Optimization of Blood Handling and Peripheral Blood Mononuclear Cell Cryopreservation of Low Cell Number Samples
Abstract
1. Introduction
2. Results
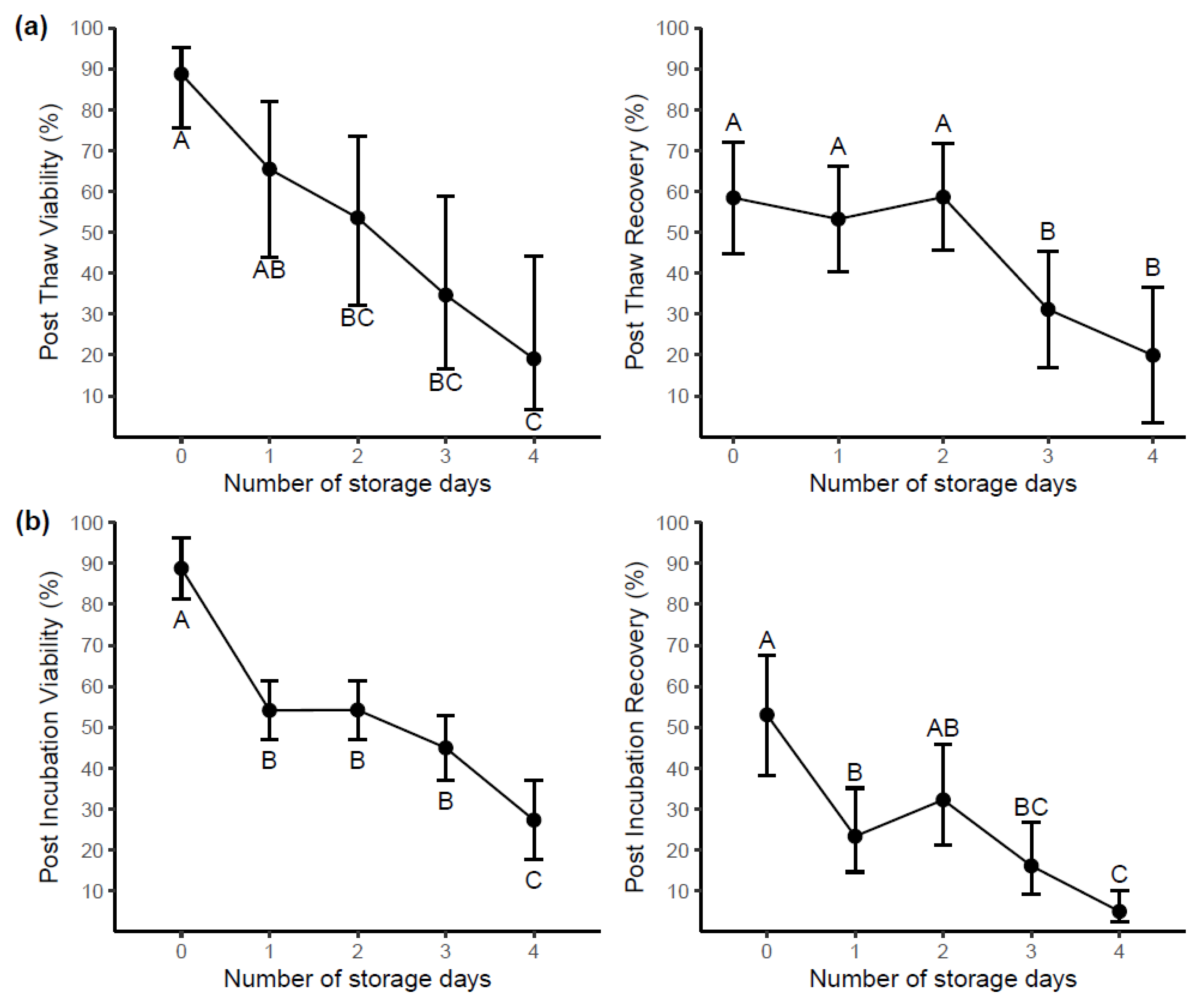
2.1. Experiment 1: Effects of Storage Temperature and of Delayed Processing on PBMC Viability and Recovery
2.1.1. Storage Assessment
2.1.2. Post-Thaw and Post-Incubation Assessment
2.1.3. Cell Functionality
2.1.4. Immunophenotyping of Cell Population
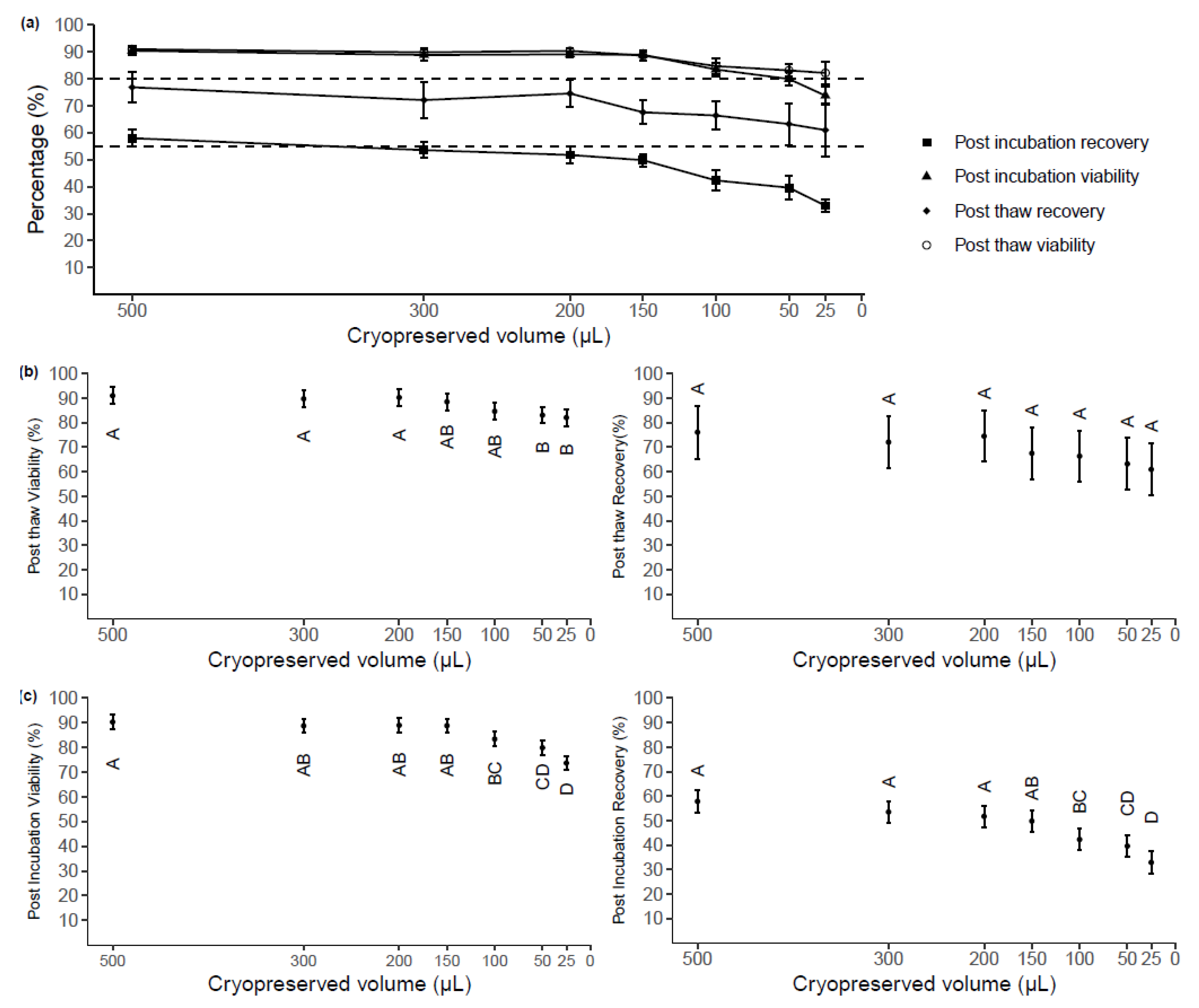
2.2. Experiment 2: Impact of Cryopreserved Cell Volume on PBMC Quality Evaluated Post-Thaw and Post-Incubation
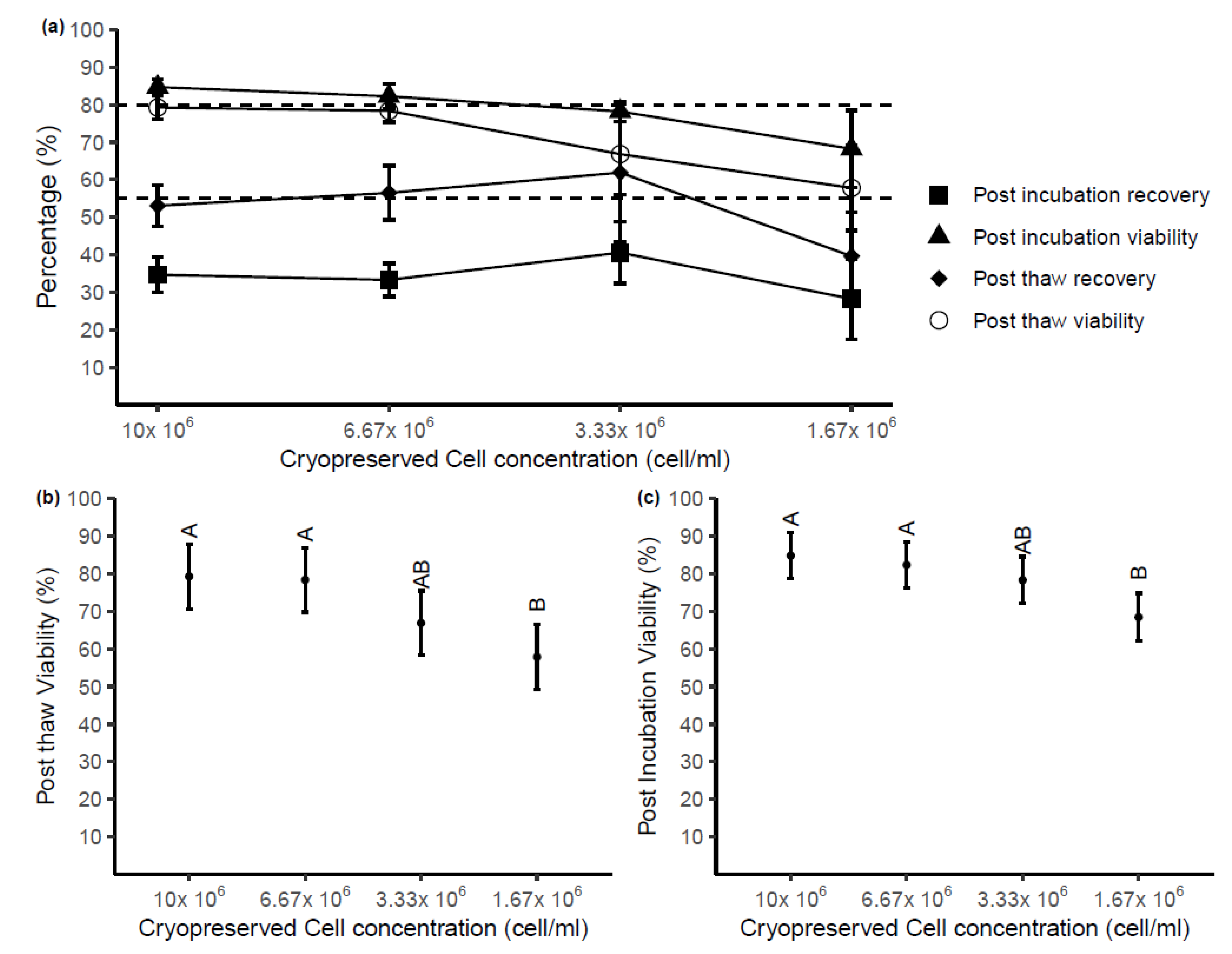
2.3. Experiment 3: Impacts of Cryopreserved Cell Concentration on PBMC Quality Evaluated Post-Thaw and Post-Incubation
