Neurotransmitters—Key Factors in Neurological and Neurodegenerative Disorders of the Central Nervous System
Abstract
1. Introduction
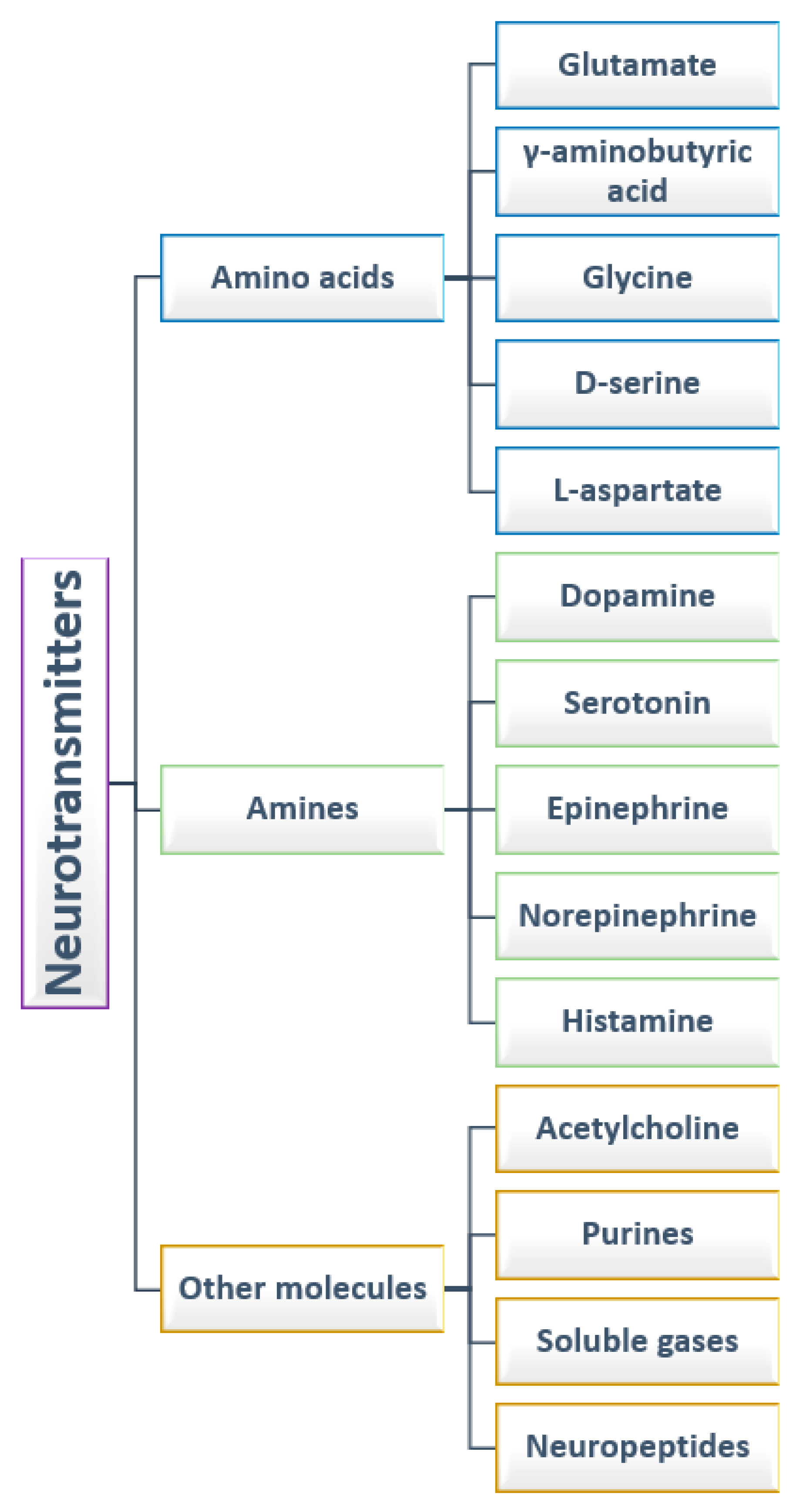
2. Neurotransmitters
2.1. Canonical Neurotransmitters
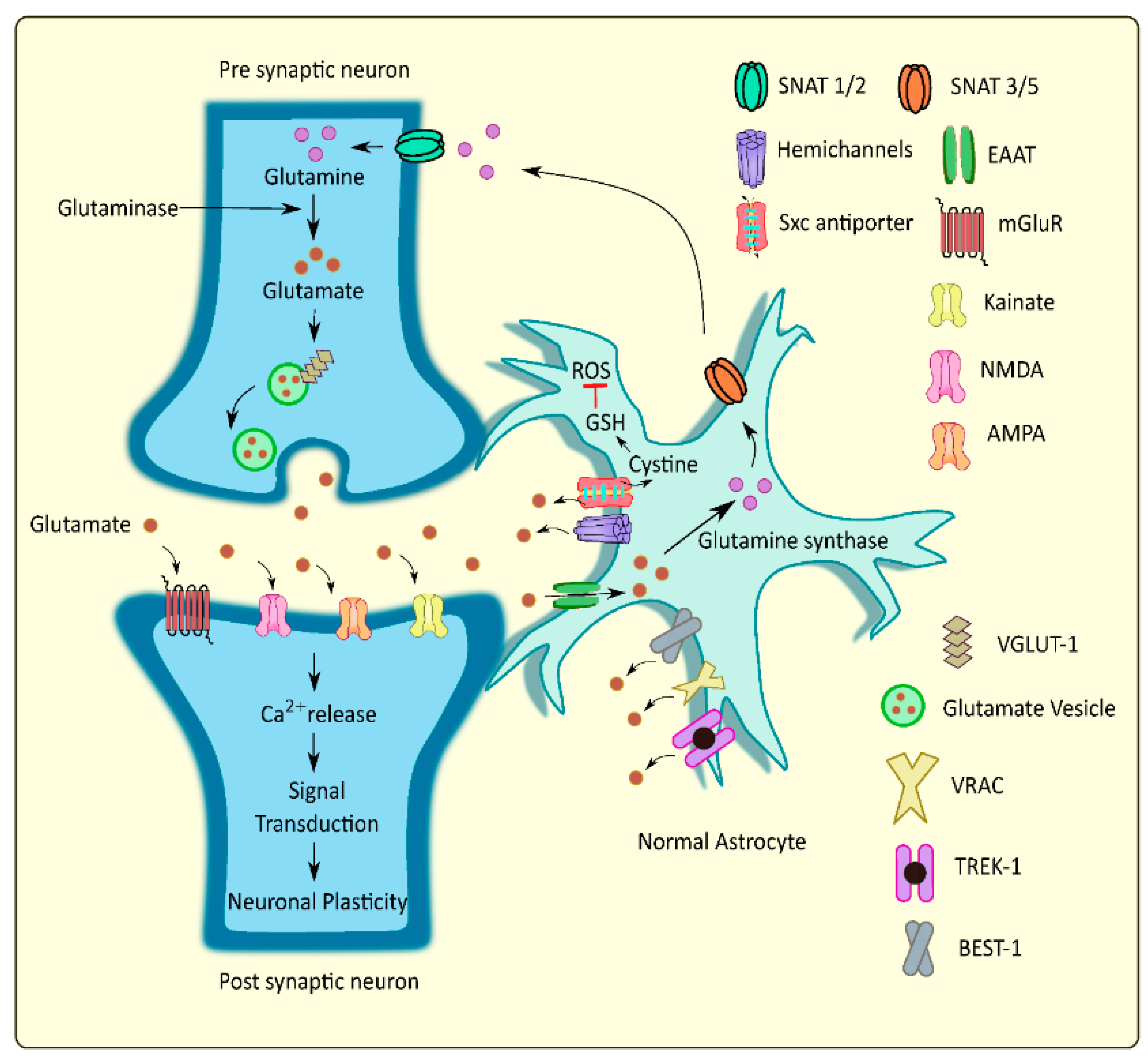
2.1.1. Amino Acids
2.1.2. Amines
2.1.3. Other Molecules
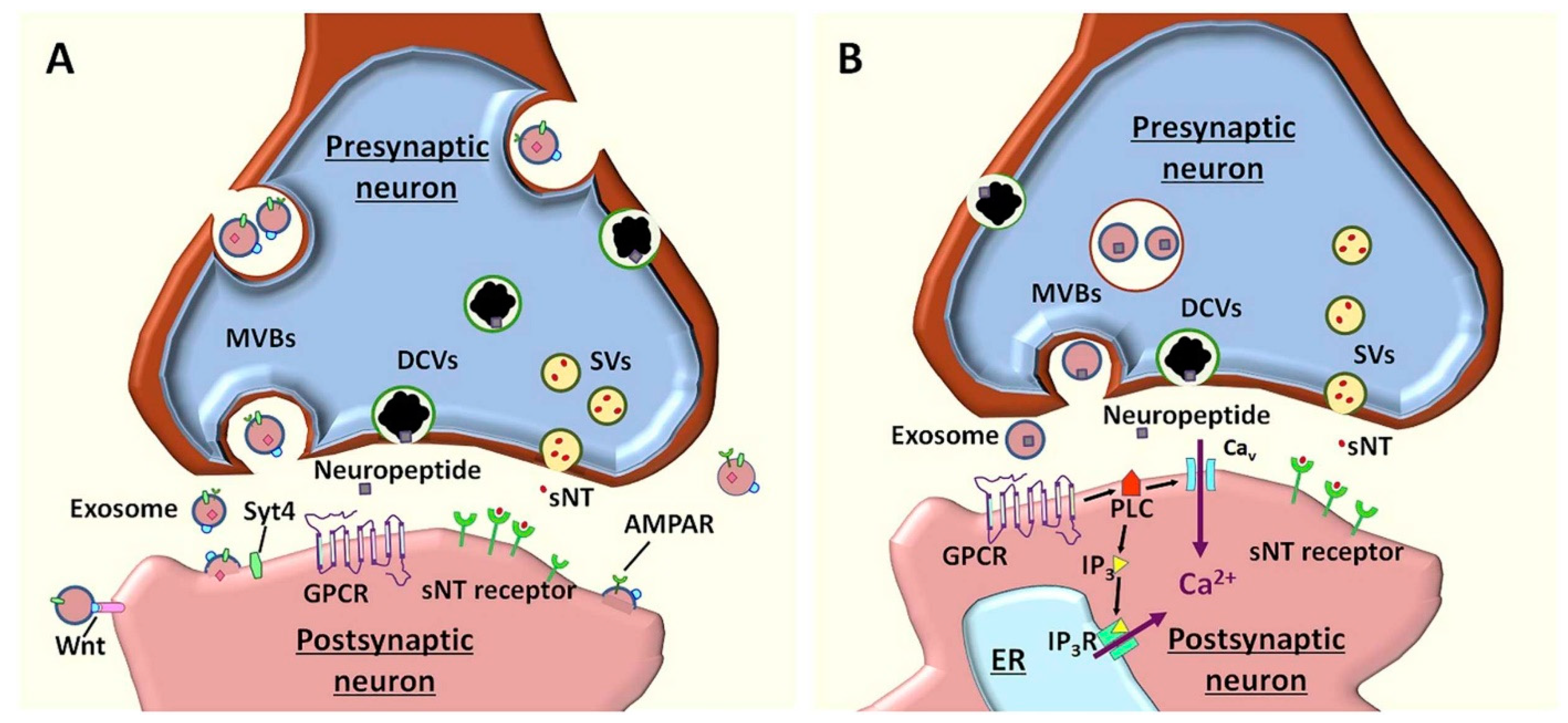
2.2. Noncanonical Neurotransmitters
3. Neurotransmitter Disorders of the CNS
3.1. Epilepsy
3.2. Multiple Sclerosis
3.3. Autism
3.4. Alzheimer’s Disease
3.5. Parkinson’s Disease
3.6. Huntington’s Disease
3.7. Schizophrenia
3.8. Depression
3.9. Amyotrophic Lateral Sclerosis
4. Neurotransmitters Detection
5. Modulation of Neurotransmitters and Neurotransmitter Transporters as a Therapeutic Strategy
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Xia, X.; Wang, Y.; Qin, Y.; Zhao, S.; Zheng, J.C. Exosome: A novel neurotransmission modulator or non-canonical neurotransmitter? Ageing Res. Rev. 2022, 74, 101558. [Google Scholar] [CrossRef]
- Hanada, T. Ionotropic Glutamate Receptors in Epilepsy: A Review Focusing on AMPA and NMDA Receptors. Biomolecules 2020, 10, 464. [Google Scholar] [CrossRef]
- Banerjee, S.; McCracken, S.; Hossain, F.; Slaughter, G. Electrochemical Detection of Neurotransmitters. Biosensors 2020, 10, 101. [Google Scholar] [CrossRef]
- Moini, J.; Koenitzer, J.; LoGalbo, A. Chapter 2—Brain neurotransmitters. In Global Emergency of Mental Disorders; Moini, J., Koenitzer, J., LoGalbo, A., Eds.; Academic Press: Cambridge, MA, USA, 2021; pp. 31–40. [Google Scholar] [CrossRef]
- Tiedje, K.E.; Stevens, K.; Barnes, S.; Weaver, D. β-Alanine as a small molecule neurotransmitter. Neurochem. Int. 2010, 57, 177–188. [Google Scholar] [CrossRef]
- Bhat, S.; El-Kasaby, A.; Freissmuth, M.; Sucic, S. Functional and Biochemical Consequences of Disease Variants in Neurotransmitter Transporters: A Special Emphasis on Folding and Trafficking Deficits. Pharmacol. Ther. 2021, 222, 107785. [Google Scholar] [CrossRef]
- Yadav, D.; Kumar, P. Restoration and targeting of aberrant neurotransmitters in Parkinson’s disease therapeutics. Neurochem. Int. 2022, 156, 105327. [Google Scholar] [CrossRef]
- Arumugasamy, S.K.; Chellasamy, G.; Gopi, S.; Govindaraju, S.; Yun, K. Current advances in the detection of neurotransmitters by nanomaterials: An update. TrAC Trends Anal. Chem. 2020, 123, 115766. [Google Scholar] [CrossRef]
- Niyonambaza, S.D.; Kumar, P.; Xing, P.; Mathault, J.; De Koninck, P.; Boisselier, E.; Boukadoum, M.; Miled, A. A Review of Neurotransmitters Sensing Methods for Neuro-Engineering Research. Appl. Sci. 2019, 9, 4719. [Google Scholar] [CrossRef]
- Onose, G.; Anghelescu, A.; Blendea, D.; Ciobanu, V.; Daia, C.; Firan, F.C.; Oprea, M.; Spinu, A.; Popescu, C.; Ionescu, A.; et al. Cellular and Molecular Targets for Non-Invasive, Non-Pharmacological Therapeutic/Rehabilitative Interventions in Acute Ischemic Stroke. Int. J. Mol. Sci. 2022, 23, 907. [Google Scholar] [CrossRef]
- Tam, K.Y.; Ju, Y. Pathological mechanisms and therapeutic strategies for Alzheimer’s disease. Neural. Regen. Res. 2022, 17, 543–549. [Google Scholar] [CrossRef]
- Satarker, S.; Bojja, S.L.; Gurram, P.C.; Mudgal, J.; Arora, D.; Nampoothiri, M. Astrocytic Glutamatergic Transmission and Its Implications in Neurodegenerative Disorders. Cells 2022, 11, 1139. [Google Scholar] [CrossRef] [PubMed]
- Murley, A.G.; Rowe, J.B. Neurotransmitter deficits from frontotemporal lobar degeneration. Brain 2018, 141, 1263–1285. [Google Scholar] [CrossRef]
- Le Gall, L.; Anakor, E.; Connolly, O.; Vijayakumar, U.G.; Duddy, W.J.; Duguez, S. Molecular and Cellular Mechanisms Affected in ALS. J. Pers. Med. 2020, 10, 101. [Google Scholar] [CrossRef] [PubMed]
- Iovino, L.; Tremblay, M.E.; Civiero, L. Glutamate-induced excitotoxicity in Parkinson’s disease: The role of glial cells. J. Pharmacol. Sci. 2020, 144, 151–164. [Google Scholar] [CrossRef] [PubMed]
- Moraes, B.J.; Coelho, P.; Fão, L.; Ferreira, I.L.; Rego, A.C. Modified Glutamatergic Postsynapse in Neurodegenerative Disorders. Neuroscience 2021, 454, 116–139. [Google Scholar] [CrossRef]
- Kazama, M.; Kato, Y.; Kakita, A.; Noguchi, N.; Urano, Y.; Masui, K.; Niida-Kawaguchi, M.; Yamamoto, T.; Watabe, K.; Kitagawa, K.; et al. Astrocytes release glutamate via cystine/glutamate antiporter upregulated in response to increased oxidative stress related to sporadic amyotrophic lateral sclerosis. Neuropathology 2020, 40, 587–598. [Google Scholar] [CrossRef]
- Mohamed, L.A.; Markandaiah, S.S.; Bonanno, S.; Pasinelli, P.; Trotti, D. Excess glutamate secreted from astrocytes drives upregulation of P-glycoprotein in endothelial cells in amyotrophic lateral sclerosis. Exp. Neurol. 2019, 316, 27–38. [Google Scholar] [CrossRef]
- Gao, F.; Yin, X.; Edden, R.A.E.; Evans, A.C.; Xu, J.; Cao, G.; Li, H.; Li, M.; Zhao, B.; Wang, J.; et al. Altered hippocampal GABA and glutamate levels and uncoupling from functional connectivity in multiple sclerosis. Hippocampus 2018, 28, 813–823. [Google Scholar] [CrossRef]
- Malekzadeh Shafaroudi, M.; Zarei, H.; Malekzadeh Shafaroudi, A.; Karimi, N.; Abedini, M. The Relationship between Glutamate and Multiple Sclerosis. Int. Biol. Biomed. J. 2018, 4, 1–13. [Google Scholar]
- Bukke, V.N.; Archana, M.; Villani, R.; Romano, A.D.; Wawrzyniak, A.; Balawender, K.; Orkisz, S.; Beggiato, S.; Serviddio, G.; Cassano, T. The Dual Role of Glutamatergic Neurotransmission in Alzheimer’s Disease: From Pathophysiology to Pharmacotherapy. Int. J. Mol. Sci. 2020, 21, 7452. [Google Scholar] [CrossRef]
- Madeira, C.; Vargas-Lopes, C.; Brandão, C.O.; Reis, T.; Laks, J.; Panizzutti, R.; Ferreira, S.T. Elevated Glutamate and Glutamine Levels in the Cerebrospinal Fluid of Patients With Probable Alzheimer’s Disease and Depression. Front. Psychiatry 2018, 9, 561. [Google Scholar] [CrossRef] [PubMed]
- Findley, C.A.; Bartke, A.; Hascup, K.N.; Hascup, E.R. Amyloid Beta-Related Alterations to Glutamate Signaling Dynamics During Alzheimer’s Disease Progression. ASN Neuro 2019, 11, 1759091419855541. [Google Scholar] [CrossRef] [PubMed]
