Development of Bone Targeting Drugs
Abstract
:1. Overview
2. Targeting Strategies
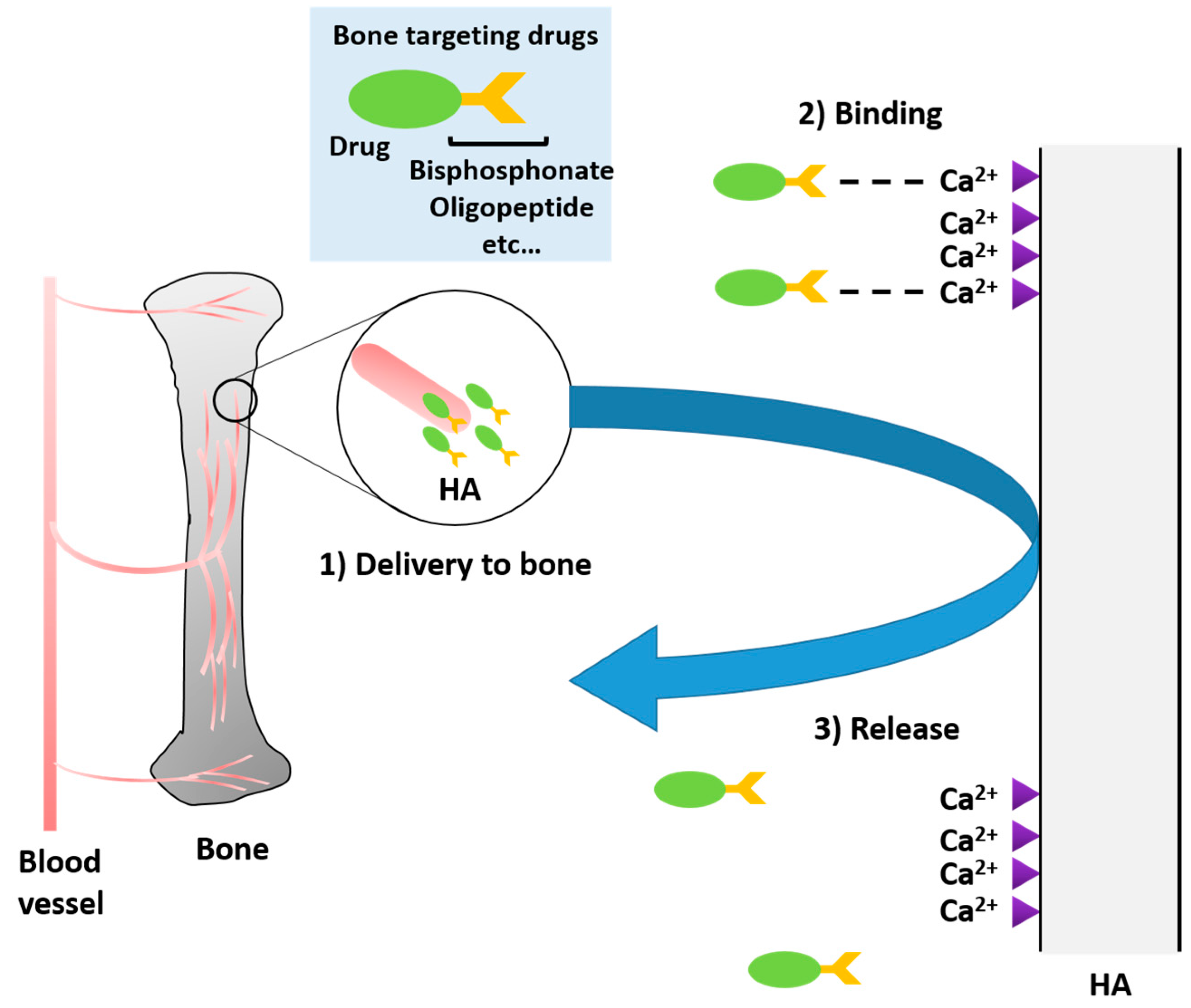
2.1. Bone-Targeting
2.1.1. Bisphosphonates
Bisphosphonates to Target Proteins
Bisphosphonates to Target Nanoparticles
2.1.2. Tetracyclines
2.1.3. Polymeric Amino Acid Targeting
2.1.4. Calcium Phosphate Biomaterials
2.2. Bone Cell-Specific Targeting
2.2.1. Osteoblast Targeting
2.2.2. Osteoclast Targeting
2.2.3. Targeting with Bone Marrow Stromal Cells (BMSCs)
3. Limitations and Perspective
4. Impact and Significance of Bone Targeting on Specific Disease Burdens
4.1. Infectious Disease
4.1.1. Acidic Oligopeptide-Modified Drug for Infectious Disease
4.1.2. BP-Modified Drug for Infectious Disease
4.2. Osteoporosis
4.2.1. Acidic Oligopeptide-Modified Drug for Osteoporosis
4.2.2. BP-Modified Drug for Osteoporosis
4.3. Rheumatoid Arthritis
4.4. Metabolic Skeletal Dysplasia
5. Future Directions
6. Conclusions
Acknowledgments
Conflicts of Interest
References
- Wang, X.; Lai, Y.; Ng, H.H.; Yang, Z.; Qin, L. Systemic drug delivery systems for bone tissue regeneration—A mini review. Curr. Pharm. Des. 2015, 21, 1575–1583. [Google Scholar]
- Russell, R.; Graham, G. BPs: The first 40 years. Bone 2011, 49, 2–19. [Google Scholar] [CrossRef] [PubMed]
- Pistone, A.; Iannazzo, D.; Espro, C.; Galvagno, S.; Tampieri, A.; Montesi, M.; Pansweri, S.; Sandri, M. Tethering of Gly-Arg-Gly-Asp-Ser-Pro-Lys peptides on Mg-Doped Hydroxyapatite. Engineering 2017, 3, 55–59. [Google Scholar] [CrossRef]
- Pistone, A.; Iannazzo, D.; Panseri, S.; Montesi, M.; Tampieri, A.; Galvagno, S. Hydroxyapatitet-magnetite-MWCNT nanocomposite as biocompatible multifunctional drug delivery system for bone tissue engineering. Nanotechnology 2014, 24, 425701. [Google Scholar] [CrossRef] [PubMed]
- Fleisch, H.; Russell, R.G.; Francis, M.D. Diphosphonates Inhibit Hydroxyapatite Dissolution in Vitro and Bone Resorption in Tissue Culture and in Vivo. Science 1969, 165, 1262–1264. [Google Scholar] [CrossRef] [PubMed]
- Iannazzo, D.; Pistone, A.; Espro, C.; Galvagno, S. Drug delivery strategies for bone tissue regeneration. In Biomimetic Approaches for Tissue Healing; Panseri, S., Taraballi, F., Cunha, C., Eds.; OMICS Group eBooks: Foster City, CA, USA, 2015; pp. 1–39. [Google Scholar]
- Hengst, V.C.; Kissel, O.T.; Storm, G. Bone targeting potential of BP-targeted liposomes: Preparation, characterization and hydroxyapatite binding in vitro. Int. J. Pharm. 2007, 331, 224–227. [Google Scholar] [CrossRef] [PubMed]
- Rodan, G.A.; Fleisch, H.A. BPs: Mechanisms of action. J. Clin. Investig. 1996, 97, 2692. [Google Scholar] [CrossRef] [PubMed]
- Reszka, A.A.; Rodan, G.A. BP mechanism of action. Curr. Rheumatol. Rep. 2003, 5, 65–74. [Google Scholar] [CrossRef] [PubMed]
