Nano–Liposomes Double Loaded with Curcumin and Tetrandrine: Preparation, Characterization, Hepatotoxicity and Anti–Tumor Effects
Abstract
:1. Introduction
2. Results
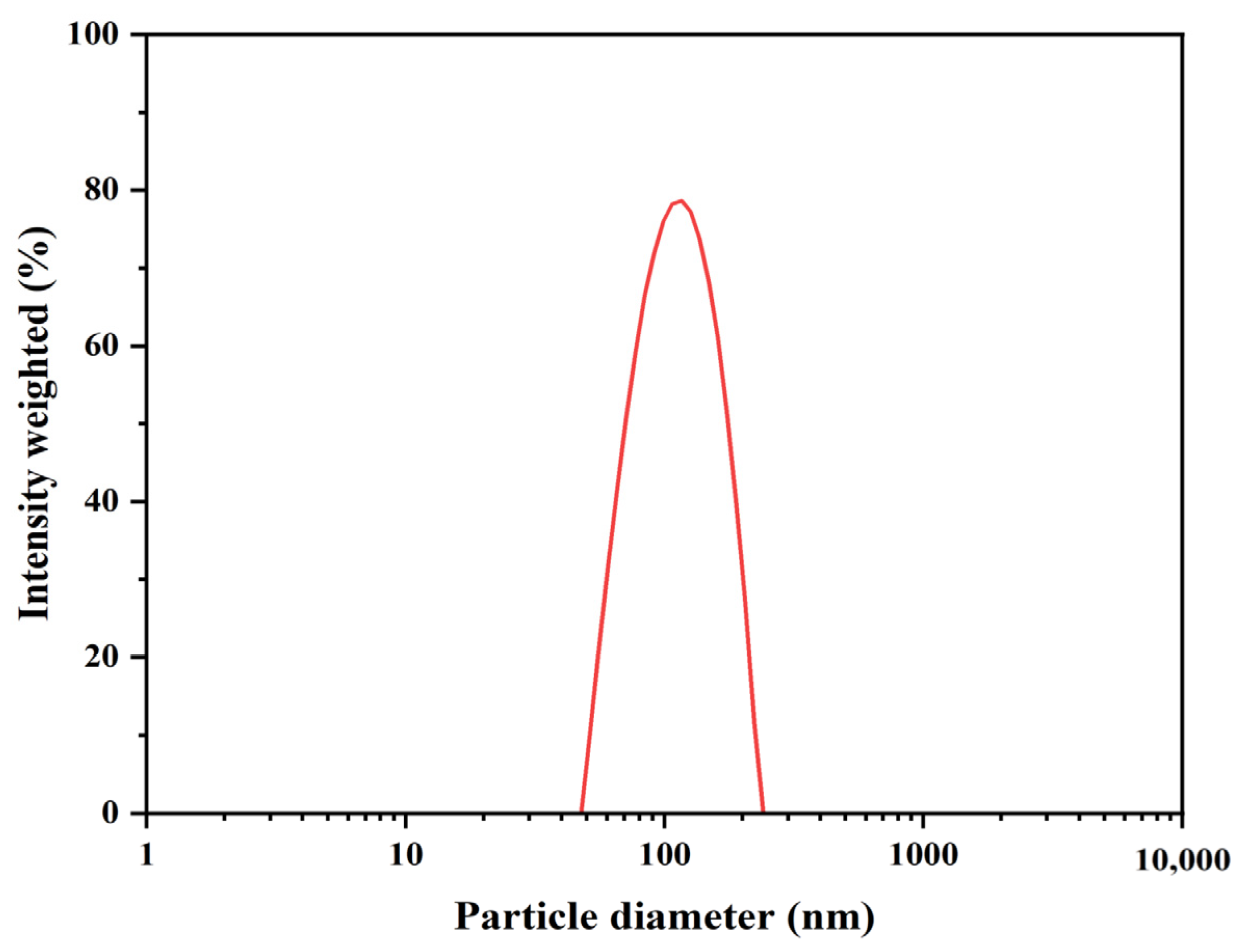
2.1. The Physical and Chemical Properties of Liposomes
2.2. The EE and LC of CUR and TET
2.3. Effect of DP Ratio on Drug–Loaded Liposomes
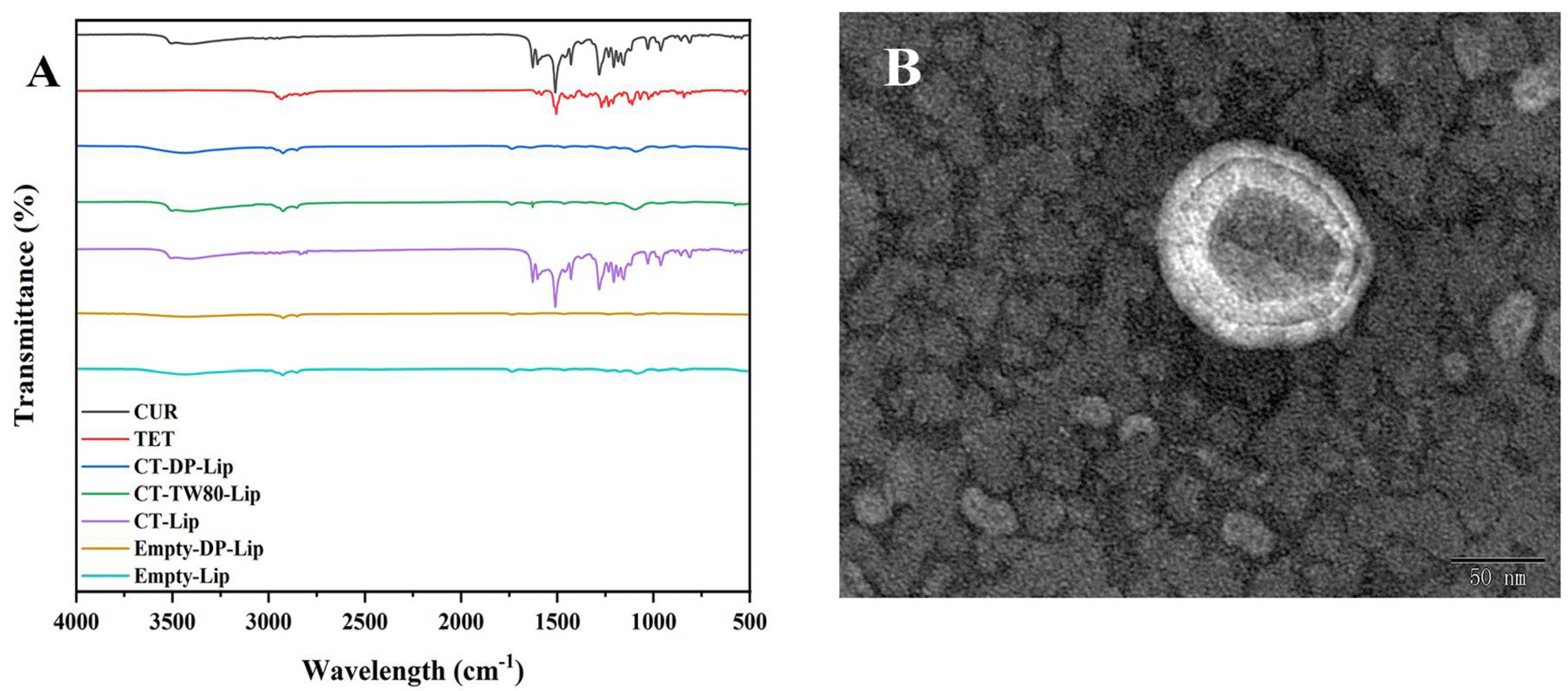
2.4. The FT–IR Spectrum
2.5. The TEM Spectrum
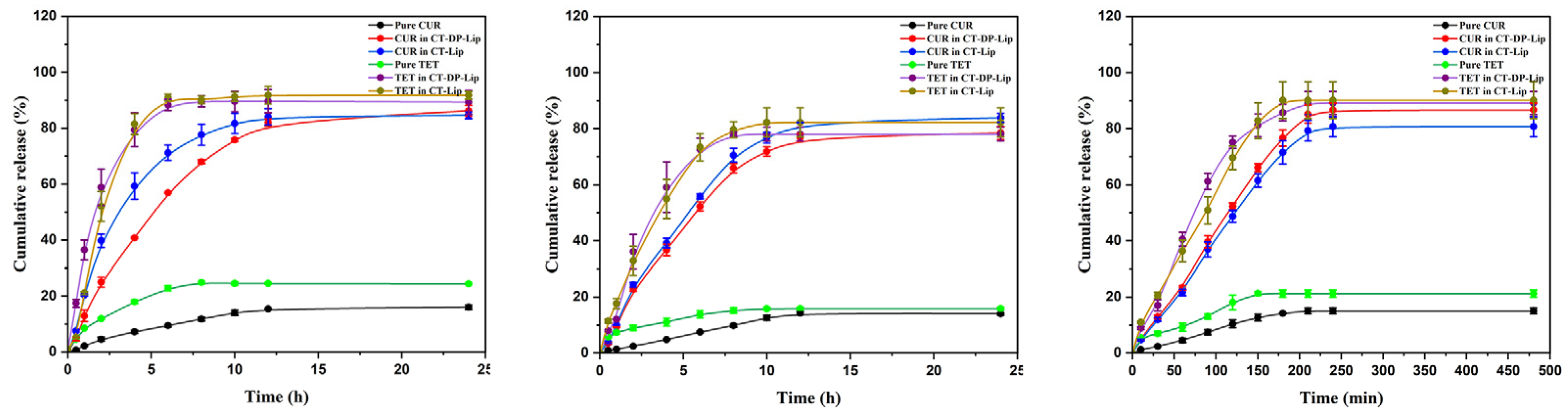
2.6. The CR of Drugs in CT–DP–Lip and CT–Lip In Vitro
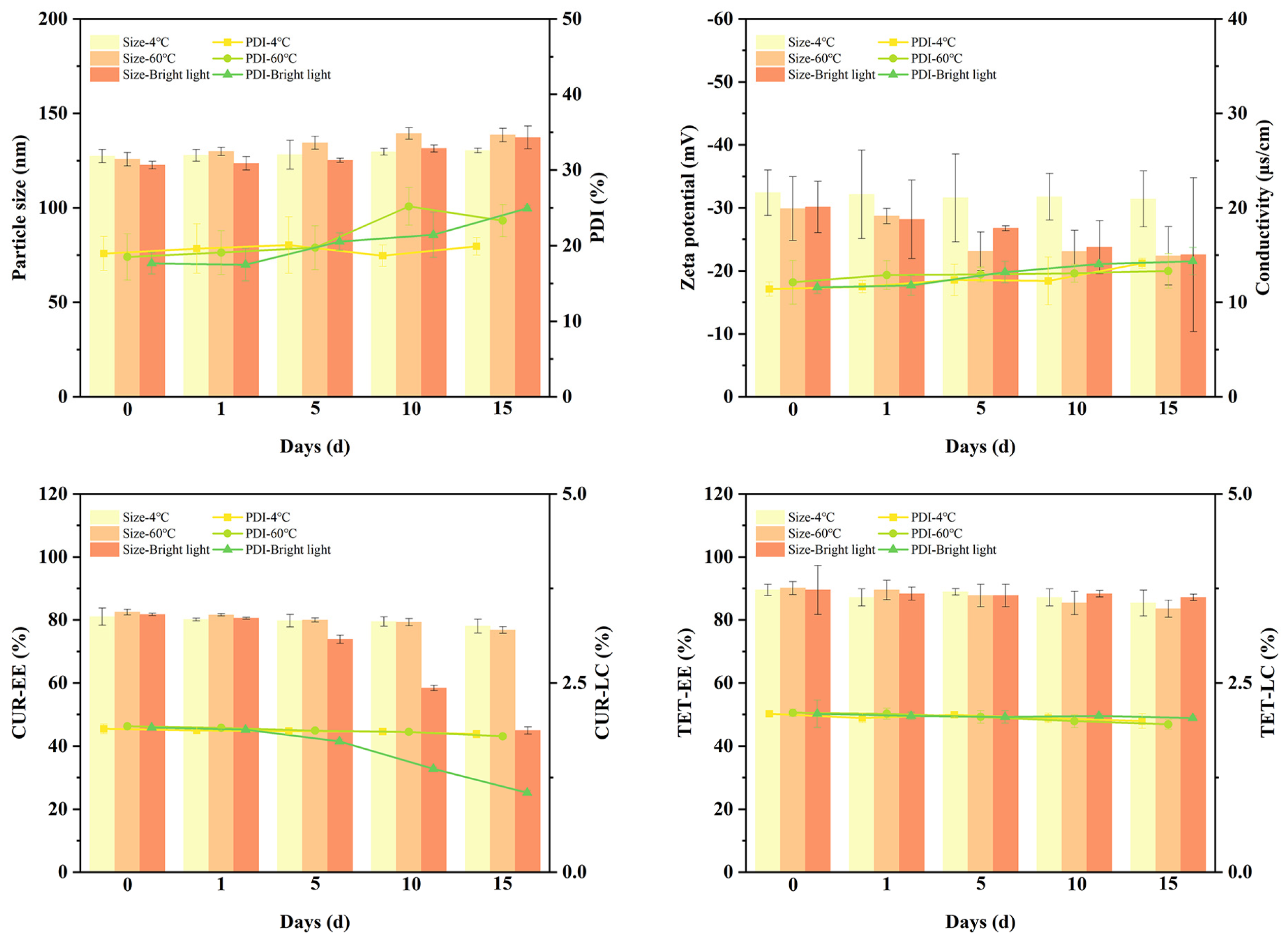
2.7. Stability Investigation of CT–DP–Lip
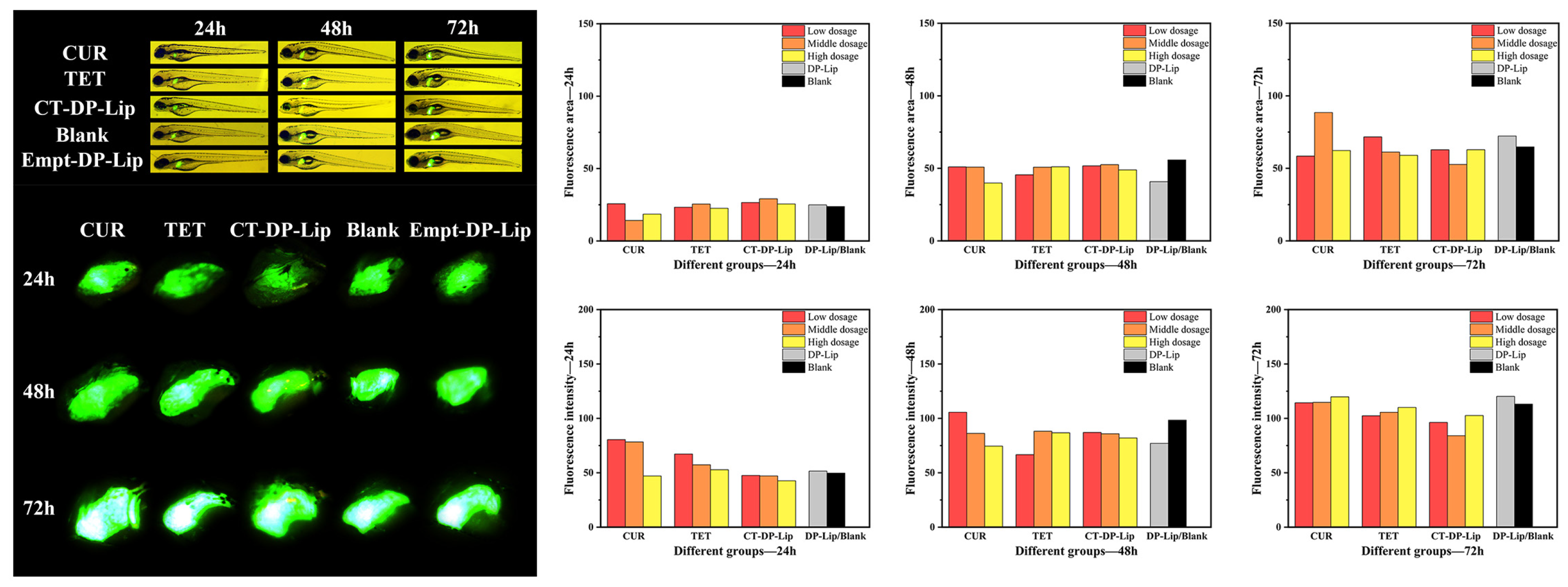
2.8. Zebrafish Liver Toxicity Test
2.8.1. The Morphological Development of Zebrafish
2.8.2. The Fluorescence Area and Intensity of Zebrafish Liver
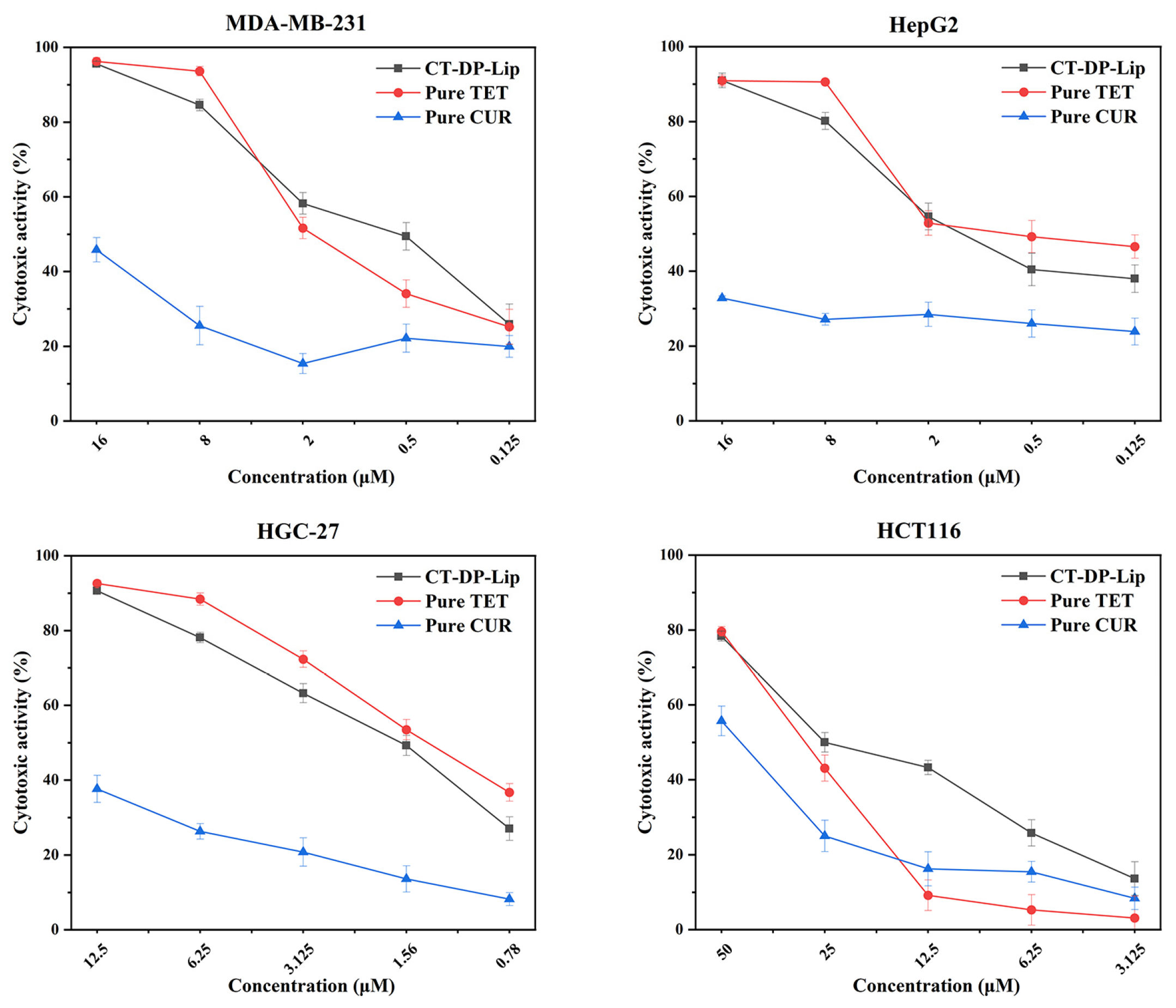
2.9. Anti–Tumor Effect In Vitro
3. Discussion
4. Materials and Methods
4.1. Materials
4.2. Animals and Cells
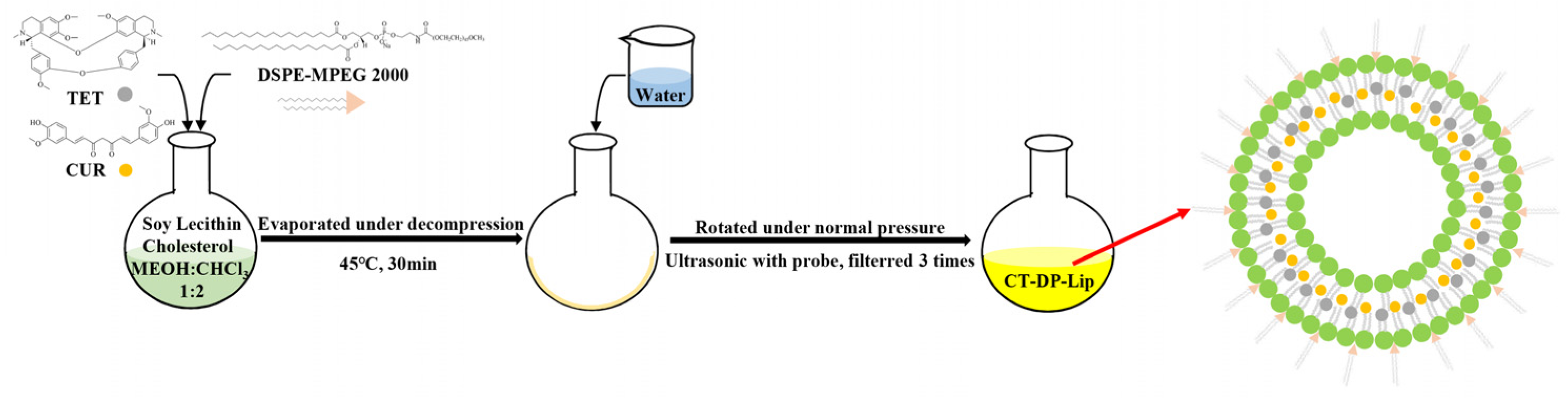
4.3. Preparation of Liposomes
4.4. Determination of Physical and Chemical Properties
4.5. Effect of DP Ratio on Drug–Loaded Liposomes
4.6. Determination of Release In Vitro
4.7. Stability Test
4.8. Zebrafish Liver Toxicity Test
4.9. Cell Culture
4.10. Anticancer Activity Assay In Vitro
4.11. Characterization Determination
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Zhou, H.; Beevers, C.S.; Huang, S. The targets of curcumin. Curr Drug Targets 2011, 12, 332–347. [Google Scholar] [CrossRef] [PubMed]
- He, Y.; Yue, Y.; Zheng, X.; Zhang, K.; Chen, S.; Du, Z. Curcumin, inflammation, and chronic diseases: How are they linked? Molecules 2015, 20, 9183–9213. [Google Scholar] [CrossRef] [PubMed]