3. Discussion
4. Materials and Methods
4.1. Experiment 1: Effects of Storage Temperature and Delayed Processing on PBMC Viability and Recovery
4.2. Experiment 2: Impact of Cryopreserved Cell Volume on PBMC Quality Evaluated Post-Thaw and Post-Incubation
4.3. Experiment 3: Impacts of Cryopreserved Cell Concentration on PBMC Quality Evaluated Post-Thaw and Post-Incubation
4.4. Statistical Analysis
5. Conclusions
- After 24 h, samples stored at RT have higher viability and yield than samples stored at 4 °C with no statistical difference in these variables when compared to samples processed immediately. When thawed these samples have less viability and recovery after an overnight incubation when compared with samples processed immediately. Further analysis reveals that 24 h of storage reduces the relative proportions of Monocytes and NK cells and a significant decrease in IFN-γ release upon PHA stimulation with a similar trend with CEF peptide stimulated cells (p = 0.68).
- After 48 h, blood samples stored at 4 °C have >50% yield of viable cells still present. When thawed, these samples have a decreased post-thaw viability compared to samples cryopreserved without delay. Samples stored at RT have an increase in contaminating LD neutrophils coupled with an increase in T cells and a decrease in B cells compared with samples stored at 4 °C. Interestingly, IFN-γ release has returned to similar levels of samples processed without delay.
