Abstract
In this study, the attenuative effects of the hydro-alcoholic extract from Mitragyna speciosa (MSE) against diabetes-induced anxiety and depression-like behaviors were examined. In addition, UPLC/ESI/TOF-MS analysis was performed to identify the phytochemical nature of MSE. DM was induced using a combination of high fructose/streptozotocin, and the diabetic rats were treated with MSE (50 and 200 mg/kg) for 5 weeks. After treatment, the animals were subjected to a forced swim test, open field test and elevated plus-maze tests. Additionally, proinflammatory cytokines and oxidative stress parameters were evaluated in the brain tissues of the rats. UPLC/ESI/TOF-MS analysis revealed that MSE is abundantly rich in polyphenolic constituents, notably flavonoid and phenolic glycosides. Behavioral tests and biochemical analyses indicated that diabetic rats showed significantly increased anxiety and depressive-like behavioral deficits, brain oxidative stress and pro-inflammatory cytokines levels (IL-1β, IL-6 and TNF-α). Treatment with MSE (50 and 200 mg/kg) significantly attenuated increased blood glucose level, depressive and anxiety-like behaviors in diabetic rats. Additionally, the antioxidant enzymes activities were markedly increased in MSE-treated animals, while TNF-α, IL-1β and IL-6 cytokines were notably suppressed. Taken together, these results suggested that MSE has potentials as antidepressant and anxiolytic-like effects and improves the brain oxido-inflammatory status in diabetic rats.
1. Introduction
Diabetes mellitus is a chronic metabolic disease which has evolved over the years as a major global public health issue. Typically, diabetes mellitus is principally depicted by excessive blood glucose concentration (hyperglycemia), together with alterations in lipid, carbohydrate and protein metabolism [1,2]. Out of the three different types of diabetes, type II diabetes mellitus is the most rampant accounting for approximately 90–95% of all global cases [1,3]. Insulin resistance, pancreatic beta cell dysfunction and insufficient insulin production are the characteristics hallmarks of type II diabetes mellitus [3]. Hyperglycemia induces excessive generation of reactive oxygen species, leading to oxidative stress, which forms the pathological and physiological basis for all diabetic complications, including nephropathy, neuropathy, cardiovascular diseases, retinopathy and Alzheimer’s disease [4].
One of the most prevailing diabetes associated comorbidity is brain disorders and psychological problems including depression, anxiety, cognitive dysfunctions and Alzheimer’s disease. In fact, it has been reported that up to 30% of DM patients are suffering from depression [5,6,7]. In addition, there is a cordial relationship between hyperglycemia and depressive disorders, as patients exhibiting psychiatric and psychological disorders such as depression and anxiety are prone to increase risk for developing DM, while depression also increases the risk of metabolic disorders particularly DM [7,8,9]. Several factors, including decrease in neurotransmission, increased oxidative and inflammatory factors as well as decrease in antioxidant defense, have been shown to promote insulin resistance and facilitate DM-induced depression [10,11]. As such, mitigating hyperglycemia induced oxidative and inflammatory damage may obviously be a viable target in the treatment of DM-induced neuropsychiatric comorbidities [7,12].
While significant progress has been made in the development of synthetic antidiabetic drugs, unfortunately, adverse reactions as well as the inability of these drugs to impede or slow down the development of DM associated comorbidity have necessitated the search for effective antidiabetic alternatives. Medicinal plants have been enormously explored for their health promoting roles and low toxicity especially in the treatment of diabetes and its associated complications [4,8,12]. Numerous bioactive components from medical plants have been found as excellent antidiabetic agents through their inhibitory effects on several diabetic related pathways [13].
Mitragyna speciosa Korth. (kratom) is an indigenous Southeast Asian plant belonging to the family Rubiaceae [14,15]. Historically, M. speciosa is used in folk medicine for treating cough, fever, diabetes, pain, diarrhea, cancer, wound, fatigue, hypertension and as a substitute for opium withdrawal [14,15,16,17]. In addition to the traditional uses of M. speciosa, accumulating evidences have illustrated the antioxidant, anti-inflammatory, antiobesity, antinociceptive and cytotoxic activities of M. speciosa [18,19,20]. Furthermore, M. speciosa extracts have been shown to show excellent anxiolytic and anti-depressant effects in mice using two behavioral experiments (forced swim and the tail suspension tests) [14,21]. Aside from the widely reported indole alkaloids (including mitragynine, speciociliatine, paynantheine and 7-hydroxymitragynine) present in M. speciosa, several other polyphenolic constituents, such as isoquercitrin, kaempferol, caffeic acid, chlorogenic acid, rutin, apigenin, quercetin, apigenin-7-glycosides, hyperoside, quercetin-3-galactoside-7-rhamnoside, kaempferol-3-glucoside and epicatecin, have also been reported [14,18,22,23]. Despite the widely reported efficacies of M. speciosa, there is lack of scientific evidence relating to its antidiabetic therapeutic value as well as its efficacy against diabetes-induced comorbidity. Hence, this study investigated the effects of M. speciosa on anxiety and depression-like behaviors, oxidative and inflammatory status in the brain of fructose/streptozotocin-induced diabetic rats.
