Potentials of Musa Species Fruits against Oxidative Stress-Induced and Diet-Linked Chronic Diseases: In Vitro and In Vivo Implications of Micronutritional Factors and Dietary Secondary Metabolite Compounds
Abstract
1. Introduction
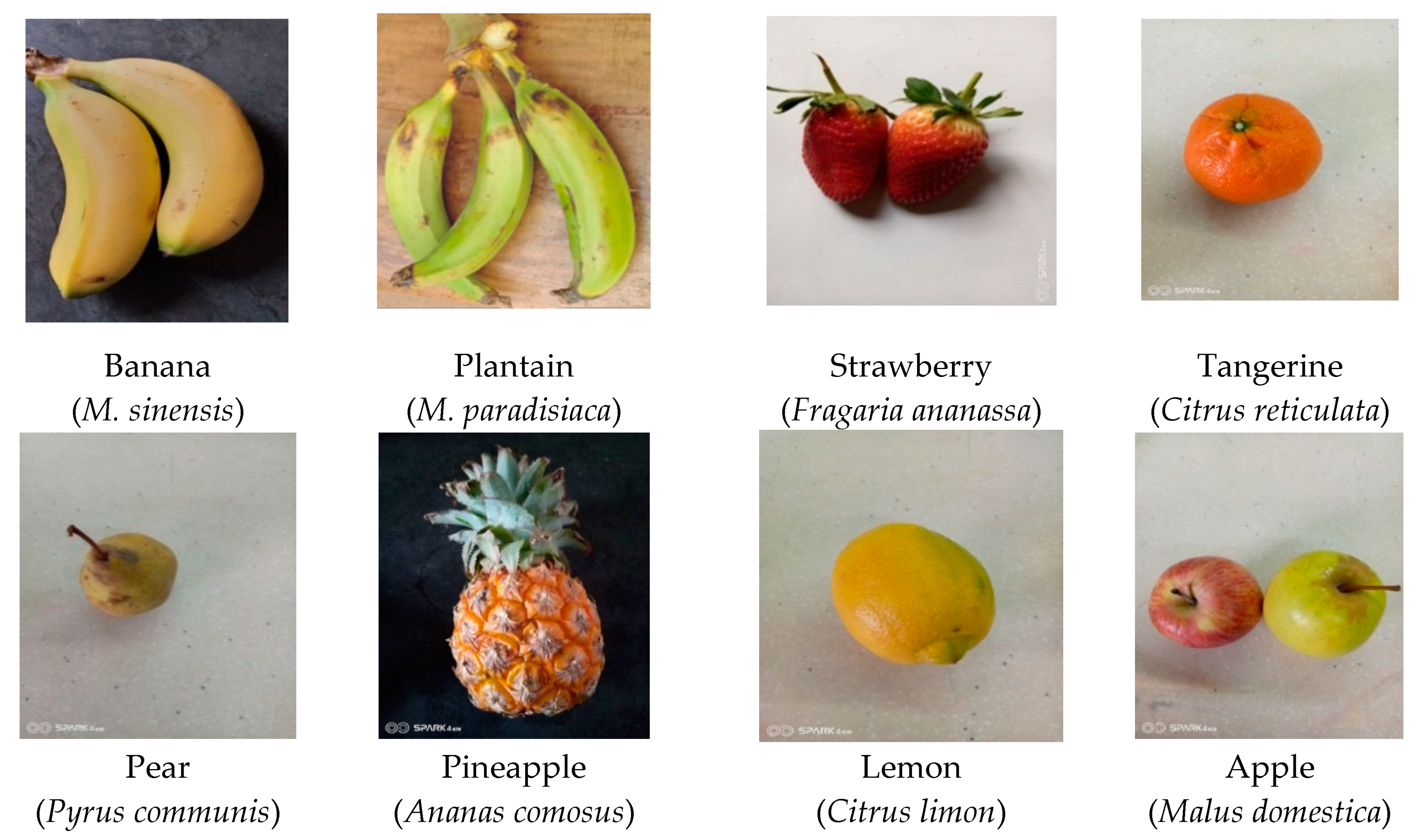
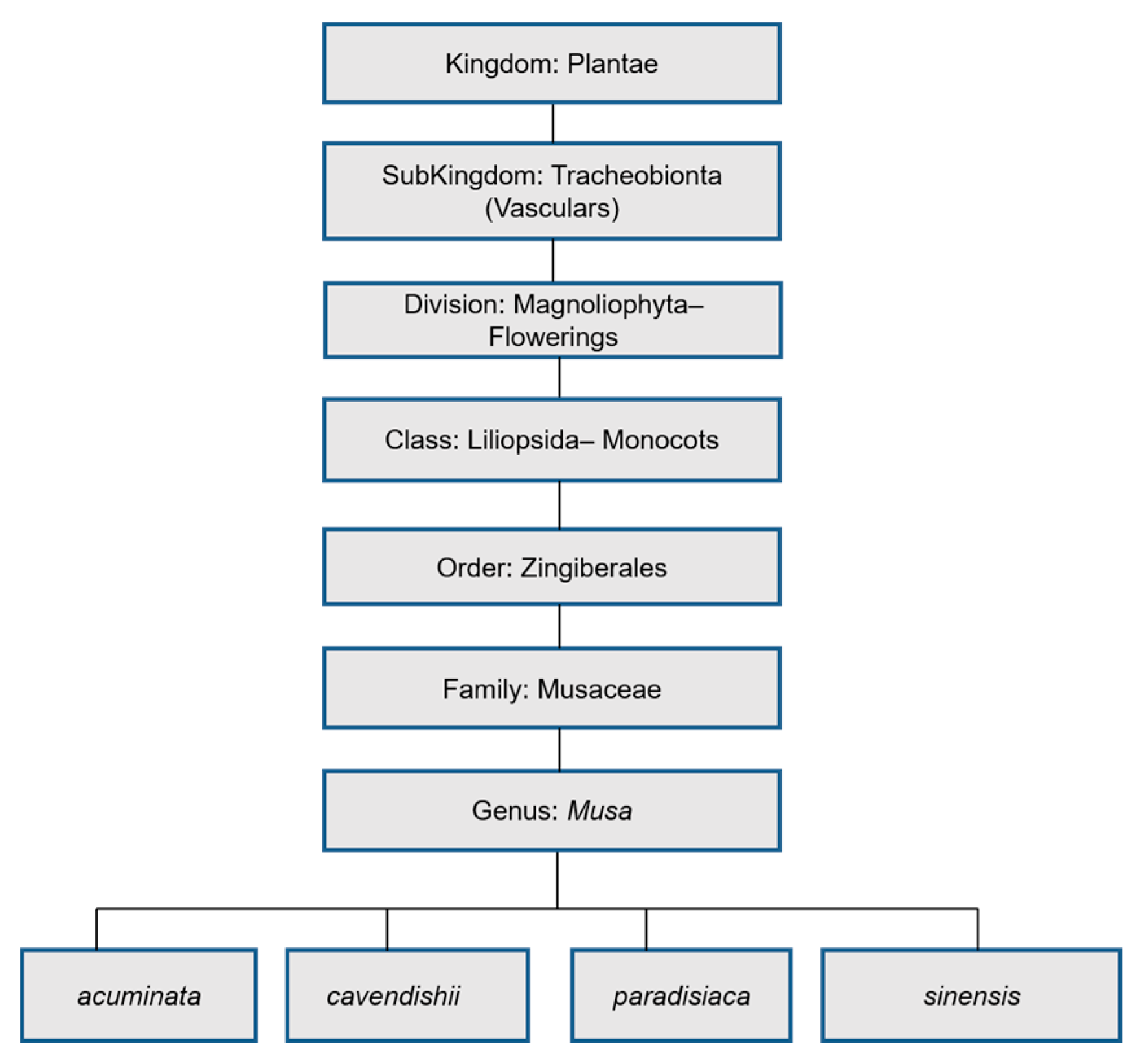
2. Overview of the Musa genus
3. Micronutrients
4. Biomechanismal Implications of Micronutritional Factors of Musa Species Fruits
4.1. Antioxidant Mechanism
4.2. Blood Sugar Balance and Immunity
4.3. Neurological Activity
4.4. Immunological, Neurological, Antioxidant and Anticancer Mechanism
4.5. Antioxidant Mechanism
4.6. Blood Sugar Balance and Antioxidant Activity
4.7. Immunological and Anti-Inflammatory Mechanism
4.8. Immunological, Antioxidant and Neurological Mechanism
5. Biological Mechanism and Pharmacological Activity of Dietary Phytocompounds of Musa Species Fruits
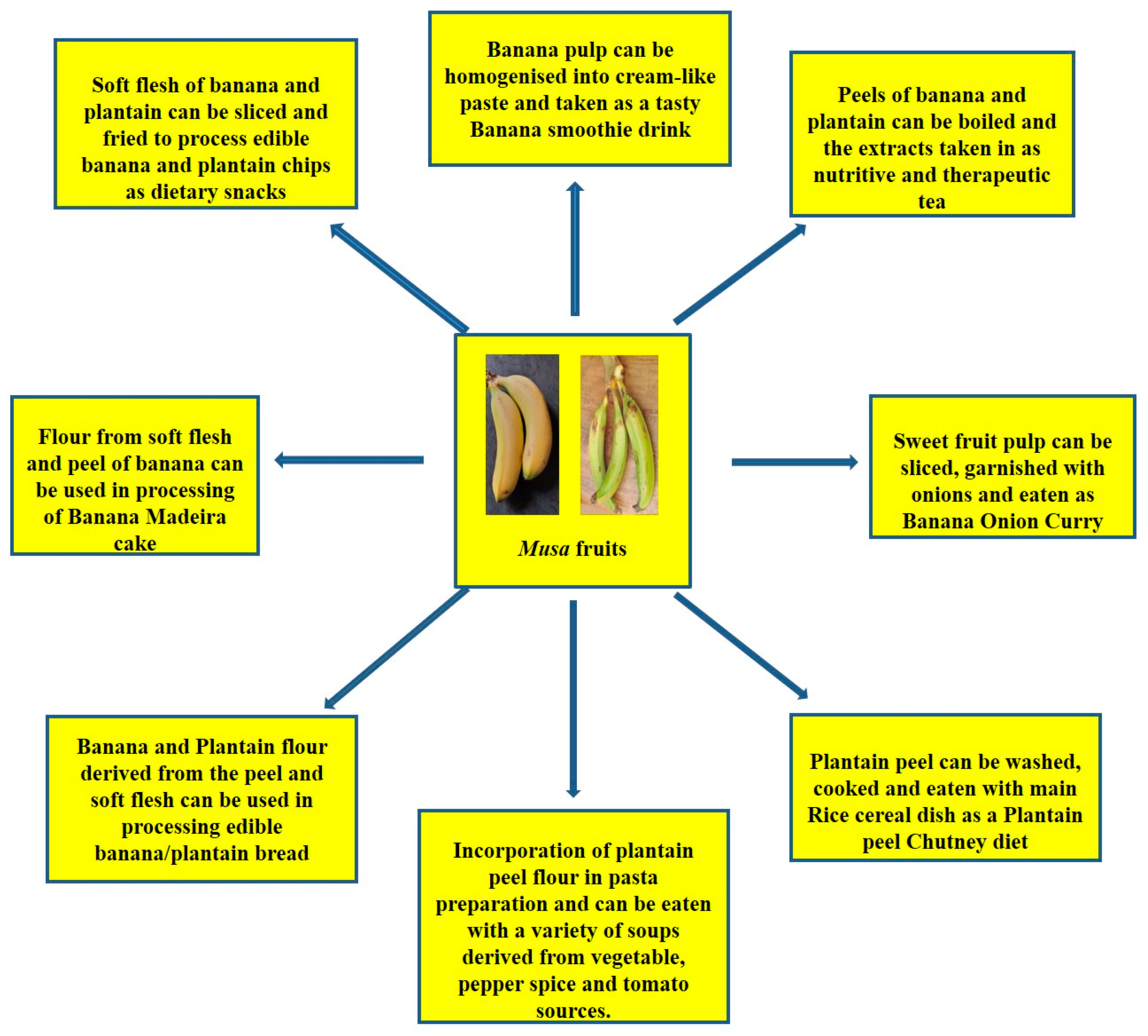
6. Dietary Incorporation of Banana and Plantain (Musa spp.)
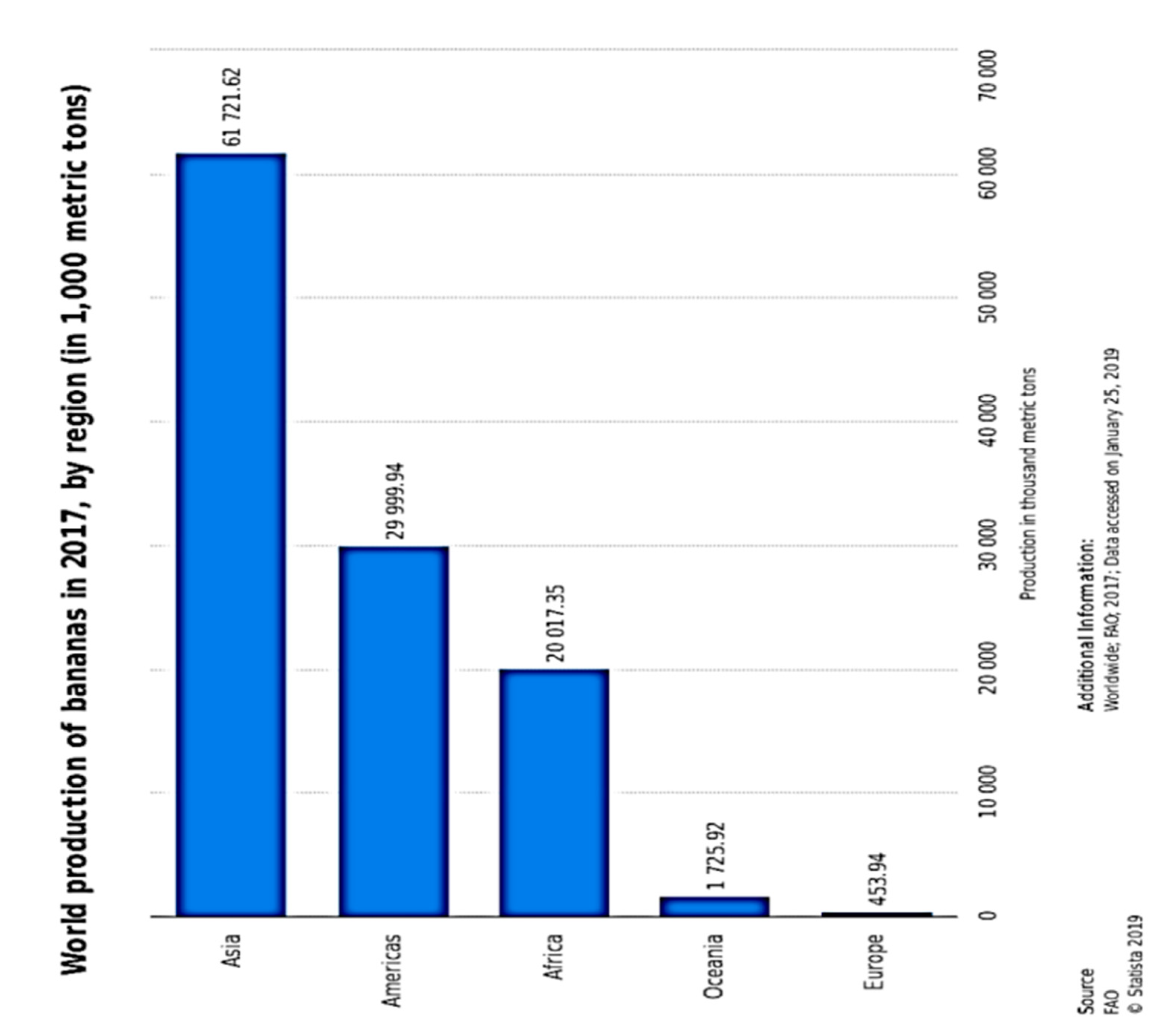
7. Production and Consumption Status of Bananas (Musa spp.)
| Rank | Country | Production (Tonnes) |
|---|---|---|
| 1st | Cameroon | 4.31 million |
| 2nd | Ghana | 3.95 million |
| 3rd | Uganda | 3.71 million |
| 4th | Colombia | 3.54 million |
| 5th | Nigeria | 3.09 million |
| 6th | Philippines | 3.07 million |
| 7th | Peru | 2.07 million |
| 8th | Ivory Coast | 1.59 million |
| 9th | Myanmar | 1.11 million |
| 10th | Democratic Republic of Congo | 1.11 million |
8. Conclusions and Perspectives
Author Contributions
Funding
Conflicts of Interest
References
- Batra, J.; Seth, P.K. Effect of iron deficiency on developing rat brain. Indian J. Clin. Biochem. 2002, 17, 108–114. [Google Scholar] [CrossRef] [PubMed]
- Tulchisky, T.H. Micronutrient Deficiency Conditions: Global Health Issues. Public Health Rev. 2010, 32, 243–255. [Google Scholar] [CrossRef]
- Rush, D. Nutrition and maternal mortality in the developing world. Am. J. Clin. Nutr. 2000, 1, 212–240. [Google Scholar] [CrossRef]
- Viteri, F.E.; Gonzalez, H. Adverse outcomes of poor micronutrient status in childhood and adolescence. Nutr. Rev. 2002, 60, 77–83. [Google Scholar] [CrossRef] [PubMed]
- Groce, N.; Challenger, E.; Berman-Bieler, R.; Farkas, A.; Yilmaz, N.; Schultink, W.; Clark, D.; Kerac, M. Malnutrition and disability: Unexplored opportunities for collaboration. Paediatr. Int. Child. Health 2014, 34, 308–314. [Google Scholar] [CrossRef]
- Bailey, L.B.; Stover, P.J.; McNulty, H.; Fenech, M.F.; Gregory 3rd, J.F.; Mills, J.L.; Pfeiffer, C.M.; Fazili, Z.; Zhang, M.; Ueland, P.M. Biomarkers of Nutrition for Development- Folate Review. J. Nutr. 2015, 145, 1636–1680. [Google Scholar] [CrossRef]
- Katona, P.; Katona-Apte, J. The interaction between nutrition and infection. Clin. Infect. Dis. 2008, 46, 1582–1588. [Google Scholar] [CrossRef]
- Darmon, N.; Ferguson, E.L.; Briend, A. A cost constraint alone has adverse effects on food selection and nutrient density: An analysis of human diets by linear programming. J. Nutr. 2002, 132, 3764–3771. [Google Scholar] [CrossRef]
- Chatterjee, M.; Roy, K.; Janarthan, M.; Das, S.; Chatterjee, M. Biological activity of carotenoids: Its implications in cancer risk and prevention. Curr. Pharm. Biotechnol. 2012, 13, 180–190. [Google Scholar] [CrossRef]
- Reuben, S.C.; Gopalan, A.; Petit, D.M.; Bishayee, A. Modulation of angiogenesis by dietary phytoconstituents in the prevention and intervention of breast cancer. Mol. Nutr. Food Res. 2012, 56, 14–29. [Google Scholar] [CrossRef]
- Nechuta, S.; Lu, W.; Zheng, Y.; Cai, H.; Bao, P.; Gu, K.; Zheng, W.; Shu, X.O. Comorbidities and breast cancer survival: A report from the Shanghai breast cancer survival study. Breast Cancer Res. Treat. 2013, 139, 227–235. [Google Scholar] [CrossRef] [PubMed]
- Fink, B.N.; Steck, S.E.; Wolff, M.S.; Britton, J.A.; Kabat, G.C.; Schroeder, J.C.; Teitelbaum, S.L.; Neugut, A.I.; Gammon, M.D. Dietary flavonoid intake and breast cancer risk among women on Long Island. Am. J. Epidemiol. 2007, 165, 514–523. [Google Scholar] [CrossRef] [PubMed]
- Cutler, G.J.; Nettleton, J.A.; Ross, J.A.; Harnack, L.S.; Jacobs, D.R., Jr.; Scrafford, C.G.; Barraj, L.M.; Mink, P.J.; Robien, K. Dietary flavonoid intake and risk of cancer in post-menopausal women: The Iowa Women’s Health Study. Int. J. Cancer 2008, 123, 664–671. [Google Scholar] [CrossRef] [PubMed]
- Kresty, L.A.; Morse, M.A.; Morgan, C.; Carlton, P.S.; Lu, J.; Gupta, A.; Blackwood, M.; Stoner, G.D. Chemoprevention of esophageal tumorigenesis by dietary administration of lyophilized black raspberries. Cancer Res. 2001, 61, 6112–6119. [Google Scholar] [PubMed]
- Hagiwara, A.; Miyashita, K.; Nakanishi, T.; Sano, M.; Tamano, S.; Kadota, T.; Koda, T.; Nakamura, M.; Imaida, K.; Ito, N.; et al. Pronounced inhibition by a natural anthocyanin, purple corn color, of 2-amino-1-methyl-6-phenylimidazo [4,5-b] pyridine (PhIP)-associated colorectal carcinogenesis in male F344 rats pretreated with 1, 2-dimethylhydrazine. Cancer Lett. 2001, 171, 17–25. [Google Scholar] [CrossRef]
