. Additionally, bone marrow-derived mononuclear cells and peripheral blood hematopoietic stem cells could decrease edema volume in primary lower limb lymphedema without serious adverse events [102,103]. Although the molecular mechanism underlying their therapeutic efficacy is unclear at present, cell-based therapy is attractive to establish new therapeutic strategies for primary and secondary lymphedema. We speculate that transplanted MSCs may improve lymphedema symptoms through anti-inflammatory, antioxidant, and immunomodulatory effects via cytokines/growth factor secretion, Tregs induction, and improvement in the microenvironment.
A major problem in current cell-based therapy is that MSCs are hardly characterized by cell surface markers and the multipotency of the isolated cell population. In 2006, the International Society for Cell & Gene Therapy Mesenchymal Stromal Cell committee proposed that the minimal criteria defining human multipotent mesenchymal stromal cells, rather than mesenchymal stem cells, were plastic adherence, expression of (≥95% positive) CD105, CD73, and CD90, lack of (≤2% positive) hematopoietic and endothelial markers CD45, CD34, CD14 or CD11b, CD79α or CD19, and HLA-DR, and the capability of differentiation into adipocyte, chondrocyte, and osteoblast lineages in vitro [107,108]. However, most MSC populations used for lymphedema therapy have not been characterized by flow cytometry or differentiation capacity assay. Furthermore, cell surface markers for animal-derived MSCs have not been defined. Since adipose-derived MSCs, especially fresh SVF or ADRCs, belong to a heterogeneous cell population, the therapeutic efficacy of ASC transplantation may vary among researchers and/or physicians. Additionally, Bucan et al. reported no differences in the hindlimb volume and lymphatic clearance of a hindlimb lymphedema mouse model between the SVF or ASC transplantation and vehicle control groups. In their study, <20% of ASCs expressed CD105 and/or stem cell antigen-1 [96]. Therefore, the characterization of MSCs used in therapy can help to eliminate the differences in therapeutic efficacy among practitioners.
In the future, the treatment of lymphedema should focus on lymphatic regeneration and on improving the microenvironment of the edematous region, such as the suppression of fibrosis and infiltration of inflammatory cells, and the regulation of CD4+ T cell balance. Although further evidence on the long-term safety and efficacy and underlying mechanisms of anti-inflammatory pharmacotherapy and cell-based therapy is necessary, these therapies may shed light on the development of a new radical therapeutic strategy for lymphedema to improve the microenvironment and immune responses.
Author Contributions
Conceptualization: R.O. and K.H.; writing—original draft preparation: R.O. and T.Y.; writing—review and editing, R.O., T.Y., M.H., S.S., S.Y. and K.H. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
Abbreviations
| ADRC | adipose-derived regenerative cell |
| ASC | adipose-derived mesenchymal stem/stromal cell |
| CCL | C–C chemokine ligand |
| CCR | C–C chemokine receptor |
| CLA | cutaneous leukocyte antigen |
| CRP | C-reactive protein |
| DAMPs | danger-associated molecular patterns |
| DC | dendritic cell |
| eNOS | endothelial nitric oxide synthase |
| GFP | green fluorescent protein |
| HMGB1 | high-mobility group box 1 |
| IFN | interferon |
| IL | interleukin |
| IL2-c | IL-2/anti-IL-2 complex |
| iNOS | inducible nitric oxide synthase |
| LEC | lymphatic endothelial cell |
| LT | leukotriene |
| LYVE-1 | lymphatic vessel endothelial hyaluronan receptor 1 |
| MSC | mesenchymal stem/stromal cell |
| QOL | quality of life |
| RT | radiation therapy |
| SVF | stromal vascular fraction |
| Th | helper T cell |
| TNF | tumor necrosis factor |
| TGF | transforming growth factor |
| Treg | regulatory T cell |
| VEGF | vascular endothelial growth factor |
| VLNT | vascularized lymph node transfer |
References
