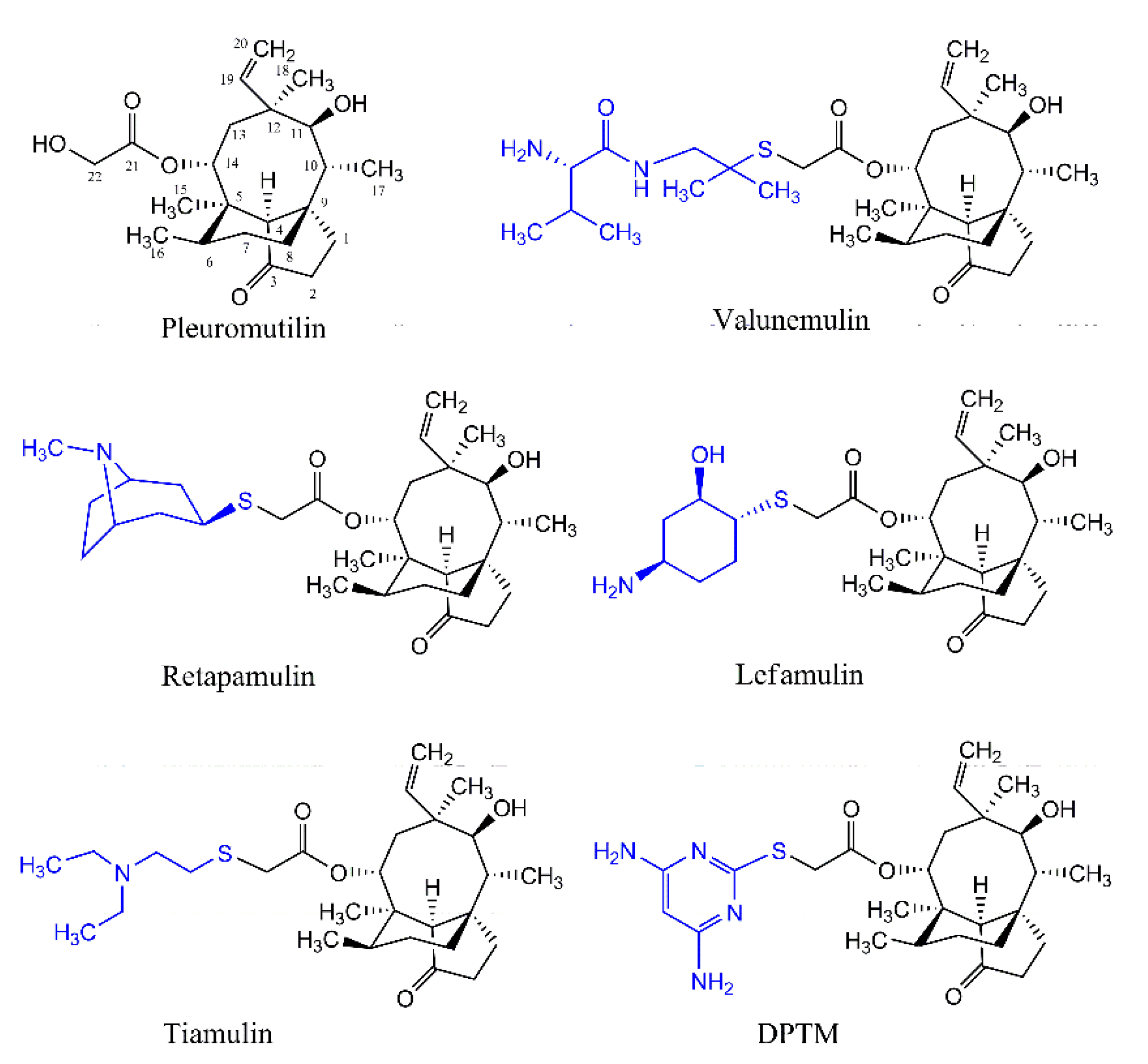
In Vitro and In Vivo Activity of 14-O-[(4,6-Diamino-pyrimidine-2-yl) thioacetyl] Mutilin against Methicillin-Resistant Staphylococcus aureus
Abstract
1. Introduction
2. Results
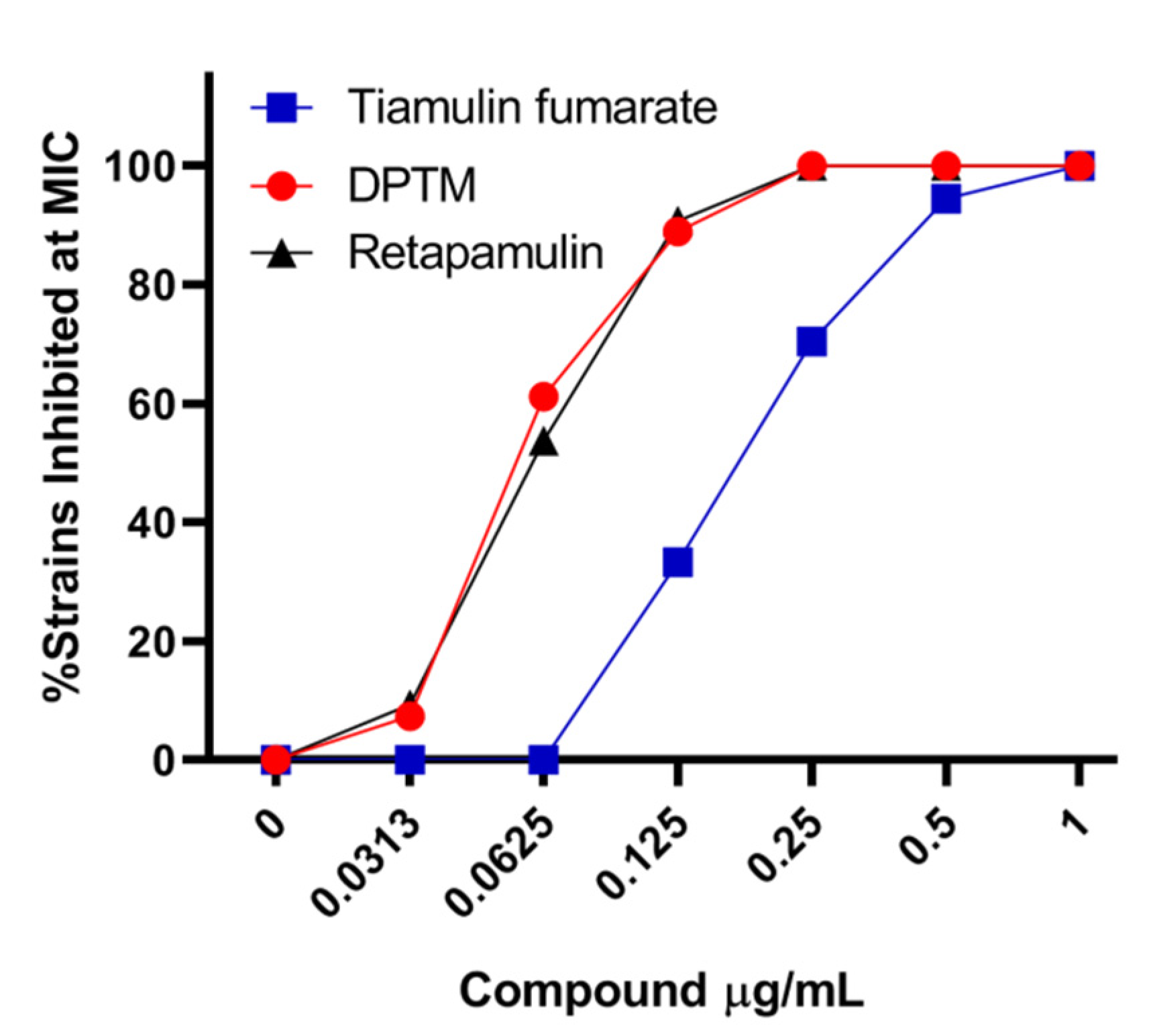
2.1. Effect of DPTM In Vitro
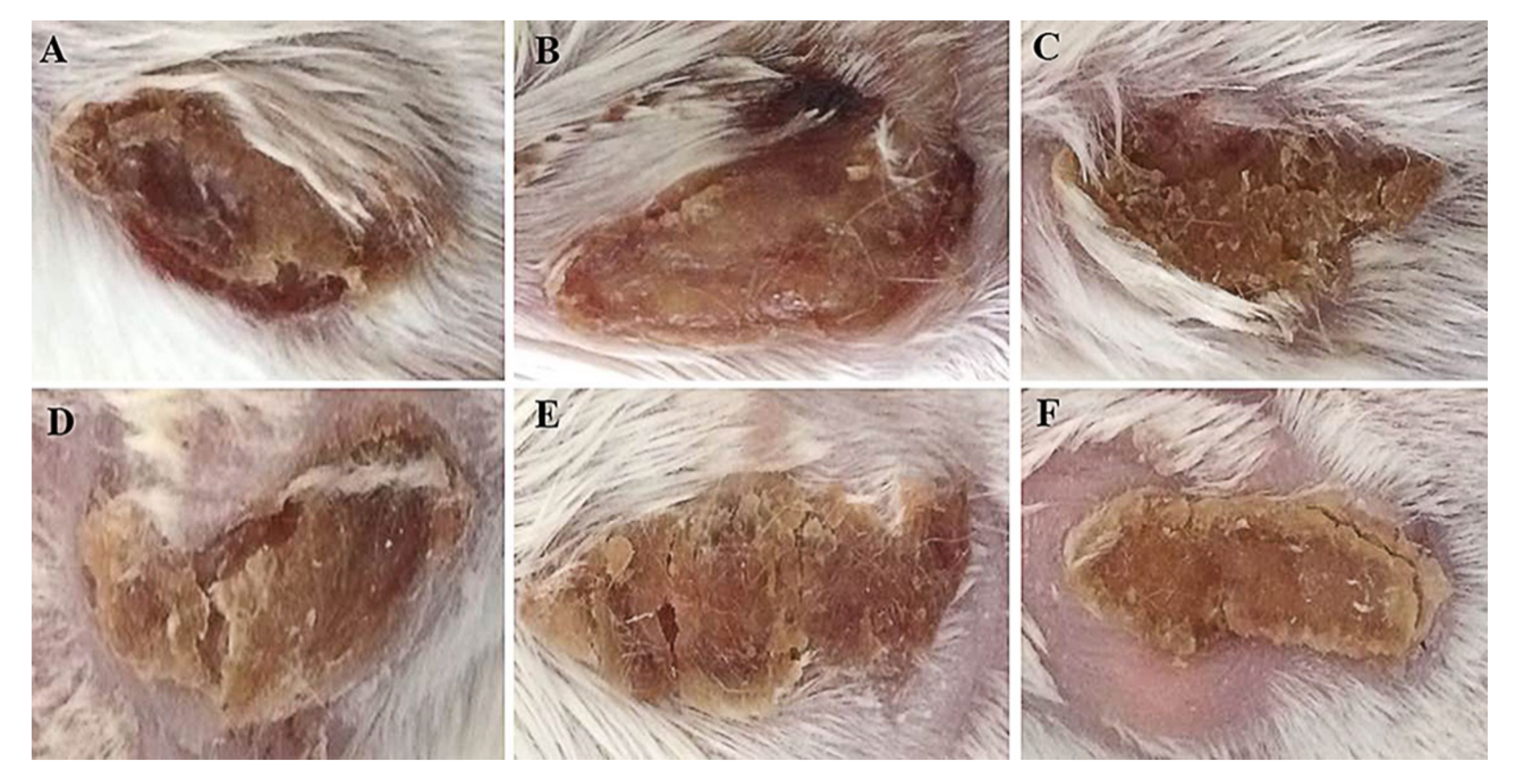
2.2. Macroscopic Evaluation of Efficacy in a Murine Skin Wound Model
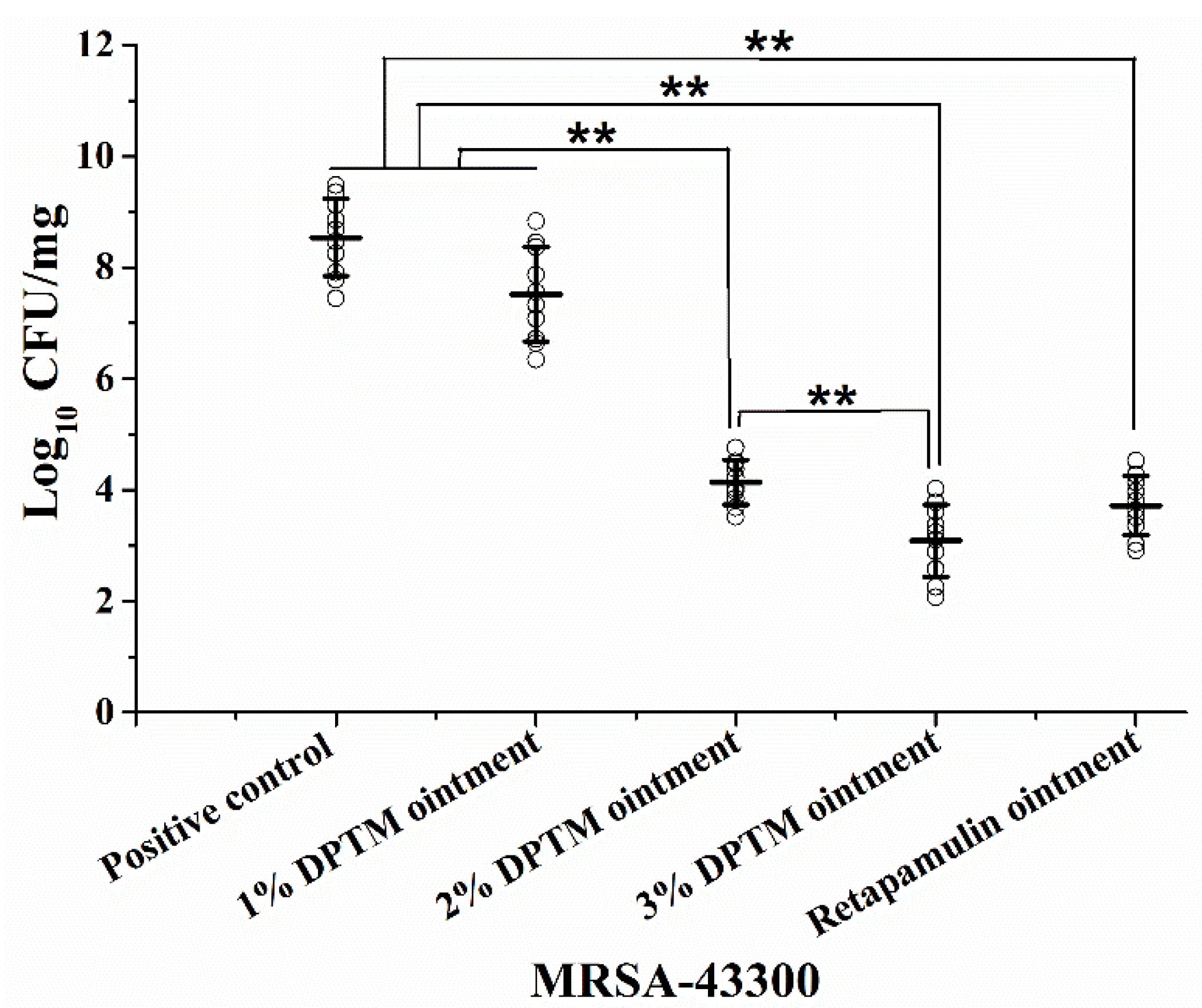
2.3. Bacterial Count in Treated Skin Wound
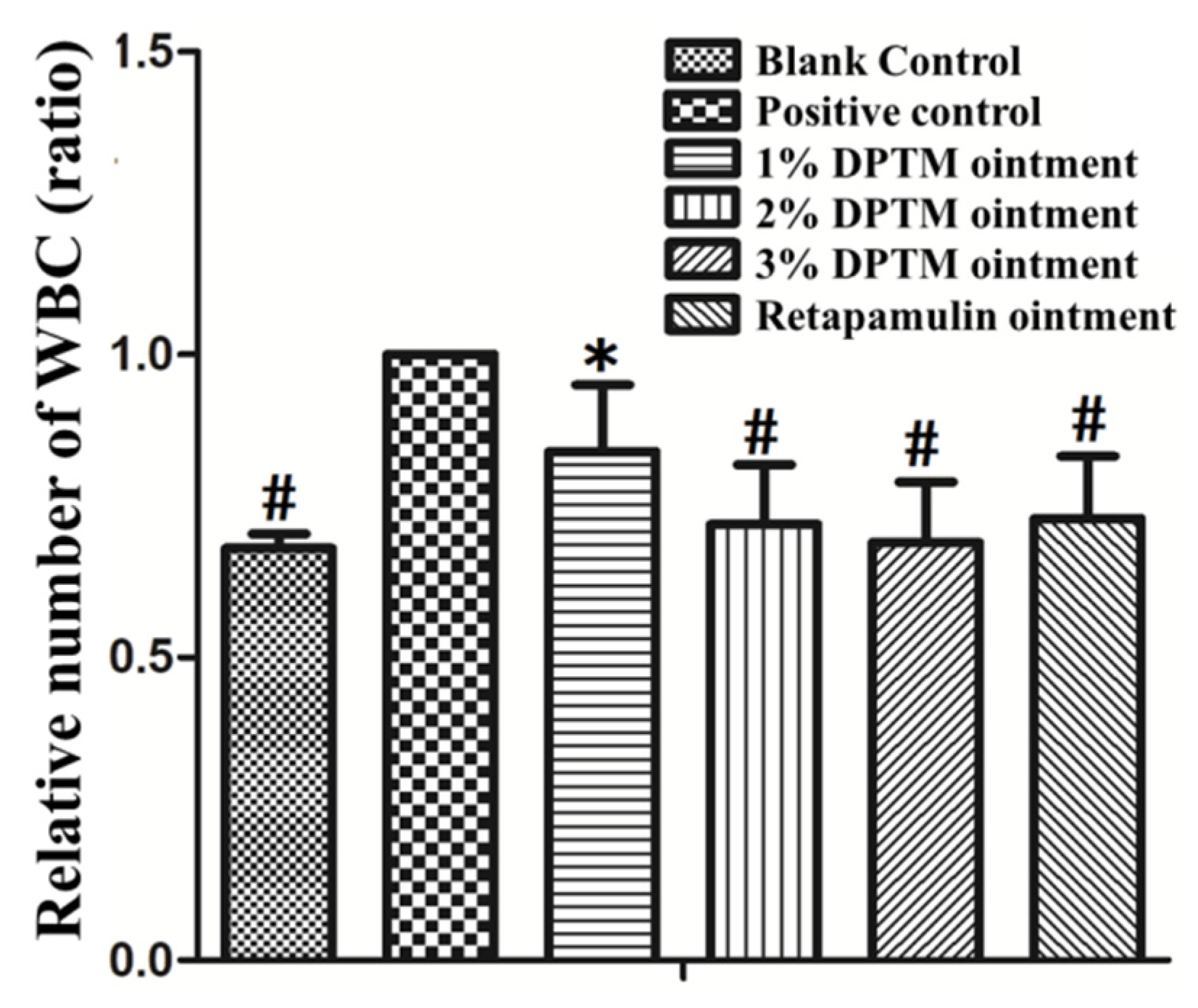
2.4. White Blood Cell (WBC) Level
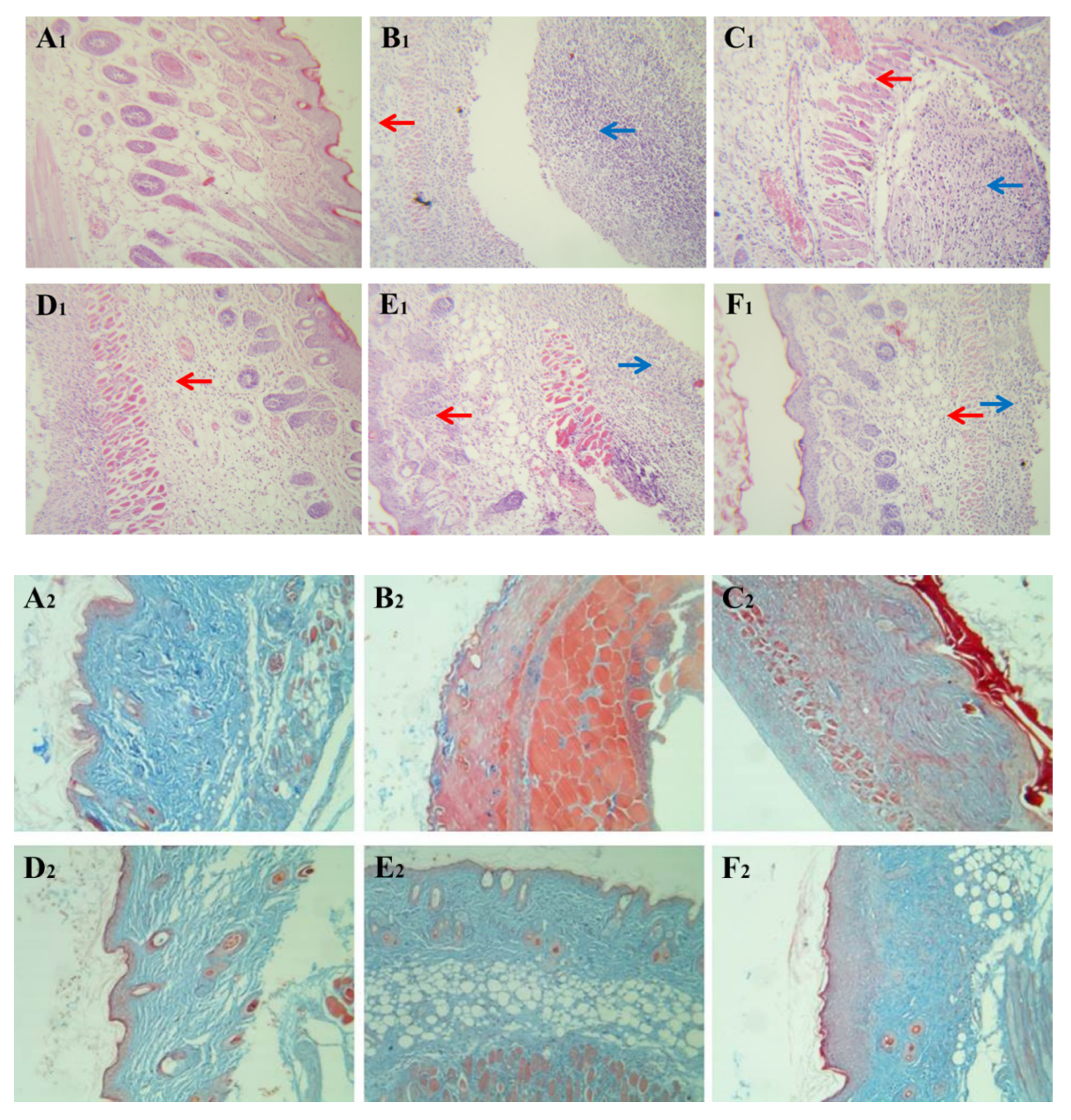
2.5. Histopathological Observation
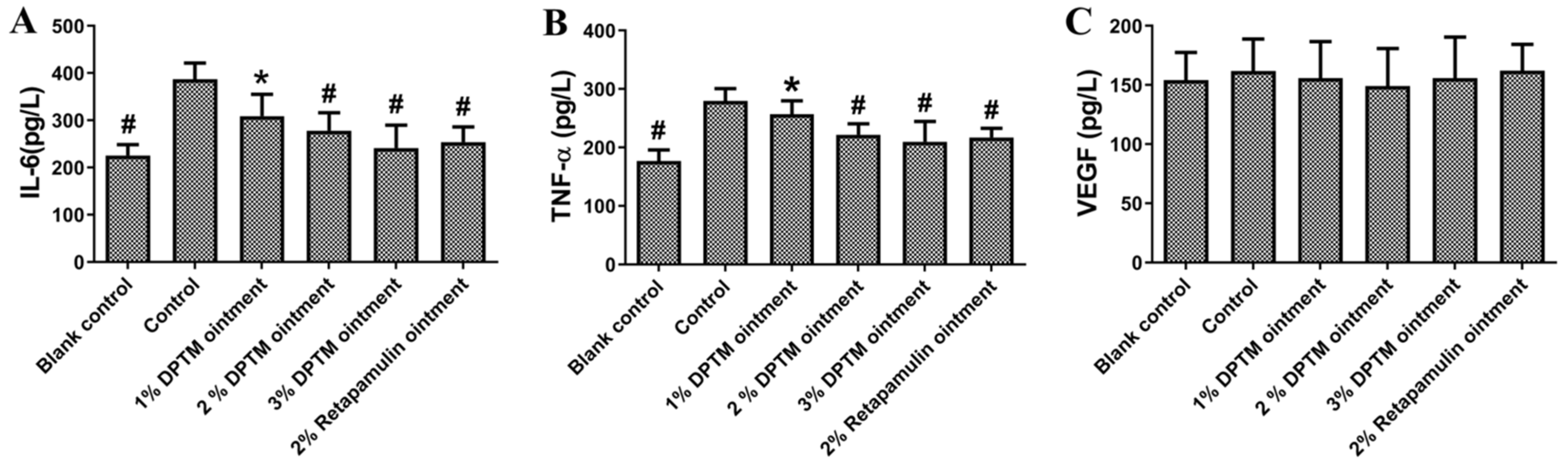
2.6. IL-6, TNF-α, and VEGF Levels
3. Discussion
4. Materials and Methods
4.1. Reagents
4.2. Bacterial Strain
4.3. Animals
4.4. MIC Determination
4.5. Skin Infection Model
4.6. Detection of WBC, IL-6, TNF-α and VEGF in Blood Serum
4.7. Counting the Colonies of MRSA and Histological Examination
4.8. Statistical Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Sample Availability
References
- Wang, C.J.; Ye, C.; Liao, L.L.; Wang, Z.H.; Hu, Y.; Deng, C.; Liu, L. Adjuvant β-lactam therapy combined with vancomycin or daptomycin for methicillin-resistant Staphylococcus aureus bacteraemia: A systematic review and meta-analysis. Antimicrob. Agents Chemoth. 2020, 64, e01377-20. [Google Scholar] [CrossRef]
