Microbiome in Immune-Mediated Uveitis
Abstract
:1. Introduction
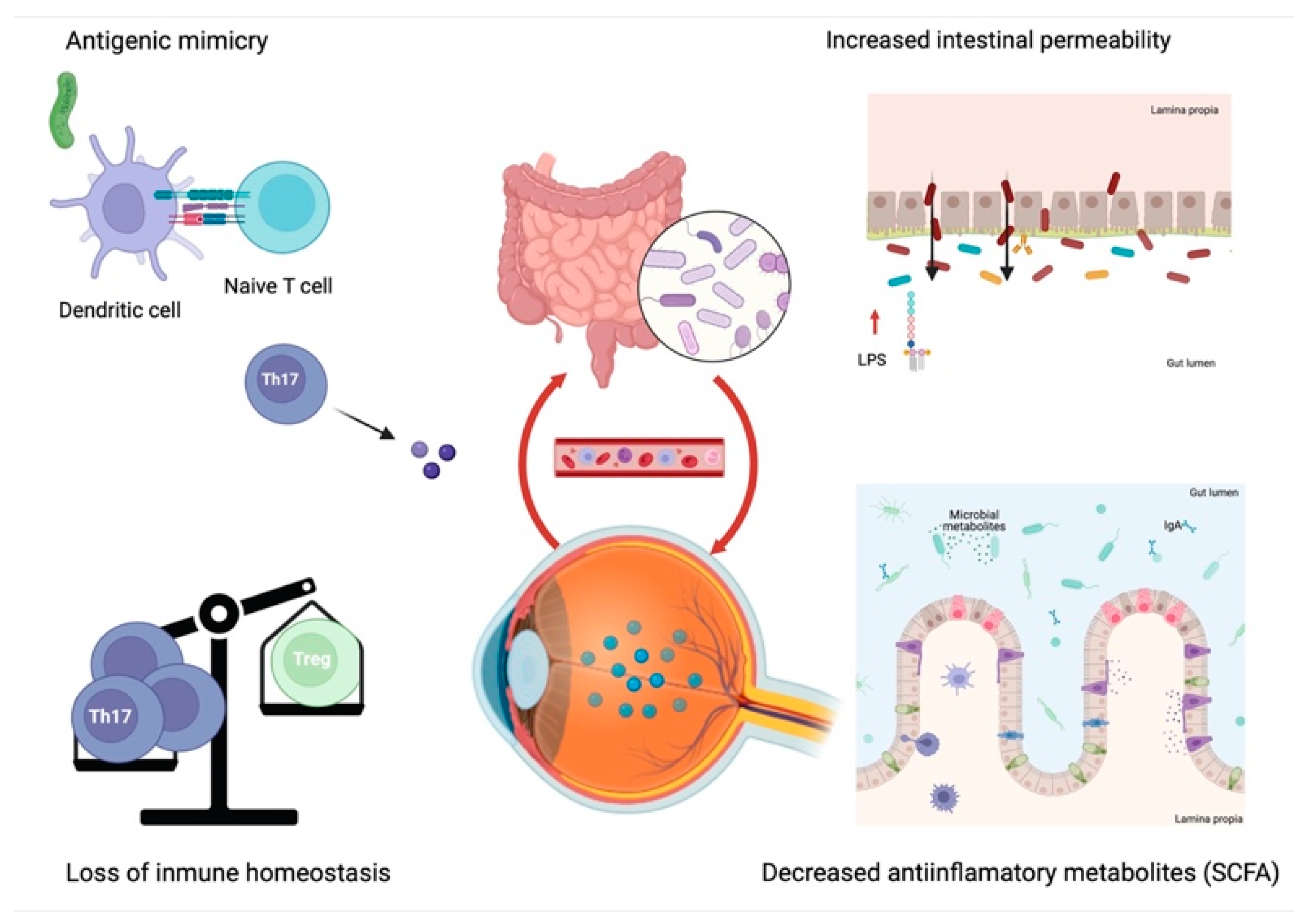
2. Mechanisms of Microbial Pathogenesis and Uveitis
2.1. Antigenic or Molecular Mimicry
2.2. Increased Intestinal Permeability
2.3. Loss of Intestinal Immune Homeostasis
2.4. Reduction of Anti-Inflammatory Microbial Metabolites
3. Microbial Dysbiosis and Uveitis
3.1. Pre-Clinical Studies
3.2. Clinical Studies
4. Therapeutic Approaches Aimed at Modifying the Intestinal Microbiota
4.1. Probiotics
4.2. Prebiotics
4.3. Antibiotic Therapy
4.4. Faecal Microbiota Transplantation (FMT)
4.5. Immunomodulatory Drugs
4.6. Biological Drugs
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Horai, R.; Caspi, R.R. Microbiome and Autoimmune Uveitis. Front Immunol. 2019, 10, 232. [Google Scholar] [CrossRef] [Green Version]
- Mochizuki, M.; Sugita, S.; Kamoi, K. Immunological homeostasis of the eye. Prog. Retin. Eye Res. 2013, 33, 10–27. [Google Scholar] [CrossRef] [PubMed]
- Levy-Clarke, G.; Jabs, D.A.; Read, R.W.; Rosenbaum, J.T.; Vitale, A.; Van Gelder, R.N. Expert Panel Recommendations for the Use of Anti–Tumor Necrosis Factor Biologic Agents in Patients with Ocular Inflammatory Disorders. Ophthalmology 2014, 121, 785–796.e3. [Google Scholar] [CrossRef]
- Lin, P. The role of the intestinal microbiome in ocular inflammatory disease. Curr. Opin. Ophthalmol. 2018, 29, 261–266. [Google Scholar] [CrossRef] [PubMed]
- Turnbaugh, P.J.; Ley, R.E.; Hamady, M.; Fraser-Liggett, C.M.; Knight, R.; Gordon, J.I. The human microbiome project. Nature 2007, 449, 804–810. [Google Scholar] [CrossRef] [PubMed]
- Eckburg, P.B.; Bik, E.M.; Bernstein, C.N.; Purdom, E.; Dethlefsen, L.; Sargent, M.; Gill, S.R.; Nelson, K.E.; Relman, D.A. Diversity of the human intestinal microbial flora. Science 2005, 308, 1635–1638. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, H.X.; Wang, Y.P. Gut Microbiota-brain Axis. Chin. Med. J. 2016, 129, 2373–2380. [Google Scholar] [CrossRef]
- Ley, R.E.; Bäckhed, F.; Turnbaugh, P.; Lozupone, C.A.; Knight, R.D.; Gordon, J.I. Obesity alters gut microbial ecology. Proc. Natl. Acad. Sci. USA 2005, 102, 11070–11075. [Google Scholar] [CrossRef] [Green Version]
- Gritz, E.C.; Bhandari, V. The human neonatal gut microbiome: A brief review. Front. Pediatr. 2015, 3, 17. [Google Scholar]
- Matenchuk, B.A.; Mandhane, P.J.; Kozyrskyj, A.L. Sleep, circadian rhythm, and gut microbiota. Sleep Med. Rev. 2020, 53, 101340. [Google Scholar] [CrossRef]
- Nell, S.; Suerbaum, S.; Josenhans, C. The impact of the microbiota on the pathogenesis of IBD: Lessons from mouse infection models. Nat. Rev. Microbiol. 2010, 8, 564–577. [Google Scholar] [CrossRef] [PubMed]
- Kc, D.; Sumner, R.; Lippmann, S. Gut microbiota and health. Postgrad. Med. 2020, 132, 274. [Google Scholar] [CrossRef] [Green Version]
- Forrester, J.V.; Kuffova, L.; Dick, A.D. Autoimmunity, Autoinflammation, and Infection in Uveitis. Am. J. Ophthalmol. 2018, 189, 77–85. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wen, X.; Hu, X.; Miao, L.; Ge, X.; Deng, Y.; Bible, P.W.; Wei, L. Epigenetics, microbiota, and intraocular inflammation: New paradigms of immune regulation in the eye. Prog. Retin. Eye Res. 2018, 64, 84–95. [Google Scholar] [CrossRef] [PubMed]
