Production Review of Accelerator-Based Medical Isotopes
Abstract
1. Introduction
1.1. Definition of Medical Isotopes
1.2. Medical Use
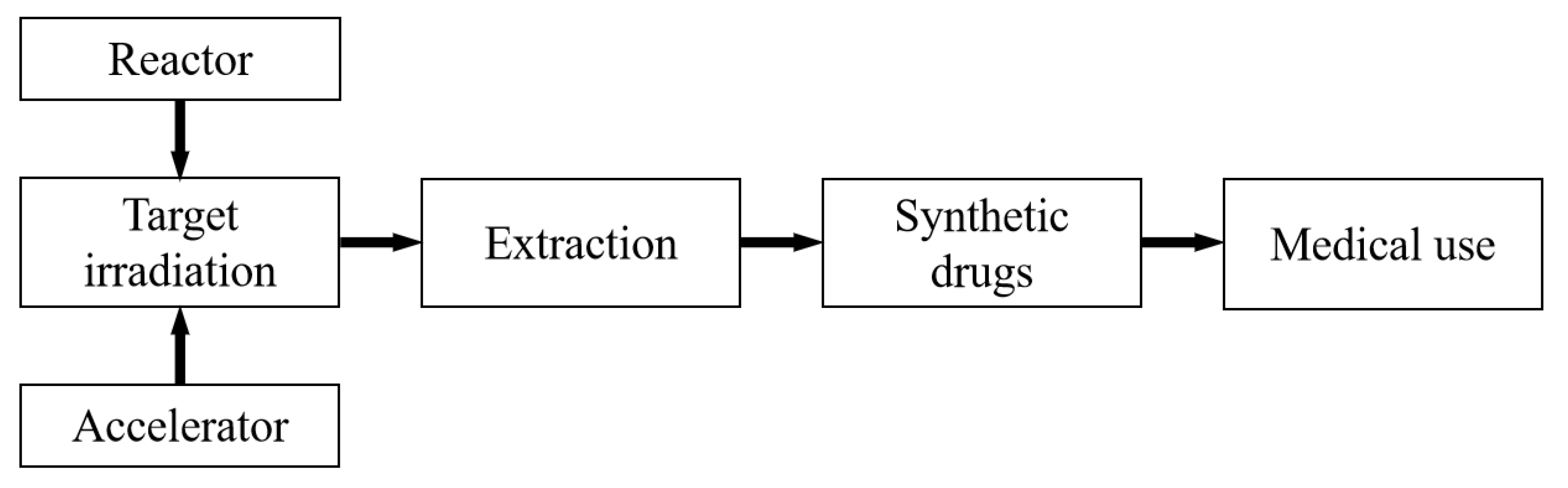
- (1a)
- In a reactor, irradiate a suitable target with neutrons to induce a nuclear reaction;
- (1b)
- In an accelerator, irradiate a suitable target with protons, alpha, or deuteron particles to induce a nuclear reaction;
- (2)
- Separate radioisotopes from the irradiated targets;
- (3)
- Combine the ligands with radioisotopes to prepare radiopharmaceuticals;
- (4)
- Employ the radiopharmaceuticals in nuclear medicine.
1.2.1. Radiopharmaceuticals for Diagnosis
1.2.2. Radiopharmaceuticals for Therapy
1.2.3. Radiopharmaceuticals for Theranostics
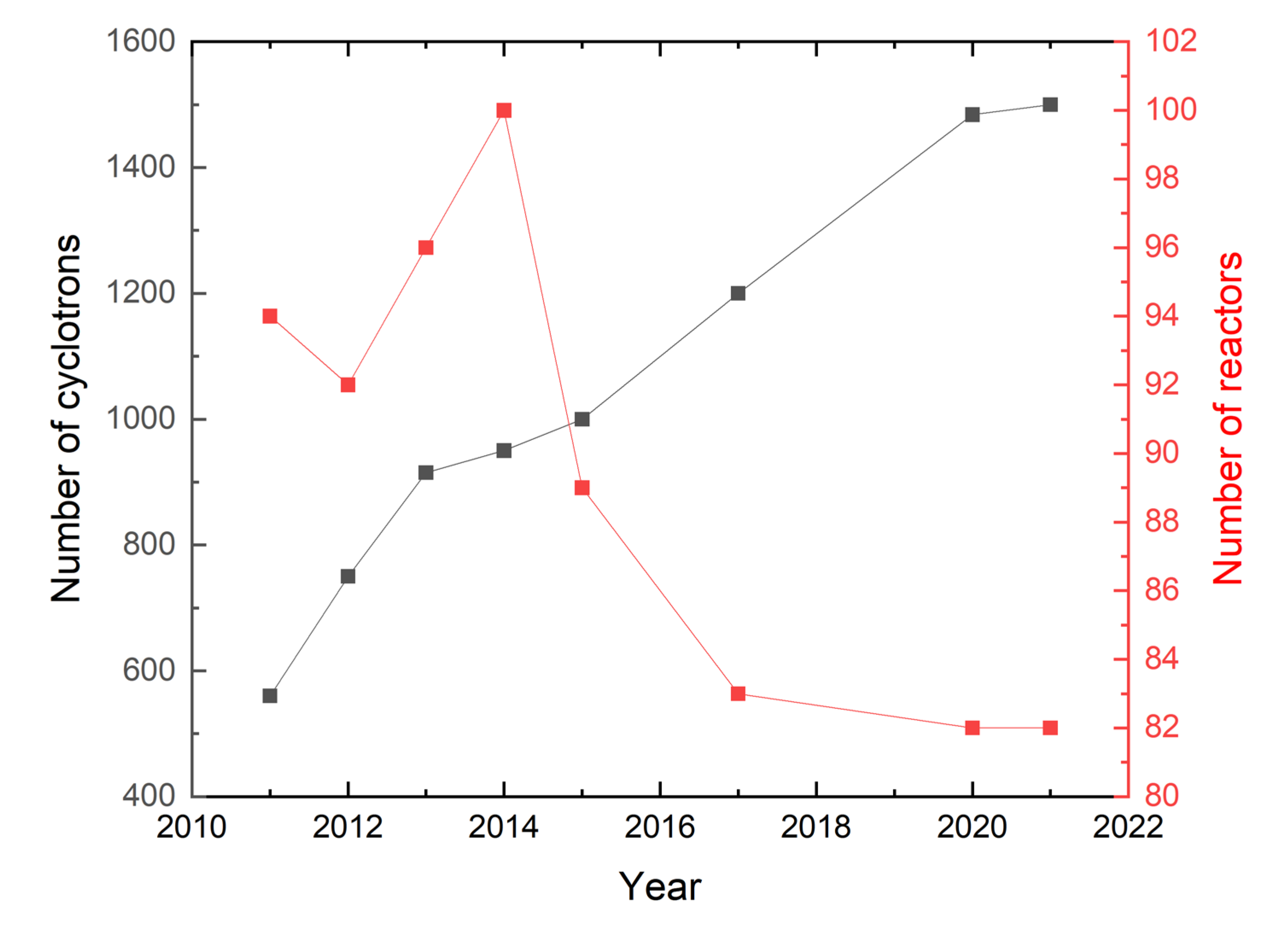
1.3. The Status of Medical Isotope Production
- (1)
- Supervision is easier, and safety is improved [40];
- (2)
- The maintenance and decommissioning costs are lower [29];
- (3)
- The amount of radioactive waste produced is less than 10% of the amount produced by a reactor, and the radiation levels are lower [41];
- (4)
- It has no risk of nuclear proliferation [42].
2. Medical Isotopes
2.1. Medical Isotopes Produced by Cyclotrons (1–5: PET Radioisotopes, 6–7: SPECT Radioisotopes, 8–10: Therapeutic Radioisotopes)
2.1.1. 18F
- (1)
- 18O (p, n) 18F: This reaction requires enriched (and more expensive) 18O target materials to produce 18F in a high yield [66]. Technology developments led to improvements in the target system and the production of 18F up to 34 GBq, as well as specific activities of 350–600 GBq/mmol 30 min after the end of bombardment [67]. Subsequently, it was found that with the irradiation of 11 MeV protons, the yield of 18F further increased directly with the proton current. However, the impurities also increased such that for a proton current of 20 μA, the yield of 56Co (4.86 MBq) and 110mAg (1.51 MBq) doubled [68]. Many developing countries do not have medical isotope production facilities. If these countries desire to become self-sufficient in the production of medical isotopes, they could start by installing low-energy cyclotrons to produce 18F [69].
- (2)
- 20Ne (d, α) 18F: This is the first production method used to produce 18F. This reaction is characterized by lower yields and low specific activity, so it is gradually being replaced. However, with production improvements, this method could again become an attractive alternative [70].
2.1.2. 68Ga
2.1.3. 64Cu
2.1.4. 89Zr
- (1)
- 89Y (p, n) 89Zr: This reaction only requires low-energy protons (5-15 MeV) and targets with natural abundance 89Y (100%), which reduces the costs significantly. The number of interference nuclear reactions is limited; hence, one can obtain a high specific activity of 89Zr [102,103,104]. The yield of this (p, n) reaction can be as high as 44 MBq/μA·h under irradiation of 14 MeV protons [105]. Various methods for the isolation and purification of 89Zr have been proposed, including solvent extraction, anion exchange chromatography, and weak cation exchange chromatography, which can obtain 89Zr with high specific activity and radionuclidic purity [106]. The proton energy from small medical cyclotrons installed in hospitals can meet the requirements for bombarding the 89Y target, which is the main reason why many hospitals have developed 89Zr production processes.
- (2)
- 89Y (d, 2n) 89Zr: This reaction uses low-energy deuterons (also 5–15 MeV) and has the same advantages as the aforementioned production method [102,103,104], as well as offering a higher yield of 58MBq/μA·h. However, one must still factor in the availability of the beam of particles and the costs of these two production methods [105]. Thus, more research is needed.
- (3)
- natSr (α, xn) 89Zr: Besides requiring α beams, if natSr targets are used, abundant quantities of impurities such as 88Zr and 86Zr can easily be produced. For the moment, this production method is only theoretically feasible [107].
2.1.5. 124I
- (1)
- 124Te (p, n) 124I: This is the main production method currently employed. Although this method offers a relatively low production rate, it can achieve high currents and use enriched targets to improve the overall yield [108]. The average yield of this reaction is 16 MBq/μA·h, and at the end of bombardment, the impurity content of 123I and 125I only reaches about 1% [111]. Dry distillation is used to extract 124I [112]. On the downside, the enriched 124Te target material costs about 10000$/g, which is relatively expensive [113].
