Role of Intrinsic Subtype Analysis with PAM50 in Hormone Receptors Positive HER2 Negative Metastatic Breast Cancer: A Systematic Review
Abstract
:1. Introduction
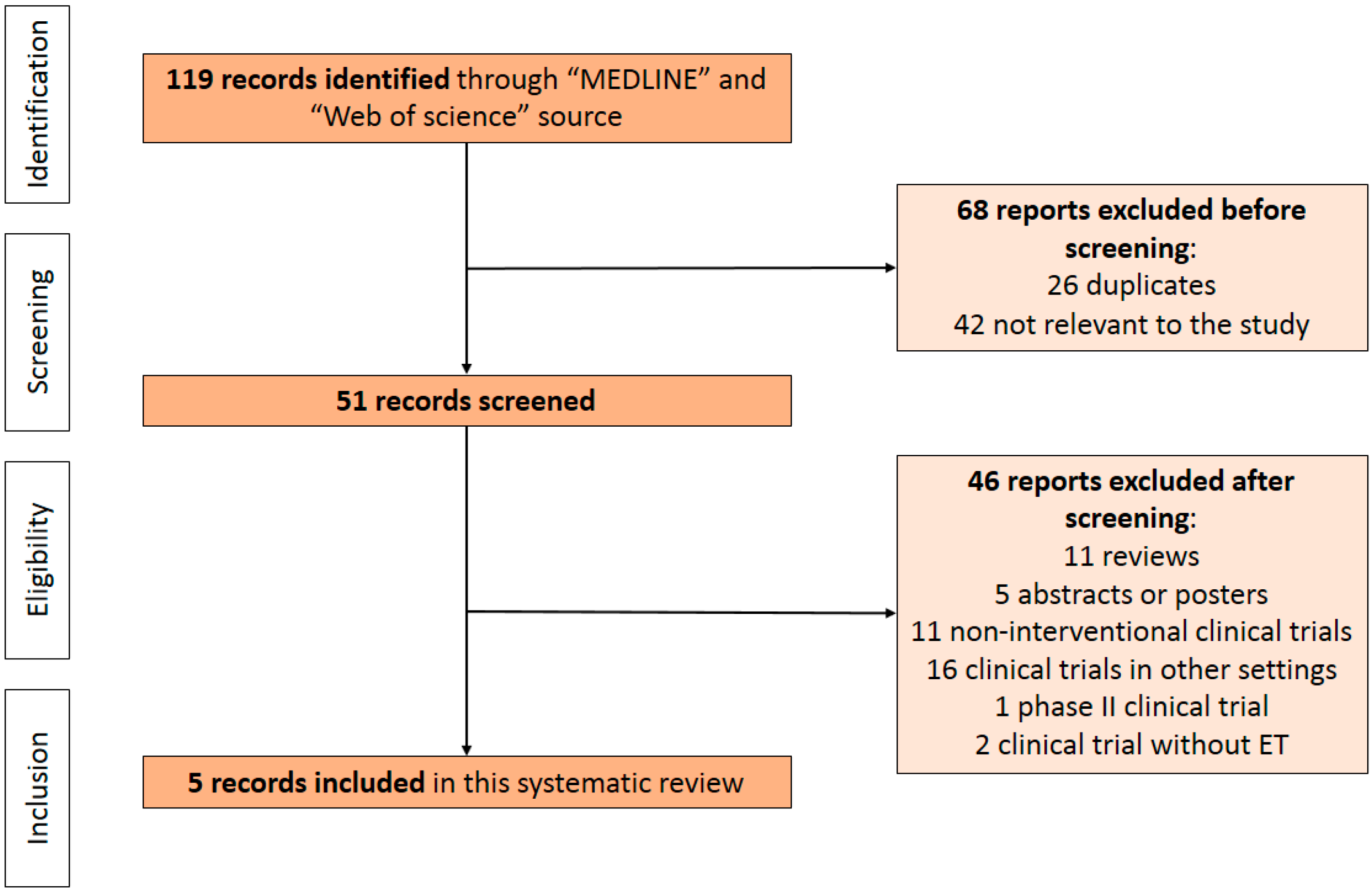
2. Methods
2.1. Data Sources and Search Strategy
2.2. Elegibility Criteria
3. Results
4. Discussion
5. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Malmgren, J.A.; Mayer, M.; Atw ood, M.K.; Kaplan, H.G. Differential presentation and survival of de novo and recurrent metastatic breast cancer over time: 1990–2010. Breast Cancer Res. Treat. 2017, 167, 579–590. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cardoso, F.; Paluch-Shimon, S.; Senkus, E.; Curigliano, G.; Aapro, M.S.; André, F.; Barrios, C.H.; Bergh, J.; Bhattacharyya, G.S.; Biganzoli, L.; et al. 5th ESO-ESMO international consensus guidelines for advanced breast cancer (ABC 5). Ann. Oncol. 2020, 31, 1623–1649. [Google Scholar] [CrossRef] [PubMed]
- Parker, J.S.; Mullins, M.; Cheang, M.C.U.; Leung, S.; Voduc, D.; Vickery, T.; Davies, S.; Fauron, C.; He, X.; Hu, Z.; et al. Supervised Risk Predictor of Breast Cancer Based on Intrinsic Subtypes. J. Clin. Oncol. 2009, 27, 1160–1167. [Google Scholar] [CrossRef] [PubMed]
- Prat, A.; Parker, J.S.; Fan, C.; Perou, C.M. PAM50 assay and the three-gene model for identifying the major and clinically relevant molecular subtypes of breast cancer. Breast Cancer Res. Treat. 2012, 135, 301–306. [Google Scholar] [CrossRef] [Green Version]
- Prat, A.; Perou, C.M. Deconstructing the molecular portraits of breast cancer. Mol. Oncol. 2010, 5, 5–23. [Google Scholar] [CrossRef]
- Prat, A.; Pineda, E.; Adamo, B.; Galván, P.; Fernandez-Martinez, A.; Gaba, L.; Díez, M.; Viladot, M.; Arance, A.; Munoz, M. Clinical implications of the intrinsic molecular subtypes of breast cancer. Breast 2015, 24, S26–S35. [Google Scholar] [CrossRef] [Green Version]
- Dunbier, A.K.; Anderson, H.; Ghazoui, Z.; Salter, J.; Parker, J.S.; Perou, C.M.; Smith, I.E.; Dowsett, M. Association between breast cancer subtypes and response to neoadjuvant anastrozole. Steroids 2011, 76, 736–740. [Google Scholar] [CrossRef]
- Ellis, M.J.; Suman, V.J.; Hoog, J.; Lin, L.; Snider, J.; Prat, A.; Parker, J.S.; Luo, J.; DeSchryver, K.; Allred, D.C.; et al. Randomized Phase II Neoadjuvant Comparison Between Letrozole, Anastrozole, and Exemestane for Postmenopausal Women With Estrogen Receptor–Rich Stage 2 to 3 Breast Cancer: Clinical and Biomarker Outcomes and Predictive Value of the Baseline PAM50-Based Intrinsic Subtype—ACOSOG Z1031. J. Clin. Oncol. 2011, 29, 2342–2349. [Google Scholar] [CrossRef] [Green Version]