- Schaefer, S.; Baum, M.; Eisenbrand, G.; Janzowski, C. Modulation of oxidative cell damage by reconstituted mixtures of phenolic apple juice extracts in human colon cell lines. Mol. Nutr. Food Res. 2006, 50, 413–417. [Google Scholar] [CrossRef]
- Rolls, B.J.; Ello-Martin, J.A.; Tohill, B.C. What can intervention studies tell us about the relationship between fruit and vegetable consumption and weight management? Nutr. Rev. 2004, 62, 1–17. [Google Scholar] [CrossRef]
- Tohill, B.C.; Seymour, J.; Serdula, M.; Kettel-Khan, L.; Rolls, B.J. What Epidemiologic Studies Tell Us about the Relationship between Fruit and Vegetable Consumption and Body Weight? Nutr. Rev. 2004, 62, 365–374. [Google Scholar] [CrossRef]
- Rautiainen, S.; Wang, L.; Lee, I.; Manson, J.E.; Buring, J.E.; Sesso, H.D. Higher intake of fruit, but not vegetables or fiber, at baseline is associated with lower risk of becoming overweight or obese in middle-aged and older women of normal BMI at baseline1-3. J. Nutr. 2015, 145, 960–968. [Google Scholar] [CrossRef]
- Lock, K.; Pomerleau, J.; Causer, L.; Altmann, D.R.; McKee, M. The global burden of disease attributable to low consumption of fruit and vegetables: Implications for the global strategy on diet. Bull. World Health Organ. 2005, 83, 100–108. [Google Scholar]
- Boeing, H.; Bechthold, A.; Bub, A.; Ellinger, S.; Haller, D.; Kroke, A.; Leschik-Bonnet, E.; Muller, M.J.; Oberritter, H.; Schulze, M.; et al. Critical review: Vegetables and fruit in the prevention of chronic diseases. Eur. J. Nutr. 2012, 51, 637–663. [Google Scholar] [CrossRef] [PubMed]
- Yu, N.; Su, X.; Wang, Z.; Dai, B.; Kang, J. Association of Dietary Vitamin A and β-carotene intake with the risk of lung cancer: A meta-analysis of 19 Publications. Nutrients 2015, 7, 9309–9932. [Google Scholar] [CrossRef] [PubMed]
- Du, H.; Li, L.; Bennett, D.; Guo, Y.; Key, T.J.; Bian, Z.; Sherliker, P.; Gao, H.; Chen, Y.; Yang, L.; et al. Fresh fruit consumption and major cardiovascular disease in China. N. Engl. J. Med. 2016, 374, 1332–1343. [Google Scholar] [CrossRef] [PubMed]
- Zhai, H.; Wang, Y.; Jiang, W. Fruit and vegetable intake and the risk of chronic obstructive pulmonary disease: A dose-response meta-analysis of observational studies. Biomed Res. Int. 2020, 2020, 1–12. [Google Scholar] [CrossRef]
- Constantine, D.; Rossel, G. The Musaceae: An annotated list of the species of Ensete, Musa and Musella, 2001. Available online: http://http://www.users.globalnet.co.uk/~drc/musa_home.htm (accessed on 11 August 2020).
- Boning, C.R. Florida’s Best Fruiting Plants, 1st ed.; Pineapple Press Inc.: Sarasota, FL, USA, 2006; pp. 1–232. [Google Scholar]
- Perriera, X.; De Langheb, E.; Donohuec, M.; Lentferd, C.; Vrydaghse, L.; Bakrya, F.; Carreel, F.; Hippolyte, I.; Horry, J.-P.; Jenny, C.; et al. Multidisciplinary perspectives on banana (Musa spp.) domestication. Proc. Natl. Acad. Sci. USA 2011, 108, 11311–11318. [Google Scholar] [CrossRef]
- Sampath Kumar, K.P.; Bhowmik, D.; Duraivel, S.; Umadevi, M. Traditional and Medicinal Uses of Banana. J. Pharm. Phytochem. 2012, 1, 51–63. [Google Scholar]
- Khawas, P.; Deka, S.C. Comparative nutritional, functional, morphological and diffractogram study on culinary banana (Musa ABB) peel at various stages of development. Int. J. Food Prop. 2016, 19, 2832–2853. [Google Scholar] [CrossRef]
- Hill, A. Plantains vs. Bananas: What’s the Difference? 2018. Available online: http://www.healthline.com/nutrition/plantain-vs-banana (accessed on 11 August 2020).
- Sulaiman, S.F.; Yusoff, N.A.M.; Eldeen, I.M.; Seow, E.M.; Sajak, A.A.B.; Supriatno, K.L.O. Correlation total phenolic and mineral contents with antioxidant activity of eight malaysian bananas (Musa sp.). J. Food Compos. Anal. 2011, 24, 1–10. [Google Scholar] [CrossRef]
- Aurore, G.; Parfait, B.; Fahrasmane, L. Bananas, raw materials for making processed food products. Trends Food Sci. Technol. 2009, 20, 78–91. [Google Scholar] [CrossRef]
- Bennett, R.N.; Shiga, T.M.; Hassimotto, N.M.; Rosa, E.A.; Lajolo, F.M.; Cordenunsi, B.R. Phenolics and antioxidant properties of fruit pulp and cell wall fractions of post-harvest banana (Musa acuminata Juss.) cultivars. J. Agric. Food Chem. 2010, 58, 7991–8003. [Google Scholar] [CrossRef]
- Menezes, E.W.; Tadini, C.C.; Tribess, T.B.; Zuleta, A.; Binaghi, J.; Pak, N.; Vera, G.; Dan, M.C.T.; Bertolini, A.C.; Cordenunsi, B.R.; et al. Chemical composition and nutritional value of unripe banana flour (Musa acuminata var. Nanicão). Plant Foods Hum. Nutr. 2011, 66, 231–237. [Google Scholar] [CrossRef] [PubMed]
- Sarawong, C.; Schoenlechner, R.; Sekiguchi, K.; Berghofer, E.; Ng, P.K.W. Effect of extrusion cooking on the physicochemical properties, resistant starch, phenolic content and antioxidant capacities of green banana flour. Food Chem. 2014, 143, 33–39. [Google Scholar] [CrossRef] [PubMed]