- After 3 days, blood samples at 4 °C have higher yields than samples stored at RT.
- When these cells are thawed they have a decrease in post-thaw recovery.
- After 4 days, four out of five (80%) of the samples store at RT are completely lost whereas the samples stored at 4 °C still have similar viability to samples stored for 3 days.
- >4 days, 100% of samples stored at RT are completely lost. Samples stored at 4 °C still have ≈40% viability until day 8. Decreasing yield/day is observed until some samples are completely lost at day 9.
- This finding supports the proposal that blood can still be collected and processed for viable PBMC from participants enrolled in clinical studies living in remote regions that might experience transportation delays.
- Additionally, our data suggest that PBMC can be successfully stored at ≥6.67 × 106 cells/mL in ≥150 µL without significant loss compared with a sample five times the size. This finding provides evidence for more opportunities to store PBMC from infants and children, as well as from individuals with limited blood draw volumes (<1 mL).
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ARCLB | Australian Red Cross Lifeblood |
| CCS | Cosmic calf serum |
| CHAVI | Centre for HIV/AIDS Vaccine Immunology |
| DMSO | Dimethyl sulfoxide |
| EDTA | Ethylenediaminetetraacetic acid |
| ENDIA | Environmental determinants of islet autoimmunity |
| IBBL | Integrated Biobank of Luxembourg |
| NHMRC | Australian National Health and Medical Research Council |
| PBMC | Peripheral blood mononuclear cells |
| RT | Room temperature |
| NK | Natural Killer |
| PHA | Phytohaemagglutinin |
| SD | Standard deviation |
| CI | Confidence interval |
| LSD | Least significant difference |
| SEM | Standard error of the mean |
| CEF | Epstein–Barr and Flu virus |
| PHA | Phytohemagglutinin A |
References
- Chang, C.-W.; Yang, S.-Y.; Yang, C.-C.; Chang, C.-W.; Wu, Y.-R. Plasma and Serum Alpha-Synuclein as a Biomarker of Diagnosis in Patients with Parkinson’s Disease. Front. Neurol. 2019, 10, 1388. [Google Scholar] [CrossRef]
- Moravkova, P.; Kohoutova, D.; Vavrova, J.; Bures, J. Serum S100A6, S100A8, S100A9 and S100A11 proteins in colorectal neoplasia: Results of a single centre prospective study. Scand. J. Clin. Lab. Investig. 2019, 80, 173–178. [Google Scholar] [CrossRef]
- Honge, B.L.; Petersen, M.S.; Olesen, R.; Moller, B.K.; Erikstrup, C. Optimizing recovery of frozen human peripheral blood mononuclear cells for flow cytometry. PLoS ONE 2017, 12, e0187440. [Google Scholar] [CrossRef] [PubMed]
- Gautam, A.; Donohue, D.; Hoke, A.; Miller, S.A.; Srinivasan, S.; Sowe, B.; Detwiler, L.; Lynch, J.; LeVangie, M.; Hammamieh, R.; et al. Investigating gene expression profiles of whole blood and peripheral blood mononuclear cells using multiple collection and processing methods. PLoS ONE 2019, 14, e0225137. [Google Scholar] [CrossRef] [PubMed]
