Solid Dosage Forms of Biopharmaceuticals in Drug Delivery Systems Using Sustainable Strategies
Abstract
1. Introduction
2. Supercritical CO2-Based Drying Techniques to Produce Solid Dosage Forms of Biopharmaceuticals in Drug Delivery Systems
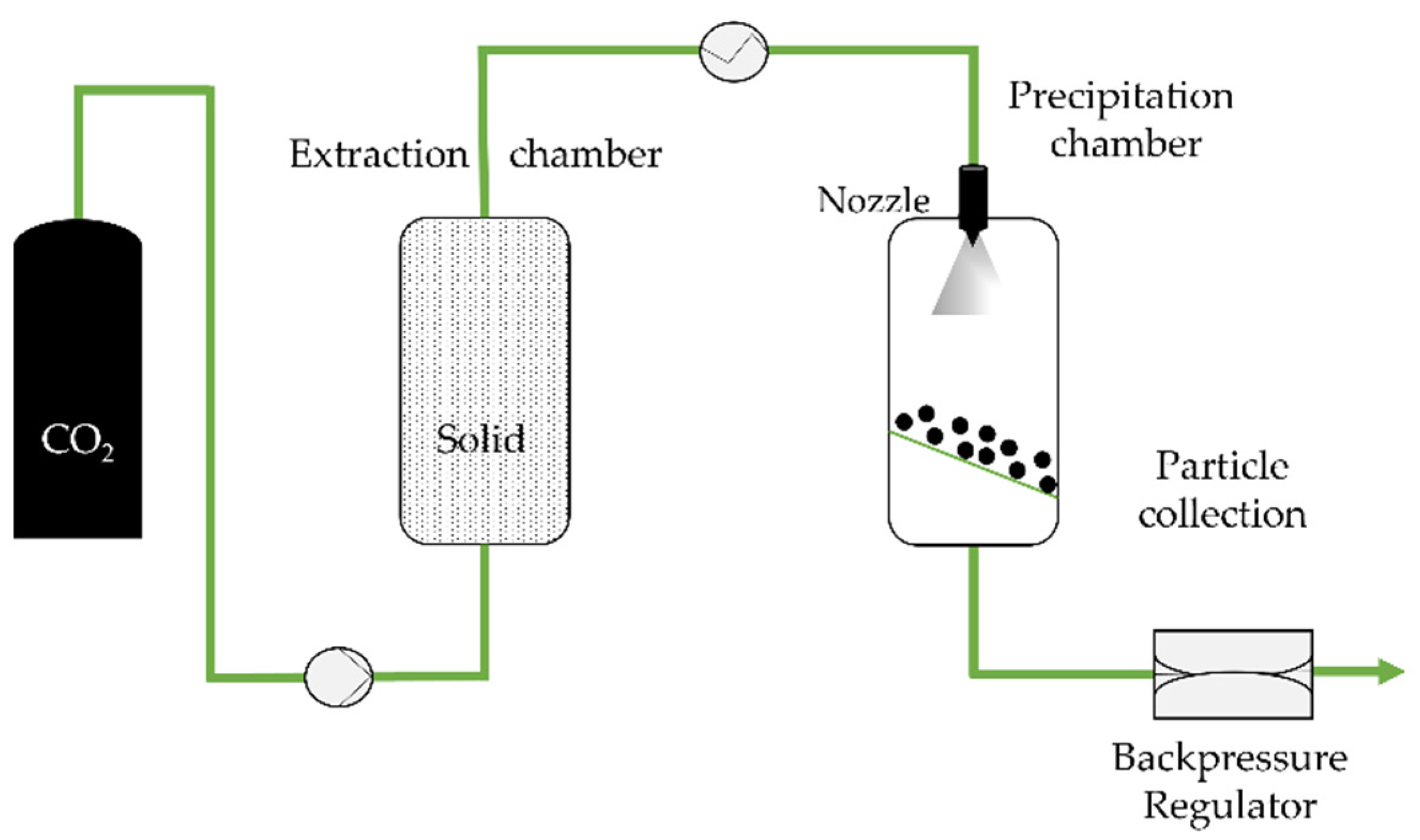
2.1. Rapid Expansion of Supercritical Solvent (RESS)
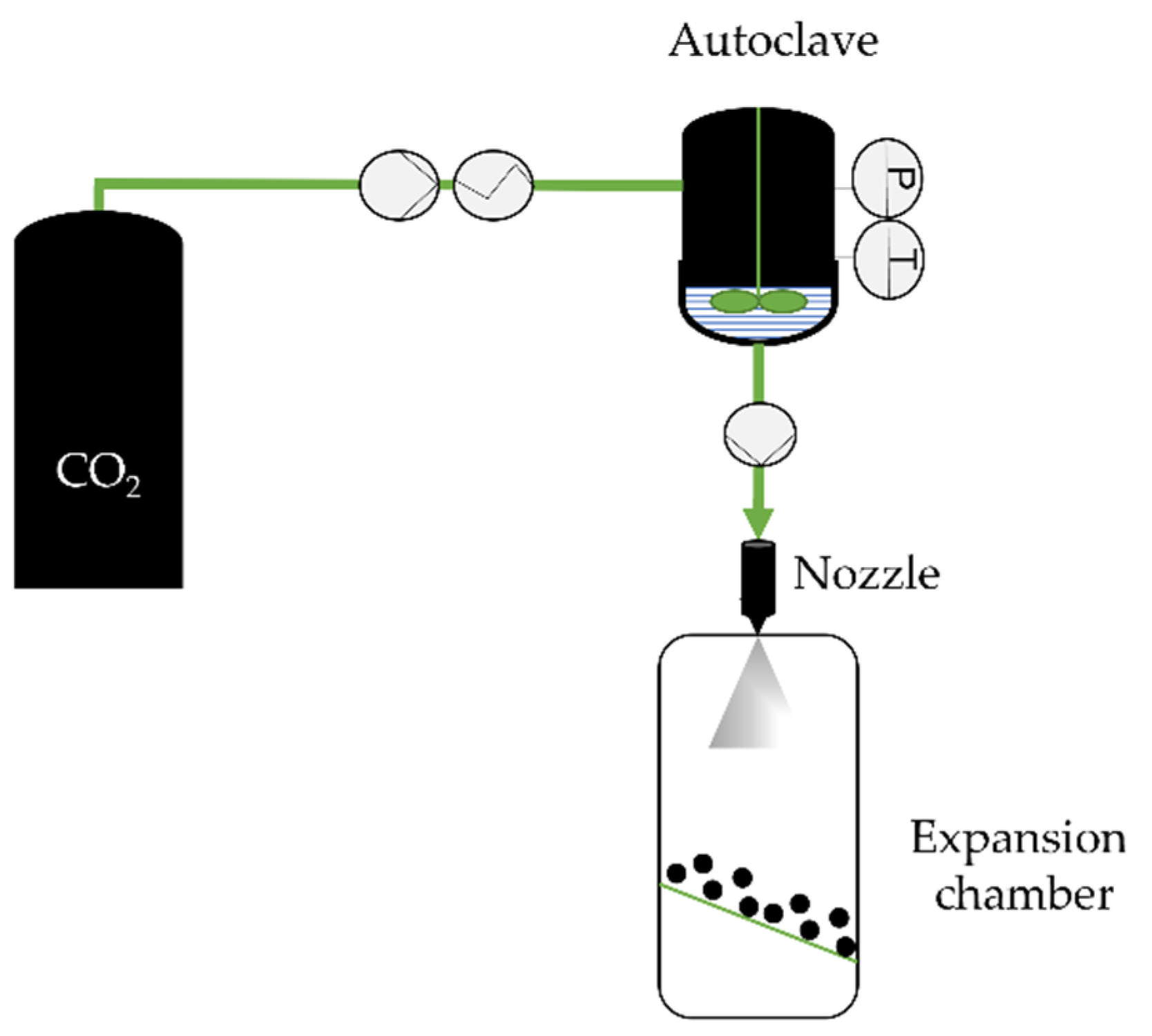
2.2. Particles from Gas-Saturated Solutions (PGSS)
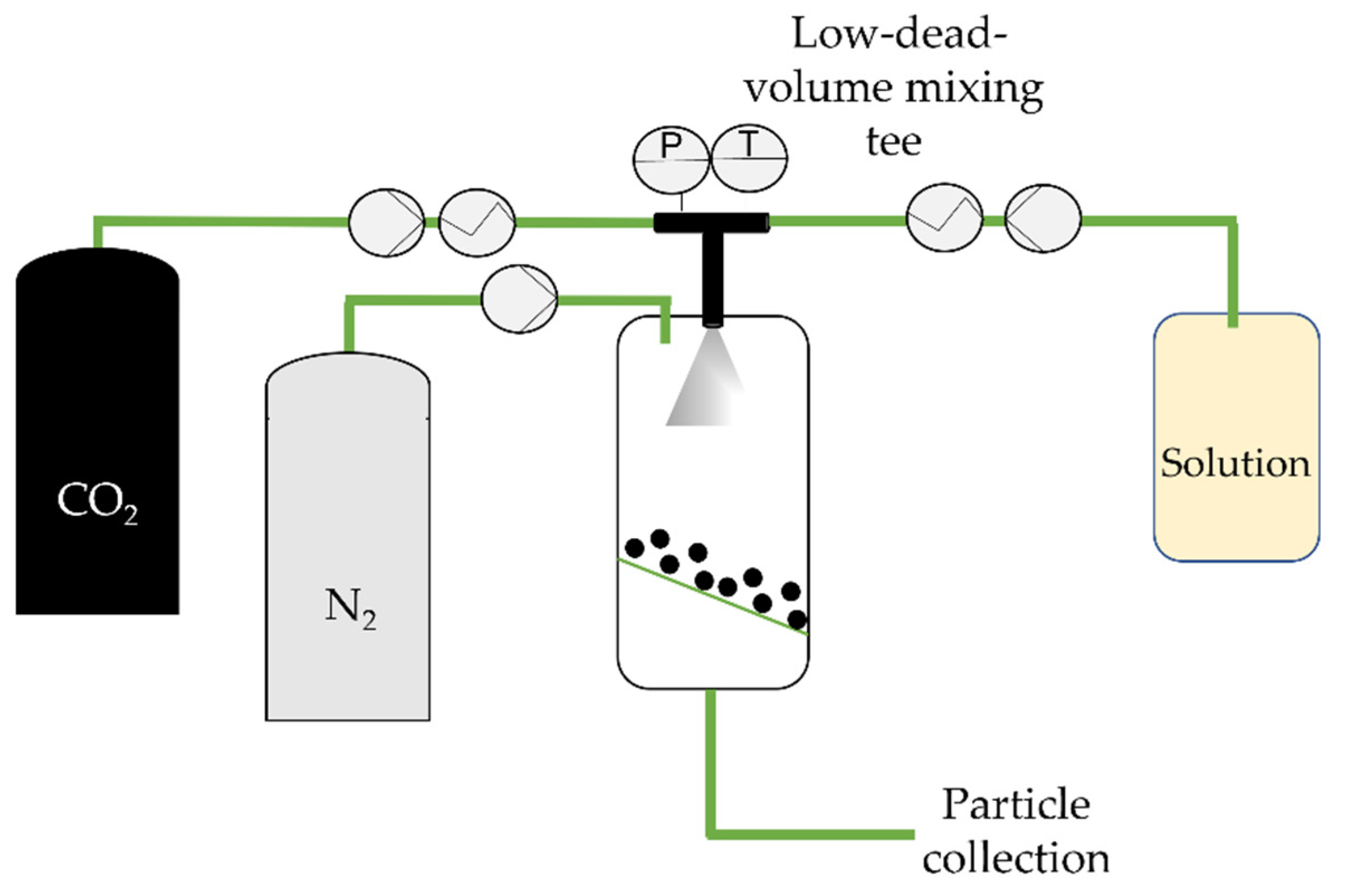
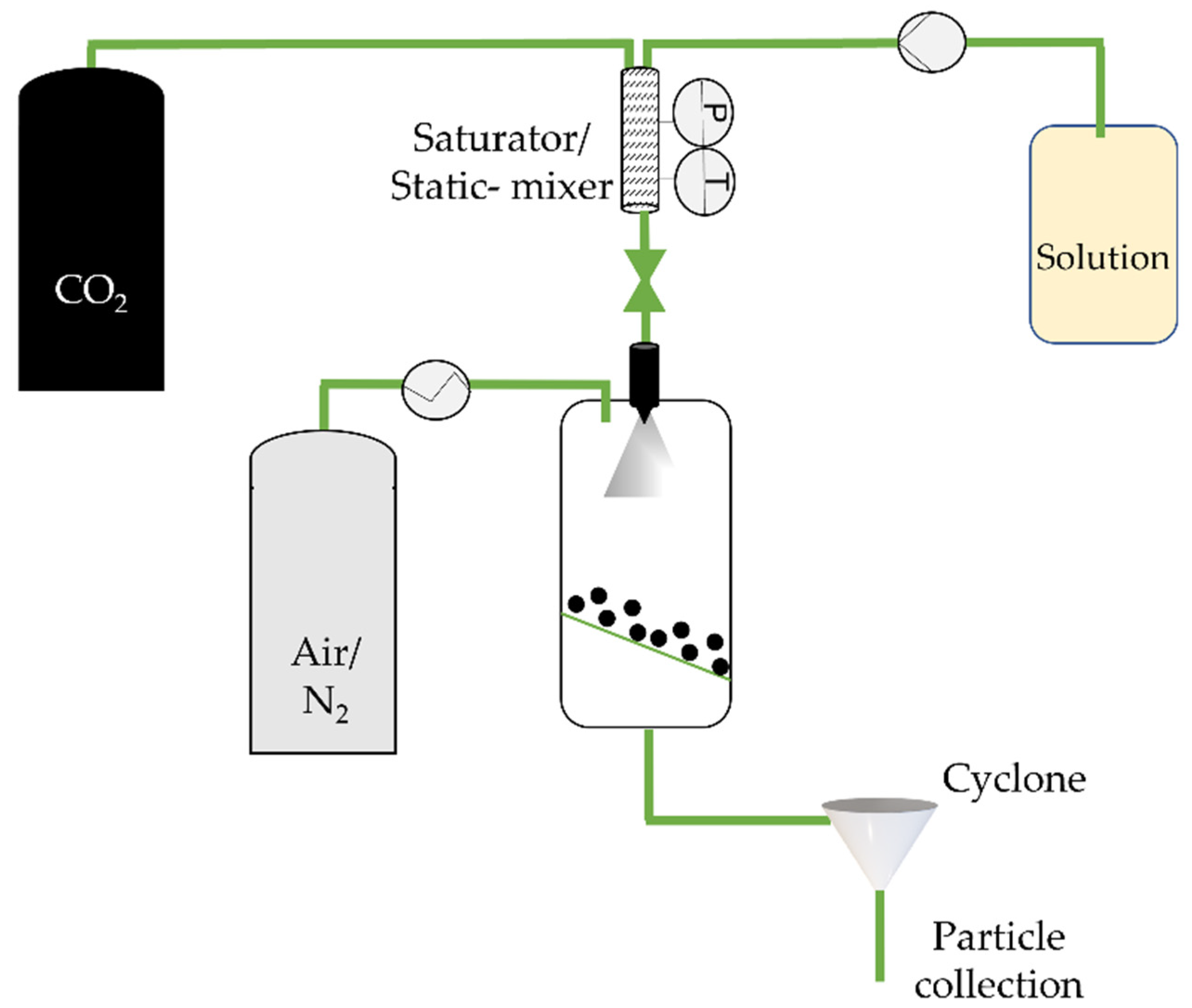
2.3. Carbon Dioxide-Assisted Nebulization with a Bubble Dryer (CAN-BD)
2.4. Supercritical Assisted Atomization (SAA)/Supercritical CO2-Assisted Spray-Drying (SASD)
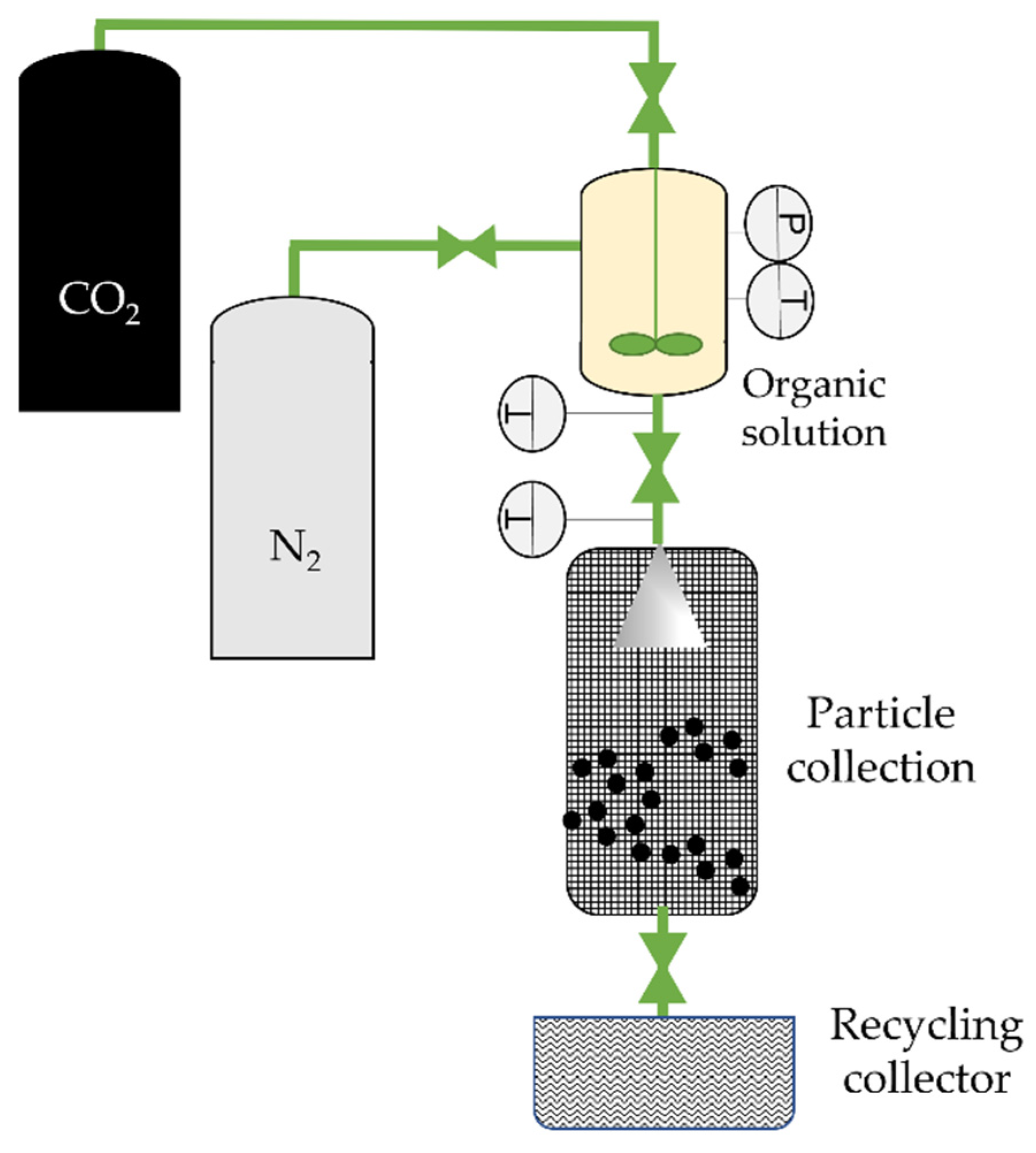
2.5. Depressurization of an Expanded Liquid Organic Solution (DELOS)
2.6. Supercritical CO2 as Anti-Solvent
3. Biopharmaceutical Stability during Freeze-Drying, Spray-Drying, and Supercritical CO2-Assisted Atomization/Spray-Drying
4. Conclusions and Future Perspectives
Author Contributions
Funding
Conflicts of Interest
References
- He, W.; Xing, X.; Wang, X.; Wu, D.; Wu, W.; Guo, J.; Mitragotri, S. Nanocarrier-Mediated Cytosolic Delivery of Biopharmaceuticals. Adv. Funct. Mater. 2020, 30, 1910566. [Google Scholar] [CrossRef]
- Kesik-Brodacka, M. Progress in Biopharmaceutical Development. Biotechnol. Appl. Biochem. 2018, 65, 306–322. [Google Scholar] [CrossRef]
- Earhart, A.P.; Holliday, Z.M.; Hofmann, H.V.; Schrum, A.G. Consideration of Dornase Alfa for the Treatment of Severe COVID-19 Acute Respiratory Distress Syndrome. New Microbes New Infect. 2020, 35, 100689. [Google Scholar] [CrossRef]
- Mitragotri, S.; Burke, P.A.; Langer, R. Overcoming the Challenges in Administering Biopharmaceuticals: Formulation and Delivery Strategies. Nat. Rev. Drug Discov. 2014, 13, 655–672. [Google Scholar] [CrossRef] [PubMed]
- Feng, Y.; Wang, H.; Zhang, S.; Zhao, Y.; Gao, J.; Zheng, Y.; Zhao, P.; Zhang, Z.; Zaworotko, M.J.; Cheng, P.; et al. Antibodies@MOFs: An In Vitro Protective Coating for Preparation and Storage of Biopharmaceuticals. Adv. Mater. 2019, 31, 1805148. [Google Scholar] [CrossRef]
- Hu, B.; Zhong, L.; Weng, Y.; Peng, L.; Huang, Y.; Zhao, Y.; Liang, X.J. Therapeutic SiRNA: State of the Art. Signal Transduct. Target. Ther. 2020, 5, 101. [Google Scholar] [CrossRef]
- Xing, Y.; Xu, Z.; Liu, T.; Shi, L.; Kohane, D.; Guo, S. Synthesis of Poly(Acyclic Orthoester)s: Acid-Sensitive Biomaterials for Enhancing Immune Responses of Protein Vaccine. Angew. Chem. Int. Ed. 2020, 59, 7235–7239. [Google Scholar] [CrossRef]
- Edmans, J.G.; Murdoch, C.; Santocildes-Romero, M.E.; Hatton, P.V.; Colley, H.E.; Spain, S.G. Incorporation of Lysozyme into a Mucoadhesive Electrospun Patch for Rapid Protein Delivery to the Oral Mucosa. Mater. Sci. Eng. C 2020, 112, 110917. [Google Scholar] [CrossRef] [PubMed]
- Shigemitsu, H.; Kubota, R.; Nakamura, K.; Matsuzaki, T.; Minami, S.; Aoyama, T.; Urayama, K.; Hamachi, I. Protein-Responsive Protein Release of Supramolecular/Polymer Hydrogel Composite Integrating Enzyme Activation Systems. Nat. Commun. 2020, 11, 3859. [Google Scholar] [CrossRef] [PubMed]
- Costa, C.; Liu, Z.; Simões, S.I.; Correia, A.; Rahikkala, A.; Seitsonen, J.; Ruokolainen, J.; Aguiar-Ricardo, A.; Santos, H.A.; Corvo, M.L. One-Step Microfluidics Production of Enzyme-Loaded Liposomes for the Treatment of Inflammatory Diseases. Colloids Surf. B Biointerfaces 2021, 199, 111556. [Google Scholar] [CrossRef] [PubMed]
- Costa, C.; Liu, Z.; Martins, J.P.; Correia, A.; Figueiredo, P.; Rahikkala, A.; Li, W.; Seitsonen, J.; Ruokolainen, J.; Hirvonen, S.-P.; et al. All-in-One Microfluidic Assembly of Insulin-Loaded pH-Responsive Nano-in-Microparticles for Oral Insulin Delivery. Biomater. Sci. 2020, 3270–3277. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Shen, H.; Xu, J.; Liu, L.; Tan, J.; Li, M.; Xu, N.; Luo, S.; Wang, J.; Yang, F.; et al. Liver-Targeted SiRNA Lipid Nanoparticles Treat Hepatic Cirrhosis by Dual Antifibrotic and Anti-Inflammatory Activities. ACS Nano 2020, 14, 6305–6322. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Guo, Z.; Kordanovski, M.; Kaltbeitzel, J.; Zhang, H.; Cao, Z.; Gu, Z.; Wich, P.R.; Lord, M.; Liang, K. Metal-Organic Frameworks as Protective Matrices for Peptide Therapeutics. J. Colloid Interface Sci. 2020, 576, 356–363. [Google Scholar] [CrossRef]
- Khaitov, M.; Nikonova, A.; Shilovskiy, I.; Kozhikhova, K.; Kofiadi, I.; Vishnyakova, L.; Nikolskii, A.; Gattinger, P.; Kovchina, V.; Barvinskaia, E.; et al. Silencing of SARS-CoV-2 with Modified SiRNA-Peptide Dendrimer Formulation. Allergy 2021, 76, 2840–2854. [Google Scholar] [CrossRef]
- Bohr, A.; Tsapis, N.; Foged, C.; Andreana, I.; Yang, M.; Fattal, E. Treatment of acute lung inflammation by pulmonary delivery of anti-TNF-α siRNA with PAMAM dendrimers in a murine model. Eur. J. Pharm. Biopharm. 2020, 156, 114–120. [Google Scholar] [CrossRef]