- Prat, A.; Fan, C.; Fernandez-Martinez, A.; Hoadley, K.; Martinello, R.; Vidal, M.; Viladot, M.; Pineda, E.; Arance, A.; Munoz, M.; et al. Response and survival of breast cancer intrinsic subtypes following multi-agent neoadjuvant chemotherapy. BMC Med. 2015, 13, 303. [Google Scholar] [CrossRef] [Green Version]
- Prat, A.; Parker, J.S.; Fan, C.; Cheang, M.C.U.; Miller, L.D.; Bergh, J.; Chia, S.K.L.; Bernard, P.S.; Nielsen, T.O.; Ellis, M.J.; et al. Concordance among gene expression-based predictors for ER-positive breast cancer treated with adjuvant tamoxifen. Ann. Oncol. 2012, 23, 2866–2873. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 88, 105906. [Google Scholar] [CrossRef]
- Prat, A.; Cheang, M.C.U.; Galván, P.; Nuciforo, P.; Paré, L.; Adamo, B.; Muñoz, M.; Viladot, M.; Press, M.F.; Gagnon, R.; et al. Prognostic Value of Intrinsic Subtypes in Hormone Receptor–Positive Metastatic Breast Cancer Treated With Letrozole With or Without Lapatinib. JAMA Oncol. 2016, 2, 1287–1294. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Johnston, S.; Pippen, J.; Pivot, X.; Lichinitser, M.; Sadeghi, S.; Dieras, V.; Gomez, H.L.; Romieu, G.; Manikhas, A.; Kennedy, M.J.; et al. Lapatinib Combined with Letrozole Versus Letrozole and Placebo As First-Line Therapy for Postmenopausal Hormone Receptor–Positive Metastatic Breast Cancer. J. Clin. Oncol. 2009, 27, 5538–5546. [Google Scholar] [CrossRef] [Green Version]
- Prat, A.; Brase, J.C.; Cheng, Y.; Nuciforo, P.; Paré, L.; Pascual, T.; Martínez, D.; Galván, P.; Vidal, M.; Adamo, B.; et al. Everolimus plus Exemestane for Hormone Receptor-Positive Advanced Breast Cancer: A PAM50 Intrinsic Subtype Analysis of BOLERO-2. Oncologist 2019, 24, 893–900. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Baselga, J.; Campone, M.; Piccart, M.; Burris, H.A., III; Rugo, H.S.; Sahmoud, T.; Noguchi, S.; Gnant, M.; Pritchard, K.I.; Lebrun, F.; et al. Everolimus in Postmenopausal Hormone-Receptor–Positive Advanced Breast Cancer. N. Engl. J. Med. 2012, 366, 520–529. [Google Scholar] [CrossRef] [Green Version]