- Fleisch, H. BPs: Mechanisms of action. Endocr. Rev. 1998, 19, 80–100. [Google Scholar] [CrossRef] [PubMed]
- Kennel, K.A.; Drake, M.T. Adverse effects of BPs: Implications for osteoporosis management. Mayo Clin. Proc. 2009, 84, 632–638. [Google Scholar] [CrossRef]
- Fleisher, K.E.; Welch, G.; Kottal, S.; Craig, R.G.; Saxena, D.; Glickman, R.S. Predicting risk for bisphosphonate-related osteonecrosis of the jaws: CTX versus radiographic markers. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 2010, 110, 509–516. [Google Scholar] [CrossRef] [PubMed]
- Katsumi, H.; Sano, J.; Nishikawak, M.; Hanzawa, K.; Sakane, T.; Yamamoto, A. Molecular design of BP-modified proteins for efficient bone targeting in vivo. PLoS ONE 2015, 10, e0135966. [Google Scholar] [CrossRef] [PubMed]
- Rawat, P.; Ahmad, I.; Thomas, S.C.; Pandey, S.; Vohora, D.; Gupta, S.; Ahmad, F.J.; Talegaonkar, S. Revisiting bone targeting potential of novel hydroxyapatite based surface modified PLGA nanoparticles of risedronate: Pharmacokinetic and biochemical assessment. Int. J. Pharm. 2016, 506, 253–261. [Google Scholar] [CrossRef] [PubMed]
- Salerno, M.; Cenni, E.; Fotia, C.; Avnet, S.; Granchi, D.; Castelli, F.; Micieli, D.; Pignatello, R.; Capulli, M.; Rucci, N.; et al. Bone-targeted doxorubicin-loaded nanoparticles as a tool for the treatment of skeletal metastases. Curr. Cancer Drug Targets 2010, 10, 649–659. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Liu, J.; Tao, S.; Chai, G.H.; Wang, J.W.; Hu, F.Q.; Yuan, H. Tetracycline-grafted PLGA nanoparticles as bone-targeting drug delivery system. Int. J. Nanomed. 2015, 10, 5671. [Google Scholar]
- Wang, G.; Li, W.; Nawaz, W.; Liao, X.; Yang, M.Q.; Zhang, L.; Khan, F.U.; Qi, X.; Chen, D.; Wang, Z.; et al. Efficacy of a Novel Epicardium Drug Delivery System for Bone Marrow Stem Cells Treating Heart Failure After Myocardial Infarction. Insights Stem Cells 2016, 2, 2. [Google Scholar]
- Shen, C.; Han, Y.; Tang, J.; Wang, B.; Lin, Q. Bone targeting study of tetracycline grafted PLGA nanoparticles drug delivery system. Nanomedicine 2016, 12, 487. [Google Scholar] [CrossRef]
- Reichert, J.C.; Cipitria, A.; Epari, D.R.; Saifzadeh, S.; Krishnakanth, P.; Berner, A.; Woodruff, M.A.; Schell, H.; Mehta, M.; Schuetz, M.A. A tissue engineering solution for segmental defect regeneration in load-bearing long bones. Sci. Transl. Med. 2012, 4, 141ra93. [Google Scholar] [CrossRef] [PubMed]
- Jeon, O.H.; Elisseeff, J. Orthopedic tissue regeneration: Cells, scaffolds, and small molecules. Drug Deliv. Transl. Res. 2016, 6, 105–120. [Google Scholar] [CrossRef] [PubMed]
- Shih, Y.V.; Hwang, Y.; Phadke, A.; Kang, H.; Hwang, N.S.; Caro, E.J.; Nguyen, S.; Siu, M.; Throdorakis, E.A.; Hianneschi, N.C.; et al. Calcium phosphate-bearing matrices induce osteogenic differentiation of stem cells through adenosine signaling. Proc. Natl. Acad. Sci. USA 2014, 111, 990–995. [Google Scholar] [CrossRef] [PubMed]