- Grada, A.A.; Phillips, T. Lymphedema: Pathophysiology and clinical manifestations. J. Am. Acad. Dermatol. 2017, 77, 1009–1020. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.; Chiang, N.; Perng, C.; Ma, H.; Lin, C.-H. Review of preclinical and clinical studies of using cell-based therapy for secondary lymphedema. J. Surg. Oncol. 2019, 121, 109–120. [Google Scholar] [CrossRef] [PubMed]
- Brown, S.; Dayan, J.H.; Coriddi, M.; Campbell, A.; Kuonqui, K.; Shin, J.; Park, H.J.; Mehrara, B.J.; Kataru, R.P. Pharmacological Treatment of Secondary Lymphedema. Front. Pharmacol. 2022, 13, 828513. [Google Scholar] [CrossRef]
- Ghezzi, F.; Uccella, S.; Cromi, A.; Bogani, G.; Robba, C.; Serati, M.; Bolis, P. Lymphoceles, Lymphorrhea, and Lymphedema after Laparoscopic and Open Endometrial Cancer Staging. Ann. Surg. Oncol. 2011, 19, 259–267. [Google Scholar] [CrossRef] [PubMed]
- Allam, O.; Park, K.E.; Chandler, L.; Mozaffari, M.A.; Ahmad, M.; Lu, X.; Alperovich, M. The impact of radiation on lymphedema: A review of the literature. Gland Surg. 2020, 9, 596–602. [Google Scholar] [CrossRef] [PubMed]
- Maruccia, M.; Elia, R.; Ciudad, P.; Nacchiero, E.; Nicoli, F.; Vestita, M.; Chen, H.; Giudice, G. Postmastectomy upper limb lymphedema: Combined vascularized lymph node transfer and scar release with fat graft expedites surgical and patients’ related outcomes. A retrospective comparative study. J. Plast. Reconstr. Aesthetic Surg. 2019, 72, 892–901. [Google Scholar] [CrossRef] [PubMed]
- Jensen, M.R.; Simonsen, L.; Karlsmark, T.; Bülow, J. Microvascular filtration is increased in the forearms of patients with breast cancer–related lymphedema. J. Appl. Physiol. 2013, 114, 19–27. [Google Scholar] [CrossRef]
- Zampell, J.C.; Yan, A.; Elhadad, S.; Avraham, T.; Weitman, E.; Mehrara, B.J. CD4+ Cells Regulate Fibrosis and Lymphangiogenesis in Response to Lymphatic Fluid Stasis. PLoS ONE 2012, 7, e49940. [Google Scholar] [CrossRef]
- Avraham, T.; Clavin, N.W.; Daluvoy, S.V.; Fernandez, J.; Soares, M.A.; Cordeiro, A.P.; Mehrara, B.J. Fibrosis Is a Key Inhibitor of Lymphatic Regeneration. Plast. Reconstr. Surg. 2009, 124, 438–450. [Google Scholar] [CrossRef]
- Avraham, T.; Daluvoy, S.; Zampell, J.; Yan, A.; Haviv, Y.S.; Rockson, S.G.; Mehrara, B.J. Blockade of Transforming Growth Factor-β1 Accelerates Lymphatic Regeneration during Wound Repair. Am. J. Pathol. 2010, 177, 3202–3214. [Google Scholar] [CrossRef]
- Kataru, R.P.; Baik, J.E.; Park, H.J.; Wiser, I.; Rehal, S.; Shin, J.Y.; Mehrara, B.J. Regulation of Immune Function by the Lymphatic System in Lymphedema. Front. Immunol. 2019, 10, 470. [Google Scholar] [CrossRef] [PubMed]
- Dayes, I.S.; Whelan, T.J.; Julian, J.A.; Parpia, S.; Pritchard, K.I.; D’Souza, D.P.; Kligman, L.; Reise, D.; Leblanc, L.; McNeely, M.; et al. Randomized Trial of Decongestive Lymphatic Therapy for the Treatment of Lymphedema in Women with Breast Cancer. J. Clin. Oncol. 2013, 31, 3758–3763. [Google Scholar] [CrossRef] [PubMed]
- Schmitz, K.H.; Troxel, A.B.; Dean, L.T.; DeMichele, A.; Brown, J.C.; Sturgeon, K.; Zhang, Z.; Evangelisti, M.; Spinelli, B.; Kallan, M.J.; et al. Effect of Home-Based Exercise and Weight Loss Programs on Breast Cancer-Related Lymphedema Outcomes Among Over-weight Breast Cancer Survivors: The WISER Survivor Randomized Clinical Trial. JAMA Oncol. 2019, 5, 1605–1613. [Google Scholar] [CrossRef] [PubMed]
- Keith, L.; Rowsemitt, C.; Richards, L.G. Lifestyle Modification Group for Lymphedema and Obesity Results in Significant Health Outcomes. Am. J. Lifestyle Med. 2017, 14, 420–428. [Google Scholar] [CrossRef]
- Liang, M.; Chen, Q.; Peng, K.; Deng, L.; He, L.; Hou, Y.; Zhang, Y.; Guo, J.; Mei, Z.; Li, L. Manual lymphatic drainage for lymphedema in patients after breast cancer surgery: A systematic review and meta-analysis of randomized controlled trials. Medicine 2020, 99, e23192. [Google Scholar] [CrossRef]
