Differences in Osteoimmunological Biomarkers Predictive of Psoriatic Arthritis among a Large Italian Cohort of Psoriatic Patients
Abstract
1. Introduction
2. Results
2.1. Clinical Features of the Study Cohorts
2.2. Biochemical Characterization of the Study Cohorts
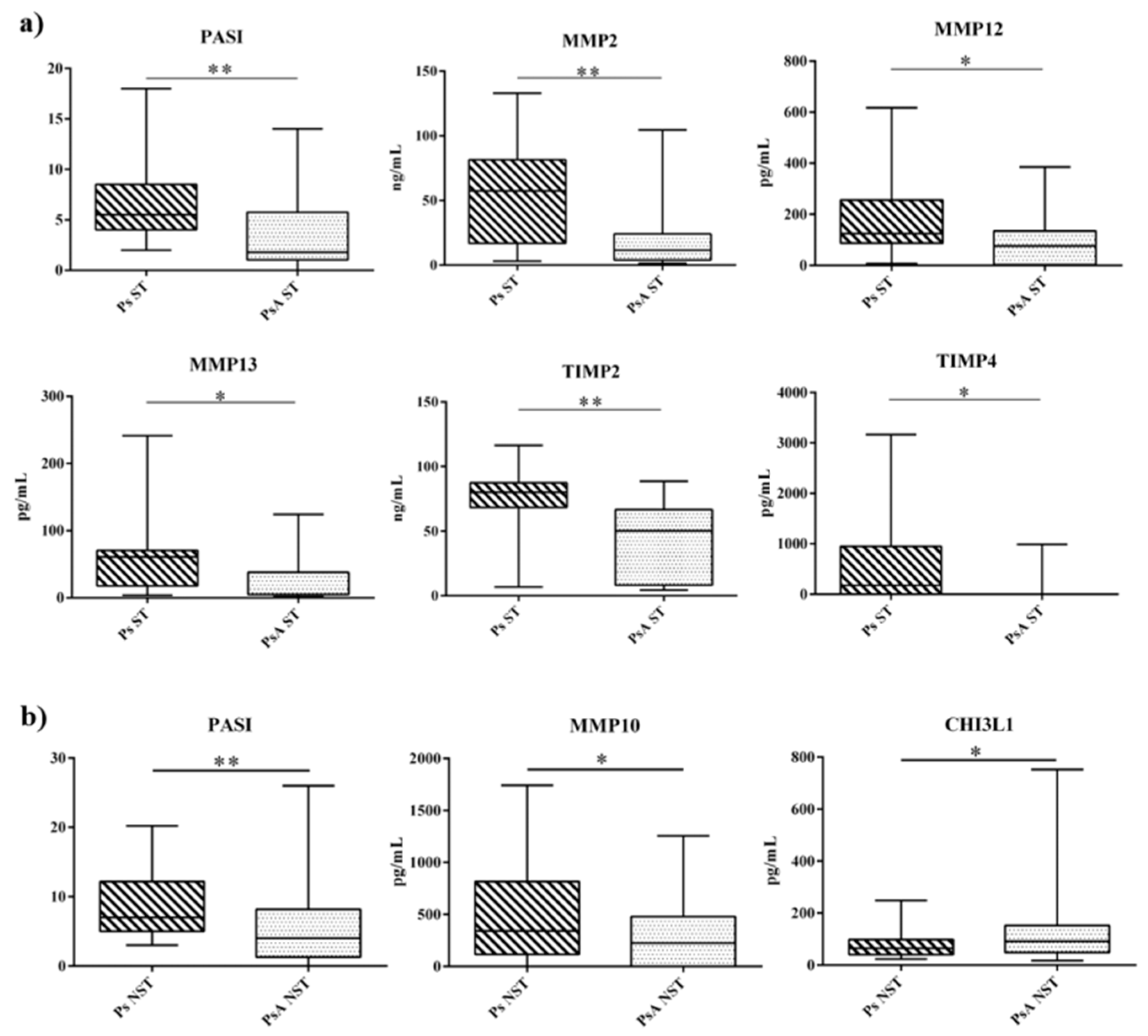
2.3. Effect of Systemic Treatments
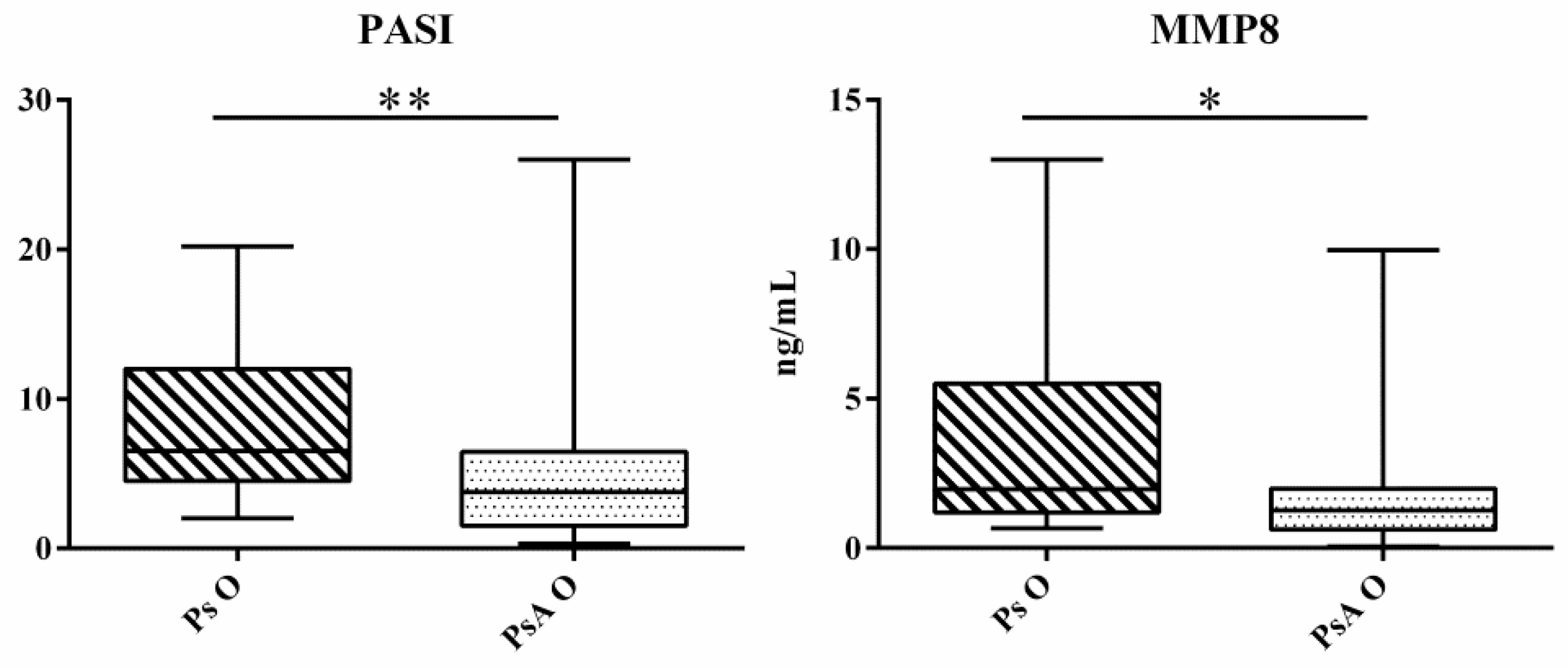
2.4. Onychopathy Biochemical Signature
3. Discussion
4. Methods
4.1. Ethical Committee
4.2. Patients Selection and Study Design
4.3. Dermatology and Rheumatology Assessment of Patients
4.4. Blood Sampling and Biochemical Determinations
4.5. Statistical Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Ritchlin, C.T.; Colbert, R.A.; Gladman, D.D. Psoriatic Arthritis. N. Eng. J. Med. 2017, 376, 957–970. [Google Scholar] [CrossRef] [PubMed]
- Kane, D.; Stafford, L.; Bresnihan, B.; FitzGerald, O. A prospective, clinical and radiological study of early psoriatic arthritis: An early synovitis clinic experience. Rheumatology 2003, 42, 1460–1468. [Google Scholar] [CrossRef] [PubMed]
- Haneke, E. Nail psoriasis: Clinical features, pathogenesis, differential diagnoses, and management. Psoriasis 2017, 7, 51–63. [Google Scholar] [CrossRef]
- Ibrahim, G.H.; Buch, M.H.; Lawson, C.; Waxman, R.; Helliwell, P.S. Evaluation of an existing screening tool for psoriatic arthritis in people with psoriasis and the development of a new instrument: The Psoriasis Epidemiology Screening Tool (PEST) questionnaire. Clin. Exp. Rheumatol. 2009, 27, 469–474. [Google Scholar] [PubMed]
- Ogdie, A. The preclinical phase of PsA: A challenge for the epidemiologist. Ann. Rheum. Dis. 2017, 76, 1481–1483. [Google Scholar] [CrossRef] [PubMed]
- Biomarkers Definitions Working Group. Biomarkers and surrogate endpoints: Preferred definitions and conceptual framework. Clin. Pharmacol. Ther. 2001, 69, 89–95. [Google Scholar] [CrossRef]
- Chandran, V.; Cook, R.J.; Edwin, J.; Shen, H.; Pellett, F.J.; Shanmugarajah, S.; Rosen, C.F.; Gladman, D.D. Soluble biomarkers differentiate patients with psoriatic arthritis from those with psoriasis without arthritis. Rheumatology 2010, 49, 1399–1405. [Google Scholar] [CrossRef]
