Extracellular Vesicles Tune the Immune System in Renal Disease: A Focus on Systemic Lupus Erythematosus, Antiphospholipid Syndrome, Thrombotic Microangiopathy and ANCA-Vasculitis
Abstract
1. Introduction
1.1. EV Nomenclature
- physical characteristics such as size (small EV and medium/large EV, with ranges defined, for instance, respectively, <100 nm or <200 nm (small), or >200 nm (large and/or medium)) or density (low, middle, high);
- biochemical composition (CD63+/CD81+− EV, Annexin A5-stained EV, etc.);
- descriptions of conditions or cell of origin (podocyte EV, hypoxic EV, large oncosomes, apoptotic bodies) [2].
1.2. EV Isolation and Detection
- flow cytometry which detects EV passing through a laser beam. Modern flow cytometers may have many lasers and fluorescence detectors, which allow to label them with multiple conjugated antibodies using the same sample. Although widely used, the analysis using flow cytometry has limitations in detecting the smallest EV whose number and surface expression may be underestimated [3]. To circumvent this limitation, an alternative bead-based technique has been developed using specifically activated beads that capture EV with a cocktail of different exosome marker epitopes allowing subsequent simultaneous detection of multiple antigens [6];
- nanoparticle tracking analysis (NTA) which visualizes EV in the liquid phase by light scattering using a light microscope. A video is taken and the NTA software tracks the Brownian motion of individual vesicles and calculates their size and total concentration. NTA with fluorescent mode detects labeled vesicles and provides quantitative and qualitative analysis. NTA can detect vesicles smaller than those distinguished by conventional flow cytometry [3].
1.3. EV and Cell-to-Cell Communication
2. EV in Physiological and Pathological Settings
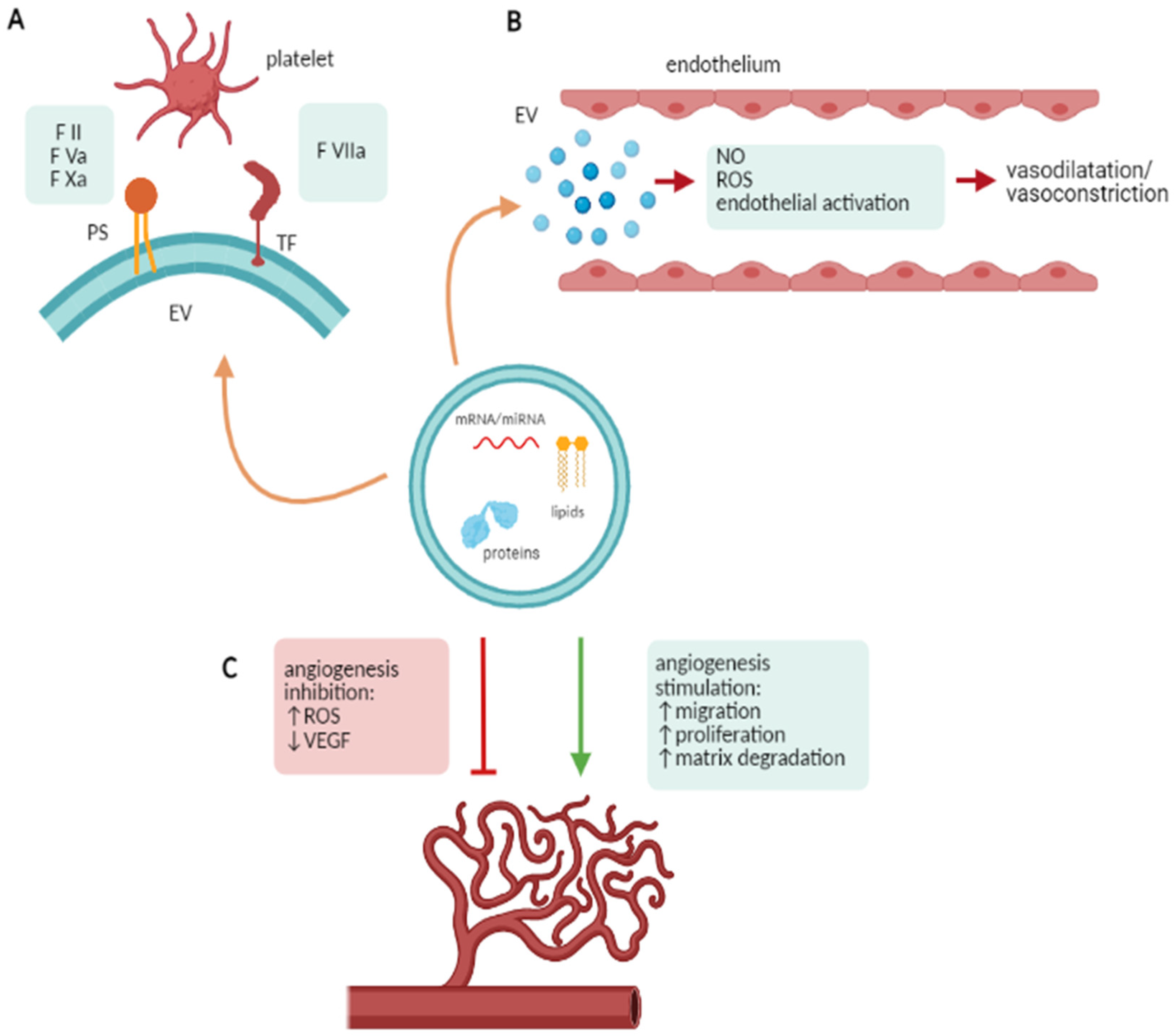
2.1. EV and Coagulation
2.2. EV and Endothelial Dysfunction
2.3. EV and Angiogenesis
2.4. EV and Immune System Modulation
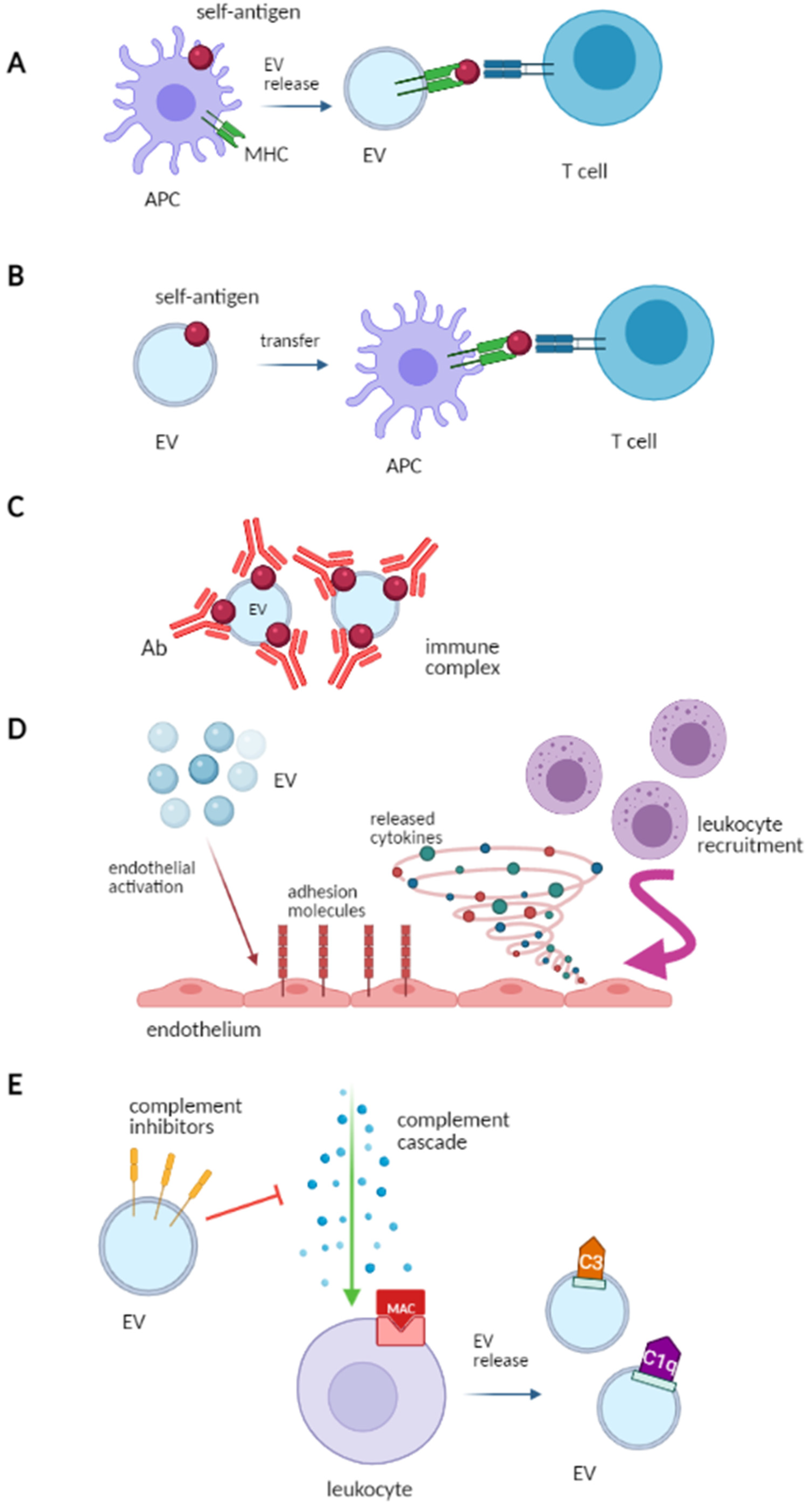
- Antigen presentationB cells can recognize foreign antigens, while T cells require antigen-presenting cells (APCs) for antigen recognition. Major histocompatibility complex class I (MHC I) and class II (MHC-II) present antigens to CD8+ and CD4+ T cells, thereby activating the immune response. APCs- and B cells-derived EV express the MHC-I, MHC-II and the T-cell costimulatory molecules, thus may take part in the antigen presentation process and in the CD8+ and CD4+ T cell activation (Figure 2A) [17].
- Source of self-antigens and IC formationEV participate in the formation of IC. Indeed, EV can express both self-antigens and MHC complexes and may activate autoreactive T-cells in autoimmune disease. As an example, the synovial fluid of patients with rheumatoid arthritis contains IC composed of platelet-derived EV and autoantibodies against citrullinated peptides [18]. Similarly, in systemic lupus erythematosus (SLE), EV carry nuclear molecules, which represent a potential source of autoantigens and participate in IC formation. Furthermore, EV-associated ICs may affect the recognition and clearance of EV by phagocytes, leading to the accumulation of cell debris and triggering the autoimmune response (Figure 2B,C) [19].
- Role of adjuvants in innate immune responseLeukocyte-derived EV activate the endothelium by upregulating adhesion molecules and releasing cytokines. This leads to leukocyte recruitment via platelet-derived EV, which promotes monocyte adhesion to the endothelium [20]. Dendritic cell-derived EV increase the NK cytotoxic activity and stimulate the release of proinflammatory cytokines by epithelial cells (Figure 2D) [21].
- Role in complement activationWhen the complement system undergoes activation, the membrane attack complex may be set down on blood cells and complement-coated EV may be released. C3-positive EV reflect the activation of the alternative pathway of the complement, while C1q-positive EV reflect the activation of the classic pathway [22]. Moreover, EV may express complement regulators on their surface (complement receptor type 1, membrane cofactor protein, decay-accelerating factor also denoted as CD59), thereby inhibiting the membrane attack complex (Figure 2E) [23].
3. EV and Renal Intercellular Communication
4. EV in Renal Disease
4.1. Antiphospholipid Syndrome
4.2. Systemic Lupus Erythematosus
4.3. Thrombotic Microangiopathies
4.4. ANCA-Associated Vasculitis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Turpin, D.; Truchetet, M.-E.; Faustin, B.; Augusto, J.-F.; Contin-Bordes, C.; Brisson, A.; Blanco, P.; Duffau, P. Role of extracellular vesicles in autoimmune diseases. Autoimmun. Rev. 2016, 15, 174–183. [Google Scholar] [CrossRef]