- Muñoz-Alcaraz, M.N.; Pérula-De-Torres, L.; Serrano-Merino, J.; Jiménez-Vílchez, A.J.; Olmo-Carmona, M.V.; Muñoz-García, M.T.; Bartolomé-Moreno, C.; Oliván-Blázquez, B.; Magallón-Botaya, R. Efficacy and efficiency of a new therapeutic approach based on activity-oriented proprioceptive antiedema therapy (TAPA) for edema reduction and improved occupational performance in the rehabilitation of breast cancer-related arm lymphedema in women: A controlled, randomized clinical trial. BMC Cancer 2020, 20, 1–11. [Google Scholar] [CrossRef]
- Barufi, S.; de Godoy, H.J.P.; de Godoy, J.M.P.; Godoy, M.D.F.G. Exercising and Compression Mechanism in the Treatment of Lymphedema. Cureus 2021, 13, e16121. [Google Scholar] [CrossRef]
- Basta, M.; Gao, L.L.; Wu, L.C. Operative Treatment of Peripheral Lymphedema: A systematic meta-analysis of the efficacy and safety of lymphovenous microsurgery and tissue transplantation. Plast. Reconstr. Surg. 2014, 133, 905–913. [Google Scholar] [CrossRef]
- Granzow, J.W.; Soderberg, J.M.; Kaji, A.H.; Dauphine, C. Review of Current Surgical Treatments for Lymphedema. Ann. Surg. Oncol. 2014, 21, 1195–1201. [Google Scholar] [CrossRef]
- Raju, A.; Chang, D.W. Vascularized Lymph Node Transfer for Treatment of Lymphedema: A comprehensive literature review. Ann. Surg. 2015, 261, 1013–1023. [Google Scholar] [CrossRef]
- Chang, E.I.; Schaverien, M.V.; Hanson, S.E.; Chu, C.K.; Hanasono, M.M. Evolution in Surgical Management of Breast Cancer-related Lymphedema: The MD Anderson Cancer Center Experience. Plast. Reconstr. Surg. Glob. Open 2020, 8, e2674. [Google Scholar] [CrossRef] [PubMed]
- Hanson, S.E.; Chang, E.I.; Schaverien, M.V.; Chu, C.; Selber, J.C.; Hanasono, M.M. Controversies in Surgical Management of Lymphedema. Plast. Reconstr. Surg. Glob. Open 2020, 8, e2671. [Google Scholar] [CrossRef]
- Gousopoulos, E.; Proulx, S.T.; Bachmann, S.B.; Scholl, J.; Dionyssiou, D.; Demiri, E.; Halin, C.; Dieterich, L.C.; Detmar, M. Regulatory T cell transfer ameliorates lymphedema and promotes lymphatic vessel function. JCI Insight 2016, 1, e89081. [Google Scholar] [CrossRef] [PubMed]
- Gardenier, J.C.; Kataru, R.P.; Hespe, G.E.; Savetsky, I.; Torrisi, J.S.; Nores, G.D.G.; Jowhar, D.K.; Nitti, M.D.; Schofield, R.C.; Carlow, D.C.; et al. Topical tacrolimus for the treatment of secondary lymphedema. Nat. Commun. 2017, 8, 14345. [Google Scholar] [CrossRef] [PubMed]
- Nores, G.D.G.; Ly, C.L.; Cuzzone, D.; Kataru, R.P.; Hespe, G.E.; Torrisi, J.S.; Huang, J.J.; Gardenier, J.C.; Savetsky, I.; Nitti, M.D.; et al. CD4+ T cells are activated in regional lymph nodes and migrate to skin to initiate lymphedema. Nat. Commun. 2018, 9, 1–14. [Google Scholar] [CrossRef]
- Zampell, J.C.; Elhadad, S.; Avraham, T.; Weitman, E.; Aschen, S.; Yan, A.; Mehrara, B.J. Toll-like receptor deficiency worsens inflammation and lymphedema after lymphatic injury. Am. J. Physiol. Physiol. 2012, 302, C709–C719. [Google Scholar] [CrossRef]
- Avraham, T.; Zampell, J.C.; Yan, A.; Elhadad, S.; Weitman, E.S.; Rockson, S.G.; Bromberg, J.; Mehrara, B.J. Th2 differentiation is necessary for soft tissue fibrosis and lymphatic dysfunction resulting from lymphedema. FASEB J. 2012, 27, 1114–1126. [Google Scholar] [CrossRef]
- Mehrara, B.J.; Park, H.J.; Kataru, R.P.; Bromberg, J.; Coriddi, M.; Baik, J.E.; Shin, J.; Li, C.; Cavalli, M.R.; Encarnacion, E.M.; et al. Pilot Study of Anti-Th2 Immunotherapy for the Treatment of Breast Cancer-Related Upper Extremity Lymphedema. Biology 2021, 10, 934. [Google Scholar] [CrossRef]
- Mazini, L.; Rochette, L.; Admou, B.; Amal, S.; Malka, G. Hopes and Limits of Adipose-Derived Stem Cells (ADSCs) and Mesenchymal Stem Cells (MSCs) in Wound Healing. Int. J. Mol. Sci. 2020, 21, 1306. [Google Scholar] [CrossRef]
- Dave, M.; Mehta, K.; Luther, J.; Baruah, A.; Dietz, A.; Faubion, W.A. Mesenchymal Stem Cell Therapy for Inflammatory Bowel Disease: A Systematic Review and Meta-analysis. Inflamm. Bowel Dis. 2015, 21, 2696–2707. [Google Scholar] [CrossRef]
- Mishra, V.K.; Shih, H.-H.; Parveen, F.; Lenzen, D.; Ito, E.; Chan, T.-F.; Ke, L.-Y. Identifying the Therapeutic Significance of Mesenchymal Stem Cells. Cells 2020, 9, 1145. [Google Scholar] [CrossRef] [PubMed]
