Molecular and Circulating Biomarkers of Gastric Cancer
Abstract
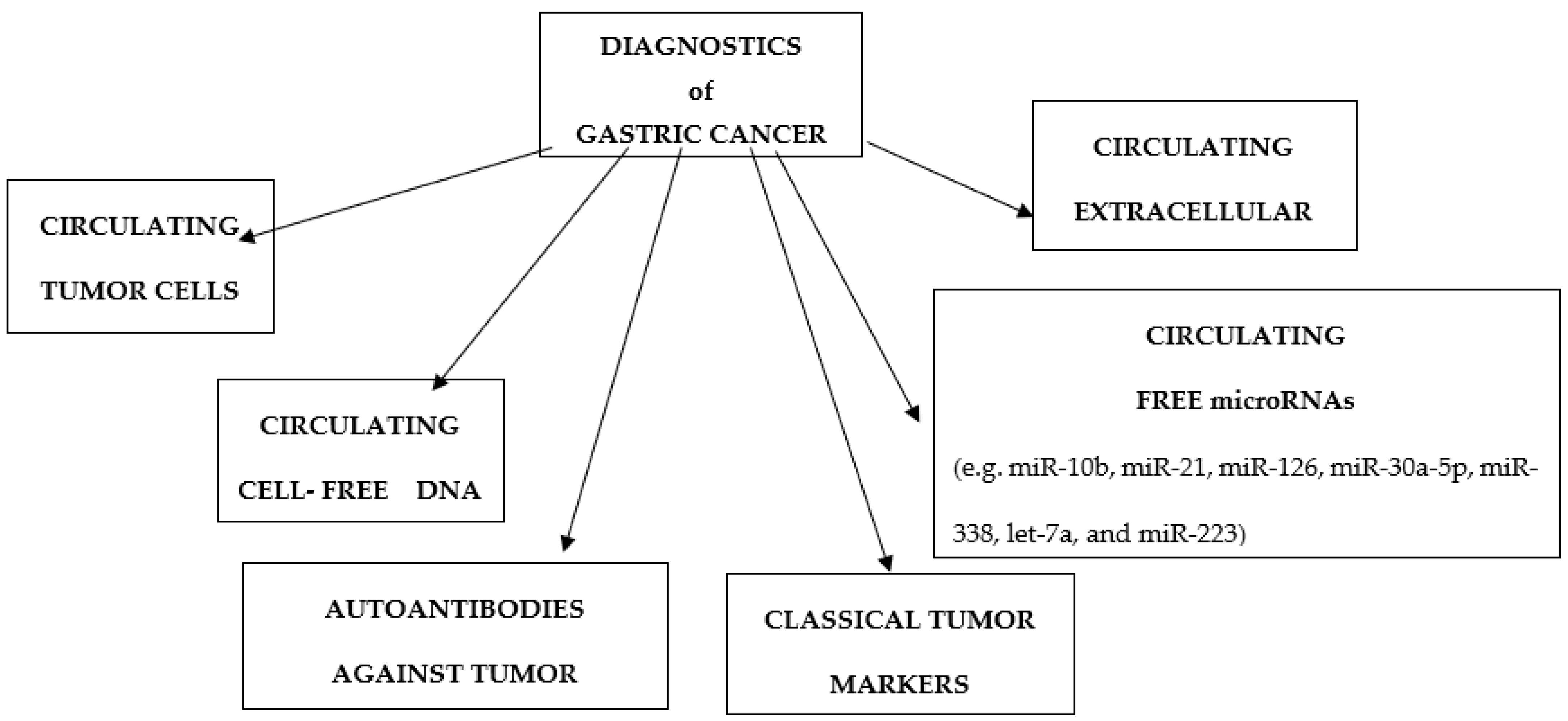
:1. Introduction
2. Classical Tumor Markers
2.1. Carcinoembryonic Antigen
2.2. Carbohydrate Antigen 19-9
2.3. Carbohydrate Antigen 72-4
2.4. Others Classical Tumor Markers
3. Circulating Tumor Cells
4. Circulating Free miRNA
5. Circulating Extracellular Vesicles
6. Circulating Cell-Free DNA
7. Autoantibodies against Tumor Associated Antigens
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Siegel, R.; Miller, K.D.; Jemal, A. Cancer statistics, 2019. CA A Cancer J. Clin. 2019, 69, 7–34. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Park, J.Y.; von Karsa, L.; Herrero, R. Prevention strategies for gastric cancer: A global perspective. Clin. Endosc. 2014, 47, 478–489. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, C.; Pinheiro, H.; Figueiredo, J.; Seruca, R.; Carneiro, F. Familial gastric cancer: Genetic susceptibility, pathology, and implications for management. Lancet Oncol. 2015, 16, e60–e70. [Google Scholar] [CrossRef]
- Hochwald, S.N.; Kim, S.; Klimstra, D.S.; Brennan, M.F.; Karpeh, M.S. Analysis of 154 actual five-year survivors of gastric cancer. J. Gastrointest. Surg. 2000, 4, 520–552. [Google Scholar] [CrossRef]
- Smyth, E.C.; Cunningham, D. Gastric cancer in 2012: Defining treatment standards and novel insights into disease biology. Nat. Rev. Clin. Oncol. 2013, 10, 73–74. [Google Scholar] [CrossRef]
- Zheng, T.H.; Zhao, J.L.; Guleng, B. Advances in molecular biomarkers for gastric cancer. Crit. Rev. Eukaryot. Gene Expr. 2015, 25, 299–305. [Google Scholar] [CrossRef]
- Matsuoka, T.; Yashiro, M. Biomarkers of gastric cancer: Current topics and future perspective. World J. Gastroenterol. 2018, 24, 2818–2832. [Google Scholar] [CrossRef]
- Allgayer, H.; Heiss, M.M.; Schildberg, F.W. Prognostic factors in gastric cancer. Br. J. Surg. 1997, 84, 1651–1664. [Google Scholar]
- Kalniņa, Z.; Meistere, I.; Kikuste, I.; Tolmanis, I.; Zayakin, P.; Linē, A. Emerging blood-based biomarkers for detection of gastric cancer. World J. Gastroenterol. 2015, 21, 11636–11653. [Google Scholar] [CrossRef]
- Konstantopoulos, K.; Thomas, S.N. Cancer cells in transit: The vascular interactions of tumor cells. Annu. Rev. Biomed. Eng. 2009, 11, 177–202. [Google Scholar] [CrossRef]
- Zhang, Y.S.; Xu, J.; Luo, G.H.; Wang, R.C.; Zhu, J.; Zhang, X.Y.; Nilsson-Ehle, P.; Xu, N. Detection of carcinoembryonic antigen mRNA in peritoneal washes from gastric cancer patients and its clinical significance. World J. Gastroenterol. 2006, 12, 1408–1411. [Google Scholar] [CrossRef] [PubMed]
