Role of Dipeptidyl Peptidase 4 Inhibitors in Antidiabetic Treatment
Abstract
1. Introduction
2. DPP4 and DPP4 Inhibitions in Diabetes
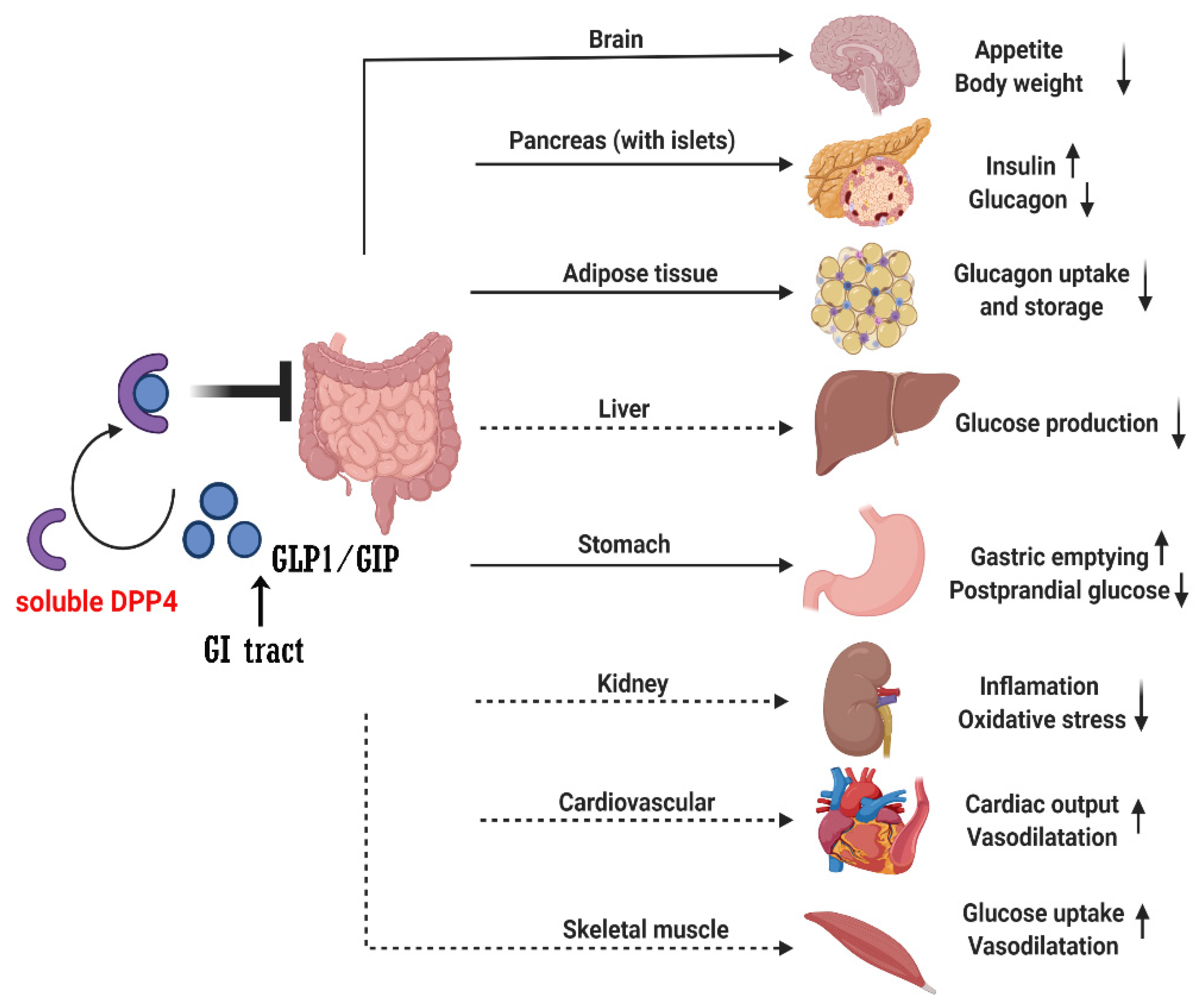
2.1. Mechanisms of Effect of DPP4i
2.2. DPP4 Inhibitors
2.3. Benefits of DPP4i
2.4. Anti-Inflammation Effects of DPP4i
2.5. Adverse Effects
3. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kos, K.; Baker, A.R.; Jernas, M.; Harte, A.L.; Clapham, J.C.; O’Hare, J.P.; Carlsson, L.; Kumar, S.; McTernan, P.G. DPP-IV inhibition enhances the antilipolytic action of NPY in human adipose tissue. Diabetes Obes. Metab. 2009, 11, 285–292. [Google Scholar] [CrossRef]
- Mentlein, R. Dipeptidyl-peptidase IV (CD26)—Role in the inactivation of regulatory peptides. Regul. Pept. 1999, 85, 9–24. [Google Scholar] [CrossRef]
- Wronkowitz, N.; Gorgens, S.W.; Romacho, T.; Villalobos, L.A.; Sanchez-Ferrer, C.F.; Peiro, C.; Sell, H.; Eckel, J. Soluble DPP4 induces inflammation and proliferation of human smooth muscle cells via protease-activated receptor 2. Biochim. Biophys. Acta 2014, 1842, 1613–1621. [Google Scholar] [CrossRef]
- Ghorpade, D.S.; Ozcan, L.; Zheng, Z.; Nicoloro, S.M.; Shen, Y.; Chen, E.; Bluher, M.; Czech, M.P.; Tabas, I. Hepatocyte-secreted DPP4 in obesity promotes adipose inflammation and insulin resistance. Nature 2018, 555, 673–677. [Google Scholar] [CrossRef]
- Holst, J.J.; Deacon, C.F. Inhibition of the activity of dipeptidyl-peptidase IV as a treatment for type 2 diabetes. Diabetes 1998, 47, 1663–1670. [Google Scholar] [CrossRef]
- Ahren, B. Dipeptidyl peptidase-4 inhibitors: Clinical data and clinical implications. Diabetes Care 2007, 30, 1344–1350. [Google Scholar] [CrossRef]
- Fan, L.; Zhou, W.; Zhang, L.; Jiang, D.; Zhao, Q.; Liu, L. Sitagliptin protects against hypoxia/reoxygenation (H/R)-induced cardiac microvascular endothelial cell injury. Am. J. Transl. Res. 2019, 11, 2099–2107. [Google Scholar]
- Kirino, Y.; Sato, Y.; Kamimoto, T.; Kawazoe, K.; Minakuchi, K.; Nakahori, Y. Interrelationship of dipeptidyl peptidase IV (DPP4) with the development of diabetes, dyslipidaemia and nephropathy: A streptozotocin-induced model using wild-type and DPP4-deficient rats. J. Endocrinol. 2009, 200, 53–61. [Google Scholar] [CrossRef]
- Kirino, Y.; Sato, Y.; Kamimoto, T.; Kawazoe, K.; Minakuchi, K. Altered dipeptidyl peptidase-4 activity during the progression of hyperinsulinemic obesity and islet atrophy in spontaneously late-stage type 2 diabetic rats. Am. J. Physiol. Endocrinol. Metab. 2011, 300, E372–E379. [Google Scholar] [CrossRef]
- Wang, X.; Xiang, J.; Huang, G.; Kang, L.; Yang, G.; Wu, H.; Jiang, K.; Liang, Z.; Yang, S. Inhibition of Podocytes DPP4 Activity Is a Potential Mechanism of Lobeliae Chinensis Herba in Treating Diabetic Kidney Disease. Front. Pharmacol. 2021, 12, 779652. [Google Scholar] [CrossRef]
- Zheng, T.P.; Liu, Y.H.; Yang, L.X.; Qin, S.H.; Liu, H.B. Increased plasma dipeptidyl peptidase-4 activities are associated with high prevalence of subclinical atherosclerosis in Chinese patients with newly diagnosed type 2 diabetes: A cross-sectional study. Atherosclerosis 2015, 242, 580–588. [Google Scholar] [CrossRef]
- Varin, E.M.; Mulvihill, E.E.; Beaudry, J.L.; Pujadas, G.; Fuchs, S.; Tanti, J.F.; Fazio, S.; Kaur, K.; Cao, X.; Baggio, L.L.; et al. Circulating Levels of Soluble Dipeptidyl Peptidase-4 Are Dissociated from Inflammation and Induced by Enzymatic DPP4 Inhibition. Cell Metab. 2019, 29, 320–334.e5. [Google Scholar] [CrossRef]
- Arnett, D.K.; Blumenthal, R.S.; Albert, M.A.; Buroker, A.B.; Goldberger, Z.D.; Hahn, E.J.; Himmelfarb, C.D.; Khera, A.; Lloyd-Jones, D.; McEvoy, J.W.; et al. 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J. Am. Coll. Cardiol. 2019, 74, 1376–1414. [Google Scholar] [CrossRef]
- Chen, L.; Magliano, D.J.; Zimmet, P.Z. The worldwide epidemiology of type 2 diabetes mellitus—Present and future perspectives. Nat. Rev. Endocrinol. 2011, 8, 228–236. [Google Scholar] [CrossRef]
- Candler, T.P.; Mahmoud, O.; Lynn, R.M.; Majbar, A.A.; Barrett, T.G.; Shield, J.P.H. Continuing rise of Type 2 diabetes incidence in children and young people in the UK. Diabet. Med. 2018, 35, 737–744. [Google Scholar] [CrossRef]
- Lascar, N.; Brown, J.; Pattison, H.; Barnett, A.H.; Bailey, C.J.; Bellary, S. Type 2 diabetes in adolescents and young adults. Lancet Diabetes Endocrinol. 2018, 6, 69–80. [Google Scholar] [CrossRef]
- Magliano, D.J.; Sacre, J.W.; Harding, J.L.; Gregg, E.W.; Zimmet, P.Z.; Shaw, J.E. Young-onset type 2 diabetes mellitus—Implications for morbidity and mortality. Nat. Rev. Endocrinol. 2020, 16, 321–331. [Google Scholar] [CrossRef]
- Goossens, G.H.; Blaak, E.E. Adipose tissue dysfunction and impaired metabolic health in human obesity: A matter of oxygen? Front. Endocrinol. 2015, 6, 55. [Google Scholar] [CrossRef]
- Muller, T.D.; Bluher, M.; Tschop, M.H.; DiMarchi, R.D. Anti-obesity drug discovery: Advances and challenges. Nat. Rev. Drug Discov. 2022, 21, 201–223. [Google Scholar] [CrossRef]
- Hauser, A.S.; Attwood, M.M.; Rask-Andersen, M.; Schioth, H.B.; Gloriam, D.E. Trends in GPCR drug discovery: New agents, targets and indications. Nat. Rev. Drug Discov. 2017, 16, 829–842. [Google Scholar] [CrossRef]
- Rask-Andersen, M.; Almen, M.S.; Schioth, H.B. Trends in the exploitation of novel drug targets. Nat. Rev. Drug Discov. 2011, 10, 579–590. [Google Scholar] [CrossRef] [PubMed]
- Kaur, P.; Mittal, A.; Nayak, S.K.; Vyas, M.; Mishra, V.; Khatik, G.L. Current Strategies and Drug Targets in the Management of Type 2 Diabetes Mellitus. Curr. Drug Targets 2018, 19, 1738–1766. [Google Scholar] [CrossRef] [PubMed]