- Théry, C.; Witwer, K.W.; Aikawa, E.; Alcaraz, M.J.; Anderson, J.D.; Andriantsitohaina, R.; Antoniou, A.; Arab, T.; Archer, F.; Atkin-Smith, G.K.; et al. Minimal information for studies of extracellular vesicles 2018 (MISEV2018): A position statement of the International Society for Extracellular Vesicles and update of the MISEV2014 guidelines. J. Extracell. Vesicles 2018, 7, 1535750. [Google Scholar] [CrossRef] [PubMed]
- Ståhl, A.-L.; Johansson, K.; Mossberg, M.; Kahn, R.; Karpman, D. Exosomes and microvesicles in normal physiology, pathophysiology, and renal diseases. Pediatr. Nephrol. 2019, 34, 11–30. [Google Scholar] [CrossRef] [PubMed]
- Yáñez-Mó, M.; Siljander, P.R.M.; Andreu, Z.; Zavec, A.B.; Borràs, F.E.; Buzas, E.I.; Buzas, K.; Casal, E.; Cappello, F.; Carvalho, J.; et al. Biological Properties of Extracellular Vesicles and their Physiological Functions. J. Extracell. Vesicles 2015, 4, 27066. [Google Scholar] [CrossRef] [PubMed]
- Coumans, F.A.W.; Brisson, A.R.; Buzas, E.I.; Dignat-George, F.; Drees, E.E.E.; El-Andaloussi, S.; Emanueli, C.; Gasecka, A.; Hendrix, A.; Hill, A.F.; et al. Methodological Guidelines to Study Extracellular Vesicles. Circ. Res. 2017, 120, 1632–1648. [Google Scholar] [CrossRef] [PubMed]
- Štok, U.; Blokar, E.; Lenassi, M.; Holcar, M.; Frank-Bertoncelj, M.; Erman, A.; Resnik, N.; Sodin-Šemrl, S.; Čučnik, S.; Pirkmajer, K.P.; et al. Characterization of Plasma-Derived Small Extracellular Vesicles Indicates Ongoing Endothelial and Platelet Activation in Patients with Thrombotic Antiphospholipid Syndrome. Cells 2020, 9, 1211. [Google Scholar] [CrossRef] [PubMed]
- Buzas, E.I.; György, B.; Nagy, G.; Falus, A.; Gay, S. Emerging role of extracellular vesicles in inflammatory diseases. Nat. Rev. Rheumatol. 2014, 10, 356–364. [Google Scholar] [CrossRef]
- Pomatto, M.A.C.; Gai, C.; Bussolati, B.; Camussi, G. Extracellular Vesicles in Renal Pathophysiology. Front. Mol. Biosci. 2017, 4, 37. [Google Scholar] [CrossRef]
- Owens, A.P., III; Mackman, N.; Weber, C.; Mause, S. Microparticles in hemostasis and thrombosis. Circ. Res. 2011, 108, 1284–1297. [Google Scholar] [CrossRef]
- Ståhl, A.-L.; Sartz, L.; Nelsson, A.; Békássy, Z.D.; Karpman, D. Shiga Toxin and Lipopolysaccharide Induce Platelet-Leukocyte Aggregates and Tissue Factor Release, a Thrombotic Mechanism in Hemolytic Uremic Syndrome. PLoS ONE 2009, 4, e6990. [Google Scholar] [CrossRef]
- Sinauridze, E.; Kireev, D.; Popenko, N.Y.; Pichugin, A.V.; Panteleev, M.; Krymskaya, O.V.; Ataullakhanov, F. Platelet microparticle membranes have 50- to 100-fold higher specific procoagulant activity than activated platelets. Thromb. Haemost. 2007, 97, 425–434. [Google Scholar]
- Pitanga, T.N.; França, L.D.A.; Rocha, V.C.J.; Meirelles, T.; Borges, V.M.; Gonçalves, M.S.; Pontes-De-Carvalho, L.C.; Noronha-Dutra, A.A.; Dos-Santos, W.L.C. Neutrophil-derived microparticles induce myeloperoxidase-mediated damage of vascular endothelial cells. BMC Cell Biol. 2014, 15, 21. [Google Scholar] [CrossRef]
- Lombardo, G.; Dentelli, P.; Togliatto, G.; Rosso, A.; Gili, M.; Gallo, S.; Deregibus, M.C.; Camussi, G.; Brizzi, M.F. Activated Stat5 trafficking Via Endothelial Cell-derived Extracellular Vesicles Controls IL-3 Pro-angiogenic Paracrine Action. Sci. Rep. 2016, 6, 25689. [Google Scholar] [CrossRef]
- Taraboletti, G.; D’Ascenzo, S.; Borsotti, P.; Giavazzi, R.; Pavan, A.; Dolo, V. Shedding of the Matrix Metalloproteinases MMP-2, MMP-9, and MT1-MMP as Membrane Vesicle-Associated Components by Endothelial Cells. Am. J. Pathol. 2002, 160, 673–680. [Google Scholar] [CrossRef]
- Yang, C.; Mwaikambo, B.R.; Zhu, T.; Gagnon, C.; LaFleur, J.; Seshadri, S.; Lachapelle, P.; Lavoie, J.-C.; Chemtob, S.; Hardy, P. Lymphocytic microparticles inhibit angiogenesis by stimulating oxidative stress and negatively regulating VEGF-induced pathways. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2008, 294, R467–R476. [Google Scholar] [CrossRef] [PubMed]
- Ezhang, B.; Eyin, Y.; Elai, R.C.; Elim, S.K. Immunotherapeutic Potential of Extracellular Vesicles. Front. Immunol. 2014, 5, 518. [Google Scholar] [CrossRef]
- Anel, A.; Gallego-Lleyda, A.; De Miguel, D.; Naval, J.; Martínez-Lostao, L. Role of Exosomes in the Regulation of T-cell Mediated Immune Responses and in Autoimmune Disease. Cells 2019, 8, 154. [Google Scholar] [CrossRef] [PubMed]
- Cloutier, N.; Tan, S.; Boudreau, L.H.; Cramb, C.; Subbaiah, R.; Lahey, L.; Albert, A.; Shnayder, R.; Gobezie, R.; Nigrovic, P.A.; et al. The exposure of autoantigens by microparticles underlies the formation of potent inflammatory components: The microparticle-associated immune complexes. EMBO Mol. Med. 2012, 5, 235–249. [Google Scholar] [CrossRef] [PubMed]
- Mobarrez, F.; Gunnarsson, I.; Svenungsson, E. Altered β2-glycoprotein I expression on microparticles in the presence of antiphospholipid antibodies. J. Thromb. Haemost. 2017, 15, 1799–1806. [Google Scholar] [CrossRef]
- Mesri, M.; Altieri, D.C. Endothelial cell activation by leukocyte microparticles. J. Immunol. 1998, 161, 4382–4387. [Google Scholar]