- Marrelli, D.; Pinto, E.; De Stefano, A.; Farnetani, M.; Garosi, L.; Roviello, F. Clinical utility of CEA, CA 19-9, and CA 72-4 in the follow-up of patients with resectable gastric cancer. Am. J. Surg. 2001, 181, 16–19. [Google Scholar] [CrossRef]
- Song, Y.X.; Liu, K.; Yang, S.-J.; Zhang, W.-H.; Chen, X.-L.; Zhao, L.-Y.; Chen, X.-Z.; Yang, K.; Zhou, Z.-G.; Hu, J.-K. Prognostic value of changes in preoperative and postoperative serum CA 19-9 levels in gastric cancer. Front. Oncol. 2020, 10, 1432–1440. [Google Scholar] [CrossRef] [PubMed]
- Louhimo, J.; Kokkola, A.; Alfthan, H.; Stenman, U.H.; Haglund, C. Preoperative hCGbeta and CA 72-4 are prognostic factors in gastric cancer. Int. J. Cancer 2004, 111, 929–933. [Google Scholar] [CrossRef]
- Tsai, M.-M.; Wang, C.-S.; Tsai, C.-Y.; Chi, Y.-C.; Tseng, Y.-H.; Lin, K.-H. Potential prognostic, diagnostic and therapeutic markers for human gastric cancer. World J. Gastroenterol. 2014, 20, 13791–13803. [Google Scholar] [CrossRef]
- Gong, W.; Su, Y.; Liu, A.; Liu, J.; Sun, D.; Jiang, T.; Xiang, J.; Chi, C.; Sun, P. Clinical characteristics and treatments of patients with alpha-fetoprotein producing gastric carcinoma. Neoplasma 2018, 65, 326–330. [Google Scholar] [CrossRef]
- Namikawa, T.; Kawanishi, Y.; Fujisawa, K.; Munekage, E.; Iwabu, J.; Munekage, M.; Maeda, H.; Kitagawa, H.; Kobayashi, M.; Hamazaki, K. Serum carbohydrate antigen 125 is a significant prognostic marker in patients with unresectable advanced or recurrent gastric cancer. Surg. Endosc. 2018, 32, 1749–1754. [Google Scholar] [CrossRef]
- Feng, F.; Tian, Y.; Xu, G.; Liu, Z.; Liu, S.; Zheng, G.; Guo, M.; Lian, X.; Fan, D.; Zhang, H. Diagnostic and prognostic value of CEA, CA19-9, AFP and CA125 for early gastric cancer. BMC Cancer 2017, 17, 737–742. [Google Scholar] [CrossRef]
- Galletti, G.; Sung, M.S.; Vahdat, L.T.; Shah, M.A.; Santana, S.M.; Altavilla, G.; Kirby, B.J.; Giannakakou, P. Isolation of breast cancer and gastric cancer circulating tumor cells by use of an anti HER2-based microfluidic device. Lab Chip 2014, 14, 147–156. [Google Scholar] [CrossRef]
- Li, T.-T.; Liu, H.; Yu, J.; Shi, G.-Y.; Zhao, L.-Y.; Li, G.-X. Prognostic and predictive blood biomarkers in gastric cancer and the potential application of circulating tumor cells. World J. Gastroenterol. 2018, 24, 2236–2246. [Google Scholar] [CrossRef]
- Mimori, K.; Fukagawa, T.; Kosaka, Y.; Ishikawa, K.; Iwatsuki, M.; Yokobori, T.; Hirasaki, S.; Takatsuno, Y.; Sakashita, H.; Ishii, H.; et al. A large-scale study of MT1-MMP as a marker for isolated tumor cells in peripheral blood and bone marrow in gastric cancer cases. Ann. Surg. Oncol. 2008, 15, 2934–2942. [Google Scholar] [CrossRef] [PubMed]