- Yardley, D.A.; Noguchi, S.; Pritchard, K.I.; Burris, H.A., III; Baselga, J.; Gnant, M.; Hortobagyi, G.N.; Campone, M.; Pistilli, B.; Piccart, M.; et al. Everolimus Plus Exemestane in Postmenopausal Patients with HR+ Breast Cancer: BOLERO-2 Final Progression-Free Survival Analysis. Adv. Ther. 2013, 30, 870–884. [Google Scholar] [CrossRef] [Green Version]
- Turner, N.C.; Liu, Y.; Zhu, Z.; Loi, S.; Colleoni, M.; Loibl, S.; DeMichele, A.; Harbeck, N.; André, F.; Bayar, M.A.; et al. Cyclin E1 Expression and Palbociclib Efficacy in Previously Treated Hormone Receptor–Positive Metastatic Breast Cancer. J. Clin. Oncol. 2019, 37, 1169–1178. [Google Scholar] [CrossRef]
- Turner, N.C.; Ro, J.; André, F.; Loi, S.; Verma, S.; Iwata, H.; Harbeck, N.; Loibl, S.; Bartlett, C.H.; Zhang, K.; et al. Palbociclib in Hormone-Receptor–Positive Advanced Breast Cancer. N. Engl. J. Med. 2015, 373, 209–219. [Google Scholar] [CrossRef] [Green Version]
- Cristofanilli, M.; Turner, N.C.; Bondarenko, I.; Ro, J.; Im, S.-A.; Masuda, N.; Colleoni, M.; DeMichele, A.; Loi, S.; Verma, S.; et al. Fulvestrant plus palbociclib versus fulvestrant plus placebo for treatment of hormone-receptor-positive, HER2-negative metastatic breast cancer that progressed on previous endocrine therapy (PALOMA-3): Final analysis of the multicentre, double-blind, phase 3 randomised controlled trial. Lancet Oncol. 2016, 17, 425–439. [Google Scholar] [CrossRef] [Green Version]
- Finn, R.S.; Liu, Y.; Zhu, Z.; Martin, M.; Rugo, H.S.; Diéras, V.; Im, S.-A.; Gelmon, K.A.; Harbeck, N.; Lu, D.R.; et al. Biomarker Analyses of Response to Cyclin-Dependent Kinase 4/6 Inhibition and Endocrine Therapy in Women with Treatment-Naïve Metastatic Breast Cancer. Clin. Cancer Res. 2020, 26, 110–121. [Google Scholar] [CrossRef] [Green Version]
- Finn, R.S.; Martin, M.; Rugo, H.S.; Jones, S.; Im, S.-A.; Gelmon, K.; Harbeck, N.; Lipatov, O.N.; Walshe, J.M.; Moulder, S.; et al. Palbociclib and Letrozole in Advanced Breast Cancer. N. Engl. J. Med. 2016, 375, 1925–1936. [Google Scholar] [CrossRef] [PubMed]
- Rugo, H.S.; Finn, R.S.; Diéras, V.; Ettl, J.; Lipatov, O.; Joy, A.A.; Harbeck, N.; Castrellon, A.; Iyer, S.; Lu, D.R.; et al. Palbociclib plus letrozole as first-line therapy in estrogen receptor-positive/human epidermal growth factor receptor 2-negative advanced breast cancer with extended follow-up. Breast Cancer Res. Treat. 2019, 174, 719–729. [Google Scholar] [CrossRef] [Green Version]