- Deacon, C.F.; Hughes, T.E.; Holst, J.J. Dipeptidyl peptidase IV inhibition potentiates the insulinotropic effect of glucagon-like peptide 1 in the anesthetized pig. Diabetes 1998, 47, 764–769. [Google Scholar] [CrossRef]
- Xiang, X.; Lang, M.; Li, Y.; Zhao, X.; Sun, H.; Jiang, W.; Ni, L.; Song, Y. Purification, identification and molecular mechanism of dipeptidyl peptidase IV inhibitory peptides from discarded shrimp (Penaeus vannamei) head. J. Chromatogr. B Analyt. Technol. Biomed. Life Sci. 2021, 1186, 122990. [Google Scholar] [CrossRef] [PubMed]
- Mulvihill, E.E.; Drucker, D.J. Pharmacology, physiology, and mechanisms of action of dipeptidyl peptidase-4 inhibitors. Endocr. Rev. 2014, 35, 992–1019. [Google Scholar] [CrossRef] [PubMed]
- Rohrborn, D.; Wronkowitz, N.; Eckel, J. DPP4 in Diabetes. Front. Immunol. 2015, 6, 386. [Google Scholar] [CrossRef] [PubMed]
- Ahren, B. DPP-4 Inhibition and the Path to Clinical Proof. Front. Endocrinol. 2019, 10, 376. [Google Scholar] [CrossRef]
- De, S.; Banerjee, S.; Kumar, S.K.A.; Paira, P. Critical Role of Dipeptidyl Peptidase IV: A Therapeutic Target for Diabetes and Cancer. Mini-Rev. Med. Chem. 2019, 19, 88–97. [Google Scholar] [CrossRef]
- Shimizu, S.; Hosooka, T.; Matsuda, T.; Asahara, S.; Koyanagi-Kimura, M.; Kanno, A.; Bartolome, A.; Etoh, H.; Fuchita, M.; Teruyama, K.; et al. DPP4 inhibitor vildagliptin preserves beta-cell mass through amelioration of endoplasmic reticulum stress in C/EBPB transgenic mice. J. Mol. Endocrinol. 2012, 49, 125–135. [Google Scholar] [CrossRef]
- Jonik, S.; Marchel, M.; Grabowski, M.; Opolski, G.; Mazurek, T. Gastrointestinal Incretins-Glucose-Dependent Insulinotropic Polypeptide (GIP) and Glucagon-like Peptide-1 (GLP-1) beyond Pleiotropic Physiological Effects Are Involved in Pathophysiology of Atherosclerosis and Coronary Artery Disease-State of the Art. Biology 2022, 11, 288. [Google Scholar] [CrossRef]
- Bekiari, E.; Rizava, C.; Athanasiadou, E.; Papatheodorou, K.; Liakos, A.; Karagiannis, T.; Mainou, M.; Rika, M.; Boura, P.; Tsapas, A. Systematic review and meta-analysis of vildagliptin for treatment of type 2 diabetes. Endocrine 2016, 52, 458–480. [Google Scholar] [CrossRef] [PubMed]
- Scott, L.J. Sitagliptin: A Review in Type 2 Diabetes. Drugs 2017, 77, 209–224. [Google Scholar] [CrossRef] [PubMed]
- Aulinger, B.A.; Bedorf, A.; Kutscherauer, G.; de Heer, J.; Holst, J.J.; Goke, B.; Schirra, J. Defining the role of GLP-1 in the enteroinsulinar axis in type 2 diabetes using DPP-4 inhibition and GLP-1 receptor blockade. Diabetes 2014, 63, 1079–1092. [Google Scholar] [CrossRef] [PubMed]
- Nauck, M.A.; Kind, J.; Kothe, L.D.; Holst, J.J.; Deacon, C.F.; Broschag, M.; He, Y.L.; Kjems, L.; Foley, J. Quantification of the Contribution of GLP-1 to Mediating Insulinotropic Effects of DPP-4 Inhibition With Vildagliptin in Healthy Subjects and Patients With Type 2 Diabetes Using Exendin [9-39] as a GLP-1 Receptor Antagonist. Diabetes 2016, 65, 2440–2447. [Google Scholar] [CrossRef] [PubMed]
- Sharma, A.; Paliwal, G.; Upadhyay, N.; Tiwari, A. Retraction Note: Therapeutic stimulation of GLP-1 and GIP protein with DPP-4 inhibitors for type-2 diabetes treatment. J. Diabetes Metab. Disord. 2015, 15, 34. [Google Scholar] [CrossRef]
- Sharma, A.; Paliwal, G.; Upadhyay, N.; Tiwari, A. Therapeutic stimulation of GLP-1 and GIP protein with DPP-4 inhibitors for type-2 diabetes treatment. J. Diabetes Metab. Disord. 2015, 14, 15. [Google Scholar] [CrossRef]
- Vilsboll, T.; Krarup, T.; Madsbad, S.; Holst, J.J. Defective amplification of the late phase insulin response to glucose by GIP in obese Type II diabetic patients. Diabetologia 2002, 45, 1111–1119. [Google Scholar] [CrossRef]
- Mentis, N.; Vardarli, I.; Kothe, L.D.; Holst, J.J.; Deacon, C.F.; Theodorakis, M.; Meier, J.J.; Nauck, M.A. GIP does not potentiate the antidiabetic effects of GLP-1 in hyperglycemic patients with type 2 diabetes. Diabetes 2011, 60, 1270–1276. [Google Scholar] [CrossRef]
- Hojberg, P.V.; Vilsboll, T.; Rabol, R.; Knop, F.K.; Bache, M.; Krarup, T.; Holst, J.J.; Madsbad, S. Four weeks of near-normalisation of blood glucose improves the insulin response to glucagon-like peptide-1 and glucose-dependent insulinotropic polypeptide in patients with type 2 diabetes. Diabetologia 2009, 52, 199–207. [Google Scholar] [CrossRef]
- Aaboe, K.; Akram, S.; Deacon, C.F.; Holst, J.J.; Madsbad, S.; Krarup, T. Restoration of the insulinotropic effect of glucose-dependent insulinotropic polypeptide contributes to the antidiabetic effect of dipeptidyl peptidase-4 inhibitors. Diabetes Obes. Metab. 2015, 17, 74–81. [Google Scholar] [CrossRef]
- Nakamura, T.; Tanimoto, H.; Okamoto, M.; Takeuchi, M.; Tsubamoto, Y.; Noda, H. GIP Receptor Antagonist, SKL-14959 Indicated Alteration of the Lipids Metabolism to Catabolism by the Inhibition of Plasma LPL Activity, Resulting in the Suppression of Weight Gain on Diets-Induced Obesity Mice. Diabetes Metab. Syndr. Obes. 2021, 14, 1095–1105. [Google Scholar] [CrossRef] [PubMed]
- Gasbjerg, L.S.; Bari, E.J.; Stensen, S.; Hoe, B.; Lanng, A.R.; Mathiesen, D.S.; Christensen, M.B.; Hartmann, B.; Holst, J.J.; Rosenkilde, M.M.; et al. Dose-dependent efficacy of the glucose-dependent insulinotropic polypeptide (GIP) receptor antagonist GIP(3–30)NH2 on GIP actions in humans. Diabetes Obes. Metab. 2021, 23, 68–74. [Google Scholar] [CrossRef] [PubMed]