- Uenosono, Y.; Arigami, T.; Kozono, T.; Yanagita, S.; Hagihara, T.; Haraguchi, N.; Matsushita, D.; Hirata, M.; Arima, H.; Funasako, Y.; et al. Clinical significance of circulating tumor cells in peripheral blood from patients with gastric cancer. Cancer 2013, 119, 3984–3991. [Google Scholar] [CrossRef] [PubMed]
- Matsusaka, S.; Chìn, K.; Ogura, M.; Suenaga, M.; Shinozaki, E.; Mishima, Y.; Terui, Y.; Mizunuma, N.; Hatake, K. Circulating tumor cells as a surrogate marker for determining response to chemotherapy in patients with advanced gastric cancer. Cancer Sci. 2010, 101, 1067–1071. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Ling, Y.; Qi, Q.; Lan, F.; Zhu, M.; Zhang, Y.; Bao, Y.; Zhang, C. Prognostic value of circulating tumor cells in advanced gastric cancer patients receiving chemotherapy. Mol. Clin. Oncol. 2017, 6, 235–242. [Google Scholar] [CrossRef] [Green Version]
- Pantel, K.; Speicher, M.R. The biology of circulating tumor cells. Oncogene 2016, 35, 1216–1224. [Google Scholar] [CrossRef]
- Finnegan, E.F.; Pasquinelli, A.E. MicroRNA biogenesis: Regulating the regulators. Crit. Rev. Biochem. Mol. Biol. 2013, 48, 51–68. [Google Scholar] [CrossRef] [Green Version]
- Heneghan, H.M.; Miller, N.; Kerin, M.J. MiRNAs as biomarkers and therapeutic targets in cancer. Curr. Opin. Pharmacol. 2010, 10, 543–550. [Google Scholar] [CrossRef]
- Li, X.; Zhang, Y.; Zhang, Y.; Ding, J.; Wu, K.; Fan, D. Survival prediction of gastric cancer by a seven-microRNA signature. Gut 2010, 59, 579–585. [Google Scholar] [CrossRef]
- Xiong, X.; Ren, H.Z.; Li, M.H.; Mei, J.H.; Wen, J.F.; Zheng, C.L. Down regulatedmiRNA-214 induces a cell cycle G1 arrest in gastric cancer cells by up-regulating the PTEN protein. Pathol. Oncol. Res. 2011, 17, 931–937. [Google Scholar] [CrossRef]
- Nishida, N.; Mimori, K.; Fabbri, M.; Yokobori, T.; Sudo, T.; Tanaka, F.; Shibata, K.; Ishii, H.; Doki, Y.; Mori, M. MicroRNA-125a-5p is an independent prognostic factor in gastric cancer and inhibits the proliferation of human gastric cancer cells in combination with trastuzumab. Clin. Cancer Res. 2011, 17, 2725–2733. [Google Scholar] [CrossRef] [Green Version]
- Feng, R.; Chen, X.; Yu, Y.; Su, L.; Yu, B.; Li, J.; Cai, Q.; Yan, M.; Liu, B.; Zhu, Z. miR-126 functions as a tumour suppressor in human gastric cancer. Cancer Lett. 2010, 298, 50–63. [Google Scholar] [CrossRef] [PubMed]
- Zheng, B.; Liang, L.; Wang, C.; Huang, S.; Cao, X.; Zha, R.; Liu, L.; Jia, D.; Tian, Q.; Wu, J.; et al. MicroRNA-148a suppresses tumor cell invasion and metastasis by downregulating ROCK1 in gastric cancer. Clin. Cancer Res. 2011, 17, 7574–7583. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Xu, Y.; Zhao, F.; Wang, Z.; Song, Y.; Luo, Y.; Zhang, X.; Jiang, L.; Sun, Z.; Miao, Z.; Xu, H. MicroRNA-335 acts as a metastasis suppressor in gastric cancer by targeting Bcl-w and specificity protein 1. Oncogene 2012, 31, 1398–1407. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, Y.Y.; Ye, Z.Y.; Zhao, Z.S.; Li, L.; Wang, Y.X.; Tao, H.Q.; Wang, H.J.; He, X.J. Clinicopathologic significance of miR-10b expression in gastric carcinoma. Hum. Pathol. 2013, 44, 1278–1285. [Google Scholar] [CrossRef] [PubMed]