- Abji, F.; Pollock, R.A.; Liang, K.; Chandran, V.; Gladman, D.D. CXCL10 Is a Possible Biomarker for the Development of Psoriatic Arthritis among Patients with Psoriasis. Arthritis Rheumatol. 2016, 68, 2911–2916. [Google Scholar] [CrossRef]
- Alenius, G.M.; Eriksson, C.; Rantapaa Dahlqvist, S. Interleukin-6 and soluble interleukin-2 receptor alpha-markers of inflammation in patients with psoriatic arthritis? Clin. Exp. Rheumatol. 2009, 27, 120–123. [Google Scholar]
- Dalbeth, N.; Pool, B.; Smith, T.; Callon, K.E.; Lobo, M.; Taylor, W.J.; Cornish, J.; McQueen, F.M. Circulating mediators of bone remodeling in psoriatic arthritis: Implications for disordered osteoclastogenesis and bone erosion. Arthritis Res. Ther. 2010, 12, R164. [Google Scholar] [CrossRef]
- Armesto, S.; Esteve, A.; Coto-Segura, P.; Drake, M.; Galache, C.; Martinez-Borra, J.; Santos-Juanes, J. [Nail psoriasis in individuals with psoriasis vulgaris: A study of 661 patients]. Actas Dermo-Sifiliogr. 2011, 102, 365–372. [Google Scholar] [CrossRef] [PubMed]
- Augustin, M.; Reich, K.; Blome, C.; Schafer, I.; Laass, A.; Radtke, M.A. Nail psoriasis in Germany: Epidemiology and burden of disease. Br. J. Dermatol. 2010, 163, 580–585. [Google Scholar] [CrossRef] [PubMed]
- Sakellariou, G.; Lombardi, G.; Vitolo, B.; Gomarasca, M.; Faraldi, M.; Caporali, R.; Banfi, G.; Montecucco, C. Serum calprotectin as a marker of ultrasound-detected synovitis in early psoriatic and rheumatoid arthritis: Results from a cross-sectional retrospective study. Clin. Exp. Rheumatol. 2019, 37, 429–436. [Google Scholar] [PubMed]
- Bartosinska, J.; Michalak-Stoma, A.; Juszkiewicz-Borowiec, M.; Kowal, M.; Chodorowska, G. The Assessment of Selected Bone and Cartilage Biomarkers in Psoriatic Patients from Poland. Mediat. Inflamm. 2015, 2015, 194535. [Google Scholar] [CrossRef]
- Merola, J.F.; Espinoza, L.R.; Fleischmann, R. Distinguishing rheumatoid arthritis from psoriatic arthritis. RMD Open 2018, 4, e000656. [Google Scholar] [CrossRef]
- Mc Ardle, A.; Flatley, B.; Pennington, S.R.; FitzGerald, O. Early biomarkers of joint damage in rheumatoid and psoriatic arthritis. Arthritis Res. Ther. 2015, 17, 141. [Google Scholar] [CrossRef]
