Biocompatibility and Biological Performance Evaluation of Additive-Manufactured Bioabsorbable Iron-Based Porous Suture Anchor in a Rabbit Model
Abstract
:1. Introduction
2. Results
2.1. In Vitro Mechanical Analyses of Bioabsorbable Iron SA
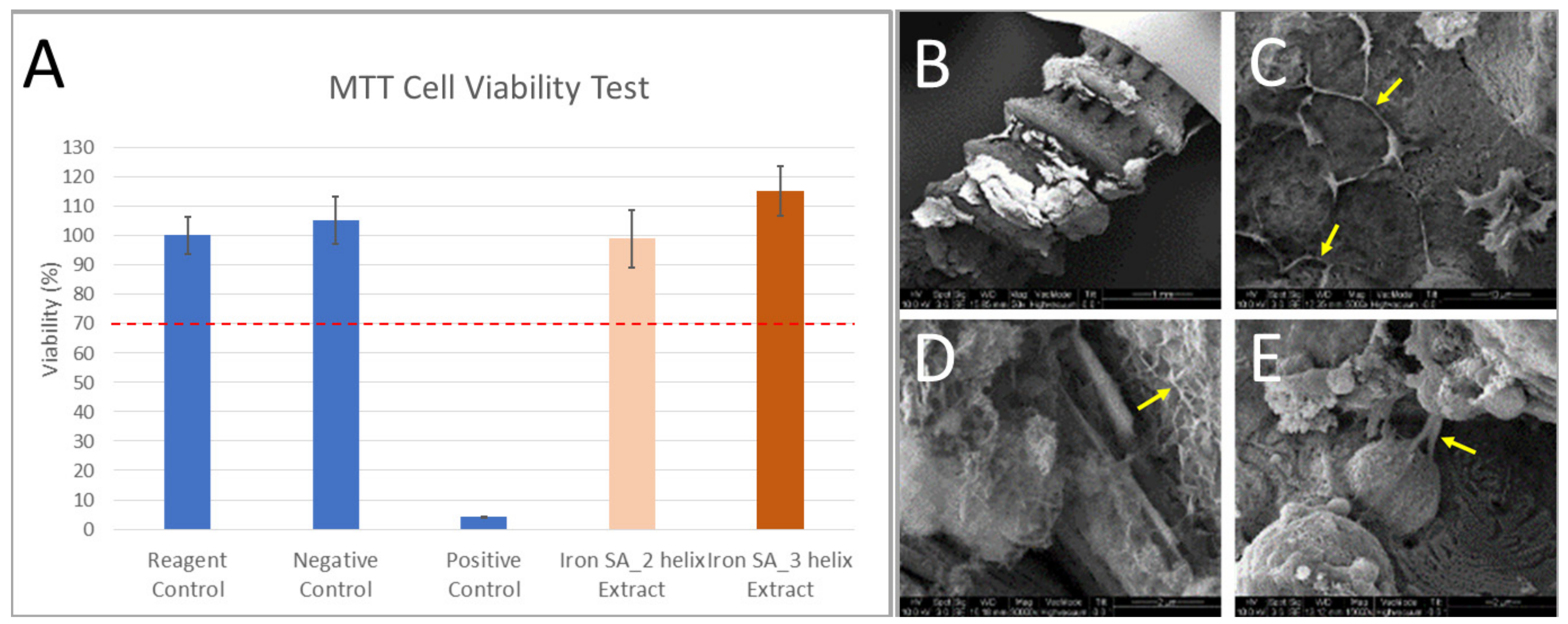
2.2. In Vitro Biocompatibility Analyses of Bioabsorbable Iron SA
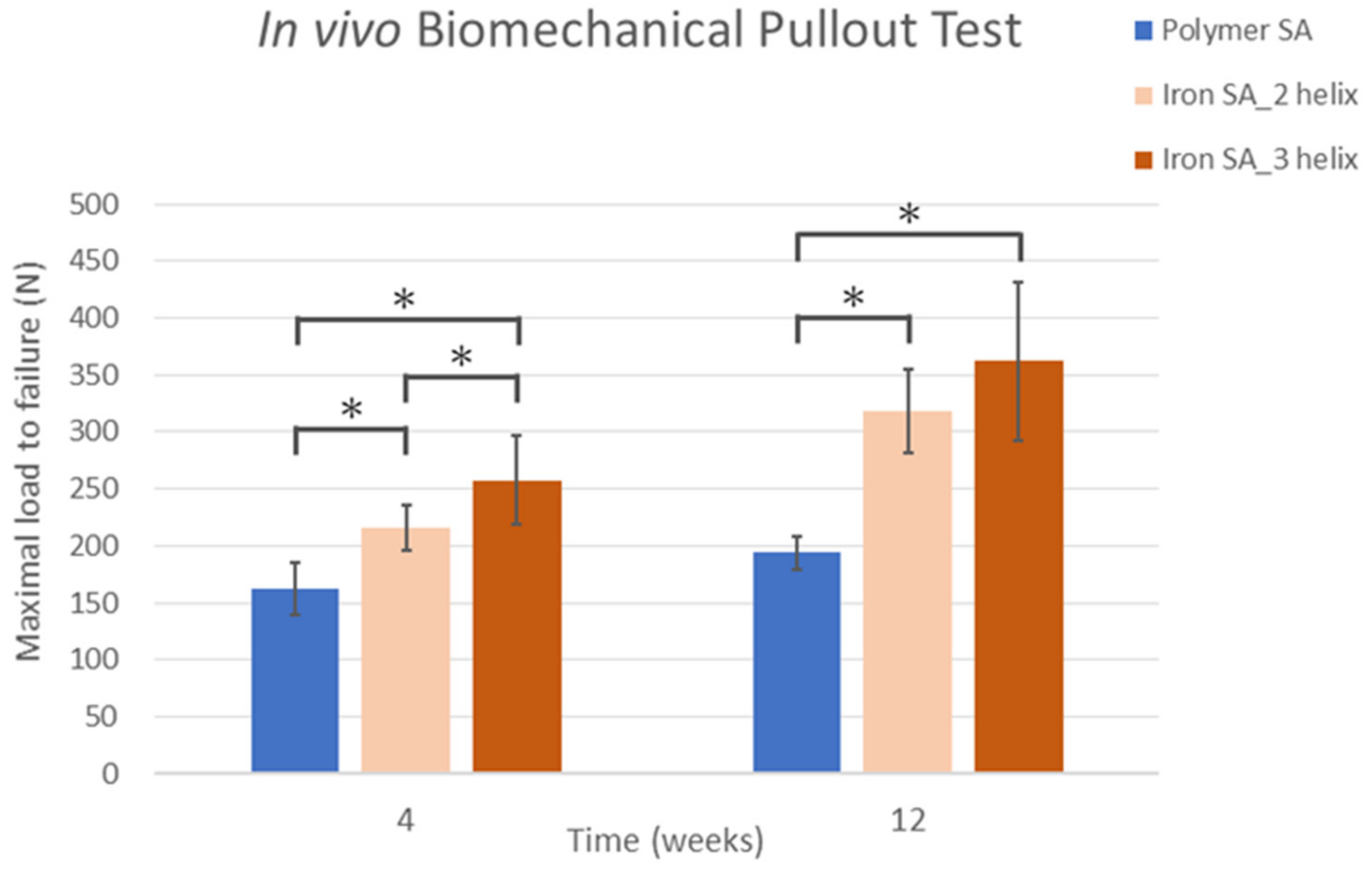
2.3. In Vivo Biomechanical Analysis
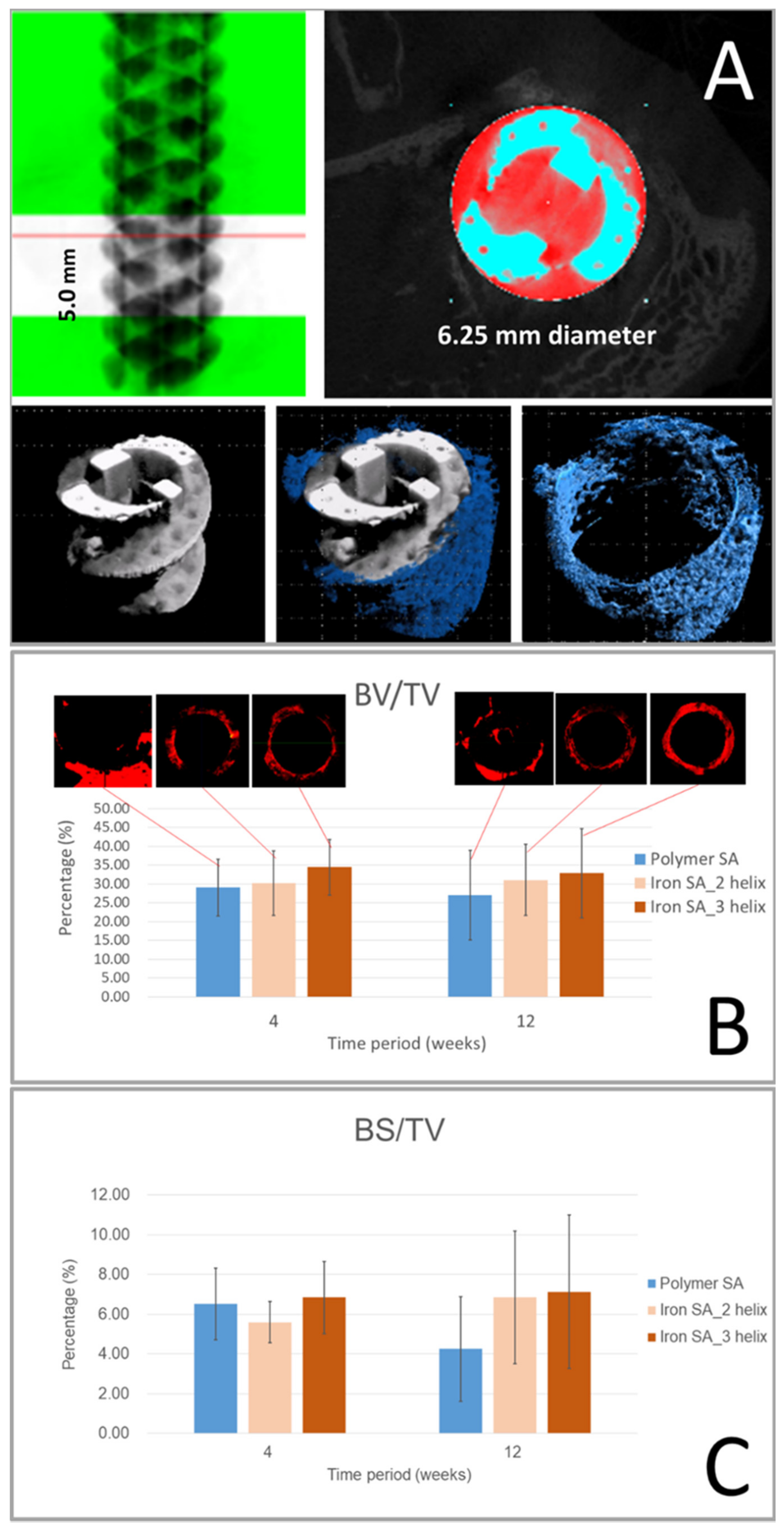
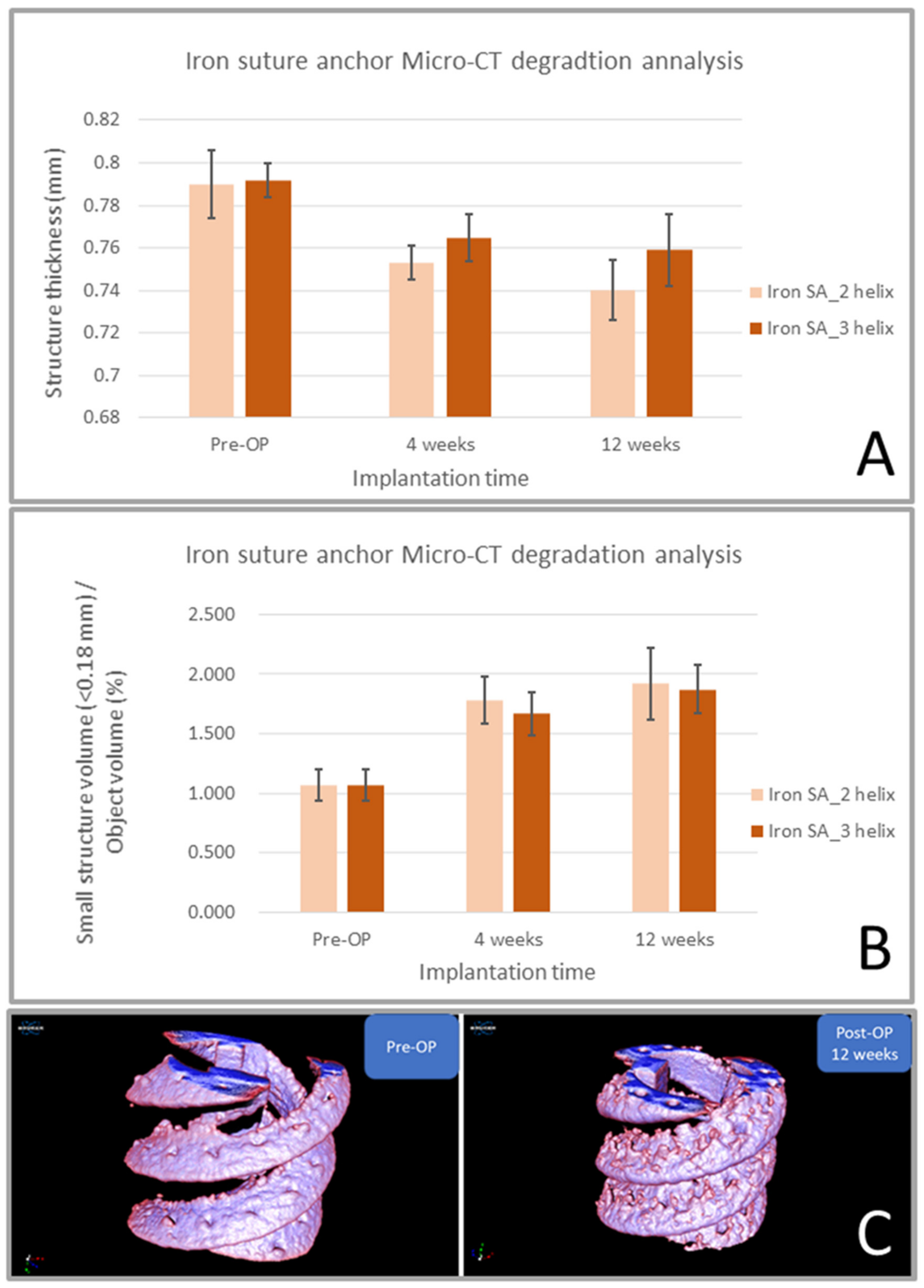
2.4. Micro-CT Analysis
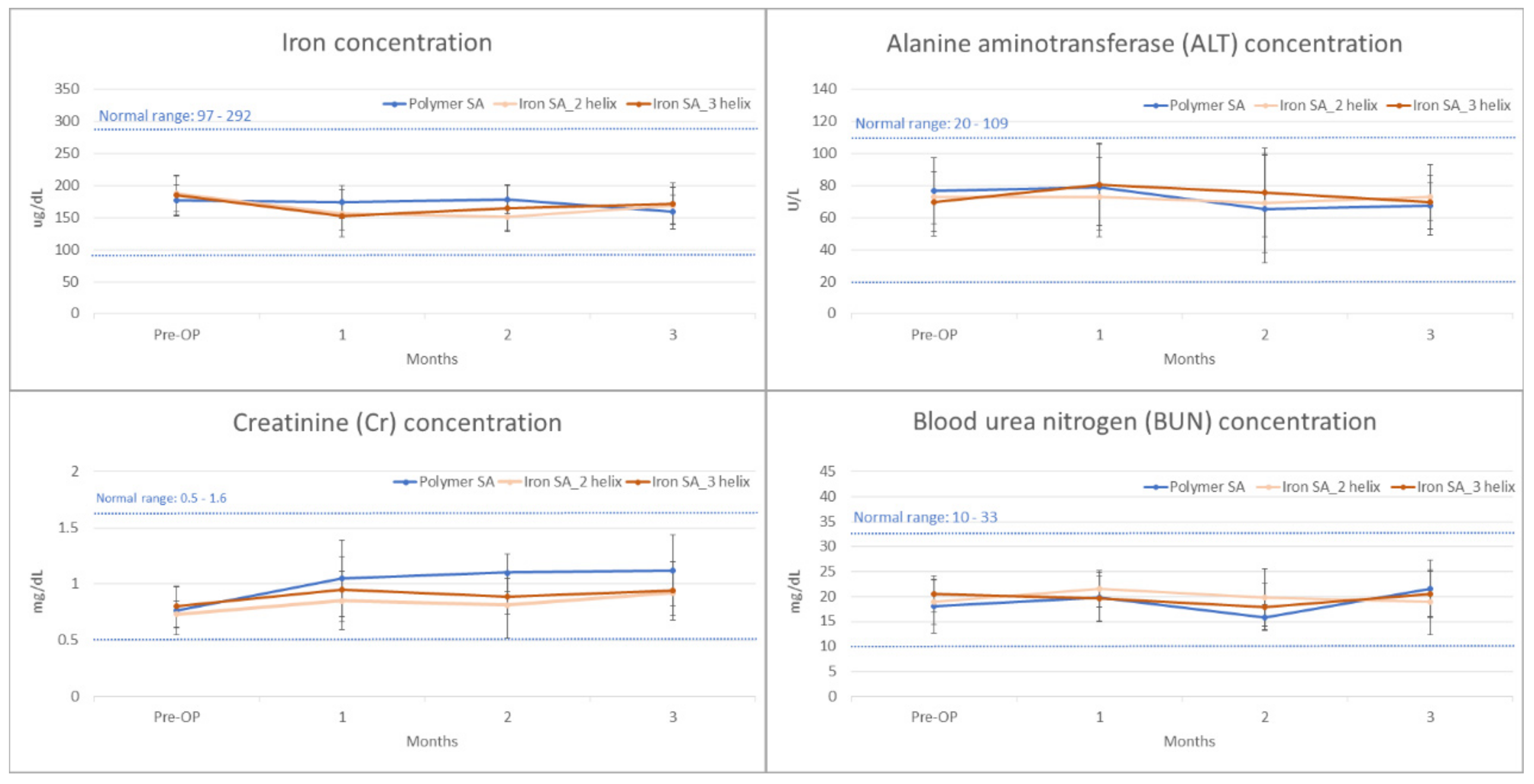
2.5. Biochemical Analysis
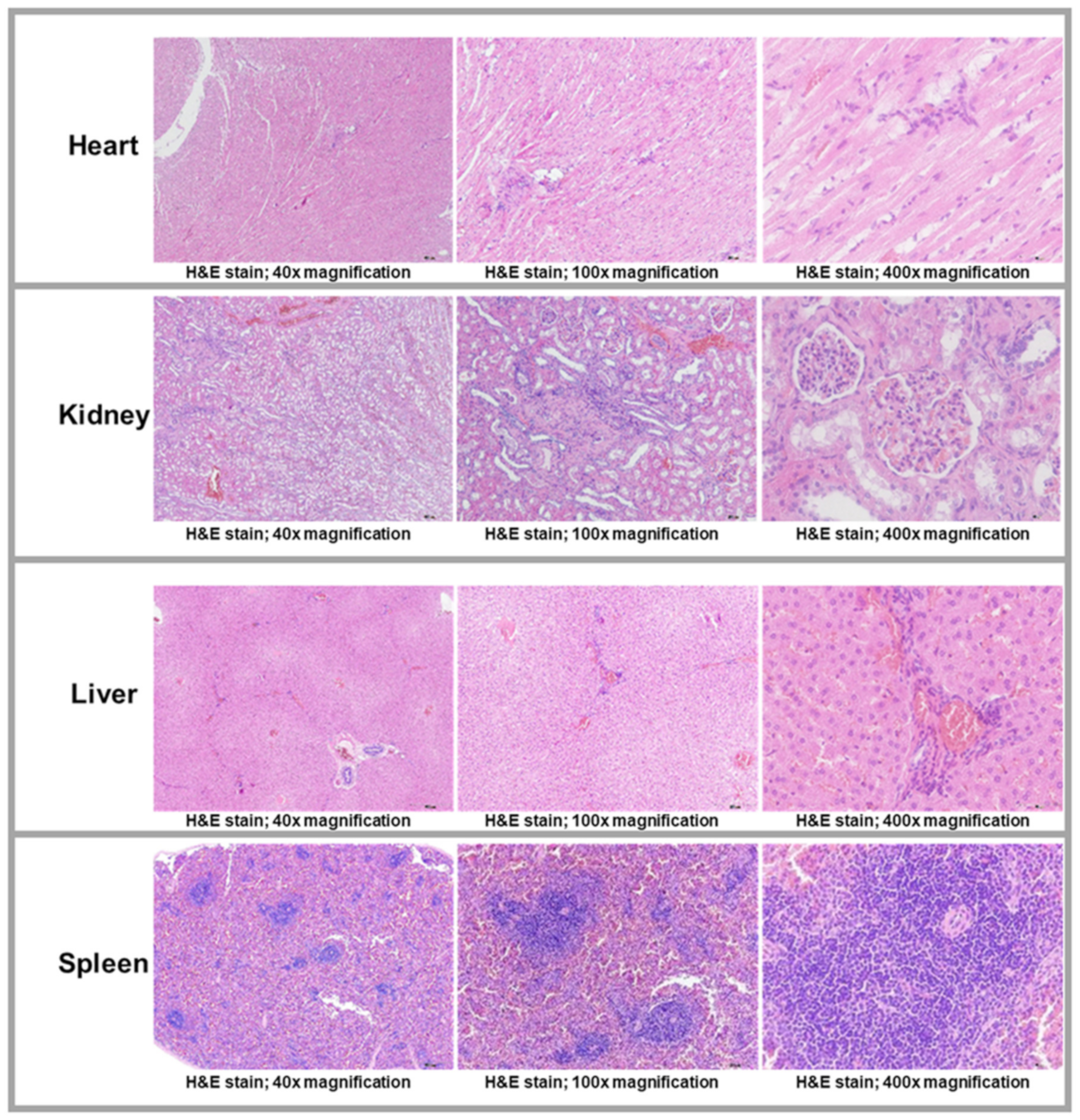
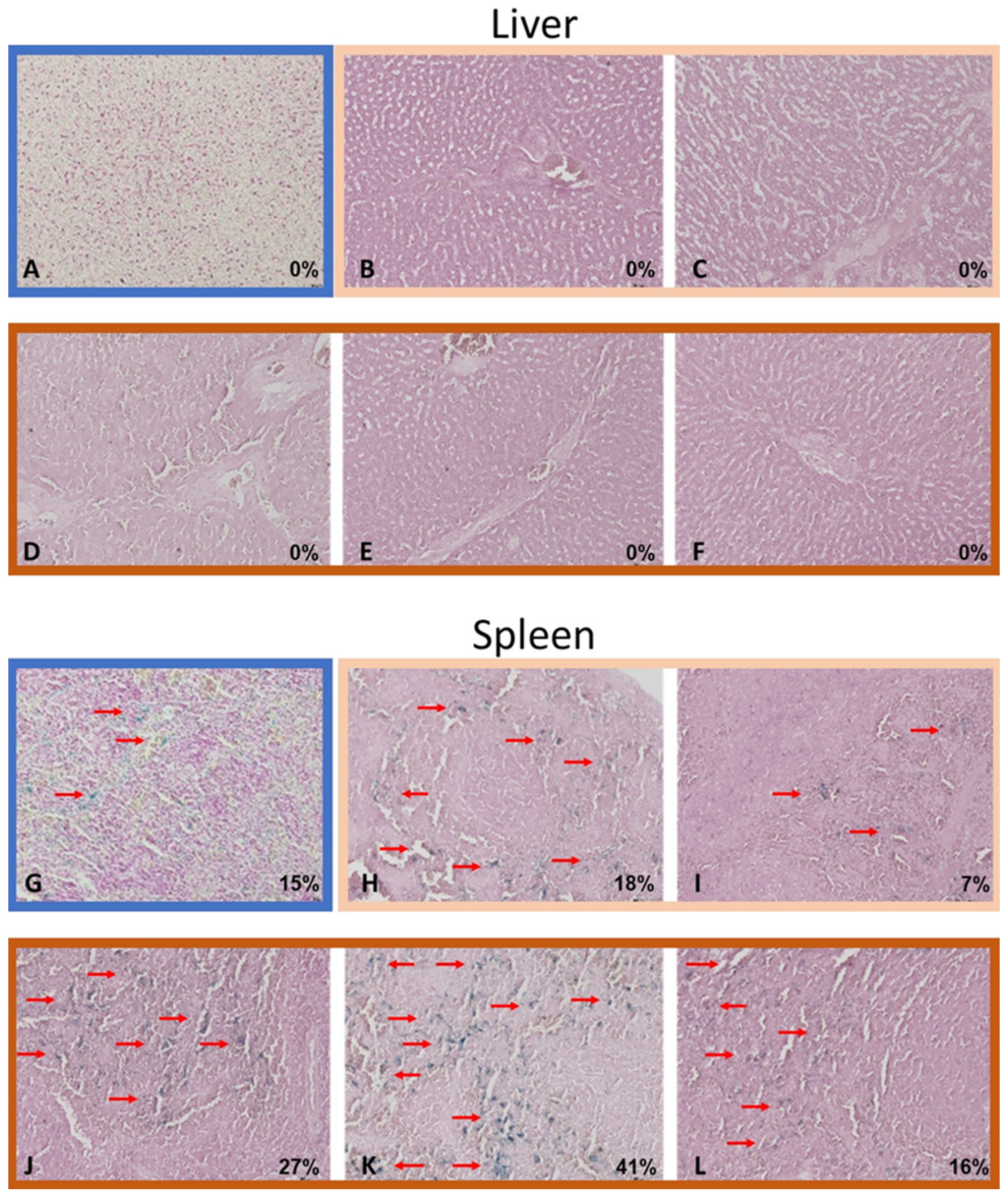
2.6. Histological and Histopathological Analyses
3. Discussion
4. Materials and Methods
4.1. Production and In Vitro Tests of Iron SAs Developed Using AM Technology
4.2. In Vivo Animal Study Design
4.3. Surgical Methods
4.4. Biomechanical Analysis
4.5. Micro-CT Analysis
4.6. Histological Analysis
4.7. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Park, J.B.; Bronzino, J.D. Biomaterials: Principles and Applications, 1st ed.; CRC Press: Boca Raton, FL, USA, 2002. [Google Scholar]
- Joung, Y.-H. Development of implantable medical devices: From an engineering perspective. Int. Neurourol. J. 2013, 17, 98. [Google Scholar] [CrossRef] [PubMed]
- Khan, W.; Muntimadugu, E.; Jaffe, M.; Domb, A.J. Implantable medical devices. In Focal Controlled Drug Delivery; Springer: Berlin/Heidelberg, Germany, 2014; pp. 33–59. [Google Scholar] [CrossRef]
- Han, H.-S.; Loffredo, S.; Jun, I.; Edwards, J.; Kim, Y.-C.; Seok, H.-K.; Witte, F.; Mantovani, D.; Glyn-Jones, S. Current status and outlook on the clinical translation of biodegradable metals. Mater. Today 2019, 23, 57–71. [Google Scholar] [CrossRef]
- Shuai, C.; Li, S.; Peng, S.; Feng, P.; Lai, Y.; Gao, C. Biodegradable metallic bone implants. Mater. Chem. Front. 2019, 3, 544–562. [Google Scholar] [CrossRef]
- Ramakrishna, S.; Mayer, J.; Wintermantel, E.; Leong, K.W. Biomedical applications of polymer-composite materials: A review. Compos. Sci. Technol. 2001, 61, 1189–1224. [Google Scholar] [CrossRef]
- Li, C.; Guo, C.; Fitzpatrick, V.; Ibrahim, A.; Zwierstra, M.J.; Hanna, P.; Lechtig, A.; Nazarian, A.; Lin, S.J.; Kaplan, D.L. Design of biodegradable, implantable devices towards clinical translation. Nat. Rev. Mater. 2020, 5, 61–81. [Google Scholar] [CrossRef]