- Guo, Y.; Liu, H.; Xiao, H.; Yuan, M.; Liu, Y.; Sedlarik, V.; Chin, W.C.; Liu, J.; Guo, L.; Li, C. Self-assembled Camptothecin derivatives—Curcuminoids conjugate for combinatorial chemo-photodynamic therapy to enhance anti-tumor efficacy. J. Photochem. Photobiol. B 2021, 215, 112124. [Google Scholar] [CrossRef] [PubMed]
- Gulcubuk, A.; Haktanir, D.; Cakiris, A.; Ustek, D.; Guzel, O.; Erturk, M.; Karabagli, M.; Akyazi, I.; Cicekci, H.; Altunatmaz, K.; et al. Effects of curcumin on proinflammatory cytokines and tissue injury in the early and late phases of experimental acute pancreatitis. Pancreatology 2013, 13, 347–354. [Google Scholar] [CrossRef]
- Moorthi, C.; Kathiresan, K. Fabrication of highly stable sonication assisted curcumin nanocrystals by nanoprecipitation method. Drug Invent. Today 2013, 5, 66–69. [Google Scholar] [CrossRef]
- Bhagya, N.; Chandrashekar, K.R. Tetrandrine and cancer—An overview on the molecular approach. Biomed. Pharmacother. 2018, 97, 624–632. [Google Scholar]
- Lin, Y.C.; Chang, C.W.; Wu, C.R. Anti-nociceptive, anti-inflammatory and toxicological evaluation of Fang-Ji-Huang-Qi-Tang in rodents. BMC Complement. Altern. Med. 2015, 15, 10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jiang, Y.; Liu, M.; Liu, H.; Liu, S. A critical review: Traditional uses, phytochemistry, pharmacology and toxicology of Stephania tetrandra S. Moore (Fen Fang Ji). Phytochem. Rev. 2020, 19, 449–489. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Qi, D.; Gao, Y.; Liang, C.; Zhang, Y.; Ma, Z.; Liu, Y.; Peng, H.; Zhang, Y.; Qin, H.; et al. History of uses, phytochemistry, pharmacological activities, quality control and toxicity of the root of Stephania tetrandra S. Moore: A review. J. Ethnopharmacol. 2020, 260, 112995. [Google Scholar] [CrossRef] [PubMed]