- Ebert, M.S.; Neilson, J.R.; Sharp, P.A. MicroRNA sponges: Competitive inhibitors of small RNAs in mammalian cells. Nat. Methods 2007, 4, 721–726. [Google Scholar] [CrossRef]
- Chun-Zhi, Z.; Lei, H.; An-Ling, Z.; Yan-Chao, F.; Xiao, Y.; Guang-Xiu, W.; Zhi-Fan, J.; Pei-Yu, P.; Qing-Yu, Z.; Chun-Sheng, K. MicroRNA-221 and microRNA-222 regulate gastric carcinoma cell proliferation and radioresistance by targeting PTEN. BMC Cancer 2010, 10, 367. [Google Scholar] [CrossRef] [Green Version]
- Kanda, M.; Kodera, Y. Recent advances in the molecular diagnostics of gastric cancer. World J. Gastroenterol. 2015, 21, 9838–9852. [Google Scholar] [CrossRef]
- Hoshino, A.; Costa-Silva, B.; Shen, T.L. Tumour exosome integrins determine organotropic metastasis. Nature 2015, 527, 329–335. [Google Scholar] [CrossRef] [Green Version]
- Xu, R.; Rai, A.; Chen, M.S.; Suwakulsiri, W.; Greening, D.W.; Simpson, R.J. Extracellular vesicles in cancer—Implications for future improvements in cancer care. Nat. Rev. Clin. Oncol. 2018, 15, 617–638. [Google Scholar] [CrossRef]
- Becker, A.; Thakur, B.K.; Weiss, J.M.; Kim, H.S.; Peinado, H.; Lyden, D. Extracellular vesicles in cancer: Cell-to-cell mediators of metastasis. Cancer Cell. 2016, 30, 836–848. [Google Scholar] [CrossRef] [Green Version]
- Liu, Y.; Cao, X. Organotropic metastasis: Role of tumor exosomes. Cell Res. 2016, 26, 149–150. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wu, L.; Zhang, X.; Zhang, B.; Shi, H.; Yuan, X.; Sun, Y.; Pan, Z.; Qian, H.; Xu, W. Exosomes derived from gastric cancer cells activate NF-kappaB pathway in macrophages to promote cancer progression. Tumour. Biol. 2016, 37, 12169–12180. [Google Scholar] [CrossRef]
- Zocco, D.; Ferruzzi, P.; Cappello, F.; Kuo, W.P.; Fais, S. Extracellular vesicles as shuttles of tumor biomarkers and anti-tumor drugs. Front. Oncol. 2014, 4, 267–273. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fu, M.; Gu, J.; Jiang, P.; Qian, H.; Xu, W.; Zhang, X. Exosomes in gastric cancer: Roles, mechanisms, and applications. Mol. Cancer 2019, 18, 41–53. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, G.; Lin, H.; Tian, R.; Zhao, P.; Huang, Y.; Pang, X.; Zhao, L.; Cao, B. VEGFR-2 inhibitor Apatinib hinders endothelial cells progression triggered by irradiated gastric cancer cells-derived exosomes. J. Cancer 2018, 9, 4049–4057. [Google Scholar] [CrossRef]