- Faller, A.L.K.; Fialho, E. Polyphenol content and antioxidant capacity in organic and conventional plant foods. J. Food Compos. Anal. 2010, 23, 561–568. [Google Scholar] [CrossRef]
- Fu, L.; Xu, B.T.; Xu, X.R.; Gan, R.Y.; Zhang, Y.; Xia, E.Q.; Li, H.B. Antioxidant capacities and total phenolic contents of 62 fruits. Food Chem. 2011, 129, 345–350. [Google Scholar] [CrossRef] [PubMed]
- Aina, D.A.; Jonathan, S.G.; Olawuyi, O.J.; Ojelabi, D.O.; Durowoju, B.M. Antioxidant, antimicrobial and phytochemical properties of alcoholic extracts of Cantharellus cibarius: A Nigerian mushroom. N. Y. Sci. J. 2012, 5, 114–120. [Google Scholar]
- Oyeyinka, B.O.; Afolayan, A.J. Comparative evaluation of the nutritive, mineral and antinutritive compositions of Musa sinensis L. (Banana) and Musa paradisiaca L. (Plantain) fruit compartments. Plants 2019, 8, 598. [Google Scholar] [CrossRef]
- Feumba, D.R.; Ashwini, R.P.; Ragu, S.M. Chemical composition of some selected fruit peels. Eur. J. Food Sci. Technol. 2016, 4, 12–21. [Google Scholar]
- Mahon, B.D.; Gordon, S.A.; Cruz, J.; Cosman, F.; Cantorna, M.T. Cytokine profile in patients with multiple Sclerosis following Vitamin D supplementation. J. Neuroimmunol. 2003, 134, 128–132. [Google Scholar] [CrossRef]
- Schleithoff, S.S.; Zittermann, A.; Tenderich, G.; Berthold, H.K.; Stehle, P.; Koerfer, R. Vitamin D supplementation improves cytokine profiles in patients with congestive heart failure: A double-blind, randomized, placebo-controlled trial. Am. J. Clin. Nutr. 2006, 83, 754–759. [Google Scholar] [CrossRef]
- Adegbaju, O.D.; Otunola, G.A.; Afolayan, A.J. Potential of Celosia species in alleviating micronutrient deficiencies and prevention of diet-related chronic diseases: A review. Aims Agric. Food 2019, 4, 458–484. [Google Scholar] [CrossRef]
- Christian, P.; Stewart, C.P. Maternal micronutrient deficiency, fetal development and the risk of chronic disease. J. Nutr. 2010, 140, 437–445. [Google Scholar] [CrossRef] [PubMed]
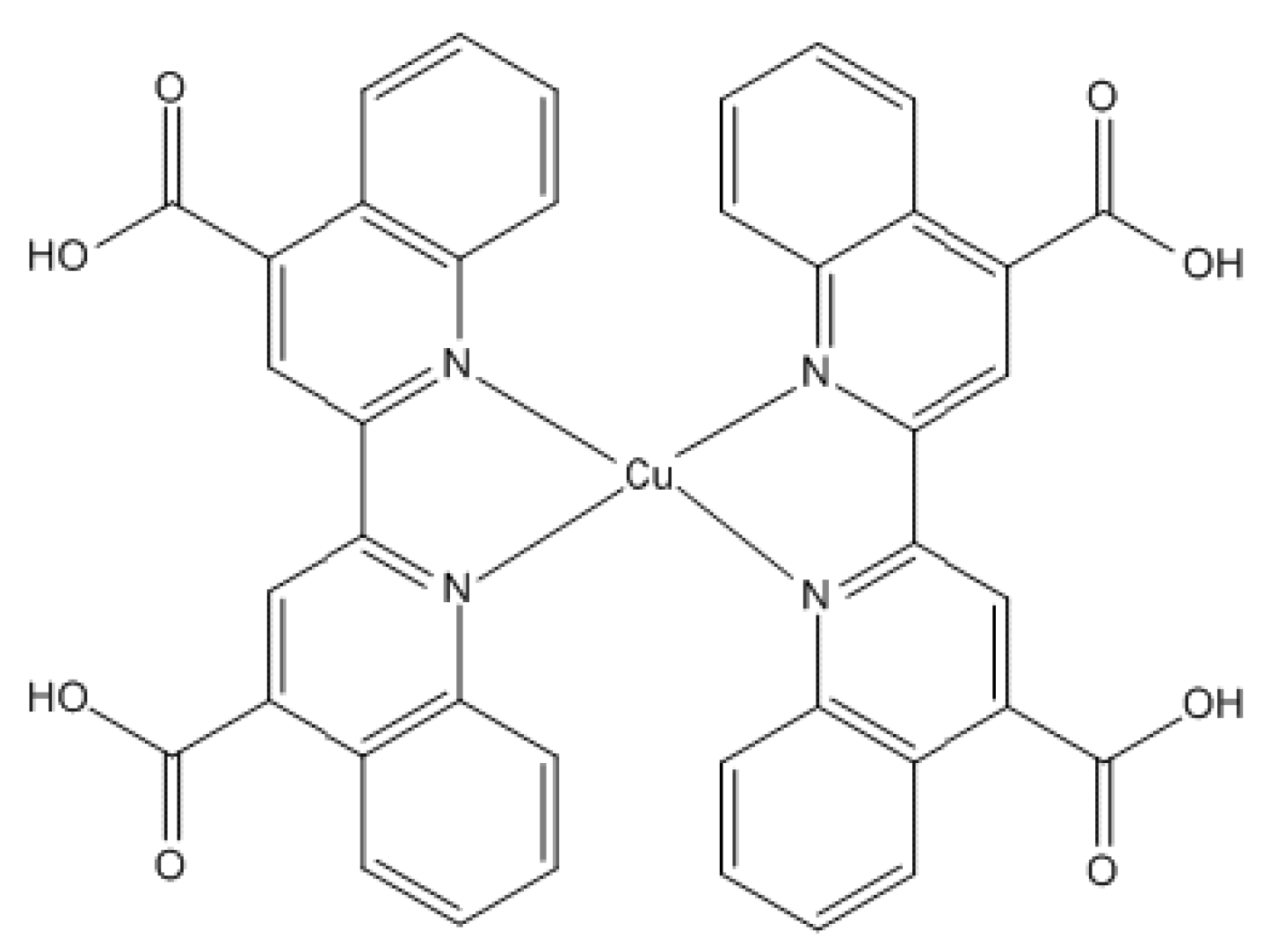
- Jomova, K.; Valko, M. Advances in metal-induced oxidative stress and human disease. Toxicology 2011, 283, 65–87. [Google Scholar] [CrossRef] [PubMed]
- Adeyemi, O.S.; Oladiji, A.T. Compositional changes in banana (Musa ssp.) fruits during ripening. Afr. J. Biotechnol. 2009, 8, 858–859. [Google Scholar]
- Selema, M.D.; Farago, M.E. Trace element concentrations in the fruit peels and trunks of Musa paradisiaca. Phytochemistry 1996, 42, 1523–1525. [Google Scholar] [CrossRef]
- Davey, M.W.; Van den Bergh, I.; Markham, R.; Swennen, R.; Keulemans, J. Genetic variability in Musa fruit provitamin A carotenoids, lutein and mineral micronutrient contents. Food Chem. 2009, 115, 806–813. [Google Scholar] [CrossRef]
- Offem, J.O.; Njoku, P.C. Mineral distribution in the fruits of the plantain plant (Musa paradisiaca) in relation to mode and degree of maturation. Food Chem. 1993, 48, 63–68. [Google Scholar] [CrossRef]
- Anderson, D.L.; Cunningham, W.C.; Lindstrom, T.R. Concentrations and intakes of H, B, S, K, Na, Cl and NaCl in foods. J. Food Comp. Anal. 1994, 7, 59–82. [Google Scholar] [CrossRef]
- Emaga, T.H.; Ronkart, S.N.; Robert, C.; Wathelet, B.; Paquot, M. Characterization of pectins extracted from banana peels (Musa AAA) under different conditions using an experimental design. Food Chem. 2008, 108, 463–471. [Google Scholar] [CrossRef]
- Stefanidou, M.; Maravelias, C.; Dona, A.; Spiliopoulou, C. Zinc: A multipurpose trace element. Arch. Toxicol. 2006, 80, 1–9. [Google Scholar] [CrossRef]
- Chasapis, C.T.; Loutsidou, A.C.; Spiliopoulou, C.A.; Stefanidou, M.E. Zinc and Human Health: An Update. Arch. Toxicol. 2012, 86, 521–534. [Google Scholar] [CrossRef]
- Olechnowicz, J.; Tinkov, A.; Skalny, A.; Suliburska, J. Zinc status is associated with inflammation, oxidative stress, lipid and glucose metabolism. J. Physiol. Sci. 2018, 68, 19–31. [Google Scholar] [CrossRef] [PubMed]
- Jarosz, M.; Szkaradek, N.; Marona, H.; Nowak, G.; Młyniec, K.; Librowsk, T. Evaluation of anti-inflammatory and ulcerogenic potentialof zinc-ibuprofen and zinc-naproxen complexes in rats. Inflammopharmacology 2017, 25, 653–663. [Google Scholar] [CrossRef] [PubMed]
- Prasad, S.N. Mitigation of acrylamide-induced behavioral deficits, oxidative impairments and neurotoxicity by oral supplements of geraniol (a monoterpene) in a rat mode. Chem. Biol. Interact. 2014, 223, 27–37. [Google Scholar] [CrossRef] [PubMed]
- Cortese, S.; Angriman, M.; Maffeis, C.; Isnard, P.; Konofal, E.; Lecendreux, M.; Purper-Ouakil, D.; Vincenzi, B.; Bernardina, B.D.; Mouren, M.C. Attention-Deficit/Hyperactivity disorder (ADHD) and Obesity: A Systematic Review of the Literature. Crit. Rev. Food Sci. Nutr. 2008, 48, 524–537. [Google Scholar] [CrossRef] [PubMed]