- Hong, S.I.; Lee, Y.M.; Park, K.H.; Ryu, B.H.; Hong, K.W.; Kim, S.; Bae, I.G.; Cho, O.H. Clinical and molecular characteristics of qacA and qacB-positive methicillin-resistant Staphylococcus aureus causing bloodstream infections. Antimicrob. Agents Chemother. 2019, 63, e02157-18. [Google Scholar] [CrossRef]
- Raz, A.; Serrano, A.; Thaker, M.; Alston, T.; Fischettia, V.A. Lysostaphin lysibody leads to effective opsonization and killing of Methicillin-resistant Staphylococcus aureus in a murine model. Antimicrob. Agents Chemother. 2018, 62, e01056-18. [Google Scholar] [CrossRef] [PubMed]
- Guardabassi, L.; Moodley, A.; Williams, A.; Stegger, M.; Damborg, P.; Halliday-Simmonds, I.; Butaye, P. High prevalence of USA300 among clinical isolates of Methicillin-resistant Staphylococcus aureus on St. Kitts and Nevis, West Indies. Front. Microbiol. 2019, 10, 1123. [Google Scholar] [CrossRef]
- Boucher, H.W.; Corey, G.R. Epidemiology of methicillin-resistant Staphylococcus aureus. Clin. Infect. Dis. 2008, 5, S344–S349. [Google Scholar] [CrossRef] [PubMed]
- Malani, P.N. National burden of invasive methicillin-resistant Staphylococcus aureus infection. JAMA 2014, 311, 1438–1439. [Google Scholar] [CrossRef] [PubMed]
- Gardete, S.; Tomasz, A. Vancomycin resistant Staphylococcus aureus infections: A review of case updating and clinical features. J. Adv. Res. 2020, 21, 169–176. [Google Scholar]