2. Results
2.1. LC-ESI-QTOF-MS Analysis for the Identification of Metabolites in MSE
The UPLC-ESI-MS/MS analysis (negative mode) was applied for secondary metabolites profiling of MSE. As portrayed in Table 1, the analysis identified 193 secondary metabolites belonging to chemically diverse classes of compounds, notably flavonoid, phenolics, flavonoid glycoside, iridoid glycosides and ellagitannins subclasses (Table 1). Among the identified compounds, glycosides accounted for the major constituents tentatively identified in MSE, viz., herbacetin-7-glucoside, eriodictyol 7-(6-trans-p-coumaroylglucoside), cynaroside A, Kaempferol 3,7,4′-triglucoside, 6-methoxykaempferol 3,7-bis(3-acetylrhamnoside), tiliroside, neoliquiritin 2″-apioside, among several others; phenolic and phenolic glycosides, viz., isoferuloyl C1-glucuronide, protocatechuic acid-3-glucoside, leonuriside A, dihydroferulic acid 4-O-glucuronide, glucocaffeic acid and 5-caffeoylquinic acid; iridoid glucosides, viz., mussaenosidic acid, secoxyloganin, shanzhiside methyl ester, theveside, geniposide and swertiapunimarins; triterpene saponins, viz., cynarasaponin F, licoricesaponin B2, tarasaponin, mabioside C and trachelosperoside A1. In addition, alkaloids including mitragynine, lycoricidinol, 10-hydroxystrictosamide, isomitraphyllic acid (16→1)-β-d-glucopyranosyl ester, reserpiline and Echitovenine; stilbenes (Z)-resveratrol 3,4′-diglucoside and (Z)-resveratrol 3-(3″-sulfoglucoside); anthocyanins, viz., malvidin 3-(6″-acetylglucoside)-5-glucoside, cyanidin 3-(2″-glucuronosylglucoside), malvidin 3-glucoside-5-(6″-malonylglucoside) and cyanidin 3-(2-glucosyl-6-caffeoylglucoside) were also tentatively identified in MSE. Other compounds, such as acridones, purine nucleosides, hydroxycinnamic acid, catechin and coumarin acids, were also revealed in MSE (Table 1).

Table 1.
Constituents tentatively identified in MSE extract using LC-ESI-QTOF-MS analysis.
2.2. Effect of MSE on Blood Glucose
The results showed that STZ injection leads to hyperglycemia as demonstrated by significant increase in blood glucose concentration of the DMG, MSE-L and DMSE groups compared to the CG (p < 0.05; Figure 1A). Treatment with MES (50 and 200 mg/kg) notably reduced the final blood glucose level by 59.4%, and by 74% when compared to the DMG group by the end of the study (p < 0.05; Figure 1A).
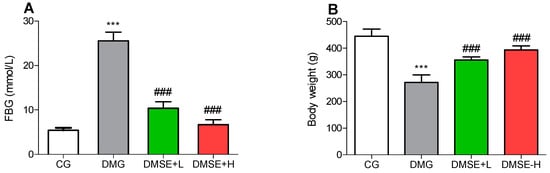
Figure 1.
Effect of MSE on (A) fasting blood glucose and (B) body weight of diabetic rats. Data represent mean ± SD. *** p < 0.05 when compared to the control group. ### p < 0.05 when compared to the diabetic group.
2.3. Effect of MSE on Body Weight
The changes in the initial to the final body weight were evaluated. As shown in Figure 1B, major differences were observed between the body weight of the rats in the DMG group and the CG group. The DMG group showed a 39% decrease in their body weight when juxtaposed with the CG group. After treatment with MSE (50 and 200 mg/kg), the body weight of the treated animals was significant increased (Figure 1B; p < 0.05).
2.4. Effect of MSE on Depressive-like Behaviors
DM induced significant increase in the immobility time of the DMG when compared to the CG group in the FST (Figure 2A; p < 0.05). However, this effect was markedly decreased in the MSE treated groups compared to the DMG group (Figure 2A; p < 0.05). Additionally, the results also revealed significant differences in the swimming time of the DMG compared to the CG group. DMG rats spent less time swimming compared to CG rats (p < 0.05, Figure 2B), whereas MSE notably increased the swimming time of the treated rats (p < 0.05; Figure 2B).
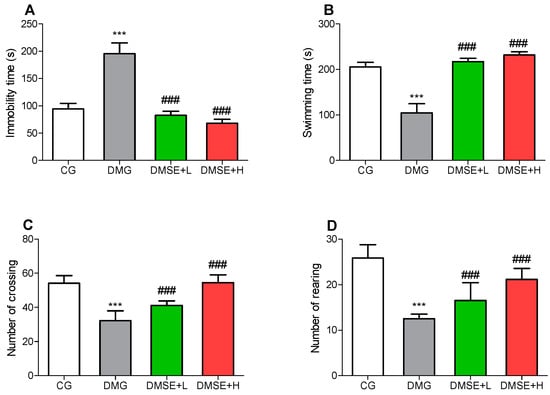
Figure 2.
Effect of MSE on (A) immobility, (B) swimming time in the forced swimming test, (C) number of crossing and (D) number of rearing in the open field test in diabetic rats. Data represent mean ± SD. *** p < 0.05 when compared to the control group. ### p < 0.05 when compared to the diabetic group.
2.5. Effect of MSE on Locomotor Activity
As shown in Figure 2, DMG rats showed significantly decreased locomotive activity, including reduced total number of crossings (Figure 2C) and rearing (Figure 2D) in the open field test when compared to the CG group. Contrariwise, MSE dose dependently improved the locomotive activity of the treated rats (Figure 2C,D).
2.6. Effect of MSE on Anxiety-like Behavior
As shown in Figure 3, DMG rats spent significantly reduced time in the open arms (Figure 3A) and the number of entries into the open arms (Figure 3B) when compared to the CG (p < 0.05). MSE induced a significant increase in the time spent in open arms as well as entries into the open arms (p < 0.05; Figure 3A,B).
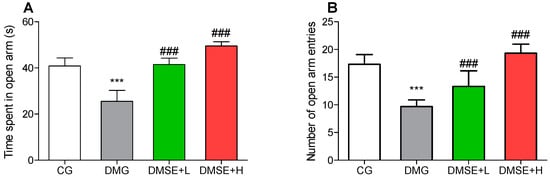
Figure 3.
Effect of MSE on the anxiety-like behavior (A) time spent in the open arm and (B) number of open arm entries in the elevated-plus maze test. Data represent mean ± SD. *** p < 0.05 when compared to the control group. ### p < 0.05 when compared to the diabetic group.
2.7. Effect of MSE on Oxidative Stress Parameters
Compared with CG, DMG showed a significantly increased level of MDA in the brain, whereas MSE treatment led to a significant decrease in MDA levels compared with the DMG group (Figure 4A; p < 0.05). The activities of brain CAT and SOD in the DMG group were obviously lower than the CG group (p < 0.05; Figure 4B,C). The activities of CAT and SOD of MSE-treated groups were markedly increased when compared with the DMG group (p < 0.05; Figure 4B,C). Additionally, the brain GSH level showed similar trend. The DMG group showed notable decrease in GSH level in comparison with the CG group. Contrariwise, MSE treatment significantly increased the brain GSH level in comparison with the DMG group (p < 0.05; Figure 4D).