- Holland, M.; Cunningham, R.; Seymour, L.; Kleinsteuber, K.; Cunningham, A.; Patel, T.; Manos, M.; Brennick, R.; Zhou, J.; Hodi, F.S.; et al. Separation, banking, and quality control of peripheral blood mononuclear cells from whole blood of melanoma patients. Cell Tissue Bank. 2018, 19, 783–790. [Google Scholar] [CrossRef]
- Ulmer, A.J.; Scholz, W.; Ernst, M.; Brandt, E.; Flad, H.-D. Isolation and Subfractionation of Human Peripheral Blood Mononuclear Cells (PBMC) by Density Gradient Centrifugation on Percoll. Immunobiology 1984, 166, 238–250. [Google Scholar] [CrossRef]
- Grievink, H.W.; Luisman, T.; Kluft, C.; Moerland, M.; Malone, K.E. Comparison of Three Isolation Techniques for Human Peripheral Blood Mononuclear Cells: Cell Recovery and Viability, Population Composition, and Cell Functionality. Biopreserv. Biobank. 2016, 14, 410–415. [Google Scholar] [CrossRef] [PubMed]
- Corkum, C.P.; Ings, D.P.; Burgess, C.; Karwowska, S.; Kroll, W.; Michalak, T.I. Immune cell subsets and their gene expression profiles from human PBMC isolated by Vacutainer Cell Preparation Tube (CPT™) and standard density gradient. BMC Immunol. 2015, 16, 48. [Google Scholar] [CrossRef]
- Jia, Y.; Xu, H.; Li, Y.; Wei, C.; Guo, R.; Wang, F.; Wu, Y.; Liu, J.; Jia, J.; Yan, J.; et al. A Modified Ficoll-Paque Gradient Method for Isolating Mononuclear Cells from the Peripheral and Umbilical Cord Blood of Humans for Biobanks and Clinical Laboratories. Biopreserv. Biobank. 2018, 16, 82–91. [Google Scholar] [CrossRef]
- Fuss, I.J.; Kanof, M.E.; Smith, P.D.; Zola, H. Isolation of Whole Mononuclear Cells from Peripheral Blood and Cord Blood. Curr. Protoc. Immunol. 2009, 85, 7.1.1–7.1.8. [Google Scholar] [CrossRef]
- Mallone, R.; Mannering, S.I.; Brooks-Worrell, B.M.; Durinovic-Bello, I.; Cilio, C.M.; Wong, F.S.; Schloot, N.C.; Immunology of Diabetes Society T‐Cell Workshop Committee. Isolation and preservation of peripheral blood mononuclear cells for analysis of islet antigen-reactive T cell responses: Position statement of the T-Cell Workshop Committee of the Immunology of Diabetes Society. Clin. Exp. Immunol. 2011, 163, 33–49. [Google Scholar] [CrossRef]
- Higdon, L.E.; Lee, K.; Tang, Q.; Maltzman, J.S. Virtual Global Transplant Laboratory Standard Operating Procedures for Blood Collection, PBMC Isolation, and Storage. Transplant. Direct 2016, 2, e101. [Google Scholar] [CrossRef] [PubMed]
- Castellanos-Uribe, M.; May, S.T.; Betsou, F. Integrated BioBank of Luxembourg–University of Luxembourg: University Biobanking Certificate. Biopreserv. Biobank. 2020, 18, 7–9. [Google Scholar] [CrossRef]
- Bull, M.; Lee, D.; Stucky, J.; Chiu, Y.-L.; Rubin, A.; Horton, H.; McElrath, M.J. Defining blood processing parameters for optimal detection of cryopreserved antigen-specific responses for HIV vaccine trials. J. Immunol. Methods 2007, 322, 57–69. [Google Scholar] [CrossRef] [PubMed]
