Current Concepts of Stem Cell Therapy for Chronic Spinal Cord Injury
Abstract
:1. Introduction
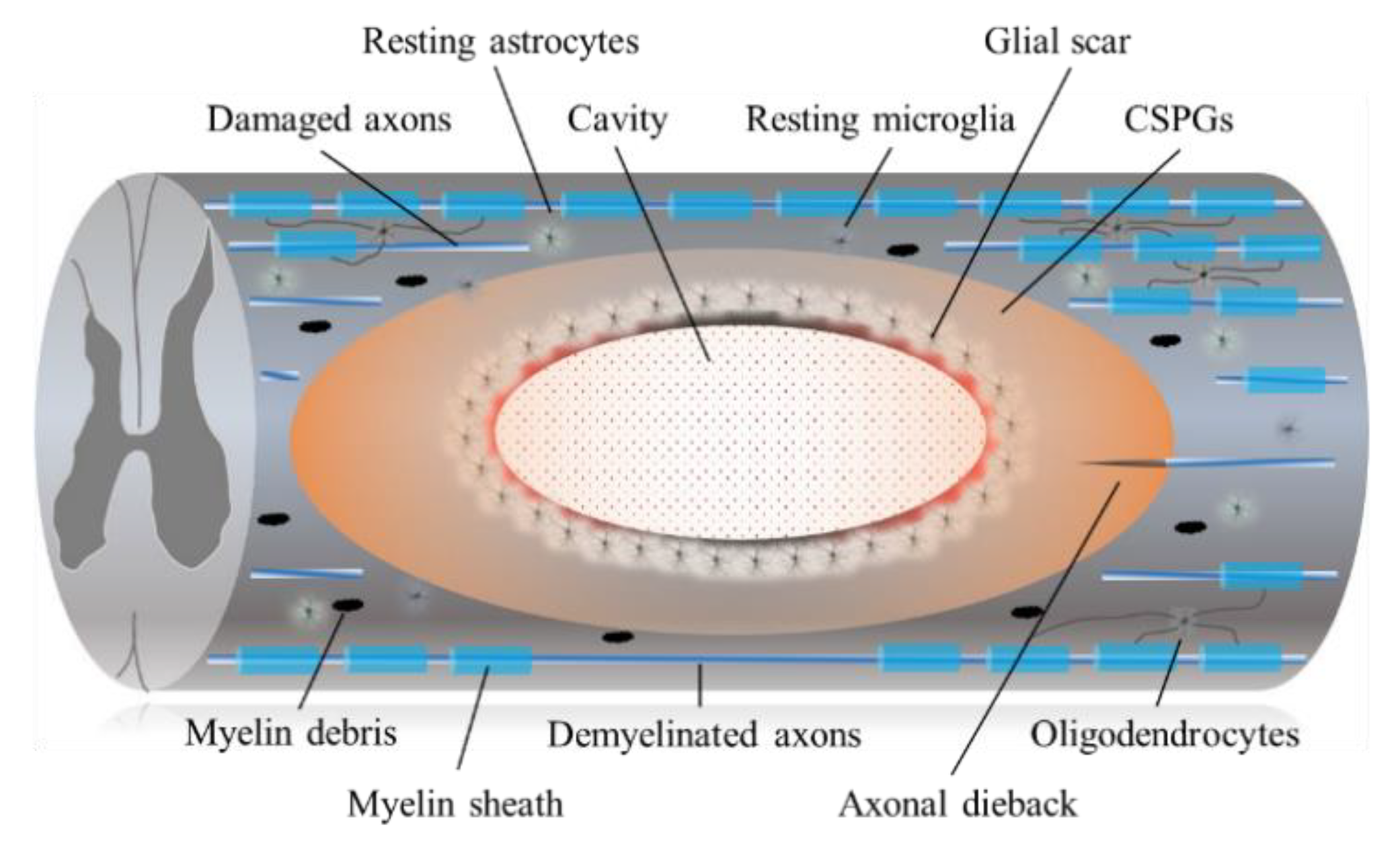
2. Barriers to Regeneration and Pathophysiology of Chronic SCI
2.1. Astrocytic and Fibrotic Scar
2.2. CSPGs and Chondroitinase ABC (ChABC)
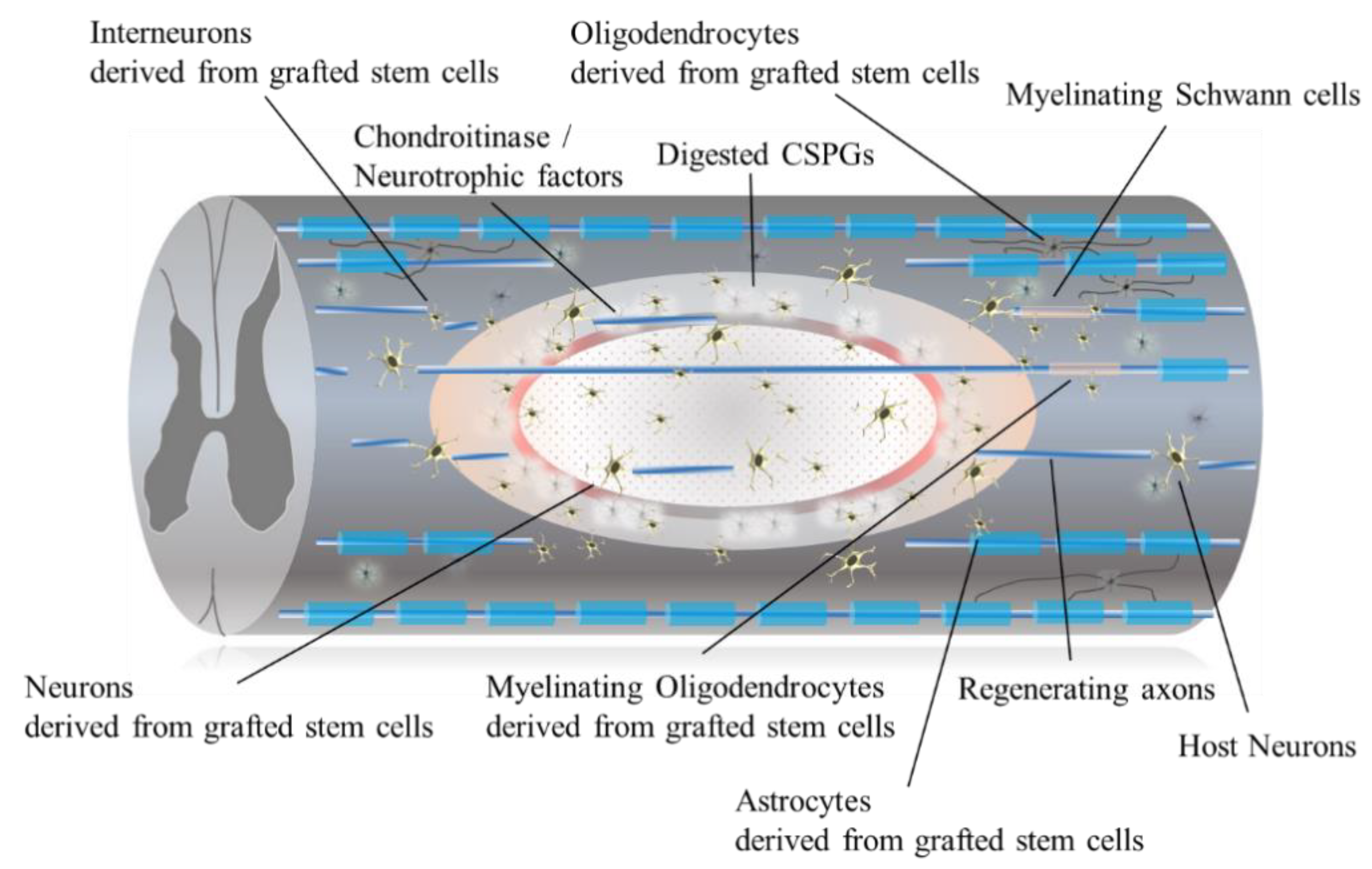
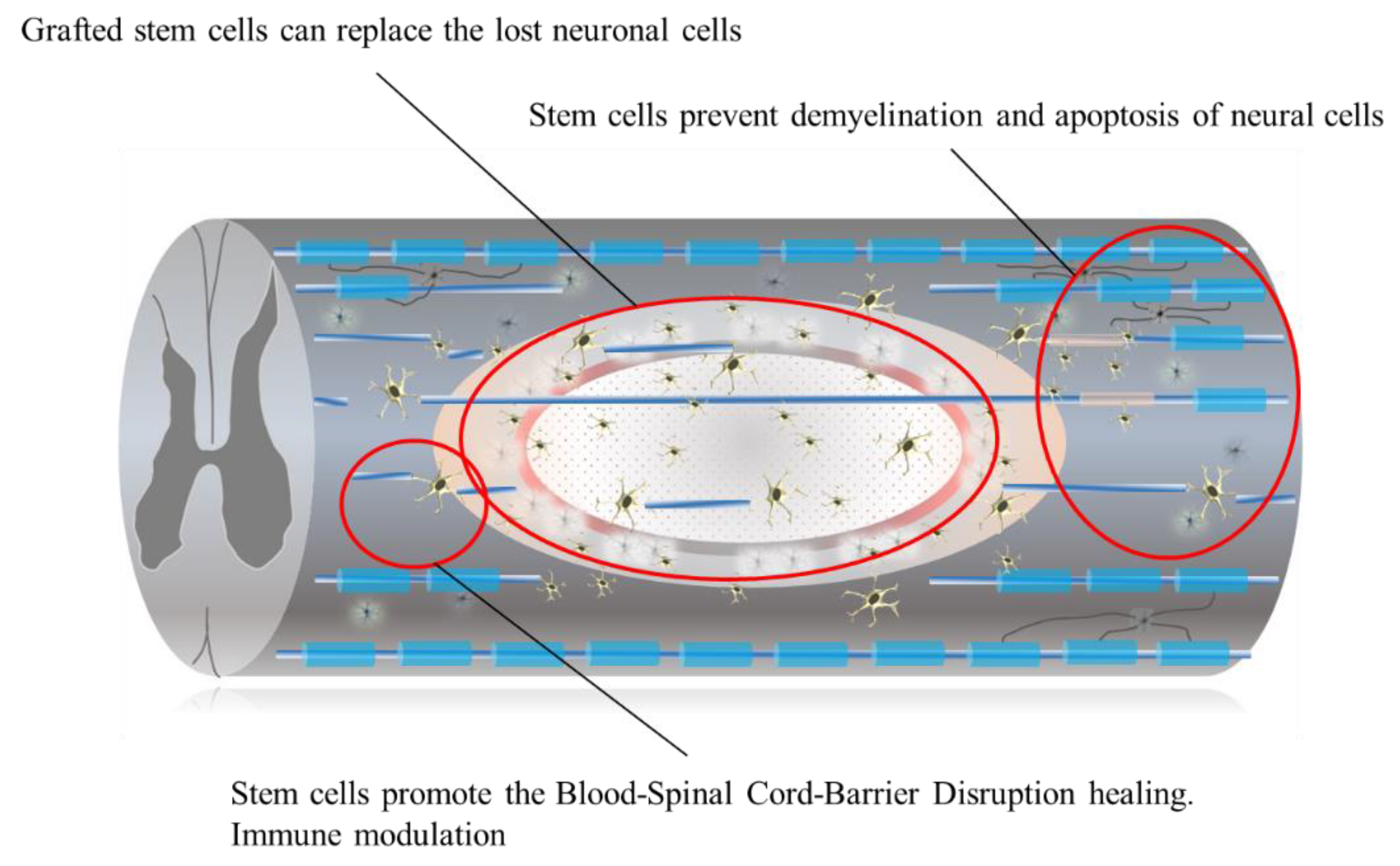
3. Cell-Based Therapies and Characteristics of Stem Cells
4. Ongoing Clinical Trials in Chronic SCI
4.1. Umbilical Cord Mesenchymal Stem Cells
4.2. Bone Marrow-Derived Mesenchymal Stem Cells
4.3. Human Mesenchymal and Hemopoietic Stem Cells: Neuro-Cells
4.4. Neural Stem/Progenitor Cells
4.5. Intravenous Transplantation of Multilineage-Differentiating Stress Enduring (Muse) Cells in Japan
5. Other Cells with Therapeutic Potential for Chronic SCI
5.1. Induced Pluripotent Stem Cells
5.2. Adipose Tissue-Derived Mesenchymal Stem Cells
5.3. Olfactory Ensheathing Cells
5.4. Schwann Cells
5.5. Biomaterial Scaffolds and Stem Cell Combinatory Treatment
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Fehlings, M.G.; Martin, A.R.; Tetreault, L.A.; Aarabi, B.; Anderson, P.; Arnold, P.M.; Brodke, D.S.; Burns, A.S.; Chiba, K.; Dettori, J.R.; et al. A clinical practice guideline for the management of patients with acute spinal cord injury: Recommendations on the role of baseline magnetic resonance imaging in clinical decision making and outcome prediction. Global Spine J. 2017, 7, 221s–230s. [Google Scholar] [CrossRef] [Green Version]
- Fehlings, M.G.; Kim, K.D.; Aarabi, B.; Rizzo, M.; Lisa, M.B.; McKerracher, L.; Vaccaro, A.R.; David, O.; Okonkwo, D.O. Rho inhibitor VX-210 in acute traumatic subaxial cervical spinal cord injury: Design of the SPinal Cord Injury Rho Inhibition InvestiGation (SPRING) clinical trial. J. Neurotrauma 2018, 35, 1049–1056. [Google Scholar] [CrossRef]
- Singh, A.; Tetreault, L.; Kalsi-Ryan, S.; Nouri, A.; Fehlings, M.G. Global prevalence and incidence of traumatic spinal cord injury. Clin. Epidemiol 2014, 6, 309–331. [Google Scholar] [CrossRef] [Green Version]
- Ahuja, C.; Fehlings, M.G. Concise review: Bridging the gap: Novel neuroregenerative and neuroprotective strategies in spinal cord injury. Stem Cells Transl. Med. 2016, 5, 914–924. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zweckberger, K.; Ahuja, C.S.; Liu, Y.; Wang, J.; Fehlings, M.G. Self-assembling peptides optimize the post-traumatic milieu and synergistically enhance the effects of neural stem cell therapy after cervical spinal cord injury. Acta. Biomater. 2016, 42, 77–89. [Google Scholar] [CrossRef] [PubMed]
- Kawabata, S.; Takano, M.; Numasawa-Kuroiwa, Y.; Itakura, G.; Kobayashi, Y.; Nishiyama, Y.; Sugai, K.; Nishimura, S.; Iwai, H.; Isoda, M.; et al. Grafted human iPS cell-derived oligodendrocyte precursor cells contribute to robust remyelination of demyelinated axons after spinal cord injury. Stem Cell Rep. 2016, 6, 1–8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lu, P.; Kadoya, K.; Tuszynski, M.H. Axonal growth and connectivity from neural stem cell grafts in models of spinal cord injury. Curr. Opin. Neurobiol. 2014, 27, 103–109. [Google Scholar] [CrossRef] [PubMed]
- Spinal cord injury (SCI) 2016 facts and figures at a glance. J. Spinal Cord Med. 2016, 9, 493–494. [CrossRef] [Green Version]
- Suzuki, H.; Ahuja, C.S.; Salewski, R.P.; Li, L.; Satkunendrarajah, K.; Nagoshi, N.; Shibata, S.; Fehlings, M.G. Neural stem cell mediated recovery is enhanced by Chondroitinase ABC pretreatment in chronic cervical spinal cord injury. PLoS ONE 2017, 12, e0182339. [Google Scholar] [CrossRef] [Green Version]
- Karimi-Abdolrezaee, S.; Eftekharpour, E.; Wang, J.; Morshead, C.M.; Fehlings, M.G. Delayed transplantation of adult neural precursor cells promotes remyelination and functional neurological recovery after spinal cord injury. J. Neurosci. 2006, 26, 3377–3389. [Google Scholar] [CrossRef]
- Salewski, R.P.; Mitchell, R.A.; Shen, C.; Fehlings, M.G. Transplantation of neural stem cells clonally derived from embryonic stem cells promotes recovery after murine spinal cord injury. Stem Cells Dev. 2015, 24, 36–50. [Google Scholar] [CrossRef] [Green Version]
- Wilcox, J.T.; Satkunendrarajah, K.; Zuccato, J.A.; Nassiri, F.; Fehlings, M.G. Neural precursor cell transplantation enhances functional recovery and reduces astrogliosis in bilateral compressive/contusive cervical spinal cord injury. Stem Cells Transl. Med. 2014, 3, 1148–1159. [Google Scholar] [CrossRef]
- Ramon y Cajal, S. Degeneration and Regeneration of the Nervous System; Oxford University Press: London, UK, 1928. [Google Scholar]
- Cafferty, W.B.; Duffy, P.; Huebner, E.; Strittmatter, S.M. MAG and OMgp synergize with Nogo-A to restrict axonal growth and neurological recovery after spinal cord trauma. J. Neurosci. 2010, 30, 1825–1837. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, M.S.; Huber, A.B.; van der Haar, M.E.; Frank, M.; Schnell, L.; Spillmann, A.A.; Christ, F.; Schwab, M.E. Nogo-A is a myelin-associated neurite outgrowth inhibitor and an antigen for monoclonal antibody IN-1. Nature 2000, 403, 434–439. [Google Scholar] [CrossRef]