- Ramsay, S.D.; Pilliar, R.M.; Santerre, J.P. Fabrication of a biodegradable calcium polyphosphate/polyvinyl-urethane carbonate composite for high load bearing osteosynthesis applications. J. Biomed. Mater. Res. Part B Appl. Biomater. 2010, 94, 178–186. [Google Scholar] [CrossRef]
- Figueiredo, L.; Fonseca, R.; Pinto, L.F.; Ferreira, F.C.; Almeida, A.; Rodrigues, A. Strategy to improve the mechanical properties of bioabsorbable materials based on chitosan for orthopedic fixation applications. J. Mech. Behav. Biomed. Mater. 2020, 103, 103572. [Google Scholar] [CrossRef]
- Staiger, M.P.; Pietak, A.M.; Huadmai, J.; Dias, G. Magnesium and its alloys as orthopedic biomaterials: A review. Biomaterials 2006, 27, 1728–1734. [Google Scholar] [CrossRef] [PubMed]
- Witte, F. The history of biodegradable magnesium implants: A review. Acta Biomater. 2010, 6, 1680–1692. [Google Scholar] [CrossRef]
- Yusop, A.H.M.; Daud, N.M.; Nur, H.; Kadir, M.R.A.; Hermawan, H. Controlling the degradation kinetics of porous iron by poly (lactic-co-glycolic acid) infiltration for use as temporary medical implants. Sci. Rep. 2015, 5, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Gorejová, R.; Oriňaková, R.; Orságová Králová, Z.; Baláž, M.; Kupková, M.; Hrubovčáková, M.; Haverová, L.; Džupon, M.; Oriňak, A.; Kaľavský, F. In vitro corrosion behavior of biodegradable iron foams with polymeric coating. Materials 2020, 13, 184. [Google Scholar] [CrossRef] [Green Version]
- Kraus, T.; Moszner, F.; Fischerauer, S.; Fiedler, M.; Martinelli, E.; Eichler, J.; Witte, F.; Willbold, E.; Schinhammer, M.; Meischel, M. Biodegradable Fe-based alloys for use in osteosynthesis: Outcome of an in vivo study after 52 weeks. Acta Biomater. 2014, 10, 3346–3353. [Google Scholar] [CrossRef] [PubMed]
- Francis, A.; Yang, Y.; Virtanen, S.; Boccaccini, A. Iron and iron-based alloys for temporary cardiovascular applications. J. Mater. Sci. Mater. Med. 2015, 26, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Zivic, F.; Grujovic, N.; Pellicer, E.; Sort, J.; Mitrovic, S.; Adamovic, D.; Vulovic, M. Biodegradable metals as biomaterials for clinical Practice: Iron-based materials. In Biomaterials in Clinical Practice, 1st ed.; Springer International Publishing: Berlin/Heidelberg, Germany, 2018; pp. 225–280. [Google Scholar]