- Rosenbaum, J.T.; Lin, P.; Asquith, M. Does the Microbiome Cause B27-related Acute Anterior Uveitis? Ocul. Immunol. Inflamm. 2016, 24, 440–444. [Google Scholar] [CrossRef]
- Jones, N.P. Immunosuppression in the Management of Presumed Non-infective Uveitis; Are We Sure What We are Treating? Notes on the Antimicrobial Properties of the Systemic Immunosuppressants. Ocul. Immunol. Inflamm. 2020, 28, 994–1003. [Google Scholar] [CrossRef] [Green Version]
- Nishida, A.; Inoue, R.; Inatomi, O.; Bamba, S.; Naito, Y.; Andoh, A. Gut microbiota in the pathogenesis of inflammatory bowel disease. Clin. J. Gastroenterol. 2018, 11, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Clapp, M.; Aurora, N.; Herrera, L.; Bhatia, M.; Wilen, E.; Wakefield, S. Gut microbiota’s effect on mental health: The gut-brain axis. Clin. Pract. 2017, 7, 987. [Google Scholar] [CrossRef]
- Angelucci, F.; Cechova, K.; Amlerova, J.; Hort, J. Antibiotics, gut microbiota, and Alzheimer’s disease. J. Neuroinflamm. 2019, 16, 108. [Google Scholar] [CrossRef]
- Kim, S.; Jazwinski, S.M. The Gut Microbiota and Healthy Aging: A Mini-Review. Gerontology 2018, 64, 513–520. [Google Scholar] [CrossRef]
- Yasar Bilge, N.S.; Pérez Brocal, V.; Kasifoglu, T.; Bilge, U.; Kasifoglu, N.; Moya, A.; Dinleyici, E.C. Intestinal microbiota composition of patients with Behçet’s disease: Differences between eye, mucocutaneous and vascular involvement. The Rheuma-BIOTA study. Clin. Exp. Rheumatol. 2020, 38 (Suppl. 127), 60–68. [Google Scholar] [PubMed]
- Ye, Z.; Zhang, N.; Wu, C.; Zhang, X.; Wang, Q.; Huang, X.; Du, L.; Cao, Q.; Tang, J.; Zhou, C.; et al. A metagenomic study of the gut microbiome in Behcet’s disease. Microbiome 2018, 6, 135. [Google Scholar] [CrossRef] [PubMed]
- Chen, Z.; Zheng, X.; Wu, X.; Wu, J.; Li, X.; Wei, Q.; Zhang, X.; Fang, L.; Jin, O.; Gu, J. Adalimumab Therapy Restores the Gut Microbiota in Patients With Ankylosing Spondylitis. Front Immunol. 2021, 12, 700570. [Google Scholar] [CrossRef] [PubMed]
- Li, M.; Yang, L.; Cao, J.; Liu, T.; Liu, X. Enriched and Decreased Intestinal Microbes in Active VKH Patients. Investig. Ophthalmol. Vis. Sci. 2022, 63, 21. [Google Scholar] [CrossRef]
- Moustafa, A.; Li, W.; Anderson, E.L.; Wong, E.H.M.; Dulai, P.S.; Sandborn, W.J.; Biggs, W.; Yooseph, S.; Jones, M.B.; Venter, C.J.; et al. Genetic risk, dysbiosis, and treatment stratification using host genome and gut microbiome in inflammatory bowel disease. Clin. Transl. Gastroenterol. 2018, 9, e132. [Google Scholar] [CrossRef]
- Rowan, S.; Taylor, A. The Role of Microbiota in Retinal Disease. Adv. Exp. Med. Biol. 2018, 1074, 429–435. [Google Scholar]
- Tanase, D.M.; Gosav, E.M.; Neculae, E.; Costea, C.F.; Ciocoiu, M.; Hurjui, L.L.; Tarniceriu, C.C.; Maranduca, M.A.; Lacatusu, C.M.; Floria, M.; et al. Role of Gut Microbiota on Onset and Progression of Microvascular Complications of Type 2 Diabetes (T2DM). Nutrients 2020, 12, 3719. [Google Scholar] [CrossRef]
- Rinninella, E.; Mele, M.C.; Merendino, N.; Cintoni, M.; Anselmi, G.; Caporossi, A.; Minnella, A.M. The Role of Diet, Micronutrients and the Gut Microbiota in Age-Related Macular Degeneration: New Perspectives from the Gut−Retina Axis. Nutrients 2018, 10, 1677. [Google Scholar] [CrossRef] [Green Version]
