Hyaluronan: Sources, Structure, Features and Applications
Abstract
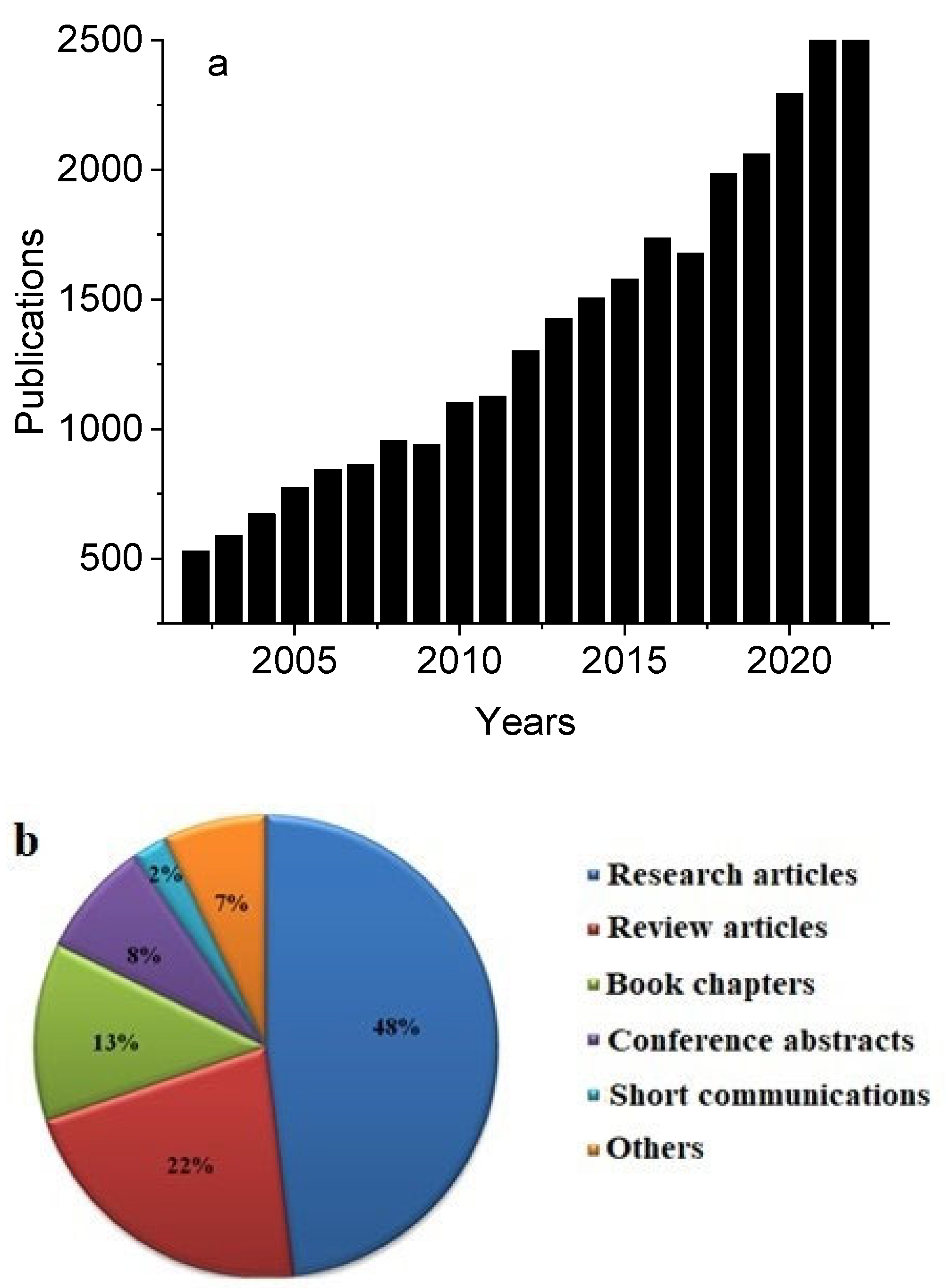
1. Introduction
2. Hyaluronan
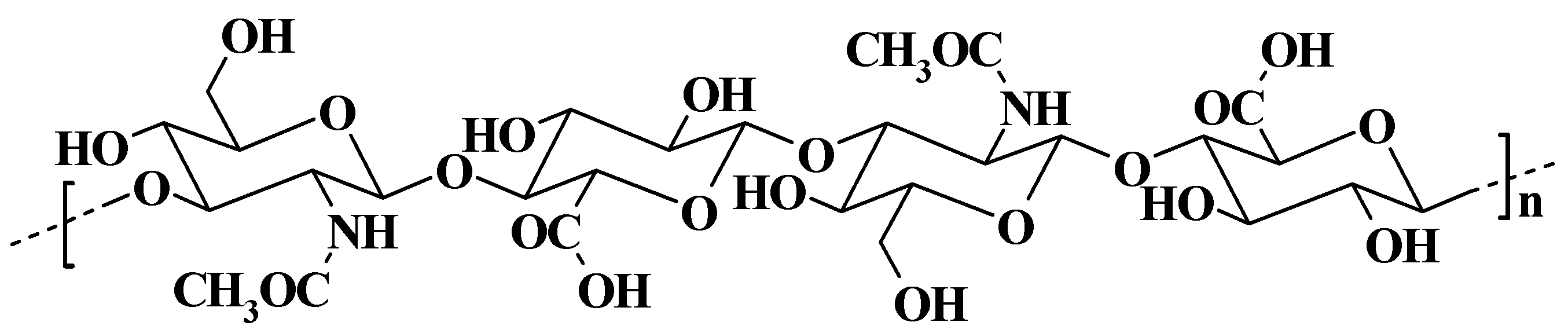
2.1. Structure and Properties of Hyaluronan
2.2. Sources of Hyaluronan
2.3. Modifications of Hyaluronan
3. Hyaluronan in Medical Practice
3.1. Hyaluronan in Dermal Filler
3.2. Hyaluronan in Tissue Engineering
3.3. Hyaluronan in Viscosupplementation
3.4. Hyaluronan in Ocular Treatment
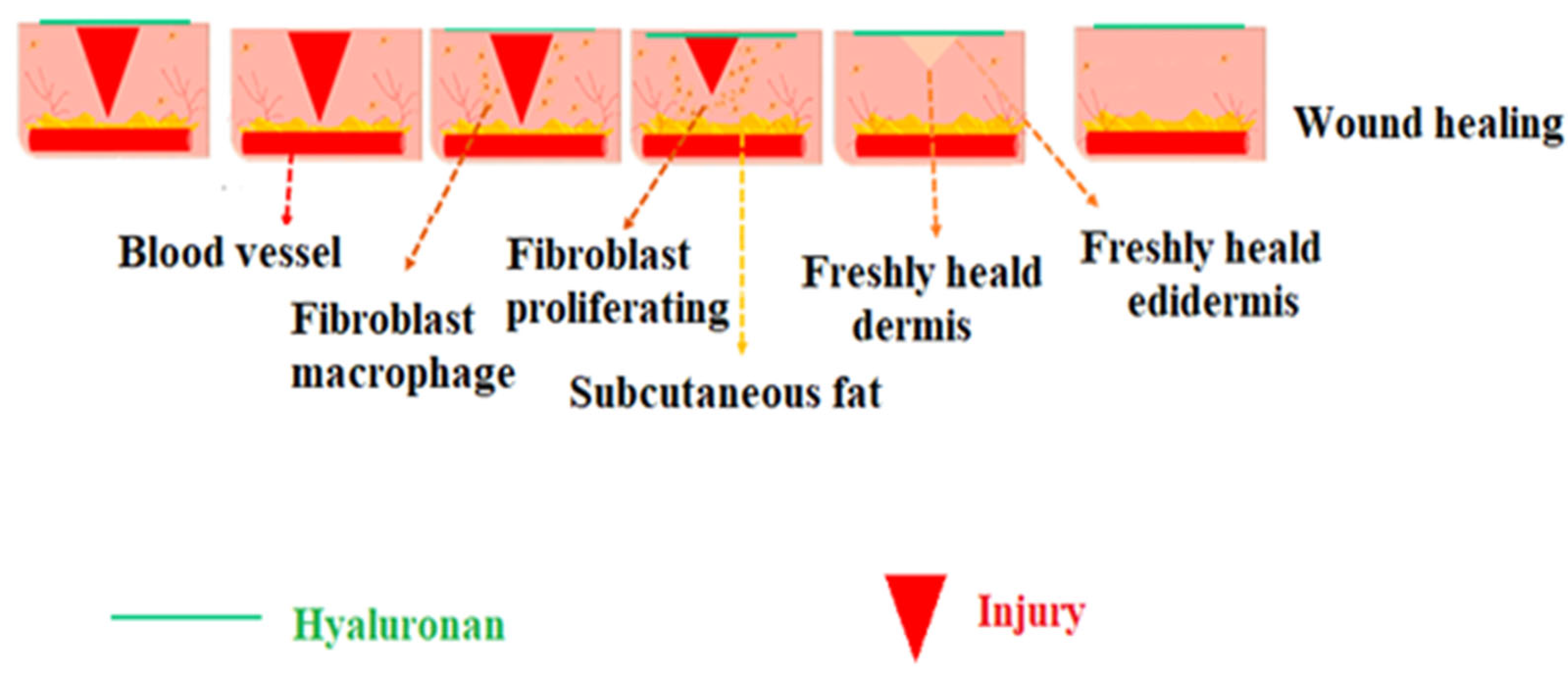
3.5. Hyaluronan in Wound Healing
3.6. Hyaluronan in Drug Delivery
3.7. Hyaluronan in Transdermal Drug Delivery
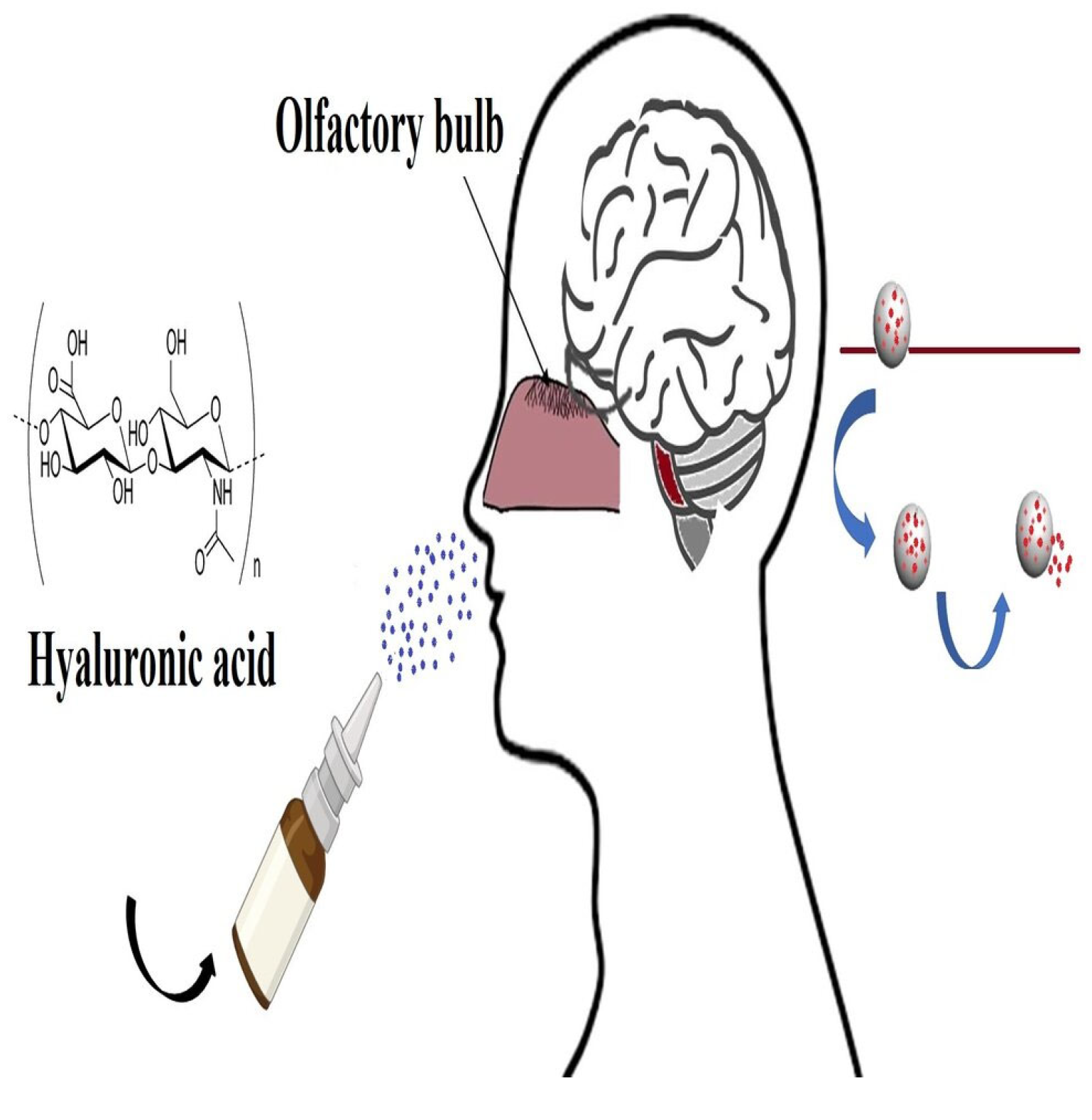
3.8. Hyaluronan in Nasal Drug Delivery
3.9. Hyaluronan in Colon Drug Delivery
3.10. Hyaluronan in Chemoprevention and Cancer Therapy
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mohammed, A.S.A.; Naveed, M.; Jost, N. Polysaccharides; classification, chemical properties, and future perspective applications in fields of pharmacology and biological medicine (A review of current applications and upcoming potentialities). J. Polym. Environ. 2021, 29, 2359–2371. [Google Scholar] [CrossRef] [PubMed]
- Hassan, M.E.; Bai, J.; Dou, D.Q. Biopolymers; definition, classification and applications. Egypt. J. Chem. 2019, 62, 1725–1737. [Google Scholar] [CrossRef]
- Ghlissi, Z.; Kallel, R.; Krichen, F.; Hakim, A.; Zeghal, K.; Boudawara, T.; Bougatef, A.; Sahnoun, Z. Polysaccharide from Pimpinella anisum seeds: Structural characterization, anti-inflammatory and laser burn wound healing in mice. Int. J. Biol. Macromol. 2020, 156, 1530–1538. [Google Scholar] [CrossRef]
- Das, H. An Overview on heteropolysaccharides. J. Glycobiol. 2022, 11, 210. [Google Scholar]
- Garantziotis, S.; Savani, R.C. Hyaluronan biology: A complex balancing act of structure, function, location and context. Matrix Biol. 2019, 78–79, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Johnson, P.; Arif, A.A.; Lee-Sayer, S.S.M.; Dong, Y. Hyaluronan and its interactions with immune cells in the healthy and inflamed lung. Front. Immunol. 2018, 9, 2787. [Google Scholar] [CrossRef] [PubMed]
- Meyer, K.; Palmer, J. The polysaccharide of the vitreous humor. J. Biol. Chem. 1935, 107, 629–634. [Google Scholar] [CrossRef]
- Csoka, A.B.; Stern, R. Hypotheses on the evolution of hyaluronan: A highly ironic acid. Glycobiology 2013, 23, 398–411. [Google Scholar] [CrossRef]
- Huang, G.; Huang, H. Application of hyaluronic acid as carriers in drug delivery. Drug Deliv. 2018, 25, 766–772. [Google Scholar] [CrossRef]
- Hrabárová, E.; Rychlý, J.; Sasinková, V.; Valachová, K.; Janigová, I.; Csomorová, K.; Juránek, I.; Šoltés, L. Structural characterisation of thiol-modified hyaluronans. Cellulose 2012, 19, 2093–2104. [Google Scholar] [CrossRef]
- Kogan, G.; Soltes, L.; Stern, R.; Gemeiner, P. Hyaluronic acid: A natural biopolymer with a broad range of biomedical and industrial applications. Biotechnol. Lett. 2007, 29, 17–25. [Google Scholar] [CrossRef] [PubMed]
- Jenkins, H.G.; Bachelard, H.S. Developmental and age-related changes in rat brain glycosaminoglycans. J. Neurochem. 1988, 51, 1634–1640. [Google Scholar] [CrossRef] [PubMed]
- Fraser, J.R.; Laurent, T.C.; Laurent, U.B. Hyaluronan: Its nature, distribution, functions and turnover. J. Intern. Med. 1997, 242, 27–33. [Google Scholar] [CrossRef] [PubMed]