- Pinto, J.T.; Faulhammer, E.; Dieplinger, J.; Dekner, M.; Makert, C.; Nieder, M.; Paudel, A. Progress in Spray-Drying of Protein Pharmaceuticals: Literature Analysis of Trends in Formulation and Process Attributes. Dry Technol. 2021, 39, 1415–1446. [Google Scholar] [CrossRef]
- Krammer, F. SARS-CoV-2 Vaccines in Development. Nature 2020, 586, 516–527. [Google Scholar] [CrossRef] [PubMed]
- Langford, A.; Bhatnagar, B.; Walters, R.; Tchessalov, S.; Ohtake, S. Drying Technologies for Biopharmaceutical Applications: Recent Developments and Future Direction. Dry Technol. 2018, 36, 677–684. [Google Scholar] [CrossRef]
- Aguiar-Ricardo, A.; Bonifácio, V.D.B.; Casimiro, T.; Correia, V.G. Supercritical Carbon Dioxide Design Strategies: From Drug Carriers to Soft Killers. Phil. Trans. R. Soc. A 2015, 373, 20150009. [Google Scholar] [CrossRef]
- Silva, A.S.; Tavares, M.T.; Aguiar-Ricardo, A. Sustainable Strategies for Nano-in-Micro Particle Engineering for Pulmonary Delivery. J. Nanopart. Res. 2014, 16. [Google Scholar] [CrossRef]
- Wang, J.L.; Hanafy, M.S.; Xu, H.; Leal, J.; Zhai, Y.; Ghosh, D.; Williams, R.O.; Smyth, H.D.C.; Cui, Z. Aerosolizable SiRNA-Encapsulated Solid Lipid Nanoparticles Prepared by Thin-Film Freeze-Drying for Potential Pulmonary Delivery. Int. J. Pharm. 2021, 596, 120215. [Google Scholar] [CrossRef]
- Corvo, M.L.; Boerman, O.C.; Oyen, W.J.G.; Van Bloois, L.; Cruz, M.E.M.; Crommelin, D.J.A.; Storm, G. Intravenous Administration of Superoxide Dismutase Entrapped in Long Circulating Liposomes II. In Vivo Fate in a Rat Model of Adjuvant Arthritis. Biochim. Biophys. Acta-Biomembr. 1999, 1419, 325–334. [Google Scholar] [CrossRef][Green Version]
- Fissore, D.; McCoy, T. Editorial: Freeze-Drying and Process Analytical Technology for Pharmaceuticals. Front. Chem. 2018, 6, 622. [Google Scholar] [CrossRef]
- Emami, F.; Vatanara, A.; Park, E.J.; Na, D.H. Drying Technologies for the Stability and Bioavailability of Biopharmaceuticals. Pharmaceutics 2018, 10, 131. [Google Scholar] [CrossRef]
- Bellary, S.; Barnett, A.H. Inhaled Insulin (Exubera®): Combining Efficacy and Convenience. Diabetes Vasc. Dis. Res. 2006, 3, 179–185. [Google Scholar] [CrossRef] [PubMed]
- Bailey, C.J.; Barnett, A.H. Why Is Exubera Being Withdrawn? BMJ 2007, 335, 1156. [Google Scholar] [CrossRef]
- Ibrahim, B.M.; Jun, S.W.; Lee, M.Y.; Kang, S.H.; Yeo, Y. Development of Inhalable Dry Powder Formulation of Basic Fibroblast Growth Factor. Int. J. Pharm. 2010, 385, 66–72. [Google Scholar] [CrossRef]
- Hannay, J.B.; Hogarth, J. On the Solubility of Solids in Gases. Philos. Trans. R. Soc. 1879, 29, 324–326. [Google Scholar] [CrossRef]
- Jovanovic, N.; Bouchard, A.; Hofland, G.W.; Witkamp, G.-J.; Crommelin, D.J.A.; Jiskoot, W. Stabilization of Proteins in Dry Powder Formulations Using Supercritical Fluid Technology. Ph.D. Thesis, Utrecht University, Utrecht, The Netherlands, 2007. [Google Scholar]
- Tavares, M.; Cabral, R.P.; Costa, C.; Martins, P.; Fernandes, A.R.; Casimiro, T.; Aguiar-Ricardo, A. Development of PLGA Dry Powder Microparticles by Supercritical CO2-Assisted Spray-Drying for Potential Vaccine Delivery to the Lungs. J. Supercrit. Fluids 2017, 128, 235–243. [Google Scholar] [CrossRef]
- Aguiar-Ricardo, A. Building Dry Powder Formulations Using Supercritical CO2 Spray Drying. Curr. Opin. Green Sustain. Chem. 2017, 5, 12–16. [Google Scholar] [CrossRef]
- Della Porta, G.; De Vittori, C.; Reverchon, E. Supercritical Assisted Atomization: A Novel Technology for Microparticles Preparation of an Asthma-Controlling Drug. AAPS PharmSciTech 2005, 6, E421–E428. [Google Scholar] [CrossRef]
- Nunes, A.V.M.; Duarte, C.M.M. Dense CO2 as a Solute, Co-Solute or Co-Solvent in Particle Formation Processes: A Review. Materials 2011, 4, 2017–2041. [Google Scholar] [CrossRef]
- Anastas, P.; Eghbali, N. Green Chemistry: Principles and Practice. Chem. Soc. Rev. 2010, 39, 301–312. [Google Scholar] [CrossRef]
- Matson, D.W.; Petersen, R.C.; Smith, R.D. Production of Powders and Films by the Rapid Expansion of Supercritical Solutions. J. Mater. Sci. 1987, 22, 1919–1928. [Google Scholar] [CrossRef]
- Matson, D.W.; Fulton, J.L.; Petersen, R.C.; Smith, R.D. Rapid Expansion of Supercritical Fluid Solutions: Solute Formation of Powders, Thin Films, and Fibers. Ind. Eng. Chem. Res. 1987, 26, 2298–2306. [Google Scholar] [CrossRef]
- Petersen, R.C.; Matson, D.W.; Smith, R.D. Rapid Precipitation of Low Vapor Pressure Solids from Supercritical Fluid Solutions: The Formation of Thin Films and Powders. J. Am. Chem. Soc. 1986, 108, 2100–2102. [Google Scholar] [CrossRef]
- Reverchon, E.; Adami, R. Nanomaterials and Supercritical Fluids. J. Supercrit. Fluids 2006, 37, 1–22. [Google Scholar] [CrossRef]
- Aguiar-Ricardo, A.; Costa, E. Supercritical Fluid Manufacture. In Pharmaceutical Inhalation Aerosol Technology, 3rd ed.; Hickey, A.J., da Rocha, S.R.P., Eds.; CRC Press: Boca Raton, FL, USA, 2019; pp. 1–21. [Google Scholar]
- Gupta, R.B.; Shim, J.-J. Solubility in Supercritical Carbon Dioxide, 1st ed.; CRC Press: Boca Raton, FL, USA, 2007; pp. 1–18. [Google Scholar]