- Munich, S.; Sobo-Vujanovic, A.; Buchser, W.J.; Beer-Stolz, D.; Vujanovic, N.L. Dendritic cell exosomes directly kill tumor cells and activate natural killer cells via TNF superfamily ligands. OncoImmunology 2012, 1, 1074–1083. [Google Scholar] [CrossRef]
- Ståhl, A.-L.; Sartz, L.; Karpman, D. Complement activation on platelet-leukocyte complexes and microparticles in enterohemorrhagic Escherichia coli–induced hemolytic uremic syndrome. Blood 2011, 117, 5503–5513. [Google Scholar] [CrossRef]
- Clayton, A.; Harris, C.L.; Court, J.; Mason, M.D.; Morgan, B.P. Antigen-presenting cell exosomes are protected from complement-mediated lysis by expression of CD55 and CD59. Eur. J. Immunol. 2003, 33, 522–531. [Google Scholar] [CrossRef] [PubMed]
- Van Balkom, B.W.; Pisitkun, T.; Verhaar, M.C.; Knepper, M.A. Exosomes and the kidney: Prospects for diagnosis and therapy of renal diseases. Kidney Int. 2011, 80, 1138–1145. [Google Scholar] [CrossRef]
- Hogan, M.C.; Johnson, K.L.; Zenka, R.M.; Charlesworth, M.C.; Madden, B.J.; Mahoney, D.W.; Oberg, A.L.; Huang, B.Q.; Leontovich, A.A.; Nesbitt, L.L.; et al. Subfractionation, characterization, and in-depth proteomic analysis of glomerular membrane vesicles in human urine. Kidney Int. 2014, 85, 1225–1237. [Google Scholar] [CrossRef]
- Moon, P.-G.; Lee, J.-E.; You, S.; Kim, T.-K.; Cho, J.-H.; Kim, I.-S.; Kwon, T.-H.; Kim, C.-D.; Park, S.-H.; Hwang, D.; et al. Proteomic analysis of urinary exosomes from patients of early IgA nephropathy and thin basement membrane nephropathy. Proteom. 2011, 11, 2459–2475. [Google Scholar] [CrossRef] [PubMed]
- Ranghino, A.; DiMuccio, V.; Papadimitriou, E.; Bussolati, B. Extracellular vesicles in the urine: Markers and mediators of tissue damage and regeneration. Clin. Kidney J. 2015, 8, 23–30. [Google Scholar] [CrossRef] [PubMed]
- Gonzales, P.A.; Pisitkun, T.; Hoffert, J.D.; Tchapyjnikov, D.; Star, R.A.; Kleta, R.; Wang, N.S.; Knepper, M.A. Large-Scale Proteomics and Phosphoproteomics of Urinary Exosomes. J. Am. Soc. Nephrol. 2009, 20, 363–379. [Google Scholar] [CrossRef] [PubMed]
- Pisitkun, T.; Shen, R.-F.; Knepper, M.A. Identification and proteomic profiling of exosomes in human urine. Proc. Natl. Acad. Sci. USA 2004, 101, 13368–13373. [Google Scholar] [CrossRef]
- Salih, M.; Zietse, R.; Hoorn, E.J. Urinary extracellular vesicles and the kidney: Biomarkers and beyond. Am. J. Physiol. Physiol. 2014, 306, F1251–F1259. [Google Scholar] [CrossRef]
- Oosthuyzen, W.; Scullion, K.M.; Ivy, J.R.; Morrison, E.E.; Hunter, R.W.; Lewis, P.J.S.; O’Duibhir, E.; Street, J.M.; Caporali, A.; Gregory, C.D.; et al. Vasopressin Regulates Extracellular Vesicle Uptake by Kidney Collecting Duct Cells. J. Am. Soc. Nephrol. 2016, 27, 3345–3355. [Google Scholar] [CrossRef] [PubMed]
- Gildea, J.J.; Seaton, J.E.; Victor, K.G.; Reyes, C.M.; Wang, D.B.; Pettigrew, A.C.; Courtner, C.E.; Shah, N.; Tran, H.T.; Van Sciver, R.E.; et al. Exosomal transfer from human renal proximal tubule cells to distal tubule and collecting duct cells. Clin. Biochem. 2014, 47, 89–94. [Google Scholar] [CrossRef] [PubMed]
- Kholia, S.; Sanchez, M.B.H.; Cedrino, M.; Papadimitriou, E.; Tapparo, M.; Deregibus, M.C.; Bruno, S.; Antico, F.; Brizzi, M.F.; Quesenberry, P.J.; et al. Mesenchymal Stem Cell Derived Extracellular Vesicles Ameliorate Kidney Injury in Aristolochic Acid Nephropathy. Front. Cell Dev. Biol. 2020, 8, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Ranghino, A.; Bruno, S.; Bussolati, B.; Moggio, A.; DiMuccio, V.; Tapparo, M.; Biancone, L.; Gontero, P.; Frea, B.; Camussi, G. The effects of glomerular and tubular renal progenitors and derived extracellular vesicles on recovery from acute kidney injury. Stem Cell Res. Ther. 2017, 8, 24. [Google Scholar] [CrossRef]
- Grange, C.; Papadimitriou, E.; Dimuccio, V.; Pastorino, C.; Molina, J.; O’Kelly, R.; Niedernhofer, L.J.; Robbins, P.D.; Camussi, G.; Bussolati, B. Urinary Extracellular Vesicles Carrying Klotho Improve the Recovery of Renal Function in an Acute Tubular Injury Model. Mol. Ther. 2020, 28, 490–502. [Google Scholar] [CrossRef] [PubMed]
- Borges, F.T.; Melo, S.A.; Özdemir, B.C.; Kato, N.; Revuelta, I.; Miller, C.A.; Ii, V.H.G.; LeBleu, V.S.; Kalluri, R. TGF-β1–Containing Exosomes from Injured Epithelial Cells Activate Fibroblasts to Initiate Tissue Regenerative Responses and Fibrosis. J. Am. Soc. Nephrol. 2013, 24, 385–392. [Google Scholar] [CrossRef]
- Jella, K.K.; Yu, L.; Yue, Q.; Friedman, D.; Duke, B.J.; Alli, A.A. Exosomal GAPDH from Proximal Tubule Cells Regulate ENaC Activity. PLoS ONE 2016, 11, e0165763. [Google Scholar] [CrossRef]
- Street, J.M.; Birkhoff, W.; Menzies, R.I.; Webb, D.J.; Bailey, M.A.; Dear, J.W. Exosomal transmission of functional aquaporin 2 in kidney cortical collecting duct cells. J. Physiol. 2011, 589, 6119–6127. [Google Scholar] [CrossRef]