- Valachová, K.; Volpi, N.; Stern, R.; Šoltés, L. Hyaluronan in medical practice. Curr. Med. Chem. 2016, 23, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Menaa, T.; Menaa, A.; Menaa, B. Hyaluronic acid and derivatives for tissue engineering. J. Biotechnol. Biomater. 2011, S3, 001. [Google Scholar]
- Burdick, J.A.; Prestwich, G.D. Hyaluronic acid hydrogels for biomedical applications. Adv. Mater. 2011, 23, 41–56. [Google Scholar] [CrossRef] [PubMed]
- Almond, A.; Sheehan, J.K. Predicting the molecular shape of polysaccharides from dynamic interactions with water. Glycobiology 2003, 13, 255–264. [Google Scholar] [CrossRef] [PubMed]
- Csapo, E.; Szokolai, H.; Juhasz, A.; Varga, N.; Janovak, L.; Dekany, I. Cross-linked and hydrophobized hyaluronic acid-based controlled drug release systems. Carbohydr. Polym. 2018, 195, 99–106. [Google Scholar] [CrossRef]
- Liu, L.; Liu, Y.; Li, J.; Du, G.; Chen, J. Microbial production of hyaluronic acid: Current state, challenges, and perspectives. Microb. Cell Fact. 2011, 10, 99. [Google Scholar] [CrossRef]
- Serban, M.A.; Yang, G.; Prestwich, G.D. Synthesis, characterization and chondroprotective properties of a hyaluronan thioethyl ether derivative. Biomaterials 2008, 29, 1388–1399. [Google Scholar] [CrossRef]
- Girish, K.S.; Kemparaju, K. The magic glue hyaluronan and its eraser hyaluronidase: A biological overview. Life Sci. 2007, 80, 1921–1943. [Google Scholar] [CrossRef] [PubMed]
- Erickson, M.; Stern, R. Chain gangs: New aspects of hyaluronan metabolism. Int. Biochem. Res. 2012, 2012, 19–28. [Google Scholar] [CrossRef] [PubMed]
- Jiang, D.; Liang, J.; Noble, P.W. Hyaluronan in tissue injury and repair. Annu. Rev. Cell Dev. Biol. 2007, 23, 435–461. [Google Scholar] [CrossRef] [PubMed]
- Jiang, D.; Liang, J.; Noble, P.W. Hyaluronan as an immune regulator in human diseases. Physiol. Rev. 2011, 91, 221–264. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Underhill, C.B.; Chen, L. Hyaluronan on the surface of tumor cells is correlated with metastatic behavior. Cancer Res. 1995, 55, 428–433. [Google Scholar] [PubMed]
- Shiedlin, A.; Bigelow, R.; Christopher, W.; Arbabi, S.; Yang, L.; Maier, R.V.; Wainwright, N.; Childs, A.; Miller, R.J. Evaluation of hyaluronan from different sources: Streptococcus zooepidemicus, rooster comb, bovine vitreous, and human umbilical cord. Biomacromolecules 2004, 5, 2122–2127. [Google Scholar] [CrossRef]
- Fakhari, A.; Berkland, C. Applications and emerging trends of hyaluronic acid in tissue engineering, as a dermal filler and in osteoarthritis treatment. Acta Biomater. 2013, 9, 7081–7092. [Google Scholar] [CrossRef] [PubMed]
- Quinones, J.P.; Bruggemann, O.; Covas, C.P.; Ossipov, D.A. Self-assembled hyaluronic acid nanoparticles for controlled release of agrochemicals and diosgenin. Carbohydr. Polym. 2017, 173, 157–169. [Google Scholar] [CrossRef]
- Roughley, P.J.; Mason, R.M. Proteins and hyaluronic acid associated with proteoglycans extracted from bovine nasal cartilage with low-ionic-strength salt solution. Biochem. Soc. Trans. 1975, 3, 140–142. [Google Scholar] [CrossRef]
- Bulpitt, P.; Aeschlimann, D. New strategy for chemical modification of hyaluronic acid: Preparation of functionalized derivatives and their use in the formation of novel biocompatible hydrogels. J. Biomed. Mater. Res. 1999, 47, 152–169. [Google Scholar] [CrossRef]
- Liu, C.; Bae, K.H.; Yamashita, A.; Chung, J.E.; Kurisawa, M. Thiol-mediated synthesis of hyaluronic acid–epigallocatechin-3-O-gallate conjugates for the formation of injectable hydrogels with free radical scavenging property and degradation resistance. Biomacromolecules 2017, 18, 3143–3155. [Google Scholar] [CrossRef]