- Prat, A.; Chaudhury, A.; Solovieff, N.; Paré, L.; Martinez, D.; Chic, N.; Martínez-Sáez, O.; Brasó-Maristany, F.; Lteif, A.; Taran, T.; et al. Correlative Biomarker Analysis of Intrinsic Subtypes and Efficacy Across the MONALEESA Phase III Studies. J. Clin. Oncol. 2021, 39, 1458–1467. [Google Scholar] [CrossRef] [PubMed]
- Hortobagyi, G.N.; Stemmer, S.M.; Burris, H.A.; Yap, Y.S.; Sonke, G.S.; Paluch-Shimon, S.; Campone, M.; Blackwell, K.L.; Andre, F.; Winer, E.P.; et al. Ribociclib as First-Line Therapy for HR-Positive, Advanced Breast Cancer. N. Engl. J. Med. 2018, 379, 2582. [Google Scholar] [CrossRef]
- Hortobagyi, G.; Stemmer, S.; Burris, H.; Yap, Y.-S.; Sonke, G.; Paluch-Shimon, S.; Campone, M.; Petrakova, K.; Blackwell, K.; Winer, E.; et al. Updated results from MONALEESA-2, a phase III trial of first-line ribociclib plus letrozole versus placebo plus letrozole in hormone receptor-positive, HER2-negative advanced breast cancer. Ann. Oncol. 2019, 30, 1842. [Google Scholar] [CrossRef] [PubMed]
- Slamon, D.J.; Neven, P.; Chia, S.; Fasching, P.A.; De Laurentiis, M.; Im, S.A.; Petrakova, K.; Bianchi, G.V.; Esteva, F.J.; Martín, M.; et al. Phase III Randomized Study of Ribociclib and Fulvestrant in Hormone Re-ceptor-Positive, Human Epidermal Growth Factor Receptor 2-Negative Advanced Breast Cancer: MONALEESA-3. J. Clin. Oncol. 2018, 36, 2465–2472. [Google Scholar] [CrossRef]
- Slamon, D.J.; Neven, P.; Chia, S.; Fasching, P.A.; De Laurentiis, M.; Im, S.-A.; Petrakova, K.; Bianchi, G.V.; Esteva, F.J.; Martín, M.; et al. Overall Survival with Ribociclib plus Fulvestrant in Advanced Breast Cancer. N. Engl. J. Med. 2020, 382, 514–524. [Google Scholar] [CrossRef]
- Tripathy, D.; Im, S.-A.; Colleoni, M.; Franke, F.; Bardia, A.; Harbeck, N.; Hurvitz, S.A.; Chow, L.; Sohn, J.; Lee, K.S.; et al. Ribociclib plus endocrine therapy for premenopausal women with hormone-receptor-positive, advanced breast cancer (MONALEESA-7): A randomised phase 3 trial. Lancet Oncol. 2018, 19, 904–915. [Google Scholar] [CrossRef]
- Im, S.-A.; Lu, Y.-S.; Bardia, A.; Harbeck, N.; Colleoni, M.; Franke, F.; Chow, L.; Sohn, J.; Lee, K.-S.; Campos-Gomez, S.; et al. Overall Survival with Ribociclib plus Endocrine Therapy in Breast Cancer. N. Engl. J. Med. 2019, 381, 307–316. [Google Scholar] [CrossRef]
- Lee, S.; Park, K.; Kim, G.M.; Jung, K.H.; Kang, S.Y.; Park, I.H.; Kim, J.H.; Ahn, H.K.; Park, W.-Y.; Im, S.-A.; et al. Exploratory analysis of biomarkers associated with clinical outcomes from the study of palbociclib plus endocrine therapy in premenopausal women with hormone receptor-positive, HER2-negative metastatic breast cancer. Breast 2022, 62, 52–60. [Google Scholar] [CrossRef]