- Hiemstra, T.F.; Charles, P.D.; Gracia, T.; Hester, S.S.; Gatto, L.; Al-Lamki, R.; Floto, R.A.; Su, Y.; Skepper, J.N.; Lilley, K.S.; et al. Human Urinary Exosomes as Innate Immune Effectors. J. Am. Soc. Nephrol. 2014, 25, 2017–2027. [Google Scholar] [CrossRef]
- Chiabotto, G.; Bruno, S.; Collino, F.; Camussi, G. Mesenchymal Stromal Cells Epithelial Transition Induced by Renal Tubular Cells-Derived Extracellular Vesicles. PLoS ONE 2016, 11, e0159163. [Google Scholar] [CrossRef]
- Biancone, L.; Bruno, S.; Deregibus, M.C.; Tetta, C.; Camussi, G. Therapeutic potential of mesenchymal stem cell-derived microvesicles. Nephrol. Dial. Transplant. 2012, 27, 3037–3042. [Google Scholar] [CrossRef] [PubMed]
- Gregorini, M.; Corradetti, V.; Pattonieri, E.F.; Rocca, C.; Milanesi, S.; Peloso, A.; Canevari, S.; De Cecco, L.; Dugo, M.; Avanzini, M.A.; et al. Perfusion of isolated rat kidney with Mesenchymal Stromal Cells/Extracellular Vesicles prevents ischaemic injury. J. Cell. Mol. Med. 2017, 21, 3381–3393. [Google Scholar] [CrossRef]
- Cervera, R.; Serrano, R.; Pons-Estel, G.; Ceberio-Hualde, L.; Shoenfeld, Y.; De Ramón, E.; Buonaiuto, V.; Jacobsen, S.; Zeher, M.; Tarr, T.; et al. Morbidity and mortality in the antiphospholipid syndrome during a 10-year period: A multicentre prospective study of 1000 patients. Ann. Rheum. Dis. 2015, 74, 1011–1018. [Google Scholar] [CrossRef]
- Alluri, R.; Chaturvedi, S.; McCrae, K.R. Extracellular Vesicles in the Antiphospholipid Syndrome. Semin. Thromb. Hemost. 2018, 44, 493–504. [Google Scholar] [CrossRef]
- Breen, K.A.; Sanchez, K.; Kirkman, N.; Seed, P.T.; Parmar, K.; Moore, G.W.; Hunt, B.J. Endothelial and platelet microparticles in patients with antiphospholipid antibodies. Thromb. Res. 2014, 135, 368–374. [Google Scholar] [CrossRef]
- Camoin-Jau, L.; Sabatier, F.; Arnoux, D.; Anfosso, F.; Bardin, N.; Veit, V.; Combes, V.; Gentile, S.; Moal, V.; Sanmarco, M.; et al. Endothelial microparticles: A potential contribution to the thrombotic complications of the antiphospholipid syndrome. Thromb. Haemost. 2004, 91, 667–673. [Google Scholar] [CrossRef] [PubMed]
- Vikerfors, A.; Mobarrez, F.; Bremme, K.; Holmström, M.; Ågren, A.; Eelde, A.; Bruzelius, M.; Antovic, A.; Wallén, H.; Svenungsson, E. Studies of microparticles in patients with the antiphospholipid syndrome (APS). Lupus 2012, 21, 802–805. [Google Scholar] [CrossRef] [PubMed]
- Willemze, R.; Bradford, R.L.; Mooberry, M.J.; Roubey, R.A.S.; Key, N.S. Plasma microparticle tissue factor activity in patients with antiphospholipid antibodies with and without clinical complications. Thromb. Res. 2013, 133, 187–189. [Google Scholar] [CrossRef] [PubMed]
- Campello, E.; Radu, C.M.; Tonello, M.; Kuzenko, A.; Bulato, C.; Hoxha, A.; Mattia, E.; Spiezia, L.; Ruffatti, A.; Simioni, P. Circulating microparticles in pregnant patients with primary anti-phospholipid syndrome: An exploratory study. Scand. J. Rheumatol. 2018, 47, 501–504. [Google Scholar] [CrossRef] [PubMed]
- Hahn, B.H.; McMahon, M.A.; Wilkinson, A.; Wallace, W.D.; Daikh, D.I.; Fitzgerald, J.D.; Karpouzas, G.A.; Merrill, J.T.; Wallace, D.J.; Yazdany, J.; et al. American College of Rheumatology guidelines for screening, treatment, and management of lupus nephritis. Arthritis Rheum. 2012, 64, 797–808. [Google Scholar] [CrossRef] [PubMed]
- Mobarrez, F.; Vikerfors, A.; Gustafsson, J.T.; Gunnarsson, I.; Zickert, A.; Larsson, A.; Pisetsky, D.S.; Wallén, H.; Svenungsson, E. Microparticles in the blood of patients with systemic lupus erythematosus (SLE): Phenotypic characterization and clinical associations. Sci. Rep. 2016, 6, 36025. [Google Scholar] [CrossRef] [PubMed]
- Burbano, C.; Villar-Vesga, J.; Orejuela, J.; Muñoz, C.; Vanegas, A.; Vásquez, G.; Rojas, M.; Castaño, D. Potential Involvement of Platelet-Derived Microparticles and Microparticles Forming Immune Complexes during Monocyte Activation in Patients with Systemic Lupus Erythematosus. Front. Immunol. 2018, 9, 322. [Google Scholar] [CrossRef]
- Nielsen, C.T.; Østergaard, O.; Johnsen, C.; Jacobsen, S.; Heegaard, N.H.H. Distinct features of circulating microparticles and their relationship to clinical manifestations in systemic lupus erythematosus. Arthritis Rheum. 2011, 63, 3067–3077. [Google Scholar] [CrossRef]
- Ullal, A.J.; Reich, C.F.; Clowse, M.; Criscione-Schreiber, L.G.; Tochacek, M.; Monestier, M.; Pisetsky, D.S. Microparticles as antigenic targets of antibodies to DNA and nucleosomes in systemic lupus erythematosus. J. Autoimmun. 2011, 36, 173–180. [Google Scholar] [CrossRef]
- Al-Mayouf, S.M.; Sunker, A.; Abdwani, R.; Al Abrawi, S.; Almurshedi, F.; Alhashmi, N.; Al Sonbul, A.; Sewairi, W.; Qari, A.; Abdallah, E.; et al. Loss-of-function variant in DNASE1L3 causes a familial form of systemic lupus erythematosus. Nat. Genet. 2011, 43, 1186–1188. [Google Scholar] [CrossRef]