- Bhagya, N.; Chandrashekar, K.R. Tetrandrine—A molecule of wide bioactivity. Phytochemistry 2016, 125, 5–13. [Google Scholar] [CrossRef]
- Chidambaram, M.; Manavalan, R.; Kathiresan, K. Nanotherapeutics to overcome conventional cancer chemotherapy limitations. J. Pharm. Pharm. Sci. 2011, 14, 67–77. [Google Scholar] [CrossRef] [PubMed]
- Farhoudi, L.; Kesharwani, P.; Majeed, M.; Johnston, T.P.; Sahebkar, A. Polymeric nanomicelles of curcumin: Potential applications in cancer. Int. J. Pharm. 2022, 617, 121622. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Castro Bravo, K.M.; Liu, J. Targeted liposomal drug delivery: A nanoscience and biophysical perspective. Nanoscale Horiz. 2021, 6, 78–94. [Google Scholar] [CrossRef] [PubMed]
- Li, M.; Du, C.; Guo, N.; Teng, Y.; Meng, X.; Sun, H.; Li, S.; Yu, P.; Galons, H. Composition design and medical application of liposomes. Eur. J. Med. Chem. 2019, 164, 640–653. [Google Scholar] [CrossRef] [PubMed]
- Chavda, V.P.; Vihol, D.; Mehta, B.; Shah, D.; Patel, M.; Vora, L.K.; Pereira-Silva, M.; Paiva-Santos, A.C. Phytochemical-loaded liposomes for anticancer therapy: An updated review. Nanomedicine 2022, 17, 547–568. [Google Scholar] [CrossRef] [PubMed]
- Antimisiaris, S.G.; Marazioti, A.; Kannavou, M.; Natsaridis, E.; Gkartziou, F.; Kogkos, G.; Mourtas, S. Overcoming barriers by local drug delivery with liposomes. Adv. Drug Deliv. Rev. 2021, 174, 53–86. [Google Scholar] [CrossRef]