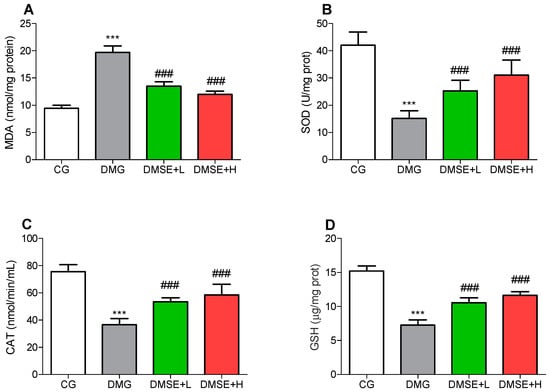
Figure 4.
Effect of MSE on oxidative stress parameters in the brain of diabetic rats (A) MDA, (B) SOD, (C) CAT and (D) GSH levels. Data represent mean ± SD. *** p < 0.05 when compared to the control group. ### p < 0.05 when compared to the diabetic group.
2.8. Effect of MSE on Proinflammatory Parameters
The levels of IL-6, IL-1β and TNF-α were increased significantly in the brain of the DMG group compared with the CG group (Figure 5A–C; p < 0.05). MSE significantly alleviated these proinflammatory cytokine levels when compared to the DMG group. Administration of MSE markedly reduced IL-6, IL-1β and TNF-α compared to the DMG group (Figure 5A–C; p < 0.05).
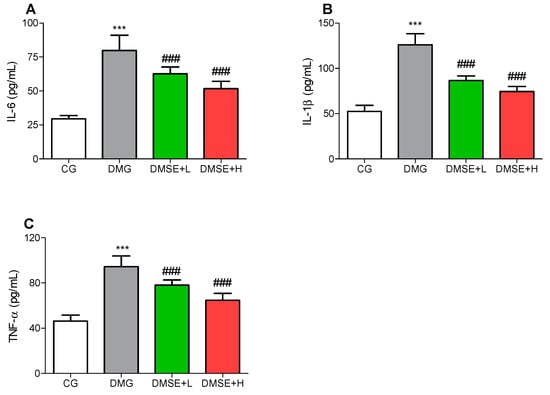
Figure 5.
Effect of MSE on proinflammatory cytokines in the brain of diabetic rats (A) IL-6, (B) IL-1β and (C) TNF-α. Data represent mean ± SD. *** p < 0.05 when compared to the control group. ### p < 0.05 when compared to the diabetic group.
3. Discussion
Anxiety and depression constitute a relatively high social hazard and high suicide rate [24] and the incidence of these two psychiatric disorders are 2–3 times higher in diabetic patients when compared to normal people [11]. One of the most sought-after therapeutic approach for the treatment of hyperglycemia and its resulting complications is to keep the blood glucose level at bay, which may subsequently limit the generation of reactive oxygen species and oxidative stress, a major factor implicated in diabetic complications, including DM-induced anxiety and depression [25,26]. Although antidiabetic medicines such as metformin and glibenclamide have been widely successful in the control of blood glucose level, several side effects have limited their success. As such, natural components have been the focus of recent research as alternatives for treating diabetes and its complications [1,4]. M. speciosa is well known traditionally and pharmacologically as an antidiabetic, antidepressant, anxiolytic and antioxidant agent. Moreover, M. speciosa have shown very strong effects of the brain and central nervous system in several models [14,16]. This study investigated the ameliorative effects of M. speciosa extract on depressive and anxiety-like behaviors, as well as oxido-inflammatory status in diabetic rats. This study showed for the first time that M. speciosa attenuated anxiety and depressive-like behavior in diabetic rats. These effects seem to be correlated with the hyperglycemic, antioxidant and anti-inflammatory effects of MSE.
High fructose and STZ-induced DM is a model that elucidates most of the underlying mechanism associated with DM, including insulin resistance, β cells dysfunction and reduced insulin availability, which has been grossly implicated in DM-induced cognitive dysfunction [27]. Furthermore, the brain is one of the major sites of insulin action, as such insulin resistance ultimately leads to neuronal cell death causing dementia, Alzheimer’s disease and depression [28,29]. In this study, DM was induced using a combination of high fructose and STZ, resulting in severe hyperglycemia, and obvious body weight decrease. The inability of the β cells to secrete insulin in DM increases catabolism and gluconeogenesis, resulting in reduced body weight due to wasting of fat storage [7,30]. The increment in blood glucose level and subsequent weight reduction in the diabetic rats were restored upon treatment with MSE.
The results from this study revealed that DM led to characteristic anxiety and depressive-like behaviors, as indicated by the increase in immobility duration (FST), decrease in entries and time spent in the open arms (EPMT) as well as reduction in the number of crossing and rearing (OFT), which were in corroboration with previous studies on DM-induced anxiety and depression [8,26,31,32]. Metabolic disorders, including diabetes and obesity, have been prominently associated a number of psychological problems particularly major depressive disorders and anxiety, and hyperglycemia is a prevalent factor that can modulate the onset, progression and deterioration of depression and anxiety [33]. MSE treatment notably decreased the duration of immobility in the FST. In addition, MSE administration significantly alleviated anxiety-like behavior in the EPM task by increasing the number of entries and time spent in the open arms.
Indeed, hyperglycemia has been widely reported to promote oxidative stress, which initiates the onset, progression and deterioration of depression [34,35]. Brain oxidative damage is manifested by reduced antioxidant enzyme activities including SOD, CAT, GSH and increased lipid peroxidation (MDA). SOD, GSH and CAT are the frontline enzymes that initiates cellular protective effects against ROS and oxidative stress element [7,36,37]. In the results presented here, SOD, GSH and CAT activities were significantly decreased, and the MDA level increased significantly in brain structures of the DMG group, which corroborates with previous reports [8,26,38]. Earlier studies have suggested that antidepressant agents could ameliorate oxidative stress, upregulate antioxidant defense, thus restoring redox homeostasis, leading to the reversal of DM-induced anxiety and depressive-like behaviors [25,38,39]. The administration of MSE markedly increase CAT, SOD and GSH activities, as well as decrease the levels of MDA in the brain tissues of treated diabetic rats.