- Rokunohe, A.; Matsuzaki, Y.; Rokunohe, D.; Sakuraba, Y.; Fukui, T.; Nakano, H.; Sawamura, D. Immunosuppressive effect of adipose-derived stromal cells on imiquimod-induced psoriasis in mice. J. Dermatol. Sci. 2015, 82, 50–53. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.S.; Sah, S.K.; Lee, J.H.; Seo, K.-W.; Kang, K.-S.; Kim, T.-Y. Human umbilical cord blood-derived mesenchymal stem cells ameliorate psoriasis-like skin inflammation in mice. Biochem. Biophys. Rep. 2016, 9, 281–288. [Google Scholar] [CrossRef]
- Jurado, M.; De La Mata, C.; Ruiz-García, A.; López-Fernández, E.; Espinosa, O.; Remigia, M.J.; Moratalla, L.; Goterris, R.; García-Martín, P.; Ruiz-Cabello, F.; et al. Adipose tissue-derived mesenchymal stromal cells as part of therapy for chronic graft-versus-host disease: A phase I/II study. Cytotherapy 2017, 19, 927–936. [Google Scholar] [CrossRef] [PubMed]
- Conrad, C.; Niess, H.; Huss, R.; Huber, S.; Von Luettichau, I.; Nelson, P.J.; Ott, H.C.; Jauch, K.-W.; Bruns, C.J. Multipotent Mesenchymal Stem Cells Acquire a Lymphendothelial Phenotype and Enhance Lymphatic Regeneration In Vivo. Circulation 2009, 119, 281–289. [Google Scholar] [CrossRef] [PubMed]
- Hwang, J.H.; Kim, I.G.; Lee, J.Y.; Piao, S.; Lee, D.S.; Lee, T.S.; Ra, J.C. Therapeutic lymphangiogenesis using stem cell and VEGF-C hydrogel. Biomaterials 2011, 32, 4415–4423. [Google Scholar] [CrossRef]
- Zhou, H.; Wang, M.; Hou, C.; Jin, X.; Wu, X. Exogenous VEGF-C Augments the Efficacy of Therapeutic Lymphangiogenesis Induced by Allogenic Bone Marrow Stromal Cells in a Rabbit Model of Limb Secondary Lymphedema. Jpn. J. Clin. Oncol. 2011, 41, 841–846. [Google Scholar] [CrossRef][Green Version]
- Shimizu, Y.; Shibata, R.; Shintani, S.; Ishii, M.; Murohara, T. Therapeutic Lymphangiogenesis with Implantation of Adipose-Derived Regenerative Cells. J. Am. Heart Assoc. 2012, 1, e000877. [Google Scholar] [CrossRef]
- Ackermann, M.; Wettstein, R.; Senaldi, C.; Kalbermatten, D.F.; Konerding, M.A.; Raffoul, W.; Erba, P. Impact of platelet rich plasma and adipose stem cells on lymphangiogenesis in a murine tail lymphedema model. Microvasc. Res. 2015, 102, 78–85. [Google Scholar] [CrossRef]
- Yoshida, S.; Hamuy, R.; Hamada, Y.; Yoshimoto, H.; Hirano, A.; Akita, S. Adipose-derived stem cell transplantation for therapeutic lymphangiogenesis in a mouse secondary lymphedema model. Regen. Med. 2015, 10, 549–562. [Google Scholar] [CrossRef]
- Hayashida, K.; Yoshida, S.; Yoshimoto, H.; Fujioka, M.; Saijo, H.; Migita, K.; Kumaya, M.; Akita, S. Adipose-Derived Stem Cells and Vascularized Lymph Node Transfers Successfully Treat Mouse Hindlimb Secondary Lymphedema by Early Reconnection of the Lymphatic System and Lymphangiogenesis. Plast. Reconstr. Surg. 2017, 139, 639–651. [Google Scholar] [CrossRef] [PubMed]
- Beerens, M.; Aranguren, X.L.; Hendrickx, B.; Dheedene, W.; Dresselaers, T.; Himmelreich, U.; Verfaillie, C.; Luttun, A. Multipotent Adult Progenitor Cells Support Lymphatic Regeneration at Multiple Anatomical Levels during Wound Healing and Lymphedema. Sci. Rep. 2018, 8, 3852. [Google Scholar] [CrossRef] [PubMed]
- Dai, T.; Jiang, Z.; Cui, C.; Sun, Y.; Lu, B.; Li, H.; Cao, W.; Chen, B.; Li, S.; Guo, L. The Roles of Podoplanin-Positive/Podoplanin-Negative Cells from Adipose-Derived Stem Cells in Lymphatic Regeneration. Plast. Reconstr. Surg. 2020, 145, 420–431. [Google Scholar] [CrossRef] [PubMed]
- Ogino, R.; Hayashida, K.; Yamakawa, S.; Morita, E. Adipose-Derived Stem Cells Promote Intussusceptive Lymphangiogenesis by Restricting Dermal Fibrosis in Irradiated Tissue of Mice. Int. J. Mol. Sci. 2020, 21, 3885. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, D.; Zaitseva, T.S.; Zhou, A.; Rochlin, D.; Sue, G.; Deptula, P.; Tabada, P.; Wan, D.; Loening, A.; Paukshto, M.; et al. Lymphatic regeneration after implantation of aligned nanofibrillar collagen scaffolds: Preliminary preclinical and clinical results. J. Surg. Oncol. 2021, 125, 113–122. [Google Scholar] [CrossRef]
- Scallan, J.P.; Zawieja, S.D.; Castorena-Gonzalez, J.A.; Davis, M.J. Lymphatic pumping: Mechanics, mechanisms and malfunction. J. Physiol. 2016, 594, 5749–5768. [Google Scholar] [CrossRef] [PubMed]