- Dejakaisaya, H.; Kwan, P.; Jones, N.C. Astrocyte and glutamate involvement in the pathogenesis of epilepsy in Alzheimer’s disease. Epilepsia 2021, 62, 1485–1493. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.; Zhang, S.; Fu, P.; Zhang, Z.; Lin, K.; Ko, J.K.; Yung, K.K. Roles of Glutamate Receptors in Parkinson’s Disease. Int. J. Mol. Sci. 2019, 20, 4391. [Google Scholar] [CrossRef] [PubMed]
- Mironova, Y.S.; Zhukova, I.A.; Zhukova, N.G.; Alifirova, V.M.; Izhboldina, O.P.; Latypova, A.V. Parkinson’s disease and glutamate excitotoxicity. Zhurnal Nevrol. Psikhiatrii Im. Korsakova 2018, 118, 50–54. [Google Scholar] [CrossRef]
- Tsuang, D.W.; Greenwood, T.A.; Jayadev, S.; Davis, M.; Shutes-David, A.; Bird, T.D. A Genetic Study of Psychosis in Huntington’s Disease: Evidence for the Involvement of Glutamate Signaling Pathways. J. Huntingt. Dis. 2018, 7, 51–59. [Google Scholar] [CrossRef]
- Alcoreza, O.B.; Patel, D.C.; Tewari, B.P.; Sontheimer, H. Dysregulation of ambient glutamate and glutamate receptors in epilepsy: An astrocytic perspective. Front. Neurol. 2021, 12, 362. [Google Scholar] [CrossRef]
- Koshal, P.; Jamwal, S.; Kumar, P. Glucagon-like Peptide-1 (GLP-1) and neurotransmitters signaling in epilepsy: An insight review. Neuropharmacology 2018, 136, 271–279. [Google Scholar] [CrossRef]
- Pokusaeva, K.; Johnson, C.; Luk, B.; Uribe, G.; Fu, Y.; Oezguen, N.; Matsunami, R.K.; Lugo, M.; Major, A.; Mori-Akiyama, Y.; et al. GABA-producing Bifidobacterium dentium modulates visceral sensitivity in the intestine. Neurogastroenterol. Motil. 2017, 29, e12904. [Google Scholar] [CrossRef]
- Strandwitz, P. Neurotransmitter modulation by the gut microbiota. Brain Res. 2018, 1693, 128–133. [Google Scholar] [CrossRef]
- Barrett, E.; Ross, R.P.; O’Toole, P.W.; Fitzgerald, G.F.; Stanton, C. γ-Aminobutyric acid production by culturable bacteria from the human intestine. J. Appl. Microbiol. 2012, 113, 411–417. [Google Scholar] [CrossRef] [PubMed]
- Bauer, K.C.; Huus, K.E.; Finlay, B.B. Microbes and the mind: Emerging hallmarks of the gut microbiota–brain axis. Cell. Microbiol. 2016, 18, 632–644. [Google Scholar] [CrossRef] [PubMed]
- Ochoa-de la Paz, L.; Zenteno, E.; Gulias-Cañizo, R.; Quiroz-Mercado, H. Taurine and GABA neurotransmitter receptors, a relationship with therapeutic potential? Expert Rev. Neurother. 2019, 19, 289–291. [Google Scholar] [CrossRef] [PubMed]
- Duman, R.S.; Sanacora, G.; Krystal, J.H. Altered Connectivity in Depression: GABA and Glutamate Neurotransmitter Deficits and Reversal by Novel Treatments. Neuron 2019, 102, 75–90. [Google Scholar] [CrossRef]
- Puts, N.A.J.; Wodka, E.L.; Harris, A.D.; Crocetti, D.; Tommerdahl, M.; Mostofsky, S.H.; Edden, R.A.E. Reduced GABA and altered somatosensory function in children with autism spectrum disorder. Autism Res. 2017, 10, 608–619. [Google Scholar] [CrossRef] [PubMed]
- Kolodny, T.; Schallmo, M.-P.; Gerdts, J.; Edden, R.A.E.; Bernier, R.A.; Murray, S.O. Concentrations of Cortical GABA and Glutamate in Young Adults With Autism Spectrum Disorder. Autism Res. 2020, 13, 1111–1129. [Google Scholar] [CrossRef]
- Kumar, V.; Vajawat, B.; Rao, N.P. Frontal GABA in schizophrenia: A meta-analysis of 1H-MRS studies. World J. Biol. Psychiatry 2021, 22, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Guazzi, M.; Striano, P. GABA strikes down again in epilepsy. Ann. Transl. Med. 2019, 7, 57. [Google Scholar] [CrossRef]
- Gong, T.; Liu, Y.; Chen, Y.; Lin, L.; Lin, Y.; Wang, G. Focal corticarl dysplasia in epilepsy is associated with GABA increase. NeuroImage Clin. 2021, 31, 102763. [Google Scholar] [CrossRef]
- Müller, J.; Timmermann, A.; Henning, L.; Müller, H.; Steinhäuser, C.; Bedner, P. Astrocytic GABA accumulation in experimental temporal lobe epilepsy. Front. Neurol. 2020, 11, 614923. [Google Scholar] [CrossRef]
- Cao, G.; Edden, R.A.E.; Gao, F.; Li, H.; Gong, T.; Chen, W.; Liu, X.; Wang, G.; Zhao, B. Reduced GABA levels correlate with cognitive impairment in patients with relapsing-remitting multiple sclerosis. Eur. Radiol. 2018, 28, 1140–1148. [Google Scholar] [CrossRef] [PubMed]
- Arm, J.; Oeltzschner, G.; Al-iedani, O.; Lea, R.; Lechner-Scott, J.; Ramadan, S. Altered in vivo brain GABA and glutamate levels are associated with multiple sclerosis central fatigue. Eur. J. Radiol. 2021, 137, 109610. [Google Scholar] [CrossRef] [PubMed]
- Jiménez-Balado, J.; Eich, T.S. GABAergic dysfunction, neural network hyperactivity and memory impairments in human aging and Alzheimer’s disease. Semin. Cell Dev. Biol. 2021, 116, 146–159. [Google Scholar] [CrossRef] [PubMed]
- Bi, D.; Wen, L.; Wu, Z.; Shen, Y. GABAergic dysfunction in excitatory and inhibitory (E/I) imbalance drives the pathogenesis of Alzheimer’s disease. Alzheimer’s Dement. 2020, 16, 1312–1329. [Google Scholar] [CrossRef] [PubMed]
- Govindpani, K.; Turner, C.; Waldvogel, H.J.; Faull, R.L.M.; Kwakowsky, A. Impaired Expression of GABA Signaling Components in the Alzheimer’s Disease Middle Temporal Gyrus. Int. J. Mol. Sci. 2020, 21, 8704. [Google Scholar] [CrossRef] [PubMed]
- Garaschuk, O.; Verkhratsky, A. GABAergic astrocytes in Alzheimer’s disease. Aging 2019, 11, 1602. [Google Scholar] [CrossRef]
- van Nuland, A.J.M.; den Ouden, H.E.M.; Zach, H.; Dirkx, M.F.M.; van Asten, J.J.A.; Scheenen, T.W.J.; Toni, I.; Cools, R.; Helmich, R.C. GABAergic changes in the thalamocortical circuit in Parkinson’s disease. Hum. Brain Mapp. 2020, 41, 1017–1029. [Google Scholar] [CrossRef]
- O’Gorman Tuura, R.L.; Baumann, C.R.; Baumann-Vogel, H. Beyond dopamine: GABA, glutamate, and the axial symptoms of Parkinson disease. Front. Neurol. 2018, 9, 806. [Google Scholar] [CrossRef]
- Murueta-Goyena, A.; Andikoetxea, A.; Gómez-Esteban, J.C.; Gabilondo, I. Contribution of the GABAergic system to non-motor manifestations in premotor and early stages of Parkinson’s disease. Front. Pharmacol. 2019, 10, 1294. [Google Scholar] [CrossRef]