- Huang, L. Early-life stress impacts the developing hippocampus and primes seizure occurrence: Cellular, molecular, and epigenetic mechanisms. Mol. Neurosci. 2014, 7, 1–15. [Google Scholar] [CrossRef]
- Csermely, P.; Somogyi, J. Zinc as a Possible Mediator of Signal Transduction in T-Lymphocytes. Acta Physiol. Hung. 1989, 74, 195–199. [Google Scholar]
- Haase, H.; Rink, L. Functional Significance of Zinc-Related Signaling Pathways in immune cells. Annu. Rev. Nutr. 2009, 29, 133–152. [Google Scholar] [CrossRef]
- Fraker, P.J.; Gershwin, M.E.; Good, R.A.; Prasad, A. Interrelationships between zinc and immune function. Fed. Proc. 1986, 45, 1474–1479. [Google Scholar]
- Hojyo, S.; Fukada, T. Zinc transporters and signaling in physiology and pathogenesis. Arch. Biochem. Biophys. 2016, 611, 43–50. [Google Scholar] [CrossRef]
- Mott, D.D.; Dingledine, R. Unraveling the role of zinc in memory. Proc. Natl. Acad. Sci. USA 2011, 108, 3103–3104. [Google Scholar] [CrossRef]
- Besser, L.; Chorin, E.; Sekler, I.; Silverman, W.F.; Atkin, S.; Russell, J.T.; Hershfinker, M. Synaptically released zinc triggers metabotropic signaling via a zinc-sensing receptor in the Hippocampus. J. Neurosci. 2009, 29, 2890–2901. [Google Scholar] [CrossRef]
- Sindreu, C.; Palmiter, R.; Storm, D. Zinc transporter ZnT-3 regulates presynaptic Erk1/2 signaling and hippocampus-dependent memory. Proc. Natl. Acad. Sci. USA 2011, 108, 3366–3370. [Google Scholar] [CrossRef] [PubMed]
- Penland, J.G. The importance of Boron nutrition for brain and psychological functions. Biol. Trace Elem. Res. 1998, 66, 299–317. [Google Scholar] [CrossRef] [PubMed]
- Coban, F.K.; Liman, R.; Cigerci, I.H.; Ince, S.; Hazman, O.; Bozkurt, M.F. The antioxidant effect of boron on oxidative stress and DNA damage in diabetic rats. Fresen. Environ. Bull. 2015, 24, 4059–4066. [Google Scholar]
- Cao, J.; Jiang, L.; Zhang, X.; Yao, X.; Geng, C.; Xue, X.; Zhong, L.F. Boric acid inhibits LPS-induced TNF-alpha formation through a thiol-dependent mechanism in THP-1 cells. J. Trace Elem. Med. Biol. 2008, 22, 189–195. [Google Scholar] [CrossRef] [PubMed]
- Zafar, H.; Ali, S. Boron inhibits the proliferating cell Nuclear Antigen Index, molybdenum containing proteins and ameliorates oxidative stress in hepatocellular carcinoma. Arch. Biochem. Biophys. 2013, 529, 66–74. [Google Scholar] [CrossRef]
- Khaliq, H.; Juming, Z.; Ke-Mei, P. The Physiological Role of Boron on Health. Biol. Trace Elem. Res. 2018, 186, 31–51. [Google Scholar] [CrossRef]
- Demirdogen, R.E. Relationship among blood boron level, diabetes mellitus, lipid metabolism, bone metabolism and obesity: Can boron be an efficient indicator for metabolic diseases? Health Sci. J. 2020, 14, 1–11. [Google Scholar] [CrossRef]
- Barranco, W.T.; Eckhert, C.D. Boric acid inhibits prostate cancer cell proliferation. Cancer Lett. 2004, 216, 21–29. [Google Scholar] [CrossRef]
- Barranco, W.T.; Eckhert, C.D. Cellular changes in boric acid-treated DU-145 prostate cancer cells. Br. J. Cancer 2006, 94, 884–890. [Google Scholar] [CrossRef]
- Korkmaz, M.; Uzgo, E.; Bakirdere, S.; Aydin, F.; Ataman, Y. Effects of dietary boron on cervical cytopathology and on micronucleus frequency in exfoliated buccal cells. Environ. Toxicol. 2007, 22, 17–25. [Google Scholar] [CrossRef] [PubMed]
- Gupta, G.P. Role of Iron (Fe) in Body. Iosr J. Appl. Chem. 2014, 7, 38–46. [Google Scholar] [CrossRef]
- Allen, L.H. Anemia and iron deficiency: Effects on pregnancy outcome. Am. J. Clin. Nutr. 2000, 71, 1280–1284. [Google Scholar] [CrossRef] [PubMed]
- Scholl, T.O.; Stein, T.P.; Smith, W.K. Leptin and maternal growth during adolescent pregnancy. Am. J. Clin. Nutr. 2000, 72, 1542–1547. [Google Scholar] [CrossRef] [PubMed]
- West, K.P., Jr.; Katz, J.; Khatry, S.K.; LeClerq, S.C.; Pradhan, E.K.; Shrestha, S.R.; Connor, P.B.; Dali, S.M.; Christian, P.; Pokhrel, R.P.; et al. Double blind, cluster randomised trial of low dose supplementation with vitamin A or beta-carotene on mortality related to pregnancy in Nepal, The NNIPS-2 study group. Br. Med. J. 1999, 318, 570–575. [Google Scholar] [CrossRef]
- Finley, J.W.; Davis, C.D. Manganese absorption and retention in Rats is affected by the type of dietary fat. Biol. Trace Elem. Res. 2001, 82, 143–158. [Google Scholar] [CrossRef]
- Merrell, P.H. The Importance of Minerals in the Long Term Health of Humans; Jost Chemical Company: St. Louis, MO, USA, 2017; pp. 1–21. [Google Scholar]
- Law, N.A.; Caudle, M.T.; Pecoraro, V.L. Manganese redox enzymes and model systems: Properties, structures, and reactivity. Adv. Inorg. Chem. 1998, 46, 305–440. [Google Scholar]
- Treiber, N.; Maity, P.; Singh, K.; Ferchiu, F.; Wlaschek, M.; Scharffetter-Kochanek, K. The role of manganese superoxide dismutase in skin aging. Dermatoendocrinology 2012, 4, 232–235. [Google Scholar] [CrossRef]
- Stover, P.J. Physiology of Folate and Vitamin B12in Health and Disease. Nutr. Rev. 2004, 62, 3–12. [Google Scholar] [CrossRef]