- Gregoriadis, G. Liposome Technology, 2nd ed.; CRC Press: Boca Raton, FL, USA, 1993. [Google Scholar]
- McCormack, B.; Gregoriadis, G. Drugs-in-cyclodextrins-in liposomes: A novel concept in drug delivery. Int. J. Pharm. 1994, 112, 249–258. [Google Scholar] [CrossRef]
- Jhan, S.; Pethe, A.M. Double-loaded liposomes encapsulating lycopene beta-cyclodextrin complexes: Preparation, optimization, and evaluation. J. Liposome Res. 2020, 30, 80–92. [Google Scholar] [CrossRef]
- Wang, Y.; Ouyang, Q.; Chang, X.; Yang, M.; He, J.; Tian, Y.; Sheng, J. Anti-photoaging effects of flexible nanoliposomes encapsulated Moringa oleifera Lam. isothiocyanate in UVB-induced cell damage in HaCaT cells. Drug Deliv. 2022, 29, 871–881. [Google Scholar] [CrossRef]
- Bi, H.; Xue, J.; Jiang, H.; Gao, S.; Yang, D.; Fang, Y.; Shi, K. Current developments in drug delivery with thermosensitive liposomes. Asian J. Pharm. Sci. 2019, 14, 365–379. [Google Scholar] [CrossRef]
- Gregoriadis, G. Stealth Liposomes; Lasic, D.D., Martin, F., Eds.; CRC Press: Boca Raton, FL, USA, 1995. [Google Scholar]
- Papahadjopoulos, D.; Allen, T.M.; Gabizon, A.; Mayhew, E.; Matthay, K.; Huang, S.K.; Lee, K.D.; Woodle, M.C.; Lasic, D.D.; Redemann, C. Sterically stabilized liposomes: Improvements in pharmacokinetics and antitumor therapeutic efficacy. Proc. Natl. Acad. Sci. USA 1991, 88, 11460–11464. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Klibanov, A.L.; Maruyama, K.; Torchilin, V.P.; Huang, L. Amphipathic polyethyleneglycols effectively prolong the circulation time of liposomes. FEBS Lett 1990, 268, 235–237. [Google Scholar] [CrossRef] [Green Version]