- Geyer, O.; Levo, Y. Glaucoma is an autoimmune disease. Autoimmun. Rev. 2020, 19, 102535. [Google Scholar] [CrossRef]
- Fu, X.; Chen, Y.; Chen, D. The Role of Gut Microbiome in Autoimmune Uveitis. Ophthalmic. Res. 2021, 64, 168–177. Available online: https://www.karger.com/Article/FullText/510212 (accessed on 20 November 2021). [CrossRef]
- Rojas, M.; Restrepo-Jiménez, P.; Monsalve, D.M.; Pacheco, Y.; Acosta-Ampudia, Y.; Ramírez-Santana, C.; Leung, P.S.C.; Ansari, A.A.; Gershwin, M.E.; Anaya, J.M. Molecular mimicry and autoimmunity. J. Autoimmun. 2018, 95, 100–123. [Google Scholar] [CrossRef]
- Rosenbaum, J.T.; Asquith, M. The microbiome and HLA-B27-associated acute anterior uveitis. Nat. Rev. Rheumatol. 2018, 14, 704–713. [Google Scholar] [CrossRef]
- Wakefield, D.; Clarke, D.; McCluskey, P. Recent Developments in HLA B27 Anterior Uveitis. Front. Immunol. 2021, 11, 608134. [Google Scholar] [CrossRef]
- Scofield, R.H.; Warren, W.L.; Koelsch, G.; Harley, J.B. A hypothesis for the HLA-B27 immune dysregulation in spondyloarthropathy: Contributions from enteric organisms, B27 structure, peptides bound by B27, and convergent evolution. Proc. Natl. Acad. Sci. USA 1993, 90, 9330–9334. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Horai, R.; Zárate-Bladés, C.; Dillenburg-Pilla, P.; Chen, J.; Kielczewski, J.L.; Silver, P.B.; Jittayasothorn, Y.; Chan, C.-C.; Yamane, H.; Honda, K.; et al. Microbiota-Dependent Activation of an Autoreactive T Cell Receptor Provokes Autoimmunity in an Immunologically Privileged Site. Immunity 2015, 43, 343–353. [Google Scholar] [CrossRef] [Green Version]
- Rosenbaum, J.T.; Lin, P.; Asquith, M. The microbiome, HLA, and the pathogenesis of uveitis. Jpn. J. Ophthalmol. 2016, 60, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Ciccia, F.; Guggino, G.; Rizzo, A.; Alessandro, R.; Luchetti, M.M.; Milling, S.; Saieva, L.; Cypers, H.; Stampone, T.; Di Benedetto, P.; et al. Dysbiosis and zonulin upregulation alter gut epithelial and vascular barriers in patients with ankylosing spondylitis. Ann. Rheum. Dis. 2017, 76, 1123–1132. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Janowitz, C.; Nakamura, Y.K.; Metea, C.; Gligor, A.; Yu, W.; Karstens, L.; Rosenbaum, J.T.; Asquith, M.; Lin, P. Disruption of Intestinal Homeostasis and Intestinal Microbiota During Experimental Autoimmune Uveitis. Investig. Opthalmol. Vis. Sci. 2019, 60, 420. [Google Scholar] [CrossRef] [Green Version]
- Zhuang, Z.; Wang, Y.; Zhu, G.; Gu, Y.; Mao, L.; Hong, M.; Li, Y.; Zheng, M. Imbalance of Th17/Treg cells in pathogenesis of patients with human leukocyte antigen B27 associated acute anterior uveitis. Sci. Rep. 2017, 7, 40414. [Google Scholar] [CrossRef] [Green Version]
- Asquith, M.J.; Stauffer, P.; Davin, S.; Mitchell, C.; Lin, P.; Rosenbaum, J.T. Perturbed Mucosal Immunity and Dysbiosis Accompany Clinical Disease in a Rat Model of Spondyloarthritis. Arthritis Rheumatol. 2016, 68, 2151–2162. [Google Scholar] [CrossRef] [Green Version]