- Gu, B.; Kelesidis, T.; Tsiodras, S.; Hindler, J.; Humphries, R.M. The emerging problem of linezolid-resistant Staphylococcus. J. Antimicrob. Chemother. 2013, 68, 4–11. [Google Scholar] [CrossRef]
- Shariati, A.; Dadashi, M.; Chegini, Z.; Belkum, A.; Mirzaii, M.; Khoramrooz, S.S.; Darban-Sarokhalil, D. The global prevalence of Daptomycin, Tigecycline, Quinupristin/Dalfopristin, and Linezolid-resistant Staphylococcus aureus and coagulase-negative staphylococci strains: A systematic review and meta-analysis. Antimicrob. Resist. In. 2020, 9, 56. [Google Scholar] [CrossRef]
- Kavanagh, F.; Hervey, A.; Robbins, W.J. Antibiotic substances from Basidiomycetes: VIII. Pleurotus multilus (Fr.) Sacc. and Pleurotus passeckerianus Pilat. Proc. Natl. Acad. Sci. USA 1951, 37, 570–574. [Google Scholar] [CrossRef] [PubMed]
- Novak, R.; Shlaes, D.M. The pleuromutilin antibiotics: A new class for human use. Curr. Opin. Invest. Drugs 2010, 11, 182–191. [Google Scholar]
- Schlunzen, F.; Pyetan, E.; Fucini, P.; Yonath, A.; Harms, J.M. Inhibition of peptide bond formation by pleuromutilins: The structure of the 50S ribosomal subunit from Deinococcus radiodurans in complex with tiamulin. Mol. Microbiol. 2004, 54, 1287–1294. [Google Scholar] [CrossRef] [PubMed]