- (2)
2.1.6. 99Mo/99mTc
- (1)
- 100Mo (p, 2n) 99mTc [116,117]: This is the main production method and is optimal with a proton energy range of 19–24 MeV and a highly enriched 100Mo target, such that 98Tc, 97Tc, and other impurities can be reduced to a minimum. According to the experimental data, with a proton beam energy of 24 MeV, the yield of 99mTc is about 592 GBq/mA·h [118]. A target irradiated with a 24 MeV proton beam at 500 μA for 12 h yielded 2.59 TBq of 99mTc [119]. GE PETtrace880 machines have obtained approximately 174 GBq after 6 h [116]. To date, TRIUMF and its partners have successfully verified the feasibility of using a 24 MeV cyclotron to produce 99mTc to supply the needs of all applications in Vancouver by developing a complete process based on 16, 19, and 24 MeV cyclotron production and applied the results to relevant patents [120]. Automated modules to separate 99mTc from irradiated targets of 100Mo are under development [121]. However, the shipped distance should be considered based on the direct product and its half-life [122];
- (2)
2.1.7. 123I
2.1.8. 225Ac
2.1.9. 211At
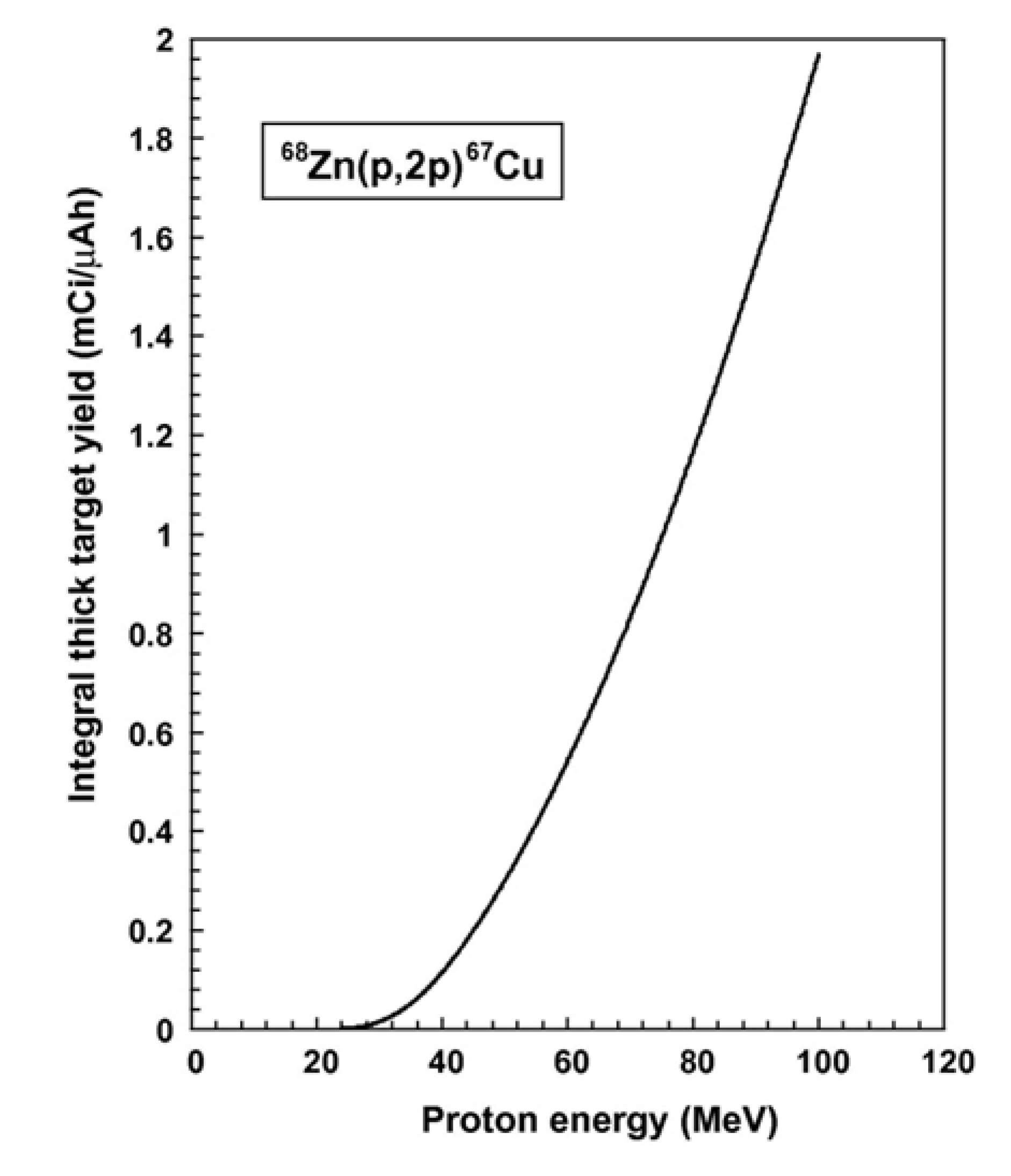
2.1.10. 67Cu
2.2. Medical Isotopes Produced by Linacs
2.2.1. 18F
2.2.2. 99Mo
2.3. Medical Isotopes Produced by Neutron Generators
2.3.1. 99Mo/99mTc
2.3.2. 67Cu
3. The Status of Medical Isotope Production via Accelerators in China
3.1. Available Accelerators for Medical Isotope Production in China
3.2. The Status of Medical Isotope Production via Accelerators
4. Summary
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Radioisotopes in Medicine [EB/OL]. Available online: https://world-nuclear.org/information-library/non-power-nuclear-applications/radioisotopes-research/radioisotopes-in-medicine.aspx (accessed on 1 June 2022).
- AMA Manual of Style Committee. AMA manual of style: A guide for authors and editors, 10 th ed.; Oxford University Press: New York, NY, USA, 2007; ISBN 978-0-19-517633-9. [Google Scholar]
- Reuzé, S.; Schernberg, A.; Orlhac, F.; Sun, R.; Chargari, C.; Dercle, L.; Deutsch, E.; Buvat, I.; Robert, C. Radiomics in nuclear medicine applied to radiation therapy: Methods, pitfalls, and challenges. Int. J. Radiat. Oncol. Biol. Phys. 2018, 102, 1117–1142. [Google Scholar] [CrossRef] [PubMed]
- Langbein, T.; Weber, W.A.; Eiber, M. Future of theranostics: An outlook on precision oncology in nuclear medicine. J. Nucl. Med. 2019, 60, 13S–19S. [Google Scholar] [CrossRef] [PubMed]
- Kar, N.R. Production and applications of radiopharmaceuticals: A review. Int. J. Pharm. Investig. 2019, 9, 36–42. [Google Scholar] [CrossRef]
- Vermeulen, K.; Vandamme, M.; Bormans, G.; Cleeren, F. Design and challenges of radiopharmaceuticals. In Seminars in Nuclear Medicine; WB Saunders: Philadelphia, PA, USA, 2019; Volume 49, pp. 339–356. [Google Scholar]
- Holly, T.A.; Abbott, B.G.; Al-Mallah, M.; Calnon, D.A.; Cohen, M.C.; DiFilippo, F.P.; Ficaro, E.P.; Freeman, M.R.; Hendel, R.C.; Jain, D.; et al. Single photon-emission computed tomography. J. Nucl. Cardiol. 2010, 17, 941–973. [Google Scholar] [CrossRef] [PubMed]
- Jaszczak, R.J.; Coleman, R.E.; Lim, C.B. SPECT: Single photon emission computed tomography. IEEE Trans. Nucl. Sci. 1980, 27, 1137–1153. [Google Scholar] [CrossRef]
- Jaszczak, R.J.; Coleman, R.E. Single photon emission computed tomography (SPECT). Principles and instrumentation. Investig. Radiol. 1985, 20, 897–910. [Google Scholar] [CrossRef]
- Valk, P.E.; Delbeke, D.; Bailey, D.L.; Townsend, D.W.; Maisey, M.N. Positron Emission Tomography; Springer: London, UK, 2005. [Google Scholar]
- Kubota, K. From tumor biology to clinical PET: A review of positron emission tomography (PET) in oncology. Ann. Nucl. Med. 2001, 15, 471–486. [Google Scholar] [CrossRef]
- Wagner, H.N., Jr. A brief history of positron emission tomography (PET). In Seminars in Nuclear Medicine; WB Saunders: Philadelphia, PA, USA, 1998; Volume 28, pp. 213–220. [Google Scholar]
- Wheat, J.M.; Currie, G.M.; Davidson, R.; Kiat, H. An introduction to nuclear medicine. Radiographer 2011, 58, 38–45. [Google Scholar] [CrossRef]
- Mariani, G.; Bruselli, L.; Kuwert, T.; Kim, E.E.; Flotats, A.; Israel, O.; Dondi, M.; Watanabe, N. A review on the clinical uses of SPECT/CT. Eur. J. Nucl. Med. Mol. Imaging 2010, 37, 1959–1985. [Google Scholar] [CrossRef]
- Palmedo, H.; Bucerius, J.; Joe, A.; Strunk, H.; Hortling, N.; Meyka, S.; Roedel, R.; Wolff, M.; Wardelmann, E.; Biersack, H.J.; et al. Integrated PET/CT in differentiated thyroid cancer: Diagnostic accuracy and impact on patient management. J. Nucl. Med. 2006, 47, 616–624. [Google Scholar]
- Liqun, H.; Shufang, L.; Ge, S.; Huan, L.; Jianguo, L.; Quan, A.; Zhongwen, W. Current Applications and Prospects of Radionuclide for Therapy. J. Isot. 2021, 34, 412. [Google Scholar]
- Rösch, F.; Baum, R.P. Generator-based PET radiopharmaceuticals for molecular imaging of tumours: On the way to THERANOSTICS. Dalton Trans. 2011, 40, 6104–6111. [Google Scholar] [CrossRef]
- Notni, J.; Wester, H.J. Re-thinking the role of radiometal isotopes: Towards a future concept for theranostic radiopharmaceuticals. J. Label. Compd. Radiopharm. 2018, 61, 141–153. [Google Scholar] [CrossRef]
- Qaim, S.M.; Scholten, B.; Neumaier, B. New developments in the production of theranostic pairs of radionuclides. J. Radioanal. Nucl. Chem. 2018, 318, 1493–1509. [Google Scholar] [CrossRef]
- Nagarajah, J.; Janssen, M.; Hetkamp, P.; Jentzen, W. Iodine symporter targeting with 124I/131I theranostics. J. Nucl. Med. 2017, 58 (Suppl. S2), 34S–38S. [Google Scholar] [CrossRef]
- Eberlein, U.; Cremonesi, M.; Lassmann, M. Individualized dosimetry for theranostics: Necessary, nice to have, or counterproductive? J. Nucl. Med. 2017, 58 (Suppl. S2), 97S–103S. [Google Scholar] [CrossRef]
- Braccini, S.; Belver-Aguilar, C.; Carzaniga, T.; Dellepiane, G.; Häffner, P.; Scampoli, P. Novel irradiation methods for theranostic radioisotope production with solid targets at the Bern medical cyclotron. In Proceedings of the International Conference on Cyclotrons and their Applications (CYC), Cape Town, South Africa, 22–27 September 2019; pp. 22–27. [Google Scholar]
- Brandt, M.; Cardinale, J.; Aulsebrook, M.L.; Gasser, G.; Mindt, T.L. An overview of PET radiochemistry, part 2: Radiometals. J. Nucl. Med. 2018, 59, 1500–1506. [Google Scholar] [CrossRef]