- Zhao, R.; Zhang, Y.; Zhang, X.; Yang, Y.; Zheng, X.; Li, X.; Liu, Y.; Zhang, Y. Exosomal long noncoding RNA HOTTIP as potential novel diagnostic and prognostic biomarker test for gastric cancer. Mol. Cancer 2018, 17, 68–72. [Google Scholar] [CrossRef]
- Guo, X.; Lv, X.; Ru, Y.; Zhou, F.; Wang, N.; Xi, H.; Zhang, K.; Li, J.; Chang, R.; Xie, T.; et al. Circulating Exosomal gastric Cancer-associated Long noncoding RNA1 as a biomarker for early detection and monitoring progression of gastric Cancer: A multiphase study. JAMA Surg. 2020, 155, 572–579. [Google Scholar] [CrossRef]
- Yoon, J.H.; Ham, I.H.; Kim, O.; Ashktorab, H.; Smoot, D.T.; Nam, S.W. Gastrokine 1 protein is a potential theragnostic target for gastric cancer. Gastric. Cancer 2018, 21, 956–967. [Google Scholar] [CrossRef] [Green Version]
- Wei, S.; Peng, L.; Yang, J.; Sang, H.; Jin, D.; Li, X. Exosomal transfer of miR-15b-3p enhances tumorigenesis and malignant transformation through the DYNLT1/Caspase-3/Caspase-9 signaling pathway in gastric cancer. J. Exp. Clin. Cancer Res. 2020, 39, 32. [Google Scholar] [CrossRef] [Green Version]
- Chen, Z.; Xie, Y.; Chen, W.; Li, T.; Chen, X.; Liu, B. microRNA-6785-5p-loaded human umbilical cord mesenchymal stem cells-derived exosomes suppress angiogenesis and metastasis in gastric cancer via INHBA. Life Sci. 2021, 284, 119222. [Google Scholar] [CrossRef]
- Bai, M.; Li, J.; Yang, H.; Zhang, H.; Zhou, Z.; Deng, T.; Ba, Y. miR-135b delivered by gastric tumor Exosomes inhibits FOXO1 expression in endothelial cells and promotes angiogenesis. Mol. Ther. 2019, 27, 1772–1783. [Google Scholar] [CrossRef] [PubMed]
- Deng, T.; Zhang, H.; Yang, H.; Wang, H.; Bai, M.; Sun, W. Exosome miR-155 derived from gastric carcinoma promotes angiogenesis by targeting the c-MYB/VEGF Axis of endothelial cells. Mol. Ther. Nucleic. Acids. 2020, 19, 1449–1459. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Z.; Zhang, H.; Deng, T.; Ning, T.; Liu, R.; Liu, D. Exosomes carrying MicroRNA-155 target Forkhead box O3 of endothelial cells and promote angiogenesis in gastric cancer. Mol. Ther. Oncolytics 2019, 15, 223–233. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Du, J.; Liang, Y.; Li, J.; Zhao, J.M.; Wang, Z.N.; Lin, X.Y. Gastric Cancer cell-derived Exosomal microRNA-23a promotes angiogenesis by targeting PTEN. Front. Oncol. 2020, 10, 326. [Google Scholar] [CrossRef] [Green Version]
- Zhang, H.; Deng, T.; Liu, R.; Bai, M.; Zhou, L.; Wang, X. Exosome-delivered EGFR regulates liver microenvironment to promote gastric cancer liver metastasis. Nat. Commun. 2017, 8, 15016. [Google Scholar] [CrossRef] [Green Version]