- Chen, F.; Huang, P.; Zhu, Y.J.; Wu, J.; Cui, D.X. Multifunctional Eu3+/Gd3+ dual-doped calcium phosphate vesicle-like nanospheres for sustained drug release and imaging. Biomaterials 2012, 33, 6447–6455. [Google Scholar] [CrossRef] [PubMed]
- Heinegård, D.; Oldberg, A. Structure and biology of cartilage and bone matrix noncollagenous macromolecules. FASEB J. 1989, 3, 2042–2051. [Google Scholar] [PubMed]
- Cao, X. Targeting osteoclast-osteoblast communication. Nat. Med. 2011, 17, 1344. [Google Scholar] [CrossRef] [PubMed]
- Sun, Y.; Ye, X.; Cai, M.; Liu, X.; Xiao, J.; Zhang, C.; Wang, Y.; Yang, L.; Liu, J.; Li, S.; et al. Osteoblast-Targeting-Peptide Modified Nanoparticle for siRNA/microRNA Delivery. ACS Nano 2016, 10, 5759–5768. [Google Scholar] [CrossRef] [PubMed]
- Bassit, A.C.; Moffat, P.; Gaumond, M.; Hamdy, R. The potential use of nanoparticles for noggin siRNA delivery to accelerate bone formation in distraction osteogenesis. J. Nanomed. Nanotechnol. 2015, 6, 1. [Google Scholar]
- Liang, C.; Guo, B.; Wu, H.; Shao, N.; Li, D.; Liu, J.; Dang, L.; Wang, C.; Li, H.; Li, S. Aptamer-functionalized lipid nanoparticles targeting osteoblasts as a novel RNA interference-based bone anabolic strategy. Nat. Med. 2015, 21, 288–294. [Google Scholar] [CrossRef] [PubMed]
- Liu, X. Bone site-specific delivery of siRNA. J. Biomed. Res. 2016, 30, 264. [Google Scholar] [PubMed]
- Smith, M.R. Osteoclast targeted therapy for prostate cancer: BPs and beyond. Urol. Oncol. 2008, 26, 420–425. [Google Scholar] [CrossRef] [PubMed]
- Edwards, J.R.; Weivoda, M.M. Osteoclasts: Malefactors of disease and targets for treatment. Discov. Med. 2012, 13, 201–210. [Google Scholar] [PubMed]
- Derubeis, A.R.; Cancedda, R. Bone marrow stromal cells (BMSCs) in bone engineering: Limitations and recent advances. Ann. Biomed. Eng. 2004, 32, 160–165. [Google Scholar] [CrossRef] [PubMed]
- Wang, D.; Miller, S.C.; Kopečková, P. Bone-targeting macromolecular therapeutics. Adv. Drug Deliv. Rev. 2005, 57, 1049–1076. [Google Scholar] [CrossRef] [PubMed]
- Pontikoglou, C.; Deschaseaux, F.; Sensebé, L.; Papadaki, H.A. Bone marrow mesenchymal stem cells: Biological properties and their role in hematopoiesis and hematopoietic stem cell transplantation. Stem Cell Rev. Rep. 2011, 7, 569–589. [Google Scholar] [CrossRef] [PubMed]
- Yang, F.; Leung, V.Y.; Luk, K.D.; Chan, D.; Cheung, K.M. Mesenchymal stem cells arrest intervertebral disc degeneration through chondrocytic differentiation and stimulation of endogenous cells. Mol. Ther. 2009, 17, 1959–1966. [Google Scholar] [CrossRef] [PubMed]