- Chen, Y.; Chen, J.; Cheng, Y.; Luo, L.; Zheng, P.; Tong, Y.; Li, Z. A lyophilized sterically stabilized liposome-containing docetaxel: In vitro and in vivo evaluation. J. Liposome Res. 2016, 27, 64–73. [Google Scholar] [CrossRef] [PubMed]
- Sriwongsitanont, S.; Ueno, M. Effect of a PEG lipid (DSPE-PEG2000) and freeze-thawing process on phospholipid vesicle size and lamellarity. Colloid Polym. Sci. 2004, 282, 753–760. [Google Scholar] [CrossRef]
- Alhakamy, N.A.; Ahmed, O.A.A.; Fahmy, U.A.; Md, S. Development and In Vitro Evaluation of 2-Methoxyestradiol Loaded Polymeric Micelles for Enhancing Anticancer Activities in Prostate Cancer. Polymers 2021, 13, 884. [Google Scholar] [CrossRef]
- Iurciuc, C.E.; Atanase, L.I.; Jérôme, C.; Sol, V.; Martin, P.; Popa, M.; Ochiuz, L. olysaccharides-Based Complex Particles’ Protective Role on the Stability and Bioactivity of Immobilized Curcumin. Int. J. Mol. Sci. 2021, 22, 3075. [Google Scholar] [CrossRef]
- Liu, H.; Yuan, M.; Liu, Y.; Guo, Y.; Xiao, H.; Guo, L.; Liu, F. Self-Monitoring and Self-Delivery of Self-Assembled Fluorescent Nanoparticles in Cancer Therapy. Int. J. Nanomed. 2021, 16, 2487–2499. [Google Scholar] [CrossRef]
- Zhang, L.; Yang, S.; Wong, L.R.; Xie, H.; Ho, P.C.L. In Vitro and In Vivo Comparison of Curcumin-Encapsulated Chitosan-Coated Poly(lactic-co-glycolic acid) Nanoparticles and Curcumin/Hydroxypropyl-β-Cyclodextrin Inclusion Complexes Administered Intranasally as Therapeutic Strategies for Alzheimer’s Disease. Mol. Pharm. 2020, 17, 4256–4269. [Google Scholar] [CrossRef]