- Christensen, M.B. Glucose-dependent insulinotropic polypeptide: Effects on insulin and glucagon secretion in humans. Dan. Med. J. 2016, 63, B5230. [Google Scholar] [PubMed]
- Ahren, B.; Schweizer, A.; Dejager, S.; Dunning, B.E.; Nilsson, P.M.; Persson, M.; Foley, J.E. Vildagliptin enhances islet responsiveness to both hyper- and hypoglycemia in patients with type 2 diabetes. J. Clin. Endocrinol. Metab. 2009, 94, 1236–1243. [Google Scholar] [CrossRef]
- Farngren, J.; Persson, M.; Schweizer, A.; Foley, J.E.; Ahren, B. Glucagon dynamics during hypoglycaemia and food-re-challenge following treatment with vildagliptin in insulin-treated patients with type 2 diabetes. Diabetes Obes. Metab. 2014, 16, 812–818. [Google Scholar] [CrossRef]
- Mannucci, E.; Nreu, B.; Montereggi, C.; Ragghianti, B.; Gallo, M.; Giaccari, A.; Monami, M.; SID-AMD Joint Panel for Italian Guidelines on Treatment of Type 2 Diabetes. Cardiovascular events and all-cause mortality in patients with type 2 diabetes treated with dipeptidyl peptidase-4 inhibitors: An extensive meta-analysis of randomized controlled trials. Nutr. Metab. Cardiovasc. Dis. 2021, 31, 2745–2755. [Google Scholar] [CrossRef]
- Molina-Vega, M.; Munoz-Garach, A.; Fernandez-Garcia, J.C.; Tinahones, F.J. The safety of DPP-4 inhibitor and SGLT2 inhibitor combination therapies. Expert Opin. Drug Saf. 2018, 17, 815–824. [Google Scholar] [CrossRef]
- Biftu, T.; Feng, D.; Qian, X.; Liang, G.B.; Kieczykowski, G.; Eiermann, G.; He, H.; Leiting, B.; Lyons, K.; Petrov, A.; et al. (3R)-4-[(3R)-3-Amino-4-(2,4,5-trifluorophenyl)butanoyl]-3-(2,2,2-trifluoroethyl)-1,4-diazepan-2-one, a selective dipeptidyl peptidase IV inhibitor for the treatment of type 2 diabetes. Bioorg. Med. Chem. Lett. 2007, 17, 49–52. [Google Scholar] [CrossRef]
- Augeri, D.J.; Robl, J.A.; Betebenner, D.A.; Magnin, D.R.; Khanna, A.; Robertson, J.G.; Wang, A.; Simpkins, L.M.; Taunk, P.; Huang, Q.; et al. Discovery and preclinical profile of Saxagliptin (BMS-477118): A highly potent, long-acting, orally active dipeptidyl peptidase IV inhibitor for the treatment of type 2 diabetes. J. Med. Chem. 2005, 48, 5025–5037. [Google Scholar] [CrossRef]
- Choy, M.; Lam, S. Sitagliptin: A novel drug for the treatment of type 2 diabetes. Cardiol. Rev. 2007, 15, 264–271. [Google Scholar] [CrossRef]
- Thareja, S.; Aggarwal, S.; Malla, P.; Haksar, D.; Bhardwaj, T.R.; Kumar, M. Saxagliptin: A new drug for the treatment of type 2 diabetes. Mini-Rev. Med. Chem. 2010, 10, 759–765. [Google Scholar] [CrossRef] [PubMed]
- White, J.R. Alogliptin for the treatment of type 2 diabetes. Drugs Today 2011, 47, 99–107. [Google Scholar] [CrossRef] [PubMed]
- Aletti, R.; Cheng-Lai, A. Linagliptin: The newest dipeptidyl peptidase-4 inhibitor for type 2 diabetes mellitus. Cardiol. Rev. 2012, 20, 45–51. [Google Scholar] [CrossRef] [PubMed]
- Raj, V.S.; Mou, H.; Smits, S.L.; Dekkers, D.H.; Muller, M.A.; Dijkman, R.; Muth, D.; Demmers, J.A.; Zaki, A.; Fouchier, R.A.; et al. Dipeptidyl peptidase 4 is a functional receptor for the emerging human coronavirus-EMC. Nature 2013, 495, 251–254. [Google Scholar] [CrossRef] [PubMed]
- Bergman, A.; Ebel, D.; Liu, F.; Stone, J.; Wang, A.; Zeng, W.; Chen, L.; Dilzer, S.; Lasseter, K.; Herman, G.; et al. Absolute bioavailability of sitagliptin, an oral dipeptidyl peptidase-4 inhibitor, in healthy volunteers. Biopharm. Drug Dispos. 2007, 28, 315–322. [Google Scholar] [CrossRef]
- Thornberry, N.A.; Weber, A.E. Discovery of JANUVIA (Sitagliptin), a selective dipeptidyl peptidase IV inhibitor for the treatment of type 2 diabetes. Curr. Top. Med. Chem. 2007, 7, 557–568. [Google Scholar] [CrossRef]
- Villhauer, E.B.; Brinkman, J.A.; Naderi, G.B.; Burkey, B.F.; Dunning, B.E.; Prasad, K.; Mangold, B.L.; Russell, M.E.; Hughes, T.E. 1-[[(3-hydroxy-1-adamantyl)amino]acetyl]-2-cyano-(S)-pyrrolidine: A potent, selective, and orally bioavailable dipeptidyl peptidase IV inhibitor with antihyperglycemic properties. J. Med. Chem. 2003, 46, 2774–2789. [Google Scholar] [CrossRef]
- Deacon, C.F. Dipeptidyl peptidase 4 inhibitors in the treatment of type 2 diabetes mellitus. Nat. Rev. Endocrinol. 2020, 16, 642–653. [Google Scholar] [CrossRef]
- He, Y.L. Clinical pharmacokinetics and pharmacodynamics of vildagliptin. Clin. Pharmacokinet. 2012, 51, 147–162. [Google Scholar] [CrossRef]
- Agency, E.M. Vildagliptin: Summary of Product Characteristics. Available online: https://www.ema.europa.eu/en/documents/product-information/galvus-eparproduct-information_en.pdf (accessed on 1 August 2020).
- Boulton, D.W. Clinical Pharmacokinetics and Pharmacodynamics of Saxagliptin, a Dipeptidyl Peptidase-4 Inhibitor. Clin. Pharmacokinet. 2017, 56, 11–24. [Google Scholar] [CrossRef]
- Scheen, A.J. Pharmacokinetics of dipeptidylpeptidase-4 inhibitors. Diabetes Obes. Metab. 2010, 12, 648–658. [Google Scholar] [CrossRef] [PubMed]
- Boulton, D.W.; Li, L.; Frevert, E.U.; Tang, A.; Castaneda, L.; Vachharajani, N.N.; Kornhauser, D.M.; Patel, C.G. Influence of renal or hepatic impairment on the pharmacokinetics of saxagliptin. Clin. Pharmacokinet. 2011, 50, 253–265. [Google Scholar] [CrossRef] [PubMed]
- Saxagliptin: Summary of Product Characteristics. Available online: https://www.ema.europa.eu/en/documents/product-information/onglyza-eparproduct-information_en.pdf (accessed on 1 August 2020).
- Linagliptin: Summary of Product Characteristics. Available online: https://www.ema.europa.eu/en/documents/product-information/trajenta-eparproduct-information_en.pdf (accessed on 1 August 2020).