- Reverchon, E.; Donsi, G.; Gorgoglione, D. Salicylic Acid Solubilization in Supercritical CO2 and Its Micronization by RESS. J. Supercrit. Fluids 1993, 6, 241–248. [Google Scholar] [CrossRef]
- Yildiz, N.; Tuna, Ş.; Döker, O.; Çalimli, A. Micronization of Salicylic Acid and Taxol (Paclitaxel) by Rapid Expansion of Supercritical Fluids (RESS). J. Supercrit. Fluids 2007, 41, 440–451. [Google Scholar] [CrossRef]
- Costa, C.; Casimiro, T.; Aguiar-Ricardo, A. Optimization of Supercritical CO2-Assisted Atomization: Phase Behavior and Design of Experiments. J. Chem. Eng. Data 2018, 63, 885–896. [Google Scholar] [CrossRef]
- Mishima, K.; Matsuyama, K.; Tanabe, D.; Yamauchi, S.; Young, T.J.; Johnston, K.P. Microencapsulation of Proteins by Rapid Expansion of Supercritical Solution with a Nonsolvent. AIChE J. 2000, 46, 857–865. [Google Scholar] [CrossRef]
- Matsuyama, K.; Mishima, K.; Hayasččhi, K.I.; Ishikawa, H.; Matsuyama, H.; Harada, T. Formation of Microcapsules of Medicines by the Rapid Expansion of a Supercritical Solution with a Nonsolvent. J. Appl. Polym. Sci. 2003, 89, 742–752. [Google Scholar] [CrossRef]
- Pathak, P.; Meziani, M.J.; Desai, T.; Sun, Y.P. Nanosizing Drug Particles in Supercritical Fluid Processing. J. Am. Chem. Soc. 2004, 126, 10842–10843. [Google Scholar] [CrossRef] [PubMed]
- Xiang, S.T.; Chen, B.Q.; Kankala, R.K.; Wang, S.B.; Chen, A.Z. Solubility Measurement and RESOLV-Assisted Nanonization of Gambogic Acid in Supercritical Carbon Dioxide for Cancer Therapy. J. Supercrit. Fluids 2019, 150, 147–155. [Google Scholar] [CrossRef]
- Ribeiro Dos Santos, I.; Richard, J.; Pech, B.; Thies, C.; Benoit, J.P. Microencapsulation of Protein Particles within Lipids Using a Novel Supercritical Fluid Process. Int. J. Pharm. 2002, 242, 69–78. [Google Scholar] [CrossRef]
- Vergara-Mendoza, M.D.S.; Ortiz-Estrada, C.H.; González-Martínez, J.; Quezada-Gallo, J.A. Microencapsulation of Coenzyme Q 10 in Poly(Ethylene Glycol) and Poly(Lactic Acid) with Supercritical Carbon Dioxide. Ind. Eng. Chem. Res. 2012, 51, 5840–5846. [Google Scholar] [CrossRef]
- Segura, M.F.; Gallego, S.; Sánchez de Toledo, J.; Soriano, A.; Ventosa, N.; Veciana, J.; Boloix, A.; Segovia Ramos, N.V. Nanovesicles and Its Use for Nucleic Acid Delivery. WO Patent 2020/229469, 19 November 2020. [Google Scholar]
- Weidner, E.; Knez, Ž.; Novak, Z. Process for Preparing Particles or Powders. WO Patent 1995/021688, 17 August 1995. [Google Scholar]
- Kerč, J.; Srčič, S.; Knez, Ž.; Senčar-Božič, P. Micronization of Drugs Using Supercritical Carbon Dioxide. Int. J. Pharm. 1999, 182, 33–39. [Google Scholar] [CrossRef]
- Hao, J.; Whitaker, M.J.; Wong, B.; Serhatkulu, G.; Shakesheff, K.M.; Howdle, S.M. Plasticization and Spraying of Poly (DL-lactic Acid) Using Supercritical Carbon Dioxide: Control of Particle Size. J. Pharm. Sci. 2004, 93, 1083–1090. [Google Scholar] [CrossRef]
- Shieh, Y.-T.; Su, J.-H.; Manivannan, G.; Lee, P.H.C.; Sawan, S.P.; Spall, W.D. Interaction of Supercritical Carbon Dioxide with Polymers. I. Crystalline Polymers. J. Appl. Polym. Sci. 1996, 59, 695–705. [Google Scholar] [CrossRef]
- Perinelli, D.R.; Bonacucina, G.; Cespi, M.; Naylor, A.; Whitaker, M.; Palmieri, G.F.; Giorgioni, G.; Casettari, L. Evaluation of P(L)LA-PEG-P(L)LA as Processing Aid for Biodegradable Particles from Gas Saturated Solutions (PGSS) Process. Int. J. Pharm. 2014, 468, 250–257. [Google Scholar] [CrossRef]
- Hao, J.; Whitaker, M.J.; Serhatkulu, G.; Shakesheff, K.M.; Howdle, S.M. Supercritical Fluid Assisted Melting of Poly(Ethylene Glycol): A New Solvent-Free Route to Microparticles. J. Mater. Chem. A 2005, 15, 1148–1153. [Google Scholar] [CrossRef]
- Jordan, F.; Naylor, A.; Kelly, C.A.; Howdle, S.M.; Lewis, A.; Illum, L. Sustained Release HGH Microsphere Formulation Produced by a Novel Supercritical Fluid Technology: In Vivo Studies. J. Control Release 2010, 141, 153–160. [Google Scholar] [CrossRef]
- Rodrigues, M.; Peiriço, N.; Matos, H.; Gomes de Azevedo, E.; Lobato, M.R.; Almeida, A.J. Microcomposites Theophylline/Hydrogenated Palm Oil from a PGSS Process for Controlled Drug Delivery Systems. J. Supercrit. Fluids 2004, 29, 175–184. [Google Scholar] [CrossRef]
- Tokunaga, S.; Ono, K.; Ito, S.; Sharmin, T.; Kato, T.; Irie, K.; Mishima, K.; Satho, T.; Harada, T.; Aida, T.M.; et al. Microencapsulation of Drug with Enteric Polymer Eudragit L100 for Controlled Release Using the Particles from Gas Saturated Solutions (PGSS) Process. J. Supercrit. Fluids 2021, 167, 105044. [Google Scholar] [CrossRef]
- Whitaker, M.J.; Hao, J.; Davies, O.R.; Serhatkulu, G.; Stolnik-Trenkic, S.; Howdle, S.M.; Shakesheff, K.M. The Production of Protein-Loaded Microparticles by Supercritical Fluid Enhanced Mixing and Spraying. J. Control Release 2005, 101, 85–92. [Google Scholar] [CrossRef] [PubMed]
- Salmaso, S.; Bersani, S.; Elvassore, N.; Bertucco, A.; Caliceti, P. Biopharmaceutical Characterisation of Insulin and Recombinant Human Growth Hormone Loaded Lipid Submicron Particles Produced by Supercritical Gas Micro-Atomisation. Int. J. Pharm. 2009, 379, 51–58. [Google Scholar] [CrossRef]