- Pillinger, G.; Loughran, N.V.; Piddock, R.E.; Shafat, M.S.; Zaitseva, L.; Abdul-Aziz, A.; Lawes, M.J.; Bowles, K.M.; Rushworth, S.A. Targeting PI3Kδ and PI3Kγ signalling disrupts human AML survival and bone marrow stromal cell mediated protection. Oncotarget 2016, 7, 39784–39795. [Google Scholar] [PubMed]
- Sekiya, I.; Larson, B.L.; Vuoristo, J.T.; Cui, J.G.; Prockop, D.J. Adipogenic differentiation of human adult stem cells from bone marrow stroma (MSCs). J. Bone Miner. Res. 2004, 19, 256–264. [Google Scholar] [CrossRef] [PubMed]
- Xie, H.; Sun, L.; Zhang, L.; Liu, T.; Chen, L.; Zhao, A.; Lei, Q.; Gao, F.; Zou, P.; Li, Q..; et al. Mesenchymal Stem Cell-Derived Macrovesicles Support Ex Vivo Expansion of Cord Blood-Derived CD34+ Cells. Stem Cells Int. 2016. [Google Scholar] [CrossRef] [PubMed]
- Rehman, F.U.; Zhao, C.; Wu, C.; Li, X.; Jiang, H.; Selke, M.; Wang, X. Synergy and translation of allogenic bone marrow stem cells after photodynamic treatment of rheumatoid arthritis with tetra sulfonatophenyl porphyrin and TiO2 nanowhiskers. Nano Res. 2016, 9, 3305–3321. [Google Scholar] [CrossRef]
- Feng, X.; Liu, X.; Cai, X.; Lin, T.; Xu, W.; Yang, C.; Liu, Y.; Yang, S.; Fu, D. The Influence of Tetracycline Inducible Targeting Rat PPARγ Gene Silencing on the Osteogenic and Adipogenic Differentiation of Bone Marrow Stromal Cells. Curr. Pharm. Des. 2016, 22, 6330. [Google Scholar] [CrossRef] [PubMed]
- Martin, J.; Grill, V. BPs–mechanisms of action. Aust. Prescr. 2000, 23, 130–132. [Google Scholar]
- Harwood, P.J.; Giannoudis, P.V. Application of bone morphogenetic proteins in orthopaedic practice: Their efficacy and side effects. Expert Opin. Drug Saf. 2005, 4, 75–89. [Google Scholar] [CrossRef] [PubMed]
- De Jong, W.H.; Borm, P. Drug delivery and nanoparticles: Applications and hazards. Int. J. Nanomed. 2008, 3, 133. [Google Scholar] [CrossRef]
- Ferreira, S.; Boratto, F.A.; Cardoso, V.N.; Serakides, R.; Fernandes, S.O.; Ferreira, L.A.; Oliveira, M.C. Alendronate-coated long-circulating liposomes containing 99 mtechnetium-ceftizoxime used to identify osteomyelitis. Int. J. Nanomed. 2015, 10, 2441–2450. [Google Scholar]
- Sekido, T.; Sakura, N.; Higashi, Y.; Miya, K.; Nitta, Y.; Nomura, M.; Sawanishi, H.; Morito, K.; Masamune, Y.; Kasugai, S.; et al. Novel drug delivery system to bone using acidic oligopeptide: Pharmacokinetic characteristics and pharmacological potential. J. Drug Target. 2001, 9, 111–121. [Google Scholar] [CrossRef] [PubMed]
- Yokogawa, K.; Miya, K.; Sekido, T.; Higashi, Y.; Nomura, M.; Fujisawa, R.; Morito, K.; Masamune, Y.; Waki, Y.; Kasugai, S.; Miyamoto, K. Selective delivery of estradiol to bone by aspartic acid oligopeptide and its effects on ovariectomized mice. Endocrinology 2001, 142, 1228–1233. [Google Scholar] [CrossRef] [PubMed]