- Jia, X.; Burdick, J.A.; Kobler, J.; Clifton, R.J.; Rosowski, J.J.; Zeitels, S.M.; Langer, R. Synthesis and characterization of in situ cross-linkable hyaluronic acid-based hydrogels with potential application for vocal fold regeneration. Macromolecules 2004, 37, 3239–3248. [Google Scholar] [CrossRef]
- Oh, E.J.; Kang, S.; Kim, B.; Jiang, G.; Cho, I.H.; Hahn, S.K. Control of the molecular degradation of hyaluronic acid hydrogels for tissue augmentation. J. Biomed. Mater. Res. A 2008, 86, 685–693. [Google Scholar] [CrossRef] [PubMed]
- Prajapati, V.D.; Maheriya, M.P. Hyaluronic acid as potential carrier in biomedical and drug delivery applications. Funct. Polysacch. Biomed. Appl. 2019, 213–265. [Google Scholar] [CrossRef]
- Calles, J.A.; Ressia, J.A.; Llabot, J.M.; Valles, E.M.; Palma, S.D. Hyaluronan–itaconic acid–glutaraldehyde films for biomedical applications: Preliminary studies. Sci. Pharm. 2016, 84, 61–72. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Messman, J.; Mays, J.W.; Baskaran, D. Polypeptide grafted hyaluronan: Synthesis and characterization. Biomacromolecules 2010, 11, 2313–2320. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Zhong, S.P.; Campoccia, D.; Williams, D.F.; Doherty, P.J.; Williams, R.L.; Benedetti, L. Biodegradation of hyaluronic acid derivatives by hyaluronidase. Biomaterials 1994, 15, 359–365. [Google Scholar] [CrossRef]
- Khunmanee, S.; Jeong, Y.; Park, H. Crosslinking method of hyaluronic-based hydrogel for biomedical applications. J. Tissue Eng. 2017, 8, 1–16. [Google Scholar] [CrossRef]
- Hintze, V.; Schnabelrauch, M.; Rother, S. Chemical modification of hyaluronan and their biomedical applications. Front. Chem. 2022, 10, 830671. [Google Scholar] [CrossRef]
- Schanté, C.E.; Zuber, G.; Herlin, C.; Vandamme, T.F. Chemical modifications of hyaluronic acid for the synthesis of derivatives for a broad range of biomedical applications. Carbohydr. Polym. 2011, 85, 469–489. [Google Scholar] [CrossRef]
- Williams, D. Essential Biomaterials Science; Cambridge University Press: Cambridge, UK, 2014; pp. 537–539. [Google Scholar]
- Luo, Y.; Kirker, K.R.; Prestwich, G.D. Cross-linked hyaluronic acid hydrogel films: New biomaterials for drug delivery. J. Control. Release 2000, 69, 169–184. [Google Scholar] [CrossRef] [PubMed]
- Carvalho, A.L.; Vale, A.C.; Sousa, M.P.; Barbosa, A.M.; Torrado, E.; Mano, J.F.; Alves, N.M. Antibacterial bioadhesive layer-by-layer coatings for orthopedic applications. J. Mater. Chem. B 2016, 4, 5385–5393. [Google Scholar] [CrossRef] [PubMed]
- Sgorla, D.; Almeida, A.; Azevedo, C.; Bunhak, E.J.; Sarmento, B.; Cavalcanti, O.A. Development and characterization of crosslinked hyaluronic acid polymeric films for use in coating processes. Int. J. Pharm. 2016, 511, 380–389. [Google Scholar] [CrossRef] [PubMed]
- Palumbo, F.S.; Fiorica, C.; Pitarresi, G.; Giorgi, M.; Abramo, F.; Gulino, A.; Di Stefano, M.; Giammona, G. Construction and evaluation of sponge scaffolds from hyaluronic acid derivatives for potential cartilage regeneration. J. Mater. Chem. B 2014, 2, 3243–3253. [Google Scholar] [CrossRef] [PubMed]
- Song, E.; Shang, J.; Ratner, D.M. Polysaccharides. In Polymer Science: A Comprehensive Reference; Matyjaszewski, K., Moller, M., Eds.; Elsevier: Oxford, UK, 2012; pp. 137–155. ISBN 978-0-08-087862-1. [Google Scholar]
- Allison, D.D.; Grande-Allen, K.J. Review. Hyaluronan: A powerful tissue engineering tool. Tissue Eng. 2006, 12, 2131–2140. [Google Scholar] [CrossRef] [PubMed]