- Hong, D.; Chou, D.-T.; Velikokhatnyi, O.I.; Roy, A.; Lee, B.; Swink, I.; Issaev, I.; Kuhn, H.A.; Kumta, P.N. Binder-jetting 3D printing and alloy development of new biodegradable Fe-Mn-Ca/Mg alloys. Acta Biomater. 2016, 45, 375–386. [Google Scholar] [CrossRef] [Green Version]
- Schinhammer, M.; Steiger, P.; Moszner, F.; Löffler, J.F.; Uggowitzer, P.J. Degradation performance of biodegradable FeMnC (Pd) alloys. Mater. Sci. Eng. C 2013, 33, 1882–1893. [Google Scholar] [CrossRef] [PubMed]
- Cheng, J.; Huang, T.; Zheng, Y. Microstructure, mechanical property, biodegradation behavior, and biocompatibility of biodegradable Fe–Fe2O3 composites. J. Biomed. Mater. Res. Part A 2014, 102, 2277–2287. [Google Scholar] [CrossRef]
- Tsai, P.I.; Chen, C.Y.; Huang, S.W.; Yang, K.Y.; Lin, T.H.; Chen, S.Y.; Sun, J.S. Improvement of bone-tendon fixation by porous titanium interference screw: A rabbit animal model. J. Orthop. Res. 2018, 36, 2633–2640. [Google Scholar] [CrossRef]
- Putra, N.; Leeflang, M.; Minneboo, M.; Taheri, P.; Fratila-Apachitei, L.; Mol, J.; Zhou, J.; Zadpoor, A. Extrusion-based 3D printed biodegradable porous iron. Acta Biomater. 2021, 121, 741–756. [Google Scholar] [CrossRef]
- Zadpoor, A.A. Bone tissue regeneration: The role of scaffold geometry. Biomater. Sci. 2015, 3, 231–245. [Google Scholar] [CrossRef]
- Wegener, B.; Sichler, A.; Milz, S.; Sprecher, C.; Pieper, K.; Hermanns, W.; Jansson, V.; Nies, B.; Kieback, B.; Müller, P.E. Development of a novel biodegradable porous iron-based implant for bone replacement. Sci. Rep. 2020, 10, 1–10. [Google Scholar] [CrossRef]
- Chahla, J.; Liu, J.N.; Manderle, B.; Beletsky, A.; Cabarcas, B.; Gowd, A.K.; Inoue, N.; Chubinskaya, S.; Trenhaile, S.; Forsythe, B. Bony ingrowth of coil-type open-architecture anchors compared with screw-type PEEK anchors for the medial row in rotator cuff repair: A randomized controlled trial. Arthrosc. J. Arthrosc. Relat. Surg. 2020, 36, 952–961. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.-H.; Kim, Y.-S.; Park, I.; Lee, H.-J.; Han, S.-Y.; Jung, S.; Shin, S.-J. A comparison of open-construct PEEK suture anchor and non-vented biocomposite suture anchor in arthroscopic rotator cuff repair: A prospective randomized clinical trial. Arthrosc. J. Arthrosc. Relat. Surg. 2020, 36, 389–396. [Google Scholar] [CrossRef] [PubMed]