- Forgione, N.; Fehlings, M.G. Rho-ROCK inhibition in the treatment of spinal cord injury. World Neurosurg. 2014, 82, e535–e539. [Google Scholar] [CrossRef] [PubMed]
- Moreau-Fauvarque, C.; Kumanogoh, A.; Camand, E.; Jaillard, C.; Barbin, G.; Boquet, I.; Love, C.; Jones, E.Y.; Kikutani, H.; Lubetzki, C.; et al. The transmembrane semaphoring Sema4D/CD100, an inhibitor of axonal growth, is expressed on oligodendrocytes and upregulated after CNS lesion. J. Neurosci. 2003, 23, 9229–9239. [Google Scholar] [CrossRef] [PubMed]
- Dubreuil, C.I.; Winton, M.J.; McKerracher, L. Rho activation patterns after spinal cord injury and the role of activated Rho in apoptosis in the central nervous system. J. Cell Biol. 2003, 162, 233–243. [Google Scholar] [CrossRef] [PubMed]
- Lord-Fontaine, S.; Yang, F.; Diep, Q.; Dergham, P.; Munzer, S.; Tremblay, P.; McKerracher, L. Local inhibition of Rho signaling by cell-permeable recombinant protein BA-210 prevents secondary damage and promotes functional recovery following acute spinal cord injury. J. Neurotrauma 2008, 25, 1309–1322. [Google Scholar] [CrossRef] [PubMed]
- Fehlings, M.G.; Theodore, N.; Harrop, J.; Maurais, G.; Kuntz, C.; Shaffrey, C.I.; Kwon, B.K.; Chapman, J.; Yee, A.; Tighe, A.; et al. A phase I/IIa clinical trial of a recombinant Rho protein antagonist in acute spinal cord injury. J. Neurotrauma 2011, 28, 787–796. [Google Scholar] [CrossRef] [PubMed]
- Alizadeh, A.; Dyck, S.M.; Karimi-Abdolrezaee, S. Myelin damage and repair in pathologic CNS: Challenges and prospects. Front. Mol. Neurosci. 2015, 8, 35. [Google Scholar] [CrossRef] [Green Version]
- Avram, S.; Shaposhnikov, S.; Buiu, C.; Mernea, M. Chondroitin sulfate proteoglycans: Structure-function relationship with implication in neural development and brain disorders. Biomed. Res. Int. 2014, 2014, 642798. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bradbury, E.J.; Moon, L.D.; Popat, R.J.; King, V.R.; Bennett, G.S.; Patel, P.N.; Fawcett, J.W.; McMahon, S.B. Chondroitinase ABC promotes functional recovery after spinal cord injury. Nature 2002, 416, 636–640. [Google Scholar] [CrossRef]
- Jones, L.L.; Sajed, D.; Tuszynski, M. Axonal regeneration through regions of chondroitin sulfate proteoglycan deposition after spinal cord injury: A balance of permissiveness and inhibition. J. Neurosci. 2003, 23, 9276–9288. [Google Scholar] [CrossRef] [PubMed]
- Ikegami, T.; Nakamura, M.; Yamane, J.; Katoh, H.; Okada, S.; Iwanami, A.; Watanabe, K.; Ishii, K.; Kato, F.; Fujita, H.; et al. Chondroitinase ABC combined with neural stem/progenitor cell transplantation enhances graft cell migration and outgrowth of growth-associated protein-43-positive fibers after rat spinal cord injury. Eur. J. Neurosci. 2005, 22, 3036–3046. [Google Scholar] [CrossRef] [PubMed]
- Carter, L.M.; Stephen, B.; McMahon, S.B.; Bradbury, E.J. Delayed treatment with chondroitinase ABC reverses chronic atrophy of rubrospinal neurons following spinal cord injury. Exp. Neurol. 2011, 228, 149–156. [Google Scholar] [CrossRef]
- Bartus, K.; James, N.D.; Didangelos, A.; Bosch, K.D.; Verhaagen, J.; Yáñez-Muñoz, R.J.; Rogers, J.H.; Schneider, B.J.; Muir, E.M.; Bradbury, E.J. Large-scale chondroitin sulfate proteoglycan digestion with chondroitinase gene therapy leads to reduced pathology and modulates macrophage phenotype following spinal cord contusion injury. J. Neurosci. 2014, 34, 4822–4836. [Google Scholar] [CrossRef]
- Baptiste, D.C.; Fehlings, M.G. Pharmacological approaches to repair the injured spinal cord. J. Neurotrauma 2006, 23, 318–334. [Google Scholar] [CrossRef]
- Katoh, H.; Yokota, K.; Fehlings, M.G. Regeneration of spinal cord connectivity through stem cell transplantation and biomaterial scaffolds. Front. Cell Neurosci. 2019, 13, 248. [Google Scholar] [CrossRef] [Green Version]
- Curtis, E.; Martin, J.R.; Gabel, B.; Sidhu, N.; Rzesiewicz, T.K.; Mandeville, R.; Van Gorp, S.; Leerink, M.; Tadokoro, T.; Marsala, S.; et al. A first-in-human, phase I study of neural stem cell transplantation for chronic spinal cord injury. Cell Stem Cell 2018, 22, 941–950. [Google Scholar] [CrossRef] [Green Version]
- Nagoshi, N.; Tsuji, O.; Nakamura, M.; Okano, H. Cell therapy for spinal cord injury using induced pluripotent stem cells. Regen. Ther. 2019, 11, 75–80. [Google Scholar] [CrossRef]
- Tsuji, O.; Sugai, K.; Yamaguchi, R.; Tashiro, S.; Nagoshi, N.; Kohyama, J.; Iida, T.; Ohkubo, T.; Itakura, G.; Isoda, M.; et al. Laying the groundwork for a first-in-human study of an induced pluripotent stem cell-based intervention for spinal cord injury. Stem Cells 2019, 37, 6–13. [Google Scholar] [CrossRef] [Green Version]
- Okubo, T.; Nagoshi, N.; Kohyama, J.; Tsuji, O.; Shinozaki, M.; Shibata, S.; Kase, Y.; Matsumoto, M.; Nakamura, M.; Okano, H. Treatment with a gamma-secretase inhibitor promotes functional recovery in human iPSC-derived transplants for chronic spinal cord injury. Stem Cell Rep. 2018, 11, 1416–1432. [Google Scholar] [CrossRef] [Green Version]
- Khazaei, M.; Siddiqui, A.M.; Fehlings, M.G. The potential for iPS-derived stem cells as a therapeutic strategy for spinal cord injury: Opportunities and challenges. J. Clin. Med. 2014, 4, 37–65. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Khazaei, M.; Ahuja, C.S.; Fehlings, M.G. Induced pluripotent stem cells for traumatic spinal cord injury. Front. Cell Dev. Biol. 2017, 4, 152. [Google Scholar] [CrossRef] [Green Version]