- Prestwich, G.D.; Kuo, J.W. Chemically-modified HA for therapy and regenerative medicine. Curr. Pharm. Biotechnol. 2008, 9, 242–245. [Google Scholar] [CrossRef] [PubMed]
- Dmitri, A.O.; Sonya, P.; Oommen, P.V.; Jöns, H. Functionalization of hyaluronic acid with chemoselective groups via a disulfide-based protection strategy for in situ formation of mechanically stable hydrogels. Biomacromolecules 2010, 11, 2247–2254. [Google Scholar]
- Crescenzi, V.; Francescangeli, A.; Capitani, D.; Mannina, L.; Renier, D.; Bellini, D. Hyaluronan networking via Ugi’s condensation using lysine as cross-linker diamine. Carbohydr. Polym. 2003, 53, 311–316. [Google Scholar] [CrossRef]
- Bhatnagar, P.; Kumari, M.; Pahuja, R.; Pant, A.B.; Shukla, Y.; Kumar, P.; Gupta, K.C. Hyaluronic acid-grafted PLGA nanoparticles for the sustained delivery of berberine chloride for an efficient suppression of Ehrlich ascites tumors. Drug Deliv. Transl. Res. 2018, 8, 565–579. [Google Scholar] [CrossRef]
- Valachová, K.; Šoltés, L. Hyaluronan as a prominent biomolecule with numerous applications in medicine. Int. J. Mol. Sci. 2021, 22, 7077. [Google Scholar] [CrossRef]
- Becker, L.C.; Bergfeld, W.F.; Belsito, D.V.; Klaassen, C.D.; Marks, J.G.; Shank, R.C.; Slaga, T.J.; Snyder, P.W.; Cosmetic Ingredient Review Expert Panel; Andersen, F.A. Final report of the safety assessment of hyaluronic acid, potassium hyaluronate, and sodium hyaluronate. Int. J. Toxicol. 2009, 28, 5–67. [Google Scholar] [CrossRef] [PubMed]
- Kassir, R.; Kolluru, A.; Kassir, M. Extensive necrosis after injection of hyaluronic acid filler: Case report and review of the literature. J. Cosmet. Dermatol. 2011, 10, 224–231. [Google Scholar] [CrossRef] [PubMed]
- Jeong, S.H.; Fan, Y.; Cheon, K.H.; Baek, J.; Kim, S.; Kim, H.E. Hyaluronic acid-hydroxyapatite nanocomposite hydrogels for enhanced biophysical and biological performance in a dermal matrix. J. Biomed. Mater. Res. A 2017, 105, 3315–3325. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Xue, Y.; Jia, B.; Bai, Y.; Zuo, Y.; Wang, S.; Zhao, Y.; Yang, W.; Tang, H. The preparation of hyaluronic acid grafted pullulan polymers and their use in the formation of novel biocompatible wound healing film. Carbohydr. Polym. 2018, 188, 92–100. [Google Scholar] [CrossRef] [PubMed]
- Boulle, K.; Glogau, R.; Kono, T.; Nathan, M.; Tezel, A.; Roca-Martinez, J.X.; Paliwal, S.; Stroumpoulis, D. A review of the metabolism of 1,4-butanediol diglycidyl ether—Crosslinked hyaluronic acid dermal fillers. Dermatol. Surg. 2013, 39, 1758–1766. [Google Scholar] [CrossRef] [PubMed]
- Santoro, S.; Russo, L.; Argenzio, V.; Borzacchiello, A. Rheological properties of crosslinked hyaluronic acid dermal fillers. J. Appl. Biomater. Biomech. 2011, 9, 127–136. [Google Scholar] [PubMed]
- Chan, B.P.; Leong, K.W. Scaffolding in tissue engineering: General approaches and tissue-specific considerations. Eur Spine J. 2008, 17 (Suppl. S4), 467–479. [Google Scholar] [CrossRef]
- Rao, N.V. Hyaluronic acid–based hydrogels for tissue engineering. Biomater. Organ Tissue Regen 2020, 551–565. [Google Scholar] [CrossRef]
- Kim, H.; Jeong, H.; Han, S.; Beack, S.; Hwang, B.W.; Shin, M.; Oh, S.S.; Hahn, S.K. Hyaluronate and its derivatives for customized biomedical applications. Biomaterials 2017, 123, 155–171. [Google Scholar] [CrossRef]
- Migliore, A.; Gigliucci, G.; Tormenta, S.; Cata, A.D.; Gallelli, L.; Iolascon, G. High molecular weight hyaluronic acid (Hyalu- brix/HyalOne) for treating symptomatic hip osteoarthritis. J. Rare Dis. Res. Treat. 2019, 4, 28–42. [Google Scholar] [CrossRef][Green Version]