- Poschenrieder, A.; Schottelius, M.; Schwaiger, M.; Kessler, H.; Wester, H.-J. The influence of different metal-chelate conjugates of pentixafor on the CXCR4 affinity. EJNMMI Res. 2016, 6, 36. [Google Scholar] [CrossRef]
- Ahn, B.C. Personalized medicine based on theranostic radioiodine molecular imaging for differentiated thyroid cancer. BioMed Res. Int. 2016, 2016, 1680464. [Google Scholar] [CrossRef]
- Miller, C.; Rousseau, J.; Ramogida, C.F.; Celler, A.; Rahmim, A.; Uribe, C.F. Implications of physics, chemistry and biology for dosimetry calculations using theranostic pairs. Theranostics 2022, 12, 232. [Google Scholar] [CrossRef]
- Ehlerding, E.B.; Ferreira, C.A.; Aluicio-Sarduy, E.; Jiang, D.; Lee, H.J.; Theuer, C.P.; Engle, J.W.; Cai, W. 86/90Y-based theranostics targeting angiogenesis in a murine breast cancer model. Mol. Pharm. 2018, 15, 2606–2613. [Google Scholar] [CrossRef]
- Ferreira, C.A.; Ehlerding, E.B.; Rosenkrans, Z.T.; Jiang, D.; Sun, T.; Aluicio-Sarduy, E.; Engle, J.W.; Ni, D.; Cai, W. 86/90Y-Labeled monoclonal antibody targeting tissue factor for pancreatic cancer theranostics. Mol. Pharm. 2020, 17, 1697–1705. [Google Scholar] [CrossRef]
- Ming-qi, L.I.; Qi-min, D.; Zuo-yong, C.; Mao-liang, L.I. Production and application of medical radionuclide: Status and urgent problems to be resolved in China. J. Isot. 2013, 26, 186. (In Chinese) [Google Scholar]
- Mushtaq, A. Reactors are indispensable for radioisotope production. Ann. Nucl. Med. 2010, 24, 759–760. [Google Scholar] [CrossRef]
- Xoubi, N.; Primm, R.T., III. Modeling of the High Flux Isotope Reactor Cycle 400; ORNL/TM-2004/251; Oak Ridge National Laboratory: Oak Ridge, Tennessee, USA, 2005. [Google Scholar]
- Ruth, T.J. The medical isotope crisis: How we got here and where we are going. J. Nucl. Med. Technol. 2014, 42, 245–248. [Google Scholar] [CrossRef]
- Koleška, M.; Lahodová, Z.; Šoltés, J.; Viererbl, L.; Ernest, J.; Vinš, M.; Stehno, J. Capabilities of the LVR-15 research reactor for production of medical and industrial radioisotopes. J. Radioanal. Nucl. Chem. 2015, 305, 51–59. [Google Scholar] [CrossRef]
- OECD-NEA. The Supply of Medical Radioisotopes: 2019 Medical Isotope Supply and Capacity Projection for the 2019–2024 Period; OECD-NEA: Paris, France, 2019. [Google Scholar]
- Gao, F.; Lin, L.; Liu, Y.; Ma, X. Production situation and technology prospect of medical isotopes. J. Isot. 2016, 29, 116–120. (In Chinese) [Google Scholar]
- Kurenkov, N.V.; Shubin, Y.N. Radionuclides for nuclear medicine. Медицинская Радиoлoгия И Радиациoнная Безoпаснoсть 1996, 41, 54–63. [Google Scholar]
- IAEA. Nuclear Research Reactors in the World; IAEA: New York, NY, USA, 1997; 120p, ISBN 92-0-100298-X. [Google Scholar]
- Hoedl, S.A.; Updegraff, W.D. The production of medical isotopes without nuclear reactors or uranium enrichment. Sci. Glob. Secur. 2015, 23, 121–153. [Google Scholar] [CrossRef]
- Van der Keur, H. Medical radioisotopes production without a nuclear reactor. 2010. Available online: http://www.laka.org/info/publicaties/2010-medical_isotopes.pdf (accessed on 20 June 2022).
- Ziwei, L.; Yuncheng, H.; Xiaoyu, W.; Jiachen, Z.; Yongfeng, W.; Qunying, H. Production Status and Technical Prospects of Medical Radioisotope 99 Mo/99m Tc. Nucl. Phys. Rev. 2019, 36, 170–183. (In Chinese) [Google Scholar]
- Starovoitova, V.N.; Tchelidze, L.; Wells, D.P. Production of medical radioisotopes with linear accelerators. Appl. Radiat. Isot. 2014, 85, 39–44. [Google Scholar] [CrossRef] [PubMed]
- Kaur, C.D.; Mishra, K.K.; Sahu, A.; Panik, R.; Kashyap, P.; Mishra, S.P.; Kumar, A. Theranostics: New era in nuclear medicine and radiopharmaceuticals. In Medical Isotopes; Naqvi, S.A.R., Imrani, M.B., Eds.; IntechOpen: London, UK, 2020. [Google Scholar]
- Zhang, T.; Fan, M.; Wei, S.; Chen, S.; Yang, F. The present situation and the prospect of medical cyclotrons in China. Sci. China Phys. Mech. Astron. 2011, 54, 260–265. [Google Scholar] [CrossRef]
- Sunderland, J.; Erdahl, C.; Bender, B.; Sensoy, L.; Watkins, G. Considerations, measurements and logistics associated with low-energy cyclotron decommissioning. In Proceedings of the AIP Conference Proceedings, Playa del Carmen, Máxico, 26–29 August 2012; American Institute of Physics: New York, NY, USA, 2012; Volume 1509, pp. 16–20. [Google Scholar]
- International Atomic Energy Agency. Alternative Radionuclide Production with a Cyclotron; IAEA Radioisotopes and Radiopharmaceuticals Reports No. 4; IAEA: Vienna, Austria, 2021. [Google Scholar]
- Chernyaev, A.P.; Varzar, S.M. Particle accelerators in modern world. Phys. At. Nucl. 2014, 77, 1203–1215. [Google Scholar] [CrossRef]
- Goethals, P.E.; Zimmermann, R.G. Cyclotrons used in Nuclear Medicine World Market Report & Directory; MEDraysintell: Louvain-la-Neuve, Belgium, 2015. [Google Scholar]
- Available online: https://www.machinedesign.com/learning-resources/whats-the-difference-between/article/21832184/what-are-the-differences-between-linear-accelerators-cyclotrons-and-synchrotrons (accessed on 1 June 2022).
- Available online: https://www.iaea.org/newscenter/news/cyclotrons-what-are-they-and-where-can-you-find-them (accessed on 10 July 2022).
- Available online: https://www.iaea.org/sites/default/files/gc/gc65-inf2.pdf (accessed on 10 July 2022).
- Available online: https://www.iaea.org/sites/default/files/gc/gc64-inf2.pdf (accessed on 10 July 2022).
- Available online: https://www.iaea.org/sites/default/files/gc/gc61inf-4_en.pdf (accessed on 10 July 2022).
- Available online: https://www.iaea.org/sites/default/files/ntr2015.pdf (accessed on 10 July 2022).
- Available online: https://www.iaea.org/sites/default/files/ntr2014.pdf (accessed on 10 July 2022).
- Available online: https://www-legacy.iaea.org/OurWork/ST/NE/Pess/assets/13-25751_rep_ntr_2013_web.pdf (accessed on 10 July 2022).
- Available online: https://www-legacy.iaea.org/OurWork/ST/NE/Pess/assets/ntr2012_web.pdf (accessed on 10 July 2022).
- Available online: https://www-legacy.iaea.org/OurWork/ST/NE/Pess/assets/ntr2011.pdf (accessed on 10 July 2022).
- Chao, A.W.; Chou, W. (Eds.) Reviews of Accelerator Science and Technology-Volume 3: Accelerators as Photon Sources; World Scientific: Chiyoda City, Tokyo, Japan, 2011. [Google Scholar]
- Leo, K.W.K.; Hashim, S. Accelerator Selection for Industry and Medical Applications. (This is a preprint article, it offers immediate access but has not been peer reviewed).