- Li, Z.; Suo, B.; Long, G.; Gao, Y.; Song, J.; Zhang, M. Exosomal miRNA-16-5p derived from M1 macrophages enhances T cell-dependent immune response by regulating PD-L1 in gastric cancer. Front. Cell. Dev. Biol. 2020, 8, 572689. [Google Scholar] [CrossRef]
- Qi, Q.; Pan, Y.F.; Shen, J.J.; Gu, X.Q.; Han, S.W.; Liao, H.H.; Jiang, Y.Z.; Zhong, L.P. Circulating DNA for detection of gastric cancer. Eur. Rev. Med. Pharmacol. Sci. 2016, 20, 2558–2564. [Google Scholar]
- Beeharry, M.K.; Liu, W.-T.; Yan, M.; Zhu, Z.-G. New blood markers detection technology: A leap in the diagnosis of gastric cancer. World J. Gastroenterol. 2016, 22, 1202–1212. [Google Scholar] [CrossRef]
- Kolesnikova, E.V.; Tamkovich, S.N.; Bryzgunova, O.E.; Shelestyuk, P.I.; Permyakova, V.I.; Vlassov, V.V.; Tuzikov, A.S.; Laktionov, P.P.; Rykova, E.Y. Circulating DNA in the blood of gastric cancer patients. Ann. N. Y. Acad. Sci. 2008, 1137, 226–231. [Google Scholar] [CrossRef]
- Park, J.L.; Kim, H.J.; Choi, B.Y.; Lee, H.C.; Jang, H.R.; Song, K.S.; Noh, S.M.; Kim, S.Y.; Han, D.S.; Kim, Y.S. Quantitative analysis of cell-free DNA in the plasma of gastric cancer patients. Oncol. Lett. 2012, 3, 921–926. [Google Scholar]
- Kim, K.; Shin, D.G.; Park, M.K.; Baik, S.H.; Kim, T.H.; Kim, S.; Lee, S. Circulating cell-free DNA as a promising biomarker in patients with gastric cancer: Diagnostic validity and significant reduction of cfDNA after surgical resection. Ann. Surg. Treat. Res. 2014, 86, 136–142. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sai, S.; Ichikawa, D.; Tomita, H.; Ikoma, D.; Tani, N.; Ikoma, H.; Kikuchi, S.; Fujiwara, H.; Ueda, Y.; Otsuji, E. Quantification of plasma cell-free DNA in patients with gastric cancer. Anticancer Res. 2007, 27, 2747–2751. [Google Scholar] [PubMed]
- Balgkouranidou, I.; Matthaios, D.; Karayiannakis, A.; Bolanaki, H.; Michailidis, P.; Xenidis, N.; Amarantidis, K.; Chelis, L.; Trypsianis, G.; Chatzaki, E.; et al. Prognostic role of APC and RASSF1A promoter methylation status in cell free circulating DNA of operable gastric cancer patients. Mutat. Res. 2015, 778, 46–51. [Google Scholar] [CrossRef] [PubMed]
- Hamakawa, T.; Kukita, Y.; Kurokawa, Y.; Miyazaki, Y.; Takahashi, T.; Yamasaki, M.; Miyata, H.; Nakajima, K.; Taniguchi, K.; Takiguchi, S.; et al. Monitoring gastric cancer progression with circulating tumour DNA. Br. J. Cancer 2015, 112, 352–356. [Google Scholar] [CrossRef]
- Preuss, K.D.; Zwick, C.; Bormann, C.; Neumann, F.; Pfreundschuh, M. Analysis of the B-cell repertoire against antigens expressed by human neoplasms. Immunol. Rev. 2002, 188, 43–50. [Google Scholar] [CrossRef]