- Ueki, M.; Takeshita, H.; Fujihara, J.; Iida, R.; Yuasa, I.; Kato, H.; Panduro, A.; Nakajima, T.; Kominato, Y.; Yasuda, T. Caucasian-specific allele in non-synonymous single nucleotide polymorphisms of the gene encoding deoxyribonuclease I-like 3, potentially relevant to autoimmunity, produces an inactive enzyme. Clin. Chim. Acta 2009, 407, 20–24. [Google Scholar] [CrossRef]
- Sisirak, V.; Sally, B.; D’Agati, V.; Martinez-Ortiz, W.; Özçakar, Z.B.; David, J.; Rashidfarrokhi, A.; Yeste, A.; Panea, C.; Chida, A.S.; et al. Digestion of Chromatin in Apoptotic Cell Microparticles Prevents Autoimmunity. Cell 2016, 166, 88–101. [Google Scholar] [CrossRef]
- López, P.; Rodríguez-Carrio, J.; Martínez-Zapico, A.; Caminal-Montero, L.; Suárez, A. Circulating microparticle subpopulations in systemic lupus erythematosus are affected by disease activity. Int. J. Cardiol. 2017, 236, 138–144. [Google Scholar] [CrossRef]
- McCarthy, E.; Moreno-Martinez, D.; Wilkinson, F.; McHugh, N.; Bruce, I.; Pauling, J.; Alexander, M.; Parker, B. Microparticle subpopulations are potential markers of disease progression and vascular dysfunction across a spectrum of connective tissue disease. BBA Clin. 2017, 7, 16–22. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Atehortúa, L.; Rojas, M.; Vásquez, G.; Muñoz-Vahos, C.H.; Vanegas-García, A.; Posada-Duque, R.A.; Castaño, D. Endothelial activation and injury by microparticles in patients with systemic lupus erythematosus and rheumatoid arthritis. Arthritis Res. 2019, 21, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Kaplan, M.J. Neutrophils in the pathogenesis and manifestations of SLE. Nat. Rev. Rheumatol. 2011, 7, 691–699. [Google Scholar] [CrossRef] [PubMed]
- Perl, A. Oxidative stress in the pathology and treatment of systemic lupus erythematosus. Nat. Rev. Rheumatol. 2013, 9, 674–686. [Google Scholar] [CrossRef]
- Winberg, L.K.; Jacobsen, S.; Nielsen, C.H. Microparticles from patients with systemic lupus erythematosus induce production of reactive oxygen species and degranulation of polymorphonuclear leukocytes. Arthritis Res. 2017, 19, 230. [Google Scholar] [CrossRef] [PubMed]
- Dieker, J.J.; Tel, J.J.; Pieterse, E.E.; Thielen, A.; Rother, N.N.; Bakker, M.; Fransen, J.J.; Dijkman, H.B.P.M.; Berden, J.H.; De Vries, J.M.; et al. Circulating Apoptotic Microparticles in Systemic Lupus Erythematosus Patients Drive the Activation of Dendritic Cell Subsets and Prime Neutrophils for NETosis. Arthritis Rheumatol. 2016, 68, 462–472. [Google Scholar] [CrossRef]
- Rother, N.; Pieterse, E.; Lubbers, J.; Hilbrands, L.; Van Der Vlag, J. Acetylated Histones in Apoptotic Microparticles Drive the Formation of Neutrophil Extracellular Traps in Active Lupus Nephritis. Front. Immunol. 2017, 8, 1136. [Google Scholar] [CrossRef]
- Sasaki, T.; Brakebusch, C.; Engel, J.; Timpl, R. Mac-2 binding protein is a cell-adhesive protein of the extracellular matrix which self-assembles into ring-like structures and binds beta1 integrins, collagens and fibronectin. EMBO J. 1998, 17, 1606–1613. [Google Scholar] [CrossRef]
- Nielsen, C.T.; Østergaard, O.; Rekvig, O.P.; Sturfelt, G.; Jacobsen, S.; Heegaard, N.H.H. Galectin-3 binding protein links circulating microparticles with electron dense glomerular deposits in lupus nephritis. Lupus 2015, 24, 1150–1160. [Google Scholar] [CrossRef] [PubMed]
- Rasmussen, N.S.; Nielsen, C.T.; Jacobsen, S. Microvesicles in active lupus nephritis show Toll-like receptor 9-dependent co-expression of galectin-3 binding protein and double-stranded DNA. Clin. Exp. Immunol. 2021, 204, 64–77. [Google Scholar] [CrossRef] [PubMed]
- Lu, J.; Hu, Z.B.; Chen, P.P.; Lu, C.C.; Zhang, J.X.; Li, X.Q.; Yuan, B.Y.; Huang, S.J.; Ma, K.L. Urinary podocyte microparticles are associated with disease activity and renal injury in systemic lupus erythematosus. BMC Nephrol. 2019, 20, 303. [Google Scholar] [CrossRef] [PubMed]
- Burbano, C.; Gómez-Puerta, J.; Muñoz-Vahos, C.; Vanegas-García, A.; Rojas, M.; Vásquez, G.; Castaño, D. HMGB1+ microparticles present in urine are hallmarks of nephritis in patients with systemic lupus erythematosus. Eur. J. Immunol. 2019, 49, 323–335. [Google Scholar] [CrossRef] [PubMed]
- Perez-Hernandez, J.; Forner, M.J.; Pinto, C.; Chaves, F.J.; Cortes, R.; Redon, J. Increased Urinary Exosomal MicroRNAs in Patients with Systemic Lupus Erythematosus. PLoS ONE 2015, 10, e0138618. [Google Scholar] [CrossRef] [PubMed]
- Solé, C.; Cortés-Hernández, J.; Felip, M.L.; Vidal, M.; Ordi-Ros, J. miR-29c in urinary exosomes as predictor of early renal fibrosis in lupus nephritis. Nephrol. Dial. Transplant. 2015, 30, 1488–1496. [Google Scholar] [CrossRef] [PubMed]
- Solé, C.; Moliné, T.; Vidal, M.; Ordi-Ros, J.; Cortés-Hernández, J. An Exosomal Urinary miRNA Signature for Early Diagnosis of Renal Fibrosis in Lupus Nephritis. Cells 2019, 8, 773. [Google Scholar] [CrossRef] [PubMed]