- Cong, Y.; Quan, C.; Liu, M.; Kiu, J.; Huang, G.; Tong, G.; Yin, Y.; Zhang, C.; Jiang, Q. Alendronate-decorated biodegradable polymeric micelles for potential bone-targeted delivery of vancomycin. J. Biomater. Sci. Polym. Ed. 2015, 26, 629–643. [Google Scholar] [CrossRef] [PubMed]
- Choi, S.W.; Kim, J.H. Design of surface-modified poly (d,l-lactide-co-glycolide) nanoparticles for targeted drug delivery to bone. J. Controll. Release 2007, 122, 24–30. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Wei, L.; Miron, R.J.; Shi, B.; Bian, Z. Bone scaffolds loaded with siRNA-Semaphorin4d for the treatment of osteoporosis related bone defects. Sci. Rep. 2016, 2, 26925. [Google Scholar] [CrossRef] [PubMed]
- Dang, L. A delivery system specifically approaching bone resorption surfaces to facilitate therapeutic modulation of MicroRans in osteoclasts. Biomaterials 2016, 52, 148–160. [Google Scholar]
- Kokkola, R.; Sundberg, E.; Ulfgren, A.K.; Palmblad, K.; Li, J.; Wang, H.; Ulloa, L.; Yang, H.; Yan, X.J.; Furie, R.; et al. High mobility group box chromosomal protein 1: A novel proinflammatory mediator in synovitis. Arthritis Rheumatol. 2002, 46, 2598–2603. [Google Scholar] [CrossRef] [PubMed]
- Nishioka, T.; Tomatsu, S.; Gutierrez, M.A.; Miyamoto, K.; Trandafirescu, G.G.; Lopez, P.L.; Grubb, J.H.; Kanai, R.; Kobayashi, H.; Yamaguchi, S.; et al. Enhancement of drug delivery to bone: Characterization of human tissue-nonspecific alkaline phosphatase tagged with an acidic oligopeptide. Mol. Genet. Metab. 2006, 88, 244–255. [Google Scholar] [CrossRef] [PubMed]
- Whyte, M.P. Hypophosphatasia—aetiology, nosology, pathogenesis, diagnosis and treatment. Nat. Rev. Endocrinol. 2016, 12, 233–246. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, T.; Yokogawa, K.; Sakura, N.; Nomura, M.; Kobayashi, S.; Miyamoto, K. Bone-targeting of quinolones conjugated with an acidic oligopeptide. Pharm. Res. 2008, 25, 2881–2888. [Google Scholar] [CrossRef] [PubMed]
- Gil, L.; Han, Y.; Opas, E.E.; Rodan, G.A.; Ruel, R.; Seedor, J.G.; Tyler, P.C.; Young, R.N. Prostaglandin E2-BP conjugates: Potential agents for treatment of osteoporosis. Bioorg. Med. Chem. 1999, 7, 901–919. [Google Scholar] [CrossRef]
- Sedghizadeh, P.P.; Sun, S.; Junka, A.F.; Richard, E.; Sadrerafi, K.; Mahabady, S.; Bakhshalian, N.; Tjokro, N.; Bartoszewicz, M.; Oleksy, M.; et al. Design, synthesis, and antimicrobial evaluation of a novel bone-targeting BP-ciprofloxacin conjugate for the treatment of osteomyelitis biofilms. J. Med. Chem 2017, 1–18. [Google Scholar]
- Holmberg, A.R.; Lerner, U.H.; Alayia, A.A.; Al-Mohanna, M.; Adra, C.; Marquez, M.; Meurling, L.; Nilsson, S. Development of a novel poly BP conjugate for treatment of skeletal metastasis and osteoporosis. Int. J. Oncol. 2010, 37, 563–567. [Google Scholar] [CrossRef] [PubMed]