- Johansen, O.E.; Neubacher, D.; von Eynatten, M.; Patel, S.; Woerle, H.J. Cardiovascular safety with linagliptin in patients with type 2 diabetes mellitus: A pre-specified, prospective, and adjudicated meta-analysis of a phase 3 programme. Cardiovasc. Diabetol. 2012, 11, 3. [Google Scholar] [CrossRef] [PubMed]
- Groop, P.H.; Cooper, M.E.; Perkovic, V.; Emser, A.; Woerle, H.J.; von Eynatten, M. Linagliptin lowers albuminuria on top of recommended standard treatment in patients with type 2 diabetes and renal dysfunction. Diabetes Care 2013, 36, 3460–3468. [Google Scholar] [CrossRef] [PubMed]
- Deacon, C.F. Dipeptidyl peptidase-4 inhibitors in the treatment of type 2 diabetes: A comparative review. Diabetes Obes. Metab. 2011, 13, 7–18. [Google Scholar] [CrossRef]
- Graefe-Mody, U.; Retlich, S.; Friedrich, C. Clinical pharmacokinetics and pharmacodynamics of linagliptin. Clin. Pharmacokinet. 2012, 51, 411–427. [Google Scholar] [CrossRef]
- Snyder, B.; Polasek, T.M.; Doogue, M.P. Reply to: Graefe-Mody, U.; Friedrich, C.; Port, A.; Ring, S.; Retlich, T.; Heise, A.; Halabi, H.-J. Woerle Effect of renal impairment on the pharmacokinetics of the dipeptidyl peptidase-4 inhibitor linagliptin. Diabetes Obes. Metab. 2011, 13, 939–946, Diabetes Obes. Metab.2012, 14, 670; Author Reply: Diabetes Obes. Metab. 2012, 14, 671–672. [Google Scholar]
- Graefe-Mody, U.; Rose, P.; Retlich, S.; Ring, A.; Waldhauser, L.; Cinca, R.; Woerle, H.J. Pharmacokinetics of linagliptin in subjects with hepatic impairment. Br. J. Clin. Pharmacol. 2012, 74, 75–85. [Google Scholar] [CrossRef]
- Rosenstock, J.; Perkovic, V.; Johansen, O.E.; Cooper, M.E.; Kahn, S.E.; Marx, N.; Alexander, J.H.; Pencina, M.; Toto, R.D.; Wanner, C.; et al. Effect of Linagliptin vs Placebo on Major Cardiovascular Events in Adults With Type 2 Diabetes and High Cardiovascular and Renal Risk: The CARMELINA Randomized Clinical Trial. JAMA 2019, 321, 69–79. [Google Scholar] [CrossRef]
- Katsiki, N.; Ofori-Asenso, R.; Ferrannini, E.; Mazidi, M. Fixed-dose combination of empagliflozin and linagliptin for the treatment of patients with type 2 diabetes mellitus: A systematic review and meta-analysis. Diabetes Obes. Metab. 2020, 22, 1001–1005. [Google Scholar] [CrossRef]
- Alogliptin: Summary of Product Characteristics. Available online: https://www.ema.europa.eu/en/documents/product-information/vipidia-eparproduct-information_en.pdf (accessed on 1 August 2020).
- Alsemeh, A.E.; Abdullah, D.M. Protective effect of alogliptin against cyclophosphamide-induced lung toxicity in rats: Impact on PI3K/Akt/FoxO1 pathway and downstream inflammatory cascades. Cell Tissue Res. 2022, 388, 417–438. [Google Scholar] [CrossRef] [PubMed]
- Biessels, G.J.; Verhagen, C.; Janssen, J.; van den Berg, E.; Zinman, B.; Rosenstock, J.; George, J.T.; Passera, A.; Schnaidt, S.; Johansen, O.E.; et al. Effect of Linagliptin on Cognitive Performance in Patients With Type 2 Diabetes and Cardiorenal Comorbidities: The CARMELINA Randomized Trial. Diabetes Care 2019, 42, 1930–1938. [Google Scholar] [CrossRef] [PubMed]
- Chikata, Y.; Iwata, H.; Miyosawa, K.; Koike, T.; Yasuda, H.; Funamizu, T.; Doi, S.; Endo, H.; Wada, H.; Naito, R.; et al. Dipeptidyl peptidase-4 inhibitors reduced long-term cardiovascular risk in diabetic patients after percutaneous coronary intervention via insulin-like growth factor-1 axis. Sci. Rep. 2022, 12, 5129. [Google Scholar] [CrossRef] [PubMed]
- Carr, R.D.; Katzeff, H.L.; Alexander, C.M.; Berger, J.P.; Xu, S.S.; Thornberry, N. Reply to: Ahren, B.; Schweizer, A.; Dejager, S.; Villhauer, E.B.; Dunning, B.E.; Foley, J.E. Mechanisms of action of the dipeptidyl peptidase-4 inhibitor vildagliptin in humans. Diabetes Obes. Metab. 2011, 13, 775–783 and Ahren, B.; Schweizer, A.; Dejager, S.; Villhauer, E.B.; Dunning, B.E.; Foley, J.E. Clinical evidence and mechanistic basis for vildagliptin’s action when added to metformin. Diabetes Obes. Metab. 2011, 13, 193–203, Diabetes Obes. Metab.2012, 14, 383–384. [Google Scholar] [CrossRef]
- Nabeno, M.; Akahoshi, F.; Kishida, H.; Miyaguchi, I.; Tanaka, Y.; Ishii, S.; Kadowaki, T. A comparative study of the binding modes of recently launched dipeptidyl peptidase IV inhibitors in the active site. Biochem. Biophys. Res. Commun. 2013, 434, 191–196. [Google Scholar] [CrossRef] [PubMed]
- Tatosian, D.A.; Guo, Y.; Schaeffer, A.K.; Gaibu, N.; Popa, S.; Stoch, A.; Langdon, R.B.; Kauh, E.A. Dipeptidyl peptidase-4 inhibition in patients with type 2 diabetes treated with saxagliptin, sitagliptin, or vildagliptin. Diabetes Ther. 2013, 4, 431–442. [Google Scholar] [CrossRef] [PubMed]
- Baranov, O.; Kahle, M.; Deacon, C.F.; Holst, J.J.; Nauck, M.A. Feedback suppression of meal-induced glucagon-like peptide-1 (GLP-1) secretion mediated through elevations in intact GLP-1 caused by dipeptidyl peptidase-4 inhibition: A randomized, prospective comparison of sitagliptin and vildagliptin treatment. Diabetes Obes. Metab. 2016, 18, 1100–1109. [Google Scholar] [CrossRef]
- Alsalim, W.; Goransson, O.; Tura, A.; Pacini, G.; Mari, A.; Ahren, B. Persistent whole day meal effects of three dipeptidyl peptidase-4 inhibitors on glycaemia and hormonal responses in metformin-treated type 2 diabetes. Diabetes Obes. Metab. 2020, 22, 590–598. [Google Scholar] [CrossRef]
- Scheen, A.J.; Charpentier, G.; Ostgren, C.J.; Hellqvist, A.; Gause-Nilsson, I. Efficacy and safety of saxagliptin in combination with metformin compared with sitagliptin in combination with metformin in adult patients with type 2 diabetes mellitus. Diabetes Metab. Res. Rev. 2010, 26, 540–549. [Google Scholar] [CrossRef]
- Addy, C.; Tatosian, D.; Glasgow, X.S.; Gendrano, I.N., 3rd; Kauh, E.; Martucci, A.; Johnson-Levonas, A.O.; Selverian, D.; Matthews, C.Z.; Gutierrez, M.; et al. Pharmacokinetic and Pharmacodynamic Effects of Multiple-dose Administration of Omarigliptin, a Once-weekly Dipeptidyl Peptidase-4 Inhibitor, in Obese Participants With and Without Type 2 Diabetes Mellitus. Clin. Ther. 2016, 38, 516–530. [Google Scholar] [CrossRef]
- Kim, Y.G.; Hahn, S.; Oh, T.J.; Kwak, S.H.; Park, K.S.; Cho, Y.M. Differences in the glucose-lowering efficacy of dipeptidyl peptidase-4 inhibitors between Asians and non-Asians: A systematic review and meta-analysis. Diabetologia 2013, 56, 696–708. [Google Scholar] [CrossRef] [PubMed]
- Cai, X.; Han, X.; Luo, Y.; Ji, L. Efficacy of dipeptidyl-peptidase-4 inhibitors and impact on beta-cell function in Asian and Caucasian type 2 diabetes mellitus patients: A meta-analysis. J. Diabetes 2015, 7, 347–359. [Google Scholar] [CrossRef] [PubMed]
- Gao, W.; Wang, Q.; Yu, S. Efficacy, safety and impact on beta-cell function of dipeptidyl peptidase-4 inhibitors plus metformin combination therapy in patients with type 2 diabetes and the difference between Asians and Caucasians: A meta-analysis. J. Endocrinol. Investig. 2016, 39, 1061–1074. [Google Scholar] [CrossRef] [PubMed]