- Garret, M.; Du, Z.; Chazalon, M.; Cho, Y.H.; Baufreton, J. Alteration of GABAergic neurotransmission in Huntington’s disease. CNS Neurosci. Ther. 2018, 24, 292–300. [Google Scholar] [CrossRef]
- Hsu, Y.-T.; Chang, Y.-G.; Chern, Y. Insights into GABAAergic system alteration in Huntington’s disease. Open Biol. 2018, 8, 180165. [Google Scholar] [CrossRef] [PubMed]
- Kölker, S. Metabolism of amino acid neurotransmitters: The synaptic disorder underlying inherited metabolic diseases. J. Inherit. Metab. Dis. 2018, 41, 1055–1063. [Google Scholar] [CrossRef]
- Mustafa, A.K.; Kim, P.M.; Snyder, S.H. D-Serine as a putative glial neurotransmitter. Neuron Glia Biol. 2004, 1, 275–281. [Google Scholar] [CrossRef][Green Version]
- Neame, S.; Safory, H.; Radzishevsky, I.; Touitou, A.; Marchesani, F.; Marchetti, M.; Kellner, S.; Berlin, S.; Foltyn, V.N.; Engelender, S.; et al. The NMDA receptor activation by d-serine and glycine is controlled by an astrocytic Phgdh-dependent serine shuttle. Proc. Natl. Acad. Sci. USA 2019, 116, 20736–20742. [Google Scholar] [CrossRef] [PubMed]
- Juliá-Palacios, N.; Molina-Anguita, C.; Sigatulina Bondarenko, M.; Cortès-Saladelafont, E.; Aparicio, J.; Cuadras, D.; Horvath, G.; Fons, C.; Artuch, R.; García-Cazorla, À.; et al. Monoamine neurotransmitters in early epileptic encephalopathies: New insights into pathophysiology and therapy. Dev. Med. Child Neurol. 2022. online ahead of print. [Google Scholar] [CrossRef]
- Franco, R.; Reyes-Resina, I.; Navarro, G. Dopamine in Health and Disease: Much More Than a Neurotransmitter. Biomedicines 2021, 9, 109. [Google Scholar] [CrossRef] [PubMed]
- Swamy, B.K.; Shiprath, K.; Rakesh, G.; Ratnam, K.V.; Manjunatha, H.; Janardan, S.; Naidu, K.C.B.; Ramesh, S.; Suresh Babu, K.; Ratnamala, A. Simultaneous detection of dopamine, tyrosine and ascorbic acid using NiO/graphene modified graphite electrode. Biointerface Res. Appl. Chem. 2020, 10, 5599–5609. [Google Scholar] [CrossRef]
- Swamy, B.K.; Shiprath, K.; Ratnam, K.V.; Manjunatha, H.; Janardan, S.; Ratnamala, A.; Naidu, K.C.B.; Ramesh, S.; Babu, K.S. Electrochemical Detection of Dopamine and Tyrosine using Metal oxide (MO, M=Cu and Ni) Modified Graphite Electrode: A Comparative Study. Biointerface Res. Appl. Chem. 2020, 10, 6460–6473. [Google Scholar] [CrossRef]
- Ou, Y.; Buchanan, A.M.; Witt, C.E.; Hashemi, P. Frontiers in electrochemical sensors for neurotransmitter detection: Towards measuring neurotransmitters as chemical diagnostics for brain disorders. Anal. Methods 2019, 11, 2738–2755. [Google Scholar] [CrossRef]
- Linan-Rico, A.; Ochoa-Cortes, F.; Beyder, A.; Soghomonyan, S.; Zuleta-Alarcon, A.; Coppola, V.; Christofi, F.L. Mechanosensory Signaling in Enterochromaffin Cells and 5-HT Release: Potential Implications for Gut Inflammation. Front. Neurosci. 2016, 10, 564. [Google Scholar] [CrossRef]
- Camilleri, M. Serotonin in the gastrointestinal tract. Curr. Opin. Endocrinol. Diabetes Obes. 2009, 16, 53–59. [Google Scholar] [CrossRef] [PubMed]
- Reigstad, C.S.; Salmonson, C.E.; Rainey, J.F., III; Szurszewski, J.H.; Linden, D.R.; Sonnenburg, J.L.; Farrugia, G.; Kashyap, P.C. Gut microbes promote colonic serotonin production through an effect of short-chain fatty acids on enterochromaffin cells. FASEB J. 2015, 29, 1395–1403. [Google Scholar] [CrossRef] [PubMed]
- Burnstock, G. Historical review: ATP as a neurotransmitter. Trends Pharmacol. Sci. 2006, 27, 166–176. [Google Scholar] [CrossRef] [PubMed]
- Nowaczyk, A.; Kowalska, M.; Nowaczyk, J.; Grześk, G. Carbon Monoxide and Nitric Oxide as Examples of the Youngest Class of Transmitters. Int. J. Mol. Sci. 2021, 22, 6029. [Google Scholar] [CrossRef] [PubMed]
- Folasire, O.; Mills, K.A.; Sellers, D.J.; Chess-Williams, R. Three Gaseous Neurotransmitters, Nitric oxide, Carbon Monoxide, and Hydrogen Sulfide, Are Involved in the Neurogenic Relaxation Responses of the Porcine Internal Anal Sphincter. J. Neurogastroenterol. Motil. 2016, 22, 141–148. [Google Scholar] [CrossRef][Green Version]
- O’Toole, T.J.; Sharma, S. Physiology, Somatostatin; StatPearls Publishing: Treasure Island, FL, USA, 2021. [Google Scholar]
- Pilozzi, A.; Carro, C.; Huang, X. Roles of β-Endorphin in Stress, Behavior, Neuroinflammation, and Brain Energy Metabolism. Int. J. Mol. Sci. 2021, 22, 338. [Google Scholar] [CrossRef]
- Lozić, M.; Šarenac, O.; Murphy, D.; Japundžić-Žigon, N. Vasopressin, Central Autonomic Control and Blood Pressure Regulation. Curr. Hypertens. Rep. 2018, 20, 11. [Google Scholar] [CrossRef]
- Lénárd, L.; László, K.; Kertes, E.; Ollmann, T.; Péczely, L.; Kovács, A.; Kállai, V.; Zagorácz, O.; Gálosi, R.; Karádi, Z. Substance P and neurotensin in the limbic system: Their roles in reinforcement and memory consolidation. Neurosci. Biobehav. Rev. 2018, 85, 1–20. [Google Scholar] [CrossRef]
- Li, C.; Wu, X.; Liu, S.; Zhao, Y.; Zhu, J.; Liu, K. Roles of Neuropeptide Y in Neurodegenerative and Neuroimmune Diseases. Front. Neurosci. 2019, 13, 869. [Google Scholar] [CrossRef]
- Dunn, J.; Grider, M.H. Physiology, Adenosine Triphosphate; StatPearls Publishing: Treasure Island, FL, USA, 2021. [Google Scholar]
- Wu, C.; Offenhäusser, A.; Mayer, D. A Highly Sensitive Amperometric Aptamer Biosensor for Adenosine Triphosphate Detection on a 64 Channel Gold Multielectrode Array. Phys. Status Solidi 2020, 217, 1900925. [Google Scholar] [CrossRef]
- Mustafa, A.K.; Gadalla, M.M.; Snyder, S.H. Signaling by Gasotransmitters. Sci. Signal. 2009, 2, re2. [Google Scholar] [CrossRef] [PubMed]
- Yi, M.; Li, H.; Wu, Z.; Yan, J.; Liu, Q.; Ou, C.; Chen, M. A promising therapeutic target for metabolic diseases: Neuropeptide Y receptors in humans. Cell. Physiol. Biochem. 2018, 45, 88–107. [Google Scholar] [CrossRef]
- You, Y.; Ikezu, T. Emerging roles of extracellular vesicles in neurodegenerative disorders. Neurobiol. Dis. 2019, 130, 104512. [Google Scholar] [CrossRef] [PubMed]
- Verweij, F.J.; Bebelman, M.P.; Jimenez, C.R.; Garcia-Vallejo, J.J.; Janssen, H.; Neefjes, J.; Knol, J.C.; de Goeij-de Haas, R.; Piersma, S.R.; Baglio, S.R.; et al. Quantifying exosome secretion from single cells reveals a modulatory role for GPCR signaling. J. Cell Biol. 2018, 217, 1129–1142. [Google Scholar] [CrossRef]