- Su, W.; Liang, Y.; Meng, Z.; Chen, X.; Lu, M.; Han, X.; Deng, X.; Zhang, Q.; Zhu, H.; Fu, T. Inhalation of Tetrandrine-hydroxypropyl-β-cyclodextrin Inclusion Complexes for Pulmonary Fibrosis Treatment. Mol. Pharm. 2020, 17, 1596–1607. [Google Scholar] [CrossRef]
- Chen, W.T.; Wu, H.T.; Chang, I.C.; Chen, H.W.; Fang, W.P. Preparation of curcumin-loaded liposome with high bioavailability by a novel method of high pressure processing. Chem. Phys. Lipids 2022, 244, 105191. [Google Scholar] [CrossRef]
- FFan, Y.; Sahdev, P.; Ochyl, L.J.; Akerberg, J.J.; Moon, J.J. Cationic liposome-hyaluronic acid hybrid nanoparticles for intranasal vaccination with subunit antigens. J. Control. Release 2015, 208, 121–129. [Google Scholar] [CrossRef] [Green Version]
- Németh, Z.; Pallagi, E.; Dobó, D.G.; Kozma, G.; Kónya, Z.; Csóka, I. An Updated Risk Assessment as Part of the QbD-Based Liposome Design and Development. Pharmaceutics 2021, 13, 1071. [Google Scholar] [CrossRef] [PubMed]
- Cheng, Z.; Liu, R.; Jiang, X. Spectroscopic studies on the interaction between tetrandrine and two serum albumins by chemometrics methods. Spectrochim. Acta A Mol. Biomol. Spectrosc. 2013, 92, 105. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, X.; Wu, Z.; Guo, C.; Guo, H.; Su, Y.; Chen, Q.; Sun, C.; Liu, Q.; Chen, D.; Mu, H. Hypoxia responsive nano-drug delivery system based on angelica polysaccharide for liver cancer therapy. Drug Deliv. 2022, 29, 138–148. [Google Scholar] [CrossRef] [PubMed]
- Elizalde-Velázquez, G.A.; Rosas-Ramírez, J.R.; Raldua, D.; García-Medina, S.; Orozco-Hernández, J.M.; Pérez, K.R.; Islas-Flores, H.; Galar-Martínez, M.; Guzmán-García, X.; Gómez-Oliván, L.M. Low concentrations of ciprofloxacin alone and in combination with paracetamol induce oxidative stress, upregulation of apoptotic-related genes, histological alterations in the liver, and genotoxicity in Danio rerio. Chemosphere 2022, 294, 133667. [Google Scholar] [CrossRef]