- Milewski, M.D.; Diduch, D.R.; Hart, J.M.; Tompkins, M.; Ma, S.-Y.; Gaskin, C.M. Bone replacement of fast-absorbing biocomposite anchors in arthroscopic shoulder labral repairs. Am. J. Sports Med. 2012, 40, 1392–1401. [Google Scholar] [CrossRef]
- Prabhu, B.; Karau, A.; Wood, A.; Dadsetan, M.; Liedtke, H.; DeWitt, T. Bioresorbable Materials for Orthopedic Applications (Lactide and Glycolide Based). In Orthopedic Biomaterials; Springer: Berlin/Heidelberg, Germany, 2018; pp. 287–344. [Google Scholar]
- Park, K.; Skidmore, S.; Hadar, J.; Garner, J.; Park, H.; Otte, A.; Soh, B.K.; Yoon, G.; Yu, D.; Yun, Y. Injectable, long-acting PLGA formulations: Analyzing PLGA and understanding microparticle formation. J. Control. Release 2019, 304, 125–134. [Google Scholar] [CrossRef] [PubMed]
- Yamauchi, S.; Tsukada, H.; Sasaki, E.; Sasaki, S.; Kimura, Y.; Yamamoto, Y.; Tsuda, E.; Ishibashi, Y. Biomechanical analysis of bioabsorbable suture anchors for rotator cuff repair using osteoporotic and normal bone models. J. Orthop. Sci. 2021. [Google Scholar] [CrossRef]
- Gorejová, R.; Haverová, L.; Oriňaková, R.; Oriňak, A.; Oriňak, M. Recent advancements in Fe-based biodegradable materials for bone repair. J. Mater. Sci. 2019, 54, 1913–1947. [Google Scholar] [CrossRef]
- Traverson, M.; Heiden, M.; Stanciu, L.A.; Nauman, E.A.; Jones-Hall, Y.; Breur, G.J. In vivo evaluation of biodegradability and biocompatibility of Fe30Mn alloy. Vet. Comp. Orthop. Traumatol. 2018, 31, 10–16. [Google Scholar]
- Hermawan, H. Updates on the research and development of absorbable metals for biomedical applications. Prog. Biomater. 2018, 7, 93–110. [Google Scholar] [CrossRef] [Green Version]
- Peuster, M.; Hesse, C.; Schloo, T.; Fink, C.; Beerbaum, P.; von Schnakenburg, C. Long-term biocompatibility of a corrodible peripheral iron stent in the porcine descending aorta. Biomaterials 2006, 27, 4955–4962. [Google Scholar] [CrossRef]
- Yang, Y.; Zhou, J.; Detsch, R.; Taccardi, N.; Heise, S.; Virtanen, S.; Boccaccini, A.R. Biodegradable nanostructures: Degradation process and biocompatibility of iron oxide nanostructured arrays. Mater. Sci. Eng. C 2018, 85, 203–213. [Google Scholar] [CrossRef]
- Visscher, L.E.; Jeffery, C.; Gilmour, T.; Anderson, L.; Couzens, G. The history of suture anchors in orthopaedic surgery. Clin. Biomech. 2019, 61, 70–78. [Google Scholar] [CrossRef] [Green Version]