- Vezzù, K.; Borin, D.; Bertucco, A.; Bersani, S.; Salmaso, S.; Caliceti, P. Production of Lipid Microparticles Containing Bioactive Molecules Functionalized with PEG. J. Supercrit. Fluids 2010, 54, 328–334. [Google Scholar] [CrossRef]
- Salmaso, S.; Elvassore, N.; Bertucco, A.; Caliceti, P. Production of Solid Lipid Submicron Particles for Protein Delivery Using a Novel Supercritical Gas-Assisted Melting Atomization Process. J. Pharm. Sci. 2009, 98, 640–650. [Google Scholar] [CrossRef]
- Hu, X.; Guo, Y.; Wang, L.; Hua, D.; Hong, Y.; Li, J. Coenzyme Q10 Nanoparticles Prepared by a Supercritical Fluid-Based Method. J. Supercrit. Fluids 2011, 57, 66–72. [Google Scholar] [CrossRef]
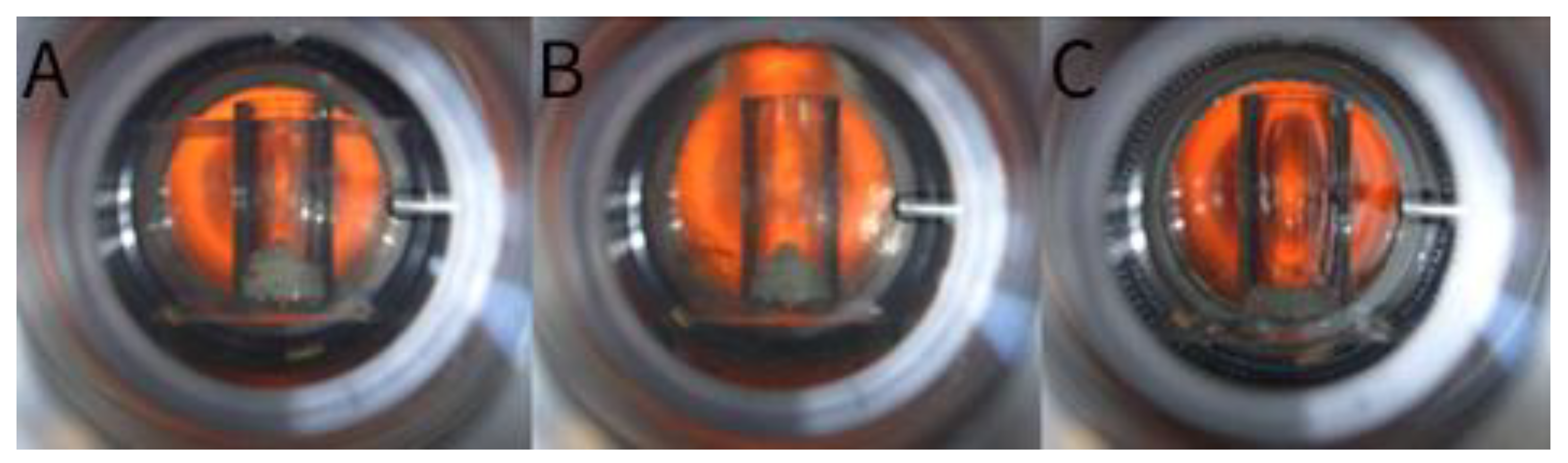
- Kelly, C.A.; Howdle, S.M.; Naylor, A.; Coxhill, G.; Tye, L.C.; Illum, L.; Lewis, A.L. Stability of Human Growth Hormone in Supercritical Carbon Dioxide. J. Pharm. Sci. 2012, 101, 56–67. [Google Scholar] [CrossRef]
- Falconer, J.R.; Wen, J.; Zargar-Shoshtari, S.; Chen, J.J.; Farid, M.; Tallon, S.J.; Alany, R.G. Preparation and Characterization of Progesterone Dispersions Using Supercritical Carbon Dioxide. Drug Dev. Ind. Pharm. 2014, 40, 458–469. [Google Scholar] [CrossRef]
- Couto, R.; Alvarez, V.; Temelli, F. Encapsulation of Vitamin B2 in Solid Lipid Nanoparticles Using Supercritical CO2. J. Supercrit. Fluids 2017, 120, 432–442. [Google Scholar] [CrossRef]
- Sievers, R.E.; Karst, U. Methods for Fine Particle Formation. U.S. Patent 5639441, 17 June 1997. [Google Scholar]
- Sievers, R.E. Formation of Aqueous Small Droplet Aerosols Assisted by Supercritical Carbon Dioxide. Aerosol Sci. Technol. 1999, 30, 3–15. [Google Scholar] [CrossRef]
- Xu, C.; Watkins, B.A.; Sievers, R.E.; Jing, X.; Trowga, P.; Gibbons, C.S.; Vecht, A. Submicron-Sized Spherical Yttrium Oxide Based Phosphors Prepared by Supercritical CO2-Assisted Aerosolization and Pyrolysis. Appl. Phys. Lett. 1997, 71, 1643–1645. [Google Scholar] [CrossRef]
- Sellers, S.P.; Clark, G.S.; Sievers, R.E.; Carpenter, J.F. Dry Powders of Stable Protein Formulations from Aqueous Solutions Prepared Using Supercritical CO2-assisted Aerosolization. J. Pharm. Sci. 2001, 90, 785–797. [Google Scholar] [CrossRef]
- Sievers, R.E.; Quinn, B.P.; Cape, S.P.; Searles, J.A.; Braun, C.S.; Bhagwat, P.; Rebits, L.G.; McAdams, D.H.; Burger, J.L.; Best, J.A.; et al. Near-Critical Fluid Micronization of Stabilized Vaccines, Antibiotics and Anti-Virals. J. Supercrit. Fluids 2007, 42, 385–391. [Google Scholar] [CrossRef]
- Cape, S.P.; Villa, J.A.; Huang, E.T.S.; Yang, T.-H.; Carpenter, J.F.; Sievers, R.E. Preparation of Active Proteins, Vaccines and Pharmaceuticals as Fine Powders Using Supercritical or Near-Critical Fluids. Pharm. Res. 2008, 25, 1967–1990. [Google Scholar] [CrossRef]
- Kisich, K.O.; Higgins, M.P.; Park, I.; Cape, S.P.; Lindsay, L.; Bennett, D.J.; Winston, S.; Searles, J.; Sievers, R.E. Dry Powder Measles Vaccine: Particle Deposition, Virus Replication, and Immune Response in Cotton Rats Following Inhalation. Vaccine 2011, 29, 905–912. [Google Scholar] [CrossRef]
- Burger, J.L.; Cape, S.P.; Braun, C.S.; McAdams, D.H.; Best, J.A.; Bhagwat, P.; Pathak, P.; Rebits, L.G.; Sievers, R.E. Stabilizing Formulations for Inhalable Powders of Live-Attenuated Measles Virus Vaccine. J. Aerosol Med. Pulm. Drug Deliv. 2008, 21, 25–34. [Google Scholar] [CrossRef] [PubMed]
- Lin, W.-H.; Griffin, D.E.; Rota, P.A.; Papania, M.; Cape, S.P.; Bennett, D.; Quinn, B.; Sievers, R.E.; Shermer, C.; Powell, K.; et al. Successful Respiratory Immunization with Dry Powder Live-Attenuated Measles Virus Vaccine in Rhesus Macaques. Proc. Natl. Acad. Sci. USA 2011, 108, 2987–2992. [Google Scholar] [CrossRef]
- Manion, J.R.; Cape, S.P.; McAdams, D.H.; Rebits, L.G.; Sievers, R.E. Inhalable Antibiotics Manufactured Through Use of Near-Critical or Supercritical Fluids. Aerosol Sci. Technol. 2012, 46, 403–410. [Google Scholar] [CrossRef]
- Reverchon, E. Process For The Production Of Micro And/Or Nano Particles. U.S. Patent 7276190, 2 October 2001. [Google Scholar]
- Adeoye, O.; Costa, C.; Casimiro, T.; Aguiar-Ricardo, A.; Cabral-Marques, H. Preparation of Ibuprofen/Hydroxypropyl-γ-Cyclodextrin Inclusion Complexes Using Supercritical CO2-Assisted Spray Drying. J. Supercrit. Fluids 2018, 133, 479–485. [Google Scholar] [CrossRef]
- Adami, R.; Osséo, L.S.; Reverchon, E. Micronization of Lysozyme by Supercritical Assisted Atomization. Biotechnol. Bioeng. 2009, 104, 1162–1170. [Google Scholar] [CrossRef]
- Reverchon, E. Supercritical-Assisted Atomization To Produce Micro- and/or Nanoparticles of Controlled Size and Distribution. Ind. Eng. Chem. Res. 2002, 41, 2405–2411. [Google Scholar] [CrossRef]
- Reverchon, E.; Porta, G. Della Spada, A. Ampicillin Micronization by Supercritical Assisted Atomization. J. Pharm. Pharmacol. 2010, 55, 1465–1471. [Google Scholar] [CrossRef]