- Navarro-Quiroz, E.; Pacheco-Lugo, L.; Navarro-Quiroz, R.; Lorenzi, H.; España-Puccini, P.; Díaz-Olmos, Y.; Almendrales, L.; Olave, V.; Gonzalez-Torres, H.; Diaz-Perez, A.; et al. Profiling analysis of circulating microRNA in peripheral blood of patients with class IV lupus nephritis. PLoS ONE 2017, 12, e0187973. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Xu, X.; Tang, X.; Bian, X.; Shen, B.; Zhao, H.; Luo, S.; Chen, Z.; Zhang, K. MicroRNA expression profile of urinary exosomes in Type IV lupus nephritis complicated by cellular crescent. J. Biol. Res. 2018, 25, 1–13. [Google Scholar] [CrossRef]
- Garcia-Vives, E.; Solé, C.; Moliné, T.; Vidal, M.; Agraz, I.; Ordi-Ros, J.; Cortés-Hernández, J. The Urinary Exosomal miRNA Expression Profile is Predictive of Clinical Response in Lupus Nephritis. Int. J. Mol. Sci. 2020, 21, 1372. [Google Scholar] [CrossRef]
- Mobarrez, F.; Fuzzi, E.; Gunnarsson, I.; Larsson, A.; Eketjäll, S.; Pisetsky, D.S.; Svenungsson, E. Microparticles in the blood of patients with SLE: Size, content of mitochondria and role in circulating immune complexes. J. Autoimmun. 2019, 102, 142–149. [Google Scholar] [CrossRef]
- Arvidsson, I.; Ståhl, A.-L.; Hedström, M.M.; Kristoffersson, A.-C.; Rylander, C.; Westman, J.S.; Storry, J.R.; Olsson, M.L.; Karpman, D. Shiga Toxin–Induced Complement-Mediated Hemolysis and Release of Complement-Coated Red Blood Cell–Derived Microvesicles in Hemolytic Uremic Syndrome. J. Immunol. 2015, 194, 2309–2318. [Google Scholar] [CrossRef]
- Varrone, E.; Carnicelli, D.; Brigotti, M. Extracellular Vesicles and Renal Endothelial Cells. Am. J. Pathol. 2021, 1–10. [Google Scholar] [CrossRef]
- Ståhl, A.-L.; Arvidsson, I.; Johansson, K.E.; Chromek, M.; Rebetz, J.; Loos, S.; Kristoffersson, A.-C.; Békássy, Z.D.; Mörgelin, M.; Karpman, D. A Novel Mechanism of Bacterial Toxin Transfer within Host Blood Cell-Derived Microvesicles. PLoS Pathog. 2015, 11, e1004619. [Google Scholar] [CrossRef]
- Johansson, K.; Willysson, A.; Kristoffersson, A.-C.; Tontanahal, A.; Gillet, D.; Ståhl, A.-L.; Karpman, D. Shiga Toxin-Bearing Microvesicles Exert a Cytotoxic Effect on Recipient Cells Only When the Cells Express the Toxin Receptor. Front. Cell. Infect. Microbiol. 2020, 10, 212. [Google Scholar] [CrossRef] [PubMed]
- Tahmasbi, L.; Karimi, M.; Kafiabadi, S.A.; Nikougoftar, M.; Haghpanah, S.; Ranjbaran, R.; Moghadam, M. Evaluation of Plasma Platelet Microparticles in Thrombotic Thrombocytopenic Purpura. Ann. Clin. Lab. Sci. 2017, 47, 62–67. [Google Scholar] [PubMed]
- Jimenez, J.J.; Jy, W.; Mauro, L.M.; Horstman, L.L.; Soderland, C.; Ahn, Y.S. Endothelial microparticles released in thrombotic thrombocytopenic purpura express von Willebrand factor and markers of endothelial activation. Br. J. Haematol. 2003, 123, 896–902. [Google Scholar] [CrossRef]
- Tati, R.; Kristoffersson, A.-C.; Ståhl, A.-L.; Rebetz, J.; Wang, L.; Licht, C.; Motto, D.; Karpman, D. Complement Activation Associated with ADAMTS13 Deficiency in Human and Murine Thrombotic Microangiopathy. J. Immunol. 2013, 191, 2184–2193. [Google Scholar] [CrossRef]
- Jennette, J.C.; Falk, R.J.; Bacon, P.A.; Basu, N.; Cid, M.C.; Ferrario, F.; Flores-Suarez, L.F.; Gross, W.L.; Guillevin, L.; Hagen, E.C.; et al. 2012 Revised International Chapel Hill Consensus Conference Nomenclature of Vasculitides. Arthritis Rheum. 2013, 65, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Weidner, S.; Hafezi-Rachti, S.; Rupprecht, H.D. Thromboembolic events as a complication of antineutrophil cytoplasmic antibody–associated vasculitis. Arthritis Rheum. 2006, 55, 146–149. [Google Scholar] [CrossRef]
- Cartin-Ceba, R.; Peikert, T.; Specks, U. Pathogenesis of ANCA-Associated Vasculitis. Curr. Rheumatol. Rep. 2012, 14, 481–493. [Google Scholar] [CrossRef]
- Gou, S.-J.; Yuan, J.; Chen, M.; Yu, F.; Zhao, M.-H. Circulating complement activation in patients with anti-neutrophil cytoplasmic antibody–associated vasculitis. Kidney Int. 2013, 83, 129–137. [Google Scholar] [CrossRef]
- Huang, Y.-M.; Wang, H.; Wang, C.; Chen, M.; Zhao, M.-H. Promotion of Hypercoagulability in Antineutrophil Cytoplasmic Antibody-Associated Vasculitis by C5a-Induced Tissue Factor-Expressing Microparticles and Neutrophil Extracellular Traps. Arthritis Rheumatol. 2015, 67, 2780–2790. [Google Scholar] [CrossRef]
- Mendoza, C.E.; Brant, E.J.; McDermott, M.L.; Froment, A.; Hu, Y.; Hogan, S.L.; Jennette, J.C.; Falk, R.J.; Nachman, P.H.; Derebail, V.K.; et al. Elevated Microparticle Tissue Factor Activity Differentiates Patients With Venous Thromboembolism in Anti-neutrophil Cytoplasmic Autoantibody Vasculitis. Kidney Int. Rep. 2019, 4, 1617–1629. [Google Scholar] [CrossRef]
- Daniel, L.; Fakhouri, F.; Joly, D.; Mouthon, L.; Nusbaum, P.; Grunfeld, J.-P.; Schifferli, J.; Guillevin, L.; Lesavre, P.; Halbwachs-Mecarelli, L. Increase of circulating neutrophil and platelet microparticles during acute vasculitis and hemodialysis. Kidney Int. 2006, 69, 1416–1423. [Google Scholar] [CrossRef] [PubMed]