- Khazaei, M.; Ahuja, C.S.; Nakashima, H.; Nagoshi, N.; Li, L.; Wang, J.; Chio, J.; Badner, A.; Seligman, D.; Ichise, A.; et al. GDNF rescues the fate of neural progenitor grafts by attenuating Notch signals in the injured spinal cord in rodents. Sci. Transl. Med. 2020, 12, eaau3538. [Google Scholar] [CrossRef] [PubMed]
- Nori, S.; Khazaei, M.; Ahuja, C.S.; Yokota, K.; Ahlfors, J.E.; Liu, Y.; Wang, J.; Shibata, S.; Chio, J.; Hettiaratchi, M.H.; et al. Human oligodendrogenic neural progenitor cells delivered with chondroitinase ABC facilitate functional repair of chronic spinal cord injury. Stem Cell Rep. 2018, 11, 1433–1448. [Google Scholar] [CrossRef] [Green Version]
- Karimi-Abdolrezaee, S.; Schut, D.; Wang, J.; Fehlings, M.G. Chondroitinase and growth factors enhance activation and oligodendrocyte differentiation of endogenous neural precursor cells after spinal cord injury. PLoS ONE 2012, 7, e37589. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Badner, A.; Siddiqui, A.M.; Fehlings, M.G. Spinal cord injuries: How could cell therapy help? Expert. Opin. Biol. Ther. 2017, 17, 529–541. [Google Scholar] [CrossRef]
- Curt, A.; Hsieh, J.; Schubert, M.; Hupp, M.; Friedl, S.; Freund, P.; Huber, E.; Pfyffer, D.; Sutter, R.; Jutzeler, C.; et al. The damaged spinal cord is a suitable target for stem cell transplantation. Neurorehabil. Neural Repair 2020, 34, 758–768. [Google Scholar] [CrossRef]
- Iwanami, A.; Kaneko, S.; Nakamura, M.; Kanemura, Y.; Mori, H.; Kobayashi, S.; Yamasaki, M.; Momoshima, S.; Ishii, H.; Ando, K.; et al. Transplantation of human neural stem cells for spinal cord injury in primates. J. Neurosci. Res. 2005, 80, 182–190. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Iwasaki, M.; Wilcox, J.T.; Nishimura, Y.; Zweckberger, K.; Suzuki, H.; Wang, J.; Liu, Y.; Karadimas, S.K.; Fehlings, M.G. Synergistic effects of self-assembling peptide and neural stem/progenitor cells to promote tissue repair and forelimb functional recovery in cervical spinal cord injury. Biomaterials 2014, 35, 2617–2629. [Google Scholar] [CrossRef] [PubMed]
- Kadoya, K.; Lu, P.; Nguyen, K.; Lee-Kubli, C.; Kumamaru, H.; Yao, L.; Knackert, J.; Poplawski, G.; Dulin, J.N.; Strobl, H.; et al. Spinal cord reconstitution with homologous neural grafts enables robust corticospinal regeneration. Nat. Med. 2016, 22, 479–487. [Google Scholar] [CrossRef] [Green Version]
- Takahashi, K.; Tanabe, K.; Ohnuki, M.; Narita, M.; Ichisaka, T.; Tomoda, K.; Yamanaka, S. Induction of pluripotent stem cells from adult human fibroblasts by defined factors. Cell 2007, 131, 861–872. [Google Scholar] [CrossRef] [Green Version]
- Takahashi, K.; Yamanaka, S. Induction of pluripotent stem cells from mouse embryonic and adult fibroblast cultures by defined factors. Cell 2006, 126, 663–676. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Okano, H.; Yamanaka, S. iPS cell technologies: Significance and applications to CNS regeneration and disease. Mol. Brain 2014, 7, 22. [Google Scholar] [CrossRef] [Green Version]
- Gore, A.; Li, Z.; Fung, H.L.; Young, J.E.; Agarwal, S.; Antosiewicz-Bourget, J.; Canto, I.; Giorgetti, A.; Israel, M.A.; Kiskinis, E.; et al. Somatic coding mutations in human induced pluripotent stem cells. Nature 2011, 471, 63–67. [Google Scholar] [CrossRef]
- Zhou, T.; Benda, C.; Dunzinger, S.; Huang, Y.; Ho, J.C.; Yang, J.; Wang, Y.; Zhang, Y.; Zhuang, Q.; Li, Y.; et al. Generation of human induced pluripotent stem cells from urine samples. Nat. Protoc. 2012, 7, 2080–2089. [Google Scholar] [CrossRef]
- Ruzicka, J.; Romanyuk, N.; Jirakova, K.; Hejcl, A.; Janouskova, O.; Machova, L.U.; Bochin, M.; Pradny, M.; Vargova, L.; Jendelova, P. The effect of iPS-derived neural Progenitors seeded on laminin-coated pHEMA-MOETACl hydrogel with dual porosity in a rat model of chronic spinal cord injury. Cell Transplant. 2019, 28, 400–412. [Google Scholar] [CrossRef] [Green Version]
- Iida, T.; Iwanami, A.; Sanosaka, T.; Kohyama, J.; Miyoshi, H.; Nagoshi, N.; Kashiwagi, R.; Toyama, Y.; Matsumoto, M.; Nakamura, M.; et al. Whole-genome DNA methylation analyses revealed epigenetic instability in tumorigenic human iPS cell-derived neural stem/progenitor cells. Stem Cells 2017, 35, 1316–1327. [Google Scholar] [CrossRef] [Green Version]
- Ogura, A.; Morizane, A.; Nakajima, Y.; Miyamoto, S.; Takahashi, J. Gamma-secretase inhibitors prevent overgrowth of transplanted neural progenitors derived from human-induced pluripotent stem cells. Stem Cells Dev. 2013, 22, 374–382. [Google Scholar] [CrossRef] [PubMed]
- Itakura, G.; Kobayashi, Y.; Nishimura, S.; Iwai, H.; Takano, M.; Iwanami, A.; Toyama, Y.; Okano, H.; Nakamura, M. Controlling immune rejection is a fail-safe system against potential tumorigenicity after human iPSC-derived neural stem cell transplantation. PLoS ONE 2015, 10, e0116413. [Google Scholar] [CrossRef]