- Kozlovski, P.; Fonseca, M.; Mohan, V.; Lukashevich, V.; Odawara, M.; Paldanius, P.M.; Kothny, W. Effect of race and ethnicity on vildagliptin efficacy: A pooled analysis of phase II and III studies. Diabetes Obes. Metab. 2017, 19, 429–435. [Google Scholar] [CrossRef][Green Version]
- Seino, Y.; Fujita, T.; Hiroi, S.; Hirayama, M.; Kaku, K. Efficacy and safety of alogliptin in Japanese patients with type 2 diabetes mellitus: A randomized, double-blind, dose-ranging comparison with placebo, followed by a long-term extension study. Curr. Med. Res. Opin. 2011, 27, 1781–1792. [Google Scholar] [CrossRef]
- Seino, Y.; Miyata, Y.; Hiroi, S.; Hirayama, M.; Kaku, K. Efficacy and safety of alogliptin added to metformin in Japanese patients with type 2 diabetes: A randomized, double-blind, placebo-controlled trial with an open-label, long-term extension study. Diabetes Obes. Metab. 2012, 14, 927–936. [Google Scholar] [CrossRef]
- Bahne, E.; Sun, E.W.L.; Young, R.L.; Hansen, M.; Sonne, D.P.; Hansen, J.S.; Rohde, U.; Liou, A.P.; Jackson, M.L.; de Fontgalland, D.; et al. Metformin-induced glucagon-like peptide-1 secretion contributes to the actions of metformin in type 2 diabetes. JCI Insight 2018, 3, e93936. [Google Scholar] [CrossRef]
- Lee, K.A.; Jin, H.Y.; Kim, Y.J.; Kim, S.S.; Cho, E.H.; Park, T.S. Real-world comparison of mono and dual combination therapies of metformin, sulfonylurea, and dipeptidyl peptidase-4 inhibitors using a common data model: A retrospective observational study. Medicine 2022, 101, e28823. [Google Scholar] [CrossRef]
- Ko, E.J.; Shin, Y.J.; Cui, S.; Lim, S.W.; Chung, B.H.; Yang, C.W. Effect of dual inhibition of DPP4 and SGLT2 on tacrolimus-induced diabetes mellitus and nephrotoxicity in rat model. Am. J. Transpl. 2022. [Google Scholar] [CrossRef]
- Morita, A.; Mukai, E.; Hiratsuka, A.; Takatani, T.; Iwanaga, T.; Lee, E.Y.; Miki, T. Distinct effects of dipeptidyl peptidase-4 inhibitor and glucagon-like peptide-1 receptor agonist on islet morphology and function. Endocrine 2016, 51, 429–439. [Google Scholar] [CrossRef]
- Yang, W.; Xu, X.; Lei, T.; Ma, J.; Li, L.; Shen, J.; Ye, B.; Zhu, S.; Meinicke, T. Efficacy and safety of linagliptin as add-on therapy to insulin in Chinese patients with type 2 diabetes mellitus: A randomized, double-blind, placebo-controlled trial. Diabetes Obes. Metab. 2021, 23, 642–647. [Google Scholar] [CrossRef] [PubMed]
- Esposito, K.; Cozzolino, D.; Bellastella, G.; Maiorino, M.I.; Chiodini, P.; Ceriello, A.; Giugliano, D. Dipeptidyl peptidase-4 inhibitors and HbA1c target of <7% in type 2 diabetes: Meta-analysis of randomized controlled trials. Diabetes Obes. Metab. 2011, 13, 594–603. [Google Scholar] [CrossRef] [PubMed]
- Scheen, A.J. The safety of gliptins: Updated data in 2018. Expert Opin. Drug Saf. 2018, 17, 387–405. [Google Scholar] [CrossRef] [PubMed]
- Wang, T.; McNeill, A.M.; Chen, Y.; O’Neill, E.A.; Engel, S.S. Characteristics of Elderly Patients Initiating Sitagliptin or Non-DPP-4-Inhibitor Oral Antihyperglycemic Agents: Analysis of a Cross-Sectional US Claims Database. Diabetes Ther. 2018, 9, 309–315. [Google Scholar] [CrossRef] [PubMed]
- Leiter, L.A.; Teoh, H.; Braunwald, E.; Mosenzon, O.; Cahn, A.; Kumar, K.M.; Smahelova, A.; Hirshberg, B.; Stahre, C.; Frederich, R.; et al. Efficacy and safety of saxagliptin in older participants in the SAVOR-TIMI 53 trial. Diabetes Care 2015, 38, 1145–1153. [Google Scholar] [CrossRef]
- Bethel, M.A.; Engel, S.S.; Green, J.B.; Huang, Z.; Josse, R.G.; Kaufman, K.D.; Standl, E.; Suryawanshi, S.; Van de Werf, F.; McGuire, D.K.; et al. Assessing the Safety of Sitagliptin in Older Participants in the Trial Evaluating Cardiovascular Outcomes with Sitagliptin (TECOS). Diabetes Care 2017, 40, 494–501. [Google Scholar] [CrossRef]
- Walker, S.R.; Komenda, P.; Khojah, S.; Al-Tuwaijri, W.; MacDonald, K.; Hiebert, B.; Tangri, N.; Nadurak, S.W.D.; Ferguson, T.W.; Rigatto, C.; et al. Dipeptidyl Peptidase-4 Inhibitors in Chronic Kidney Disease: A Systematic Review of Randomized Clinical Trials. Nephron 2017, 136, 85–94. [Google Scholar] [CrossRef]
- Trakarnvanich, T.; Satirapoj, B.; Suraamornkul, S.; Chirananthavat, T.; Sanpatchayapong, A.; Claimon, T. Effect of Dipeptidyl Peptidase-4 (DPP-4) Inhibition on Biomarkers of Kidney Injury and Vascular Calcification in Diabetic Kidney Disease: A Randomized Controlled Trial. J. Diabetes Res. 2021, 2021, 7382620. [Google Scholar] [CrossRef]
- Sitagliptin: Summary of Product Characteristics. Available online: https://www.ema.europa.eu/en/documents/product-information/januvia-eparproduct-information_en.pdf (accessed on 1 August 2020).
- He, Y.L.; Wang, Y.; Bullock, J.M.; Deacon, C.F.; Holst, J.J.; Dunning, B.E.; Ligueros-Saylan, M.; Foley, J.E. Pharmacodynamics of vildagliptin in patients with type 2 diabetes during OGTT. J. Clin. Pharmacol. 2007, 47, 633–641. [Google Scholar] [CrossRef]
- Christopher, R.; Covington, P.; Davenport, M.; Fleck, P.; Mekki, Q.A.; Wann, E.R.; Karim, A. Pharmacokinetics, pharmacodynamics, and tolerability of single increasing doses of the dipeptidyl peptidase-4 inhibitor alogliptin in healthy male subjects. Clin. Ther. 2008, 30, 513–527. [Google Scholar] [CrossRef]
- Klemann, C.; Wagner, L.; Stephan, M.; von Horsten, S. Cut to the chase: A review of CD26/dipeptidyl peptidase-4’s (DPP4) entanglement in the immune system. Clin. Exp. Immunol. 2016, 185, 1–21. [Google Scholar] [CrossRef] [PubMed]
- Zhong, J.; Rao, X.; Deiuliis, J.; Braunstein, Z.; Narula, V.; Hazey, J.; Mikami, D.; Needleman, B.; Satoskar, A.R.; Rajagopalan, S. A potential role for dendritic cell/macrophage-expressing DPP4 in obesity-induced visceral inflammation. Diabetes 2013, 62, 149–157. [Google Scholar] [CrossRef] [PubMed]
- Zhou, S.T.; Cui, W.; Kong, L.; Yang, X. Efficacy of Sitagliptin on Nonalcoholic Fatty Liver Disease in High-fat-diet-fed Diabetic Mice. Curr. Med. Sci. 2022. [Google Scholar] [CrossRef] [PubMed]
- Allam, M.M.; Ibrahim, R.M.; El Gazzar, W.B.; Said, M.A. Dipeptedyl peptidase-4 (DPP-4) inhibitor downregulates HMGB1/TLR4/NF-kappaB signaling pathway in a diabetic rat model of non-alcoholic fatty liver disease. Arch. Physiol. Biochem. 2021. [Google Scholar] [CrossRef] [PubMed]
- Ren, J.; Wang, X.; Yee, C.; Gorrell, M.D.; McLennan, S.V.; Twigg, S.M. Sitagliptin Is More Effective Than Gliclazide in Preventing Pro-Fibrotic and Pro-Inflammatory Changes in a Rodent Model of Diet-Induced Non-Alcoholic Fatty Liver Disease. Molecules 2022, 27, 727. [Google Scholar] [CrossRef]
- Cao, Q.; Xu, D.; Chen, Y.; Long, Y.; Dai, F.; Gui, L.; Lu, Y. Sitagliptin Reduces Endothelial Dysfunction and Apoptosis Induced by High-Fat Diet and Palmitate in Thoracic Aortas and Endothelial Cells via ROS-ER Stress-CHOP Pathway. Front. Pharmacol. 2021, 12, 670389. [Google Scholar] [CrossRef]