- Lee, C.G.; Hartl, D.; Lee, G.R.; Koller, B.; Matsuura, H.; Da Silva, C.A.; Sohn, M.H.; Cohn, L.; Homer, R.J.; Kozhich, A.A.; et al. Role of breast regression protein 39 (BRP-39)/chitinase 3-like-1 in Th2 and IL-13-induced tissue responses and apoptosis. J. Exp. Med. 2009, 206, 1149–1166. [Google Scholar] [CrossRef]
- Di Rosa, M.; Distefano, G.; Zorena, K.; Malaguarnera, L. Chitinases and immunity: Ancestral molecules with new functions. Immunobiology 2016, 221, 399–411. [Google Scholar] [CrossRef]
- Rathcke, C.N.; Johansen, J.S.; Vestergaard, H. YKL-40, a biomarker of inflammation, is elevated in patients with type 2 diabetes and is related to insulin resistance. Inflamm. Res. 2006, 55, 53–59. [Google Scholar] [CrossRef]
- Di Rosa, M.; Tibullo, D.; Vecchio, M.; Nunnari, G.; Saccone, S.; Di Raimondo, F.; Malaguarnera, L. Determination of chitinases family during osteoclastogenesis. Bone 2014, 61, 55–63. [Google Scholar] [CrossRef]
- Coffman, F.D. Chitinase 3-Like-1 (CHI3L1): A putative disease marker at the interface of proteomics and glycomics. Crit. Rev. Clin. Lab. Sci. 2008, 45, 531–562. [Google Scholar] [CrossRef] [PubMed]
- Andersen, O.A.; Dixon, M.J.; Eggleston, I.M.; van Aalten, D.M. Natural product family 18 chitinase inhibitors. Nat. Prod. Rep. 2005, 22, 563–579. [Google Scholar] [CrossRef] [PubMed]
- Imai, Y.; Tsuda, T.; Aochi, S.; Futatsugi-Yumikura, S.; Sakaguchi, Y.; Nakagawa, N.; Iwatsuki, K.; Yamanishi, K. YKL-40 (chitinase 3-like-1) as a biomarker for psoriasis vulgaris and pustular psoriasis. J. Dermatol. Sci. 2011, 64, 75–77. [Google Scholar] [CrossRef] [PubMed]
- Tan, A.L.; Benjamin, M.; Toumi, H.; Grainger, A.J.; Tanner, S.F.; Emery, P.; McGonagle, D. The relationship between the extensor tendon enthesis and the nail in distal interphalangeal joint disease in psoriatic arthritis--a high-resolution MRI and histological study. Rheumatology 2007, 46, 253–256. [Google Scholar] [CrossRef] [PubMed]
- Aydin, S.Z.; Castillo-Gallego, C.; Ash, Z.R.; Marzo-Ortega, H.; Emery, P.; Wakefield, R.J.; Wittmann, M.; McGonagle, D. Ultrasonographic assessment of nail in psoriatic disease shows a link between onychopathy and distal interphalangeal joint extensor tendon enthesopathy. Dermatology 2012, 225, 231–235. [Google Scholar] [CrossRef] [PubMed]