- Barber, F.A.; Herbert, M.A. Cyclic loading biomechanical analysis of the pullout strengths of rotator cuff and glenoid anchors: 2013 update. Arthrosc. J. Arthrosc. Relat. Surg. 2013, 29, 832–844. [Google Scholar] [CrossRef]
- Chaudhry, S.; Dehne, K.; Hussain, F. A review of suture anchors. Orthop. Trauma 2019, 33, 263–270. [Google Scholar] [CrossRef]
- Chae, S.W.; Kang, J.Y.; Lee, J.; Han, S.H.; Kim, S.Y. Effect of structural design on the pullout strength of suture anchors for rotator cuff repair. J. Orthop. Res.® 2018, 36, 3318–3327. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Horoz, L.; Hapa, O.; Barber, F.A.; Hüsemoğlu, B.; Özkan, M.; Havitçioğlu, H. Suture anchor fixation in osteoporotic bone: A biomechanical study in an ovine model. Arthrosc. J. Arthrosc. Relat. Surg. 2017, 33, 68–74. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.-C.; Lam, T.-N.; Amalia, L.; Chen, K.-H.; Yang, K.-Y.; Muslih, M.R.; Singh, S.S.; Tsai, P.-I.; Lee, Y.-T.; Jain, J. Tailoring grain sizes of the biodegradable iron-based alloys by pre-additive manufacturing microalloying. Sci. Rep. 2021, 11, 1–12. [Google Scholar]
- Yamakado, K.; Kitaoka, K.; Yamada, H.; Hashiba, K.; Nakamura, R.; Tomita, K. The influence of mechanical stress on graft healing in a bone tunnel. Arthrosc. J. Arthrosc. Relat. Surg. 2002, 18, 82–90. [Google Scholar] [CrossRef]
- Pyka, G.; Kerckhofs, G.; Schrooten, J.; Wevers, M. The effect of spatial micro-CT image resolution and surface complexity on the morphological 3D analysis of open porous structures. Mater. Charact. 2014, 87, 104–115. [Google Scholar] [CrossRef]
- Chiu, Y.-R.; Hsu, Y.-T.; Wu, C.-Y.; Lin, T.-H.; Yang, Y.-Z.; Chen, H.-Y. Fabrication of asymmetrical and gradient hierarchy structures of poly-p-xylylenes on multiscale regimes based on a vapor-phase sublimation and deposition process. Chem. Mater. 2020, 32, 1120–1130. [Google Scholar] [CrossRef]
- Van Dalen, G.; Koster, M. 2D & 3D particle size analysis of micro-CT images. In Proceedings of the Bruker Micro-CT User Meeting, Brussels, Belgium, 13 November 2012; pp. 3–5. [Google Scholar]
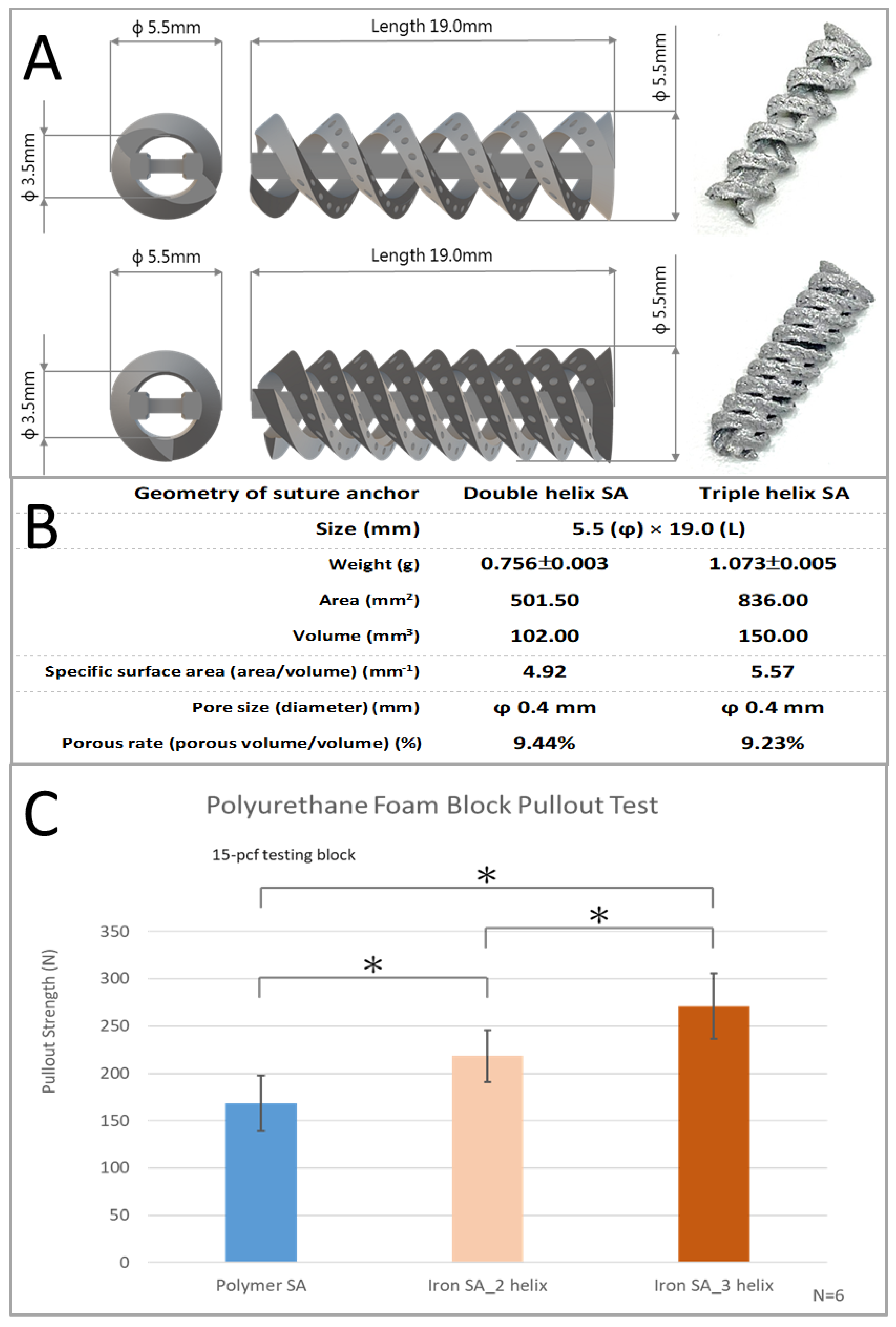

| Group | Pullout Strength (N) | p Value vs. Polymer SA | p Value vs. Polymer SA |
|---|---|---|---|