- Itakura, G.; Kawabata, S.; Ando, M.; Nishiyama, Y.; Sugai, K.; Ozaki, M.; Iida, T.; Ookubo, T.; Kojima, K.; Kashiwagi, R.; et al. Fail-safe system against potential tumorigenicity after transplantation of iPSC derivatives. Stem Cell Rep. 2017, 8, 673–684. [Google Scholar] [CrossRef] [PubMed]
- Owen, M.; Friedenstein, A.J. Stromal stem cells: Marrow-derived osteogenic precursors. Ciba Found Symp. 1988, 136, 42–60. [Google Scholar] [CrossRef] [PubMed]
- Yagura, K.; Ohtaki, H.; Tsumuraya, T.; Sato, A.; Miyamoto, K.; Kawada, N.; Suzuki, K.; Nakamura, M.; Kanzaki, K.; Dohi, K.; et al. The enhancement of CCL2 and CCL5 by human bone marrow-derived mesenchymal stem/stromal cells might contribute to inflammatory suppression and axonal extension after spinal cord injury. PLoS ONE 2020, 15, e0230080. [Google Scholar] [CrossRef] [PubMed]
- Wright, K.T.; El Masri, W.; Osman, A.; Roberts, S.; Chamberlain, G.; Ashton, B.A.; Johnson, W.E. Bone marrow stromal cells stimulate neurite outgrowth over neural proteoglycans (CSPG), myelin associated glycoprotein and Nogo-A. Biochem. Biophys. Res. Commun. 2007, 354, 559–566. [Google Scholar] [CrossRef] [PubMed]
- Wright, K.T.; Uchida, K.; Bara, J.J.; Roberts, S.; El Masri, W.; Johnson, W.E. Spinal motor neurite outgrowth over glial scar inhibitors is enhanced by coculture with bone marrow stromal cells. Spine J. 2014, 14, 1722–1733. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Neuhuber, B.; Himes, B.T.; Shumsky, J.S.; Gallo, G.; Fischer, I. Axon growth and recovery of function supported by human bone marrow stromal cells in the injured spinal cord exhibit donor variation. Brain. Res. 2005, 1035, 73–85. [Google Scholar] [CrossRef]
- Honmou, O.; Yamashita, T.; Morita, T.; Oshigiri, T.; Hirota, R.; Iyama, S.; Kato, J.; Sasaki, Y.; Ishiai, S.; Ito, Y.M.; et al. Intravenous infusion of auto serum-expanded autologous mesenchymal stem cells in spinal cord injury patients: 13 case series. Clin. Neurol. Neurosurg. 2021, 203, 106565. [Google Scholar] [CrossRef] [PubMed]
- Japan should put the brakes on stem-cell sales. Nature 2019, 565, 535–536. [CrossRef]
- Albu, S.; Kumru, H.; Coll, R.; Vives, J.; Vallés, M.; Benito-Penalva, J.; Rodríguez, L.; Codinach, M.; Hernández, J.; Navarro, X.; et al. Clinical effects of intrathecal administration of expanded Wharton jelly mesenchymal stromal cells in patients with chronic complete spinal cord injury: A randomized controlled study. Cytotherapy 2021, 23, 146–156. [Google Scholar] [CrossRef]
- Reyhani, S.; Abbaspanah, B.; Mousavi, S.H. Umbilical cord-derived mesenchymal stem cells in neurodegenerative disorders: From literature to clinical practice. Regen. Med. 2020, 15, 1561–1578. [Google Scholar] [CrossRef] [PubMed]
- Lim, W.L.; Liau, L.L.; Ng, M.H.; Shiplu, R.C.; Law, J.X. Current progress in tendon and ligament tissue engineering. Tissue Eng. Regen. Med. 2019, 16, 549–571. [Google Scholar] [CrossRef]
- Rehman, J.; Traktuev, D.; Li, J.; Merfeld-Clauss, S.; Temm-Grove, C.J.; Bovenkerk, J.E.; Pell, C.L.; Johnstone, B.H.; Considine, R.V.; March, K.L. Secretion of angiogenic and antiapoptotic factors by human adipose stromal cells. Circulation 2004, 109, 1292–1298. [Google Scholar] [CrossRef] [PubMed]
- Uccelli, A.; Moretta, L.; Pistoia, V. Mesenchymal stem cells in health and disease. Nat. Rev. Immunol. 2008, 8, 726. [Google Scholar] [CrossRef] [PubMed]
- Sorrell, J.M.; Baber, M.A.; Caplan, A.I. Influence of adult mesenchymal stem cells on in vitro vascular formation. Tissue. Eng. Part A 2009, 15, 1751–1761. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hofer, H.R.; Tuan, R.S. Secreted trophic factors of mesenchymal stem cells support neurovascular and musculoskeletal therapies. Stem Cell Res. Ther. 2016, 7, 131. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Weiss, M.L.; Anderson, C.; Medicetty, S.; Seshareddy, K.; Weiss, R.J.; VanderWerff, I.; Troyer, D.; McIntosh, K.R. Immune properties of human umbilical cord Wharton’s jelly-derived cells. Stem Cells 2008, 26, 2865–2874. [Google Scholar] [CrossRef] [PubMed]
- Avanzini, M.; Bernardo, M.E.; Cometa, A.M.; Perotti, C.; Zaffaroni, N.; Novara, F.; Visai, L.; Antonia Moretta, A.; Fante, C.D.; Villa, R.; et al. Generation of mesenchymal stromal cells in the presence of platelet lysate: A phenotypic and functional comparison of umbilical cord blood-and bone marrow-derived progenitors. Haematologica 2009, 94, 1649–1660. [Google Scholar] [CrossRef] [PubMed]
- Lim, J.; Razi, Z.R.M.; Law, J.X.; Nawi, A.M.; Idrus, R.B.H.; Chin, T.G.; Mustangin, M.; Ng, M.H. Mesenchymal stromal cells from the maternal segment of human umbilical cord is ideal for bone regeneration in allogenic setting. Tissue. Eng. Regen. Med. 2018, 15, 75–87. [Google Scholar] [CrossRef] [PubMed]
- Kemp, K.; Mallam, E.; Hares, K.; Witherick, J.; Scolding, N.; Wilkins, A. Mesenchymal stem cells restore frataxin expression and increase hydrogen peroxide scavenging enzymes in Friedreich ataxia fibroblasts. PLoS ONE 2011, 6, e26098. [Google Scholar] [CrossRef] [PubMed]
- Da Costa Gonçalves, F.; Grings, M.; Nunes, N.S.; Pinto, F.O.; Garcez, T.N.A.; Visioli, F.; Leipnitz, G.; Paz, A.H. Antioxidant properties of mesenchymal stem cells against oxidative stress in a murine model of colitis. Biotechnol. Lett. 2017, 39, 613–622. [Google Scholar] [CrossRef] [PubMed]