- Chapman, C.J.; Healey, G.F.; Murray, A.; Boyle, P.; Robertson, C.; Peek, L.J.; Allen, J.; Thorpe, A.J.; Hamilton-Fairley, G.; Parsy-Kowalska, C.B.; et al. EarlyCDT®-Lung test: Improved clinical utility through additional autoantibody assays. Tumour Biol. 2012, 33, 1319–1326. [Google Scholar] [CrossRef] [Green Version]
- Meistere, I.; Kalnina, Z.; Silina, K.; Line, A. Cancer-associated autoantibodies as biomarkers for early detection and prognosis is cancer: An update. Curr. Canc. Ther. Rev. 2013, 9, 10. [Google Scholar] [CrossRef]
- Werner, S.; Chen, H.; Tao, S.; Brenner, H. Systematic review: Serum autoantibodies in the early detection of gastric cancer. Int. J. Cancer 2015, 136, 2243–2252. [Google Scholar] [CrossRef] [Green Version]
- Wu, M.; Mao, C.; Chen, Q. Serum p53 protein and anti-p53 antibodies are associated with increased cancer risk: A case–control study of 569 patients and 879 healthy controls. Mol. Biol. Rep. 2010, 37, 339–343. [Google Scholar] [CrossRef]
- Zhang, J.Y.; Casiano, C.A.; Peng, X.X. Enhancement of antibody detection in cancer using panel of recombinant tumor-associated antigens. Cancer Epidemiol. Biomark. Prev. 2003, 12, 136–143. [Google Scholar]
- Xu, Q.W.; Zhao, W.; Wang, Y. An integrated genome-wide approach to discover tumor-specific antigens as potential immunologic and clinical targets in cancer. Cancer Res. 2012, 72, 6351–6361. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Meistere, I.; Werner, S.; Zayakin, P.; Siliņa, K.; Rulle, U.; Pismennaja, A.; Šantare, D.; Kikuste, I.; Isajevs, S.; Leja, M.; et al. The prevalence of cancer-associated autoantibodies in patients with gastric cancer and progressive grades of premalignant lesions. Cancer Epidemiol. Biomark. Prev. 2017, 26, 1564–1574. [Google Scholar] [CrossRef] [PubMed]
- Zayakin, P.; Ancāns, G.; Siliņa, K.; Meistere, I.; Kalniņa, Z.; Andrejeva, D.; Endzeliņš, E.; Ivanova, L.; Pismennaja, A.; Ruskule, A.; et al. Tumor-associated autoantibody signature for the early detection of gastric cancer. Int. J. Cancer 2013, 132, 137–147. [Google Scholar] [CrossRef]
- Zhou, S.L.; Ku, J.W.; Fan, Z.M.; Yue, W.B.; Du, F.; Zhou, Y.F.; Liu, Y.L.; Li, Y.; Tang, S.; Hu, Y.L.; et al. Detection of autoantibodies to a panel of tumor-associated antigens for the diagnosis values of gastric cardia adenocarcinoma. Dis. Esophagus 2015, 28, 371–379. [Google Scholar] [CrossRef] [PubMed]
- Schreiber, R.D.; Old, L.J.; Smyth, M.J. Cancer immunoediting: Integrating immunity’s roles in cancer suppression and promotion. Science 2011, 331, 1565–1570. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Leja, M.; Line, A. Early detection of gastric cancer beyond endoscopy-new methods. Best Pract. Res. Clin. Gastroenterol. 2021, 50–51, 101731. [Google Scholar] [CrossRef] [PubMed]
| Group/Markers | Significance | Study |
|---|---|---|
| Classical tumor markers | ||