In addition to oxidative stress, numerous studies have reported that neuroinflammation plays a vital role in diabetes-induced depressive and anxiety owing to increased levels of proinflammatory cytokines. DM is associated with neuroinflammation, which may lead to damages or even death of brain neurons. Jawale et al. reported that DM increased the levels of TNF-α in the brain, which mediated anxiety and depressive-like behavior [40,41]. Inflammatory process in DM is a by-product of excessive generation of reactive species and increased oxidative stress, leading to the trigger of NF-κB signaling and subsequent increase in proinflammatory genes [25]. In agreement with previous studies, the level of proinflammatory cytokines (TNF-α, IL-1β and IL-6) was significantly increased in the brain tissues of DMG rats, suggesting neuroinflammation, whereas treatment with MSE attenuated the increased levels of these inflammatory cytokines, suggesting that MSE presents antidepressant-like and anxiolytic effects that may be partly dependent on its antioxidant and anti-inflammatory effects.
The bioactivity of any natural product especially medicinal plant is largely dependent on the nature and composition of the compounds present in such plant. The existence of polyphenolic compounds in several plant extracts have been reported to be largely responsible for numerous biological activities, notably antioxidant, antidiabetic, antidepressant and anti-inflammatory properties [12,42,43]. In M. speciosa, indole alkaloids have been extensively identified as one of the major taxonomic markers of the plant and these compounds have been widely believed to be responsible for the effect of the plant on the brain, pain perception and other activities [44]. However, recent reports have indicated that the presence of other compounds, especially polyphenolic constituents in M. speciosa, which strengthens the notion that several other bioactive constituents besides indole alkaloids seems to contribute to bioactive properties of the plant [18,23]. The results obtained from the QTOF-MS analysis of MSE indicated the presence of huge amounts of compounds, ranging from flavonoids, flavonoid glycosides, phenolics, alkaloids, terpene glycosides, stilbenoids and iridoid glycosides. Polyphenolic compounds, especially flavonoids and phenolics, have been reported to be responsible for several antidiabetic and antidiabetic complication effects. The antidiabetic and antidepressant profile of MSE is obviously supported by its chemical constituents. For instance, isoliquiritigenin attenuated DM-induced renal and aortic injury, and displayed significant neuroprotective and antidepressant effects via its effects of oxidative stress and inflammation [45,46,47]. Silvestro et al. reported that quercetin displayed antidepressant-like actions due to its antioxidant, anti-inflammatory and neuroprotective effects in several animal models [48]. In addition, esculetin demonstrated antidiabetic and antidepressant-like properties in DM-induced hepatorenal oxidative damage and LPS-induced neuroinflammatory and depressive-like behavior in mice through its inhibition of oxidative and inflammatory pathways [49,50]. In another report, swertiamarin attenuated hyperglycemia, nephropathy and oxidative stress in DM models [51,52]. Taken together, the synergistic association between all the various groups of compounds in MSE acting on multiple pathways could have collectively exerted the antidiabetic, antidepressant and anxiolytic effects observed in this study. This results further supported the involvement of other bioactive compounds other than indole alkaloids in the bioactivity of kratom plants [18].
4. Materials and Methods
4.1. Preparation of M. speciosa Extract
Fresh kratom leaves were purchased from a local garden at Nakhon Si Thammarat Province, Thailand. The plant specimen collected was authenticated at the Faculty of Traditional Thai Medicine, Prince of Songkla University, Hat Yai, Thailand and the specimen was preserved at the herbarium of the faculty (Voucher number; KRA-001-22). The dried and powdered kratom leaves were extracted using 80% methanol (w/v:1:10) in a shaker for 24 h. The extract was filtered, and the leaves mass was subjected to two other rounds of extraction using the same condition as earlier stated. The combined extract was evaporated using a rotary evaporator to approximately 30% of the initial volume. The remaining extract solution was refrigerated at 4 °C overnight. Thereafter, the solution was decanted, centrifuged and lyophilized to obtain a hydroscopic brown colored powder (MSE), which was stored at 4 °C until use.
4.2. Metabolite Profiling Using Ultra-High-Performance Liquid Chromatography Coupled to Electrospray Time-of-Flight Tandem Mass Spectrometry (UPLC/ESI/TOF-MS)
The secondary metabolites in MSE were profiled using UHPLC-ESI-QTOF-MS. MSE was dissolved in 50% methanol solution, filtered and the solution obtained after filtration was subjected to the analysis using previously described parameters [53].
4.3. Animals and Experimental Design
Six-week-old male Sprague Dawley (SD) rats (140 ± 20 g) were raised under standard conditions (temperature of 22 ± 2 °C, 65 ± 5% relative humidity and a natural photo period of 12 h light/dark cycle). The experimental protocol adhered to the instructions stipulated by Guide for the Care and Use of Laboratory Animals, National Institutes of Health, and approved by the Animal Ethics Committee of The Second Wuhu Second Peoples Hospital (ethics approval number: WheyLLWYH-2021-0908). All the rats were acclimatized for one week on normal rat chow and water ad libitum. After a week of adaptation, the rats were randomly divided into four treatment groups (6 rats/group) as follows: control group (CG): treated with normal saline; diabetic model group (DMG): treated with normal saline; diabetic + MSE-L (DMSE-L): diabetic rats treated with 50 mg/kg MSE; diabetic + MSE-H (DMSE-H): diabetic rats treated with 200 mg/kg MSE.