- Weinberg, A.; Betensky, R.A.; Zhang, L.; Ray, G. Effect of Shipment, Storage, Anticoagulant, and Cell Separation on Lymphocyte Proliferation Assays for Human Immunodeficiency Virus-Infected Patients. Clin. Diagn. Lab. Immunol. 1998, 5, 804–807. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, D.T.; Decker, D.; Zaworski, P.; Klott, K.; McGonigal, J.; Ghazal, N.; Sly, L.; Chung, B.; VanderLugt, J.; Chen, K.S. Evaluation of Peripheral Blood Mononuclear Cell Processing and Analysis for Survival Motor Neuron Protein. PLoS ONE 2012, 7, e50763. [Google Scholar] [CrossRef]
- Agashe, C.; Chiang, D.; Grishin, A.; Masilamani, M.; Jones, S.M.; Wood, R.A.; Sicherer, S.H.; Burks, A.W.; Leung, D.Y.M.; Dawson, P.; et al. Impact of granulocyte contamination on PBMC integrity of shipped blood samples: Implications for multi-center studies monitoring regulatory T cells. J. Immunol. Methods 2017, 449, 23–27. [Google Scholar] [CrossRef]
- Penno, M.A.; Thomson, R.L.; Couper, J.J. Bunbury to Bundaberg, Darwin to Dover: Establishing a successful Regional Participation Program for the ENDIA type 1 diabetes cohort study. Med. J. Aust. 2016, 205, 486. [Google Scholar] [CrossRef]
- Olson, W.C.; Smolkin, M.E.; Farris, E.M.; Fink, R.J.; Czarkowski, A.R.; Fink, J.H.; Chianese-Bullock, K.A.; Slingluff, C.L., Jr. Shipping blood to a central laboratory in multicenter clinical trials: Effect of ambient temperature on specimen temperature, and effects of temperature on mononuclear cell yield, viability and immunologic function. J. Transl. Med. 2011, 9, 26. [Google Scholar] [CrossRef]
- Kloverpris, H.; Fomsgaard, A.; Handley, A.; Ackland, J.; Sullivan, M.; Goulder, P. Dimethyl sulfoxide (DMSO) exposure to human peripheral blood mononuclear cells (PBMCs) abolish T cell responses only in high concentrations and following coincubation for more than two hours. J. Immunol. Methods 2010, 356, 70–78. [Google Scholar] [CrossRef]
- Nazarpour, R.; Zabihi, E.; Alijanpour, E.; Abedian, Z.; Mehdizadeh, H.; Rahimi, F. Optimization of Human Peripheral Blood Mononuclear Cells (PBMCs) Cryopreservation. Int. J. Mol. Cell. Med. 2012, 1, 88–93. [Google Scholar] [PubMed]
- Disis, M.L.; dela Rosa, C.; Goodell, V.; Kuan, L.-Y.; Chang, J.C.; Kuus-Reichel, K.; Clay, T.M.; Kim Lyerly, H.; Bhatia, S.; Ghanekar, S.A.; et al. Maximizing the retention of antigen specific lymphocyte function after cryopreservation. J. Immunol. Methods 2006, 308, 13–18. [Google Scholar] [CrossRef] [PubMed]
- Sarzotti-Kelsoe, M.; Needham, L.K.; Rountree, W.; Bainbridge, J.; Gray, C.M.; Fiscus, S.A.; Ferrari, G.; Stevens, W.S.; Stager, S.L.; Binz, W.; et al. The Center for HIV/AIDS Vaccine Immunology (CHAVI) multi-site quality assurance program for cryopreserved Human Peripheral Blood Mononuclear Cells. J. Immunol. Methods 2014, 409, 21–30. [Google Scholar] [CrossRef] [PubMed]
- Kierstead, L.S.; Dubey, S.; Meyer, B.; Tobery, T.W.; Mogg, R.; Fernandez, V.R.; Long, R.; Guan, L.; Gaunt, C.; Collins, K.; et al. Enhanced Rates and Magnitude of Immune Responses Detected against an HIV Vaccine: Effect of Using an Optimized Process for Isolating PBMC. AIDS Res. Hum. Retroviruses 2007, 23, 86–92. [Google Scholar] [CrossRef]