- Sandre, M.K.; Rohekar, S. Psoriatic arthritis and nail changes: Exploring the relationship. Semin. Arthritis Rheum. 2014, 44, 162–169. [Google Scholar] [CrossRef] [PubMed]
- Skroza, N.; Proietti, I.; Pampena, R.; La Viola, G.; Bernardini, N.; Nicolucci, F.; Tolino, E.; Zuber, S.; Soccodato, V.; Potenza, C. Correlations between psoriasis and inflammatory bowel diseases. BioMed Res. Int. 2013, 2013, 983902. [Google Scholar] [CrossRef]
- Schons, K.R.; Beber, A.A.; Beck Mde, O.; Monticielo, O.A. Nail involvement in adult patients with plaque-type psoriasis: Prevalence and clinical features. An. Bras. Dermatol. 2015, 90, 314–319. [Google Scholar] [CrossRef]
- Lombardi, G.; Perego, S.; Sansoni, V.; Diani, M.; Banfi, G.; Altomare, G. Anti-adalimumab antibodies in psoriasis: Lack of clinical utility and laboratory evidence. BMJ Open 2016, 6, e011941. [Google Scholar] [CrossRef]
- Sobolewski, P.; Walecka, I.; Dopytalska, K. Nail involvement in psoriatic arthritis. Reumatologia 2017, 55, 131–135. [Google Scholar] [CrossRef]
- Nwomeh, B.C.; Liang, H.X.; Diegelmann, R.F.; Cohen, I.K.; Yager, D.R. Dynamics of the matrix metalloproteinases MMP-1 and MMP-8 in acute open human dermal wounds. Wound Repair Regen. 1998, 6, 127–134. [Google Scholar] [CrossRef] [PubMed]
- Mezentsev, A.; Nikolaev, A.; Bruskin, S. Matrix metalloproteinases and their role in psoriasis. Gene 2014, 540, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Hitchon, C.A.; Danning, C.L.; Illei, G.G.; El-Gabalawy, H.S.; Boumpas, D.T. Gelatinase expression and activity in the synovium and skin of patients with erosive psoriatic arthritis. J. Rheumatol. 2002, 29, 107–117. [Google Scholar]
- Ritchlin, C. Psoriatic disease-from skin to bone. Nat. Clin. Pract. Rheumatol. 2007, 3, 698–706. [Google Scholar] [CrossRef] [PubMed]
- Alenius, G.M.; Jonsson, S.; Wallberg Jonsson, S.; Ny, A.; Rantapaa Dahlqvist, S. Matrix metalloproteinase 9 (MMP-9) in patients with psoriatic arthritis and rheumatoid arthritis. Clin. Exp. Rheumatol. 2001, 19, 760. [Google Scholar] [PubMed]
- Palazzi, C.; Lubrano, E.; D’Angelo, S.; Olivieri, I. Beyond early diagnosis: Occult psoriatic arthritis. J. Rheumatol. 2010, 37, 1556–1558. [Google Scholar] [CrossRef] [PubMed]