- Liu, D.; Zhang, Q.; Wang, J.; Guan, S.; Cai, D.; Liu, J. Inhibition of growth and metastasis of breast cancer by targeted delivery of 17-hydroxy-jolkinolide B via hyaluronic acid-coated liposomes. Carbohydr. Polym. 2021, 257, 117572. [Google Scholar] [CrossRef]
- Gholibegloo, E.; Mortezazadeh, T.; Salehian, F.; Ramazani, A.; Amanlou, M.; Khoobi, M. Improved curcumin loading, release, solubility and toxicity by tuning the molar ratio of cross-linker to beta-cyclodextrin. Carbohydr. Polym. 2019, 213, 70–78. [Google Scholar] [CrossRef]
- Deng, M.; Chen, H.; Xie, L.; Liu, K.; Zhang, X.; Li, X. Tea saponins as natural emulsifiers and cryoprotectants to prepare silymarin nanoemulsion. LWT 2022, 156, 113042. [Google Scholar] [CrossRef]
- Pham, D.T.; Thao, N.T.P.; Thuy, B.T.P.; Tran, V.; Nguyen, T.Q.C.; Nguyen, N.N.T. Silk fibroin hydrogel containing Sesbania sesban L. extract for rheumatoid arthritis treatment. Drug Deliv 2022, 29, 882–888. [Google Scholar] [CrossRef]
- Song, J.; Long, J.; Xie, L.; Sun, Q.; Zhang, L.; Chen, H.; Deng, M.; Li, X. Solubilization and changes of physicochemical properties of baicalin by nano sponge, and toxicity of zebrafish liver. J. Drug Deliv. Sci. Technol. 2020, 60, 102003. [Google Scholar] [CrossRef]
- Liu, Y.S.; Yuan, M.H.; Zhang, C.Y.; Liu, H.M.; Liu, J.R.; Wei, A.L.; Ye, Q.; Zeng, B.; Li, M.F.; Guo, Y.P.; et al. Puerariae Lobatae radix flavonoids and puerarin alleviate alcoholic liver injury in zebrafish by regulating alcohol and lipid metabolism. Biomed. Pharm. 2021, 134, 111121. [Google Scholar] [CrossRef] [PubMed]