- Ducar, C.; Smith, D.; Pinzon, C.; Stirewalt, M.; Cooper, C.; McElrath, M.J.; Hural, J.; Network, N.H.V.T. Benefits of a comprehensive quality program for cryopreserved PBMC covering 28 clinical trials sites utilizing an integrated, analytical web-based portal. J. Immunol. Methods 2014, 409, 9–20. [Google Scholar] [CrossRef] [PubMed]
- Posevitz-Fejfar, A.; Posevitz, V.; Gross, C.C.; Bhatia, U.; Kurth, F.; Schutte, V.; Bar-Or, A.; Meuth, S.G.; Wiendl, H. Effects of Blood Transportation on Human Peripheral Mononuclear Cell Yield, Phenotype and Function: Implications for Immune Cell Biobanking. PLoS ONE 2014, 9, e115920. [Google Scholar] [CrossRef]
- Gottfried-Blackmore, A.; Rubin, S.J.S.; Bai, L.; Aluko, S.; Yang, Y.; Park, W.; Habtezion, A. Effects of processing conditions on stability of immune analytes in human blood. Sci. Rep. 2020, 10, 17328. [Google Scholar] [CrossRef]
- Diks, A.M.; Bonroy, C.; Teodosio, C.; Groenland, R.J.; de Mooij, B.; de Maertelaere, E.; Neirynck, J.; Philippe, J.; Orfao, A.; van Dongen, J.J.M.; et al. Impact of blood storage and sample handling on quality of high dimensional flow cytometric data in multicenter clinical research. J. Immunol. Methods 2019, 475, 112616. [Google Scholar] [CrossRef]
- Garraud, O.; Moreau, T. Effect of blood storage on lymphocyte subpopulations. J. Immunol. Methods 1984, 75, 95–98. [Google Scholar] [CrossRef]
- Huang, H.S.; Su, I.J.; Huang, M.J. The effect of blood storage on lymphocyte subpopulations. Zhonghua Min Guo Wei Sheng Wu Ji Mian Yi Xue Za 1987, 20, 46–51. [Google Scholar]
- Weiblen, B.J.; Debell, K.; Giorgio, A.; Valeri, C.R. Monoclonal antibody testing of lymphocytes after overnight storage. J. Immunol. Methods 1984, 70, 179–183. [Google Scholar] [CrossRef]
- Betensky, R.A.; Connick, E.; Devers, J.; Landay, A.L.; Nokta, M.; Plaeger, S.; Rosenblatt, H.; Schmitz, J.L.; Valentine, F.; Wara, D.; et al. Shipment Impairs Lymphocyte Proliferative Responses to Microbial Antigens. Clin. Diagn. Lab. Immunol. 2000, 7, 759–763. [Google Scholar] [CrossRef] [PubMed]
- Nicholson, J.K.; Jones, B.M.; Cross, G.D.; McDougal, J.S. Comparison of T and B cell analyses on fresh and aged blood. J. Immunol. Methods 1984, 73, 29–40. [Google Scholar] [CrossRef]
- Sureda-Vives, M.; Morell-Garcia, D.; Rubio-Alaejos, A.; Valina, L.; Robles, J.; Bauca, J.M. Stability of serum, plasma and urine osmolality in different storage conditions: Relevance of temperature and centrifugation. Clin. Biochem. 2017, 50, 772–776. [Google Scholar] [CrossRef]
- Howie, S.R. Blood sample volumes in child health research: Review of safe limits. Bull. World Health Organ. 2011, 89, 46–53. [Google Scholar] [CrossRef]