- Hafez, P.; Chowdhury, S.R.; Jose, S.; Law, J.X.; Ruszymah, B.H.I.; Ramzisham, A.R.M.; Ng, M.H. Development of an in vitro cardiac ischemic model using primary human cardiomyocytes. Cardiovasc. Eng. Technol. 2018, 9, 529–538. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.; Tang, F.; Xiao, Z.; Han, G.; Wang, N.; Yin, N.; Chen, B.; Jiang, X.; Yun, C.; Han, W.; et al. Clinical study of NeuroRegen scaffold combined with human mesenchymal stem cells for the repair of chronic complete spinal cord injury. Cell Transplant. 2017, 26, 891–900. [Google Scholar] [CrossRef] [PubMed]
- Przekora, A.; Juszkiewicz, L. The effect of autologous adipose tissue-derived mesenchymal stem cells’ therapy in the treatment of chronic posttraumatic spinal cord injury in a domestic ferret patient. Cell Transplant. 2020, 29, 963689720928982. [Google Scholar] [CrossRef]
- Escalhão, C.C.M.; Ramos, I.P.; Hochman-Mendez, C.; Brunswick, T.H.K.; Souza, S.A.L.; Gutfilen, B.; Dos Santos Goldenberg, R.C.; Coelho-Sampaio, T. Safety of allogeneic canine adipose tissue-derived mesenchymal stem cell intraspinal transplantation in dogs with chronic spinal cord injury. Stem Cells Int. 2017, 2017, 3053759. [Google Scholar] [CrossRef] [PubMed]
- Lattanzi, W.; Geloso, M.C.; Saulnier, N.; Giannetti, S.; Puglisi, M.A.; Corvino, V.; Gasbarrini, A.; Michetti, F. Neurotrophic features of human adipose tissue-derived stromal cells: In vitro and in vivo studies. J. Biomed. Biotechnol. 2011, 2011, 468705. [Google Scholar] [CrossRef] [Green Version]
- Wei, X.; Du, Z.; Zhao, L.; Feng, D.; Wei, G.; He, Y.; Tan, J.; Lee, W.H.; Hampel, H.; Dodel, R.; et al. IFATS collection: The conditioned media of adipose stromal cells protect against hypoxia-ischemia-induced brain damage in neonatal rats. Stem Cells 2009, 27, 478–488. [Google Scholar] [CrossRef]
- Zhou, Z.; Chen, Y.; Zhang, H.; Min, S.; Yu, B.; He, B.; Jin, A. Comparison of mesenchymal stromal cells from human bone marrow and adipose tissue for the treatment of spinal cord injury. Cytotherapy 2013, 15, 434–448. [Google Scholar] [CrossRef]
- Menezes, K.; Nascimento, M.A.; Gonçalves, J.P.; Cruz, A.S.; Lopes, D.V.; Curzio, B.; Bonamino, M.; de Menezes, J.R.; Borojevic, R.; Rossi, M.I.; et al. Human mesenchymal cells from adipose tissue deposit laminin and promote regeneration of injured spinal cord in rats. PLoS ONE 2014, 9, e96020. [Google Scholar] [CrossRef]
- Bydon, M.; Dietz, A.B.; Goncalves, S.; Moinuddin, F.M.; Alvi, M.A.; Goyal, A.; Yolcu, Y.; Hunt, C.L.; Garlanger, K.L.; Del Fabro, A.S.; et al. CELLTOP Clinical Trial: First report from a phase 1 trial of autologous adipose tissue-derived mesenchymal stem cells in the treatment of paralysis due to traumatic spinal cord injury. Mayo Clin. Proc. 2020, 95, 406–414. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Saberi, H.; Moshayedi, P.; Aghayan, H.R.; Arjmand, B.; Hosseini, S.K.; Emami-Razavi, S.H.; Rahimi-Movaghar, V.; Raza, M.; Firouzi, M.S. Treatment of chronic thoracic spinal cord injury patients with autologous Schwann cell transplantation: An interim report on safety considerations and possible outcomes. Neurosci. Lett. 2008, 443, 46–50. [Google Scholar] [CrossRef] [PubMed]
- Assinck, P.; Sparling, J.S.; Dworski, S.; Duncan, G.J.; Wu, D.L.; Liu, J.; Kwon, B.K.; Biernaskie, J.; Miller, F.D.; Tetzlaff, W. Transplantation of skin precursor-derived Schwann cells yields better locomotor outcomes and reduces bladder pathology in rats with chronic spinal cord injury. Stem Cell Rep. 2020, 15, 140–155. [Google Scholar] [CrossRef] [PubMed]
- Boerboom, A.; Dion, V.; Chariot, A.; Franzen, R. Molecular mechanisms involved in Schwann cell plasticity. Front. Mol. Neurosci. 2017, 10, 38. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yazdani, S.O.; Hafizi, M.; Zali, A.R.; Atashi, A.; Ashrafi, F.; Seddighi, A.S.; Soleimani, M. Safety and possible outcome assessment of autologous Schwann cell and bone marrow mesenchymal stromal cell co-transplantation for treatment of patients with chronic spinal cord injury. Cytotherapy 2013, 15, 782–791. [Google Scholar] [CrossRef] [PubMed]
- Oraee-Yazdani, S.; Hafizi, M.; Atashi, A.; Ashrafi, F.; Seddighi, A.S.; Hashemi, S.M.; Seddighi, A.; Soleimani, M.; Zali, A.b. Co-transplantation of autologous bone marrow mesenchymal stem cells and Schwann cells through cerebral spinal fluid for the treatment of patients with chronic spinal cord injury: Safety and possible outcome. Spinal Cord 2016, 54, 102–109. [Google Scholar] [CrossRef]
- Cheng, H.; Liu, X.; Hua, R.; Dai, G.; Wang, X.; Gao, J.; An, Y. Clinical observation of umbilical cord mesenchymal stem cell transplantation in treatment for sequelae of thoracolumbar spinal cord injury. J. Transl. Med. 2014, 12, 253. [Google Scholar] [CrossRef] [Green Version]
- Vaquero, J.; Zurita, M.; Rico, M.A.; Aguayo, C.; Bonilla, C.; Marin, E.; Tapiador, N.; Sevilla, M.; Vazquez, D.; Carballido, J.; et al. Intrathecal administration of autologous mesenchymal stromal cells for spinal cord injury: Safety and efficacy of the 100/3 guideline. Cytotherapy 2018, 20, 806–819. [Google Scholar] [CrossRef] [PubMed]