- Davidovich, C.; Bashan, A.; Auerbach-Nevo, T.; Yaggie, R.D.; Gontarek, R.R.; Yonath, A. Induced-fit tightens pleuromutilins, binding to ribosomes and remote interactions enable their selectivity. Proc. Natl. Acad. Sci. USA 2007, 104, 4291–4296. [Google Scholar] [CrossRef]
- Burch, D.G. Tiamulin activity against Brachyspira hyodysenteriae. Vet. Rec. 2008, 163, 760. [Google Scholar]
- Stipkovits, L.; Ripley, P.H.; Tenk, M.; Glavits, R.; Molnar, T.; Fodor, L. The efficacy of valnemulin (Econor) in the control of disease caused by experimental infection of calves with Mycoplasma bovis. Res. Vet. Sci. 2005, 78, 207–215. [Google Scholar] [CrossRef]
- Scangarella-Oman, N.E.; Shawar, R.M.; Bouchillon, S.; Hoban, D. Microbiological profile of a new topical antibacterial: Retapamulin ointment 1%. Expert. Rev. Anti. Infect. Ther. 2009, 7, 269–279. [Google Scholar] [CrossRef] [PubMed]
- Powell, D.; Donato, A. In community-acquired bacterial pneumonia, lefamulin was noninferior to moxifloxacin at 96 h after the first dose. Ann. Intern. Med. 2020, 4, Jc22. [Google Scholar] [CrossRef]
- Yi, Y.; Xu, X.; Liu, Y.; Xu, S.; Huang, X.; Liang, J.; Shang, R. Synthesis and antibacterial activities of novel pleuromutilin derivatives with a substituted pyrimidine moiety. Eur. J. Med. Chem. 2017, 126, 687–695. [Google Scholar] [CrossRef]
- Fu, Y.; Ma, L.; Yi, Y.; Fan, Y.; Liang, J.; Shang, R. A new pleuromutilin candidate with potent antibacterial activity against Pasteurella multocida. Microb. Pathogenesis. 2019, 127, 202–207. [Google Scholar] [CrossRef]