- Brogan, P.A.; Shah, V.; Brachet, C.; Harnden, A.; Mant, D.; Klein, N.; Dillon, M.J. Endothelial and platelet microparticles in vasculitis of the young. Arthritis Rheum. 2004, 50, 927–936. [Google Scholar] [CrossRef] [PubMed]
- Kahn, R.; Mossberg, M.; Ståhl, A.-L.; Johansson, K.; Lindman, I.L.; Heijl, C.; Segelmark, M.; Mörgelin, M.; Leeb-Lundberg, L.F.; Karpman, D. Microvesicle transfer of kinin B1-receptors is a novel inflammatory mechanism in vasculitis. Kidney Int. 2017, 91, 96–105. [Google Scholar] [CrossRef]
- Prikryl, P.; Satrapova, V.; Frydlova, J.; Hruskova, Z.; Zima, T.; Tesar, V.; Vokurka, M. Mass spectrometry-based proteomic exploration of the small urinary extracellular vesicles in ANCA-associated vasculitis in comparison with total urine. J. Proteom. 2020, 233, 104067. [Google Scholar] [CrossRef]
- Surmiak, M.; Gielicz, A.; Stojkov, D.; Szatanek, R.; Wawrzycka-Adamczyk, K.; Yousefi, S.; Simon, H.-U.; Sanak, M. LTB4 and 5-oxo-ETE from extracellular vesicles stimulate neutrophils in granulomatosis with polyangiitis. J. Lipid Res. 2020, 61, 1–9. [Google Scholar] [CrossRef]
- Surmiak, M.; Kosalka-Węgiel, J.; Polański, S.; Sanak, M. Endothelial cells response to neutrophil-derived extracellular vesicles miRNAs in anti-PR3 positive vasculitis. Clin. Exp. Immunol. 2021, 1–16. [Google Scholar] [CrossRef]
- Wang, Y.; Bai, Y.; Liu, Y.; Noel, S.W.; Yan, Q.; Thi, H.P.; Sun, X.; Wei, W.; Ma, J.; Zheng, F. Plasma exosomal miRNAs involved in endothelial injury in microscopic polyangiitis patients. FASEB J. 2020, 34, 6215–6228. [Google Scholar] [CrossRef]
- Manojlovic, M.; Juto, A.; Jonasdottir, A.; Colic, J.; Vojinovic, J.; Nordin, A.; Bruchfeld, A.; Gunnarsson, I.; Mobarrez, F.; Antovic, A. Microparticles expressing myeloperoxidase as potential biomarkers in anti-neutrophil cytoplasmic antibody (ANCA)-associated vasculitides (AAV). J. Mol. Med. 2020, 98, 1279–1286. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Chang, D.-Y.; Chen, M.; Zhao, M.-H. HMGB1 contributes to glomerular endothelial cell injury in ANCA-associated vasculitis through enhancing endothelium-neutrophil interactions. J. Cell. Mol. Med. 2017, 21, 1351–1360. [Google Scholar] [CrossRef] [PubMed]
- Antovic, A.; Mobarrez, F.; Manojlovic, M.; Soutari, N.; Baggemar, V.D.P.; Nordin, A.; Bruchfeld, A.; Vojinovic, J.; Gunnarsson, I. Microparticles Expressing Myeloperoxidase and Complement C3a and C5a as Markers of Renal Involvement in Antineutrophil Cytoplasmic Antibody–associated Vasculitis. J. Rheumatol. 2020, 47, 714–721. [Google Scholar] [CrossRef]
- Miao, D.; Ma, T.-T.; Chen, M.; Zhao, M.-H. Platelets release proinflammatory microparticles in anti-neutrophil cytoplasmic antibody-associated vasculitis. Rheumatology 2019, 58, 1432–1442. [Google Scholar] [CrossRef] [PubMed]
| Study | EV Biomarkers | Cellular Origin of EV | Study Findings | Reference |
|---|---|---|---|---|
| Štok, U.; et al. | CD8, CD44, CD133/1, CD62P | Platelets, endothelial cells, lymphocytes, antigen-presenting cells | EV increased in patients with thrombotic events EV reflect endothelial and platelet chronic activation | [6] |
| Chaturvedi, S.; et al., Breen, K.A.; et al. | CD41, CD61, CD51, CD105 | Endothelial cells, platelets | EV increased in aPL+ patients EV reflect endothelial and platelet chronic activation | [44,45] |
| Chaturvedi, S.; et al., Willemze, R.; et al. | Tissue factor (TF) | Endothelial cells | TF + EV increased in APS TF activity increased in EV from aPL+ patients | [44,48] |
| Mobarrez, F.; et al. | β2GPI+ | EV β2GPI+ reduced in SLE aPL+ Anti-β2GPI may bind to β2GPI expressed by EV | [19] | |
| Campello, E.; et al. | Phosphatidylserine (PS), Endoglin, Tissue factor (TF) | Endothelial cells, platelets | PS+ EV, endoglin+ EV and endothelium-derived EV increased in 1st and 2nd trimester of pregnancy; TF+ EV and platelet-derived EV increased in 3rd trimester of pregnancy Correlation with thrombosis and systemic platelet and endothelial activation in obstetric APS | [49] |
| Study | EV Concentration | Cellular Origin of EV | EV Pathological Significance | Reference |
|---|---|---|---|---|
| Burbano, C.; et al. | Increased in SLE compared to healthy controls | platelet | Formation of immune complexes, source of nuclear antigens, correlation with disease activity | [52] |
| López, P.; et al. | Increased in SLE compared to healthy controls | platelet, monocyte, T lymphocyte | EV level correlated with: disease activity, glucocorticoid therapy, endothelial vasodilatation | [58] |
| Atehortúa, L.; et al. | Endothelial cell activation, endothelial injury, | [60] | ||
| Winberg, L.-K.; et al., Dieker, J.J.; et al., Rother, N.; et al. | In vitro stimulation of polymorphonuclear leukocytes with EV from SLE patients increased ROS production EV promote neutrophil activation and NETs production | [63,64,65] | ||
| Nielsen, C.T.; et al., Rasmussen, N.S.; et al. | IgG/galectin-3 binding protein (G3BP)+ EV are involved in the pathogenesis of lupus nephritis | [67,68] | ||