- Chen, W.; Zhang, Y.; Yang, S.; Sun, J.; Qiu, H.; Hu, X.; Niu, X.; Xiao, Z.; Zhao, Y.; Zhou, Y.; et al. NeuroRegen scaffolds combined with autologous bone marrow mononuclear cells for the repair of acute complete spinal cord injury: A 3-year clinical study. Cell Transplant. 2020, 29, 963689720950637. [Google Scholar] [CrossRef]
- De Munter, J.P.J.M.; Shafarevich, I.; Liundup, A.; Pavlov, D.; Wolters, E.C.; Gorlova, A.; Veniaminova, E.; Umriukhin, A.; Kalueff, A.; Svistunov, A.; et al. Neuro-Cells therapy improves motor outcomes and suppresses inflammation during experimental syndrome of amyotrophic lateral sclerosis in mice. CNS Neurosci. Ther. 2020, 26, 504–517. [Google Scholar] [CrossRef]
- Sigurjonsson, O.E.; Perreault, M.C.; Egeland, T.; Glover, J.C. Adult human hematopoietic stem cells produce neurons efficiently in the regenerating chicken embryo spinal cord. Proc. Natl. Acad. Sci. USA 2005, 102, 5227–5232. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hofstetter, C.P.; Schwarz, E.J.; Hess, D.; Widenfalk, J.; El Manira, A.; Prockop, D.J.; Olson, L. Marrow stromal cells form guiding strands in the injured spinal cord and promote recovery. Proc. Natl. Acad. Sci. USA 2002, 99, 2199–2204. [Google Scholar] [CrossRef] [Green Version]
- Manley, N.C.; Priest, C.A.; Denham, J.; Wirth, E.D., 3rd; Lebkowski, J.S. Human embryonic stem cell-derived oligodendrocyte progenitor cells: Preclinical efficacy and safety in cervical spinal cord injury. Stem Cells Transl. Med. 2017, 6, 1917–1929. [Google Scholar] [CrossRef]
- Farzaneh, M.; Anbiyaiee, A.; Khoshnam, S.E. Human pluripotent stem cells for spinal cord injury. Curr. Stem Cell Res. Ther. 2020, 15, 135–143. [Google Scholar] [CrossRef] [PubMed]
- Sadat-Ali, M.; Al-Dakheel, D.A.; Ahmed, A.; Al-Turki, H.A.; Al-Omran, A.S.; Acharya, S.; Al-Bayat, M.I. Spinal cord injury regeneration using autologous bone marrow-derived neurocytes and rat embryonic stem cells: A comparative study in rats. World J. Stem Cells 2020, 12, 1591–1602. [Google Scholar] [CrossRef] [PubMed]
- Schroeder, J.; Kueper, J.; Leon, K.; Liebergall, M. Stem cells for spine surgery. World J. Stem Cells 2015, 7, 186–194. [Google Scholar] [CrossRef] [PubMed]
- Kanno, H. Regenerative therapy for neuronal diseases with transplantation of somatic stem cells. World J. Stem Cells 2013, 5, 163–171. [Google Scholar] [CrossRef] [PubMed]
- Walker, P.A.; Letourneau, P.A.; Bedi, S.; Shah, S.K.; Jimenez, F.; Cox, C.S., Jr. Progenitor cells as remote "bioreactors": Neuroprotection via modulation of the systemic inflammatory response. World J. Stem Cells 2011, 3, 9–18. [Google Scholar] [CrossRef] [PubMed]
- Assinck, P.; Duncan, G.J.; Hilton, B.J.; Plemel, J.R.; Tetzlaff, W. Cell transplantation therapy for spinal cord injury. Nat. Neurosci. 2017, 20, 637. [Google Scholar] [CrossRef]
- Ashammakhi, N.; Kim, H.J.; Ehsanipour, A.; Bierman, R.D.; Kaarela, O.; Xue, C.; Khademhosseini, A.; Seidlits, S.K. Regenerative Therapies for Spinal Cord Injury. Tissue Eng. Part B Rev. 2019, 25, 471–491. [Google Scholar] [CrossRef] [PubMed]
- StemCells Inc. Pathway Study; StemCells Inc.: Newark, CA, USA, 2015. [Google Scholar]
- StemCells Inc. Phase II Trial in Cervical Spinal Cord Injury (SCI); StemCells Inc.: Newark, CA, USA, 2015. [Google Scholar]
- Anderson, A.J.; Piltti, K.M.; Hooshmand, M.J.; Nishi, R.A.; Cummings, B.J. Preclinical efficacy failure of human CNS-derived stem cells for use in the Pathway Study of Cervical Spinal Cord Injury. Stem Cell Rep. 2017, 8, 249–263. [Google Scholar] [CrossRef] [PubMed]
- Dezawa, M.; Kanno, H.; Hoshino, M.; Cho, H.; Matsumoto, N.; Itokazu, Y.; Tajima, N.; Yamada, H.; Sawada, H.; Ishikawa, H.; et al. Specific induction of neuronal cells from bone marrow stromal cells and application for autologous transplantation. J. Clin. Investig. 2004, 113, 1701–1710. [Google Scholar] [CrossRef] [Green Version]
- Dezawa, M. The Muse cell discovery, thanks to wine and science. Adv. Exp. Med. Biol. 2018, 1103, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Kajitani, T.; Endo, T.; Iwabuchi, N.; Inoue, T.; Takahashi, Y.; Abe, T.; Niizuma, K.; Tominaga, T. Association of intravenous administration of human Muse cells with deficit amelioration in a rat model of spinal cord injury. J. Neurosurg. Spine 2021, 1–8. [Google Scholar] [CrossRef]
- Dezawa, M. Clinical trials of Muse cells. Adv. Exp. Med. Biol. 2018, 1103, 305–307. [Google Scholar] [CrossRef]
- Rao, Y.; Zhu, W.; Guo, Y.; Jia, C.; Qi, R.; Qiao, R.; Cao, D.; Zhang, H.; Cui, Z.; Yang, L.; et al. Long-term outcome of olfactory ensheathing cell transplantation in six patients with chronic complete spinal cord injury. Cell Transplant. 2013, 22, S21–S25. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Adnan, H.; Xu, B.; Wang, J.; Wang, C.; Li, F.; Tang, K. Effects of transplantation of olfactory ensheathing cells in chronic spinal cord injury: A systematic review and meta-analysis. Eur. Spine J. 2015, 24, 919–930. [Google Scholar] [CrossRef]
- Wu, J.; Sun, T.; Ye, C.; Yao, J.; Zhu, B.; He, H. Clinical observation of fetal olfactory ensheathing glia transplantation (OEGT) in patients with complete chronic spinal cord injury. Cell Transplant. 2012, 21, S33–S37. [Google Scholar] [CrossRef] [Green Version]