- Killeavy, E.E.; Jogl, G.; Gregory, S.T. Tiamulin-resistant mutants of the thermophilic bacteriumt Thermus thermophiles. Antibiotics 2020, 9, 313. [Google Scholar] [CrossRef]
- Deng, Z.H.; Yin, J.J.; Luo, W.; Kotian, R.N.; Gao, S.S.; Yi, Z.Q.; Xiao, W.F.; Li, W.P.; Li, Y.S. The effect of earthworm extract on promoting skin wound healing. Biosci. Rep. 2018, 38, 20171366. [Google Scholar] [CrossRef] [PubMed]
- Han, H.M.; Ko, S.; Cheong, M.J.; Bang, J.K.; Seo, C.H.; Luchian, T.; Park, Y. Myxinidin 2 and myxinidin 3 suppress inflammatory responses through STAT3 and MAPKs to promote wound healing. Oncotarget 2017, 8, 87582–87597. [Google Scholar] [CrossRef]
- Kaczynska, K.; Kogut, E.; Zajac, D.; Jampolska, M.; Andrzejewski, K.; Sulejczak, D.; Lipkowski, A.W.; Kleczkowska, P. Neurotensin-based hybrid peptide’s anti-inflammatory activity in murine model of a contact sensitivity response. Eur. J. Pharm. Sci. 2016, 93, 84–89. [Google Scholar] [CrossRef]
- Gorwitz, R.J.; Kruszon-Moran, D.; Mcallister, S.K.; Mcquillan, G.; McDougal, L.K.; Fosheim, G.E.; Jensen, B.J.; Killgore, G.; Tenover, F.C.; Kuehnert, M.J. Changes in the prevalence of nasal colonization with Staphylococcus aureus in the United States, 2001. J. Infect. Dis. 2008, 197, 1226–1234. [Google Scholar] [CrossRef] [PubMed]