- Huskinsson, E.; Maggini, S.; Ruf, M. The influence of micronutrients on cognitive function and performance. J. Int. Med. Res. 2007, 35, 1–19. [Google Scholar] [CrossRef]
- Duthie, S.J. Folic Acid Deficiency and Cancer: Mechanisms of DNA Instability. Br. Med. Bull. 1999, 55, 578–592. [Google Scholar] [CrossRef] [PubMed]
- Courtemanche, C.; Elson-Schwab, I.; Mashiyama, S.T.; Kerry, N.; Ames, B.N. Folate deficiency inhibits the proliferation of primary human CD8+ T lymphocytes in vitro. J. Immunol. 2004, 173, 3186–3192. [Google Scholar] [CrossRef] [PubMed]
- Yoshii, K.; Hosomi, K.; Sawane, K.; Kunisawa, J. Metabolism of dietary and microbial vitamin B family in the regulation of host immunity. J. Front. Nutr. 2019, 6, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Reynolds, E.H.; Preece, J.; Johnson, A.L. Folate metabolism in epileptic and psychiatric patients. J. Neurol. Neurosurg. Psychiatry 1971, 34, 726–732. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Duthie, S.J.; Hawdon, A. DNA instability (strand breakage, uracil misincorporation and defective repair) is increased by folic acid depletion in human lymphocytes in vitro. Faseb J. 1998, 12, 1491–1497. [Google Scholar] [CrossRef]
- Morrell, M.J. Folic Acid and Epilepsy. Curr. Rev. 2002, 2, 31–34. [Google Scholar] [CrossRef]
- Al-Fartusie, F.S.; Mohssan, S.N. Essential Trace Elements and Their Vital Roles in human body. Indian J. Adv. Chem. Sci. 2017, 5, 127–136. [Google Scholar]
- Myint, Z.W.; Oo, T.H.; Thein, K.Z.; Tun, A.M.; Saeed, H. Copper Deficiency Anemia: Review Article. Ann. Hematol. 2018, 97, 1527–1534. [Google Scholar] [CrossRef]
- Bonham, M.; O’Connor, J.M.; Hannigan, B.M.; Strain, J.J. The immune system as a physiological indicator of marginal copper status? Br. J. Nutr. 2002, 87, 393–403. [Google Scholar] [CrossRef]
- Davis, C.D. Low dietary copper increases fecal free radical production, fecal water alkaline phosphatase activity and cytotoxicity in healthy men. J. Nutr. 2003, 133, 522–527. [Google Scholar] [CrossRef]
- Araya, M.; Pizarro, F.; Olivares, M.; Arredondo, M.; Gonzalez, M.; Mendez, M. Understanding copper homeostasis in humans and copper effects on health. Biol. Res. 2006, 39, 183–187. [Google Scholar] [CrossRef] [PubMed]
- Copper: Essential for Human Health 2018. Available online: https://copperalliance.org.uk/knowledge-base/education/education-resources/copper-essential-human-health (accessed on 11 August 2020).
- Kaur, A. Biological functions of Vitamin B complex and effects on human health in both excess and deficiency levels. Pharma Tutor 2015, 3, 40–47. [Google Scholar]
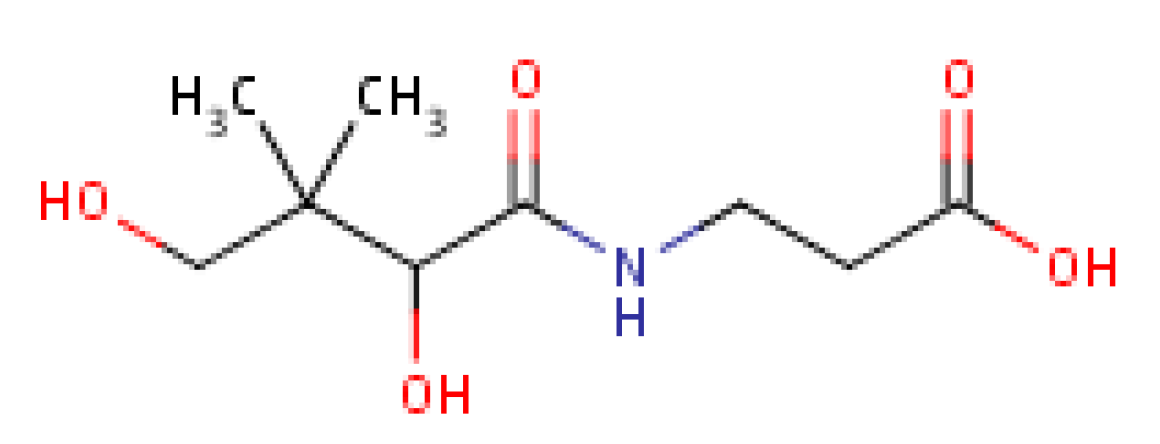
- Rucker, R.; Bauerly, K. Pantothenic Acid. Handbook of Vitamins, 5th ed.; Zempleni, J., Suttie, J., Gregory, J.F., III, Stover, P.J., Eds.; CRC Press: Boca Raton, FL, USA, 2013; Chapter 8; pp. 325–349. [Google Scholar]
- Schramm, M.; Wiegmann, K.; Schramm, S.; Gluschko, A.; Herb, M.; Utermohlen, O.; Kröonke, M. Riboflavin (vitamin B2) deficiency impairs NADPH oxidase 2 (Nox2) priming and defense against Listeria monocytogenes. Eur. J. Immunol. 2014, 44, 728–741. [Google Scholar] [CrossRef]
- Marashly, E.T.; Bohlega, S.A. Riboflavin has neuroprotective potential: Focus on parkinson’s disease and migraine. Front. Neurol. 2017, 8, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Kunisawa, J.; Kiyono, H. Vitamin-mediated regulation of intestinal immunity. Front. Immunol. 2013, 4, 1–6. [Google Scholar] [CrossRef]
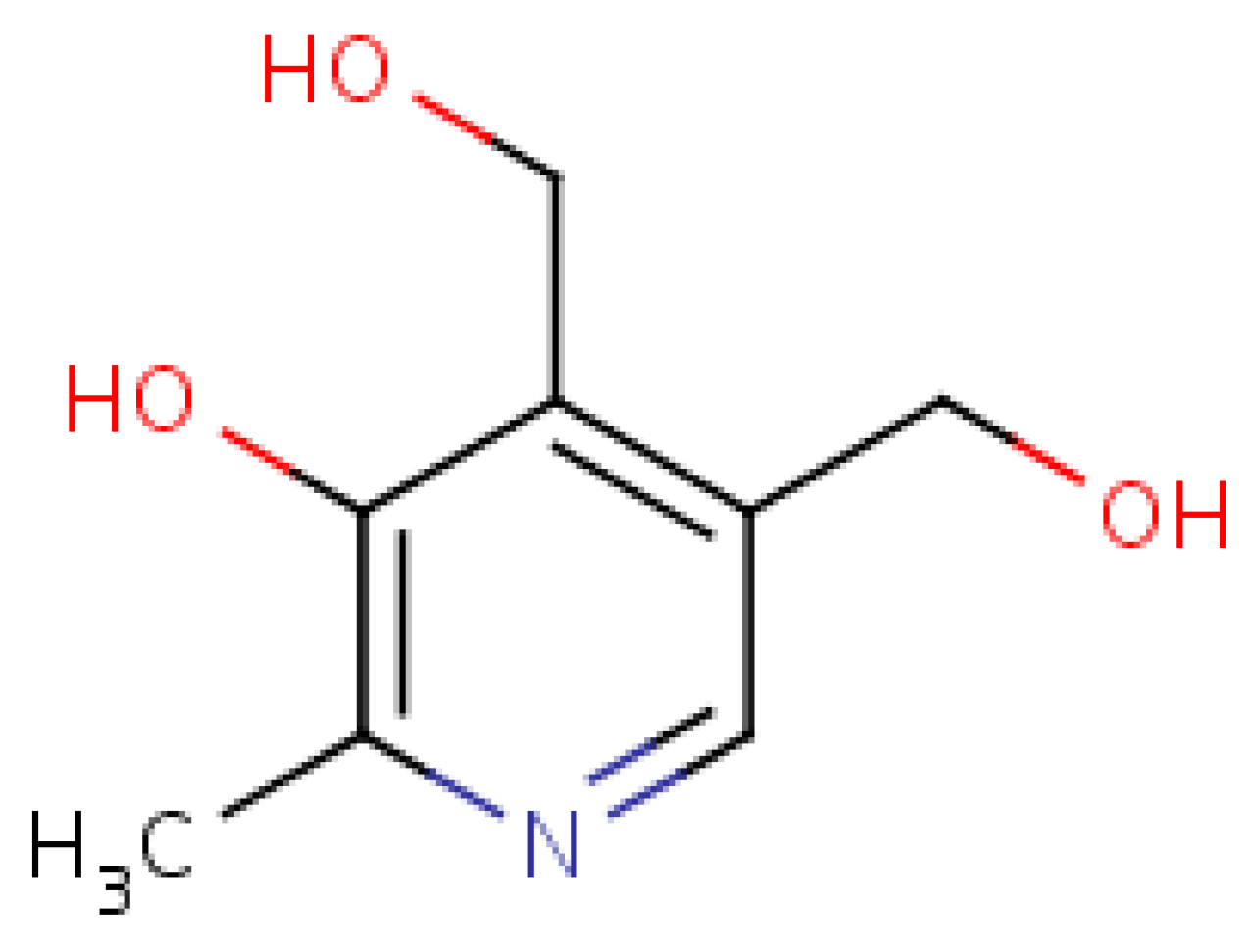
- Velásquez, M.; Méndez, D.; Moneriz, C. Pyridoxine decreases oxidative stress on human erythrocyte membrane protein in vitro. Open Biochem. J. 2019, 13, 37–44. [Google Scholar] [CrossRef]
- Bradford, A. Vitamin B6: Sources and Benefits. LiveScience. 2015, pp. 1–13. Available online: https://www.livescience.com/51920-vitamin-b6.html (accessed on 11 August 2020).
- Vermeulen, E.G.; Stehouwer, C.D.; Twisk, J.W.; van den Berg, M.; de Jong, S.C.; Mackaay, A.J.; Campen, C.V.; Visser, F.C.; Jakobs, C.; Bulterijs, E.J. Effect of Homocysteine-Lowering Treatment with Folic Acid plus Vitamin B6 on progression of subclinical atherosclerosis: A randomised, placebo-controlled Trial. Lancet 2000, 355, 517–522. [Google Scholar] [CrossRef]
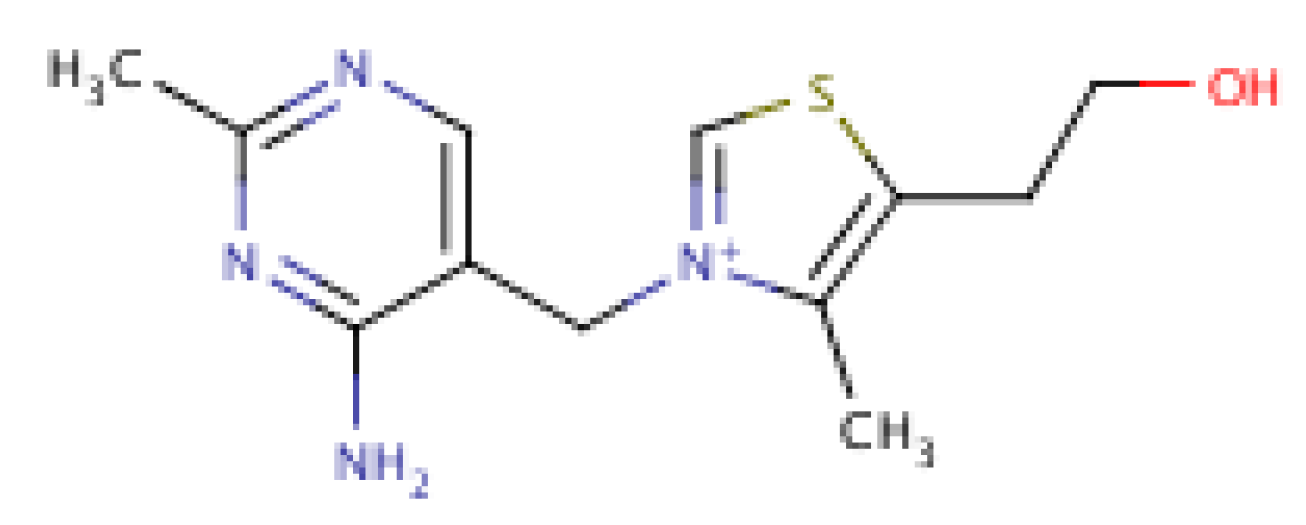
- Hirsch, J.A.; Parrott, J. New considerations on the neuromodulatory role of Thiamine. Pharmacology 2012, 89, 111–116. [Google Scholar] [CrossRef]
- Singleton, C.K.; Martin, P.R. Molecular mechanisms of Thiamine Utilization. Curr. Mol. Med. 2001, 1, 197–207. [Google Scholar] [CrossRef]
- Calderón-Ospina, C.A.; Nava-Mesa, M.O. B vitamins in the nervous system: Current knowledge of the biochemical modes of action and synergies of thiamine, pyridoxine, and cobalamin. Cns Neurosci. 2020, 26, 5–13. [Google Scholar] [CrossRef]
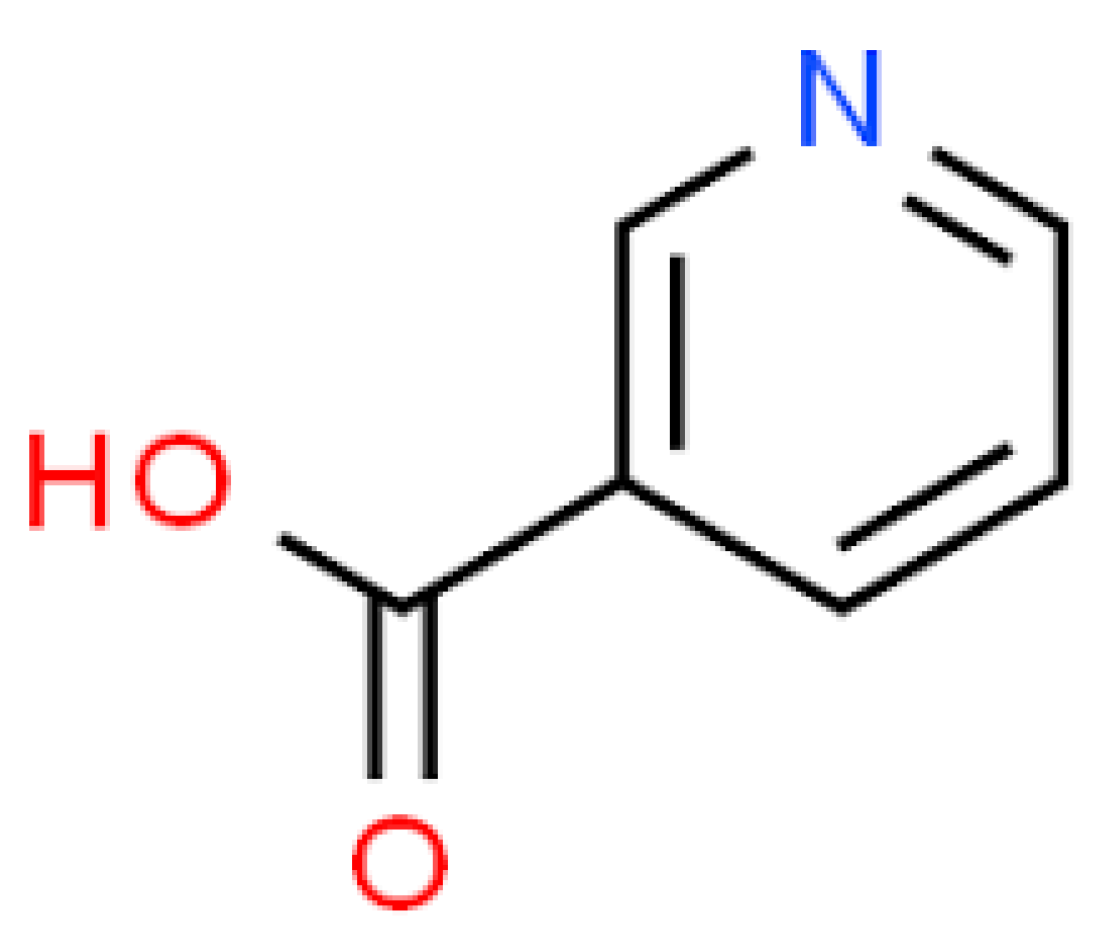