- Saeedi, S.; Israel, S.; Nagy, C.; Turecki, G. The emerging role of exosomes in mental disorders. Transl. Psychiatry 2019, 9, 122. [Google Scholar] [CrossRef] [PubMed]
- Shi, M.; Liu, C.; Cook, T.J.; Bullock, K.M.; Zhao, Y.; Ginghina, C.; Li, Y.; Aro, P.; Dator, R.; He, C.; et al. Plasma exosomal α-synuclein is likely CNS-derived and increased in Parkinson’s disease. Acta Neuropathol. 2014, 128, 639–650. [Google Scholar] [CrossRef]
- Rudolph, L.M.; Cornil, C.A.; Mittelman-Smith, M.A.; Rainville, J.R.; Remage-Healey, L.; Sinchak, K.; Micevych, P.E. Actions of steroids: New neurotransmitters. J. Neurosci. 2016, 36, 11449–11458. [Google Scholar] [CrossRef]
- D’Aniello, S.; Somorjai, I.; Garcia-Fernàndez, J.; Topo, E.; D’Aniello, A. D-Aspartic acid is a novel endogenous neurotransmitter. FASEB J. 2011, 25, 1014–1027. [Google Scholar] [CrossRef]
- Guzman-Martinez, L.; Maccioni, R.B.; Andrade, V.; Navarrete, L.P.; Pastor, M.G.; Ramos-Escobar, N. Neuroinflammation as a common feature of neurodegenerative disorders. Front. Pharmacol. 2019, 10, 1008. [Google Scholar] [CrossRef]
- Pchitskaya, E.; Popugaeva, E.; Bezprozvanny, I. Calcium signaling and molecular mechanisms underlying neurodegenerative diseases. Cell Calcium 2018, 70, 87–94. [Google Scholar] [CrossRef]
- García-Cazorla, À.; Artuch, R. Chapter 67—Neurotransmitter disorders. In Rosenberg’s Molecular and Genetic Basis of Neurological and Psychiatric Disease, 6th ed.; Rosenberg, R.N., Pascual, J.M., Eds.; Academic Press: Cambridge, MA, USA, 2020; pp. 917–929. [Google Scholar] [CrossRef]
- Brennenstuhl, H.; Jung-Klawitter, S.; Assmann, B.; Opladen, T. Inherited disorders of neurotransmitters: Classification and practical approaches for diagnosis and treatment. Neuropediatrics 2019, 50, 002–014. [Google Scholar] [CrossRef]
- Mastrangelo, M. Epilepsy in inherited neurotransmitter disorders: Spotlights on pathophysiology and clinical management. Metab. Brain Dis. 2021, 36, 29–43. [Google Scholar] [CrossRef] [PubMed]
- Akyuz, E.; Polat, A.K.; Eroglu, E.; Kullu, I.; Angelopoulou, E.; Paudel, Y.N. Revisiting the role of neurotransmitters in epilepsy: An updated review. Life Sci. 2021, 265, 118826. [Google Scholar] [CrossRef] [PubMed]
- McGrath, T.; Baskerville, R.; Rogero, M.; Castell, L. Emerging Evidence for the Widespread Role of Glutamatergic Dysfunction in Neuropsychiatric Diseases. Nutrients 2022, 14, 917. [Google Scholar] [CrossRef] [PubMed]
- Zhu, L.; Chen, L.; Xu, P.; Lu, D.; Dai, S.; Zhong, L.; Han, Y.; Zhang, M.; Xiao, B.; Chang, L.; et al. Genetic and molecular basis of epilepsy-related cognitive dysfunction. Epilepsy Behav. 2020, 104, 106848. [Google Scholar] [CrossRef] [PubMed]
- Abreu, C.M.; Soares-dos-Reis, R.; Melo, P.N.; Relvas, J.B.; Guimarães, J.; Sá, M.J.; Cruz, A.P.; Mendes Pinto, I. Emerging Biosensing Technologies for Neuroinflammatory and Neurodegenerative Disease Diagnostics. Front. Mol. Neurosci. 2018, 11, 164. [Google Scholar] [CrossRef] [PubMed]
- Dobson, R.; Giovannoni, G. Multiple sclerosis—A review. Eur. J. Neurol. 2019, 26, 27–40. [Google Scholar] [CrossRef]
- McGinley, M.P.; Goldschmidt, C.H.; Rae-Grant, A.D. Diagnosis and treatment of multiple sclerosis: A review. JAMA 2021, 325, 765–779. [Google Scholar] [CrossRef]
- Hauser, S.L.; Cree, B.A.C. Treatment of Multiple Sclerosis: A Review. Am. J. Med. 2020, 133, 1380–1390.e2. [Google Scholar] [CrossRef]
- Pajarillo, E.; Rizor, A.; Lee, J.; Aschner, M.; Lee, E. The role of astrocytic glutamate transporters GLT-1 and GLAST in neurological disorders: Potential targets for neurotherapeutics. Neuropharmacology 2019, 161, 107559. [Google Scholar] [CrossRef]
- Dyment, D.A.; Ebers, G.C.; Dessa Sadovnick, A. Genetics of multiple sclerosis. Lancet Neurol. 2004, 3, 104–110. [Google Scholar] [CrossRef]
- Marotta, R.; Risoleo, M.C.; Messina, G.; Parisi, L.; Carotenuto, M.; Vetri, L.; Roccella, M. The Neurochemistry of Autism. Brain Sci. 2020, 10, 163. [Google Scholar] [CrossRef] [PubMed]
- McCarty, P.J.; Pines, A.R.; Sussman, B.L.; Wyckoff, S.N.; Jensen, A.; Bunch, R.; Boerwinkle, V.L.; Frye, R.E. Resting State Functional Magnetic Resonance Imaging Elucidates Neurotransmitter Deficiency in Autism Spectrum Disorder. J. Pers. Med. 2021, 11, 969. [Google Scholar] [CrossRef] [PubMed]
- Saitow, F.; Takumi, T.; Suzuki, H. Change in serotonergic modulation contributes to the synaptic imbalance of neuronal circuit at the prefrontal cortex in the 15q11-13 duplication mouse model of autism. Neuropharmacology 2020, 165, 107931. [Google Scholar] [CrossRef]
- Kotajima-Murakami, H.; Hagihara, H.; Sato, A.; Hagino, Y.; Tanaka, M.; Katoh, Y.; Nishito, Y.; Takamatsu, Y.; Uchino, S.; Miyakawa, T.; et al. Exposure to GABAA Receptor Antagonist Picrotoxin in Pregnant Mice Causes Autism-Like Behaviors and Aberrant Gene Expression in Offspring. Front. Psychiatry 2022, 13, 821354. [Google Scholar] [CrossRef]
- Häge, A.; Banaschewski, T.; Buitelaar, J.K.; Dijkhuizen, R.M.; Franke, B.; Lythgoe, D.J.; Mechler, K.; Williams, S.C.R.; Dittmann, R.W.; the TACTICS Consortium Trials. Glutamatergic medication in the treatment of obsessive compulsive disorder (OCD) and autism spectrum disorder (ASD)—Study protocol for a randomised controlled trial. Trials 2016, 17, 141. [Google Scholar] [CrossRef]
- Abdul, F.; Sreenivas, N.; Kommu, J.V.S.; Banerjee, M.; Berk, M.; Maes, M.; Leboyer, M.; Debnath, M. Disruption of circadian rhythm and risk of autism spectrum disorder: Role of immune-inflammatory, oxidative stress, metabolic and neurotransmitter pathways. Rev. Neurosci. 2022, 33, 93–109. [Google Scholar] [CrossRef]
- Pavăl, D. A dopamine hypothesis of autism spectrum disorder. Dev. Neurosci. 2017, 39, 355–360. [Google Scholar] [CrossRef]
- Pavăl, D.; Micluția, I.V. The Dopamine Hypothesis of Autism Spectrum Disorder Revisited: Current Status and Future Prospects. Dev. Neurosci. 2021, 43, 73–83. [Google Scholar] [CrossRef]