- Synowiecki, M.A.; Perk, L.R.; Nijsen, J.F.W. Production of novel diagnostic radionuclides in small medical cyclotrons. EJNMMI Radiopharm. Chem. 2018, 3, 3. [Google Scholar] [CrossRef]
- Zuoyuan, D.; Bin, W. Securities Research Report-In-Depth Discussion Series-Nuclear Medicine; Pacific Securities: Guangdong, China, 2019. [Google Scholar]
- Yuan, Z. FDA approved radiopharmaceuticals. In Foreign Medical Sciences; Section of Radiation Medicine and Nuclear Medicine: Tianjin, China, 2000; Volume 24, pp. 161–163. ISSN 1001-098X. [Google Scholar]
- Racette, B.A.; Antenor, J.A.; McGee-Minnich, L.; Moerlein, S.M.; Videen, T.O.; Kotagal, V.; Perlmutter, J.S. [18F] FDOPA PET and clinical features in parkinsonism due to manganism. Mov. Disord. 2005, 20, 492–496. [Google Scholar] [CrossRef]
- Zhao, P.; Zhang, B.; Gao, S.; Li, X. Clinical features, MRI, and 18F-FDG-PET in differential diagnosis of Parkinson disease from multiple system atrophy. Brain Behav. 2020, 10, e01827. [Google Scholar] [CrossRef]
- Rahmim, A.; Zaidi, H. PET versus SPECT: Strengths, limitations and challenges. Nucl. Med. Commun. 2008, 29, 193–207. [Google Scholar] [CrossRef]
- Ruth, T.J.; Wolf, A.P. Absolute cross sections for the production of 18F via the 18O (p, n) 18F reaction. Radiochim. Acta 1979, 26, 21–24. [Google Scholar] [CrossRef]
- Hess, E.; Blessing, G.; Coenen, H.H.; Qaim, S.M. Improved target system for production of high purity [18F] fluorine via the 18O (p, n) 18F reaction. Appl. Radiat. Isot. 2000, 52, 1431–1440. [Google Scholar] [CrossRef]
- Kambali, I.; Parwanto; Suryanto, H.; Huda, N.; Listiawadi, F.D.; Astarina, H.; Ismuha, R.R.; Kardinah. Dependence of 18F Production Yield and Radioactive Impurities on Proton Irradiation Dose. Phys. Res. Int. 2017, 2017, 2124383. [Google Scholar] [CrossRef]
- P Perini, E.A.; Skopchenko, M.; Hong, T.T.; Harianto, R.; Maître, A.; Rodríguez, M.R.R.; de Oliveira Santos, N.; Guo, Y.; Qin, X.; Zeituni, C.A.; et al. Pre-feasibility study for establishing radioisotope and radiopharmaceutical production facilities in developing countries. Curr. Radiopharm. 2019, 12, 187–200. [Google Scholar] [CrossRef]
- Barnhart, T.E.; Nickles, R.J.; Roberts, A.D. Revisiting Low Energy Deuteron Production of [18F] Fluoride and Fluorine for PET. In Proceedings of the AIP Conference Proceedings, Denton, Texas, USA, 12-16 November 2002; American Institute of Physics: New York, NY, USA, 2003; Volume 680, pp. 1086–1089. [Google Scholar]
- Haug, A.R.; Cindea-Drimus, R.; Auernhammer, C.J.; Reincke, M.; Wängler, B.; Uebleis, C.; Schmidt, G.P.; Göke, B.; Bartenstein, P.; Hacker, M. The role of 68Ga-DOTATATE PET/CT in suspected neuroendocrine tumors. J. Nucl. Med. 2012, 53, 1686–1692. [Google Scholar] [CrossRef]
- Kręcisz, P.; Czarnecka, K.; Królicki, L.; Mikiciuk-Olasik, E.b.; Szymański, P. Radiolabeled peptides and antibodies in medicine. Bioconjugate Chem. 2020, 32, 25–42. [Google Scholar] [CrossRef]
- Vaughn, B.A. Chelation Approaches for the Theranostic Radioisotopes of Copper, Scandium and Lutetium; State University of New York at Stony Brook: York, NE, USA, 2021. [Google Scholar]
- Krebs, S.; O’Donoghue, J.A.; Biegel, E.; Beattie, B.J.; Reidy, D.; Lyashchenko, S.K.; Lewis, J.S.; Bodei, L.; Weber, W.A.; Pandit-Taskar, N. Comparison of 68Ga-DOTA-JR11 PET/CT with dosimetric 177Lu-satoreotide tetraxetan (177Lu-DOTA-JR11) SPECT/CT in patients with metastatic neuroendocrine tumors undergoing peptide receptor radionuclide therapy. Eur. J. Nucl. Med. Mol. Imaging 2020, 47, 3047–3057. [Google Scholar] [CrossRef]
- Maffey-Steffan, J.; Scarpa, L.; Svirydenka, A.; Nilica, B.; Mair, C.; Buxbaum, S.; Bektic, J.; von Guggenberg, E.; Uprimny, C.; Horninger, W.; et al. The 68Ga/177Lu-theragnostic concept in PSMA-targeting of metastatic castration–resistant prostate cancer: Impact of post-therapeutic whole-body scintigraphy in the follow-up. Eur. J. Nucl. Med. Mol. Imaging 2020, 47, 695–712. [Google Scholar] [CrossRef]
- Scarpa, L.; Buxbaum, S.; Kendler, D.; Fink, K.; Bektic, J.; Gruber, L.; Decristoforo, C.; Uprimny, C.; Lukas, P.; Horninger, W.; et al. The 68Ga/177Lu theragnostic concept in PSMA targeting of castration-resistant prostate cancer: Correlation of SUVmax values and absorbed dose estimates. Eur. J. Nucl. Med. Mol. Imaging 2017, 44, 788–800. [Google Scholar] [CrossRef]
- Sartor, O.; Herrmann, K. Prostate Cancer Treatment: 177Lu-PSMA-617 Considerations, Concepts, and Limitations. J. Nucl. Med. 2022, 63, 823–829. [Google Scholar] [CrossRef]
- Velikyan, I. 68Ga-based radiopharmaceuticals: Production and application relationship. Molecules 2015, 20, 12913–12943. [Google Scholar] [CrossRef]
- Lin, M.; Waligorski, G.J.; Lepera, C.G. Production of curie quantities of 68Ga with a medical cyclotron via the 68Zn (p, n) 68Ga reaction. Appl. Radiat. Isot. 2018, 133, 1–3. [Google Scholar] [CrossRef]
- Razbash, A.A.; Sevastianov, Y.u.G.; Krasnov, N.N.; Leonov, A.I.; Pavlekin, V.E. Germanium-68 row of products. In Proceedings of the 5th International Conference on Isotopes, 5ICI, Brussels, Belgium, 25–29 April 2005 ; Medimond: Bologna, Italy; p. 147. [Google Scholar]
- Rösch, F. Past, present and future of 68Ge/68Ga generators. Appl. Radiat. Isot. 2013, 76, 24–30. [Google Scholar] [CrossRef]
- Engle, J.; Lopez-Rodriguez, V.; Gaspar-Carcamo, R.; Valdovinos, H.; Valle-Gonzalez, M.; Trejo-Ballado, F.; Severin, G.W.; Barnhart, T.; Nickles, R.; Avila-Rodriguez, M.A. Very high specific activity 66/68Ga from zinc targets for PET. Appl. Radiat. Isot. 2012, 70, 1792–1796. [Google Scholar] [CrossRef]
- Sadeghi, M.; Kakavand, T.; Rajabifar, S.; Mokhtari, L.; Rahimi-Nezhad, A. Cyclotron production of 68Ga via proton-induced reaction on 68Zn target. Nukleonika 2009, 54, 25–28. [Google Scholar]
- Nelson, B.J.; Wilson, J.; Richter, S.; Duke, M.J.M.; Wuest, M.; Wuest, F. Taking cyclotron 68Ga production to the next level: Expeditious solid target production of 68Ga for preparation of radiotracers. Nucl. Med. Biol. 2020, 80, 24–31. [Google Scholar] [CrossRef]
- Mardon, A.; Saleem, H.; Parish, G.; Syed, M.; Inayat, E.; Henry, J.; Heinen, L.; Amiscaray, D.E.; Dong, F.; Mak, E.; et al. What in the World is Medical Isotope Production? Golden Meteorite Press: Edmonton, Alberta, Canada, 2021. [Google Scholar]
- Pandey, M.K.; Byrne, J.F.; Jiang, H.; Packard, A.B.; DeGrado, T.R. Cyclotron production of 68Ga via the 68Zn (p, n) 68Ga reaction in aqueous solution. Am. J. Nucl. Med. Mol. Imaging 2014, 4, 303. [Google Scholar]
- Keinänen, O.; Fung, K.; Brennan, J.M.; Zia, N.; Harris, M.; van Dam, E.; Biggin, C.; Hedt, A.; Stoner, J.; Donnelly, P.S.; et al. Harnessing 64Cu/67Cu for a theranostic approach to pretargeted radioimmunotherapy. Proc. Natl. Acad. Sci. USA 2020, 117, 28316–28327. [Google Scholar] [CrossRef]
- Pfeifer, A.; Knigge, U.; Mortensen, J.; Oturai, P.; Berthelsen, A.K.; Loft, A.; Binderup, T.; Rasmussen, P.; Elema, D.; Klausen, T.L.; et al. Clinical PET of neuroendocrine tumors using 64Cu-DOTATATE: First-in-humans study. J. Nucl. Med. 2012, 53, 1207–1215. [Google Scholar] [CrossRef]
- Avila-Rodriguez, M.A.; Nye, J.A.; Nickles, R.J. Simultaneous production of high specific activity 64Cu and 61Co with 11.4 MeV protons on enriched 64Ni nuclei. Appl. Radiat. Isot. 2007, 65, 1115–1120. [Google Scholar] [CrossRef]
- Szelecsényi, F.; Kovács, Z.; Nagatsu, K.; Zhang, M.R.; Suzuki, K. Excitation function of (p, α) nuclear reaction on enriched 67Zn: Possibility of production of 64Cu at low energy cyclotron. Radiochim. Acta 2014, 102, 465–472. [Google Scholar] [CrossRef]
- Obata, A.; Kasamatsu, S.; McCarthy, D.W.; Welch, M.J.; Saji, H.; Yonekura, Y.; Fujibayashi, Y. Production of therapeutic quantities of 64Cu using a 12 MeV cyclotron. Nucl. Med. Biol. 2003, 30, 535–539. [Google Scholar] [CrossRef]
- McCarthy, D.W.; Shefer, R.E.; Klinkowstein, R.E.; Bass, L.A.; Margeneau, W.H.; Cutler, C.S.; Anderson, C.J.; Welch, M.J. Efficient production of high specific activity 64Cu using a biomedical cyclotron. Nucl. Med. Biol. 1997, 24, 35–43. [Google Scholar] [CrossRef]