4.4. Diabetes Induction
Firstly, the diabetic groups (DMG, DMSE-L and DMSE-H) were given 30% fructose solution ad libitum in lieu of normal tap water for four weeks to induce insulin resistance, while the CG group received normal tap water during the same period. Thereafter, DM was induced in overnight-fasted fructose-fed rat groups by intraperitoneal injection of streptozotocin (STZ, 35 mg/kg) solubilized in sodium citrate buffer solution (pH 4.5), while the CG rats were injected with the same volume of sodium citrate buffer. The STZ injected rats were give 5% glucose solution for 24 h in other to avoid possible hypoglycemic state due to STZ injection. The fasting blood glucose (FBG) concentration of all the animals was measured after 3 days of STZ administration with a portable Accu check guide glucometer (Roche Diabetes Care, Mannheim, Germany) and rats with blood glucose concentration >13.88 mmol/L (250 mg/dL) were adjudged as diabetic. MSE was administered to DMSE-L and DMSE-H at 50 and 200 mg/kg, respectively, via oral gavage, while normal saline was administered to the CG and DMG groups daily for five weeks. The dose selection of MSE was based on previous studies [18,54,55,56]. Periodic measurement of the blood glucose concentration and body weights were evaluated.
4.5. Open Field Test
The test was performed using a rectangular wooden open field with dimensions 40 × 50 × 65 cm, and the floor of the field was divided into six concentric units. The rats were placed in the middle of the field. The rats’ ambulation including the total number of crossings with all four paws and the number of rearing was recorded for 5 min. A trained observer blinded to the treatment protocol evaluated the total number of cross and rearing of each animal.
4.6. Elevated Plus Maze Test
The EPMT was made up of two open and two closed arms with (50 × 10 cm) perpendicularly arranged and linked by a central sheath 50 cm high from the floor. Each rat was gradually positioned in the central square of the apparatus, facing the open arms and allowed to explore for 300 s. The time spent and number of entries into the open arms was measured during a 5 min period. In other to eliminate any olfactory cues, the apparatus was cleaned with 70% alcohol between each examination.
4.7. Forced Swimming Test
The forced swimming test apparatus consisted of a cylindrical shaped glass container (40 × 30 cm) filled with water (23 ± 2 °C) to a depth of 30 cm. The rats were initially forced to swim for 15 min. After 24 h, the rats were subjected to the same procedure for 5 min, during the period the immobility and swimming time were manually recorded. Immobility time was taken as the period where no activity was initiated by the rats except for movements that kept the rat’s head above water. A trained observer blinded to the treatment protocol evaluated the swimming and immobility time of each animal. The experimental timeline is shown in Figure 6.
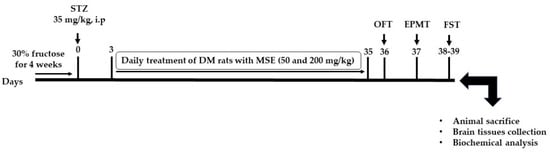
Figure 6.
Experimental schematic diagram.
4.8. Sacrifice and Sample Collection
The rats were fasted for 12 h and humanely sacrificed by euthanizing with sodium thiopental (150 mg/kg). The brain tissues were dissected from the rats, cleaned with physiological saline solution and instantly fixed in 10% neutral buffered formalin solution for further histopathological analysis. Another portion of the brain tissues were preserved at −70 °C for further analysis.
4.9. Analysis of Oxidative and Inflammatory Biomarkers
The isolated whole brain tissues were homogenized using potassium phosphate buffer (pH 6.5). After centrifugation (6000× g for 30 min at 4 °C), the supernatant collected was used for evaluating glutathione (GSH), superoxide dismutase (SOD), catalase (CAT) and malondialdehyde (MDA) levels using assay kits from Jiancheng Biotechnology, Nanjing, China. Likewise, proinflammatory cytokine levels; interleukin 6 (IL-6), interleukin 1β (IL-1β) and tumor necrosis factor alpha (TNF-α) were measured using ELISA kits obtained from Abcam, Cambridge, UK, following the manufacturers procedures.
4.10. Statistical Analysis
Statistical analysis of the data was performed using GraphPad Prism software (version 5.0, GraphPad Software, Inc. San Diego, CA, USA) and normal distribution of the data was checked by the Kolmogorov–Smirnov test. Data displayed mean ± standard deviation and were analyzed by one way ANOVA followed by Tukey’s post-hoc test. p < 0.05 indicated statistical significance.
5. Conclusions
The findings from this study demonstrated that the administration of MSE attenuated depressive and anxiety-like behaviors induced by fructose/STZ diabetic rats. The alleviative effects of MSE were mediated through the reduction of oxidative stress and neuroinflammation (revealed by decreased MDA, IL-6, IL-1β and TNF-α levels) in the brain of the treated diabetic rats. Furthermore, LC-ESI-MS analysis of MSE revealed the overwhelming majority polyphenolic compounds, including phenolic, flavonoids, terpenoids, iridoids and their glycosidic bound forms. Overall, the results highlighted the potential biological effects of MSE in the treatment of diabetes and its associated comorbidity.
Author Contributions
Conceptualization, O.J.O.; methodology, L.C., S.F. and O.J.O.; formal analysis, L.C., S.F. and O.J.O.; investigation, L.C., S.F. and O.J.O.; resources, L.C.; data curation, L.C., S.F. and O.J.O.; writing—original draft preparation, L.C. and O.J.O.; writing—review and editing, S.F. and O.J.O.; supervision, S.F. and O.J.O.; project administration, O.J.O.; funding acquisition, L.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board of The Second Wuhu Second Peoples Hospital (ethics approval number: WheyLLWYH-2021-0908).
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Sample Availability
Samples of the compounds are not available from the authors.