- Nakamura, Y.K.; Metea, C.; Karstens, L.; Asquith, M.; Gruner, H.; Moscibrocki, C.; Lee, I.; Brislawn, C.J.; Jansson, J.K.; Rosenbaum, J.T.; et al. Gut Microbial Alterations Associated With Protection From Autoimmune Uveitis. Investig. Ophthalmol. Vis. Sci. 2016, 57, 3747–3758. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nakamura, Y.K.; Janowitz, C.; Metea, C.; Asquith, M.; Karstens, L.; Rosenbaum, J.T.; Lin, P. Short chain fatty acids ameliorate immune-mediated uveitis partially by altering migration of lymphocytes from the intestine. Sci. Rep. 2017, 7, 11745. [Google Scholar] [CrossRef] [PubMed]
- Asquith, M.; Davin, S.; Stauffer, P.; Michell, C.; Janowitz, C.; Lin, P.; Ensign-Lewis, J.; Kinchen, J.M.; Koop, D.R.; Rosenbaum, J.T. Intestinal Metabolites Are Profoundly Altered in the Context of HLA-B27 Expression and Functionally Modulate Disease in a Rat Model of Spondyloarthritis. Arthritis Rheumatol. 2017, 69, 1984–1995. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, X.; Su, W.; Wan, T.; Yu, J.; Zhu, W.; Tang, F.; Liu, G.; Olsen, N.; Liang, D.; Zheng, S.G. Sodium butyrate regulates Th17/Treg cell balance to ameliorate uveitis via the Nrf2/HO-1 pathway. Biochem. Pharmacol. 2017, 142, 111–119. [Google Scholar] [CrossRef] [PubMed]
- Matysiak, A.; Kabza, M.; Karolak, J.; Jaworska, M.; Rydzanicz, M.; Ploski, R.; Szaflik, J.; Gajecka, M. Characterization of Ocular Surface Microbial Profiles Revealed Discrepancies between Conjunctival and Corneal Microbiota. Pathogens 2021, 10, 405. [Google Scholar] [CrossRef] [PubMed]
- Zysset-Burri, D.C.; Schlegel, I.; Lincke, J.-B.; Jaggi, D.; Keller, I.; Heller, M.; Lagache, S.B.; Wolf, S.; Zinkernagel, M.S. Understanding the Interactions Between the Ocular Surface Microbiome and the Tear Proteome. Investig. Ophthalmol. Vis. Sci. 2021, 62, 8. [Google Scholar] [CrossRef] [PubMed]
- Gomes, J.Á.P.; Frizon, L.; Demeda, V.F. Ocular Surface Microbiome in Health and Disease. Asia-Pac. J. Ophthalmol. 2020, 9, 505–511. [Google Scholar] [CrossRef]
- Gündüz, A.; Gündüz, A.; Cumurcu, T.; Seyrek, A. Conjunctival flora in Behçet patients. Can. J. Ophthalmol. 2008, 43, 476–479. [Google Scholar] [CrossRef]
- Aragona, P.; Baudouin, C.; del Castillo, J.M.B.; Messmer, E.; Barabino, S.; Merayo-Lloves, J.; Brignole-Baudouin, F.; Inferrera, L.; Rolando, M.; Mencucci, R.; et al. The ocular microbiome and microbiota and their effects on ocular surface pathophysiology and disorders. Surv. Ophthalmol. 2021, 66, 907–925. [Google Scholar] [CrossRef]
- Li, J.J.; Yi, S.; Wei, L. Ocular Microbiota and Intraocular Inflammation. Front. Immunol. 2020, 11, 609765. [Google Scholar] [CrossRef]
- Petrillo, F.; Pignataro, D.; Lavano, M.A.; Santella, B.; Folliero, V.; Zannella, C.; Astarita, C.; Gagliano, C.; Franci, G.; Avitabile, T.; et al. Current Evidence on the Ocular Surface Microbiota and Related Diseases. Microorganisms 2020, 8, 1033. [Google Scholar] [CrossRef] [PubMed]
- Streilein, J.W. Ocular immune privilege: Therapeutic opportunities from an experiment of nature. Nat. Rev. Immunol. 2003, 3, 879–889. [Google Scholar] [CrossRef] [PubMed]
- Ozkan, J.; Willcox, M.D. The Ocular Microbiome: Molecular Characterisation of a Unique and Low Microbial Environment. Curr. Eye Res. 2019, 44, 685–694. [Google Scholar] [CrossRef] [PubMed]