- Chen, Z.-R.; Huang, J.-B.; Yang, S.-L.; Hong, F.-F. Role of Cholinergic Signaling in Alzheimer’s Disease. Molecules 2022, 27, 1816. [Google Scholar] [CrossRef]
- Ashrafi, H.; Azadi, A.; Mohammadi-Samani, S.; Hamidi, M. New Candidate Delivery System for Alzheimer’s Disease: Deferoxamine Nanogels. Biointerface Res. Appl. Chem. 2020, 10, 7106–7119. [Google Scholar] [CrossRef]
- Borah, P.; Mattaparthi, V.S.K. Computational investigation on the role of C-Terminal of human albumin on the dimerization of A Aβ1-42 peptide. Biointerface Res. Appl. Chem. 2020, 10, 4944–4955. [Google Scholar] [CrossRef]
- Dinparast, L.; Zengin, G.; Bahadori, M.B. Cholinesterases Inhibitory Activity of 1H-benzimidazole Derivatives. Biointerface Res. Appl. Chem. 2021, 11, 10739–10745. [Google Scholar] [CrossRef]
- Haghighatseir, N.; Ashrafi, H.; Rafiei, P.; Azadi, A. Dexamethasone ameliorates Alzheimer’s pathological condition via inhibiting Nf-κB and mTOR signaling pathways. Biointerface Res. Appl. Chem. 2020, 10, 5792–5796. [Google Scholar] [CrossRef]
- Talebi, M.; Talebi, M.; Samarghandian, S. Association of Crocus sativus with Cognitive Dysfunctions and Alzheimer’s Disease: A Systematic Review. Biointerface Res. Appl. Chem. 2021, 11, 7468–7492. [Google Scholar] [CrossRef]
- Busnatu, Ș.; Niculescu, A.-G.; Bolocan, A.; Petrescu, G.E.D.; Păduraru, D.N.; Năstasă, I.; Lupușoru, M.; Geantă, M.; Andronic, O.; Grumezescu, A.M.; et al. Clinical Applications of Artificial Intelligence—An Updated Overview. J. Clin. Med. 2022, 11, 2265. [Google Scholar] [CrossRef] [PubMed]
- Donovan, N.; Mecca, A.; Smith, G.; Gatchel, J. Molecular imaging in alzheimer’s disease: Linking pathologic, neurotransmitter, synaptic and clinical findings relevant to geriatric psychiatry. Am. J. Geriatr. Psychiatry 2020, 28, S4. [Google Scholar] [CrossRef]
- Singh, A.K.; Halder-Sinha, S.; Clement, J.P.; Kundu, T.K. Epigenetic modulation by small molecule compounds for neurodegenerative disorders. Pharmacol. Res. 2018, 132, 135–148. [Google Scholar] [CrossRef]
- Czubowicz, K.; Jęśko, H.; Wencel, P.; Lukiw, W.J.; Strosznajder, R.P. The Role of Ceramide and Sphingosine-1-Phosphate in Alzheimer’s Disease and Other Neurodegenerative Disorders. Mol. Neurobiol. 2019, 56, 5436–5455. [Google Scholar] [CrossRef]
- Schiavone, S.; Trabace, L. Small Molecules: Therapeutic Application in Neuropsychiatric and Neurodegenerative Disorders. Molecules 2018, 23, 411. [Google Scholar] [CrossRef]
- Agarwal, M.; Alam, M.R.; Haider, M.K.; Malik, M.Z.; Kim, D.-K. Alzheimer’s Disease: An Overview of Major Hypotheses and Therapeutic Options in Nanotechnology. Nanomaterials 2021, 11, 59. [Google Scholar] [CrossRef] [PubMed]
- Ueda, K.; Shinohara, S.; Yagami, T.; Asakura, K.; Kawasaki, K. Amyloid β protein potentiates Ca2+ influx through L-type voltage-sensitive Ca2+ channels: A possible involvement of free radicals. J. Neurochem. 1997, 68, 265–271. [Google Scholar] [CrossRef] [PubMed]
- Nimmrich, V.; Grimm, C.; Draguhn, A.; Barghorn, S.; Lehmann, A.; Schoemaker, H.; Hillen, H.; Gross, G.; Ebert, U.; Bruehl, C. Amyloid β Oligomers (Aβ1–42 Globulomer) Suppress Spontaneous Synaptic Activity by Inhibition of P/Q-Type Calcium Currents. J. Neurosci. 2008, 28, 788–797. [Google Scholar] [CrossRef] [PubMed]
- Lovinger, D.M. Neurotransmitter roles in synaptic modulation, plasticity and learning in the dorsal striatum. Neuropharmacology 2010, 58, 951–961. [Google Scholar] [CrossRef]
- Guo, F.; Liu, X.; Cai, H.; Le, W. Autophagy in neurodegenerative diseases: Pathogenesis and therapy. Brain Pathol. 2018, 28, 3–13. [Google Scholar] [CrossRef]
- Rahman, M.M.; Ferdous, K.S.; Ahmed, M. Emerging Promise of Nanoparticle-Based Treatment for Parkinson’s disease. Biointerface Res. Appl. Chem. 2020, 10, 7135–7151. [Google Scholar] [CrossRef]
- Abudukeyoumu, N.; Hernandez-Flores, T.; Garcia-Munoz, M.; Arbuthnott, G.W. Cholinergic modulation of striatal microcircuits. Eur. J. Neurosci. 2019, 49, 604–622. [Google Scholar] [CrossRef]
- Jamwal, S.; Kumar, P. Insight Into the Emerging Role of Striatal Neurotransmitters in the Pathophysiology of Parkinson’s Disease and Huntington’s Disease: A Review. Curr. Neuropharmacol. 2019, 17, 165–175. [Google Scholar] [CrossRef]
- Klein, M.O.; Battagello, D.S.; Cardoso, A.R.; Hauser, D.N.; Bittencourt, J.C.; Correa, R.G. Dopamine: Functions, Signaling, and Association with Neurological Diseases. Cell. Mol. Neurobiol. 2019, 39, 31–59. [Google Scholar] [CrossRef]
- Cai, Y.; Xing, L.; Yang, T.; Chai, R.; Wang, J.; Bao, J.; Shen, W.; Ding, S.; Chen, G. The neurodevelopmental role of dopaminergic signaling in neurological disorders. Neurosci. Lett. 2021, 741, 135540. [Google Scholar] [CrossRef]
- Dienel, S.J.; Lewis, D.A. Alterations in cortical interneurons and cognitive function in schizophrenia. Neurobiol. Dis. 2019, 131, 104208. [Google Scholar] [CrossRef]
- Krystal, J.H.; Anticevic, A.; Yang, G.J.; Dragoi, G.; Driesen, N.R.; Wang, X.-J.; Murray, J.D. Impaired Tuning of Neural Ensembles and the Pathophysiology of Schizophrenia: A Translational and Computational Neuroscience Perspective. Biol. Psychiatry 2017, 81, 874–885. [Google Scholar] [CrossRef] [PubMed]
- Erjavec, G.N.; Sagud, M.; Perkovic, M.N.; Strac, D.S.; Konjevod, M.; Tudor, L.; Uzun, S.; Pivac, N. Depression: Biological markers and treatment. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2021, 105, 110139. [Google Scholar] [CrossRef] [PubMed]
- Hasan, M.R.; Paul, B.K.; Ahmed, K.; Mahmud, S.; Dutta, M.; Hosen, M.S.; Hassan, M.M.; Bhuyian, T. Computational Analysis of Network Model Based Relationship of Mental Disorder with Depression. Biointerface Res. Appl. Chem. 2020, 10, 6293–6305. [Google Scholar] [CrossRef]
- Pan, J.-X.; Xia, J.-J.; Deng, F.-L.; Liang, W.-W.; Wu, J.; Yin, B.-M.; Dong, M.-X.; Chen, J.-J.; Ye, F.; Wang, H.-Y.; et al. Diagnosis of major depressive disorder based on changes in multiple plasma neurotransmitters: A targeted metabolomics study. Transl. Psychiatry 2018, 8, 130. [Google Scholar] [CrossRef]