- Guarneri, V.; Giovannelli, S.; Ficarra, G.; Bettelli, S.; Maiorana, A.; Piacentini, F.; Barbieri, E.; Dieci, M.V.; D’Amico, R.; Jovic, G.; et al. Comparison of HER-2 and Hormone Receptor Expression in Primary Breast Cancers and Asynchronous Paired Metastases: Impact on Patient Management. Oncologist 2008, 13, 838–844. [Google Scholar] [CrossRef] [PubMed]
- Cheang, M.C.U.; Chia, S.K.; Voduc, D.; Gao, D.; Leung, S.; Snider, J.; Watson, M.; Davies, S.; Bernard, P.S.; Parker, J.S.; et al. Ki67 Index, HER2 Status, and Prognosis of Patients with Luminal B Breast Cancer. JNCI J. Natl. Cancer Inst. 2009, 101, 736–750. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cejalvo, J.M.; de Dueñas, E.M.; Galván, P.; García-Recio, S.; Gasión, O.B.; Paré, L.; Antolín, S.; Martinello, R.; Blancas, I.; Adamo, B.; et al. Intrinsic Subtypes and Gene Expression Profiles in Primary and Metastatic Breast Cancer. Cancer Res. 2017, 77, 2213–2221. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pommier, R.M.; Sanlaville, A.; Tonon, L.; Kielbassa, J.; Thomas, E.; Ferrari, A.; Sertier, A.-S.; Hollande, F.; Martinez, P.; Tissier, A.; et al. Comprehensive characterization of claudin-low breast tumors reflects the impact of the cell-of-origin on cancer evolution. Nat. Commun. 2020, 11, 3431. [Google Scholar] [CrossRef]
| A | |||||||
| EGF30008 [13] HR+/HER2- pts (n = 644) | |||||||
| % (n°) Overall Population | mPFS (Months) Overall Population | mPFS (Months) ET + LAPATINIB | mPFS (Months) ET + PBO | ||||
| Lum A | 52 (335) | 16.9 (95% CI, 14.1–19.9) | NA | NA | |||
| Lum B | 30 (196) | 11.0 (95% CI, 9.6–13.6) | NA | NA | |||
| HER2E | 3 (16) | 4.7 (95% CI, 2.7–10.8) | NA | NA | |||
| Basal-like | 3 (21) | 4.1 (95% CI, 2.5–13.8) | NA | NA | |||
| Normal-like | 12 (76) | NA | NA | NA | |||
| B | |||||||
| PALOMA-2 [21] All pts (n = 455) | |||||||
| % (n°) Overall Population | mPFS (Months) Overall Population | mPFS (Months) LETRO + PALB | mPFS (Months) LETRO + PBO | HR | |||
| Lum A | 50.3 (229) | NA | 30.4 | 17.0 | 0.55 (95% CI, 0.39–0.77; p = 0.0005) | ||
| Lum B | 29.7 (135) | NA | 16.9 | 11.0 | 0.51 (95% CI, 0.34–0.77; p = 0.0019) | ||
| HER2E | 18.7 (85) | NA | NA | NA | NA | ||