| Polymer SA | 168.54 ± 29.45 | ||
| Iron SA_2 Helix | 218.43 ± 27.53 | 0.0126 | |
| Iron SA_3 Helix | 270.94 ± 34.76 | 0.0003 | 0.0158 |
| Viability ± SD (%) | |
|---|---|
| Reagent Control | 100 ± 6.46 |
| Negative Control | 105.1 ± 7.95 |
| Positive Control | 4.22 ± 0.12 |
| Iron SA_2 Helix Extract | 98.83 ± 9.61 |
| Iron SA_3 Helix Extract | 115.08 ± 8.45 |
| Inter-Group Statistical Analysis | ||||
|---|---|---|---|---|
| Weeks | Group | Pullout Strength (N) | p Value vs. Polymer SA | p Value vs. Iron SA_2 Helix |
| 4 | Polymer SA | 162.36 ± 23.02 | ||
| Iron SA_2 Helix | 216.23 ± 20.07 | 0.015 | ||
| Iron SA_3 Helix | 257.85 ± 38.66 | 0.004 | 0.0413 | |
| 12 | Polymer SA | 193.80 ± 14.28 | ||
| Iron SA_2 Helix | 318.59 ± 36.58 | 0.0001 | ||
| Iron SA_3 Helix | 361.97 ± 69.45 | 0.0002 | 0.2056 | |
| Intra-group statistical analysis | ||||
| Group | p value between 4 vs. 12 weeks | |||
| Polymer SA | 0.0175 | |||
| Iron SA_2 helix | 0.0001 | |||
| Iron SA_3 helix | 0.0094 | |||
| BV/TV Inter-Group Statistical Analysis | ||||
|---|---|---|---|---|
| Weeks | Group | BV/TV (%) | p Value vs. Polymer SA | p Value vs. Iron SA_2 Helix |
| 4 | Polymer SA | 29.04 ± 7.57 | ||
| Iron SA_2 Helix | 30.19 ± 8.55 | 0.8102 | ||
| Iron SA_3 Helix | 34.42 ± 7.33 | 0.2395 | 0.3792 | |
| 12 | Polymer SA | 27.01 ± 11.86 | ||
| Iron SA_2 Helix | 31.02 ± 9.46 | 0.5319 | ||
| Iron SA_3 Helix | 32.89 ± 11.81 | 0.4097 | 0.7683 | |
| BV/TV Intra-Group Statistical Analysis | ||||
| Group | p Value between 4 vs. 12 Weeks | |||
| Polymer SA | 0.7311 | |||
| Iron SA_2 Helix | 0.8765 | |||
| Iron SA_3 Helix | 0.7929 | |||
| BS/TV Inter-Group Statistical Analysis | ||||
| Weeks | Group | BS/TV (%) | p Value vs. Polymer SA | p Value vs. Iron SA_2 Helix |
| 4 | Polymer SA | 6.52 ± 1.80 | ||
| Iron SA_2 Helix | 5.60 ± 1.04 | 0.3038 | ||
| Iron SA_3 Helix | 6.84 ± 1.82 | 0.7657 | 0.1780 | |
| 12 | Polymer SA | 4.25 ± 2.64 | ||
| Iron SA_2 Helix | 6.85 ± 3.34 | 0.1656 | ||
| Iron SA_3 Helix | 7.13 ± 3.87 | 0.1630 | 0.8959 | |
| BS/TV Intra-Group Statistical Analysis | ||||
| Group | p value between 4 vs. 12 Weeks | |||
| Polymer SA | 0.1124 | |||
| Iron SA_2 Helix | 0.4020 | |||
| Iron SA_3 Helix | 0.8714 | |||
| ST Inter-Group Statistical Analysis | ||||
| Weeks | Group | ST (mm) | p Value vs. Pre-OP | p Value vs. 4 Weeks |
| Pre-OP | Iron SA_2 helix | 0.790 ± 0.016 | ||