References
- Makinde, E.A.; Radenahmad, N.; Adekoya, A.E.; Olatunji, O.J. Tiliacora triandra extract possesses antidiabetic effects in high fat diet/streptozotocin-induced diabetes in rats. J. Food Biochem. 2020, 44, e13239. [Google Scholar] [CrossRef] [PubMed]
- Song, P.; Sun, C.; Li, J.; Long, T.; Yan, Y.; Qin, H.; Makinde, E.A.; Famurewa, A.C.; Jaisi, A.; Nie, Y.; et al. Tiliacora triandra extract and its major constituent attenuates diabetic kidney and testicular impairment by modulating redox imbalance and pro-inflammatory responses in rats. J. Sci. Food Agric. 2021, 101, 1598–1608. [Google Scholar] [CrossRef] [PubMed]
- Erukainure, O.L.; Oyebode, O.A.; Ijomone, O.M.; Chukwuma, C.I.; Koorbanally, N.A.; Islam, M.S. Raffia palm (Raphia hookeri G. Mann & H. Wendl) wine modulates glucose homeostasis by enhancing insulin secretion and inhibiting redox imbalance in a rat model of diabetes induced by high fructose diet and streptozotocin. J. Ethnopharmacol. 2019, 237, 159–170. [Google Scholar] [CrossRef] [PubMed]
- Olatunji, O.J.; Chen, H.; Zhou, Y. Lycium chinense leaves extract ameliorates diabetic nephropathy by suppressing hyperglycemia mediated renal oxidative stress and inflammation. Biomed. Pharmacother. 2018, 102, 1145–1151. [Google Scholar] [CrossRef] [PubMed]
- Anderson, R.J.; Freedland, K.E.; Clouse, R.E.; Lustman, P.J. The prevalence of comorbid depression in adults with diabetes: A meta-analysis. Diabetes Care 2001, 24, 1069–1078. [Google Scholar] [CrossRef] [Green Version]
- Moulton, C.D.; Pickup, J.C.; Ismail, K. The link between depression and diabetes: The search for shared mechanisms. Lancet Diabetes Endocrinol. 2015, 3, 461–471. [Google Scholar] [CrossRef]
- Zimath, P.L.; Dalmagro, A.P.; Mota da Silva, L.; Malheiros, A.; Maria de Souza, M. Myrsinoic acid B from Myrsine coriacea reverses depressive-like behavior and brain oxidative stress in streptozotocin-diabetic rats. Chem. Biol. Interact. 2021, 347, 109603. [Google Scholar] [CrossRef]
- Rahmani, G.; Farajdokht, F.; Mohaddes, G.; Babri, S.; Ebrahimi, V.; Ebrahimi, H. Garlic (Allium sativum) improves anxiety- and depressive-related behaviors and brain oxidative stress in diabetic rats. Arch. Physiol. Biochem. 2020, 126, 95–100. [Google Scholar] [CrossRef]
- Siddiqui, S. Depression in type 2 diabetes mellitus-a brief review. Diabetes Metab. Syndr. Clin. Res. Rev. 2014, 8, 62–65. [Google Scholar] [CrossRef]
- de Morais, H.; de Souza, C.P.; da Silva, L.M.; Ferreira, D.M.; Werner, M.F.; Andreatini, R.; da Cunha, J.M.; Zanoveli, J.M. Increased oxidative stress in prefrontal cortex and hippocampus is related to depressive-like behavior in streptozotocin-diabetic rats. Behav. Brain Res. 2014, 258, 52–64. [Google Scholar] [CrossRef]
- Menezes Zanoveli, J.; de Morais, H.; Caroline da Silva Dias, I.; Karoline Schreiber, A.; Pasquini de Souza, C.; Maria da Cunha, J. Depression associated with diabetes: From pathophysiology to treatment. Curr. Diabetes Rev. 2016, 12, 165–178. [Google Scholar] [CrossRef] [PubMed]
- Pang, X.; Makinde, E.A.; Eze, F.N.; Olatunji, O.J. Securidaca inappendiculata polyphenol rich extract counteracts cognitive deficits, neuropathy, neuroinflammation and oxidative stress in diabetic encephalopathic rats via p38 MAPK/Nrf2/HO-1 pathways. Front. Pharmacol. 2021, 12, 737764. [Google Scholar] [CrossRef] [PubMed]
- Makinde, E.A.; Ovatlarnporn, C.; Adekoya, A.E.; Nwabor, O.F.; Olatunji, O.J. Antidiabetic, antioxidant and antimicrobial activity of the aerial part of Tiliacora triandra. S. Afr. J. Bot. 2019, 125, 337–343. [Google Scholar] [CrossRef]
- Ahmad, I.; Prabowo, W.C.; Arifuddin, M.; Fadraersada, J.; Indriyanti, N.; Herman, H.; Purwoko, R.Y.; Nainu, F.; Rahmadi, A.; Paramita, S.; et al. Mitragyna species as pharmacological agents: From abuse to promising pharmaceutical products. Life 2022, 12, 193. [Google Scholar] [CrossRef]
- Domnic, G.; Jeng-Yeou Chear, N.; Abdul Rahman, S.F.; Ramanathan, S.; Lo, K.-W.; Singh, D.; Mohana-Kumaran, N. Combinations of indole based alkaloids from Mitragyna speciosa (Kratom) and cisplatin inhibit cell proliferation and migration of nasopharyngeal carcinoma cell lines. J. Ethnopharmacol. 2021, 279, 114391. [Google Scholar] [CrossRef] [PubMed]
- Meireles, V.; Rosado, T.; Barroso, M.; Soares, S.; Gonçalves, J.; Luís, Â.; Caramelo, D.; Simão, A.Y.; Fernández, N.; Duarte, A.P.; et al. Mitragyna speciosa: Clinical, toxicological aspects and analysis in biological and non-biological samples. Medicines 2019, 6, 35. [Google Scholar] [CrossRef] [Green Version]
- Singh, D.; Narayanan, S.; Vicknasingam, B. Traditional and non-traditional uses of Mitragynine (Kratom): A survey of the literature. Brain Res. Bull. 2016, 126, 41–46. [Google Scholar] [CrossRef]
- Goh, Y.S.; Karunakaran, T.; Murugaiyah, V.; Santhanam, R.; Abu Bakar, M.H.; Ramanathan, S. Accelerated solvent extractions (ASE) of Mitragyna speciosa Korth. (Kratom) leaves: Evaluation of its cytotoxicity and antinociceptive activity. Molecules 2021, 26, 3704. [Google Scholar] [CrossRef]