- Vestergaard, M.; Frees, D.; Ingmer, H. Antibiotic resistance and the MRSA problem. Microbiol. Spectrum 2019, 7, 1–23. [Google Scholar] [CrossRef] [PubMed]
- Angebault, C.; Andremont, A. Antimicrobial agent exposure and the emergence and spread of resistant microorganisms: Issues associated with study design. Eur. J. Clin. Microbiol. Infect. Dis. 2013, 32, 581–595. [Google Scholar] [CrossRef]
- Papastefan, S.T.; Buonpane, C.; Ares, G.; Benyamen, B.; Helenowski, I.; Hunter, C.J. Impact of decolonization protocols and recurrence in pediatric MRSA skin and soft-tissue infections. J. Surg. Res. 2019, 242, 70–77. [Google Scholar] [CrossRef]
- Chen, W.J.; He, C.Y.; Yang, H.; Shu, W.; Cui, Z.L.; Tang, R.; Zhang, C.; Liu, Q. Prevalence and molecular characterization of methicillin-resistant Staphylococcus aureus with mupirocin, fusidic acid and/or retapamulin resistance. BMC. Microbiol. 2020, 20, 183. [Google Scholar] [CrossRef]
- Xia, X.; Li, Z.; Liu, K.; Wu, Y.; Jiang, D.; Lai, Y. Staphylococcal LTA-induced miR-143 inhibits Propionibacterium acnesmediated inflammatory response in skin. J. Invest. Dermatol. 2016, 136, 621–630. [Google Scholar] [CrossRef]
- Li, R.; Wang, J.; Wang, X.; Zhou, J.; Wang, M.; Ma, H.; Xiao, S. Increased betaTrCP are associated with miquimod-induced psoriasis-like skin inflammation in mice via NF-kappaB signaling pathway. Gene 2016, 592, 164–171. [Google Scholar] [CrossRef]