| Basal-like | 0.5 (2) | NA | NA | NA | NA | ||
| Normal-like | 0.9 (4) | NA | NA | NA | NA | ||
| C | |||||||
| BOLERO-2 [15] All pts (n = 261) | |||||||
| % (n°) Overall Population | % (n°) Primary Tumors (n = 209#) | % (n°) Metastasis (N = 50#) | mPFS (Months) Overall Population | mPFS (Months) EXE + EVE | mPFS (Months) EXE + PBO | HR | |
| Lum A | 46.7 (122) | 48.3 (101) | 40.0 (20) | 6.2 (95% CI, 4.37–8.31) | 8.3 (95% CI, 5.59–11.10) | 4.1 (95% CI, 2.63–5.26) | 0.39 (95% CI, 0.25–0.61; p < 0.0001) |
| Lum B | 15.7 (41) | 14.8 (31) | 20.0 (10) | 5.4 (95% CI, 4.04–8.05) | 6.8 (95% CI, 4.11–11.70) | 2.8 (95% CI, 1.48–7.13) | 0.69 (95% CI, 0.34–1.39; p = 0.349) |
| HER2E | 21.5 (56) | 18.7 (39) | 32.0 (16) | 5.2 (95% CI, 3.91–6.70) | 5.8 (95% CI, 3.91–7.36) | 4.1 (95% CI, 1.74–5.29) | 0.49 (95% CI, 0.26–0.90; p = 0.034) |
| Basal-like | 1.9 (5) | 1.9 (4) | 2.0 (1) | 3.2 (95% CI, 1.51 to no result) | NA | NA | NA |
| Normal-like | 14.2 (37) | 16.3 (34) | 6.0 (3) | 6.8 (95% CI, 4.07–11.07) | NA | NA | NA |
| All Luminals | 62.4 (163) | 63.1 (132) | 60.0 (30) | 6.7 (95% CI, 4.40–8.05) | 8.7 (95% CI, 6.67–11.07) | 4.1 (95% CI, 2.66–4.37) | 0.37 (95% CI, 0.26–0.52; p < 0.0001) |
| All Non-luminals | 37.6 (98) | 36.9 (77) | 40.0 (20) | 5.2 (95% CI, 3.45–6.70) | 5.8 (95% CI, 3.91–8.18) | 4.1 (95% CI, 2.76–5.29) | 0.47 (95% CI, 0.26–0.85; p = 0.027) |
| D | |||||||
| BOLERO-2 [15] All pts (n = 261) | |||||||
| % (n°) Overall Population | mPFS (Months) Overall Population | mPFS (Months) FULV + PALB | mPFS (Months) FULV + PBO | HR | |||
| Lum A | 44.0 (133) | NA | 16.6 | 4.8 | 0.41 (95% CI, 0.25–0.66) | ||
| Lum B | 30.8 (93) | NA | 9.2 | 3.5 | 0.64 (95% CI, 0.38–1.09) | ||
| HER2E | 20.9 (63) | NA | NA | NA | NA | ||
| Basal-like | 1.7 (5) | NA | NA | NA | NA | ||
| Normal-like | 2.6 (8) | NA | NA | NA | NA | ||
| All Non-luminals | 25.2 (76) | NA | 9.5 | 5.5 | 0.58 (95% CI, 0.34–0.99) | ||
| E | |||||||
| MONALEESA-2 [24] | MONALEESA-3 [26] | MONALEESA-7 [28] | |||||
| All pts (n = 358) | All pts (n = 489) | All pts (n = 313) | |||||
| % (n°) | % (n°) | % (n°) | |||||
| Lum A | 50.0 (179) | 48.7 (238) | 39.9 (125) | ||||
| Lum B | 28.8 (103) | 19.6 (96) | 25.2 (79) | ||||
| HER2E | 7.5 (27) | 14.9 (73) | 15.0 (47) | ||||
| Basal-like | 2.5 (9) | 1.4 (7) | 4.5 (14) | ||||
| Normal-like | 11.2 (40) | 15.3 (75) | 15.3 (48) | ||||
| F | |||||||
| All MONALEESA Trials [23] All pts (n = 1160) | |||||||