- Lipszyc, P.S.; Cremaschi, G.A.; Zubilete, M.Z.; Bertolino, M.L.A.; Capani, F.; Genaro, A.M.; Wald, M.R. Niacin modulates pro-inflammatory cytokine secretion: A potential mechanism involved in its anti-atherosclerotic effect. Open Cardiovasc. Med. J. 2013, 7, 90–98. [Google Scholar] [CrossRef] [PubMed]
- Hegyi, J.; Schwartz, R.A.; Hegyi, V. Pellagra: Dermatitis, dementia, and diarrhea. Int. J. Dermatol. 2004, 43, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Amanullah, S.; Seeber, C. Niacin deficiency resulting in neuropsychiatric symptoms: A case study and review of literature. Clin. Neuropsychiatry 2010, 7, 10–14. [Google Scholar]
- Arun, P.; Padmakumaran Nair, K.G.; Manojkumar, V.; Deepadevi, K.V.; Lakshmi, L.R.; Kurup, P.A. Decreased hemolysis and lipid peroxidation in blood during storage in the presence of nicotinic acid. Vox Sang. 1999, 76, 220–225. [Google Scholar] [CrossRef]
- Boyonoski, A.C.; Gallacher, L.M.; ApSimon, M.M.; Jacobs, R.M.; Shah, G.M.; Poirier, G.G.; Kirkland, J.B. Niacin deficiency in rats increases the severity of Ethylnitrosourea-induced Anemia and Leukopenia. J. Nutr. 2000, 130, 1102–1107. [Google Scholar] [CrossRef][Green Version]
- Yuvaraj, S.; Premkumar, V.G.; Vijayasarathy, K.; Gangadaran, S.G.D.; Sachdanandam, P. Augmented antioxidant status in tamoxifen treated post-menopausal women with breast cancer on co-administration with coenzyme q10, niacin and riboflavin. Cancer Chemother. Pharm. 2008, 61, 933–941. [Google Scholar] [CrossRef]
- Cho, K.; Kim, H.; Rodriguez-Iturbe, B.; Vaziri, N.D. Niacin ameliorates oxidative stress, inflammation, proteinuria, and hypertension in rats with chronic renal failure. Am. J. Physiol. Ren. Physiol. 2009, 297, 106–113. [Google Scholar] [CrossRef]
- Ganji, S.H.; Kashyap, M.L.; Kamanna, V.S. Niacin inhibits fat accumulation and oxidative stress in human hepatocytes and regresses hepatic steatosis in experimental rat model. J. Clin. Lipidol. 2014, 8, 349–350. [Google Scholar] [CrossRef]
- Ganji, S.H.; Kashyap, M.L.; Kamanna, V.S. Niacin inhibits fat accumulation, oxidative stress and inflammatory cytokine IL-8 in cultured hepatocytes: Impact on non-alcoholic fatty liver disease. Metabolism 2015, 64, 982–990. [Google Scholar] [CrossRef]
- Wall, M. Ascorbic acid, vitamin A, and mineral composition of banana (Musa sp.) and papaya (Carica papaya) cultivars grown in Hawaii. J. Food Compos. Anal. 2006, 19, 434–445. [Google Scholar] [CrossRef]
- Englberger, L.; Wills, R.B.H.; Blades, B.; Dufficy, L.; Daniells, J.W.; Coyne, T. Carotenoid content and flesh colour of selected banana cultivars growing in Australia. Food Nutr. Bull. 2006, 27, 281–291. [Google Scholar] [CrossRef] [PubMed]
- Khawas, P.; Das, A.J.; Sit, N.; Badwaik, L.S.; Deka, S.C. Nutritional composition of culinary Musa ABB at different stages of development. Am. J. Food Technol. 2014, 2, 80–87. [Google Scholar] [CrossRef]
- Subagio, A.; Morita, N.; Sawada, S. Carotenoids and their fatty-acid esters in banana peel. J. Nutr. Sci. Vitam. 1996, 42, 553–566. [Google Scholar] [CrossRef] [PubMed]
- Chun, J.; Lee, J.; Ye, L.; Exler, J.; Eitenmiller, R.R. Tocopherol and tocotrienol contents of raw and processed fruits and vegetables in the United States diet. J. Food Compos. Anal. 2006, 19, 196–204. [Google Scholar] [CrossRef]
- Waghmare, A.G.; Arya, S.S. Use of fruit by-products in the preparation of hypo-glycemic thepla: Indian unleavened vegetable flat bread. J. Food Process. Preserv. 2014, 38, 1198–1206. [Google Scholar] [CrossRef]
- Borges, C.V.; Amorim, V.B.; Ramlov, F.; Ledo, C.A.; Donato, M.; Maraschin, M.; Amorim, E.P. Characterisation of metabolic profile of banana genotypes, aiming at biofortified Musa spp. Cultivars. Food Chem. 2014, 145, 496–504. [Google Scholar] [CrossRef]
- Mokbel, M.S.; Hashinga, F. Antibacterial and Antioxidant Activities of Banana (Musa AAA cv. Cavendish) Fruits Peel. Am. J. Biochem. Biotechnol. 2005, 1, 125–131. [Google Scholar] [CrossRef]
- Aboul-Enein, A.M.; Salama, Z.A.; Gaafar, A.A.; Aly, H.F.; Abou-Elella, F.; Ahmed, H.A. Identification of phenolic compounds from banana peel (Musa paradisiaca L.) as antioxidant and antimicrobial agents. J. Chem. Pharm. Res. 2016, 8, 46–55. [Google Scholar]
- Someya, S.; Yoshiki, Y.; Okubo, K. Antioxidant compounds from banana (Musa cavendish). Food Chem. 2002, 79, 351–354. [Google Scholar] [CrossRef]
- Anyasi, T.A.; Jideani, A.I.O.; Mchau, G.R.A. Phenolics and essential mineral profile of organic acid pre-treated unripe banana flour. Food Res. Int. 2018, 104, 100–109. [Google Scholar] [CrossRef]
- Braicu, C.; Gherman, C.D.; Irimie, A.; Berindan-Neagoe, I. Epigallocatechin-3-Gallate (EGCG) inhibits cell proliferation and migratory behaviour of triple negative breast cancer cells. J. Nanosci. Nanotechnol. 2013, 13, 632–637. [Google Scholar] [CrossRef] [PubMed]
- Shirakami, Y.; Sakai, H.; Kochi, T.; Seishima, M.; Shimizu, M. Catechins and Its Role in Chronic Diseases. Adv. Exp. Med. Biol. 2016, 929, 67–90. [Google Scholar] [PubMed]