- Hilgers, K.; Stoll, T.; Skakun, Y.; Coenen, H.H.; Qaim, S.M. Cross-section measurements of the nuclear reactions natZn (d, x) 64Cu, 66Zn (d, α) 64Cu and 68Zn (p, αn) 64Cu for production of 64Cu and technical developments for small-scale production of 67Cu via the 70Zn (p, α) 67Cu process. Appl. Radiat. Isot. 2003, 59, 343–351. [Google Scholar] [CrossRef]
- Elomaa, V.V.; Jurttila, J.; Rajander, J.; Solin, O. Automation of 64Cu production at Turku PET Centre. Appl. Radiat. Isot. 2014, 89, 74–78. [Google Scholar] [CrossRef]
- Zeisler, S.K.; Pavan, R.A.; Orzechowski, J.; Langlois, R.; Rodrigue, S.; Van Lier, J.E. Production of 64Cu on the Sherbrooke TR-PET cyclotron. J. Radioanal. Nucl. Chem. 2003, 257, 175–177. [Google Scholar] [CrossRef]
- Thieme, S.; Walther, M.; Pietzsch, H.J.; Henniger, J.; Preusche, S.; Mäding, P.; Steinbach, J. Module-assisted preparation of 64Cu with high specific activity. Appl. Radiat. Isot. 2012, 70, 602–608. [Google Scholar] [CrossRef]
- Van der Meulen, N.P.; Hasler, R.; Blanc, A.; Farkas, R.; Benešová, M.; Talip, Z.; Müller, C.; Schibli, R. Implementation of a new separation method to produce qualitatively improved 64Cu. J. Label. Compd. Radiopharm. 2019, 62, 460–470. [Google Scholar] [CrossRef]
- Xie, Q.; Zhu, H.; Wang, F.; Meng, X.; Ren, Q.; Xia, C.; Yang, Z. Establishing reliable Cu-64 production process: From target plating to molecular specific tumor micro-PET imaging. Molecules 2017, 22, 641. [Google Scholar] [CrossRef]
- Ohya, T.; Nagatsu, K.; Suzuki, H.; Fukada, M.; Minegishi, K.; Hanyu, M.; Fukumura, T.; Zhang, M.-R. Efficient preparation of high-quality 64Cu for routine use. Nucl. Med. Biol. 2016, 43, 685–691. [Google Scholar] [CrossRef]
- Verel, I.; Visser GW, M.; Boellaard, R.; Stigter-van Walsum, M.; Snow, G.B.; Van Dongen, G.A. 89Zr immuno-PET: Comprehensive procedures for the production of 89Zr-labeled monoclonal antibodies. J. Nucl. Med. 2003, 44, 1271–1281. [Google Scholar]
- Vento, J.; Mulgaonkar, A.; Woolford, L.; Nham, K.; Christie, A.; Bagrodia, A.; de Leon, A.D.; Hannan, R.; Bowman, I.; McKay, R.M.; et al. PD-L1 detection using 89Zr-atezolizumab immuno-PET in renal cell carcinoma tumorgrafts from a patient with favorable nivolumab response. J. Immunother. Cancer 2019, 7, 144. [Google Scholar] [CrossRef]
- Taghilo, M.; Kakavand, T.; Rajabifar, S.; Sarabadani, P. Cyclotron production of 89Zr: A potent radionuclide for positron emission tomography. Int. J. Phys. Sci. 2012, 7, 1321–1325. [Google Scholar] [CrossRef]
- Ciarmatori, A.; Cicoria, G.; Pancaldi, D.; Infantino, A.; Boschi, S.; Fanti, S.; Marengo, M. Some experimental studies on 89Zr production. Radiochim. Acta 2011, 99, 631–634. [Google Scholar] [CrossRef]
- Sadeghi, M.; Enferadi, M.; Bakhtiari, M. Accelerator production of the positron emitter zirconium-89. Ann. Nucl. Energy 2012, 41, 97–103. [Google Scholar] [CrossRef]
- Tang, Y.; Li, S.; Yang, Y.; Chen, W.; Wei, H.; Wang, G.; Yang, J.; Liao, J.; Luo, S.; Liu, N. A simple and convenient method for production of 89Zr with high purity. Appl. Radiat. Isot. 2016, 118, 326–330. [Google Scholar] [CrossRef] [PubMed]
- Deri, M.A.; Zeglis, B.M.; Francesconi, L.C.; Lewis, J.S. PET imaging with 89Zr: From radiochemistry to the clinic. Nucl. Med. Biol. 2013, 40, 3–14. [Google Scholar] [CrossRef]
- Kandil, S.A.; Spahn, I.; Scholten, B.; Saleh, Z.A.; Saad, S.M.M.; Coenen, H.H.; Qaim, S.M. Excitation functions of (α, xn) reactions on natRb and natSr from threshold up to 26 MeV: Possibility of production of 87Y, 88Y and 89Zr. Appl. Radiat. Isot. 2007, 65, 561–568. [Google Scholar] [CrossRef]
- Liqiang, L.; Feng, W.; Teli, L.; Hua, Z.; Zhi, Y. Production of Iodine-124 and Its Application in PET Molecular Imaging. J. Isot. 2018, 31, 188. (In Chinese) [Google Scholar]
- Freudenberg, L.S.; Jentzen, W.; Stahl, A.; Bockisch, A.; Rosenbaum-Krumme, S.J. Clinical applications of 124I-PET/CT in patients with differentiated thyroid cancer. Eur. J. Nucl. Med. Mol. Imaging 2011, 38, 48–56. [Google Scholar] [CrossRef]
- Aboian, M.S.; Huang, S.-y.; Hernandez-Pampaloni, M.; Hawkins, R.A.; VanBrocklin, H.F.; Huh, Y.; Vo, K.T.; Gustafson, W.C.; Matthay, K.K.; Seo, Y. 124I-MIBG PET/CT to monitor metastatic disease in children with relapsed neuroblastoma. J. Nucl. Med. 2021, 62, 43–47. [Google Scholar] [CrossRef]
- Lewis, J.S. Production, Use and Applications of 124I. PowerPoint Slides; Memorial–Sloan Kettering Cancer Center: New York, NY, USA, 2020. [Google Scholar]
- Braghirolli AM, S.; Waissmann, W.; da Silva, J.B.; dos Santos, G.R. Production of iodine-124 and its applications in nuclear medicine. Appl. Radiat. Isot. 2014, 90, 138–148. [Google Scholar] [CrossRef]
- Bzowski, P.; Borys, D.; Gorczewski, K.; Chmura, A.; Daszewska, K.; Gorczewska, I.; Kastelik-Hryniewiecka, A.; Szydło, M.; d’Amico, A.; Sokół, M. Efficiency of 124I radioisotope production from natural and enriched tellurium dioxide using 124Te (p, xn) 124I reaction. EJNMMI Phys. 2022, 9, 41. [Google Scholar] [CrossRef]
- Bastian, T.; Coenen, H.H.; Qaim, S.M. Excitation functions of 124Te (d, xn) 124,125 I reactions from threshold up to 14 MeV: Comparative evaluation of nuclear routes for the production of 124I. Appl. Radiat. Isot. 2001, 55, 303–308. [Google Scholar] [CrossRef]
- Payolla, F.B.; Massabni, A.C.; Orvig, C. Radiopharmaceuticals for diagnosis in nuclear medicine: A short review. Eclética Química 2019, 44, 11–19. [Google Scholar]
- Schaffer, P.; Bénard, F.; Bernstein, A.; Buckley, K.; Celler, A.; Cockburn, N.; Corsaut, J.; Dodd, M.; Economou, C.; Eriksson, T.; et al. Direct production of 99mTc via 100Mo (p, 2n) on small medical cyclotrons. Phys. Procedia 2015, 66, 383–395. [Google Scholar] [CrossRef]
- Takacs, S.; Hermanne, A.; Ditroi, F.; Tárkányi, F.; Aikawa, M. Reexamination of cross sections of the 100Mo (p, 2n) 99mTc reaction. Nucl. Instrum. Methods Phys. Res. Sect. B Beam Interact. Mater. At. 2015, 347, 26–38. [Google Scholar] [CrossRef]
- Scholten, B.; Lambrecht, R.M.; Cogneau, M.; Ruiz, H.V.; Qaim, S.M. Excitation functions for the cyclotron production of 99mTc and 99Mo. Appl. Radiat. Isot. 1999, 51, 69–80. [Google Scholar] [CrossRef]
- Rodrigue, S.; van Lier, J.E.; van Lier, M.A.S.E. Cyclotron production of 99mTc: An approach to the medical isotope crisis. J. Nucl. Med. 2010, 51, 13N. [Google Scholar]
- Hoehr, C.; Bénard, F.; Buckley, K.; Crawford, J.; Gottberg, A.; Hanemaayer, V.; Kunz, P.; Ladouceur, K.; Radchenko, V.; Ramogida, C.; et al. Medical isotope production at TRIUMF–from imaging to treatment. Phys. Procedia 2017, 90, 200–208. [Google Scholar] [CrossRef]
- Pillai, M.R.A.; Dash, A.; Knapp, F.F.R. Sustained availability of 99mTc: Possible paths forward. J. Nucl. Med. 2013, 54, 313–323. [Google Scholar] [CrossRef]
- Lebeda, O.; van Lier, E.J.; Štursa, J.; Ráliš, J.; Zyuzin, A. Assessment of radionuclidic impurities in cyclotron produced 99mTc. Nucl. Med. Biol. 2012, 39, 1286–1291. [Google Scholar] [CrossRef]
- Pupillo, G.; Esposito, J.; Gambaccini, M.; Haddad, F.; Michel, N. Experimental cross section evaluation for innovative 99Mo production via the (α, n) reaction on 96Zr target. J. Radioanal. Nucl. Chem. 2014, 302, 911–917. [Google Scholar] [CrossRef]
- Hagiwara, M.; Yashima, H.; Sanami, T.; Yonai, S. Measurement of the excitation function of 96Zr (α, n) 99Mo for an alternative production source of medical radioisotopes. J. Radioanal. Nucl. Chem. 2018, 318, 569–573. [Google Scholar] [CrossRef]
- Jacobson, A.F.; Deng, H.; Lombard, J.; Lessig, H.J.; Black, R.R. 123I-meta-iodobenzylguanidine scintigraphy for the detection of neuroblastoma and pheochromocytoma: Results of a meta-analysis. J. Clin. Endocrinol. Metab. 2010, 95, 2596–2606. [Google Scholar] [CrossRef]
- Eslami, M.; Kakavand, T.; Mirzaii, M. Simulation of Proton beam using the MCNPX code; A prediction for the production of 123 I via 124 Xe (p, x) 123 I reaction. In Proceedings of the DAE-BRNS symposium on nuclear physics, Mumbai, India, 2–6 December 2013; Volume 58, p. 860. [Google Scholar]
- EXFOR. Experimental Nuclear Reaction Data. 2011. Available online: http://www-nds.iaea.org/exfor (accessed on 15 June 2022).