- Reverchon, E.; Porta, G. Della Micronization of Antibiotics by Supercritical Assisted Atomization. J. Supercrit. Fluids 2003, 26, 243–252. [Google Scholar] [CrossRef]
- Reverchon, E.; Spada, A. Erythromycin Micro-Particles Produced by Supercritical Fluid Atomization. Powder Technol. 2004, 141, 100–108. [Google Scholar] [CrossRef]
- Reverchon, E.; Antonacci, A. Chitosan Microparticles Production by Supercritical Fluid Processing. Ind. Eng. Chem. Res. 2006, 45, 5722–5728. [Google Scholar] [CrossRef]
- Reverchon, E.; Antonacci, A. Polymer Microparticles Production by Supercritical Assisted Atomization. J. Supercrit. Fluids 2007, 39, 444–452. [Google Scholar] [CrossRef]
- Reverchon, E.; Antonacci, A. Drug–Polymer Microparticles Produced by Supercritical Assisted Atomization. Biotechnol. Bioeng. 2007, 97, 1626–1637. [Google Scholar] [CrossRef] [PubMed]
- Cabral, R.P.; Sousa, A.M.L.; Silva, A.S.; Paninho, A.I.; Temtem, M.; Costa, E.; Casimiro, T.; Aguiar-Ricardo, A. Design of Experiments Approach on the Preparation of Dry Inhaler Chitosan Composite Formulations by Supercritical CO2-Assisted Spray-Drying. J. Supercrit. Fluids 2016, 116, 26–35. [Google Scholar] [CrossRef]
- Restani, R.B.; Silva, A.S.; Pires, R.F.; Cabral, R.; Correia, I.J.; Casimiro, T.; Bonifácio, V.D.B.; Aguiar-Ricardo, A. Nano-in-Micro POxylated Polyurea Dendrimers and Chitosan Dry Powder Formulations for Pulmonary Delivery. Part. Part. Syst. Charact. 2016, 33, 851–858. [Google Scholar] [CrossRef]
- Silva, A.S.; Sousa, A.M.; Cabral, R.P.; Silva, M.C.; Costa, C.; Miguel, S.P.; Bonifácio, V.D.B.; Casimiro, T.; Correia, I.J.; Aguiar-Ricardo, A. Aerosolizable Gold Nano-in-Micro Dry Powder Formulations for Theragnosis and Lung Delivery. Int. J. Pharm. 2017, 519, 240–249. [Google Scholar] [CrossRef]
- Silva, M.; Silva, A.; Fernandez-Lodeiro, J.; Casimiro, T.; Lodeiro, C.; Aguiar-Ricardo, A. Supercritical CO2-Assisted Spray Drying of Strawberry-Like Gold-Coated Magnetite Nanocomposites in Chitosan Powders for Inhalation. Materials 2017, 10, 74. [Google Scholar] [CrossRef]
- Cai, M.-Q.; Guan, Y.-X.; Yao, S.-J.; Zhu, Z.-Q. Supercritical Fluid Assisted Atomization Introduced by Hydrodynamic Cavitation Mixer (SAA-HCM) for Micronization of Levofloxacin Hydrochloride. J. Supercrit. Fluids 2008, 43, 524–534. [Google Scholar] [CrossRef]
- Silva, A.S.; Shopsowitz, K.E.; Correa, S.; Morton, S.W.; Dreaden, E.C.; Casimiro, T.; Aguiar-Ricardo, A.; Hammond, P.T. Rational Design of Multistage Drug Delivery Vehicles for Pulmonary RNA Interference Therapy. Int. J. Pharm. 2020, 591, 119989. [Google Scholar] [CrossRef] [PubMed]
- Costa, C.; Nobre, B.; Matos, A.S.; Silva, A.S.; Casimiro, T.; Corvo, M.L.; Aguiar-Ricardo, A. Inhalable Hydrophilic Molecule-Loaded Liposomal Dry Powder Formulations Using Supercritical CO2–Assisted Spray-Drying. J. CO2 Util. 2021, 53, 101709. [Google Scholar] [CrossRef]
- Zalepugin, D.Y.; Tilkunova, N.A.; Fronchek, E.V.; Gallyamov, M.O.; Chernyshova, I.V.; Mishin, V.S.; Yashin, Y.S.; Grigoryev, T.E.; Gamzazade, A.I.; Khokhlov, A.R. Production of New Haemostatic Materials by Deposition of Dispersed Proteins onto Porous Matrices Using Supercritical Carbon Dioxide. Russ. J. Phys. Chem. B 2010, 4, 1047–1050. [Google Scholar] [CrossRef]
- Della Porta, G.; Adami, R.; Della Porta, G.; Adami, R.; Del Gaudio, P.; Prota, L.; Aquino, R.; Reverchon, E. Albumin/Gentamicin Microspheres Produced by Supercritical Assisted Atomization: Optimization of Size, Drug Loading and Release. J. Pharm. Sci. 2010, 90, 4720–4729. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.; Guan, Y.X.; Yao, S.J.; Zhu, Z.Q. Controllable Preparation and Formation Mechanism of BSA Microparticles Using Supercritical Assisted Atomization with an Enhanced Mixer. J. Supercrit. Fluids 2011, 56, 97–104. [Google Scholar] [CrossRef]
- Adami, R.; Liparoti, S.; Reverchon, E. A New Supercritical Assisted Atomization Configuration, for the Micronization of Thermolabile Compounds. Chem. Eng. J. 2011, 173, 55–61. [Google Scholar] [CrossRef]
- Du, Z.; Guan, Y.X.; Yao, S.J.; Zhu, Z.Q. Supercritical Fluid Assisted Atomization Introduced by an Enhanced Mixer for Micronization of Lysozyme: Particle Morphology, Size and Protein Stability. Int. J. Pharm. 2011, 421, 258–268. [Google Scholar] [CrossRef]
- Du, Z.; Tang, C.; Guan, Y.X.; Yao, S.J.; Zhu, Z.Q. Bioactive Insulin Microparticles Produced by Supercritical Fluid Assisted Atomization with an Enhanced Mixer. Int. J. Pharm. 2013, 454, 174–182. [Google Scholar] [CrossRef] [PubMed]
- Shen, Y.B.; Guan, Y.X.; Yao, S.J. Supercritical Fluid Assisted Production of Micrometric Powders of the Labile Trypsin and Chitosan/Trypsin Composite Microparticles. Int. J. Pharm. 2015, 489, 226–236. [Google Scholar] [CrossRef]
- Hong, D.X.; Yun, Y.L.; Guan, Y.X.; Yao, S.J. Preparation of Micrometric Powders of Parathyroid Hormone (PTH1–34)-Loaded Chitosan Oligosaccharide by Supercritical Fluid Assisted Atomization. Int. J. Pharm. 2018, 545, 389–394. [Google Scholar] [CrossRef] [PubMed]