- Masrori, P.; Van Damme, P. Amyotrophic lateral sclerosis: A clinical review. Eur. J. Neurol. 2020, 27, 1918–1929. [Google Scholar] [CrossRef] [PubMed]
- Al-Chalabi, A.; van den Berg, L.H.; Veldink, J. Gene discovery in amyotrophic lateral sclerosis: Implications for clinical management. Nat. Rev. Neurol. 2017, 13, 96–104. [Google Scholar] [CrossRef]
- Ghazy, E.; Rahdar, A.; Barani, M.; Kyzas, G.Z. Nanomaterials for Parkinson disease: Recent progress. J. Mol. Struct. 2021, 1231, 129698. [Google Scholar] [CrossRef]
- Matys, J.; Gieroba, B.; Jóźwiak, K. Recent developments of bioanalytical methods in determination of neurotransmitters in vivo. J. Pharm. Biomed. Anal. 2020, 180, 113079. [Google Scholar] [CrossRef]
- Sangubotla, R.; Kim, J. Recent trends in analytical approaches for detecting neurotransmitters in Alzheimer’s disease. TrAC Trends Anal. Chem. 2018, 105, 240–250. [Google Scholar] [CrossRef]
- Mobed, A.; Hasanzadeh, M.; Ahmadalipour, A.; Fakhari, A. Recent advances in the biosensing of neurotransmitters: Material and method overviews towards the biomedical analysis of psychiatric disorders. Anal. Methods 2020, 12, 557–575. [Google Scholar] [CrossRef]
- Moody, A.S.; Sharma, B. Multi-metal, Multi-wavelength Surface-Enhanced Raman Spectroscopy Detection of Neurotransmitters. ACS Chem. Neurosci. 2018, 9, 1380–1387. [Google Scholar] [CrossRef] [PubMed]
- Rabie, H.; Zhang, Y.; Pasquale, N.; Lagos, M.J.; Batson, P.E.; Lee, K.-B. NIR Biosensing of Neurotransmitters in Stem Cell-Derived Neural Interface Using Advanced Core–Shell Upconversion Nanoparticles. Adv. Mater. 2019, 31, 1806991. [Google Scholar] [CrossRef] [PubMed]
- Su, Y.; Bian, S.; Sawan, M. Real-time in vivo detection techniques for neurotransmitters: A review. Analyst 2020, 145, 6193–6210. [Google Scholar] [CrossRef]
- Zhang, M.-Y.; Beyer, C.E. Measurement of neurotransmitters from extracellular fluid in brain by in vivo microdialysis and chromatography–mass spectrometry. J. Pharm. Biomed. Anal. 2006, 40, 492–499. [Google Scholar] [CrossRef]
- Cernat, A.; Ştefan, G.; Tertis, M.; Cristea, C.; Simon, I. An overview of the detection of serotonin and dopamine with graphene-based sensors. Bioelectrochemistry 2020, 136, 107620. [Google Scholar] [CrossRef]
- Beitollahi, H.; Safaei, M.; Tajik, S. Different electrochemical sensors for determination of dopamine as neurotransmitter in mixed and clinical samples: A review. Anal. Bioanal. Chem. Res. 2019, 6, 81–96. [Google Scholar]
- Chauhan, N.; Soni, S.; Agrawal, P.; Balhara, Y.P.S.; Jain, U. Recent advancement in nanosensors for neurotransmitters detection: Present and future perspective. Process Biochem. 2020, 91, 241–259. [Google Scholar] [CrossRef]
- Durairaj, S.; Sidhureddy, B.; Cirone, J.; Chen, A. Nanomaterials-Based Electrochemical Sensors for In Vitro and In Vivo Analyses of Neurotransmitters. Appl. Sci. 2018, 8, 1504. [Google Scholar] [CrossRef]
- Madhurantakam, S.; Karnam, J.B.; Brabazon, D.; Takai, M.; Ahad, I.U.; Balaguru Rayappan, J.B.; Krishnan, U.M. “Nano”: An Emerging Avenue in Electrochemical Detection of Neurotransmitters. ACS Chem. Neurosci. 2020, 11, 4024–4047. [Google Scholar] [CrossRef]
- Nunez, C.N.; Krasley, A.; Bulumulla, C.; Beyene, A. Nanotechnology for biosensor development. Biophys. J. 2022, 121, 154a. [Google Scholar] [CrossRef]
- Ganesana, M.; Trikantzopoulos, E.; Maniar, Y.; Lee, S.T.; Venton, B.J. Development of a novel micro biosensor for in vivo monitoring of glutamate release in the brain. Biosens. Bioelectron. 2019, 130, 103–109. [Google Scholar] [CrossRef] [PubMed]
- Dudina, A.; Frey, U.; Hierlemann, A. Carbon-Nanotube-Based Monolithic CMOS Platform for Electrochemical Detection of Neurotransmitter Glutamate. Sensors 2019, 19, 3080. [Google Scholar] [CrossRef] [PubMed]
- Sun, Y.; Nguyen, T.N.H.; Anderson, A.; Cheng, X.; Gage, T.E.; Lim, J.; Zhang, Z.; Zhou, H.; Rodolakis, F.; Arslan, I.; et al. In Vivo Glutamate Sensing inside the Mouse Brain with Perovskite Nickelate–Nafion Heterostructures. ACS Appl. Mater. Interfaces 2020, 12, 24564–24574. [Google Scholar] [CrossRef]
- Li, Y.-T.; Jin, X.; Tang, L.; Lv, W.-L.; Xiao, M.-M.; Zhang, Z.-Y.; Gao, C.; Zhang, G.-J. Receptor-Mediated Field Effect Transistor Biosensor for Real-Time Monitoring of Glutamate Release from Primary Hippocampal Neurons. Anal. Chem. 2019, 91, 8229–8236. [Google Scholar] [CrossRef]
- Alamry, K.A.; Hussein, M.A.; Choi, J.-w.; El-Said, W.A. Non-enzymatic electrochemical sensor to detect γ-aminobutyric acid with ligand-based on graphene oxide modified gold electrode. J. Electroanal. Chem. 2020, 879, 114789. [Google Scholar] [CrossRef]
- Iwai, N.T.; Kramaric, M.; Crabbe, D.; Wei, Y.; Chen, R.; Shen, M. GABA Detection with Nano-ITIES Pipet Electrode: A New Mechanism, Water/DCE–Octanoic Acid Interface. Anal. Chem. 2018, 90, 3067–3072. [Google Scholar] [CrossRef]
- Yue, H.Y.; Zhang, H.J.; Huang, S.; Lu, X.X.; Gao, X.; Song, S.S.; Wang, Z.; Wang, W.Q.; Guan, E.H. Highly sensitive and selective dopamine biosensor using Au nanoparticles-ZnO nanocone arrays/graphene foam electrode. Mater. Sci. Eng. C 2020, 108, 110490. [Google Scholar] [CrossRef]
- Ling, X.; Shi, R.; Zhang, J.; Liu, D.; Weng, M.; Zhang, C.; Lu, M.; Xie, X.; Huang, L.; Huang, W. Dual-Signal Luminescent Detection of Dopamine by a Single Type of Lanthanide-Doped Nanoparticles. ACS Sens. 2018, 3, 1683–1689. [Google Scholar] [CrossRef]
- Halawa, M.I.; Wu, F.; Fereja, T.H.; Lou, B.; Xu, G. One-pot green synthesis of supramolecular β-cyclodextrin functionalized gold nanoclusters and their application for highly selective and sensitive fluorescent detection of dopamine. Sens. Actuators B Chem. 2018, 254, 1017–1024. [Google Scholar] [CrossRef]
- Selvolini, G.; Lazzarini, C.; Marrazza, G. Electrochemical Nanocomposite Single-Use Sensor for Dopamine Detection. Sensors 2019, 19, 3097. [Google Scholar] [CrossRef] [PubMed]
- Adumitrăchioaie, A.; Tertiș, M.; Suciu, M.; Graur, F.; Cristea, C. A novel immunosensing platform for serotonin detection in complex real samples based on graphene oxide and chitosan. Electrochim. Acta 2019, 311, 50–61. [Google Scholar] [CrossRef]