- Srichana, K.; Janchawee, B.; Prutipanlai, S.; Raungrut, P.; Keawpradub, N. Effects of mitragynine and a crude alkaloid extract derived from Mitragyna speciosa korth. On permethrin elimination in rats. Pharmaceutics 2015, 7, 10–26. [Google Scholar] [CrossRef] [Green Version]
- Parthasarathy, S.; Bin Azizi, J.; Ramanathan, S.; Ismail, S.; Sasidharan, S.; Mohd, M.I.; Mansor, S.M. Evaluation of antioxidant and antibacterial activities of aqueous, methanolic and alkaloid extracts from Mitragyna speciosa (rubiaceae family) leaves. Molecules 2009, 14, 3964–3974. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Idayu, N.F.; Hidayat, M.T.; Moklas, M.A.M.; Sharida, F.; Raudzah, A.R.N.; Shamima, A.R.; Apryani, E. Antidepressant-like effect of mitragynine isolated from Mitragyna speciosa Korth in mice model of depression. Phytomedicine 2011, 18, 402–407. [Google Scholar] [CrossRef] [PubMed]
- Brown, P.N.; Lund, J.A.; Murch, S.J. A botanical, phytochemical and ethnomedicinal review of the genus Mitragyna Korth: Implications for products sold as kratom. J. Ethnopharmacol. 2017, 202, 302–325. [Google Scholar] [CrossRef]
- Zakaria, F.; Tan, J.-K.; Faudzi, S.M.M.; Rahman, M.B.A.; Ashari, S.E. Ultrasound-assisted extraction condition optimization using response surface methodology from Mitragyna speciosa (Korth.) Havil leaves. Ultrason. Sonochem. 2021, 81, 105851. [Google Scholar] [CrossRef] [PubMed]
- Gerhard, D.M.; Wohleb, E.S.; Duman, R.S. Emerging treatment mechanisms for depression: Focus on glutamate and synaptic plasticity. Drug Discov. Today 2016, 21, 454–464. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Olatunji, O.J.; Zuo, J.; Olatunde, O.O. Securidaca inappendiculata stem extract confers robust antioxidant and antidiabetic effects against high fructose/streptozotocin induced type 2 diabetes in rats. Exploration of bioactive compounds using UHPLC-ESI-QTOF-MS. Arch. Physiol. Biochem. 2021, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Bampi, S.R.; Casaril, A.M.; Fronza, M.G.; Domingues, M.; Vieira, B.; Begnini, K.R.; Seixas, F.K.; Collares, T.V.; Lenardão, E.J.; Savegnago, L. The selenocompound 1-methyl-3-(phenylselanyl)-1H-indole attenuates depression-like behavior, oxidative stress, and neuroinflammation in streptozotocin-treated mice. Brain Res. Bull. 2020, 161, 158–165. [Google Scholar] [CrossRef]
- Gasparin, A.T.; Rosa, E.S.; Jesus, C.H.A.; Guiloski, I.C.; da Silva de Assis, H.C.; Beltrame, O.C.; Dittrich, R.L.; Pacheco, S.D.G.; Zanoveli, J.M.; da Cunha, J.M. Bixin attenuates mechanical allodynia, anxious and depressive-like behaviors associated with experimental diabetes counteracting oxidative stress and glycated hemoglobin. Brain Res. 2021, 1767, 147557. [Google Scholar] [CrossRef]
- Tyagi, A.; Pugazhenthi1, S. Targeting insulin resistance to treat cognitive dysfunction. Mol. Neurobiol. 2021, 58, 2672–2691. [Google Scholar] [CrossRef]
- Kong, S.H.; Park, Y.J.; Lee, J.Y.; Cho, N.H.; Moon, M.K. Insulin resistance is associated with cognitive decline among older Koreans with normal baseline cognitive function: A prospective community-based cohort study. Sci. Rep. 2018, 8, 650. [Google Scholar] [CrossRef] [Green Version]
- Leonard, B.E.; Wegener, G. Inflammation, insulin resistance and neuroprogression in depression. Acta Neuropsychiatr. 2020, 32, 1–9. [Google Scholar] [CrossRef] [Green Version]
- Ibrahim, M.A.; Habila, J.D.; Koorbanally, N.A.; Islam, M.S. Butanol fraction of Parkia biglobosa (Jacq.) G. Don leaves enhance pancreatic β-cell functions, stimulates insulin secretion and ameliorates other type 2 diabetes-associated complications in rats. J. Ethnopharmacol. 2016, 183, 103–111. [Google Scholar] [CrossRef]
- Bikri, S.; Aboussaleh, Y.; Berrani, A.; Louragli, I.; Hafid, A.; Chakib, S.; Ahami, A. Effects of date seeds administration on anxiety and depressive symptoms in streptozotocin-induced diabetic rats: Biochemical and behavioral evidences. J. Basic Clin. Physiol. Pharmacol. 2021, 32, 1031–1040. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.W.; Hong, T.W.; Wang, Y.J.; Chen, K.C.; Pei, J.C.; Chuang, T.Y.; Lai, W.S.; Tsai, S.H.; Chu, R.; Chen, W.C.; et al. Ophiocordyceps formosana improves hyperglycemia and depression-like behavior in an STZ-induced diabetic mouse model. BMC Complement. Altern. Med. 2016, 16, 310. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wu, X.; Wang, J.; Song, L.; Guan, Y.; Cao, C.; Cui, Y.; Zhang, Y.; Liu, C. Catalpol weakens depressive-like behavior in mice with streptozotocin-induced hyperglycemia via PI3K/AKT/Nrf2/HO-1 signaling pathway. Neuroscience 2021, 473, 102–118. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Yang, C.; Elsheikh, N.A.H.; Li, C.; Yang, F.; Wang, G.; Li, L. HO-1 reduces heat stress-induced apoptosis in bovine granulosa cells by suppressing oxidative stress. Aging 2019, 11, 5535–5547. [Google Scholar] [CrossRef] [PubMed]
- Reus, G.Z.; Carlessi, A.S.; Silva, R.H.; Ceretta, L.B.; Quevedo, J. Relationship of oxidative stress as a link between diabetes mellitus and major depressive disorder. Oxid. Med. Cell. Longev. 2019, 2019, 1–6. [Google Scholar] [CrossRef]