- Barbour, K.E.; Helmick, C.G.; Boring, M.; Brady, T.J. Vital Signs: Prevalence of doctor-diagnosed arthritis and arthritis-attributable activity limitation—United States, 2013–2015. MMWR Morb. Mortal. Wkly Rep. 2017, 66, 246–253. [Google Scholar] [CrossRef]
- Mayol, L.; Biondi, M.; Russo, L.; Malle, B.M.; Schwach-Abdellaoui, K.; Borzacchiello, A. Amphiphilic hyaluronic acid derivatives toward the design of micelles for the sustained delivery of hydrophobic drugs. Carbohydr. Polym. 2014, 102, 110–116. [Google Scholar] [CrossRef] [PubMed]
- Peck, J.; Slovek, A.; Miro, P.; Vij, N.; Traube, B.; Lee, C.; Berger, A.A.; Kassem, H.; Kaye, A.D.; Sherman, W.F.; et al. A comprehensive review of viscosupplementation in osteoarthritis of the knee. Orthop. Rev. 2021, 13, 25549. [Google Scholar] [CrossRef] [PubMed]
- Ghosh, P.; Guidolin, D. Potential mechanism of action of intra-articular hyaluronan therapy in osteoarthritis: Are the effects molecular weight dependent? Semin. Arthritis. Rheum. 2002, 32, 10–37. [Google Scholar] [CrossRef] [PubMed]
- Vehof, J.; Snieder, H.; Jansonius, N.; Hammond, C.J. Prevalence and risk factors of dry eye in 79,866 participants of the population-based lifelines cohort study in the Netherlands. Ocul. Surf. 2021, 19, 83–93. [Google Scholar] [CrossRef] [PubMed]
- Aragona, P.; Papa, V.; Micali, A.; Santocono, M.; Milazzo, G. Long-term treatment with sodium hyaluronate–containing artificial tears reduces ocular surface damage in patients with dry eye. Br. J. Ophthalmol. 2002, 86, 181–184. [Google Scholar] [CrossRef] [PubMed]
- Hynnekleiv, L.; Magno, M.; Vernhardsdottir, R.R.; Moschowits, E.; Tønseth, K.A.; Dartt, D.A.; Vehof, J.; Utheim, T.P. Hyaluronic acid in the treatment of dry eye disease. Acta Ophthalmol. 2022, 100, 844–860. [Google Scholar] [CrossRef] [PubMed]
- Van Setten, G.B. Impact of attrition, intercellular shear in dry eye disease: When cells are challenged and neurons are triggered. Int. J. Mol. Sci. 2020, 21, 4333. [Google Scholar] [CrossRef]
- Paugh, J.R.; Nguyen, A.L.; Ketelson, H.A.; Christensen, M.T. Precorneal residence time of artificial tears measured in dry eye subjects. Optom. Vis. Sci. 2008, 85, 725–731. [Google Scholar] [CrossRef]
- Aravinthan, A.; Park, J.K.; Hossain, M.A.; Sharmila, J.; Kim, H.J.; Kang, C.W.; Kim, N.S.; Kim, J.H. Collagen-based sponge hastens wound healing via decrease of inflammatory cytokines. 3 Biotech 2018, 8, 487. [Google Scholar] [CrossRef]
- Broughton, G.; Janis, J.; Attinger, C. Wound healing: An overview. Plast. Reconstr. Surg. 2006, 117, 1e-S–32e-S. [Google Scholar] [CrossRef]
- Enoch, S.; Leaper, D. Basic science of wound healing. Surgery 2005, 23, 37–42. [Google Scholar]
- Stern, R.; Asari, A.A.; Sugahara, K.N. Hyaluronan fragments: An information-rich system. Eur. J. Cell Biol. 2006, 85, 699–715. [Google Scholar] [CrossRef] [PubMed]
- Sudhakar, K.; Ji, S.M.; Kummara, M.R.; Han, S.S. Recent progress on hyaluronan-based products for wound healing applications. Pharmaceutics 2022, 14, 2235. [Google Scholar] [CrossRef] [PubMed]
- Ling, Y.; Shengmao, L.; Shengnan, J.; Feng, X. Emerging frontiers in drug delivery with special focus on novel techniques for targeted therapies. Biomed. Pharmacother. 2023, 165, 115049. [Google Scholar]