- Mahato, K.; Purohit, B.; Bhardwaj, K.; Jaiswal, A.; Chandra, P. Novel electrochemical biosensor for serotonin detection based on gold nanorattles decorated reduced graphene oxide in biological fluids and in vitro model. Biosens. Bioelectron. 2019, 142, 111502. [Google Scholar] [CrossRef]
- Amatatongchai, M.; Sitanurak, J.; Sroysee, W.; Sodanat, S.; Chairam, S.; Jarujamrus, P.; Nacapricha, D.; Lieberzeit, P.A. Highly sensitive and selective electrochemical paper-based device using a graphite screen-printed electrode modified with molecularly imprinted polymers coated Fe3O4@Au@SiO2 for serotonin determination. Anal. Chim. Acta 2019, 1077, 255–265. [Google Scholar] [CrossRef]
- Ramos, M.M.V.; Carvalho, J.H.S.; de Oliveira, P.R.; Janegitz, B.C. Determination of serotonin by using a thin film containing graphite, nanodiamonds and gold nanoparticles anchored in casein. Measurement 2020, 149, 106979. [Google Scholar] [CrossRef]
- Yang, Y.; Zeng, Y.; Tang, C.; Zhu, X.; Lu, X.; Liu, L.; Chen, Z.; Li, L. Voltammetric determination of 5-hydroxytryptamine based on the use of platinum nanoparticles coated with molecularly imprinted silica. Microchim. Acta 2018, 185, 219. [Google Scholar] [CrossRef]
- Baluta, S.; Lesiak, A.; Cabaj, J. Graphene Quantum Dots-based Electrochemical Biosensor for Catecholamine Neurotransmitters Detection. Electroanalysis 2018, 30, 1781–1790. [Google Scholar] [CrossRef]
- Dong, W.; Ren, Y.; Bai, Z.; Jiao, J.; Chen, Y.; Han, B.; Chen, Q. Synthesis of tetrahexahedral Au-Pd core–shell nanocrystals and reduction of graphene oxide for the electrochemical detection of epinephrine. J. Colloid Interface Sci. 2018, 512, 812–818. [Google Scholar] [CrossRef]
- Immanuel, S.; Sivasubramanian, R. Fabrication of two-dimensional chemically reduced graphene oxide nanosheets for the electrochemical determination of epinephrine. Bull. Mater. Sci. 2020, 43, 79. [Google Scholar] [CrossRef]
- Moghaddam, H.M.; Razmara, Z.; Makarem, A.; Aflatoonian, M.R. A nanocomposite material based on carbon nanotubes and Fe3O4@SiO2 for the high selective and sensitive electrochemical determination of norepinephrine. Int. J. Electrochem. Sci. 2018, 13, 3070–3079. [Google Scholar] [CrossRef]
- Queiroz, D.F.; Dadamos, T.R.; Machado, S.A.; Martines, M.A. Electrochemical Determination of Norepinephrine by Means of Modified Glassy Carbon Electrodes with Carbon Nanotubes and Magnetic Nanoparticles of Cobalt Ferrite. Sensors 2018, 18, 1223. [Google Scholar] [CrossRef] [PubMed]
- Gajjala, R.K.R.; Palathedath, S.K. Cu@Pd core-shell nanostructures for highly sensitive and selective amperometric analysis of histamine. Biosens. Bioelectron. 2018, 102, 242–246. [Google Scholar] [CrossRef] [PubMed]
- Hadi, M.; Mostaanzadeh, H. Sensitive Detection of Histamine at Metal-Organic Framework (Ni-BTC) Crystals and Multi-Walled Carbon Nanotubes Modified Glassy Carbon Electrode. Russ. J. Electrochem. 2018, 54, 1045–1052. [Google Scholar] [CrossRef]
- Kant, R.; Gupta, B.D. Fiber-Optic SPR Based Acetylcholine Biosensor Using Enzyme Functionalized Ta2O5 Nanoflakes for Alzheimer’s Disease Diagnosis. J. Lightwave Technol. 2018, 36, 4018–4024. [Google Scholar] [CrossRef]
- Chauhan, N.; Tiwari, S.; Narayan, T.; Jain, U. Bienzymatic assembly formed @ Pt nano sensing framework detecting acetylcholine in aqueous phase. Appl. Surf. Sci. 2019, 474, 154–160. [Google Scholar] [CrossRef]
- Chauhan, N.; Balayan, S.; Jain, U. Sensitive biosensing of neurotransmitter: 2D material wrapped nanotubes and MnO2 composites for the detection of acetylcholine. Synth. Met. 2020, 263, 116354. [Google Scholar] [CrossRef]
- Balasubramanian, P.; Balamurugan, T.S.T.; Chen, S.-M.; Chen, T.-W. Facile Synthesis of Spinel-Type Copper Cobaltite Nanoplates for Enhanced Electrocatalytic Detection of Acetylcholine. ACS Sustain. Chem. Eng. 2019, 7, 7642–7651. [Google Scholar] [CrossRef]
- Niello, M.; Gradisch, R.; Loland, C.J.; Stockner, T.; Sitte, H.H. Allosteric Modulation of Neurotransmitter Transporters as a Therapeutic Strategy. Trends Pharmacol. Sci. 2020, 41, 446–463. [Google Scholar] [CrossRef]
- Underhill, S.M.; Ingram, S.L.; Ahmari, S.E.; Veenstra-VanderWeele, J.; Amara, S.G. Neuronal excitatory amino acid transporter EAAT3: Emerging functions in health and disease. Neurochem. Int. 2019, 123, 69–76. [Google Scholar] [CrossRef]
- Morland, C.; Nordengen, K. N-Acetyl-Aspartyl-Glutamate in Brain Health and Disease. Int. J. Mol. Sci. 2022, 23, 1268. [Google Scholar] [CrossRef]
- Cheng, M.H.; Bahar, I. Monoamine transporters: Structure, intrinsic dynamics and allosteric regulation. Nat. Struct. Mol. Biol. 2019, 26, 545–556. [Google Scholar] [CrossRef] [PubMed]
- Alasmari, F. Caffeine induces neurobehavioral effects through modulating neurotransmitters. Saudi Pharm. J. 2020, 28, 445–451. [Google Scholar] [CrossRef]
- Sarkar, A.; Lehto, S.M.; Harty, S.; Dinan, T.G.; Cryan, J.F.; Burnet, P.W.J. Psychobiotics and the Manipulation of Bacteria-Gut-Brain Signals. Trends Neurosci. 2016, 39, 763–781. [Google Scholar] [CrossRef]
- Bravo, J.A.; Forsythe, P.; Chew, M.V.; Escaravage, E.; Savignac, H.M.; Dinan, T.G.; Bienenstock, J.; Cryan, J.F. Ingestion of Lactobacillus strain regulates emotional behavior and central GABA receptor expression in a mouse via the vagus nerve. Proc. Natl. Acad. Sci. USA 2011, 108, 16050–16055. [Google Scholar] [CrossRef]
- Yoon, N.Y.; Ngo, D.-N.; Kim, S.-K. AcetylcholineSsterase inhibitory activity of novel chitooligosaccharide derivatives. Carbohydr. Polym. 2009, 78, 869–872. [Google Scholar] [CrossRef]
- Sherman, C. The defining features of drug intoxication and addiction can be traced to disruptions in neuron-to neuron signaling. Natl. Inst. Drug Abus. Adv. Addict. Sci. 2017, 21, 4. [Google Scholar]


| Detection System | Detected NT | Performance Indicators | Ref. |
|---|---|---|---|
| Glutamate oxidase entrapped in a chitosan matrix cast onto the microelectrode surface (i.e., platinum wire covered with poly-o-phenylenediamine) and coated with ascorbate oxidase | Glutamate | Sensitivity: 0.097 ± 0.001 nA μM−1 Linearity range: 5–150 μM Detection limit: 0.044 μM | [146] |