| Lu, J.; et al., Vanegas-García, A.; et al. | Urinary podocyte-derived EV increased in SLE | Urinary EV | Urinary podocyte-derived EV level correlated with systemic disease activity and renal injury Urinary EV high-mobility group box 1 molecule (HMGB1)+ were found to be higher in lupus nephritis | [69,70] |
| Felip, M.L.; et al., Solé, C.; et al., Navarro-Quiroz, E.; et al., Li, Y.; et al., Garcia-Vives, E.; et al. | EV derived miRNA | miR-21, miR-150, and miR-29c, miR-31, miR-107, and miR-135b-5p correlated with renal injury in lupus nephritis | [72,73,74,75,76] | |
| Mobarrez, F.; et al. | EV containing mitochondrial molecules (mitoEV) | mitoEV were associated with disease activity, immune complex formation and renal damage | [77] |
| Disease | Study | Cellular Origin of EV | EV Biomarkers | EV Pathological Significance | Reference |
|---|---|---|---|---|---|
| STEC-HUS | Ståhl, A.-L.; et al., Arvidsson, I.; et al. | platelets, monocytes, neutrophils | Tissue factor, phosphatidylserine (PS), C3, C9 | Promotion of thrombosis EV reflect complement activation | [22,78] |
| STEC-HUS | Varrone, E.; et al., Ståhl, A.-L.; et al., Johansson, K.; et al. | EV carrying Shiga toxin | Delivery system of Shiga toxin to the kidney involvement in renal cell injury | [79,80,81] | |
| TTP | Tahmasbi, L.; et al., Jimenez, J.J.; et al. | platelets, endothelial cells | CD62E (E-selectin), VWF, intercellular adhesion molecule 1 (ICAM-1), platelet endothelial cell adhesion molecule (PECAM-1; CD31) and endoglin (CD105) | Pro-coagulant and pro-adhesive roles | [82,83] |
| TTP | Tati, R.; et al. | Endothelial cells | C3, C9 | EV reflect complement activation | [84] |
| Study | EV Biomarkers | EV Cellular Origin | Study Findings | Reference |
|---|---|---|---|---|
| Daniel, L.; et al. | proteinase 3 (PR3), myeloperoxidase (MPO) | EV released from primed neutrophils in vitro | EV can induce endothelial activation, ROS production, cytokines release | [91] |
| Brogan, P.A.; et al. | Platelets, neutrophils, endothelial cells | EV level increased in vasculitis Decrease of neutrophil-derived EV after treatment Endothelial-derived EV correlated with disease activity | [92] | |
| Kahn, R.; et al. | B1 kinin receptor | Leukocytes | EV level increased in vasculitis Neutrophil-derived B1+ EV found on glomerular endothelial cells and renal injury | [93] |
| Prikryl, P.; et al. | Urinary EV | Proteomic EV profiling showed different regulation of proteins potentially involved in vasculitis pathogenesis | [94] | |
| Surmiak, M.; et al. | leukotriene (LT)B4, 5-oxo-eicosatetraenoic acid (5-oxo-ETE) | EV enriched in LTB4 and 5-oxo-ETE in granulomatosis with polyangiitis | [95] | |
| Wang, Y.; et al. | Sequencing analysis of EV miRNA cargo in microscopic polyangiitis identified a correlation between miR-185-3p, miR-125a-3p and both the clinical activity score and proteinuria | [97] | ||
| Manojlovic, M.; et al. | myeloperoxidase (MPO), PTX3, high mobility group box 1 (HMGB1) | PTX3+ and HMGB1+ EV correlated with disease activity HMGB1 potentially associated with renal injury | [98] | |
| Antovic, A.; et al. | myeloperoxidase (MPO), C3a, C5a | MPO C3a+ and C5a+ EV increased in vasculitis, particularly in patients with renal involvement C3a and C5a expressed on EV correlated with disease activity | [100] | |
| Miao, D.; et al. | chemokines, adhesion molecules, growth and apoptotic factors | Platelets | Increased EV in vasculitis EV correlate with disease activity and renal injury | [101] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mazzariol, M.; Camussi, G.; Brizzi, M.F. Extracellular Vesicles Tune the Immune System in Renal Disease: A Focus on Systemic Lupus Erythematosus, Antiphospholipid Syndrome, Thrombotic Microangiopathy and ANCA-Vasculitis. Int. J. Mol. Sci. 2021, 22, 4194. https://doi.org/10.3390/ijms22084194
Mazzariol M, Camussi G, Brizzi MF. Extracellular Vesicles Tune the Immune System in Renal Disease: A Focus on Systemic Lupus Erythematosus, Antiphospholipid Syndrome, Thrombotic Microangiopathy and ANCA-Vasculitis. International Journal of Molecular Sciences. 2021; 22(8):4194. https://doi.org/10.3390/ijms22084194
Chicago/Turabian StyleMazzariol, Martina, Giovanni Camussi, and Maria Felice Brizzi. 2021. "Extracellular Vesicles Tune the Immune System in Renal Disease: A Focus on Systemic Lupus Erythematosus, Antiphospholipid Syndrome, Thrombotic Microangiopathy and ANCA-Vasculitis" International Journal of Molecular Sciences 22, no. 8: 4194. https://doi.org/10.3390/ijms22084194
APA StyleMazzariol, M., Camussi, G., & Brizzi, M. F. (2021). Extracellular Vesicles Tune the Immune System in Renal Disease: A Focus on Systemic Lupus Erythematosus, Antiphospholipid Syndrome, Thrombotic Microangiopathy and ANCA-Vasculitis. International Journal of Molecular Sciences, 22(8), 4194. https://doi.org/10.3390/ijms22084194