- Santo, I.E.; Campardelli, R.; Albuquerque, E.C.; de Melo, S.V.; Della Porta, G.; Reverchon, E. Liposomes Preparation Using a Supercritical Fluid Assisted Continuous Process. Chem. Eng. J. 2014, 249, 153–159. [Google Scholar] [CrossRef]
- Campardelli, R.; Espirito Santo, I.; Albuquerque, E.C.; de Melo, S.V.; Della Porta, G.; Reverchon, E. Efficient Encapsulation of Proteins in Submicro Liposomes Using a Supercritical Fluid Assisted Continuous Process. J. Supercrit. Fluids 2016, 107, 163–169. [Google Scholar] [CrossRef]
- Trucillo, P.; Campardelli, R.; Reverchon, E. A Versatile Supercritical Assisted Process for the One-Shot Production of Liposomes. J. Supercrit. Fluids 2019, 146, 136–143. [Google Scholar] [CrossRef]
- Ventosa, N.; Sala, S.; Veciana, J.; Torres, J.; Llibre, J. Depressurization of an Expanded Liquid Organic Solution (DELOS): A New Procedure for Obtaining Submicron- Or Micron-Sized Crystalline Particles. Cryst. Growth Des. 2001, 1, 299–303. [Google Scholar] [CrossRef]
- Ventosa, N.; Sala, S.; Veciana, J. DELOS Process: A Crystallization Technique Using Compressed Fluids-1. Comparison to the GAS Crystallization Method. J. Supercrit. Fluids 2003, 26, 33–45. [Google Scholar] [CrossRef]
- Muntó, M.; Ventosa, N.; Veciana, J. Synergistic Solubility Behaviour of a Polyoxyalkylene Block Co-Polymer and Its Precipitation from Liquid CO2-Expanded Ethanol as Solid Microparticles. J. Supercrit. Fluids 2008, 47, 290–295. [Google Scholar] [CrossRef]
- Muntó, M.; Ventosa, N.; Sala, S.; Veciana, J. Solubility Behaviors of Ibuprofen and Naproxen Drugs in Liquid “CO2-Organic Solvent” Mixtures. J. Supercrit. Fluids 2008, 47, 147–153. [Google Scholar] [CrossRef]
- Sala, S.; Córdoba, A.; Moreno-Calvo, E.; Elizondo, E.; Muntó, M.; Rojas, P.E.; Larrayoz, M.À.; Ventosa, N.; Veciana, J. Crystallization of Microparticulate Pure Polymorphs of Active Pharmaceutical Ingredients Using CO 2-Expanded Solvents. Cryst. Growth Des. 2012, 12, 1717–1726. [Google Scholar] [CrossRef]
- Elizondo, E.; Larsen, J.; Hatzakis, N.S.; Cabrera, I.; Bjørnholm, T.; Veciana, J.; Stamou, D.; Ventosa, N. Influence of the Preparation Route on the Supramolecular Organization of Lipids in a Vesicular System. J. Am. Chem. Soc. 2012, 134, 1918–1921. [Google Scholar] [CrossRef]
- Elizondo, E.; Veciana, J.; Ventosa, N. Nanostructuring Molecular Materials as Particles and Vesicles for Drug Delivery, Using Compressed and Supercritical Fluids. Nanomedicine 2012, 7, 1391–1408. [Google Scholar] [CrossRef]
- Cano-Sarabia, M.; Ventosa, N.; Sala, S.; Patiño, C.; Arranz, R.; Veciana, J. Preparation of Uniform Rich Cholesterol Unilamellar Nanovesicles Using CO2-Expanded Solvents. Langmuir 2008, 24, 2433–2437. [Google Scholar] [CrossRef]
- Merlo-Mas, J.; Tomsen-Melero, J.; Corchero, J.L.; González-Mira, E.; Font, A.; Pedersen, J.N.; García-Aranda, N.; Cristóbal-Lecina, E.; Alcaina-Hernando, M.; Mendoza, R.; et al. Application of Quality by Design to the Robust Preparation of a Liposomal GLA Formulation by DELOS-Susp Method. J. Supercrit. Fluids 2021, 173, 105204. [Google Scholar] [CrossRef]
- Cabrera, I.; Elizondo, E.; Esteban, O.; Corchero, J.L.; Melgarejo, M.; Pulido, D.; Córdoba, A.; Moreno, E.; Unzueta, U.; Vazquez, E.; et al. Multifunctional Nanovesicle-Bioactive Conjugates Prepared by a One-Step Scalable Method Using CO2 -Expanded Solvents. Nano Lett. 2013, 13, 3766–3774. [Google Scholar] [CrossRef] [PubMed]
- Davies, O.R.; Lewis, A.L.; Whitaker, M.J.; Tai, H.; Shakesheff, K.M.; Howdle, S.M. Applications of Supercritical CO2 in the Fabrication of Polymer Systems for Drug Delivery and Tissue Engineering. Adv. Drug Deliv. Rev. 2008, 60, 373–387. [Google Scholar] [CrossRef]
- Kalani, M.; Yunus, R. Application of Supercritical Antisolvent Method in Drug Encapsulation: A Review. Int. J. Nanomed. 2011, 6, 1429–1442. [Google Scholar] [CrossRef]
- Elvassore, N.; Bertucco, A.; Caliceti, P. Production of Protein-Loaded Polymeric Microcapsules by Compressed CO2 in a Mixed Solvent. Ind. Eng. Chem. Res. 2001, 40, 795–800. [Google Scholar] [CrossRef]
- Franco, P.; De Marco, I. Supercritical Antisolvent Process for Pharmaceutical Applications: A Review. Processes 2020, 8, 938. [Google Scholar] [CrossRef]
- Yeo, S.-D.; Lim, G.-B.; Debendetti, P.G.; Bernstein, H. Formation of Microparticulate Protein Powder Using a Supercritical Fluid Antisolvent. Biotechnol. Bioeng. 1993, 41, 341–346. [Google Scholar] [CrossRef]
- Yeo, S.; Debenedetti, P.G.; Patro, S.Y.; Przybycien, T.M. Secondary Structure Characterization of Microparticulate Insulin Powders. J. Pharm. Sci. 1994, 83, 1651–1656. [Google Scholar] [CrossRef]
- Bleich, J.; Kleinebudde, P.; Müller, B.W. Influence of Gas Density and Pressure on Microparticles Produced with the ASES Process. Int. J. Pharm. 1994, 106, 77–84. [Google Scholar] [CrossRef]
- Palakodaty, S.; York, P.; Pritchard, J. Supercritical Fluid Processing of Materials from Aqueous Solutions: The Application of SEDS to Lactose as a Model Substance. Pharm. Res. 1998, 15, 1835–1843. [Google Scholar] [CrossRef]