| % (n°) Overall Population | % (n°) Primary tumors (n = 835) | % (n°) Metastasis (N = 325) | mPFS (Months) Overall Population | mPFS (Months) ET + RIBO | mPFS (Months) ET + PBO | HR | |
| Lum A | 46.7 (542) | 49.9 (417) | 38.1 (124) | NA | 29.60 (95% CI, 23.03 to no result) | 19.48 (95% CI, 15.61–24.80) | 0.63 (95% CI, 0.49–0.83; p < 0.001) |
| Lum B | 24.0 (278) | 21.7 (181) | 30.5 (99) | NA | 22.21 (95% CI, 18.79 to no result) | 12.85 (95% CI, 10.84–14.82) | 0.52 (95% CI, 0.38–0.72; p < 0.001) |
| HER2E | 12.7 (147) | 11.2 (93) | 16.8 (55) | NA | 16.39 (95% CI, 12.71–24.60) | 5.52 (95% CI, 3.12–9.17) | 0.39 (95% CI, 0.25–0.60; p < 0.001) |
| Basal-like | 2.6 (30) | 2.4 (20) | 2.9 (9) | NA | 3.71 (95% CI, 1.91–13.00) | 3.58 (95% CI, 1.87 to no result) | 1.15 (95% CI, 0.46–2.83; p = 0.77) |
| Normal-like | 14.0 (163) | 14.8 (124) | 11.7 (38) | NA | 22.34 (95% CI, 16.56 to no result) | 11.10 (95% CI, 7.39–16.56) | 0.47 (95% CI, 0.30–0.72; p < 0.001) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Canino, F.; Piacentini, F.; Omarini, C.; Toss, A.; Barbolini, M.; Vici, P.; Dominici, M.; Moscetti, L. Role of Intrinsic Subtype Analysis with PAM50 in Hormone Receptors Positive HER2 Negative Metastatic Breast Cancer: A Systematic Review. Int. J. Mol. Sci. 2022, 23, 7079. https://doi.org/10.3390/ijms23137079
Canino F, Piacentini F, Omarini C, Toss A, Barbolini M, Vici P, Dominici M, Moscetti L. Role of Intrinsic Subtype Analysis with PAM50 in Hormone Receptors Positive HER2 Negative Metastatic Breast Cancer: A Systematic Review. International Journal of Molecular Sciences. 2022; 23(13):7079. https://doi.org/10.3390/ijms23137079
Chicago/Turabian StyleCanino, Fabio, Federico Piacentini, Claudia Omarini, Angela Toss, Monica Barbolini, Patrizia Vici, Massimo Dominici, and Luca Moscetti. 2022. "Role of Intrinsic Subtype Analysis with PAM50 in Hormone Receptors Positive HER2 Negative Metastatic Breast Cancer: A Systematic Review" International Journal of Molecular Sciences 23, no. 13: 7079. https://doi.org/10.3390/ijms23137079
APA StyleCanino, F., Piacentini, F., Omarini, C., Toss, A., Barbolini, M., Vici, P., Dominici, M., & Moscetti, L. (2022). Role of Intrinsic Subtype Analysis with PAM50 in Hormone Receptors Positive HER2 Negative Metastatic Breast Cancer: A Systematic Review. International Journal of Molecular Sciences, 23(13), 7079. https://doi.org/10.3390/ijms23137079