- Heissigerova, J.; Stangova, P.S.; Klimova, A.; Svozilkova, P.; Hrncir, T.; Stepankova, R.; Kverka, M.; Tlaskalova-Hogenova, H.; Forrester, J.V. The Microbiota Determines Susceptibility to Experimental Autoimmune Uveoretinitis. J. Immunol. Res. 2016, 2016, 5065703. [Google Scholar] [CrossRef] [Green Version]
- Zárate-Bladés, C.R.; Horai, R.; Mattapallil, M.J.; Ajami, N.J.; Wong, M.; Petrosino, J.F.; Itoh, K.; Chan, C.-C.; Caspi, R.R. Gut microbiota as a source of a surrogate antigen that triggers autoimmunity in an immune privileged site. Gut Microbes 2017, 8, 59–66. [Google Scholar] [CrossRef]
- Dusek, O.; Fajstova, A.; Klimova, A.; Svozilkova, P.; Hrncir, T.; Kverka, M.; Coufal, S.; Slemin, J.; Tlaskalova-Hogenova, H.; Forrester, J.V.; et al. Severity of Experimental Autoimmune Uveitis Is Reduced by Pretreatment with Live Probiotic Escherichia coli Nissle 1917. Cells 2020, 10, 23. [Google Scholar] [CrossRef]
- Kim, J.; Choi, S.H.; Kim, Y.J.; Jeong, H.J.; Ryu, J.S.; Lee, H.J.; Kim, T.W.; Im, S.-H.; Oh, J.Y.; Kim, M.K. Clinical Effect of IRT-5 Probiotics on Immune Modulation of Autoimmunity or Alloimmunity in the Eye. Nutrients 2017, 9, 1166. [Google Scholar] [CrossRef]
- Furusawa, Y.; Obata, Y.; Fukuda, S.; Endo, T.A.; Nakato, G.; Takahashi, D.; Nakanishi, Y.; Uetake, C.; Kato, K.; Kato, T.; et al. Commensal microbe-derived butyrate induces the differentiation of colonic regulatory T cells. Nature 2013, 504, 446–450. [Google Scholar] [CrossRef]
- Lin, P.; Bach, M.; Asquith, M.; Lee, A.Y.; Akileswaran, L.; Stauffer, P.; Davin, S.; Pan, Y.; Cambronne, E.D.; Dorris, M.; et al. HLA-B27 and Human β2-Microglobulin Affect the Gut Microbiota of Transgenic Rats. PLoS ONE 2014, 9, e105684. [Google Scholar] [CrossRef]
- Chakravarthy, S.K.; Jayasudha, R.; Prashanthi, G.S.; Ali, M.H.; Sharma, S.; Tyagi, M.; Shivaji, S. Dysbiosis in the Gut Bacterial Microbiome of Patients with Uveitis, an Inflammatory Disease of the Eye. Indian J. Microbiol. 2018, 58, 457–469. [Google Scholar] [CrossRef]
- Jayasudha, R.; Chakravarthy, S.K.; Prashanthi, G.S.; Sharma, S.; Tyagi, M.; Shivaji, S. Implicating Dysbiosis of the Gut Fungal Microbiome in Uveitis, an Inflammatory Disease of the Eye. Investig. Ophthalmol. Vis. Sci. 2019, 60, 1384–1393. [Google Scholar] [CrossRef] [Green Version]
- Huang, X.; Ye, Z.; Cao, Q.; Su, G.; Wang, Q.; Deng, J.; Zhou, C.; Kijlstra, A.; Yang, P. Gut Microbiota Composition and Fecal Metabolic Phenotype in Patients With Acute Anterior Uveitis. Investig. Ophthalmol. Vis. Sci. 2018, 59, 1523–1531. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Consolandi, C.; Turroni, S.; Emmi, G.; Severgnini, M.; Fiori, J.; Peano, C.; Biagi, E.; Grassi, A.; Rampelli, S.; Silvestri, E.; et al. Behçet’s syndrome patients exhibit specific microbiome signature. Autoimmun. Rev. 2015, 14, 269–276. [Google Scholar] [CrossRef] [Green Version]
- Shimizu, J.; Kubota, T.; Takada, E.; Takai, K.; Fujiwara, N.; Arimitsu, N.; Ueda, Y.; Wakisaka, S.; Suzuki, T.; Suzuki, N. Bifidobacteria Abundance-Featured Gut Microbiota Compositional Change in Patients with Behcet’s Disease. PLoS ONE 2016, 11, e0153746. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ye, Z.; Wu, C.; Zhang, N.; Du, L.; Cao, Q.; Huang, X.; Tang, J.; Wang, Q.; Li, F.; Zhou, C.; et al. Altered gut microbiome composition in patients with Vogt-Koyanagi-Harada disease. Gut Microbes 2020, 11, 539–555. [Google Scholar] [CrossRef]