| Iron SA_3 helix | 0.792 ± 0.008 | |||
| 4 | Iron SA_2 helix | 0.753 ± 0.008 | 0.0005 | |
| Iron SA_3 helix | 0.765 ± 0.011 | 0.0007 | ||
| 12 | Iron SA_2 helix | 0.740 ± 0.014 | 0.0002 | 0.0765 |
| Iron SA_3 helix | 0.759 ± 0.017 | 0.0016 | 0.4846 | |
| ST Intra-Group Statistical Analysis | ||||
| Time period | p value between 2 vs. 3 helix | |||
| Pre-OP | 0.7898 | |||
| 4 weeks | 0.056 | |||
| 12 weeks | 0.0607 | |||
| SSV/OV Inter-Group Statistical Analysis | ||||
| Weeks | Group | SSV/OV (%) | p Value vs. Pre-OP | p Value vs. 4 Weeks |
| Pre-OP | Iron SA_2 helix | 1.068 ± 0.128 | ||
| Iron SA_3 helix | 1.064 ± 0.132 | |||
| 4 | Iron SA_2 helix | 1.780 ± 0.194 | 0.0001 | |
| Iron SA_3 helix | 1.666 ± 0.179 | 0.0001 | ||
| 12 | Iron SA_2 helix | 1.920 ± 0.301 | 0.0001 | 0.3608 |
| Iron SA_3 helix | 1.871 ± 0.205 | 0.0001 | 0.0948 | |
| SSV/OV Intra-Group Statistical Analysis | ||||
| Time period | p value between 2 vs. 3 Helix | |||
| Pre-OP | 0.9586 | |||
| 4 weeks | 0.315 | |||
| 12 weeks | 0.7485 | |||
| Iron Concentration (μg/dL) | ||||
|---|---|---|---|---|
| Pre-OP | 4 Weeks | 8 Weeks | 12 Weeks | |
| Polymer SA | 176.39 ± 24.84 | 173.51 ± 25.49 | 178.48 ± 21.97 | 158.43 ± 26.28 |
| Iron SA_2 Helix | 186.85 ± 28.54 | 156.87 ± 36.52 | 150.87 ± 23.68 | 168.96 ± 28.57 |
| Iron SA_3 Helix | 184.54 ± 30.58 | 152.47 ± 22.25 | 164.86 ± 34.85 | 170.65 ± 32.58 |
| Alanine Transaminase (ALT) Concentration (U/L) | ||||
| Pre-OP | 4 weeks | 8 weeks | 12 weeks | |
| Polymer SA | 76.58 ± 20.58 | 78.52 ± 26.54 | 65.44 ± 33.52 | 67.61 ± 18.72 |
| Iron SA_2 Helix | 72.86 ± 24.27 | 72.54 ± 24.20 | 68.84 ± 30.79 | 72.86 ± 20.11 |
| Iron SA_3 Helix | 69.68 ± 18.57 | 80.54 ± 25.67 | 75.28 ± 27.65 | 69.81 ± 11.92 |
| Creatinine (Cr) Concentration (mg/dL) | ||||
| Pre-OP | 4 weeks | 8 weeks | 12 weeks | |
| Polymer SA | 0.76 ± 0.21 | 1.05 ± 0.34 | 1.10 ± 0.17 | 1.12 ± 0.32 |
| Iron SA_2 Helix | 0.73 ± 0.12 | 0.85 ± 0.26 | 0.81 ± 0.29 | 0.92 ± 0.20 |
| Iron SA_3 Helix | 0.80 ± 0.18 | 0.95 ± 0.29 | 0.89 ± 0.16 | 0.94 ± 0.26 |
| Blood Urea Nitrogen (BUN) Concentration (mg/dL) | ||||
| Pre-OP | 4 weeks | 8 weeks | 12 weeks | |
| Polymer SA | 17.99 ± 5.31 | 19.85 ± 4.97 | 15.87 ± 2.59 | 21.52 ± 5.81 |
| Iron SA_2 Helix | 18.85 ± 4.52 | 21.54 ± 3.58 | 19.83 ± 5.78 | 18.85 ± 6.58 |