- Piironen, V.; Toivo, J.; Puupponen-Pimiä, R.; Lampi, A. Plant sterols in vegetables, fruits and berries. J. Sci. Food Agric. 2003, 83, 330–337. [Google Scholar] [CrossRef]
- Sidhu, J.S.; Zafar, T.A. Bioactive compounds in banana fruits and their health benefits. Food. Q. Saf. 2018, 2, 183–188. [Google Scholar] [CrossRef]
- Villaverde, J.J.; Oliveira, L.; Vilela, C.; Domingues, R.M.; Freitas, N.; Cordeiro, N.; Freire, C.S.R.; Silverstre, A.J.D. High valuable compounds from the unripe peel of several Musa species cultivated in Madeira Island (Portugal). Ind. Crop Prod. 2013, 42, 507–512. [Google Scholar] [CrossRef]
- Knapp, F.F.; Nicholas, H.J. The sterols and triterpenes of banana pulp. J. Food Sci. 1969, 34, 584–586. [Google Scholar] [CrossRef]
- Kibria, A.A.; Kamrunnessa; Rahman, M.; Kar, A. Extraction and evaluation of phytochemicals from banana peels (Musa sapientum) and banana plants (Musa paradisiaca). Malays. Halal Res. 2019, 2, 22–26. [Google Scholar] [CrossRef]
- Velumani, S. Phytochemical screening and antioxidant activity of banana peel. IJARIIE Int. J. 2016, 2, 91–102. [Google Scholar]
- Yoon, W.J.; Lee, N.H.; Hyun, C.G. Limonene suppresses lipopolysaccharide-induced production of nitric oxide, prostaglandin E2 and pro-inflammatory cytokines in RAW 264-7 macrophages. J. Oleo Sci. 2010, 59, 415–421. [Google Scholar] [CrossRef]
- Fu, X.; Cheng, S.; Liao, Y.; Huang, B.; Du, B.; Zeng, W.; Jiang, Y.M.; Duan, X.W.; Yang, Z.Y. Comparative analysis of pigments in red and yellow banana fruit. Food Chem. 2018, 239, 1009–1018. [Google Scholar] [CrossRef]
- Seymour, G.B. Banana. In Biochemistry of Fruit Ripening; Seymour, J.E., Tucker, G.A., Eds.; Chapman and Hall: New York, NY, USA, 1993; pp. 83–106. [Google Scholar]
- González-Montelongo, R.; Lobo, G.; Gonzalez, M. Antioxidant activity in banana peel extracts: Testing extraction conditions and related bioactive compounds. Food Chem. 2010, 119, 1030–1039. [Google Scholar] [CrossRef]
- Choudhary, S.P.; Tran, L.S. Phytosterols: Perspectives in human nutrition and clinical therapy. Curr. Med. Chem. 2011, 18, 4557–4567. [Google Scholar] [CrossRef] [PubMed]
- Ponchet, M.; Martin-Tanguy, J.; Marais, A.; Martin, C. Hydroxycinnamoyl acid amides and aromatic amines in the inflorescences of some Araceae species. Phytochemistry 1980, 21, 2865–2869. [Google Scholar] [CrossRef]
- Waalkes, T.P.; Sjoerdsma, A.; Creveling, C.R.; Weissbach, H.; Udenfriend, S. Serotonin, Norepinephrine, and Related Compounds in Bananas. Science 1958, 127, 648–650. [Google Scholar] [CrossRef]
- Kanazawa, K.; Sakakibara, H. High content of dopamine, a strong antioxidant in Cavendish banana. J. Agric. Food Chem. 2000, 48, 844–848. [Google Scholar] [CrossRef] [PubMed]
- Nonogaki, K. New insights into sympathetic regulation of glucose and fat metabolism. Diabetologia 2000, 43, 533–549. [Google Scholar] [CrossRef] [PubMed]
- Stanner, S.A.; Hughes, J.; Kelly, C.N.; Buttriss, J. A review of the epidemiological evidence for the ‘antioxidant hypothesis’. Public Health Nutr. 2004, 7, 407–422. [Google Scholar] [CrossRef] [PubMed]
- Jain, S.K.; Pemberton, P.W.; Raymond, A.S.; McMahon, F.T.; Burrows, P.C.; Aboutwerat, A.; Warnes, T.W. Oxidative stress in chronic hepatitis C: Not just a feature of late stage disease. J. Hepatol. 2002, 36, 805–811. [Google Scholar] [CrossRef]
- Van de Casteele, M.; Zaman, Z.; Zeegers, M.; Servaes, R.; Fevery, J.; Nevens, F. Blood antioxidant levels in patient with alcoholic liver disease correlate with the degree of liver impairment and are not specific to alcoholic liver injury itself. Aliment. Pharm. 2002, 16, 985–992. [Google Scholar] [CrossRef]
- Sugiura, M. Bioactive Food as Dietary Interventions for Liver and Gastrointestinal Disease; Elsevier: Amsterdam, The Netherlands, 2013; Chapter 27; pp. 421–436. [Google Scholar]
- Murillo, A.G.; Di Marco, D.M.; Fernandez, M.L. The potential of non-provitamin A carotenoids for the prevention and treatment of non-alcoholic fatty liver disease. Biology 2016, 5, 42. [Google Scholar] [CrossRef]
- Tan, B.L.; Norhaizan, M.E. Curcumin Combination Chemotherapy: The implication and efficacy in cancer. Molecules 2019, 24, 527. [Google Scholar] [CrossRef] [PubMed]
- Mahoney, C.W.; Azzi, A. Vitamin E Inhibits Protein Kinase C Activity. Biochem. Biophys. Res. Commun. 1988, 154, 694–697. [Google Scholar] [CrossRef]
- Devaraj, S.; Jialal, I. The effects of alpha-tocopherol on critical cells in atherogenesis. Curr. Opin. Lipidol. 1998, 9, 11–15. [Google Scholar] [CrossRef] [PubMed]
- Cecchini, T.; Ciaroni, S.; Ferri, P.; Ambrogini, P.; Cuppini, R.; Santi, S.; Grande, P.D. Alpha-tocopherol, an exogenous factor of adult hippocampal neurogenesis regulation. J. Neurosci. Res. 2003, 73, 447–455. [Google Scholar] [CrossRef] [PubMed]
- Rimbach, G.; Minihane, A.M.; Majewicz, J.; Fischer, A.; Pallauf, J.; Virgli, F.; Weinberg, P.D. Regulation of cell signalling by Vitamin E. Proc. Nutr. Soc. 2002, 61, 415–425. [Google Scholar] [CrossRef]