- Pan, C.Y.; Chen, J.Y.; Lin, T.L.; Lin, C.H. In vitro activities of three synthetic peptides derived from epinecidin-1 and an anti-lipopolysaccharide factor against Propionibacterium acnes, Candida albicans, and Trichomonas vaginalis. Peptides 2009, 30, 1058–1068. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.Y.; Seong, I.W.; Kim, J.S.; Cheon, K.A.; Gu, S.H.; Kim, H.H.; Park, K.H. Enhancement of cutaneous immune response to bacterial infection after low-level light therapy with 1072 nm infrared light: A preliminary study. J. Photoch. Photobio. B. 2011, 105, 175–182. [Google Scholar]
- Clinical Laboratory Standards Institute. Methods for Dilution Antimicrobial Susceptibility Tests for Bacteria that Grow Aerobically, approved standard-ninth edition; Clinical and Laboratory Standards Institute: Wayne, PA, USA, 2012. [Google Scholar]
- Boon, R.J.; Beale, A.S. Response of Streptococcus pyogenes to therapy with amoxicillin or amoxicillin-clavulanic acid in a mouse model of mixed infection caused by Staphylococcus aureus and Streptococcus pyogenes. Antimicrob. Agents Chemother. 1987, 31, 1204–1209. [Google Scholar] [CrossRef] [PubMed]