- Pagliai, G.; Dinu, M.; Fiorillo, C.; Becatti, M.; Turroni, S.; Emmi, G.; Sofi, F. Modulation of gut microbiota through nutritional interventions in Behçet’s syndrome patients (the MAMBA study): Study protocol for a randomized controlled trial. Trials 2020, 21, 511. [Google Scholar] [CrossRef]
- Costello, M.E.; Ciccia, F.; Willner, D.; Warrington, N.; Robinson, P.C.; Gardiner, B.; Marshall, M.; Kenna, T.J.; Triolo, G.; Brown, M.A. Brief Report: Intestinal Dysbiosis in Ankylosing Spondylitis: Gut Microbiome and AS-Related Genes. Arthritis Rheumatol. 2015, 67, 686–691. [Google Scholar] [CrossRef]
- Tito, R.Y.; Cypers, H.; Joossens, M.; Varkas, G.; Van Praet, L.; Glorieus, E.; Bosch, F.V.D.; De Vos, M.; Raes, J.; Elewaut, D. Brief Report: Dialister as a Microbial Marker of Disease Activity in Spondyloarthritis. Arthritis Rheumatol. 2017, 69, 114–121. [Google Scholar] [CrossRef] [PubMed]
- Arboleya, S.; Watkins, C.; Stanton, C.; Ross, R.P. Gut Bifidobacteria Populations in Human Health and Aging. Front. Microbiol. 2016, 7, 1204. [Google Scholar] [CrossRef] [Green Version]
- De Oliveira, G.L.V.; Leite, A.Z.; Higuchi, B.S.; Gonzaga, M.I.; Mariano, V.S. Intestinal dysbiosis and probiotic applications in autoimmune diseases. Immunology 2017, 152, 1–12. [Google Scholar] [CrossRef]
- Holscher, H.D. Dietary fiber and prebiotics and the gastrointestinal microbiota. Gut Microbes 2017, 8, 172–184. [Google Scholar] [CrossRef] [PubMed]
- Zmora, N.; Suez, J.; Elinav, E. You are what you eat: Diet, health and the gut microbiota. Nat. Rev. Gastroenterol. Hepatol. 2019, 16, 35–56. [Google Scholar] [CrossRef] [PubMed]
- De Filippis, F.; Pellegrini, N.; Vannini, L.; Jeffery, I.B.; La Storia, A.; Laghi, L.; Serrazanetti, D.I.; di Cagno, R.; Ferrocino, I.; Lazzi, C.; et al. High-level adherence to a Mediterranean diet beneficially impacts the gut microbiota and associated metabolome. Gut 2016, 65, 1812–1821. [Google Scholar] [CrossRef] [PubMed]
- Okai, S.; Usui, F.; Ohta, M.; Mori, H.; Kurokawa, K.; Matsumoto, S.; Kato, T.; Miyauchi, E.; Ohno, H.; Shinkura, R. Intestinal IgA as a modulator of the gut microbiota. Gut Microbes 2017, 8, 486–492. [Google Scholar] [CrossRef] [Green Version]
- Okai, S.; Usui, F.; Yokota, S.; Hori-I, Y.; Hasegawa, M.; Nakamura, T.; Kurosawa, M.; Okada, S.; Yamamoto, K.; Nishiyama, E.; et al. High-affinity monoclonal IgA regulates gut microbiota and prevents colitis in mice. Nat. Microbiol. 2016, 1, 16103. [Google Scholar] [CrossRef] [PubMed]
- van Nood, E.; Vrieze, A.; Nieuwdorp, M.; Fuentes, S.; Zoetendal, E.G.; de Vos, W.M.; Visser, C.E.; Kuijper, E.J.; Bartelsman, J.F.W.M.; Tijssen, J.G.P.; et al. Duodenal infusion of donor feces for recurrent Clostridium difficile. N. Engl. J. Med. 2013, 368, 407–415. [Google Scholar] [CrossRef] [Green Version]
- Choi, R.Y.; Asquith, M.; Rosenbaum, J.T. Fecal transplants in spondyloarthritis and uveitis: Ready for a clinical trial? Curr. Opin. Rheumatol. 2018, 30, 303–309. [Google Scholar] [CrossRef]
- Rossi, D.C.; Ribi, C.; Guex-Crosier, Y. Treatment of chronic non-infectious uveitis and scleritis. Swiss Med. Wkly. 2019, 149, w20025. [Google Scholar] [CrossRef] [Green Version]