- Katsumi, H.; Takashima, M.; Sano, J.; Nishiyama, K.; Kitamura, N.; Sakane, T.; Hibi, T.; Yamamoto, A. Development of polyethylene glycol-conjugated alendronate, a novel nitrogen-containing BP derivative: Evaluation of absorption, safety, and effects after intrapulmonary administration in rats. J. Pharm. Sci. 2011, 100, 3783–3792. [Google Scholar] [CrossRef] [PubMed]
- Ossipov, D.A. BP-modified biomaterials for drug delivery and bone tissue engineering. Expert Opin. Drug Deliv. 2015, 12, 1443–1458. [Google Scholar] [CrossRef] [PubMed]
- Taniguchi, N.; Kawahara, K.I.; Yone, K.; Hashiguchi, T.; Yamakuchi, M.; Goto, M.; Inoue, K.; Yamada, S.; Ijiri, K.; Matsunaga, S.; et al. High mobility group box chromosomal protein 1 plays a role in the pathogenesis of rheumatoid arthritis as a novel cytokine. Arthritis Rheum. 2003, 48, 971–981. [Google Scholar] [CrossRef] [PubMed]
- Huttunen, H.J.; Kuja-Panula, J.; Rauvala, H. Receptor for advanced glycation end products (RAGE) signaling induces CREB-dependent chromogranin expression during neuronal differentiation. J. Biol. Chem. 2002, 277, 38635–38646. [Google Scholar] [CrossRef] [PubMed]
- Van Beijnum, J.R.; Buurman, W.A.; Griffioen, A.W. Convergence and amplification of toll-like receptor (TLR) and receptor for advanced glycation end products (RAGE) signaling pathways via high mobility group B1 (HMGB1). Angiogenesis 2008, 11, 91–99. [Google Scholar] [CrossRef] [PubMed]
- Frame, B.; Parfitt, A.M. Metabolic bone disease. Ann. Int. Med. 1972, 77, 655–656. [Google Scholar] [CrossRef]
- Allgrove, J. Metabolic bone disease. Paediatr. Child Health 2007, 17, 253–259. [Google Scholar] [CrossRef]
- Krakow, D.; Rimoin, D.L. The skeletal dysplasia’s. Genet. Med. 2010, 12, 327–341. [Google Scholar] [CrossRef] [PubMed]
- Pinhas, R.; Mays, S. Metabolic bone disease. In Advances in Human Paleopathology, 1st ed.; John Wiley & Sons Ltd.: Chichester, UK, 2008; pp. 215–251. [Google Scholar]
- Harris, P.E.; Bouloux, P.M.G. Metabolic bone disease. In Endocrinology in Clinical Practice, 2nd ed.; CRC Press: London, UK, 2014; pp. 243–261. [Google Scholar]
- Tomatsu, S.; Montaño, A.M.; Dung, V.C.; Ohashi, A.; Oikawa, H.; Oguma, T.; Orii, T.; Varrera, L.; Sly, W.S. Enhancement of drug delivery: Enzyme-replacement therapy for murine Morquio A syndrome. Mol. Ther. 2010, 18, 1094–1102. [Google Scholar] [CrossRef] [PubMed]
- Tomatsu, S.; Mackenzie, W.G.; Theroux, M.C.; Mason, R.W.; Thacker, M.M.; Shaffer, T.H.; Montano, A.M.; Rowan, D.; Sly, W.; Almeciga, C.J.; et al. Current and emerging treatments and surgical interventions for Morquio A Syndrome: A review. Res. Rep. Endocr. Disord. 2012, 2, 65–77. [Google Scholar] [CrossRef] [PubMed]