- Schoels, M.M.; Aletaha, D.; Alasti, F.; Smolen, J.S. Disease activity in psoriatic arthritis (PsA): Defining remission and treatment success using the DAPSA score. Ann. Rheum. Dis. 2016, 75, 811–818. [Google Scholar] [CrossRef]
- Garrett, S.; Jenkinson, T.; Kennedy, L.G.; Whitelock, H.; Gaisford, P.; Calin, A. A new approach to defining disease status in ankylosing spondylitis: The Bath Ankylosing Spondylitis Disease Activity Index. J. Rheumatol. 1994, 21, 2286–2291. [Google Scholar]
- Healy, P.J.; Helliwell, P.S. Measuring clinical enthesitis in psoriatic arthritis: Assessment of existing measures and development of an instrument specific to psoriatic arthritis. Arthritis Rheum. 2008, 59, 686–691. [Google Scholar] [CrossRef]
- Helliwell, P.S.; Firth, J.; Ibrahim, G.H.; Melsom, R.D.; Shah, I.; Turner, D.E. Development of an assessment tool for dactylitis in patients with psoriatic arthritis. J. Rheumatol. 2005, 32, 1745–1750. [Google Scholar]
- Rich, P.; Scher, R.K. Nail Psoriasis Severity Index: A useful tool for evaluation of nail psoriasis. J. Am. Acad. Dermatol. 2003, 49, 206–212. [Google Scholar] [CrossRef]
- Damiani, G.; Franchi, C.; Pigatto, P.; Altomare, A.; Pacifico, A.; Petrou, S.; Leone, S.; Pace, M.C.; Fiore, M. Outcomes assessment of hepatitis C virus-positive psoriatic patients treated using pegylated interferon in combination with ribavirin compared to new Direct-Acting Antiviral agents. World J. Hepatol. 2018, 10, 329–336. [Google Scholar] [CrossRef] [PubMed]
- Adawi, M.; Damiani, G.; Bragazzi, N.L.; Bridgewood, C.; Pacifico, A.; Conic, R.R.Z.; Morrone, A.; Malagoli, P.; Pigatto, P.D.M.; Amital, H.; et al. The Impact of Intermittent Fasting (Ramadan Fasting) on Psoriatic Arthritis Disease Activity, Enthesitis, and Dactylitis: A Multicentre Study. Nutrients 2019, 11, 601. [Google Scholar] [CrossRef] [PubMed]
- Damiani, G.; Watad, A.; Bridgewood, C.; Pigatto, P.D.M.; Pacifico, A.; Malagoli, P.; Bragazzi, N.L.; Adawi, M. The Impact of Ramadan Fasting on the Reduction of PASI Score, in Moderate-To-Severe Psoriatic Patients: A Real-Life Multicenter Study. Nutrients 2019, 11, 277. [Google Scholar] [CrossRef] [PubMed]
- Kocic, H.; Damiani, G.; Stamenkovic, B.; Tirant, M.; Jovic, A.; Tiodorovic, D.; Peris, K. Dietary compounds as potential modulators of microRNA expression in psoriasis. Ther. Adv. Chronic Dis. 2019, 10. [Google Scholar] [CrossRef]