- Chen, K.; Sinelnikov, M.Y.; Reshetov, I.V.; Timashev, P.; Gu, Y.; Mu, L.; Lu, P.; Zhang, Y. Therapeutic Potential of Mesenchymal Stem Cells for Postmastectomy Lymphedema: A Literature Review. Clin. Transl. Sci. 2020, 14, 54–61. [Google Scholar] [CrossRef] [PubMed]
- Ly, C.L.; Nores, G.D.G.; Kataru, R.P.; Mehrara, B.J. T helper 2 differentiation is necessary for development of lymphedema. Transl. Res. 2018, 206, 57–70. [Google Scholar] [CrossRef]
- Qiu, Y.; Chen, Y.; Fu, X.; Zhang, L.; Tian, J.; Hao, Q. HMGB1 promotes lymphangiogenesis of human lymphatic endothelial cells in vitro. Med. Oncol. 2010, 29, 358–363. [Google Scholar] [CrossRef]
- Zampell, J.C.; Yan, A.; Avraham, T.; Andrade, V.; Malliaris, S.; Aschen, S.; Rockson, S.G.; Mehrara, B.J. Temporal and spatial patterns of endogenous danger signal expression after wound healing and in response to lymphedema. Am. J. Physiol. Physiol. 2011, 300, C1107–C1121. [Google Scholar] [CrossRef]
- Ghanta, S.; Cuzzone, D.A.; Torrisi, J.S.; Albano, N.J.; Joseph, W.J.; Savetsky, I.L.; Gardenier, J.C.; Chang, D.; Zampell, J.C.; Mehrara, B.J. Regulation of inflammation and fibrosis by macrophages in lymphedema. Am. J. Physiol. Circ. Physiol. 2015, 308, H1065–H1077. [Google Scholar] [CrossRef] [PubMed]
- Ogata, F.; Fujiu, K.; Matsumoto, S.; Nakayama, Y.; Shibata, M.; Oike, Y.; Koshima, I.; Watabe, T.; Nagai, R.; Manabe, I. Excess Lymphangiogenesis Cooperatively Induced by Macrophages and CD4+ T Cells Drives the Pathogenesis of Lymphedema. J. Investig. Dermatol. 2015, 136, 706–714. [Google Scholar] [CrossRef] [PubMed]
- Gardenier, J.C.; Hespe, G.E.; Kataru, R.P.; Savetsky, I.; Torrisi, J.S.; Nores, G.D.G.; Dayan, J.J.; Chang, D.; Zampell, J.; Martinez-Corral, I.; et al. Diphtheria toxin–mediated ablation of lymphatic endothelial cells results in progressive lymphedema. JCI Insight 2016, 1, e84095. [Google Scholar] [CrossRef]
- Baluk, P.; Fuxe, J.; Hashizume, H.; Romano, T.; Lashnits, E.; Butz, S.; Vestweber, D.; Corada, M.; Molendini, C.; Dejana, E.; et al. Functionally specialized junctions between endothelial cells of lymphatic vessels. J. Exp. Med. 2007, 204, 2349–2362. [Google Scholar] [CrossRef] [PubMed]
- Tal, O.; Lim, H.Y.; Gurevich, I.; Milo, I.; Shipony, Z.; Ng, L.G.; Angeli, V.; Shakhar, G. DC mobilization from the skin requires docking to immobilized CCL21 on lymphatic endothelium and intralymphatic crawling. J. Exp. Med. 2011, 208, 2141–2153. [Google Scholar] [CrossRef]
- Weber, M.; Hauschild, R.; Schwarz, J.; Moussion, C.; de Vries, I.; Legler, D.F.; Luther, S.A.; Bollenbach, T.; Sixt, M. Interstitial Dendritic Cell Guidance by Haptotactic Chemokine Gradients. Science 2013, 339, 328–332. [Google Scholar] [CrossRef]
- Teijeira, A.; Rouzaut, A.; Melero, I. Initial Afferent Lymphatic Vessels Controlling Outbound Leukocyte Traffic from Skin to Lymph Nodes. Front. Immunol. 2013, 4, 433. [Google Scholar] [CrossRef]
- Russo, E.; Teijeira, A.; Vaahtomeri, K.; Willrodt, A.-H.; Bloch, J.; Nitschké, M.; Santambrogio, L.; Kerjaschki, D.; Sixt, M.; Halin, C. Intralymphatic CCL21 Promotes Tissue Egress of Dendritic Cells through Afferent Lymphatic Vessels. Cell Rep. 2016, 14, 1723–1734. [Google Scholar] [CrossRef]
- Syrbe, U.; Siveke, J.; Hamann, A. Th1/Th2 subsets: Distinct differences in homing and chemokine receptor expression? Springer Semin. Immunopathol. 1999, 21, 263–285. [Google Scholar] [CrossRef]
- Reiss, Y.; Proudfoot, A.E.; Power, C.A.; Campbell, J.; Butcher, E.C. CC Chemokine Receptor (CCR)4 and the CCR10 Ligand Cutaneous T Cell–attracting Chemokine (CTACK) in Lymphocyte Trafficking to Inflamed Skin. J. Exp. Med. 2001, 194, 1541–1547. [Google Scholar] [CrossRef]
- Agace, W.W. Tissue-tropic effector T cells: Generation and targeting opportunities. Nat. Rev. Immunol. 2006, 6, 682–692. [Google Scholar] [CrossRef] [PubMed]
- Ni, Z.; Walcheck, B. Cutaneous lymphocyte-associated antigen (CLA) T cells up-regulate P-selectin ligand expression upon their activation. Clin. Immunol. 2009, 133, 257–264. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Ly, C.; Cuzzone, D.; Kataru, R.P.; Mehrara, B.J. Small Numbers of CD4+ T Cells Can Induce Development of Lymphedema. Plast. Reconstr. Surg. 2019, 143, 518e–526e. [Google Scholar] [CrossRef] [PubMed]