- Sawamoto, K.; Suzuki, Y.; Mackenzie, W.G.; Therouz, M.C.; Pizarro, C.; Yabe, H.; Orii, K.E.; Mason, R.W.; Orii, T.; Tomatsu, S. Current therapies for Morquio A syndrome and their clinical outcomes. Expert Opin. Orphan Drugs 2016, 4, 941–951. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Wei, L.; Miron, R.J.; Shi, B.; Bian, Z. Prevention of alveolar bone loss in an osteoporotic animal model via interference of semaphorin 4D. J. Dent. Res. 2014, 93, 1095–1100. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Wei, L.; Miron, R.J.; Shi, B.; Bian, Z. Anabolic bone formation via a site-specific bone-targeting delivery system by interfering with semaphorin 4D expression. J. Bone Miner. Res. 2015, 30, 286–296. [Google Scholar] [CrossRef] [PubMed]
| Targeting Moieties | Targeted Tissues | Specific Drugs and Moieties | Primary Limitations |
|---|---|---|---|
| Bisphosphonates [12,43,44,45] | All skeletal tissues | samarium-153, pamidronate, alendronate, risedronate | Cytotoxicity, osteonecrosis |
| Tetracycline derivatives [16,17,18] | All skeletal tissues | Estradiol | Lack of specificity, gastrointestinal distress |
| PLGA USAuNPs [19,46,47] | Cell-specific | Under review | Lack of understanding in mechanism, size restriction, inflammatory response |
| CKIP-1 [48,49] | Osteoblasts | CkIP-1 siRNA | Off target drug delivery and circulation time limitations |
| l-(asp)6, l-(glu)6 [50,51,52] | All bone tissue | CD6-TNSALP, CD8-TNSALP | Nonnative functioning, inadequate bone delivery |
| Calcium Phosphates (CaP’s) [26,31] | Resorption surfaces | b-TCP + copolymers PLA-DX-PEG,ACP/PLLA nanofibrous scaffold | Calcium toxicity from overabundance, osteosarcoma |
| SDSSD [24,25,26,27] | Osteoblasts | PTH 1-84, PTH 1-34 | Circulation time limitations |
| BMSC specific aptamer [35,36] | BMSCs | miR-188-3p antagomir | Circulation time limitations |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stapleton, M.; Sawamoto, K.; Alméciga-Díaz, C.J.; Mackenzie, W.G.; Mason, R.W.; Orii, T.; Tomatsu, S. Development of Bone Targeting Drugs. Int. J. Mol. Sci. 2017, 18, 1345. https://doi.org/10.3390/ijms18071345
Stapleton M, Sawamoto K, Alméciga-Díaz CJ, Mackenzie WG, Mason RW, Orii T, Tomatsu S. Development of Bone Targeting Drugs. International Journal of Molecular Sciences. 2017; 18(7):1345. https://doi.org/10.3390/ijms18071345
Chicago/Turabian StyleStapleton, Molly, Kazuki Sawamoto, Carlos J. Alméciga-Díaz, William G. Mackenzie, Robert W. Mason, Tadao Orii, and Shunji Tomatsu. 2017. "Development of Bone Targeting Drugs" International Journal of Molecular Sciences 18, no. 7: 1345. https://doi.org/10.3390/ijms18071345
APA StyleStapleton, M., Sawamoto, K., Alméciga-Díaz, C. J., Mackenzie, W. G., Mason, R. W., Orii, T., & Tomatsu, S. (2017). Development of Bone Targeting Drugs. International Journal of Molecular Sciences, 18(7), 1345. https://doi.org/10.3390/ijms18071345