- Young, T.J.; Johnston, K.P.; Mishima, K.; Tanaka, H. Encapsulation of Lysozyme in a Biodegradable Polymer by Precipitation with a Vapor-over-Liquid Antisolvent. J. Pharm. Sci. 1999, 88, 640–650. [Google Scholar] [CrossRef]
- Kankala, R.K.; Zhang, Y.S.; Wang, S.-B.; Lee, C.-H.; Chen, A.-Z. Supercritical Fluid Technology: An Emphasis on Drug Delivery and Related Biomedical Applications. Adv. Healthc. Mater. 2017, 6, 1700433. [Google Scholar] [CrossRef]
- Rodrigues, M.A.; Li, J.; Padrela, L.; Almeida, A.; Matos, H.A.; de Azevedo, E.G. Anti-Solvent Effect in the Production of Lysozyme Nanoparticles by Supercritical Fluid-Assisted Atomization Processes. J. Supercrit. Fluids 2009, 48, 253–260. [Google Scholar] [CrossRef]
- Kang, Y.; Yang, C.; Ouyang, P.; Yin, G.; Huang, Z.; Yao, Y.; Liao, X. The Preparation of BSA-PLLA Microparticles in a Batch Supercritical Anti-Solvent Process. Carbohydr. Polym. 2009, 77, 244–249. [Google Scholar] [CrossRef]
- Fusaro, F.; Kluge, J.; Mazzotti, M.; Muhrer, G. Compressed CO2 Antisolvent Precipitation of Lysozyme. J. Supercrit. Fluids 2009, 49, 79–92. [Google Scholar] [CrossRef]
- Jin, H.Y.; Xia, F.; Zhao, Y.P. Preparation of Hydroxypropyl Methyl Cellulose Phthalate Nanoparticles with Mixed Solvent Using Supercritical Antisolvent Process and Its Application in Co-Precipitation of Insulin. Adv. Powder Technol. 2012, 23, 157–163. [Google Scholar] [CrossRef]
- Roy, I.; Gupta, M.N. Freeze-Drying of Proteins: Some Emerging Concerns. Biotechnol. Appl. Biochem. 2004, 39, 165–177. [Google Scholar] [CrossRef]
- Zhai, S.; Hansen, R.K.; Taylor, R.; Skepper, J.N.; Sanches, R.; Slater, N.K.H. Effect of Freezing Rates and Excipients on the Infectivity of a LiveViral Vaccine during Lyophilization. Biotechnol. Prog. 2004, 20, 1113–1120. [Google Scholar] [CrossRef]
- Arsiccio, A.; Pisano, R. The Preservation of Lyophilized Human Growth Hormone Activity: How Do Buffers and Sugars Interact? Pharm. Res. 2018, 35, 131. [Google Scholar] [CrossRef] [PubMed]
- Ajmera, A.; Scherließ, R. Stabilisation of Proteins via Mixtures of Amino Acids during Spray Drying. Int. J. Pharm. 2014, 463, 98–107. [Google Scholar] [CrossRef] [PubMed]
- Fernandes, D.A.; Leandro, P.; Costa, E.; Corvo, M.L. Dry Powder Inhaler Formulation of Cu,Zn-Superoxide Dismutase by Spray Drying: A Proof-of-Concept. Powder Technol. 2021, 389, 131–137. [Google Scholar] [CrossRef]
- Ji, S.; Thulstrup, P.W.; Mu, H.; Hansen, S.H.; van de Weert, M.; Rantanen, J.; Yang, M. Investigation of Factors Affecting the Stability of Lysozyme Spray Dried from Ethanol-Water Solutions. Int. J. Pharm. 2017, 534, 263–271. [Google Scholar] [CrossRef]

| Year | Active Compound | Co-Solvent | Solid Dosage Form | Observations | Ref. |
|---|---|---|---|---|---|
| 2000 | Lysozyme * Lipase | Ethanol | PEG 1 PMMA 2 P(DLLA) 3 P(St) 4 PLGA 5 PEG-PPG 6 | Lower diameters for ethanol as a co-solvent The size is more influenced by the polymer feed composition | [44] |
| 2002 | BSA 7 | N/A | Dynasan®114 Gelucire®50-02 | Similar RESS method Dynasan®114-based microparticle diameter < 50 µm 13% < BSA content < 62% Gelucire®50-02-based microparticles with a mean size of 543 µm 36% < BSA content < 67% | [48] |
| 2012 | Co-enzyme Q10 | Ethanol Acetone Dichloromethane | PEG 1 P(DLLA) 3 | Microparticle diameter between 2–8 µm PEG coating results in higher microparticles Higher coQ10 release for higher microparticles | [49] |
| 2013 | Insulin | Ethanol | Tripalmitin | RESS is combined with the supercritical assisted drying (SAD) 3.5 µm < PSD 8 < 11 µm Insulin content of 33.1% | [50] |
| Year | Active Compound | Co-Solvent | Solid Dosage Form | Observations | Ref. |
|---|---|---|---|---|---|
| 2005 | RNase A Lysozyme Insulin Salmon calcitonin | N/A | P(DLLA) | 10 µm < PS 1 < 300 µm Insulin and salmon calcitonin microparticles with rough morphologies Poor particle size control RNase A and lysozyme retained their enzymatic activity Stored insulin microparticles decrease in activity at 25 °C for 1 week and 1 month Due to the low dosage of calcitonin, the salmon calcitonin was mixed with polymer powder and freeze-dried | [60] |
| 2009 | Insulin Recombinant human growth hormone (rh-GH) | 1 mL of DMSO 2 containing the protein | Tristearin/Phosphatidylcholine/PEG5000 | Spherical particles with a mean diameter of 197 nm Insulin recovery of 57 ± 8% rh-GH recovery 48 ± 5% Glucose reduction of 50% with the lower dose and 70% at the higher dose, in 1–2 h. | [61] |
| 2009 | Insulin | 1 mL of DMSO containing the protein | Tristearin/Phosphatidylcholine/PEG/Tween80 Tristearin/Phosphatidylcholine/dioctyl sulfosuccinate | The authors defined the process as GAMA Binodal size distribution two main particle size populations. The main fraction had a diameter range of 200–400 nm, and a minor fraction had a diameter range of 80–120 nm. | [63] |
| 2010 | RNase A | 1 mL of DMSO containing the enzyme | Tristearin/Phosphatidylcholine/PEG5000 | The higher the T, the higher the product yield The higher the T, the higher the particle size EE up to 80% The enzyme retained its a residual activity of about 83% | [62] |