- Trocha, M.; Fleszar, M.G.; Fortuna, P.; Lewandowski, L.; Gostomska-Pampuch, K.; Sozanski, T.; Merwid-Lad, A.; Krzystek-Korpacka, M. Sitagliptin Modulates Oxidative, Nitrative and Halogenative Stress and Inflammatory Response in Rat Model of Hepatic Ischemia-Reperfusion. Antioxidants 2021, 10, 1168. [Google Scholar] [CrossRef]
- Xu, L.; Shao, F. Sitagliptin protects renal glomerular endothelial cells against high glucose-induced dysfunction and injury. Bioengineered 2022, 13, 655–666. [Google Scholar] [CrossRef]
- Li, Y.; Lv, X.; Jiang, M.; Jin, Z. Sitagliptin ameliorates hypoxia-induced damages in endometrial stromal cells: An implication in endometriosis. Bioengineered 2022, 13, 800–809. [Google Scholar] [CrossRef]
- Kong, L.; Deng, J.; Zhou, X.; Cai, B.; Zhang, B.; Chen, X.; Chen, Z.; Wang, W. Sitagliptin activates the p62-Keap1-Nrf2 signalling pathway to alleviate oxidative stress and excessive autophagy in severe acute pancreatitis-related acute lung injury. Cell. Death Dis. 2021, 12, 928. [Google Scholar] [CrossRef]
- Moulton, C.D.; Rokakis, A.S.; Pickup, J.C.; Young, A.H.; Stahl, D.; Ismail, K. SITAgliptin for Depressive Symptoms in Type 2 Diabetes: A Feasibility Randomized Controlled Trial. Psychosom. Med. 2021, 83, 913–923. [Google Scholar] [CrossRef] [PubMed]
- Han, C.K.; Lee, W.F.; Hsu, C.J.; Huang, Y.L.; Lin, C.Y.; Tsai, C.H.; Huang, C.C.; Fong, Y.C.; Wu, M.H.; Liu, J.F.; et al. DPP4 reduces proinflammatory cytokine production in human rheumatoid arthritis synovial fibroblasts. J. Cell. Physiol. 2021, 236, 8060–8069. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.C.; Sung, P.H.; Yang, Y.H.; Chiang, J.Y.; Yip, H.K.; Yang, C.C. Dipeptidyl peptidase 4 promotes peritoneal fibrosis and its inhibitions prevent failure of peritoneal dialysis. Commun. Biol. 2021, 4, 144. [Google Scholar] [CrossRef] [PubMed]
- Teragawa, H.; Morimoto, T.; Fujii, Y.; Ueda, T.; Sakuma, M.; Shimabukuro, M.; Arasaki, O.; Node, K.; Nomiyama, T.; Ueda, S. Effect of Anagliptin versus Sitagliptin on Inflammatory Markers: Sub-Analysis from the REASON Trial. Diabetes Metab. Syndr. Obes. 2020, 13, 4993–5001. [Google Scholar] [CrossRef]
- Wang, M.; Dong, Y.; Wu, J.; Li, H.; Zhang, J.; Lu, L.; Zhang, Y.; Zhou, Z.; Fan, S.; Li, D.; et al. Sitagliptin Mitigates Total Body Irradiation-Induced Hematopoietic Injury in Mice. Oxid. Med. Cell. Longev. 2020, 2020, 8308616. [Google Scholar] [CrossRef]
- Li, R.; Zeng, X.; Yang, M.; Feng, J.; Xu, X.; Bao, L.; Ye, T.; Wang, X.; Xue, B.; Huang, Y. Antidiabetic DPP-4 Inhibitors Reprogram Tumor Microenvironment That Facilitates Murine Breast Cancer Metastasis Through Interaction With Cancer Cells via a ROS-NF-small ka, CyrillicB-NLRP3 Axis. Front. Oncol. 2021, 11, 728047. [Google Scholar] [CrossRef]
- Prakash, S.; Rai, U.; Kosuru, R.; Tiwari, V.; Singh, S. Amelioration of diet-induced metabolic syndrome and fatty liver with sitagliptin via regulation of adipose tissue inflammation and hepatic Adiponectin/AMPK levels in mice. Biochimie 2020, 168, 198–209. [Google Scholar] [CrossRef]
- Yang, M.; Chen, X.; Chen, X.; Liu, H.; Zhang, Z. Protective effect of vildagliptin on myocardial injury in septic rats by regulating TLR-4/NF-kappaB pathway. Minerva Med. 2021, 112, 522–524. [Google Scholar] [CrossRef]
- Fouad, M.R.; Salama, R.M.; Zaki, H.F.; El-Sahar, A.E. Vildagliptin attenuates acetic acid-induced colitis in rats via targeting PI3K/Akt/NFkappaB, Nrf2 and CREB signaling pathways and the expression of lncRNA IFNG-AS1 and miR-146a. Int. Immunopharmacol. 2021, 92, 107354. [Google Scholar] [CrossRef]
- Khalil, R.; Shata, A.; Abd El-Kader, E.M.; Sharaf, H.; Abdo, W.S.; Amin, N.A.; Saber, S. Vildagliptin, a DPP-4 inhibitor, attenuates carbon tetrachloride-induced liver fibrosis by targeting ERK1/2, p38alpha, and NF-kappaB signaling. Toxicol. Appl. Pharmacol. 2020, 407, 115246. [Google Scholar] [CrossRef]
- Liu, Y.; Qi, Y. Vildagliptin, a CD26/DPP4 inhibitor, ameliorates bleomycin-induced pulmonary fibrosis via regulating the extracellular matrix. Int. Immunopharmacol. 2020, 87, 106774. [Google Scholar] [CrossRef] [PubMed]
- Pengrattanachot, N.; Cherngwelling, R.; Jaikumkao, K.; Pongchaidecha, A.; Thongnak, L.; Swe, M.T.; Chatsudthipong, V.; Lungkaphin, A. Atorvastatin attenuates obese-induced kidney injury and impaired renal organic anion transporter 3 function through inhibition of oxidative stress and inflammation. Biochim. Biophys. Acta Mol. Basis Dis. 2020, 1866, 165741. [Google Scholar] [CrossRef]
- Nazeem, M.; Wahdan, S.A.; El-Naga, R.N.; Gad, A.M. Saxagliptin ameliorated the depressive-like behavior induced by chronic unpredictable mild stress in rats: Impact on incretins and AKT/PI3K pathway. Eur. J. Pharmacol. 2021, 912, 174602. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Qi, X.; Zhang, G.; Zhang, Y.; Tian, J. Saxagliptin protects against hypoxia-induced damage in H9c2 cells. Chem. Biol. Interact. 2020, 315, 108864. [Google Scholar] [CrossRef] [PubMed]
- Nistala, R.; Meuth, A.I.; Smith, C.; An, J.; Habibi, J.; Hayden, M.R.; Johnson, M.; Aroor, A.; Whaley-Connell, A.; Sowers, J.R.; et al. DPP4 inhibition mitigates ANG II-mediated kidney immune activation and injury in male mice. Am. J. Physiol. Renal. Physiol. 2021, 320, F505–F517. [Google Scholar] [CrossRef]
- Chen, Z.; Yu, J.; Fu, M.; Dong, R.; Yang, Y.; Luo, J.; Hu, S.; Li, W.; Xu, X.; Tu, L. Dipeptidyl peptidase-4 inhibition improves endothelial senescence by activating AMPK/SIRT1/Nrf2 signaling pathway. Biochem. Pharmacol. 2020, 177, 113951. [Google Scholar] [CrossRef]
- El-Sahar, A.E.; Shiha, N.A.; El Sayed, N.S.; Ahmed, L.A. Alogliptin Attenuates Lipopolysaccharide-Induced Neuroinflammation in Mice Through Modulation of TLR4/MYD88/NF-kappaB and miRNA-155/SOCS-1 Signaling Pathways. Int. J. Neuropsychopharmacol. 2021, 24, 158–169. [Google Scholar] [CrossRef]
- Salama, R.M.; Nasr, M.M.; Abdelhakeem, J.I.; Roshdy, O.K.; ElGamal, M.A. Alogliptin attenuates cyclophosphamide-induced nephrotoxicity: A novel therapeutic approach through modulating MAP3K/JNK/SMAD3 signaling cascade. Drug Chem. Toxicol. 2022, 45, 1254–1263. [Google Scholar] [CrossRef]
- Guo, Q.; Zhang, S.; Huang, J.; Liu, K. Alogliptin inhibits IL-1beta-induced inflammatory response in fibroblast-like synoviocytes. Int. Immunopharmacol. 2020, 83, 106372. [Google Scholar] [CrossRef]
- Wang, S.C.; Wang, X.Y.; Liu, C.T.; Chou, R.H.; Chen, Z.B.; Huang, P.H.; Lin, S.J. The Dipeptidyl Peptidase-4 Inhibitor Linagliptin Ameliorates Endothelial Inflammation and Microvascular Thrombosis in a Sepsis Mouse Model. Int. J. Mol. Sci. 2022, 23, 3065. [Google Scholar] [CrossRef]
- El-Ghannam, M.S.; Saad, M.A.; Nassar, N.N.; El-Yamany, M.F.; El-Bahy, A.A.Z. Linagliptin ameliorates acetic acid-induced colitis via modulating AMPK/SIRT1/PGC-1alpha and JAK2/STAT3 signaling pathway in rats. Toxicol. Appl. Pharmacol. 2022, 438, 115906. [Google Scholar] [CrossRef]