- Sharma, S.K.; Kadiyala, V.; Naidu, G.; Dhir, V. A randomized controlled trial to study the efficacy of sulfasalazine for axial disease in ankylosing spondylitis. Int. J. Rheum. Dis. 2018, 21, 308–314. [Google Scholar] [CrossRef]
- Llorenç, V.; Nakamura, Y.; Metea, C.; Karstens, L.; Molins, B.; Lin, P. Antimetabolite Drugs Exhibit Distinctive Immunomodulatory Mechanisms and Effects on the Intestinal Microbiota in Experimental Autoimmune Uveitis. Investig. Opthalmol. Vis. Sci. 2022, 63, 30. [Google Scholar] [CrossRef]
- Ward, M.M.; Deodhar, A.; Gensler, L.S.; Dubreuil, M.; Yu, D.; Khan, M.A.; Visser, C.E.; Kuijper, E.J.; Bartelsman, J.F.W.M.; Tijssen, J.G.P.; et al. 2019 Update of the American College of Rheumatology/Spondylitis Association of America/Spondyloarthritis Research and Treatment Network Recommendations for the Treatment of Ankylosing Spondylitis and Nonradiographic Axial Spondyloarthritis. Arthritis Rheumatol. 2019, 71, 1599–1613. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, Q.D.; Merrill, P.; Jaffe, G.J.; Dick, A.D.; Kurup, S.K.; Sheppard, J.; Schlaen, A.; Pavesio, C.; Cimino, L.; Van Calster, J.; et al. Adalimumab for prevention of uveitic flare in patients with inactive non-infectious uveitis controlled by corticosteroids (VISUAL II): A multicentre, double-masked, randomised, placebo-controlled phase 3 trial. Lancet 2016, 388, 1183–1192. [Google Scholar] [CrossRef] [Green Version]
- Suhler, E.B.; Adán, A.; Brézin, A.P.; Fortin, E.; Goto, H.; Jaffe, G.J. Safety and Efficacy of Adalimumab in Patients with Noninfectious Uveitis in an Ongoing Open-Label Study: VISUAL III. Ophthalmology 2018, 125, 1075–1087. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Goto, H.; Zako, M.; Namba, K.; Hashida, N.; Kaburaki, T.; Miyazaki, M.; Sonoda, K.-H.; Abe, T.; Mizuki, N.; Kamoi, K.; et al. Adalimumab in Active and Inactive, Non-Infectious Uveitis: Global Results from the VISUAL I and VISUAL II Trials. Ocul. Immunol. Inflamm. 2019, 27, 40–50. [Google Scholar] [CrossRef]
- You, C.; Sahawneh, H.; Ma, L.; Kubaisi, B.; Schmidt, A.; Foster, S. A review and update on orphan drugs for the treatment of noninfectious uveitis. Clin. Ophthalmol. 2017, 11, 257–265. [Google Scholar] [CrossRef] [Green Version]
- Ohno, S.; Umebayashi, I.; Matsukawa, M.; Goto, T.; Yano, T. Safety and efficacy of infliximab in the treatment of refractory uveoretinitis in Behçet’s disease: A large-scale, long-term postmarketing surveillance in Japan. Arthritis Res. Ther. 2019, 21, 2. [Google Scholar] [CrossRef] [Green Version]
- Ribaldone, D.G.; Caviglia, G.P.; Abdulle, A.; Pellicano, R.; Ditto, M.C.; Morino, M.; Fusaro, E.; Saracco, G.M.; Bugianesi, E.; Astegiano, M. Adalimumab Therapy Improves Intestinal Dysbiosis in Crohn’s Disease. J. Clin. Med. 2019, 8, 1646. [Google Scholar] [CrossRef] [Green Version]
- Weersma, R.K.; Zhernakova, A.; Fu, J. Interaction between drugs and the gut microbiome. Gut 2020, 69, 1510–1519. [Google Scholar] [CrossRef]
- Zhou, Y.; Xu, Z.Z.; He, Y.; Yang, Y.; Liu, L.; Lin, Q.; Nie, Y.; Li, M.; Zhi, F.; Liu, S.; et al. Gut Microbiota Offers Universal Biomarkers across Ethnicity in Inflammatory Bowel Disease Diagnosis and Infliximab Response Prediction. mSystems 2018, 3, e00188-17. Available online: https://journals.asm.org/doi/10.1128/mSystems.00188-17 (accessed on 17 January 2022). [CrossRef] [Green Version]