- Chiaramonte, M.G.; Cheever, A.W.; Malley, J.D.; Donaldson, D.D.; Wynn, T.A. Studies of murine schistosomiasis reveal interleukin-13 blockade as a treatment for established and progressive liver fibrosis. Hepatology 2001, 34, 273–282. [Google Scholar] [CrossRef] [PubMed]
- Wynn, T.A. Fibrotic disease and the TH1/TH2 paradigm. Nat. Rev. Immunol. 2004, 4, 583–594. [Google Scholar] [CrossRef]
- Clavin, N.W.; Avraham, T.; Fernandez, J.; Daluvoy, S.V.; Soares, M.A.; Chaudhry, A.; Mehrara, B.J. TGF-β1 is a negative regulator of lymphatic regeneration during wound repair. Am. J. Physiol. Circ. Physiol. 2008, 295, H2113–H2127. [Google Scholar] [CrossRef]
- Kataru, R.P.; Kim, H.; Jang, C.; Choi, D.K.; Koh, B.I.; Kim, M.; Gollamudi, S.; Kim, Y.-K.; Lee, S.-H.; Koh, G.Y. T Lymphocytes Negatively Regulate Lymph Node Lymphatic Vessel Formation. Immunity 2011, 34, 96–107. [Google Scholar] [CrossRef]
- Kim, H.; Kataru, R.; Koh, G.Y. Inflammation-associated lymphangiogenesis: A double-edged sword? J. Clin. Investig. 2014, 124, 936–942. [Google Scholar] [CrossRef]
- Shin, K.; Kataru, R.P.; Park, H.J.; Kwon, B.-I.; Kim, T.W.; Hong, Y.K.; Lee, S.-H. TH2 cells and their cytokines regulate formation and function of lymphatic vessels. Nat. Commun. 2015, 6, 6196. [Google Scholar] [CrossRef]
- Savetsky, I.L.; Ghanta, S.; Gardenier, J.C.; Torrisi, J.S.; Nores, G.D.G.; Hespe, G.E.; Nitti, M.D.; Kataru, R.P.; Mehrara, B.J. Th2 Cytokines Inhibit Lymphangiogenesis. PLoS ONE 2015, 10, e0126908. [Google Scholar] [CrossRef]
- Karlsen, T.V.; Karkkainen, M.J.; Alitalo, K.; Wiig, H. Transcapillary fluid balance consequences of missing initial lymphatics studied in a mouse model of primary lymphoedema. J. Physiol. 2006, 574, 583–596. [Google Scholar] [CrossRef]
- Cuzzone, D.A.; Weitman, E.S.; Albano, N.J.; Ghanta, S.; Savetsky, I.; Gardenier, J.C.; Joseph, W.J.; Torrisi, J.S.; Bromberg, J.F.; Olszewski, W.; et al. IL-6 regulates adipose deposition and homeostasis in lymphedema. Am. J. Physiol. Circ. Physiol. 2014, 306, H1426–H1434. [Google Scholar] [CrossRef] [PubMed]
- Torrisi, J.S.; Hespe, G.E.; Cuzzone, D.A.; Savetsky, I.L.; Nitti, M.D.; Gardenier, J.C.; Nores, G.D.G.; Jowhar, D.; Kataru, R.; Mehrara, B.J. Inhibition of Inflammation and iNOS Improves Lymphatic Function in Obesity. Sci. Rep. 2016, 6, 19817. [Google Scholar] [CrossRef] [PubMed]
- Mand, S.; Debrah, A.; Klarmann, U.; Batsa, L.; Marfo-Debrekyei, Y.; Kwarteng, A.; Specht, S.; Belda-Domene, A.; Fimmers, R.; Taylor, M.; et al. Doxycycline Improves Filarial Lymphedema Independent of Active Filarial Infection: A Randomized Controlled Trial. Clin. Infect. Dis. 2012, 55, 621–630. [Google Scholar] [CrossRef] [PubMed]
- Henehan, M.; Montuno, M.; De Benedetto, A. Doxycycline as an anti-inflammatory agent: Updates in dermatology. J. Eur. Acad. Dermatol. Venereol. 2017, 31, 1800–1808. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, K.; Radhakrishnan, K.; Wong, Y.M.; Rockson, S.G. Anti-Inflammatory Pharmacotherapy with Ketoprofen Ameliorates Experimental Lymphatic Vascular Insufficiency in Mice. PLoS ONE 2009, 4, e8380. [Google Scholar] [CrossRef] [PubMed]
- Rockson, S.G.; Tian, W.; Jiang, X.; Kuznetsova, T.; Haddad, F.; Zampell, J.; Mehrara, B.; Sampson, J.P.; Roche, L.; Kim, J.; et al. Pilot studies demonstrate the potential benefits of antiinflammatory therapy in human lymphedema. JCI Insight 2018, 3, e123775. [Google Scholar] [CrossRef]
- Tian, W.; Rockson, S.G.; Jiang, X.; Kim, J.; Begaye, A.; Shuffle, E.M.; Tu, A.B.; Cribb, M.; Nepiyushchikh, Z.; Feroze, A.H.; et al. Leukotriene B4 antagonism ameliorates experimental lymphedema. Sci. Transl. Med. 2017, 9, eaal3920. [Google Scholar] [CrossRef] [PubMed]
- Cribb, M.; Sestito, L.; Rockson, S.; Nicolls, M.; Thomas, S.; Dixon, J. The Kinetics of Lymphatic Dysfunction and Leukocyte Expansion in the Draining Lymph Node during LTB4 Antagonism in a Mouse Model of Lymphedema. Int. J. Mol. Sci. 2021, 22, 4455. [Google Scholar] [CrossRef]