- Saito, H.; Nakamura, Y.; Inagaki, M.; Yamadera, S.; Misawa, H.; Sato, N.; Oguchi, T.; Inagaki, T.; Tsuji, Y.; Tsuji, M.; et al. Linagliptin Inhibits Interleukin-6 Production Through Toll-Like Receptor 4 Complex and Lipopolysaccharide-Binding Protein Independent Pathway in vitro Model. J. Inflamm. Res. 2021, 14, 5681–5686. [Google Scholar] [CrossRef] [PubMed]
- Wu, T.J.; Hsieh, Y.J.; Lu, C.W.; Lee, C.J.; Hsu, B.G. Linagliptin Protects against Endotoxin-Induced Acute Kidney Injury in Rats by Decreasing Inflammatory Cytokines and Reactive Oxygen Species. Int. J. Mol. Sci. 2021, 22, 1190. [Google Scholar] [CrossRef] [PubMed]
- Reijrink, M.; De Boer, S.A.; Van Roon, A.M.; Slart, R.; Fernandez, B.O.; Feelisch, M.; Heerspink, H.J.L.; Van Goor, H.; Hillebrands, J.L.; Mulder, D.J. Plasma Nitrate Levels Are Related to Metabolic Syndrome and Are Not Altered by Treatment with DPP-4 Inhibitor Linagliptin: A Randomised, Placebo-Controlled Trial in Patients with Early Type 2 Diabetes Mellitus. Antioxidants 2021, 10, 1548. [Google Scholar] [CrossRef] [PubMed]
- Arab, H.H.; Eid, A.H.; Mahmoud, A.M.; Senousy, M.A. Linagliptin mitigates experimental inflammatory bowel disease in rats by targeting inflammatory and redox signaling. Life Sci. 2021, 273, 119295. [Google Scholar] [CrossRef]
- Mayer, A.L.; Scheitacker, I.; Ebert, N.; Klein, T.; Amann, K.; Daniel, C. The dipeptidyl peptidase 4 inhibitor linagliptin ameliorates renal injury and accelerated resolution in a rat model of crescentic nephritis. Br. J. Pharmacol. 2021, 178, 878–895. [Google Scholar] [CrossRef]
- Okuyama, T.; Shirakawa, J.; Tajima, K.; Ino, Y.; Vethe, H.; Togashi, Y.; Kyohara, M.; Inoue, R.; Miyashita, D.; Li, J.; et al. Linagliptin Ameliorates Hepatic Steatosis via Non-Canonical Mechanisms in Mice Treated with a Dual Inhibitor of Insulin Receptor and IGF-1 Receptor. Int. J. Mol. Sci. 2020, 21, 7815. [Google Scholar] [CrossRef]
- Tang, P.M.; Zhang, Y.Y.; Hung, J.S.; Chung, J.Y.; Huang, X.R.; To, K.F.; Lan, H.Y. DPP4/CD32b/NF-kappaB Circuit: A Novel Druggable Target for Inhibiting CRP-Driven Diabetic Nephropathy. Mol. Ther. 2021, 29, 365–375. [Google Scholar] [CrossRef]
- Wang, H.; Li, Y.; Zhang, X.; Xu, Z.; Zhou, J.; Shang, W. DPP-4 Inhibitor Linagliptin Ameliorates Oxidized LDL-Induced THP-1 Macrophage Foam Cell Formation and Inflammation. Drug Des. Devel. Ther. 2020, 14, 3929–3940. [Google Scholar] [CrossRef]
- Aboulmagd, Y.M.; El-Bahy, A.A.Z.; Menze, E.T.; Azab, S.S.; El-Demerdash, E. Role of linagliptin in preventing the pathological progression of hepatic fibrosis in high fat diet and streptozotocin-induced diabetic obese rats. Eur. J. Pharmacol. 2020, 881, 173224. [Google Scholar] [CrossRef]
- Virta, J.; Hellberg, S.; Liljenback, H.; Stahle, M.; Silvola, J.M.U.; Huusko, J.; Soderstrom, M.; Knuuti, J.; Nuutila, P.; Yla-Herttuala, S.; et al. Effects of dipeptidyl peptidase 4 inhibition on inflammation in atherosclerosis: A (18)F-fluorodeoxyglucose study of a mouse model of atherosclerosis and type 2 diabetes. Atherosclerosis 2020, 305, 64–72. [Google Scholar] [CrossRef] [PubMed]
- Zhang, G.; Kim, S.; Gu, X.; Yu, S.P.; Wei, L. DPP-4 Inhibitor Linagliptin is Neuroprotective in Hyperglycemic Mice with Stroke via the AKT/mTOR Pathway and Anti-apoptotic Effects. Neurosci. Bull. 2020, 36, 407–418. [Google Scholar] [CrossRef] [PubMed]
- Jedlowski, P.M.; Jedlowski, M.F.; Fazel, M.T. DPP-4 Inhibitors and Increased Reporting Odds of Bullous Pemphigoid: A Pharmacovigilance Study of the FDA Adverse Event Reporting System (FAERS) from 2006 to 2020. Am. J. Clin. Dermatol. 2021, 22, 891–900. [Google Scholar] [CrossRef] [PubMed]
- Huang, J.; Jia, Y.; Sun, S.; Meng, L. Adverse event profiles of dipeptidyl peptidase-4 inhibitors: Data mining of the public version of the FDA adverse event reporting system. BMC Pharmacol. Toxicol. 2020, 21, 68. [Google Scholar] [CrossRef]
- Bajaj, H.S.; Ye, C.; Jain, E.; Venn, K.; Stein, E.; Aronson, R. Glycemic Improvement with a Fixed-dose combination of DPP-4 inhibitor + metformin in patients with Type 2 diabetes (GIFT study). Diabetes Obes. Metab. 2018, 20, 195–199. [Google Scholar] [CrossRef]
- Kim, H.J.; Jeong, I.K.; Hur, K.Y.; Kim, S.K.; Noh, J.H.; Chun, S.W.; Kang, E.S.; Rhee, E.J.; Choi, S.H. Comparison of Efficacy of Glimepiride, Alogliptin, and Alogliptin-Pioglitazone as the Initial Periods of Therapy in Patients with Poorly Controlled Type 2 Diabetes Mellitus: An Open-Label, Multicenter, Randomized, Controlled Study. Diabetes Metab. J. 2022. [Google Scholar] [CrossRef]
- Korbut, A.I.; Taskaeva, I.S.; Bgatova, N.P.; Muraleva, N.A.; Orlov, N.B.; Dashkin, M.V.; Khotskina, A.S.; Zavyalov, E.L.; Konenkov, V.I.; Klein, T.; et al. SGLT2 Inhibitor Empagliflozin and DPP4 Inhibitor Linagliptin Reactivate Glomerular Autophagy in db/db Mice, a Model of Type 2 Diabetes. Int. J. Mol. Sci. 2020, 21, 2987. [Google Scholar] [CrossRef]
| DPP4i | Chemistry | Metabolism | Half-Life | Elimination Method |
|---|---|---|---|---|
| Sitagliptin | β-amino acid based | Minimal | 12.5 h | Predominantly (>80%) renal |
| Vildagliptin | Cyanopyrrolidine | Hydrolysis (cytochromeindependent) to form an inactive metabolite | ~2 h | Metabolism (parent) and renal (metabolite) |
| Saxagliptin | Cyanopyrrolidine | Hydrolysis (cytochrome P450 3A4 or P450 3A5) to form an activemetabolite | 2.5 h (parent), 3 h (metabolite) | Metabolism (parent) and renal (metabolite) |
| Alogliptin | Modified pyrimidinedione | Minimal | 20 h | Predominantly (>70%) renal |
| Linagliptin | Xanthine based | Minimal | ~12 h (effective), >100 h (terminal) | Predominantly biliary (<6% renal) |
| DPP4i | Trial (Year) | Median Follow-Up, Years | Mean/Median Age, Years | Female (Total) | BMI, kg/m2 * | HbA1c, mmol/mol (%) * | Baseline Metformin, % | Baseline eGFR, mL/min/ [1.73 m]2 * | Prior ASCVD, % | Prior CHF, % |
|---|---|---|---|---|---|---|---|---|---|---|
| Sitagliptin | TECOS (2015) | 3.0 | 65 | 4212 | 30.2 | 55 (7.2) | 81 | 75 | 100 | 18 |
| (14,523) | ||||||||||
| Saxagliptin | SAVOR-TIMI (2013) | 2.1 | 65 | 5590 | 31.2 | 64 (8.0) | 69 | 73 | 78 | 13 |
| (16,492) | ||||||||||
| Alogliptin | EXAMINE (2013) | 1.5 | 61 | 1722 | 28.7 | 64 (8.0) | NA | 71 | 100 | 28 |
| (5380) | ||||||||||
| Linagliptin | CARMEL (2019) | 2.2 | 66 | 2582 | 31.4 | 64 (8.0) | 54 | 55 | 57 | 27 |
| (6979) |
| DPP4i | Dose (mg/Day) | HbA1c Reduction |
|---|---|---|
| Sitagliptin | 100 | 0.5–1.0 |
| Saxagliptin | 5 | 0.5–1.0 |
| Alogliptin | 25 | 0.6 (mean value) |
| Linagliptin | 5 | 0.5–0.7 |
| DPP4i | Experimental Model | Mechanism of the Effects | Ref. |
|---|---|---|---|
| Sitagliptin | HFD-fed diabetic mice | Inhibited fatty liver inflammation; downregulates HMGB1/TLR4/NF-κB signaling pathway | [108,109] |