- Kugelberg, E.; Norstrom, T.; Petersen, T.K.; Duvold, T.; Andersson, D.I.; Hughes, D. Establishment of a superficial skin infection model in mice by using Staphylococcus aureus and Streptococcus pyogenes. Antimicrob. Agents Chemother. 2005, 49, 3435–3441. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fu, Y.; Leng, C.; Fan, Y.; Ma, X.; Li, X.; Wang, X.; Guo, Z.; Wang, X.; Shang, R. In Vitro and In Vivo Activity of 14-O-[(4,6-Diamino-pyrimidine-2-yl) thioacetyl] Mutilin against Methicillin-Resistant Staphylococcus aureus. Molecules 2021, 26, 3277. https://doi.org/10.3390/molecules26113277
Fu Y, Leng C, Fan Y, Ma X, Li X, Wang X, Guo Z, Wang X, Shang R. In Vitro and In Vivo Activity of 14-O-[(4,6-Diamino-pyrimidine-2-yl) thioacetyl] Mutilin against Methicillin-Resistant Staphylococcus aureus. Molecules. 2021; 26(11):3277. https://doi.org/10.3390/molecules26113277
Chicago/Turabian StyleFu, Yunxing, Chunqing Leng, Yuan Fan, Xia Ma, Xianghui Li, Xuefei Wang, Zhenghuan Guo, Xiujun Wang, and Ruofeng Shang. 2021. "In Vitro and In Vivo Activity of 14-O-[(4,6-Diamino-pyrimidine-2-yl) thioacetyl] Mutilin against Methicillin-Resistant Staphylococcus aureus" Molecules 26, no. 11: 3277. https://doi.org/10.3390/molecules26113277
APA StyleFu, Y., Leng, C., Fan, Y., Ma, X., Li, X., Wang, X., Guo, Z., Wang, X., & Shang, R. (2021). In Vitro and In Vivo Activity of 14-O-[(4,6-Diamino-pyrimidine-2-yl) thioacetyl] Mutilin against Methicillin-Resistant Staphylococcus aureus. Molecules, 26(11), 3277. https://doi.org/10.3390/molecules26113277