| 2010 | Human growth hormone (hGH) | N/A | P(DLLA) PLGA Excipients 3 | Rounded particles with few pores Apparent size around 93 μm 56.1 μm < D50 4 < 104.5 μm 97.1% < EE < 100% | [57] |
| 2011 | Co-enzyme Q10 | N/A | PEG6000 | Particle size of 190 nm 220 nm < Dv50 5 < 2.36 µm Enzyme recovery yield of 89.8% 6 | [64] |
| 2011 | Human growth hormone (hGH) | N/A | PLGA P(DLLA) Poloxamer 407 | EE of 98.3 ± 4.6% The structural integrity of hGH is unaffected by scCO | [65] |
| 2013 | Progesterone (PGN) | N/A | PEG400/PEG4000 (50:50) D-α-tocopheryl PEG1000 succinate (TPGS) Gelucire 44/14 | At T of approximately 56 °C, process yields of 95.7% for PNG-loaded TPGS86.3% for PNG-loaded PEG93.3% for PNG-loaded Gelucire 44/14 PGN showed high dissolution rates for all the formulations | [66] |
| 2014 | Bovine serum albumin (BSA) | N/A | P(LLA) -PEG1500- P(LLA) | 19. 07 µm < PS50 < 78.63 µm 29.19% < Process yield < 41.74% 96.85% < EE < 101.75% | [55] |
| Year | Active Compound | Nanocarrier | Co-Solvent | Solid Dosage Form | Observations | Ref. |
|---|---|---|---|---|---|---|
| 2009 | Lysozyme | N/A | Ethanol | N/A | Spherical microparticles 1.0 µm < PSD < 4.0 µm Lysozyme remained stable with biological activity from 95% to 100%. | [80] |
| 2009 | Lysozyme Trypsin | N/A | N/A | N/A | 80% of trypsin and 65% of lysozyme particles have a diameter smaller than 5 µm | [95] |
| 2010 | Gentamicin sulfate * | N/A | N/A | BSA | Mean diameter of 2 µm 1.70 µm < D50 > 2.24 µm EE > 95.6% | [96] |
| 2011 | BSA | N/A | N/A | N/A | Well-defined, hollow, and spherical BSA microparticles 0.3 µm < PSD < 5.0 µm | [97] |
| 2011 | BSA | N/A | N/A | N/A | The solubility of BSA is dependent on processing temperature | [98] |
| 2011 | Lysozyme | N/A | Ethanol | N/A | SAA-HCM 1 0.2 µm < PS < 5.0 µm Lysozyme kept 85% of its activity | [99] |
| 2013 | Insulin | N/A | N/A | N/A | SAA-HCM 0.5 µm < PS < 5.0 µm | [100] |
| 2015 | Trypsin | N/A | N/A | Chitosan | SAA-HCM 0.2 µm < PS < 4.0 µm LE 2 up to 91.8% Trypsin retained > 70% of its enzymatic activity | [101] |
| 2017 | BSA | N/A | Acetonitrile | PLGA | 1.7 µm < MMAD 3 < 3.5 µm FPF 4 of 43% BSA showed both chemical and structural stability | [30] |
| 2018 | Parathyroid hormone | N/A | N/A | Chitosan oligosaccharide | SAA-HCM 1.0 µm < MMAD < 5.0 µm FPF of 63.51% LE up to 92.8% | [102] |
| 2020 | SiRNA 5 | Mesoporous silica nanoparticles Poly-L-arginine Hyaluronic acid | Ethanol | Chitosan (CHT) | 3.0 µm < Dv,50 < 4.0 µm FPF of 44.4% EEsiRNA of 11.4% onto LBL nanosystems Entrapment efficiency of the LbL nanoparticles of 28.7% in CHT powder 90% of gene silencing from CHT-LbL siRNA | [93] |
| Year | Active Compound | Co-Solvent | Solid Dosage Form | Observations | Ref. |
|---|---|---|---|---|---|
| 1993 | Insulin | DMSO DMFA 1 | N/A | 90% of the particles with a diameter smaller than 4 µm 10% of the particles with a diameter smaller than 1 µm Blood glucose level decreases over the time | [120] |
| 1999 | Lysozyme | DCM 2 | (a) P(LLA) 3 (b) PLGA | PCA (a) 250 µm < Diameter < 500 µm (b) 5 µm < Diameter < 60 µm CO2 at high velocity through an annular region in a coaxial nozzle results in spherical and uniform particles | [124] |
| 2001 | Insulin | (a) DCM (b) DCM- DMSO (50:50,%v/v) | P(LLA) 3 | (a) 1 µm < Diameter < 3 µm (b) 0.5 µm < Diameter < 2 µm | [118] |
| 2009 | Lysozyme | Water/EtOH | N/A | SEDS Fiber formation at higher pressures 0.1 µm < PSD < 0.4 µm Lysozyme activity was recovered from all spherical particles | [126] |
| 2009 | BSA | DCM | P(LLA) 3 | PS < 2.5 µm The secondary BSA structure is not affected BSA content of 17.11% | [127] |
| 2009 | Lysozyme | DMSO | N/A | PCA: PS < 100 nm GAS: 233 nm < PS < 302 nm Formation of the lysozyme particles involves spinodal decomposition | [128] |
| 2012 | Insulin | DMSO/Acetone | HPMCP 4 | 138 nm < PS < 342 nm EE up to 100% 10. 76% < Insulin loading < 16.04% | [129] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Costa, C.; Casimiro, T.; Corvo, M.L.; Aguiar-Ricardo, A. Solid Dosage Forms of Biopharmaceuticals in Drug Delivery Systems Using Sustainable Strategies. Molecules 2021, 26, 7653. https://doi.org/10.3390/molecules26247653
Costa C, Casimiro T, Corvo ML, Aguiar-Ricardo A. Solid Dosage Forms of Biopharmaceuticals in Drug Delivery Systems Using Sustainable Strategies. Molecules. 2021; 26(24):7653. https://doi.org/10.3390/molecules26247653
Chicago/Turabian StyleCosta, Clarinda, Teresa Casimiro, Maria Luísa Corvo, and Ana Aguiar-Ricardo. 2021. "Solid Dosage Forms of Biopharmaceuticals in Drug Delivery Systems Using Sustainable Strategies" Molecules 26, no. 24: 7653. https://doi.org/10.3390/molecules26247653
APA StyleCosta, C., Casimiro, T., Corvo, M. L., & Aguiar-Ricardo, A. (2021). Solid Dosage Forms of Biopharmaceuticals in Drug Delivery Systems Using Sustainable Strategies. Molecules, 26(24), 7653. https://doi.org/10.3390/molecules26247653