- Kakavand, T.; Sadeghi, M.; Kamali Moghaddam, K.; Shokri Bonab, S.; Fateh, B. Computer simulation techniques to design Xenon-124 solid target for iodine-123 production. Iran. J. Radiat. Res. 2008, 5, 207–212. [Google Scholar]
- Tárkányi, F.; Qaim, S.M.; Stöcklin, G.; Sajjad, M.; Lambrecht, R.M.; Schweickert, H. Excitation functions of (p, 2n) and (p, pn) reactions and differential and integral yields of 123I in proton induced nuclear reactions on highly enriched 124Xe. Int. J. Radiat. Appl. Instrumentation. Part A Appl. Radiat. Isot. 1991, 42, 221–228. [Google Scholar] [CrossRef]
- Hupf, H.B.; Beaver, J.E.; Armbruster, J.M.; Pendola, J.P. Production of ultra-pure I-123 from the 123 Te (p, n) 123 I reaction. AIP Conf Proc 2001, 576, 845–848. [Google Scholar]
- Mertens, J. New Development in Radio-Iodinated Radiopharmaceuticals for SPECT and Radionuclide Therapy. In Proceedings of the IAEA-CN-130 International Symposium on Trends in Radiopharmaceuticals ISTR-2005, Vienna, Austria, 14–18 November 2005; IAEA: New York, NY, USA; pp. 101–103. [Google Scholar]
- Scholten, B.; Qaim, S.M.; Stöcklin, G. Excitation functions of proton induced nuclear reactions on natural tellurium and enriched 123Te: Production of 123I via the 123Te (p, n) 123I-process at a low-energy cyclotron. Int. J. Radiat. Appl. Instrumentation. Part A Appl. Radiat. Isot. 1989, 40, 127–132. [Google Scholar] [CrossRef]
- Kratochwil, C.; Haberkorn, U.; Giesel, F.L. 225Ac-PSMA-617 for therapy of prostate cancer. In Seminars in Nuclear Medicine; WB Saunders: Philadelphia, PA, USA, 2020; Volume 50, pp. 133–140. [Google Scholar]
- Kratochwil, C.; Bruchertseifer, F.; Giesel, F.L.; Weis, M.; Verburg, F.A.; Mottaghy, F.; Kopka, K.; Apostolidis, C.; Haberkorn, U.; Morgenstern, A. 225Ac-PSMA-617 for PSMA-targeted α-radiation therapy of metastatic castration-resistant prostate cancer. J. Nucl. Med. 2016, 57, 1941–1944. [Google Scholar] [CrossRef]
- Zacherl, M.J.; Gildehaus, F.J.; Mittlmeier, L.; Böning, G.; Gosewisch, A.; Wenter, V.; Unterrainer, M.; Schmidt-Hegemann, N.; Belka, C.; Kretschmer, A. First clinical results for PSMA-targeted α-therapy using 225Ac-PSMA-I&T in advanced-mCRPC patients. J. Nucl. Med. 2021, 62, 669–674. [Google Scholar]
- Królicki, L.; Kunikowska, J.; Bruchertseifer, F.; Koziara, H.; Królicki, B.; Jakuciński, M.; Pawlak, D.; Rola, R.; Morgenstern, A.; Rosiak, E.; et al. 225Ac-and 213Bi-substance P analogues for glioma therapy. In Seminars in Nuclear Medicine; WB Saunders: Philadelphia, PA, USA, 2020; Volume 50, pp. 141–151. [Google Scholar]
- Nagatsu, K.; Suzuki, H.; Fukada, M.; Ito, T.; Ichinose, J.; Honda, Y.; Minegishi, K.; Higashi, T.; Zhang, M.-R. Cyclotron production of 225Ac from an electroplated 226Ra target. Eur. J. Nucl. Med. Mol. Imaging 2021, 49, 279–289. [Google Scholar] [CrossRef]
- Lee, K.C. 225Ac production at KIRAMS. In Proceedings of the IAEA Workshop on the Supply of 225Ac, Vienna, Austria, 9–10 October 2018, (unpublished). [Google Scholar]
- Bruchertseifer, F.; Kellerbauer, A.; Malmbeck, R.; Morgenstern, A. Targeted alpha therapy with bismuth-213 and actinium-225: Meeting future demand. J. Label. Compd. Radiopharm. 2019, 62, 794–802. [Google Scholar] [CrossRef]
- Ermolaev, S.; Zhuikov, B.; Kokhanyuk, V.; Matushko, V.; Kalmykov, S.N.; Aliev, R.A.; Tananaev, I.G.; Myasoedov, B.F. Production of actinium, thorium and radium isotopes from natural thorium irradiated with protons up to 141 MeV. Radiochim. Acta 2012, 100, 223–229. [Google Scholar] [CrossRef]
- Chen, D.; Liu, W.; Huang, Q.; Cao, S.; Tian, W.; Yin, X.; Tan, C.; Wang, J.; Chu, J.; Jia, Z.; et al. Accelerator Production of the Medical Isotope 211At and Monoclonal Antibody Labeling. Acta Chim. Sin. 2021, 79, 1376–1384. [Google Scholar] [CrossRef]
- Watabe, T.; Kaneda-Nakashima, K.; Shirakami, Y.; Liu, Y.; Ooe, K.; Teramoto, T.; Toyoshima, A.; Shimosegawa, E.; Nakano, T.; Kanai, Y.; et al. Targeted alpha therapy using astatine (211At)-labeled phenylalanine: A preclinical study in glioma bearing mice. Oncotarget 2020, 11, 1388. [Google Scholar] [CrossRef]
- Zalutsky, M.R.; Reardon, D.A.; Akabani, G.; Coleman, R.E.; Friedman, A.H.; Friedman, H.S.; McLendon, R.E.; Wong, T.Z.; Bigner, D.D. Clinical experience with α-particle–emitting 211At: Treatment of recurrent brain tumor patients with 211At-labeled chimeric antitenascin monoclonal antibody 81C6. J. Nucl. Med. 2008, 49, 30–38. [Google Scholar] [CrossRef] [PubMed]
- Lindegren, S.; Albertsson, P.; Bäck, T.; Jensen, H.; Palm, S.; Aneheim, E. Realizing clinical trials with astatine-211: The chemistry infrastructure. Cancer Biother. Radiopharm. 2020, 35, 425–436. [Google Scholar] [CrossRef]
- Cederkrantz, E.; Andersson, H.; Bernhardt, P.; Bäck, T.; Hultborn, R.; Jacobsson, L.; Jensen, H.; Lindegren, S.; Ljungberg, M.; Magnander, T.; et al. Absorbed doses and risk estimates of 211At-MX35 F (ab’) 2 in intraperitoneal therapy of ovarian cancer patients. Int. J. Radiat. Oncol. Biol. Phys. 2015, 93, 569–576. [Google Scholar] [CrossRef]
- Washiyama, K.; Oda, T.; Sasaki, S.; Aoki, M.; Gomez, F.L.G.; Taniguchi, M.; Nishijima, K.-i.; Takahashi, K. At-211 production using the CYPRIS MP-30. J. Med. Imaging Radiat. Sci. 2019, 50, S42. [Google Scholar] [CrossRef]
- Alfarano, A.; Abbas, K.; Holzwarth, U.; Bonardi, M.; Groppi, F.; Alfassi, Z.; Menapace, E.; Gibson, P. Thick target yield measurement of 211At through the nuclear reaction 209Bi (α, 2n). In Journal of Physics: Conference Series; IOP Publishing: Bristol, UK, 2006; Volume 41, p. 009. [Google Scholar]
- Feng, Y.; Zalutsky, M.R. Production, purification and availability of 211At: Near term steps towards global access. Nucl. Med. Biol. 2021, 100, 12–23. [Google Scholar] [CrossRef]
- Guérard, F.; Gestin, J.F.; Brechbiel, M.W. Production of [211At]-astatinated radiopharmaceuticals and applications in targeted α-particle therapy. Cancer Biother. Radiopharm. 2013, 28, 1–20. [Google Scholar] [CrossRef]
- Cullinane, C.; Jeffery, C.M.; Roselt, P.D.; van Dam, E.M.; Jackson, S.; Kuan, K.; Jackson, P.; Binns, D.; van Zuylekom, J.; Harris, M.; et al. Peptide receptor radionuclide therapy with 67Cu-CuSarTATE is highly efficacious against a somatostatin-positive neuroendocrine tumor model. J. Nucl. Med. 2020, 61, 1800–1805. [Google Scholar] [CrossRef]
- DeNardo, S.J.; DeNardo, G.L.; Kukis, D.L.; Shen, S.; Kroger, L.A.; DeNardo, D.A.; Goldstein, D.S.; Mirick, G.R.; Salako, Q.; Mausner, L.F.; et al. 67Cu-21T-BAT-Lym-1 pharmacokinetics, radiation dosimetry, toxicity and tumor regression in patients with lymphoma. J. Nucl. Med. 1999, 40, 302–310. [Google Scholar]
- Pupillo, G.; Sounalet, T.; Michel, N.; Mou, L.; Esposito, J.; Haddad, F. New production cross sections for the theranostic radionuclide 67Cu. Nucl. Instrum. Methods Phys. Res. Sect. B Beam Interact. Mater. At. 2018, 415, 41–47. [Google Scholar] [CrossRef]
- Katabuchi, T.; Watanabe, S.; Ishioka, N.S.; Iida, Y.; Hanaoka, H.; Endo, K.; Matsuhashi, S. Production of 67Cu via the 68Zn (p, 2p) 67Cu reaction and recovery of 68Zn target. J. Radioanal. Nucl. Chem. 2008, 277, 467–470. [Google Scholar] [CrossRef]
- Mou, L.; Martini, P.; Pupillo, G.; Cieszykowska, I.; Cutler, C.S.; Mikołajczak, R. 67Cu production capabilities: A mini review. Molecules 2022, 27, 1501. [Google Scholar] [CrossRef] [PubMed]
- Hovhannisyan, G.H.; Stepanyan, A.V.; Saryan, E.R.; Amirakyan, L.A. Methods of Production the Isotope 67Cu. J. Contemp. Phys. (Armen. Acad. Sci.) 2020, 55, 183–190. [Google Scholar] [CrossRef]
- Kin, T.; Nagai, Y.; Iwamoto, N.; Minato, F.; Iwamoto, O.; Hatsukawa, Y.; Segawa, M.; Harada, H.; Konno, C.; Ochiai, K.; et al. New production routes for medical isotopes 64Cu and 67Cu using accelerator neutrons. J. Phys. Soc. Jpn. 2013, 82, 034201. [Google Scholar] [CrossRef]
- Szelecsényi, F.; Steyn, G.F.; Dolley, S.G.; Kovács, Z.; Vermeulen, C.; Van der Walt, T.N. Investigation of the 68Zn (p, 2p) 67Cu nuclear reaction: New measurements up to 40 MeV and compilation up to 100 MeV. Nucl. Instrum. Methods Phys. Res. Sect. B Beam Interact. Mater. At. 2009, 267, 1877–1881. [Google Scholar] [CrossRef]
- Pandey, M.K.; DeGrado, T.R. Cyclotron production of PET radiometals in liquid targets: Aspects and prospects. Curr. Radiopharm. 2021, 14, 325–339. [Google Scholar] [CrossRef]
- Deng, X.; Rong, J.; Wang, L.; Vasdev, N.; Zhang, L.; Josephson, L.; Liang, S.H. Chemistry for positron emission tomography: Recent advances in 11C-, 18F-, 13N-, and 15O-labeling reactions. Angew. Chem. Int. Ed. 2019, 58, 2580–2605. [Google Scholar] [CrossRef]
- McQuade, P.; Rowland, D.J.; Lewis, J.S.; Welch, M.J. Positron-emitting isotopes produced on biomedical cyclotrons. Curr. Med. Chem. 2005, 12, 807–818. [Google Scholar] [CrossRef]