| Variables | Total Cases (n = 100) | Ps Group (n = 50) | PsA Group (n = 50) | CTRL Group (n = 20) |
|---|---|---|---|---|
| Age median (IQR), years | 49 (19–82) | 48 (19–82) | 48 (28–79) | 48 (29–67) |
| Female, n (%) | 28 (28) | 17 (34) | 11 (22) | 10 (50) |
| Male, n (%) | 72 (72) | 33 (66) | 39 (78) | 10 (50) |
| BMI median (IQR), kg/m2 | 25 (23–28) | 25 (23–29) | 26 (23–28) | 24 (22–25) |
| Ps duration median (IQR), months | 195 (83–319) | 200 (67–347) | 195 (110–317) | - |
| Eruptive/stable Ps, (n) | - | 39/11 | - | |
| PsA duration median (IQR), months | - | - | 25 (4–110) | - |
| PASI median (IQR) | 5 (2–8) | 6 (5–12) | 4 (1–7) | - |
| Onychopathy (n) | 43 | 19 | 24 | - |
| Non systemic therapy (n) | 64 | 31 | 33 | - |
| Systemic therapy (n) | 36 | 19 | 17 | - |
| Acitretin (n) (dose) | 1 (20 mg/die) | 1 (20 mg/die) | 0 | - |
| CsA (n) (dose) | 6 (237.5 (221.3–257.5) mg/die) | 5 (250 (220–260) mg/die) | 1 (225 mg/die) | - |
| MTX (n) (dose) | 28 (15 (15–17.5) mg/week) | 13 (15 (15–17.5) mg/die) | 15 (15 (15–16.25) mg/die) | - |
| Systemic prednisone (n) (dose) | 1 (10 mg/die) | - | 1 (10 mg/die) | - |
| Markers | CTRL Group (n = 20) | Ps Group (n = 50) | PsA Group (n = 50) | CTRL vs. Ps p-Value | CTRL vs. PsA p-Value |
|---|---|---|---|---|---|
| MMP1 (pg/mL) | 35.00 (35.00–35.00) | 471.20 (159.10–1033.00) | 608.00 (35.00–1266.00) | p < 0.001 ⇑ | p = 0.001 ⇑ |
| MMP2 (ng/mL) | 91.70 (74.58–102.26) | 21.18 (7.8–76.60) | 16.52 (4.75–78.11) | p < 0.001 ⇓ | p < 0.001 ⇓ |
| MMP3 (ng/mL) | 6.27 (3.10–11.67) | 2.39 (1.14–4.93) | 2.29 (0.74–4.44) | n.s | n.s |
| MMP7 (ng/mL) | 0.86 (0.47–1.16) | 0.42 (0.22–1.08) | 0.38 (0.19–1.31) | n.s | n.s |
| MMP8 (ng/mL) | 0.61 (0.51–0.71) | 1.35 (0.83–3.01) | 1.32 (0.71–3.15) | p = 0.001 ⇑ | p = 0.009 ⇑ |
| MMP9 (ng/mL) | 0.83 (0.61–1.25) | 8.22 (3.31–11.72) | 6.59 (3.35–11.63) | p < 0.001 ⇑ | p < 0.001 ⇑ |
| MMP10 (pg/mL) | 1.60 (1.60–1.60) | 317 (1.60–824.30) | 257.47 (1.60–541.60) | p < 0.001 ⇑ | p < 0.001 ⇑ |
| MMP12 (pg/mL) | 1.00 (1.00–444.20) | 86.63 (11.76–165.40) | 76.99 (7.65–144.10) | n.s | n.s |
| MMP13 (pg/mL) | 4.90 (4.90–4.90) | 24.8 5(4.90–63.21) | 4.90 (4.90–49.19) | p = 0.004 ⇑ | n.s |