- Ezike, T.C.; Okpala, U.S.; Onoja, U.L.; Nwike, C.P.; Ezeako, E.C.; Okpara, O.J.; Okoroafor, C.C.; Eze, S.C.; Kalu, O.L.; Odoh, E.C.; et al. Advances in drug delivery systems, challenges and future directions. Heliyon 2023, 9, e17488. [Google Scholar] [CrossRef] [PubMed]
- Zhijian, L.; Yan, D.; Huile, G. Development and application of hyaluronic acid in tumor targeting drug delivery. Acta Pharm. Sin. B 2019, 9, 1099–1112. [Google Scholar]
- Alaniz, L.; Cabrera, P.V.; Blanco, G.; Ernst, G.; Rimoldi, G.; Alvarez, E.; Hajos, S.E. Interaction of CD44 with different forms of hyaluronic acid. Its role in adhesion and migration of tumor cells. Cell Commun. Adhes. 2016, 9, 117–130. [Google Scholar] [CrossRef]
- Fu, C.P.; Cai, X.-Y.; Chen, S.-L.; Yu, H.-W.; Fang, Y.; Feng, X.-C.; Zhang, L.-M.; Li, C.-Y. Hyaluronic acid-based nanocarriers for anticancer drug delivery. Polymers 2023, 15, 2317. [Google Scholar] [CrossRef]
- Yang, C.; Wang, X.; Yao, X.; Zhang, Y.; Wu, W.; Jiang, X. Hyaluronic acid nanogels with enzyme-sensitive cross-linking group for drug delivery. J. Control. Release 2015, 205, 206–217. [Google Scholar] [CrossRef]
- Famili, A.; Rajagopal, K. Bio-orthogonal cross-linking chemistry enables in situ protein encapsulation and provides sustained release from hyaluronic acid based hydrogels. Mol. Pharm. 2017, 14, 1961–1968. [Google Scholar] [CrossRef]
- Kim, Y.K.; Jang, Y.S.; Kim, S.Y.; Lee, M.H. Functions achieved by the hyaluronic acid derivatives coating and hydroxide film on bio-absorbed Mg. Appl. Surf. Sci. 2019, 473, 31–39. [Google Scholar] [CrossRef]
- Alipoor, R.; Ayan, M.; Hamblin, M.R.; Ranjbar, R.; Rashki, S. Hyaluronic acid-based nanomaterials as a new approach to the treatment and prevention of bacterial infections. Front. Bioeng. Biotechnol. 2022, 10, 913912. [Google Scholar] [CrossRef] [PubMed]
- Bayer, I.S. Hyaluronic acid and controlled release: A review. Molecules 2020, 25, 2649. [Google Scholar] [CrossRef] [PubMed]
- Cho, H.J. Recent progresses in the development of hyaluronic acid-based nanosystems for tumor-targeted drug delivery and cancer imaging. J. Pharm. Investig. 2020, 50, 115–129. [Google Scholar] [CrossRef]
- Chen, B.; Miller, R.J.; Dhal, P.K. Hyaluronic acid-based drug conjugates: State-of-the-art and perspectives. J. Biomed. Nanotechnol. 2014, 10, 4–16. [Google Scholar] [CrossRef] [PubMed]
- Juhaščik, M.; Andrej, K.; Gloria, H. Recent advances of hyaluronan for skin delivery: From structure to fabrication strategies and applications. Polymers 2022, 14, 4833. [Google Scholar] [CrossRef] [PubMed]
- Alimardani, V.; Abolmaali, S.S.; Yousefi, G.; Rahiminezhad, Z.; Abedi, M.; Tamaddon, A.; Ahadian, S. Microneedle arrays combined with nanomedicine approaches for transdermal delivery of tTherapeutics. J. Clin. Med. 2021, 10, 181. [Google Scholar] [CrossRef] [PubMed]
- Liu, S.; Jin, M.; Quan, Y.; Kamiyama, F.; Katsumi, H. The development and characteristics of novel microneedle arrays fabricated from hyaluronic acid, and their application in the transdermal delivery of insulin. J. Control Release 2012, 161, 933–941. [Google Scholar] [CrossRef]
- Fakhraei, L.S.; Kim, Y.; Kang, G.; Suyong, K.; Seunghee, L.; Hyungil, J. Tissue interlocking dissolving microneedles for accurate and efficient transdermal delivery of biomolecules. Sci. Rep. 2019, 9, 7886. [Google Scholar] [CrossRef]
- Nur, F.N.A.; Nik, N.N.G.; Yew, H.W. Concept design of transdermal microneedles for diagnosis and drug delivery: A review. Adv. Eng. Mater. 2021, 23, 2100503. [Google Scholar]