- Kasseroller, R.G.; Schrauzer, G.N. Treatment of Secondary Lymphedema of the Arm with Physical Decongestive Therapy and Sodium Selenite: A review. Am. J. Ther. 2000, 7, 273–279. [Google Scholar] [CrossRef]
- Bruns, F.; Micke, O.; Bremer, M. Current status of selenium and other treatments for secondary lymphedema. J. Support. Oncol. 2004, 1, 121–130. [Google Scholar]
- Han, H.W.; Yang, E.J.; Lee, S.-M. Sodium Selenite Alleviates Breast Cancer-Related Lymphedema Independent of Antioxidant Defense System. Nutrients 2019, 11, 1021. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.; Lee, B.; Kim, Y.; Min, S.; Yang, E.; Lee, S. Effects of Sodium Selenite Injection on Serum Metabolic Profiles in Women Diagnosed with Breast Cancer-Related Lymphedema—Secondary Analysis of a Randomized Placebo-Controlled Trial Using Global Metabolomics. Nutrients 2021, 13, 3253. [Google Scholar] [CrossRef] [PubMed]
- McLoughlin, R.F.; Berthon, B.S.; Jensen, M.E.; Baines, K.J.; Wood, L.G. Short-chain fatty acids, prebiotics, synbiotics, and systemic inflammation: A systematic review and meta-analysis. Am. J. Clin. Nutr. 2017, 106, 930–945. [Google Scholar] [CrossRef] [PubMed]
- Vafa, S.; Haghighat, S.; Janani, L.; Totmaj, A.S.; Navaei, M.; Amirinejad, A.; Emamat, H.; Salehi, Z.; Zarrati, M. The effects of synbiotic supplementation on serum inflammatory markers and edema volume in breast cancer survivors with lymphedema. EXCLI J. 2020, 19, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Vafa, S.; Zarrati, M.; Malakootinejad, M.; Totmaj, A.S.; Zayeri, F.; Salehi, M.; Sanati, V.; Haghighat, S. Calorie restriction and synbiotics effect on quality of life and edema reduction in breast cancer-related lymphedema, a clinical trial. Breast 2020, 54, 37–45. [Google Scholar] [CrossRef]
- Navaei, M.; Haghighat, S.; Janani, L.; Vafa, S.; Totmaj, A.S.; Lahiji, M.R.; Emamat, H.; Salehi, Z.; Amirinejad, A.; Izad, M.; et al. The Effects of Synbiotic Supplementation on Antioxidant Capacity and Arm Volumes in Survivors of Breast Cancer-Related Lymphedema. Nutr. Cancer 2019, 72, 62–73. [Google Scholar] [CrossRef]
- Jorgensen, K.A.; Koefoed-Nielsen, P.B.; Karamperis, N. Calcineurin Phosphatase Activity and Immunosuppression. A Review on the Role of Calcineurin Phosphatase Activity and the Immunosuppressive Effect of Cyclosporin A and Tacrolimus. Scand. J. Immunol. 2003, 57, 93–98. [Google Scholar] [CrossRef]
- McKinstry, K.K.; Strutt, T.M.; Bautista, B.; Zhang, W.; Kuang, Y.; Cooper, A.; Swain, S.L. Effector CD4 T-cell transition to memory requires late cognate interactions that induce autocrine IL-2. Nat. Commun. 2014, 5, 5377. [Google Scholar] [CrossRef]
- Yoon, S.-H.; Kim, K.Y.; Wang, Z.; Park, J.-H.; Bae, S.M.; Kim, S.-Y.; Song, H.-Y.; Jeon, J.Y. EW-7197, a Transforming Growth Factor-Beta Type I Receptor Kinase Inhibitor, Ameliorates Acquired Lymphedema in a Mouse Tail Model. Lymphat. Res. Biol. 2020, 18, 433–438. [Google Scholar] [CrossRef]
- Avraham, T.; Yan, A.; Zampell, J.C.; Daluvoy, S.V.; Haimovitz-Friedman, A.; Cordeiro, A.P.; Mehrara, B.J. Radiation therapy causes loss of dermal lymphatic vessels and interferes with lymphatic function by TGF-β1-mediated tissue fibrosis. Am. J. Physiol. Physiol. 2010, 299, C589–C605. [Google Scholar] [CrossRef] [PubMed]
- Park, H.S.; Jung, I.M.; Choi, G.H.; Hahn, S.; Yoo, Y.S.; Lee, T. Modification of a Rodent Hindlimb Model of Secondary Lymphedema: Surgical Radicality versus Radiotherapeutic Ablation. BioMed Res. Int. 2013, 2013, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Kawai, Y.; Shiomi, H.; Abe, H.; Naka, S.; Kurumi, Y.; Tani, T. Cell transplantation therapy for a rat model of secondary lymphedema. J. Surg. Res. 2014, 189, 184–191. [Google Scholar] [CrossRef] [PubMed]
- Aggarwal, S.; Pittenger, M.F. Human mesenchymal stem cells modulate allogeneic immune cell responses. Blood 2005, 105, 1815–1822. [Google Scholar] [CrossRef]