| Authors | Study Type | Modulation–Intervention | Findings | |
|---|---|---|---|---|
| Horai et al., 2015 [35] | Experimental Spontaneous EAU | Decreased bacterial load of the microbiota |
|
|
| Zárate-Baldés et al., 2017 [55] | Experimental Spontaneous EAU |
|
| |
| Nakamura et al., 2016 [41] | Experimental Induced EAU |
|
| |
| Heissigerova et al., 2016 [54] | Experimental Induced EAU |
|
| |
| Dusek et al., 2020 [56] | Experimental Induced EAU | Supplementation with probiotics |
|
|
| Kim et al., 2017 [57] | Experimental Induced EAU |
|
| |
| Chen et al., 2017 [44] | Experimental EAU | Supplementation with prebiotics |
|
|
| Nakamura et al., 2017 [42] | Experimental Induced EAU |
|
| |
| Authors | Disease | n Patients and n Control | Findings |
|---|---|---|---|
| Kalyana et al., 2018 [60] | NIU | 13 NIU vs. 13 healthy |
|
| Jayasudha et al., 2019 [61] | 14 NIU vs. 24 healthy |
| |
| Huang et al., 2018 [62] | AAU | 38 AAU vs. 40 healthy |
|
| Consolandi et al., 2015 [63] | BD | 22 BD vs. 16 healthy |
|
| Yasar et al., 2020 [21] | 27 BD vs. 10 healthy 3 clinical forms of BD |
| |
| Shimizu et al., 2016 [64] | 12 BD vs. 12 healthy |
| |
| Ye et al., 2018 [22] | 32 BD vs. 74 healthy |
| |
| Ye et al., 2020 [65] | VKH | 82 VKH vs. 63 healthy |
|
| Authors | Disease | n Patients and n Control | Study Type | Findings |
|---|---|---|---|---|
| Tito et al., 2017 [68] | AS | 27 AS vs. 15 healthy | Causality |
|
| Costello et al., 2015 [67] | 9 AS vs. 9 healthy |
| ||
| Chen et al., 2021 [23] | 30 AS vs. 24 healthy | Modulation |
| |
| Ribaldone et al., 2019 [87] | IBD | 20 CD pre- and post-ADA treatment |
| |
| Zhou et al., 2018 [89] | 72 CD, 51 UC vs. 73 healthy 16 CD pre- and post-IFX |
|
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rodríguez-Fernández, C.A.; Iglesias, M.B.; de Domingo, B.; Conde-Pérez, K.; Vallejo, J.A.; Rodríguez-Martínez, L.; González-Barcia, M.; Llorenç, V.; Mondelo-Garcia, C.; Poza, M.; et al. Microbiome in Immune-Mediated Uveitis. Int. J. Mol. Sci. 2022, 23, 7020. https://doi.org/10.3390/ijms23137020
Rodríguez-Fernández CA, Iglesias MB, de Domingo B, Conde-Pérez K, Vallejo JA, Rodríguez-Martínez L, González-Barcia M, Llorenç V, Mondelo-Garcia C, Poza M, et al. Microbiome in Immune-Mediated Uveitis. International Journal of Molecular Sciences. 2022; 23(13):7020. https://doi.org/10.3390/ijms23137020
Chicago/Turabian StyleRodríguez-Fernández, Carmen Antía, Manuel Busto Iglesias, Begoña de Domingo, Kelly Conde-Pérez, Juan A. Vallejo, Lorena Rodríguez-Martínez, Miguel González-Barcia, Victor Llorenç, Cristina Mondelo-Garcia, Margarita Poza, and et al. 2022. "Microbiome in Immune-Mediated Uveitis" International Journal of Molecular Sciences 23, no. 13: 7020. https://doi.org/10.3390/ijms23137020
APA StyleRodríguez-Fernández, C. A., Iglesias, M. B., de Domingo, B., Conde-Pérez, K., Vallejo, J. A., Rodríguez-Martínez, L., González-Barcia, M., Llorenç, V., Mondelo-Garcia, C., Poza, M., & Fernández-Ferreiro, A. (2022). Microbiome in Immune-Mediated Uveitis. International Journal of Molecular Sciences, 23(13), 7020. https://doi.org/10.3390/ijms23137020