| TIMP1 (ng/mL) | 78.74 (66.65–109.45) | 101.19 (17.17–114.69) | 85.53 (17.71–113.35) | n.s | n.s |
| TIMP2 (ng/mL) | 90.71 (72.38–105.16) | 70.77 (10.09–83.73) | 59.83 (8.91–76.81) | p = 0.011 ⇓ | p < 0.001 ⇓ |
| TIMP3 (ng/mL) | 0.09 (0.09–1.66) | 8.79 (0.76–10.73) | 6.98 (0.61–9.17) | p < 0.001 ⇑ | p < 0.001 ⇑ |
| TIMP4 (pg/mL) | 1072.75 (701.90–1934.00) | 27.11 (1.70–320.90) | 1.70 (1.70–175.20) | p < 0.001 ⇓ | p < 0.001 ⇓ |
| OPG (pmol/L) | 6.46 (3.83–8.51) | 5.58 (4.23–6.99) | 5.67 (4.51–6.95) | n.s | n.s |
| RANKL (pmol/L) | 393.95 (295.50–943.00) | 148.20 (81.75–293.20) | 165.40 (86.79–235.20) | p < 0.001 ⇓ | p < 0.001 ⇓ |
| PINP (ng/mL) | 46.17 (33.55–62.88) | 5.94 (5.01–7.40) | 7.08 (4.87–8.22) | p < 0.001 ⇓ | p < 0.001 ⇓ |
| CTx-I (ng/mL) | 1.70 (1.38–2.14) | 0.55 (0.44–0.61) | 0.51 (0.40–0.62) | p < 0.001 ⇓ | p < 0.001 ⇓ |
| CTx-II (ng/mL) | 0.25 (0.19–0.29) | 0.26 (0.20–0.31) | 0.26 (0.20–0.30) | n.s | n.s |
| DKK1 (ng/mL) | 0.27 (0.23–0.37) | 2.79 (2.30–3.74) | 2.80 (2.02–3.53) | p < 0.001 ⇑ | p < 0.001 ⇑ |
| SOST (pg/mL) | 55.17 (35.37–97.10) | 147.95 (111.20–186.70) | 154.20 (126.90–196.60) | p < 0.001 ⇑ | p < 0.001 ⇑ |
| CHI3L1 (pg/mL) | 70.19 (31.87–118.80) | 65.98 (47.81–107.00) | 83.11 (47.33–114.90) | n.s | n.s |
| Markers | Ps Duration | PsA Duration | Ps PASI | PsA PASI | ||||
|---|---|---|---|---|---|---|---|---|
| p | r | p | r | p | r | p | r | |
| MMP1 | 0.486 | −0.10 | 0.790 | −0.04 | 0.216 | 0.18 | 0.647 | 0.07 |
| MMP2 | 0.001 | 0.46 | 0.929 | 0.01 | 0.322 | −0.14 | 0.205 | −0.18 |
| MMP3 | 0.549 | 0.09 | 0.458 | 0.11 | 0.459 | −0.11 | 0.829 | −0.03 |
| MMP7 | 0.651 | 0.07 | 0.120 | −0.23 | 0.316 | 0.14 | 0.746 | −0.05 |
| MMP8 | 0.177 | 0.19 | 0.098 | −0.24 | 0.040 | 0.29 | 0.054 | 0.27 |
| MMP9 | 0.630 | 0.07 | 0.306 | −0.15 | 0.257 | 0.16 | 0.226 | 0.17 |
| MMP10 | 0.876 | 0.02 | 0.025 | −0.32 | 0.004 | 0.40 | 0.057 | 0.27 |
| MMP12 | 0.001 | 0.45 | 0.418 | −0.12 | 0.372 | −0.13 | 0.313 | −0.15 |
| MMP13 | 0.010 | 0.36 | 0.392 | −0.13 | 0.667 | −0.06 | 0.781 | −0.04 |
| TIMP1 | 0.016 | 0.34 | 0.049 | −0.29 | 0.935 | 0.01 | 0.361 | −0.13 |
| TIMP2 | 0.037 | 0.30 | 0.203 | −0.19 | 0.871 | 0.02 | 0.372 | −0.13 |
| TIMP3 | 0.042 | 0.29 | 0.087 | −0.25 | 0.946 | 0.01 | 0.709 | −0.05 |