- Bonet, I.J.M.; Araldi, D.; Green, P.G.; Levine, J.D. Topical coapplication of hyaluronan with transdermal drug delivery enhancers attenuates inflammatory and neuropathic pain. Pain 2023, 164, 2653–2664. [Google Scholar] [CrossRef] [PubMed]
- Araldi, D.; Ferrari, L.F.; Levine, J.D. Hyperalgesic priming (type II) induced by repeated opioid exposure: Maintenance mechanisms. Pain 2017, 158, 1204–1216. [Google Scholar] [CrossRef] [PubMed]
- Junqueira, L.A.; Polonini, H.; Loures, S.; Raposo, N.R.B.; Ferreira, A.O.; Brandao, M.A.F. Permeation efficacy of a transdermal vehicle with steroidal hormones and nonsteroidal anti-inflammatory agents as model drugs. Curr. Drug Deliv. 2019, 16, 136–141. [Google Scholar] [CrossRef] [PubMed]
- Yuan, M.; Niu, J.; Xiao, Q.; Ya, H.; Zhang, Y.; Fan, Y.; Li, L.; Li, X. Hyaluronan-modified transfersomes based hydrogel for enhanced transdermal delivery of indomethacin. Drug Deliv. 2022, 29, 1232–1242. [Google Scholar] [CrossRef] [PubMed]
- Son, S.U.; Lim, J.W.; Kang, T.; Jung, J.; Lim, E.-K. Hyaluronan-based nanohydrogels as effective carriers for transdermal delivery of lipophilic agents: Towards transdermal drug administration in neurological disorders. Nanomaterials 2017, 7, 427. [Google Scholar] [CrossRef] [PubMed]
- Horvát, S.; Fehér, A.; Wolburg, H.; Sipos, P.; Veszelka, S.; Tóth, A.; Kis, L.; Kurunczi, A.; Balogh, G.; Kürti, L.; et al. Sodium hyaluronate as a mucoadhesive component in nasal formulation enhances delivery of molecules to brain tissue. Eur. J. Pharm. Biopharm. 2009, 72, 252–259. [Google Scholar] [CrossRef]
- Garcia-Garcia, E.; Andrieux, K.; Gil, S.; Couvreur, P. Colloidal carriers and blood–brain barrier (BBB) translocation: A way to deliver drugs to the brain? Int. J. Pharm. 2005, 298, 274–292. [Google Scholar] [CrossRef]
- Wolburg, H.; Wolburg-Buchholz, K.; Sam, H.; Horvát, S.; Deli, M.A.; Mack, A.F. Epithelial and endothelial barriers in the olfactory region of the nasal cavity of the rat. Histochem. Cell Biol. 2008, 130, 127–140. [Google Scholar] [CrossRef]
- Lim, S.T.; Forbes, B.; Berry, D.J.; Martin, G.P.; Brown, M.B. In vivo evaluation of novel hyaluronan/chitosan microparticulate delivery systems for the nasal delivery of gentamicinin rabbits. Int. J. Pharm. 2002, 231, 73–82. [Google Scholar] [CrossRef]
- Huh, Y.; Cho, H.J.; Yoon, I.S.; Choi, M.K.; Kim, J.S.; Oh, E.; Chung, S.-J.; Shim, C.-K.; Kim, D.-D. Preparation and evaluation of spray-dried hyaluronic acid microspheres for intranasal delivery of fexofenadine hydrochloride. Eur. J. Pharm. Sci. 2010, 40, 9–15. [Google Scholar] [CrossRef] [PubMed]
- Hersh, D.S.; Wadajkar, A.S.; Roberts, N.; Perez, J.G.; Connolly, N.P.; Frenkel, V.; Winkles, J.A.; Woodworth, G.F.; Kim, A.J. Evolving drug delivery strategies to overcome the blood brain barrier. Curr. Pharm. Des. 2016, 22, 1177–1193. [Google Scholar] [CrossRef] [PubMed]
- Lisbeth, I. Nasal drug delivery: New developments and strategies. Drug Discov. Today 2002, 7, 1184–1189. [Google Scholar]
- Bitter, C.; Suter-Zimmermann, K.; Surbera, C. Nasal drug delivery in humans. Curr. Probl. Dermatol. 2011, 40, 20–35. [Google Scholar] [PubMed]
- Laffleur, F.; Hörmann, N.; Gust, R.; Ganner, A. Synthesis, characterization and evaluation of hyaluronic acid-based polymers for nasal delivery. Int. J. Pharm. 2023, 631, 122496. [Google Scholar] [CrossRef] [PubMed]
- Casula, E.; Manca, M.L.; Perra, M.; Pedraz, J.L.; Lopez-Mendez, T.B.; Lozano, A.; Calvo, E.; Zaru, M.; Manconi, M. Nasal spray formulations based on combined hyalurosomes and glycerosomes loading Zingiber officinalis extract as green and natural strategy for the treatment of rhinitis and rhinosinusitis. Antioxidants 2021, 10, 1109. [Google Scholar] [CrossRef]