- Lima, C.; Escada, P.; Pratas-Vital, J.; Branco, C.; Arcangeli, C.A.; Lazzeri, G.; Maia, C.A.; Capucho, C.; Hasse-Ferreira, A.; Peduzzi, J.D. Olfactory mucosal autografts and rehabilitation for chronic traumatic spinal cord injury. Neurorehabil. Neural Repair 2010, 24, 10–22. [Google Scholar] [CrossRef]
- Iwatsuki, K.; Tajima, F.; Ohnishi, Y.; Nakamura, T.; Ishihara, M.; Hosomi, K.; Ninomiya, K.; Moriwaki, T.; Yoshimine, T. A pilot clinical study of olfactory mucosa autograft for chronic complete spinal cord injury. Neurol. Med. Chir. 2016, 56, 285–292. [Google Scholar] [CrossRef] [Green Version]
- Wang, S.; Lu, J.; Li, Y.A.; Zhou, H.; Ni, W.F.; Zhang, X.L.; Zhu, S.P.; Chen, B.B.; Xu, H.; Wang, X.Y.; et al. Autologous olfactory lamina propria transplantation for chronic spinal cord injury: Three-year follow-up outcomes from a prospective double-blinded clinical trial. Cell Transplant. 2016, 25, 141–157. [Google Scholar] [CrossRef]
- Wang, N.; Xiao, Z.; Zhao, Y.; Wang, B.; Li, X.; Li, J.; Dai, J. Collagen scaffold combined with human umbilical cord-derived mesenchymal stem cells promote functional recovery after scar resection in rats with chronic spinal cord injury. J. Tissue Eng. Regen. Med. 2018, 12, e1154–e1163. [Google Scholar] [CrossRef] [PubMed]
- Amr, S.M.; Gouda, A.; Koptan, W.T.; Galal, A.A.; Abdel-Fattah, D.S.; Rashed, L.A.; Atta, H.M.; Abdel-Aziz, M.T. Bridging defects in chronic spinal cord injury using peripheral nerve grafts combined with a chitosan-laminin scaffold and enhancing regeneration through them by co-transplantation with bone-marrow-derived mesenchymal stem cells: Case series of 14 patients. J. Spinal Cord Med. 2014, 37, 54–71. [Google Scholar] [CrossRef] [Green Version]
- Martínez-Ramos, C.; Doblado, L.R.; Mocholi, E.L.; Alastrue-Agudo, A.; Petidier, M.S.; Giraldo, E.; Pradas, M.M.; Moreno-Manzano, V. Biohybrids for spinal cord injury repair. J. Tissue Eng. Regen. Med. 2019, 13, 509–521. [Google Scholar] [CrossRef]
- Peng, Z.; Gao, W.; Yue, B.; Jiang, J.; Gu, Y.; Dai, J.; Chen, L.; Shi, Q. Promotion of neurological recovery in rat spinal cord injury by mesenchymal stem cells loaded on nerve-guided collagen scaffold through increasing alternatively activated macrophage polarization. J. Tissue Eng. Regen. Med. 2018, 12, e1725–e1736. [Google Scholar] [CrossRef]
- Li, X.; Tan, J.; Xiao, Z.; Zhao, Y.; Han, S.; Liu, D.; Yin, W.; Li, J.; Li, J.; Wanggou, S.; et al. Transplantation of hUC-MSCs seeded collagen scaffolds reduces scar formation and promotes functional recovery in canines with chronic spinal cord injury. Sci. Rep. 2017, 7, 43559. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tian, L.; Prabhakaran, M.P.; Ramakrishna, S. Strategies for regeneration of components of nervous system: Scaffolds, cells and biomolecules. Regen. Biomater. 2015, 2, 31–45. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Raspa, A.; Marchini, A.; Pugliese, R.; Mauri, M.; Maleki, M.; Vasita, R.; Gelain, F. A biocompatibility study of new nanofibrous scaffolds for nervous system regeneration. Nanoscale 2016, 8, 253–265. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Liu, D.; Xiao, Z.; Zhao, Y.; Han, S.; Chen, B.; Dai, J. Scaffold-facilitated locomotor improvement post complete spinal cord injury: Motor axon regeneration versus endogenous neuronal relay formation. Biomaterials 2019, 197, 20–31. [Google Scholar] [CrossRef]
- Liu, W.; Xu, B.; Xue, W.; Yang, B.; Fan, Y.; Chen, B.; Xiao, Z.; Xue, X.; Sun, Z.; Shu, M.; et al. A functional scaffold to promote the migration and neuronal differentiation of neural stem/progenitor cells for spinal cord injury repair. Biomaterials 2020, 243, 119941. [Google Scholar] [CrossRef]
- Yang, L.; Chueng, S.D.; Li, Y.; Patel, M.; Rathnam, C.; Dey, G.; Wang, L.; Cai, L.; Lee, K.B. A biodegradable hybrid inorganic nanoscaffold for advanced stem cell therapy. Nat. Commun. 2018, 9, 3147. [Google Scholar] [CrossRef] [Green Version]
| Identifier | Study Title | Phase | Subjects (Participants) | Cell Therapy | Route of Administration | Combination |
|---|---|---|---|---|---|---|
| NCT03979742 | Umbilical Cord Blood Cell Transplant Into Injured Spinal Cord With Lithium Carbonate or Placebo Followed by Locomotor Training | Phase 2 | 27 | UC Blood Mononuclear Stem Cells | Transplant into injured spinal cord | Oral lithium carbonate Locomotor Training |
| NCT03521323 | Intrathecal Transplantation of UC-MSC in Patients With Early Stage of Chronic Spinal Cord Injury | Phase 2 | 66 | Umbilical Cord Mesenchymal Stem Cells | Intrathecal | |
| NCT03505034 | Intrathecal Transplantation of UC-MSC in Patients With Late Stage of Chronic Spinal Cord Injury | Phase 2 | 43 | Umbilical Cord Mesenchymal Stem Cells | Intrathecal | |
| NCT04213131 | Efficacy and Safety of hUC-MSCs and hUCB-MSCs in the Treatment of Chronic Spinal Cord Injury | Not Applicable | 42 | hUC-MSCs and hUCB-MSCs | Transplant into injured spinal cord | |
| NCT04205019 | Safety Stem Cells in Spinal Cord Injury | Phase 1 | 10 | Neuro-Cells (Autologous Fresh Stem Cells Containing Product) | Intrathecal | |