| Diet-induced NAFLD | Inhibited pro-fibrotic and pro-inflammatory changes | [110] | |
| HFD-fed rats | Ameliorated apoptosis via alleviating ROS and ER stress | [111] | |
| Hepatic ischemia-reperfusion rat | Modulates oxidative, nitrative and halogenative stress and inflammatory response | [112] | |
| High glucose-induced human renal glomerular endothelial cells | Reversed the high glucose-induced oxidative stress, inflammation, and increased permebility via regulating KLF6 | [113] | |
| Hypoxia-induced damages in endometrial stromal cells | Suppressed the expressions of the proinflammatory cytokines including TNF-α, IL-6 and MCP-1; mitigated the activation of the p-38 MAPK and NF-κB pathways | [114] | |
| Severe acute pancreatitis companied with acute lung injury | Reduced oxidative stress and excessive autophagy through the p62–Keap1–Nrf2 signaling pathway | [115] | |
| Depressive symptoms in T2DM | No effect | [116] | |
| Human rheumatoid arthritis synovial fibroblasts | Increased proinflammatory cytokine production, enhanced the risk of RA development (sitagliptin and vildagliptin) | [117] | |
| Chlorhexidine gluconate induced peritoneal dialysis rats | Reversed the EMT process, angiogenesis, oxidative stress, and inflammation | [118] | |
| Low-density lipoprotein cholesterol in diabetes (REASON) Trial | Did not affect the levels of inflammatory markers | [119] | |
| Total body irradiation induced hematopoietic cells injury | Inhibited NOX4-mediated oxidative stress and alleviated inflammation | [120] | |
| Breast cancer | Reprograms tumor microenvironment via a ROS–NRF2–HO-1–NF-kB–NLRP3 axis | [121] | |
| Obese mice | Inhibited adipose tissue inflammation, metabolic syndrome, and fatty liver via regulation of adiponectin and AMPK levels | [122] | |
| Vildaliptin | Rheumatoid arthritis | Increased proinflammatory cytokine IL-1β, IL-6, and IL-13 production | [117] |
| Septic rats with myocardial injury | Inhibited the activation of NF-κB by promoting Nrf2 to alleviate the inflammatory response | [123] | |
| Acetic acid-induced colitis in rats | Inhibited the expression of lncRNA IFNG-AS1 and miR-146a, PI3K/Akt/NFκB pathway, and activated CREB and nuclear factor erythroid 2-related factor 2 (Nrf2) signaling pathways | [124] | |
| Carbon tetrachloride-induced liver fibrosis | Attenuates liver fibrosis by targeting ERK1/2, p38α, and NF-κB signaling. | [125] | |
| Bleomycin-induced pulmonary fibrosis | Attenuated inflammation and fibrosis in bleomycin-induced pulmonary tissue via inhibiting the activity of CD26/DPP4 | [126] | |
| HFD-fed rats with impaired renal function | Attenuated insulin resistance and renal lipid accumulation-induced lipotoxicity | [127] | |
| Saxagliptin | Chronic unpredictable mild stress induced depression in rats | Increased the incretin hormones, GLP-1 and GIP, and the activation PI3K/AKT signaling pathway | [128] |
| Breast cancer | Reprogramed tumor microenvironment via a ROS–NRF2–HO-1–NF-kB–NLRP3 axis | [121] | |
| H9c2 cardiomyocyte cell line | Ameliorated hypoxia-induced inflammation via upregulation of Nrf2 and HO-1 | [129] | |
| Angiotensin II kidney injury model | Improved Angiotensin II suppressed anti-inflammatory regulatory T cell and T helper 2 lymphocyte activity | [130] | |
| Young and old SD rats | Improved endothelial senescence by activating AMPK/SIRT1/Nrf2 signaling pathway | [131] | |
| Alogliptin | Cyclophosphamide-induced lung toxicity in rats | Ameliorated lung toxicity by mitigating the oxidative, inflammatory, and fibrotic impacts | [75] |
| Lipopolysaccharide-induced neuroinflammation in mice | Attenuated neuroinflammation through modulation of TLR4/MYD88/NF-κB and miRNA-155/SOCS-1 signaling pathways | [132] | |
| Cyclophosphamide-induced nephrotoxicity Wistar rats | Attenuated nephrotoxicity through modulating MAP3K/JNK/SMAD3 signaling cascade | [133] | |
| Fibroblast-like synoviocytes | Inhibited IL-1β-induced inflammatory response | [134] | |
| Linagliptin | Sepsis mouse | Suppressed expressions of IL-1β and intercellular adhesion molecule 1 via a NF-κB-dependent pathway | [135] |
| Acetic acid-induced colitis rats | Activated AMPK-SIRT1-PGC-1α pathway and suppressed JAK2/STAT3 signaling pathway | [136] | |
| LPS induced U937 cells | Inhibited inflammation around the TLR-4-mediated pathway. | [137] | |
| Acute kidney injury in rats | Decreased inflammatory cytokines and ROS | [138] | |
| Early T2DM | Not altered plasma nitrate levels | [139] | |
| Experimental autoimmune myocarditis mice | Suppressed oxidative stress in EAM hearts | [81] | |
| Trinitrobenzene sulfonic acid-evoked colitis in rats | Curbed inflammation through the suppression of colonic IL-6, TNF-α, and upregulation of IL-10 | [140] | |
| Anti-glomerular basement membrane antibody induced in nephritis rats | Improved resolution of glomerular injury and healing in non-diabetic renal disease | [141] | |
| OSI-906-induced hepatic steatosis | Improved hepatic steatosis via an insulin-signaling-independent pathway | [142] | |
| Diabetic injured kidney | Inhibited the CRP/CD32b/NF-kB-driven renal inflammation and fibrosis | [143] | |
| Oxidized LDL-induced THP-1 macrophage foam cell formation | Decreased the expression of CD36 and LOX-1 and increased the expression of the cholesterol transporter ABCG1 | [144] | |
| HFD and streptozotocin (STZ) induced diabetic rats: liver fibrosis with T2DM | Improved insulin sensitivity and lipid profile and reduced inflammatory mediators, and collagen depositions | [145] | |
| Atherosclerosis and T2D mice | Improved glucose tolerance and reduced hepatic inflammation but had no effect on plaque burden or atherosclerotic inflammation | [146] | |
| Hyperglycemic mice with stroke | Exerted a neuroprotective effect through activation of the Akt/mTOR pathway along with anti-apoptotic and anti-inflammatory mechanisms | [147] | |
| Mouse bone marrow macrophages | Increased M2 macrophage polarization by inhibiting DPP-4 expression and activity | [130] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yin, R.; Xu, Y.; Wang, X.; Yang, L.; Zhao, D. Role of Dipeptidyl Peptidase 4 Inhibitors in Antidiabetic Treatment. Molecules 2022, 27, 3055. https://doi.org/10.3390/molecules27103055
Yin R, Xu Y, Wang X, Yang L, Zhao D. Role of Dipeptidyl Peptidase 4 Inhibitors in Antidiabetic Treatment. Molecules. 2022; 27(10):3055. https://doi.org/10.3390/molecules27103055
Chicago/Turabian StyleYin, Ruili, Yongsong Xu, Xin Wang, Longyan Yang, and Dong Zhao. 2022. "Role of Dipeptidyl Peptidase 4 Inhibitors in Antidiabetic Treatment" Molecules 27, no. 10: 3055. https://doi.org/10.3390/molecules27103055
APA StyleYin, R., Xu, Y., Wang, X., Yang, L., & Zhao, D. (2022). Role of Dipeptidyl Peptidase 4 Inhibitors in Antidiabetic Treatment. Molecules, 27(10), 3055. https://doi.org/10.3390/molecules27103055