| carcino-embryonic antigen (CEA) | Prognostic biomarker | [10,11] |
| carbohydrate antigen (CA 19-9) | Prognostic biomarker | [12,13] |
| carbohydrate antigen 72-4 (CA72-4) | Prognostic biomarker | [14] |
| Circulating tumor cells | Prognostic and monitoring biomarker Chemotherapy response | [20–24] |
| Circulating free microRNAs | Diagnosis, metastasis, monitoring response to treatment | [27–34] |
| Circulating extracellular vesicles | Diagnosis and prognostic biomarker | [43–46] |
| Circulating free DNA | Diagnosis and monitoring response to treatment | [47–53] |
| Autoantibodies against tumor associated antigens | Diagnosis and monitoring response to treatment | [58–61] |
| Symbol | Location | Materials | Function | Biomarker |
|---|---|---|---|---|
| miRNA-21 | (17q23.1) | Circulation | Cell proliferation, invasion | Early detection |
| miRNA-22 | (17p13.3) | Tissue | Proliferation, migration, invasion | Early detection |
| miRNA-29c | (1q32.2) | Tissue | Proliferation, adhesion, invasion | Early detection |
| miRNA-141 | 12p13.31) | Tissue | migration | Early detection |
| miRNA-191 | (3p21.31) | Tissue, circulation | Proliferation, adhesion, invasion | Early detection |
| miRNA-26a | (3p22.2) | Tissue | Proliferation, migration, invasion, cell cycle | Monitoring recurrences |
| miRNA-185 | (22q11.2) | Tissue | Proliferation, metastasis | Monitoring recurrences |
| miRNA-196a | (17q21.32) | Tissue, circulation | Proliferation, metastasis | Monitoring recurrences |
| miRNA-25 | (7q22.1) | Tissue, circulation | Migration, invasion | Prediction of survival |
| miRNA-183 | (7q32.2) | Tissue | Proliferation, migration, invasion | Prediction of survival |
| miRNA-192 | (11q13.1) | Tissue | Proliferation, migration, invasion | Prediction of survival |
| miRNA-17-5p | (13q31.3) | Circulating | Apoptosis, proliferation, migration, invasion | Prediction of treatment response |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jelski, W.; Mroczko, B. Molecular and Circulating Biomarkers of Gastric Cancer. Int. J. Mol. Sci. 2022, 23, 7588. https://doi.org/10.3390/ijms23147588
Jelski W, Mroczko B. Molecular and Circulating Biomarkers of Gastric Cancer. International Journal of Molecular Sciences. 2022; 23(14):7588. https://doi.org/10.3390/ijms23147588
Chicago/Turabian StyleJelski, Wojciech, and Barbara Mroczko. 2022. "Molecular and Circulating Biomarkers of Gastric Cancer" International Journal of Molecular Sciences 23, no. 14: 7588. https://doi.org/10.3390/ijms23147588
APA StyleJelski, W., & Mroczko, B. (2022). Molecular and Circulating Biomarkers of Gastric Cancer. International Journal of Molecular Sciences, 23(14), 7588. https://doi.org/10.3390/ijms23147588