- Farrokhi, A.S.; Zarnani, A.-H.; Kahmini, F.R.; Moazzeni, S.M. Mesenchymal stem cells induce expansion of regulatory T cells in abortion-prone mice. Reproduction 2021, 161, 477–487. [Google Scholar] [CrossRef]
- Bucan, A.; Dhumale, P.; Jørgensen, M.G.; Dalaei, F.; Wiinholt, A.; Hansen, C.R.; Hvidsten, S.; Baun, C.; Hejbøl, E.K.; Schrøder, H.D.; et al. Comparison between stromal vascular fraction and adipose derived stem cells in a mouse lymphedema model. J. Plast. Surg. Hand Surg. 2020, 54, 302–311. [Google Scholar] [CrossRef]
- Hou, C.; Wu, X.; Jin, X. Autologous Bone Marrow Stromal Cells Transplantation for the Treatment of Secondary Arm Lymphedema: A Prospective Controlled Study in Patients with Breast Cancer Related Lymphedema. Jpn. J. Clin. Oncol. 2008, 38, 670–674. [Google Scholar] [CrossRef]
- Maldonado, G.E.M.; Pérez, C.A.A.; Covarrubias, E.E.A.; Cabriales, S.A.M.; Leyva, L.A.; Pérez, J.C.J.; Almaguer, D.G. Autologous stem cells for the treatment of post-mastectomy lymphedema: A pilot study. Cytotherapy 2011, 13, 1249–1255. [Google Scholar] [CrossRef]
- Toyserkani, N.M.; Jensen, C.H.; Andersen, D.C.; Sheikh, S.P.; Sørensen, J.A. Treatment of Breast Cancer-Related Lymphedema with Adipose-Derived Regenerative Cells and Fat Grafts: A Feasibility and Safety Study. STEM CELLS Transl. Med. 2017, 6, 1666–1672. [Google Scholar] [CrossRef]
- Toyserkani, N.; Jensen, C.H.; Tabatabaeifar, S.; Jørgensen, M.; Hvidsten, S.; Simonsen, J.A.; Andersen, D.C.; Sheikh, S.; Sørensen, J.A. Adipose-derived regenerative cells and fat grafting for treating breast cancer-related lymphedema: Lymphoscintigraphic evaluation with 1 year of follow-up. J. Plast. Reconstr. Aesthetic Surg. 2018, 72, 71–77. [Google Scholar] [CrossRef]
- Jørgensen, M.G.; Toyserkani, N.M.; Jensen, C.H.; Andersen, D.C.; Sheikh, S.P.; Sørensen, J.A. Adipose-derived regenerative cells and lipotransfer in alleviating breast cancer-related lymphedema: An open-label phase I trial with 4 years of follow-up. STEM CELLS Transl. Med. 2021, 10, 844–854. [Google Scholar] [CrossRef] [PubMed]
- Ismail, A.M.; Abdou, S.M.; AbdelNaby, A.Y.; Hamdy, M.; el Saka, A.; Gawaly, A. Stem Cell Therapy Using Bone Marrow-Derived Mononuclear Cells in Treatment of Lower Limb Lymphedema: A Randomized Controlled Clinical Trial. Lymphat. Res. Biol. 2018, 16, 270–277. [Google Scholar] [CrossRef] [PubMed]
- Ehyaeeghodraty, V.; Molavi, B.; Nikbakht, M.; Mohammadi, A.M.; Mohammadi, S.; Fallahi, B.; Mousavi, S.A.; Vaezi, M.; Sefidbakht, S.; Ehyaeeghodraty, N. Effects of mobilized peripheral blood stem cells on treatment of primary lower extremity lymphedema. J. Vasc. Surg. Venous Lymphat. Disord. 2019, 8, 445–451. [Google Scholar] [CrossRef]
- Hsu, J.F.; Yu, R.P.; Stanton, M.E.W.; Wang, M.J.; Wong, A.K. Current Advancements in Animal Models of Postsurgical Lymphedema: A Systematic Review. Adv. Wound Care 2021, 11, 399–418. [Google Scholar] [CrossRef]
- Jørgensen, M.G.; Toyserkani, N.M.; Hansen, C.R.; Hvidsten, S.; Baun, C.; Hejbøl, E.K.; Schrøder, H.D.; Sørensen, J.A. Quantification of Chronic Lymphedema in a Revised Mouse Model. Ann. Plast. Surg. 2018, 81, 594–603. [Google Scholar] [CrossRef]
- de Castro, L.L.; Lopes-Pacheco, M.; Weiss, D.J.; Cruz, F.F.; Rocco, P.R.M. Current understanding of the immunosuppressive properties of mesenchymal stromal cells. Klin. Wochenschr. 2019, 97, 605–618. [Google Scholar] [CrossRef] [PubMed]
- Dominici, M.; Le Blanc, K.; Mueller, I.; Slaper-Cortenbach, I.; Marini, F.C.; Krause, D.S.; Deans, R.J.; Keating, A.; Prockop, D.J.; Horwitz, E.M. Minimal criteria for defining multipotent mesenchymal stromal cells. The International Society for Cellular Therapy position statement. Cytotherapy 2006, 8, 315–317. [Google Scholar] [CrossRef]
- Viswanathan, S.; Shi, Y.; Galipeau, J.; Krampera, M.; Leblanc, K.; Martin, I.; Nolta, J.; Phinney, D.G.; Sensebe, L. Mesenchymal stem versus stromal cells: International Society for Cell & Gene Therapy (ISCT®) Mesenchymal Stromal Cell committee position statement on nomenclature. Cytotherapy 2019, 21, 1019–1024. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).