- Ye, Q.; Liu, H.; Fang, C.; Liu, Y.; Liu, X.; Liu, J.; Zhang, C.; Zhang, T.; Peng, C.; Guo, L. Cardiotoxicity evaluation and comparison of diterpene alkaloids on zebrafish. Drug Chem. Toxicol. 2021, 44, 294–301. [Google Scholar] [CrossRef] [PubMed]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Song, J.-W.; Liu, Y.-S.; Guo, Y.-R.; Zhong, W.-X.; Guo, Y.-P.; Guo, L. Nano–Liposomes Double Loaded with Curcumin and Tetrandrine: Preparation, Characterization, Hepatotoxicity and Anti–Tumor Effects. Int. J. Mol. Sci. 2022, 23, 6858. https://doi.org/10.3390/ijms23126858
Song J-W, Liu Y-S, Guo Y-R, Zhong W-X, Guo Y-P, Guo L. Nano–Liposomes Double Loaded with Curcumin and Tetrandrine: Preparation, Characterization, Hepatotoxicity and Anti–Tumor Effects. International Journal of Molecular Sciences. 2022; 23(12):6858. https://doi.org/10.3390/ijms23126858
Chicago/Turabian StyleSong, Jia-Wen, Yu-Shi Liu, Yu-Rou Guo, Wen-Xiao Zhong, Yi-Ping Guo, and Li Guo. 2022. "Nano–Liposomes Double Loaded with Curcumin and Tetrandrine: Preparation, Characterization, Hepatotoxicity and Anti–Tumor Effects" International Journal of Molecular Sciences 23, no. 12: 6858. https://doi.org/10.3390/ijms23126858
APA StyleSong, J.-W., Liu, Y.-S., Guo, Y.-R., Zhong, W.-X., Guo, Y.-P., & Guo, L. (2022). Nano–Liposomes Double Loaded with Curcumin and Tetrandrine: Preparation, Characterization, Hepatotoxicity and Anti–Tumor Effects. International Journal of Molecular Sciences, 23(12), 6858. https://doi.org/10.3390/ijms23126858