- Schmitz, J. The production of [124I] iodine and [86Y] yttrium. Eur. J. Nucl. Med. Mol. Imaging 2011, 38, 4–9. [Google Scholar] [CrossRef]
- van der Meulen, N.P.; Bunka, M.; Domnanich, K.A.; Müller, C.; Haller, S.; Vermeulen, C.; Türler, A.; Schibli, R. Cyclotron production of 44Sc: From bench to bedside. Nucl. Med. Biol. 2015, 42, 745–751. [Google Scholar] [CrossRef]
- van der Meulen, N.P.; Hasler, R.; Talip, Z.; Grundler, P.V.; Favaretto, C.; Umbricht, C.A.; Müller, C.; Dellepiane, G.; Carzaniga, T.S.; Braccini, S. Developments toward the implementation of 44Sc production at a medical cyclotron. Molecules 2020, 25, 4706. [Google Scholar] [CrossRef]
- Lagunas-Solar, M.C.; Jungerman, J.A.; Paulson, D.W. Cyclotron production of Thallium-201 via the 205 Tl (p, 5n) 201 Pb→ 201 Tl reaction. In Proceedings of the International Symposium on Radiopharmaceuticals, Seattle, WA, USA, 18–23 March 1979; Society of Nuclear Medicine: New York, NY, USA; pp. 779–789. [Google Scholar]
- Misiak, R.; Walczak, R.; Wąs, B.; Bartyzel, M.; Mietelski, J.W.; Bilewicz, A. 47Sc production development by cyclotron irradiation of 48Ca. J. Radioanal. Nucl. Chem. 2017, 313, 429–434. [Google Scholar] [CrossRef]
- Abel, E.P.; Domnanich, K.; Clause, H.K.; Kalman, C.; Walker, W.; Shusterman, J.A.; Greene, J.; Gott, M.; Severin, G.W. Production, collection, and purification of 47Ca for the generation of 47Sc through isotope harvesting at the national superconducting cyclotron laboratory. ACS Omega 2020, 5, 27864–27872. [Google Scholar] [CrossRef]
- Lawrence, J.H. Nuclear physics and therapy: Preliminary report on a new method for the treatment of leukemia and polycythemia. Radiology 1940, 35, 51–60. [Google Scholar] [CrossRef]
- Hupf, H.B.; Beaver, J.E. Cyclotron production of carrier-free gallium-67. Int. J. Appl. Radiat. Isot. 1970, 21, 75–76. [Google Scholar] [CrossRef]
- do Carmo, S.J.C.; Scott, P.J.H.; Alves, F. Production of radiometals in liquid targets. EJNMMI Radiopharm. Chem. 2020, 5, 2. [Google Scholar] [CrossRef]
- Skliarova, H.; Cisternino, S.; Cicoria, G.; Marengo, M.; Cazzola, E.; Gorgoni, G.; Palmieri, V. Medical Cyclotron Solid Target Preparation by Ultrathick Film Magnetron Sputtering Deposition. Instruments 2019, 3, 21. [Google Scholar] [CrossRef]
- McNeil, B.L.; Robertson, A.K.; Fu, W.; Yang, H.; Hoehr, C.; Ramogida, C.F.; Schaffer, P. Production, purification, and radiolabeling of the 203Pb/212Pb theranostic pair. EJNMMI Radiopharm. Chem. 2021, 6, 6. [Google Scholar] [CrossRef]
- Gracheva, N.; Carzaniga, T.S.; Schibli, R.; Braccini, S.; van der Meulen, N.P. 165Er: A new candidate for Auger electron therapy and its possible cyclotron production from natural holmium targets. Appl. Radiat. Isot. 2020, 159, 109079. [Google Scholar] [CrossRef]
- Nelson, B.J.B.; Wilson, J.; Andersson, J.D.; Wuest, F. High yield cyclotron production of a novel 133/135La theranostic pair for nuclear medicine. Sci. Rep. 2020, 10, 22203. [Google Scholar] [CrossRef] [PubMed]
- Dey, M.K.; Gupta, A.D.; Chakrabarti, A. Design of ultra-light superconducting proton cyclotron for production of isotopes for medical applications. Proc. Cyclotr. 2013, 2013, 447–450. [Google Scholar]
- Waites, L.H.; Alonso, J.R.; Conrad, J. IsoDAR: A cyclotron-based neutrino source with applications to medical isotope production. AIP Conf. Proc 2019, 2160, 040001. [Google Scholar]
- Waites, L.H.; Alonso, J.; Conrad, J.M.; Koser, D.; Winklehner, D. Tools for the Development and Applications of the IsoDAR Cyclotron. Energy (MeV/Nucl.) 2021, 60, 30. [Google Scholar]
- Pramudita, A. Linacs for medical isotope production. In Proceeding on the scientific meeting and presentation on accelerator technology and its applications: Physics, nuclear reactor, Yogyakarta, Indonesia, 13 December 2011; National Nuclear Energy Agency: Tangerang, Jawa Barat, Indonesia, 2012; Volume 47, pp. 11–16. [Google Scholar]
- Griswold, J.R.; Medvedev, D.G.; Engle, J.W.; Copping, R.; Fitzsimmons, J.; Radchenko, V.; Cooley, J.; Fassbender, M.; Denton, D.; Murphy, K.; et al. Large scale accelerator production of 225Ac: Effective cross sections for 78–192 MeV protons incident on 232Th targets. Appl. Radiat. Isot. 2016, 118, 366–374. [Google Scholar] [CrossRef]
- Zhuikov, B.L.; Ermolaev, S.V. Radioisotope research and development at the Linear Accelerator of the Institute for Nuclear Research of RAS. Phys.-Uspekhi 2021, 64, 1311. [Google Scholar] [CrossRef]
- Antipov, K.; Ayzatsky, M.; Akchurin, Y.I.; Boriskin, V.; Beloglasov, V.; Biller, E.; Demidov, N.; Dikiy, N.; Dovbnya, A.; Dovbush, L.; et al. Electron linacs in NSC KIPT: R&D and application. Вoпрoсы Атoмнoй Науки И Техники 2001, 37, 40–47. [Google Scholar]
- Danagulyan, A.S.; Hovhannisyan, G.H.; Bakhshiyan, T.M.; Avagyan, R.H.; Avetisyan, A.E.; Kerobyan, I.A.; Dallakyan, R.K. Formation of medical radioisotopes 111In, 117m Sn, 124Sb, and 177Lu in photonuclear reactions. Phys. At. Nucl. 2015, 78, 447–452. [Google Scholar] [CrossRef]
- Courtney, W.; Sowder, K.; McGyver, M.; Stevenson, N.; Brown, D. The challenges of commercial isotope production on a linear accelerator. Nucl. Instrum. Methods Phys. Res. Sect. B Beam Interact. Mater. At. 2007, 261, 739–741. [Google Scholar] [CrossRef]
- Matthews, M.; Saey, P.; Bowyer, T.; Vandergrift, G.; Cutler, N.R.C.; Ponsard, B.; Mikolajczak, R.; Tsipenyuk, Y.; Solin, L.; Fisher, D.; et al. Workshop on Signatures of Medical and Industrial Isotope Production: A Review; Pacific Northwest National Laboratory: Richland, Washington, USA, 2010. [Google Scholar]
- Dikiy, N.P.; Dovbnya, A.N.; Medvedyeva, E.P.; Tur, Y.D. Experience of Technetium-99m Generation for Nuclear Medicine on Electron Linac; VANT: Kharkov, Ukraine, 1997; pp. 165–167. [Google Scholar]
- Uvarov, V.L.; Dikiy, N.P.; Dovbnya, A.N.; Medvedyeva, Y.P.; Pugachov, G.D.; Tur, Y.D. Electron Accelerator’s Based Production of Technetium-99m for Nuclear Medicine. Bull. Amer. Phys. Soc. 1997, 42, 1338. [Google Scholar]
- De Jong, M. Producing medical isotopes using X-rays. Sin Proc. IPAC 2012, 12, 3177. [Google Scholar]
- Chemerisov, S.; Bailey, J.; Heltemes, T.; Jonah, C.; Makarashvili, V.; Tkac, P.; Rotsch, D.; Virgo, M.; Vandegrift, G. Results of the Six-and-a-Half Day Electron-Accelerator Irradiation of Enriched Mo-100 Targets for the Production of Mo-99; Argonne National Lab.(ANL): Argonne, IL, USA, 2016. [Google Scholar]
- Takeda, T.; Fujiwara, M.; Kurosawa, M.; Takahashi, N.; Tamura, M.; Kawabata, T.; Fujikawa, Y.; Suzuki, K.N.; Abe, N.; Kubota, T.; et al. 99mTc production via the (γ, n) reaction on natural Mo. J. Radioanal. Nucl. Chem. 2018, 318, 811–821. [Google Scholar] [CrossRef]
- Szpunar, B.; Rangacharyulu, C.; Date, S.; Ejiri, H. Estimate of production of medical isotopes by photo-neutron reaction at the Canadian light source. Nucl. Instrum. Methods Phys. Res. Sect. A Accel. Spectrometers Detect. Assoc. Equip. 2013, 729, 41–50. [Google Scholar] [CrossRef]
- Babcock, C.; Goodacre, T.D.; Amani, P.; Au, M.; Bricault, P.; Brownell, M.; Cade, B.; Chen, K.; Egoriti, L.; Johnson, J.; et al. Offline target and ion source studies for TRIUMF-ARIEL. Nucl. Instrum. Methods Phys. Res. Sect. B Beam Interact. Mater. At. 2020, 463, 464–467. [Google Scholar] [CrossRef]
- Danon, Y.; Block, R.C.; Testa, R.; Testa, R.; Moore, H. Medical isotope production using a 60 MeV linear electron accelerator. Trans.-Am. Nucl. Soc. 2008, 98, 894. [Google Scholar]
- Yagi, M.; Kondo, K. Preparation of carrier-free 67Cu by the 68Zn (γ, p) reaction. Int. J. Appl. Radiat. Isot. 1978, 29, 757–759. [Google Scholar] [CrossRef]
- Hovhannisyan, G.H.; Bakhshiyan, T.M.; Dallakyan, R.K. Photonuclear production of the medical isotope 67Cu. Nucl. Instrum. Methods Phys. Res. Sect. B Beam Interact. Mater. At. 2021, 498, 48–51. [Google Scholar] [CrossRef]
- Gopalakrishna, A.; Suryanarayana, S.; Naik, H.; Nayak, B.; Patil, B.; Devraju, S.; Upreti, R.; Kinhikar, R.; Deshpande, D.; Maletha, P.; et al. Production of 99Mo and 64Cu in a mixed field of photons and neutrons in a clinical electron linear accelerator. J. Radioanal. Nucl. Chem. 2018, 317, 1409–1417. [Google Scholar] [CrossRef]
- Maslov, O.D.; Sabel’nikov, A.V.; Dmitriev, S.N. Preparation of 225Ac by 226Ra (γ, n) photonuclear reaction on an electron accelerator, MT-25 microtron. Radiochemistry 2006, 48, 195–197. [Google Scholar] [CrossRef]
- Robertson, A.K.H.; Ramogida, C.F.; Schaffer, P.; Radchenko, V. Development of 225Ac radiopharmaceuticals: TRIUMF perspectives and experiences. Curr. Radiopharm. 2018, 11, 156–172. [Google Scholar] [CrossRef]
- Inagaki, M.; Sekimoto, S.; Tanaka, W.; Tadokoro, T.; Ueno, Y.; Kani, Y.; Ohtsuki, T. Production of 47Sc, 67Cu, 68Ga, 105Rh, 177Lu, and 188Re using electron linear accelerator. J. Radioanal. Nucl. Chem. 2019, 322, 1703–1709. [Google Scholar] [CrossRef]