| TIMP4 | 0.065 | 0.26 | 0.052 | 0.28 | 0.041 | −0.29 | 0.497 | −0.10 |
| OPG | 0.341 | 0.14 | 0.176 | 0.20 | 0.067 | −0.26 | 0.448 | −0.11 |
| RANKL | 0.335 | −0.14 | 0.616 | −0.07 | 0.450 | −0.11 | 0.680 | 0.06 |
| PINP | 0.571 | −0.08 | 0.638 | −0.07 | 0.999 | 0.00 | 0.480 | 0.10 |
| CTX-I | 0.215 | −0.18 | 0.341 | 0.14 | 0.048 | 0.28 | 0.440 | 0.11 |
| CTX-II | 0.398 | 0.12 | 0.956 | −0.01 | 0.124 | −0.22 | 0.161 | −0.20 |
| DKK1 | 0.233 | 0.17 | 0.684 | −0.06 | 0.474 | −0.10 | 0.985 | 0.00 |
| SOST | 0.015 | 0.34 | 0.343 | −0.14 | 0.286 | −0.15 | 0.421 | −0.12 |
| CHI3L1 | 0.010 | 0.36 | 0.384 | 0.13 | 0.284 | −0.15 | 0.596 | 0.08 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Diani, M.; Perego, S.; Sansoni, V.; Bertino, L.; Gomarasca, M.; Faraldi, M.; Pigatto, P.D.M.; Damiani, G.; Banfi, G.; Altomare, G.; et al. Differences in Osteoimmunological Biomarkers Predictive of Psoriatic Arthritis among a Large Italian Cohort of Psoriatic Patients. Int. J. Mol. Sci. 2019, 20, 5617. https://doi.org/10.3390/ijms20225617
Diani M, Perego S, Sansoni V, Bertino L, Gomarasca M, Faraldi M, Pigatto PDM, Damiani G, Banfi G, Altomare G, et al. Differences in Osteoimmunological Biomarkers Predictive of Psoriatic Arthritis among a Large Italian Cohort of Psoriatic Patients. International Journal of Molecular Sciences. 2019; 20(22):5617. https://doi.org/10.3390/ijms20225617
Chicago/Turabian StyleDiani, Marco, Silvia Perego, Veronica Sansoni, Lucrezia Bertino, Marta Gomarasca, Martina Faraldi, Paolo Daniele Maria Pigatto, Giovanni Damiani, Giuseppe Banfi, Gianfranco Altomare, and et al. 2019. "Differences in Osteoimmunological Biomarkers Predictive of Psoriatic Arthritis among a Large Italian Cohort of Psoriatic Patients" International Journal of Molecular Sciences 20, no. 22: 5617. https://doi.org/10.3390/ijms20225617
APA StyleDiani, M., Perego, S., Sansoni, V., Bertino, L., Gomarasca, M., Faraldi, M., Pigatto, P. D. M., Damiani, G., Banfi, G., Altomare, G., & Lombardi, G. (2019). Differences in Osteoimmunological Biomarkers Predictive of Psoriatic Arthritis among a Large Italian Cohort of Psoriatic Patients. International Journal of Molecular Sciences, 20(22), 5617. https://doi.org/10.3390/ijms20225617