- Feng, C.; Han, Y.X.; Guo, H.H.; Ma, X.L.; Wang, Z.Q.; Wang, L.L.; Zheng, W.-S.; Jiang, J.-D. Self-assembling HA/PEI/dsRNA-p21 ternary complexes for CD44 mediated small active RNA delivery to colorectal cancer. Drug Deliv. 2017, 24, 1537–1548. [Google Scholar] [CrossRef]
- Hua, S.; Marks, E.; Schneider, J.J.; Keely, S. Advances in oral nano-delivery systems for colon targeted drug delivery in inflammatory bowel disease: Selective targeting to diseased versus healthy tissue. Nanomed. Nanotechnol. Biol. Med. 2015, 11, 1117–1132. [Google Scholar] [CrossRef]
- Kotla, N.G.; Burke, O.; Pandit, A.; Rochev, Y. An orally administrated hyaluronan functionalized polymeric hybrid nanoparticle system for colon-specific drug delivery. Nanomaterials 2019, 9, 1246. [Google Scholar] [CrossRef]
- Batist, G.; Gelmon, K.A.; Chi, K.N.; Miller, W.H.; Chia, S.K.; Mayer, L.D.; Swenson, C.E.; Janoff, A.S.; Louie, A.C. Safety, Pharmacokinetics, and efficacy of CPX-1 liposome injection in patients with advanced solid tumors. Clin. Cancer Res. 2009, 15, 692–700. [Google Scholar] [CrossRef]
- Allen, T.M.; Cullis, P.R. Liposomal drug delivery systems: From concept to clinical applications. Adv. Drug Deliv. Rev. 2013, 65, 36–48. [Google Scholar] [CrossRef]
- Fallacara, A.; Baldini, E.; Manfredini, S.; Vertuani, S. Hyaluronic acid in the third millennium. Polymers 2018, 10, 701. [Google Scholar] [CrossRef] [PubMed]
- Montagner, I.M.; Merlo, A.; Carpanese, D.; Zuccolotto, G.; Renier, D.; Campisi, M.; Pasut, G.; Zanovello, P.; Rosato, A. Drug conjugation to hyaluronan widens therapeutic indications for ovarian cancer. Oncoscience 2015, 2, 373–381. [Google Scholar] [CrossRef] [PubMed]
- Han, N.K.; Shin, D.H.; Kim, J.S.; Weon, K.Y.; Jang, C.Y.; Kim, J.S. Hyaluronan-conjugated liposomes encapsulating gemcitabine for breast cancer stem cells. Int. J. Nanomed. 2016, 11, 1413–1425. [Google Scholar] [CrossRef]
- Gupta, R.C.; Lall, R.; Srivastava, A.; Sinha, A. Hyaluronic acid: Molecular mechanisms and therapeutic trajectory. Front. Vet. Sci. 2019, 6, 192. [Google Scholar] [CrossRef] [PubMed]

| Source | Occurrence | Reference |
|---|---|---|
| Humans | Urine, epidermis, dermis, serum, vitreous body, umbilical cord, synovial fluid | [27,28] |
| Bacteria | Certain bacteria capsules (such as those of streptococci) | [26] |
| Roosters | Rooster comb | [19] |
| Sheep | Synovial fluid, medulla cortex, lungs | [13] |
| Rabbits | Renal papillae, kidney, vitreous body, muscle, liver | [14] |
| Rats | Lung, kidney, brain, liver | [14] |
| Cattle | Bovine nasal cartilage | [29] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Valachová, K.; Hassan, M.E.; Šoltés, L. Hyaluronan: Sources, Structure, Features and Applications. Molecules 2024, 29, 739. https://doi.org/10.3390/molecules29030739
Valachová K, Hassan ME, Šoltés L. Hyaluronan: Sources, Structure, Features and Applications. Molecules. 2024; 29(3):739. https://doi.org/10.3390/molecules29030739
Chicago/Turabian StyleValachová, Katarína, Mohamed E. Hassan, and Ladislav Šoltés. 2024. "Hyaluronan: Sources, Structure, Features and Applications" Molecules 29, no. 3: 739. https://doi.org/10.3390/molecules29030739
APA StyleValachová, K., Hassan, M. E., & Šoltés, L. (2024). Hyaluronan: Sources, Structure, Features and Applications. Molecules, 29(3), 739. https://doi.org/10.3390/molecules29030739