| Monolithic platform based on carbon-nanotube field-effect transistors | Glutamate | Linearity range: 250–500 μM Detection limit: 3 μM | [147] |
| Perovskite nickelate-Nafion (i.e., polymeric ion-permeable membrane) heterostructure | Glutamate | Sensitivity: 0.327 ± 0.07 nA μM−1 mm−2 Linearity range: 1–700 μM Detection limit: 16 nM | [148] |
| Reduced graphene oxide-based field-effect transistor biosensor functionalized with mGluR | Glutamate | Linearity range: 1 fM–100 pM Detection limit: 1 fM | [149] |
| Enzyme-free electrochemical sensor based on graphene oxide modified gold electrode | GABA | Linearity range: 250 nM–100 μM Detection limit: 98 nM | [150] |
| nanoITIES (interface between two immiscible electrolyte solutions) pipet electrodes | GABA | Linearity range: 0.25–1.0 mM Detection limit: 22.4 μM | [151] |
| Gold nanoparticles-zinc oxide nanocone arrays/graphene foam electrode | Dopamine | Sensitivity: 4.36 μA mM−1 Detection limit: 0.04 μM | [152] |
| Label-free luminescent NaGdF4:Tb nanoparticles | Dopamine | Linearity range: 0–10 μM Detection limit: ~30 nM | [153] |
| Supramolecular β-cyclodextrin functionalized gold nanoclusters | Dopamine | Linearity range: 100.0 nM–80.0 μM Detection limit: 20.0 nM | [154] |
| Graphite screen-printed electrodes modified by a nanocomposite made of polyaniline and gold nanoparticles | Dopamine | Linearity range: 1–100 μM Detection limit: 0.86 μM | [155] |
| Nanocomposite platform based on graphene oxide/chitosan modified screen-printed electrode | Serotonin | Sensitivity: 0.05 μA mM−1 Detection range: 10 nM–100 μM Detection limit: 3.2 nM | [156] |
| Gold-nanorattles-reduced graphene oxide nanocomposite coated onto the gold nanoparticles deposited glassy carbon electrode (GCE) | Serotonin | Linear dynamic range: 3 × 10−6–1 × 10−3 M Detection limit: 3.87 (±0.02) × 10−7 M | [157] |
| Graphite-paste electrode modified with nanoparticles (i.e., Fe3O4@Au@SiO2) coated with molecularly imprinted polymer | Serotonin | Linearity range: 0.01–1000 μM Detection limit: 0.002 μM | [158] |
| GCE coated with a biofilm of graphite, nanodiamonds, and gold nanoparticles anchored in casein | Serotonin | Sensitivity: 0.18 μA mM−1 Linear dynamic range: 0.3–3.0 μM Detection limit: 0.1 μM | [159] |
| Platinum nanoparticles coated with molecularly imprinted silica drop-cast onto a GCE | Serotonin | Linearity range: 0.05–80 μM Detection limit: 0.02 μM | [160] |
| Laccase modified GCE coated with graphene quantum dots | Epinephrine | Sensitivity: 2.9 μA mM−1 cm−2 Linearity range: 1–120 × 10−6 M Detection limit: 83 nM | [161] |
| Tetrahexahedral gold-palladium core-shell nanocrystals on reduced graphene oxide nanosheets | Epinephrine | Linear detection range: 0.001–1000 μM Detection limit: 0.0012 μM | [162] |
| GCE modified with chemically reduced graphene oxide nanosheets | Epinephrine | Two different linearity ranges: 10–300 and 400–1300 μM Detection limit 1.6 μM | [163] |
| Graphite screen-printed electrode modified with a nanocomposite of magnetic Fe3O4@SiO2 nanoparticles and carbon nanotubes | Norepinephrine | Linearity range: 0.5–400 μM Detection limit: 0.2 μM | [164] |
| GCE modified with carbon nanotubes and magnetic nanoparticles of cobalt ferrite | Norepinephrine | Linearity range: 0.16–1.91 mM Detection limit: 0.76 μM | [165] |
| Copper-palladium core-shell nanostructures on pencil graphite substrate | Histamine | Sensitivity: 0.082 μA μM−1 cm−2 Detection limit: 3.2 ± 0.1 nM | [166] |
| Nickel-based metal-organic framework crystals and multi-walled carbon nanotubes modified GCE | Histamine | Sensitivity: 0.19 μA μM−1 Linearity range: 1.00–160.00 μM Detection limit: 0.41 μM | [167] |
| Fiber-optic surface plasmon resonance (SPR)-based biosensor covered with multilayers of silver metal and tantalum (V) oxide nanoflakes functionalized with acetylcholinesterase enzyme | Acetylcholine | Sensitivity: 8.709 nm/μM Detection limit: 38 nM | [168] |
| Acetylcholinesterase and choline esterase co-immobilized on platinum nanoparticles and metallic organic framework modified gold electrode | Acetylcholine | Linearity range: 0.01–500 μM Detection limit: 0.01 μM | [169] |
| Acetylcholinesterase and choline esterase co-immobilized over a gold electrode coated with a nanocomposite layer of multi-walled carbon nanotubes and reduced graphene oxide | Acetylcholine | Linearity range: 0.1–100 μM Detection limit: 0.1 μM | [170] |
| Enzyme-free electrochemical sensor based on spinel-type copper cobaltite nanoplates | Acetylcholine | Linear dynamic range: 0.2–3500 μM Detection limit: 30 nM | [171] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Teleanu, R.I.; Niculescu, A.-G.; Roza, E.; Vladâcenco, O.; Grumezescu, A.M.; Teleanu, D.M. Neurotransmitters—Key Factors in Neurological and Neurodegenerative Disorders of the Central Nervous System. Int. J. Mol. Sci. 2022, 23, 5954. https://doi.org/10.3390/ijms23115954
Teleanu RI, Niculescu A-G, Roza E, Vladâcenco O, Grumezescu AM, Teleanu DM. Neurotransmitters—Key Factors in Neurological and Neurodegenerative Disorders of the Central Nervous System. International Journal of Molecular Sciences. 2022; 23(11):5954. https://doi.org/10.3390/ijms23115954
Chicago/Turabian StyleTeleanu, Raluca Ioana, Adelina-Gabriela Niculescu, Eugenia Roza, Oana Vladâcenco, Alexandru Mihai Grumezescu, and Daniel Mihai Teleanu. 2022. "Neurotransmitters—Key Factors in Neurological and Neurodegenerative Disorders of the Central Nervous System" International Journal of Molecular Sciences 23, no. 11: 5954. https://doi.org/10.3390/ijms23115954
APA StyleTeleanu, R. I., Niculescu, A.-G., Roza, E., Vladâcenco, O., Grumezescu, A. M., & Teleanu, D. M. (2022). Neurotransmitters—Key Factors in Neurological and Neurodegenerative Disorders of the Central Nervous System. International Journal of Molecular Sciences, 23(11), 5954. https://doi.org/10.3390/ijms23115954