- Radel, R.; Sengbusch, E.; Piefer, G. Recent Progress on the PNL Accelerator-Based Intense Fusion Neutron Source. Trans. Am. Nucl. Soc. 2016, 114, 11–12. [Google Scholar]
- Rotsch, D.A.; Brown, M.A.; Nolen, J.A.; Brossard, T.; Henning, W.F.; Chemerisov, S.D.; Gromov, R.G.; Greene, J. Electron linear accelerator production and purification of scandium-47 from titanium dioxide targets. Appl. Radiat. Isot. 2018, 131, 77–82. [Google Scholar] [CrossRef] [PubMed]
- Melville, G.; Allen, B.J. Cyclotron and linac production of Ac-225. Appl. Radiat. Isot. 2009, 67, 549–555. [Google Scholar] [CrossRef]
- Deshpande, A.; Dixit, T.; Bhat, S.; Jadhav, P.; Kottawar, A.; Krishnan, R.; Thakur, K.; Vidwans, M.; Waingankar, A. Design of High Energy Linac for Generation of Isotopes for Medical Applications. In Proceedings of the IPAC 2021-12th International Particle Accelerator Conference, Campinas, SP, Brazi, 24-28 May 2021; JACoW Publishing: Geneva, Switzerland, 2021; pp. 2472–2474. [Google Scholar]
- Leung, K.N. New compact neutron generator system for multiple applications. Nucl. Technol. 2020, 206, 1607–1614. [Google Scholar] [CrossRef]
- Kononov, V.N.; Bokhovko, M.V.; Kononov, O.E.; Soloviev, N.A.; Chu, W.T.; Nigg, D. Accelerator-based fast neutron sources for neutron therapy. Nucl. Instrum. Methods Phys. Res. Sect. A Accel. Spectrometers Detect. Assoc. Equip. 2006, 564, 525–531. [Google Scholar] [CrossRef]
- Cloth, P.; Conrads, H. Neutronics of a dense-plasma focus—An investigation of a fusion plasma. Nucl. Sci. Eng. 1977, 62, 591–600. [Google Scholar] [CrossRef]
- Csikai, J.; Dóczi, R. Applications of neutron generators. Handb. Nucl. Chem. 2011, 3, 363. [Google Scholar]
- Reijonen, J. Compact neutron generators for medical, home land security, and planetary exploration. In Proceedings of the 2005 Particle Accelerator Conference, Knoxville, TN, USA, 16–20 May 2005; pp. 49–53. [Google Scholar]
- Dovbnya, A.N.; Kuplennikov, E.L.; Tsymba, V.A.; Krasil’nikov, V.V. Possibility of 99mT c production at neutron generator. Вoпрoсы Атoмнoй Науки И Техники 2009, 5, 64–66. [Google Scholar]
- Pagdon, K.; Gentile, C.; Cohen, A.; Ascione, G.; Baker, G. Production of Tc-99m from naturally occurring molybdenum absent uranium. In Proceedings of the 2011 IEEE/NPSS 24th Symposium on Fusion Engineering, Chicago, IL, USA, 26–30 June 2011; pp. 1–4. [Google Scholar]
- Mausolf, E.J.; Johnstone, E.V.; Mayordomo, N.; Williams, D.L.; Guan, E.Y.Z.; Gary, C.K. Fusion-Based Neutron Generator Production of Tc-99m and Tc-101: A Prospective Avenue to Technetium Theranostics. Pharmaceuticals 2021, 14, 875. [Google Scholar] [CrossRef]
- National Academies of Sciences, Engineering, and Medicine. Molybdenum-99 for Medical Imaging; National Academies Press: Washington, DC, USA, 2016. [Google Scholar]
- Youker, A.J.; Chemerisov, S.D.; Tkac, P.; Kalensky, M.; Heltemes, T.A.; Rotsch, D.A.; Vandegrift, G.F.; Krebs, J.F.; Makarashvili, V.; Stepinski, D.C. Fission-produced Mo-99 without a nuclear reactor. J. Nucl. Med. 2017, 58, 514–517. [Google Scholar] [CrossRef][Green Version]
- Leung, K.N.; Leung, J.K.; Melville, G. Feasibility study on medical isotope production using a compact neutron generator. Appl. Radiat. Isot. 2018, 137, 23–27. [Google Scholar] [CrossRef] [PubMed]
- Badwar, S.; Ghosh, R.; Lawriniang, B.M.; Vansola, V.; Sheela, Y.; Naik, H.; Naik, Y.; Suryanarayana, S.V.; Jyrwa, B.; Ganesan, S. Measurement of formation cross-section of 99Mo from the 98Mo (n, γ) and 100Mo (n, 2n) reactions. Appl. Radiat. Isot. 2017, 129, 117–123. [Google Scholar] [CrossRef] [PubMed]
- Auditore, L.; Amato, E.; Baldari, S. Theoretical estimation of 64Cu production with neutrons emitted during 18F production with a 30 MeV medical cyclotron. Appl. Radiat. Isot. 2017, 122, 229–234. [Google Scholar] [CrossRef] [PubMed]
- Pandit-Taskar, N.; Batraki, M.; Divgi, C.R. Radiopharmaceutical therapy for palliation of bone pain from osseous metastases. J. Nucl. Med. 2004, 45, 1358–1365. [Google Scholar]
- Kim, S.K.; Choi, H.D. New technique for Producing Therapeutic Radioisotope 89Sr. In Proceedings of the Korean Nuclear Society Conference, jeju, Korea, 26–26 May 2005; Korean Nuclear Society: Seoul, Korea; pp. 751–752. [Google Scholar]
- Molla, N.I.; Basunia, S.; Miah, M.R.; Hossain, S.M.; Rahman, M.M.; Spellerberg, S.; Qaim, S.M. Radiochemical Study of 45Sc (n, p) 45Ca and 89Y (n, p) 89Sr Reactions in the Neutron Energy Range of 13.9 to 14.7 MeV. Radiochim. Acta 1998, 80, 189–192. [Google Scholar] [CrossRef]
- Capogni, M.; Capone, M.; Pietropaolo, A.; Fazio, A.; Dellepiane, G.; Falconi, R.; Colangeli, A.; Palomba, S.; Valentini, G.; Fantuzi, M.; et al. 64Cu production by 14 MeV neutron beam. J. Neutron Res. 2020, 22, 257–264. [Google Scholar] [CrossRef]
- Voyles, A.; Basunia, M.; Batchelder, J.; Bauer, J.; Becker, T.; Bernstein, L.; Matthews, E.; Renne, P.; Rutte, D.; Unzueta, M.; et al. Measurement of the 64Zn, 47Ti (n, p) cross sections using a DD neutron generator for medical isotope studies. Nucl. Instrum. Methods Phys. Res. Sect. B Beam Interact. Mater. At. 2017, 410, 230–239. [Google Scholar] [CrossRef]
- Mellard, S.C.; Biegalski, S.R. MCNP based simulations for the optimization of radioxenon via DD and DT neutron generators from 132Xe. J. Radioanal. Nucl. Chem. 2018, 318, 313–322. [Google Scholar] [CrossRef]
- Weicheng, Z. Short-lived medical isotopes produced by 14MeV neutron generator. At. Energy Sci. Technol 1981, 03, 366–368. (In Chinese) [Google Scholar]
- Yuntao, L.; Shizhong, A.; Jixin, L. Current Situation and Development Trend of Nuclear Technology Application. Sci. Technol. Rev. 2022, 40, 88–97. (In Chinese) [Google Scholar]
- Huang, Z.; Wang, J.; Ma, Z.; Lu, X.; Wei, Z.; Zhang, S.; Liu, Y.; Zhang, Z.; Zhang, Y.; Yao, Z. Design of a compact D–D neutron generator. Nucl. Instrum. Methods Phys. Res. Sect. A Accel. Spectrometers Detect. Assoc. Equip. 2018, 904, 107–112. [Google Scholar] [CrossRef]
- Jixin, L.; Yuqing, C.; Guang, L.; Xuesong, D.; Yijia, S.; Laicheng, Q.; Yuping, L.; Hua, J.; Guiqun, L. Production process of 64Cu by C-30 cyclotron. In Annual Report for China Institute of Atomic Energy; China Institute of Atomic Energy: Beijing, China, 2013. [Google Scholar]
| Country | Reactor | Power [MW] | Year of First Criticality | Estimated Retirement Time |
|---|---|---|---|---|
| Belgium | BR-2 | 100 | 1961 | 2026 |
| Netherlands | HFR | 45 | 1961 | 2024 |
| Czech Republic | LVR-15 | 10 | 1957 | 2028 |
| Poland | MARIA | 20 | 1974 | 2030 |
| South Africa | SAFARI-1 | 20 | 1965 | 2030 |
| Russia | WWR-TS | 15 | 1964 | 2025 |
| United States | HFIR | 100 | 1965 | 2035 |
| Australia | OPAL | 20 | 2006 | 2057 |
| Germany | FRM-II | 20 | 2004 | 2054 |
| Type | The Energy of Particles [MeV] | Application |
|---|---|---|
| Small medical cyclotron | <20 | Short-lived radioisotopes for PET |
| Medium-energy cyclotron | 20–35 | Production of SPECT and some PET radioisotopes |
| High-energy cyclotron | >35 | Production of radioisotopes for therapy |
| Facility/Location | Nuclear Reaction | Irradiation Parameters | Yield |
|---|---|---|---|
| Fukui Medical University | 64Ni(p, n)64Cu | 12 MeV, (50 ± 3) μA | 2-24 GBq in 2 h |
| The University of Sherbrooke PET Imaging Centre | 64Ni(p, n)64Cu | 15 MeV, 18 μA | 3.9 GBq in 4 h |
| IBA | 64Ni(p, n)64Cu | 10 MeV, 12 μA | 5123 MBq in 3 h |
| Paul Scherrer Institute | 64Ni(p, n)64Cu | 11 MeV, 40–50 μA | Max 8.2 GBq in 4–5 h |
| Turku PET Centre | 64Ni(p, n)64Cu | 15.7 MeV, < 100 μA | Max 9.4GBq after purification |
| Sumitomo HM-20 cyclotron | 64Ni(p, n)64Cu | 12.5 MeV, 20 μA | 7.4 GBq in 5–7 h |
| NIRS AVF-930 cyclotron | 64Ni(p, n)64Cu | 24 MeV HH+, 10 eμA | 5.2-13GBq in 1–3 h |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, Y.; Chen, D.; dos Santos Augusto, R.; Liang, J.; Qin, Z.; Liu, J.; Liu, Z. Production Review of Accelerator-Based Medical Isotopes. Molecules 2022, 27, 5294. https://doi.org/10.3390/molecules27165294
Wang Y, Chen D, dos Santos Augusto R, Liang J, Qin Z, Liu J, Liu Z. Production Review of Accelerator-Based Medical Isotopes. Molecules. 2022; 27(16):5294. https://doi.org/10.3390/molecules27165294
Chicago/Turabian StyleWang, Yiwei, Daiyuan Chen, Ricardo dos Santos Augusto, Jixin Liang, Zhi Qin, Juntao Liu, and Zhiyi Liu. 2022. "Production Review of Accelerator-Based Medical Isotopes" Molecules 27, no. 16: 5294. https://doi.org/10.3390/molecules27165294
APA StyleWang, Y., Chen, D., dos Santos Augusto, R., Liang, J., Qin, Z., Liu, J., & Liu, Z. (2022). Production Review of Accelerator-Based Medical Isotopes. Molecules, 27(16), 5294. https://doi.org/10.3390/molecules27165294