| NCT01676441 | Safety and Efficacy of Autologous Mesenchymal Stem Cells in Chronic Spinal Cord Injury | Phase 2 Phase 3 | 20 | Autologous Mesenchymal Stem Cells | Injection into the intramedullary and intrathecal space | |
| NCT01393977 | Difference Between Rehabilitation Therapy and Stem Cells Transplantation in Patients With Spinal Cord Injury in China | Phase 2 | 60 | Autologous BMSCs | Intrathecal | Rehabilitation |
| NCT02688062 | NeuroRegen Scaffold™ With Bone Marrow Mononuclear Cells Transplantation vs. IntraduralDecompression and Adhesiolysis in SCI | Phase 1 Phase 2 | 22 | BMMCs | Transplant into injured spinal cord (v.s. Surgical intradural decompression and adhesiolysis) | NeuroRegen Scaffold |
| NCT02688049 | NeuroRegen Scaffold™ Combined With Stem Cells for Chronic Spinal Cord Injury Repair | Phase 1 Phase 2 | 30 | Mesenchymal Stem Cells/NSCs | Transplant into injured spinal cord | NeuroRegen scaffold |
| NCT02352077 | NeuroRegen Scaffold™ With Stem Cells for Chronic Spinal Cord Injury Repair | Phase 1 | 30 | Bone Marrow Mononuclear Cells/Mesenchymal Stem Cells | Transplant into injured spinal cord | NeuroRegen Scaffold |
| NCT01772810 | Safety Study of Human Spinal Cord-derived Neural Stem Cell Transplantation for the Treatment of Chronic SCI | Phase 1 | 8 | Human Spinal Cord derived NSCs | Surgical implantation | |
| NCT02574585 | Autologous Mesenchymal Stem Cells Transplantation in Thoracolumbar Chronic and Complete Spinal Cord Injury Spinal Cord Injury | Phase 2 | 40 | Autologous Mesenchymal Cells | Percutaneous injections | |
| NCT02574572 | Autologous Mesenchymal Stem Cells Transplantation in Cervical Chronic and Complete Spinal Cord Injury | Phase 1 | 10 | Autologous Mesenchymal Cells | Transplant into injured spinal cord | |
| NCT01676441 | Safety and Efficacy of Autologous Mesenchymal Stem Cells in Chronic Spinal Cord Injury | Phase 2 Phase 3 | 20 | Autologous Mesenchymal Stem Cells | Injection into the intramedullary and intrathecal space | |
| NCT01354483 (Comleted) | Umbilical Cord Blood Mononuclear Cell Transplant to Treat Chronic Spinal Cord Injury | Phase 1 Phase 2 | 20 | Umbilical Cord Blood Mononuclear Cell | Transplant into injured spinal cord | Methylprednisolone Lithium Carbonate Tablet Rehabilitation |
| NCT01186679 (Comleted) | Safety and Efficacy of Autologous Bone Marrow Stem Cells in Treating Spinal Cord Injury | Phase 1 Phase 2 | 12 | Autologous BMSCs | Intrathecal | laminectomy |
| NCT02152657 (Comleted) | Evaluation of Autologous Mesenchymal Stem Cell Transplantation in Chronic Spinal Cord Injury: a PilotStudy | Not Applicable | 5 | Mesenchymal Stem Cells | Percutaneous injection | |
| NCT01909154 (Comleted) | Safety Study of Local Administration of Autologous Bone Marrow Stromal Cells in Chronic Paraplegia | Phase 1 | 12 | Mesenchymal Stromal Cells | Intrathecal | |
| NCT01873547 (Comleted) | Different Efficacy Between Rehabilitation Therapy and Stem Cells Transplantation in Patients With SCI in China | Phase 3 | 300 | Umbilical Cord Mesenchymal Stem Cells | Intrathecal | |
| NCT03003364 (Completed) | Intrathecal Administration of Expanded Wharton’s Jelly Mesenchymal Stem Cells in Chronic Traumatic Spinal Cord Injury | Phase 1 Phase 2 | 10 | Mesenchymal Stem Cells | Intrathecal | |
| NCT02354625 (Completed) | The Safety of ahSC in Chronic SCI With Rehabilitation | Phase 1 | 8 | Autologous human Schwann cells | Transplant into injured spinal cord | Rehabilitation |
| NCT02570932 (Comleted) | Administration of Expanded Autologous Adult Bone Marrow Mesenchymal Cells in Established Chronic Spinal Cord Injuries | Phase 2 | 10 | Autologous BMSCs | Intrathecal |
| Cells | Source | Advantages | Disadvantages | Results | References |
|---|---|---|---|---|---|
| Neural Stem Cells/Neural Precursor Cells | Central Nervous System iPSCs |
|
|
| [7,9,10,11,12,30,31,32,33,34,35,36,37,38,39,40,41,42,43] |
| Induced Pluripotent Stem Cells(iPSCs) | Skin, Blood, Umbilical Cord, Adipose Tissue |
| [6,9,31,32,33,34,35,44,45,46,47,48,49,50,51,52,53] | ||
| Bone Marrow Mesenchymal Stem Cells | Bone Marrow |
|
|
| [54,55,56,57,58,59,60,61] |
| Umbilical Cord Mesenchymal Stem Cells | Umbilical Cord | [62,63,64,65,66,67,68,69,70,71,72,73,74] | |||
| Adipose Mesenchymal Stem Cells | Fat | [75,76,77,78,79,80,81] | |||
| Schwann Cells | Nervous System |
| No differentiation into neurons and astrocytes |
| [82,83,84,85,86] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Suzuki, H.; Sakai, T. Current Concepts of Stem Cell Therapy for Chronic Spinal Cord Injury. Int. J. Mol. Sci. 2021, 22, 7435. https://doi.org/10.3390/ijms22147435
Suzuki H, Sakai T. Current Concepts of Stem Cell Therapy for Chronic Spinal Cord Injury. International Journal of Molecular Sciences. 2021; 22(14):7435. https://doi.org/10.3390/ijms22147435
Chicago/Turabian StyleSuzuki, Hidenori, and Takashi Sakai. 2021. "Current Concepts of Stem Cell Therapy for Chronic Spinal Cord Injury" International Journal of Molecular Sciences 22, no. 14: 7435. https://doi.org/10.3390/ijms22147435
APA StyleSuzuki, H., & Sakai, T. (2021). Current Concepts of Stem Cell Therapy for Chronic Spinal Cord Injury. International Journal of Molecular Sciences, 22(14), 7435. https://doi.org/10.3390/ijms22147435