| Iron SA_3 Helix | 20.54 ± 3.67 | 19.63 ± 4.57 | 17.88 ± 4.73 | 20.52 ± 4.52 |
| Semi-Quantitative Analysis for Prussian-Blue (Iron Stain) of Spleen | ||||
|---|---|---|---|---|
| Simple Scoring of Spleen Iron Store | Percentage of Spleen Iron Store (%) | p Value vs. Polymer SA | p Value vs. Iron SA_2 Helix | |
| Polymer SA | + | 25.5 ± 14.8 | ||
| Iron SA_2 Helix | + | 22.4 ± 11.8 | 0.6967 | |
| Iron SA_3 Helix | + | 24.9 ± 16.1 | 0.9477 | 0.7653 |
| Semi-Quantitative Analysis for Prussian-Blue (Iron Stain) of Liver | ||||
| Simple Scoring for Iron Store in Liver | ||||
| Polymer SA | Not Detectable (ND) | |||
| Iron SA_2 Helix | Not Detectable (ND) | |||
| Iron SA_3 Helix | Not Detectable (ND) | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tai, C.-C.; Lo, H.-L.; Liaw, C.-K.; Huang, Y.-M.; Huang, Y.-H.; Yang, K.-Y.; Huang, C.-C.; Huang, S.-I.; Shen, H.-H.; Lin, T.-H.; et al. Biocompatibility and Biological Performance Evaluation of Additive-Manufactured Bioabsorbable Iron-Based Porous Suture Anchor in a Rabbit Model. Int. J. Mol. Sci. 2021, 22, 7368. https://doi.org/10.3390/ijms22147368
Tai C-C, Lo H-L, Liaw C-K, Huang Y-M, Huang Y-H, Yang K-Y, Huang C-C, Huang S-I, Shen H-H, Lin T-H, et al. Biocompatibility and Biological Performance Evaluation of Additive-Manufactured Bioabsorbable Iron-Based Porous Suture Anchor in a Rabbit Model. International Journal of Molecular Sciences. 2021; 22(14):7368. https://doi.org/10.3390/ijms22147368
Chicago/Turabian StyleTai, Chien-Cheng, Hon-Lok Lo, Chen-Kun Liaw, Yu-Min Huang, Yen-Hua Huang, Kuo-Yi Yang, Chih-Chieh Huang, Shin-I Huang, Hsin-Hsin Shen, Tzu-Hung Lin, and et al. 2021. "Biocompatibility and Biological Performance Evaluation of Additive-Manufactured Bioabsorbable Iron-Based Porous Suture Anchor in a Rabbit Model" International Journal of Molecular Sciences 22, no. 14: 7368. https://doi.org/10.3390/ijms22147368
APA StyleTai, C.-C., Lo, H.-L., Liaw, C.-K., Huang, Y.-M., Huang, Y.-H., Yang, K.-Y., Huang, C.-C., Huang, S.-I., Shen, H.-H., Lin, T.-H., Lu, C.-K., Liu, W.-C., Sun, J.-S., Tsai, P.-I., & Chen, C.-Y. (2021). Biocompatibility and Biological Performance Evaluation of Additive-Manufactured Bioabsorbable Iron-Based Porous Suture Anchor in a Rabbit Model. International Journal of Molecular Sciences, 22(14), 7368. https://doi.org/10.3390/ijms22147368