- Ramachandran, H.; Laux, J.; Moldovan, I.; Caspell, R.; Lehmann, P.V.; Subbramanian, R.A. Optimal Thawing of Cryopreserved Peripheral Blood Mononuclear Cells for Use in High-Throughput Human Immune Monitoring Studies. Cells 2012, 1, 313–324. [Google Scholar] [CrossRef] [PubMed]
- Bates, D.; Mächler, M.B.; Bolker, B.; Walker, C.S. Fitting linear mixed-effects models using lme4. J. Stat. Softw. 2015, 67, 1–48. [Google Scholar] [CrossRef]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2018. [Google Scholar]
- Jørgensen, E.; Pedersen, A. How to Obtain Those Nasty Standard Errors from Transformed Data—And Why They Should Not Be Used; Internal Report 7: 1–20; Faculty of Agricultural Sciences, Aarhus University: Aarhus, Denmark, 1998. [Google Scholar]
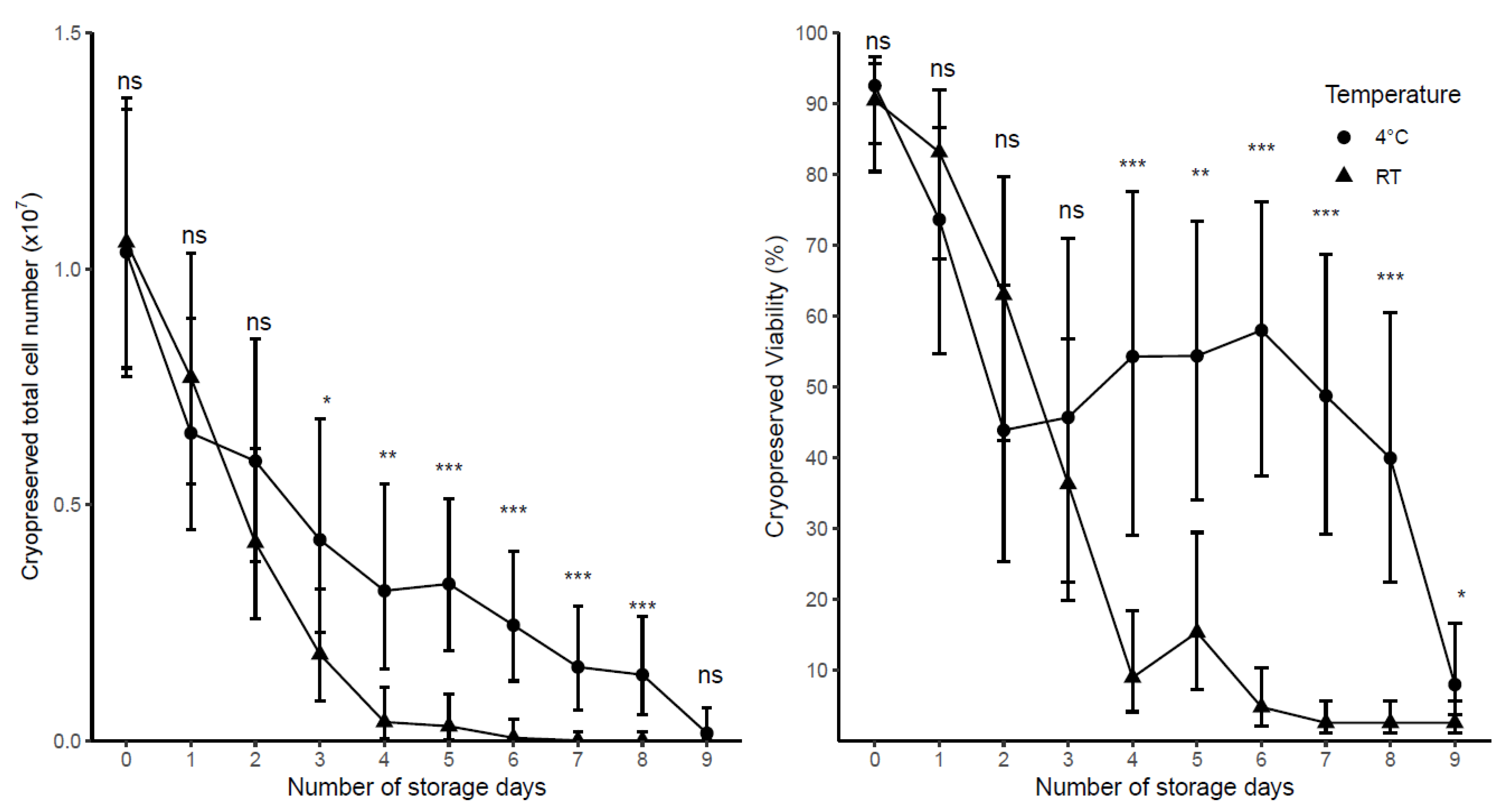
| Day | Cryopreserved Viability (%) | Cryopreserved Total Viable Cell Number (× 107) | ||
|---|---|---|---|---|
| 4 °C | RT | 4 °C | RT | |
| 0 | 92.53 (84.30, 96.62) | 90.45 (80.40, 95.62) | 1.04 (0.77, 1.34) | 1.06 (0.79, 1.36) |
| 1 | 73.61 * (54.73, 86.55) | 83.14 ns (68.11, 91.92) | 0.65 * (0.45, 0.90) | 0.77 ns (0.54, 1.03) |
| 2 | 43.84 *** (25.28, 64.31) | 62.97 ** (42.42, 79.69) | 0.59 ** (0.38, 0.85) | 0.42 *** (0.26. 0.62) |
| 3 | 45.66 *** (22.41, 70.97) | 36.25 *** (19.77, 56.76) | 0.43 *** (0.23, 0.68) | 0.18 *** (0.08, 0.32) |
| 4 | 54.27 *** (28.97, 77.54) | 8.90 *** (4.06, 18.39) | 0.32 *** (0.15, 0.54) | 0.04 *** (0.00, 0.11) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hope, C.M.; Huynh, D.; Wong, Y.Y.; Oakey, H.; Perkins, G.B.; Nguyen, T.; Binkowski, S.; Bui, M.; Choo, A.Y.L.; Gibson, E.; et al. Optimization of Blood Handling and Peripheral Blood Mononuclear Cell Cryopreservation of Low Cell Number Samples. Int. J. Mol. Sci. 2021, 22, 9129. https://doi.org/10.3390/ijms22179129
Hope CM, Huynh D, Wong YY, Oakey H, Perkins GB, Nguyen T, Binkowski S, Bui M, Choo AYL, Gibson E, et al. Optimization of Blood Handling and Peripheral Blood Mononuclear Cell Cryopreservation of Low Cell Number Samples. International Journal of Molecular Sciences. 2021; 22(17):9129. https://doi.org/10.3390/ijms22179129
Chicago/Turabian StyleHope, Christopher M., Dao Huynh, Ying Ying Wong, Helena Oakey, Griffith Boord Perkins, Trung Nguyen, Sabrina Binkowski, Minh Bui, Ace Y. L. Choo, Emily Gibson, and et al. 2021. "Optimization of Blood Handling and Peripheral Blood Mononuclear Cell Cryopreservation of Low Cell Number Samples" International Journal of Molecular Sciences 22, no. 17: 9129. https://doi.org/10.3390/ijms22179129
APA StyleHope, C. M., Huynh, D., Wong, Y. Y., Oakey, H., Perkins, G. B., Nguyen, T., Binkowski, S., Bui, M., Choo, A. Y. L., Gibson, E., Huang, D., Kim, K. W., Ngui, K., Rawlinson, W. D., Sadlon, T., Couper, J. J., Penno, M. A. S., Barry, S. C., & on behalf of the ENDIA Study Group. (2021). Optimization of Blood Handling and Peripheral Blood Mononuclear Cell Cryopreservation of Low Cell Number Samples. International Journal of Molecular Sciences, 22(17), 9129. https://doi.org/10.3390/ijms22179129