- Gu, F.; Chauhan, V.; Chauhan, A. Glutathione redox imbalance in brain disorders. Curr. Opin. Clin. Nutr. Metab. Care 2015, 18, 89–95. [Google Scholar] [CrossRef]
- Ceriello, A. New insights on oxidative stress and diabetic complications may lead to a “causal” antioxidant therapy. Diabetes Care 2003, 26, 1589–1596. [Google Scholar] [CrossRef] [Green Version]
- Moylan, S.; Berk, M.; Dean, O.M.; Samuni, Y.; Williams, L.J.; O’Neil, A.; Hayley, A.C.; Pasco, J.A.; Anderson, G.; Jacka, F.N.; et al. Oxidative & nitrosative stress in depression: Why so much stress? Neurosci. Biobehav. Rev. 2014, 45, 46–62. [Google Scholar]
- Zborowski, V.A.; Heck, S.O.; Vencato, M.; Pinton, S.; Marques, L.S.; Nogueira, C.W. Keap1/Nrf2/HO-1 signaling pathway contributes to p-chlorodiphenyl diselenide antidepressant-like action in diabetic mice. Psychopharmacology 2020, 237, 363–374. [Google Scholar] [CrossRef] [PubMed]
- Jawale, A.; Datusalia, A.K.; Bishnoi, M.; Sharma, S.S. Reversal of diabetes-induced behavioral and neurochemical deficits by cinnamaldehyde. Phytomedicine 2016, 23, 923–930. [Google Scholar] [CrossRef] [PubMed]
- Patel, S.S.; Ray, R.S.; Sharma, A.; Mehta, V.; Katyal, A.; Udayabanu, M. Antidepressant and anxiolytic like effects of Urtica dioica leaves in streptozotocin induced diabetic mice. Metab. Brain Dis. 2018, 33, 1281–1292. [Google Scholar] [CrossRef] [PubMed]
- Eze, F.N.; Jayeoye, T.J. Chromolaena odorata (Siam weed): A natural reservoir of bioactive compounds with potent anti-fibrillogenic, antioxidative, and cytocompatible properties. Biomed. Pharmacother. 2021, 141, 111811. [Google Scholar] [CrossRef] [PubMed]
- Pathak, L.; Agrawal, Y.; Dhir, A. Natural polyphenols in the management of major depression. Expert Opin. Investig. Drugs. 2013, 22, 863–880. [Google Scholar] [CrossRef] [PubMed]
- Flores-Bocanegra, L.; Raja, H.A.; Graf, T.N.; Augustinović, M.; Wallace, E.D.; Hematian, S.; Kellogg, J.J.; Todd, D.A.; Cech, N.B.; Oberlies, N.H. The chemistry of kratom [Mitragyna speciosa]: Updated characterization data and methods to elucidate indole and oxindole alkaloids. J. Nat. Prod. 2020, 83, 2165–2177. [Google Scholar] [CrossRef]
- Alzahrani, S.; Said, E.; Ajwah, S.M.; Alsharif, S.Y.; El-Bayoumi, K.S.; Zaitone, S.A.; Qushawy, M.; Elsherbiny, N.M. Isoliquiritigenin attenuates inflammation and modulates Nrf2/caspase-3 signalling in STZ-induced aortic injury. J. Pharm. Pharmacol. 2021, 73, 193–205. [Google Scholar] [CrossRef]
- Sun, L.; Yang, Z.; Zhang, J.; Wang, J. Isoliquiritigenin attenuates acute renal injury through suppressing oxidative stress, fibrosis and JAK2/STAT3 pathway in streptozotocin-induced diabetic rats. Bioengineered 2021, 12, 11188–11200. [Google Scholar] [CrossRef]
- Prajapati, R.; Seong, S.H.; Park, S.E.; Paudel, P.; Jung, H.A.; Choi, J.S. Isoliquiritigenin, a potent human monoamine oxidase inhibitor, modulates dopamine D1, D3, and vasopressin V1A receptors. Sci. Rep. 2021, 11, 23528. [Google Scholar] [CrossRef]
- Silvestro, S.; Bramanti, P.; Mazzon, E. Role of quercetin in depressive-like behaviors: Findings from animal models. Appl. Sci. 2021, 11, 7116. [Google Scholar] [CrossRef]
- Prabakaran, D.; Ashokkumar, N. Protective effect of esculetin on hyperglycemia-mediated oxidative damage in the hepatic and renal tissues of experimental diabetic rats. Biochimie 2013, 95, 366–373. [Google Scholar] [CrossRef]
- Zhu, L.; Nang, C.; Luo, F.; Pan, H.; Zhang, K.; Liu, J.; Zhou, R.; Gao, J.; Chang, X.; He, H.; et al. Esculetin attenuates lipopolysaccharide (LPS)-induced neuroinflammatory processes and depressive-like behavior in mice. Physiol. Behav. 2016, 163, 184–192. [Google Scholar] [CrossRef] [PubMed]
- Jaishree, V.; Narsimha, S. Swertiamarin and quercetin combination ameliorates hyperglycemia, hyperlipidemia and oxidative stress in streptozotocin-induced type 2 diabetes mellitus in wistar rats. Biomed. Pharmacother. 2020, 130, 110561. [Google Scholar] [CrossRef] [PubMed]
- Parwani, K.; Patel, F.; Bhagwat, P.; Dilip, H.; Patel, D.; Thiruvenkatam, V.; Mandal, P. Swertiamarin mitigates nephropathy in high-fat diet/streptozotocin-induced diabetic rats by inhibiting the formation of advanced glycation end products. Arch. Physiol. Biochem. 2021, 1–19. [Google Scholar] [CrossRef] [PubMed]
- Eze, F.N.; Tola, A.J. Protein glycation and oxidation inhibitory activity of Centella asiatica phenolics (CAP) in glucose-mediated bovine serum albumin glycoxidation. Food Chem. 2020, 332, 127302. [Google Scholar] [CrossRef]
- Reanmongkol, W.; Keawpradub, N.; Sawangjaroen, K. Effects of the extracts from Mitragyna speciosa Korth. leaves on analgesic and behavioral activities in experimental animals. Songklanakarin J. Sci. Technol. 2007, 29, 1. [Google Scholar]
- Vijeepallam, K.; Pandy, V.; Kunasegaran, T.; Murugan, D.D.; Naidu, M. Mitragyna speciosa leaf extract exhibits antipsychotic-like effect with the potential to alleviate positive and negative symptoms of psychosis in mice. Front. Pharmacol. 2016, 7, 464. [Google Scholar] [CrossRef] [Green Version]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).