- van Aalst, J.A.; Burmeister, W.; Fox, P.L.; Graham, L.M. α-tocopherol preserves endothelial cell migration in the presence of cell-oxidized low-density lipoprotein by inhibiting changes in cell membrane fluidity. Eur. J. Vasc. Surg. 2004, 39, 229–237. [Google Scholar] [CrossRef]
- Brigelius-Flohé, R.; Traber, M.G. Vitamin E: Function and metabolism. Faseb J. 1999, 13, 1145–1155. [Google Scholar] [CrossRef]
- Evans, H.M.; Bishop, K.S. On the existence of a hitherto unrecognized dietary factor essential for reproduction. Science 1922, 56, 650–661. [Google Scholar] [CrossRef]
- Sen, C.K.; Khanna, S.; Roy, S.; Packer, L. Molecular basis of vitamin E action: Tocotrienols potently inhibit glutamate-induced pp60c-scr kinase activation of HT4 neuronal cells. J. Biol. Chem. 2000, 275, 13049–13055. [Google Scholar] [CrossRef]
- Williamson, G.; Manach, C. Bioavailability and bioefficacy of polyphenols in humans II: Review of 93 intervention studies. Am. J. Clin. Nutr. 2005, 81, 243–255. [Google Scholar] [CrossRef]
- Bernatoniene, J.; Kopustinskiene, D.M. The role of catechins in cellular responses to oxidative stress. Molecules 2018, 23, 965. [Google Scholar] [CrossRef] [PubMed]
- Rowley, T.J.; Bitner, B.F.; Ray, J.D.; Lathen, D.R.; Smithson, A.T.; Dallon, B.W.; Plowman, C.J.; Bikman, B.T.; Hansen, J.M.; Dorenkott, M.R.; et al. Monomeric cocoa catechins enhance β-cell function by increasing mitochondrial respiration. J. Nutr. Biochem. 2017, 49, 30–41. [Google Scholar] [CrossRef] [PubMed]
- Weinreb, O.; Amit, T.; Mandel, S.; Youdim, M.B.H. Neuroprotective molecular mechanisms of (-)-epigallocatechin-3-gallate: A reflective outcome of its antioxidant, iron chelating and neuritogenic properties. Genes Nutr. 2009, 4, 283–496. [Google Scholar] [CrossRef] [PubMed]
- Hadjipavlou-Litina, D.; Kontogiorgis, C.; Pontiki, E.; Dakanali, M.; Akoumianaki, A.; Katerinopoulos, H.E. Anti-inflammatory and antioxidant activity of coumarins designed as potential fluorescent zinc sensors. J. Enzym. Inhib. Med. Chem. 2007, 22, 287–292. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.; Kim, N.H.; Park, Y.S.; Kim, H.; Lee, S.; Wang, Q.; Kim, Y.K. 7-diethylamino-3(2′-benzoxazolyl)-coumarin is a novel microtubule inhibitor with antimitotic activity in multidrug resistant cancer cells. Biochem. Pharm. 2009, 77, 1773–1779. [Google Scholar] [CrossRef]
- Sandeep, G.; Sri Ranganath, Y.; Bhasker, S.; Rajkumar, N. Synthesis and Biological Screening of Some Novel Coumarin Derivatives. Asian J. Res. Chem. 2009, 2, 46–48. [Google Scholar]
- Ramesh, B.; Sumana, T. Synthesis and anti-inflammatory activity of Pyrazolines. E-J. Chem. 2010, 7, 514–516. [Google Scholar] [CrossRef]
- Pelkonen, O.; Raunio, H.; Rautio, A.; Pasanen, M.; Lang, M.A. The metabolism of coumarin. In Coumarins: Biology, Applications and Mode of Action; O’Kennedy, R., Thornes, R.D., Eds.; John Wiley: New York, NY, USA, 1997; pp. 67–92. [Google Scholar]
- Loprinzi, C.L.; Kugler, J.W.; Sloan, J.A.; Rooke, T.W.; Quella, S.K.; Novotny, P.; Mowat, R.B.; Michalak, J.C.; Stella, P.J.; Levitt, R.; et al. Lack of effect of coumarin in women with lymphedema after treatment for breast cancer. N. Engl. J. Med. 1999, 340, 346–350. [Google Scholar] [CrossRef]
- Finn, G.; Kenealy, E.; Creaven, B.; Egan, D. Coumarinyl aldehyde as a Michael acceptor type of calorimetric and fluorescent probe for cyanide in water. Cancer Lett. 2002, 18, 54–61. [Google Scholar]
- Rohini, K.; Srikumar, P.S. Therapeutic role of coumarins and coumarin-related compounds. J. Catal. 2014, 5, 1–3. [Google Scholar] [CrossRef]
- Groutas, W.C.; Abrams, W.R.; Carroll, R.T.; Moi, M.K.; Miller, K.E.; Margolis, M.T. Specific inhibition of human leukocyte elastase by substituted alpha-pyrones. Experientia 1984, 40, 361–362. [Google Scholar] [CrossRef] [PubMed]
- Budzisz, E.; Brzezinska, E.; Krajewska, U.; Rozalski, M. Cytotoxic effects, alkylating properties and molecular modelling of coumarin derivatives and their phosphonic analogues. Eur. J. Med. Chem. 2003, 38, 597–603. [Google Scholar] [CrossRef]
- Ostlund, R.E. Phytosterols and cholesterol metabolism. Curr. Opin. Lipidol. 2004, 15, 37–41. [Google Scholar] [CrossRef] [PubMed]
- Cohn, J.S.; Kamili, A.; Wat, E.; Chung, R.W.S.; Tanday, S. Dietary phospholipids and intestinal cholesterol absorption. Nutrients 2010, 2, 116–127. [Google Scholar] [CrossRef] [PubMed]
- Lin, X.; Racette, S.B.; Lefevre, M.; Spearie, C.A.; Most, M.; Ma, L.; Ostlund, R.E., Jr. The effects of phytosterols present in natural food matrices on cholesterol metabolism and LDL-cholesterol: A controlled feeding trial. Eur. J. Clin. Nutr. 2010, 64, 1481–1487. [Google Scholar] [CrossRef]
- Lin, X.; Ma, L.; Racette, S.B.; Spearie, C.L.A.; Ostlund, R.E., Jr. Phytosterol glycosides reduce cholesterol absorption in humans. Am. J. Physiol. Gastrointest. Liver Physiol. 2009, 296, 931–935. [Google Scholar] [CrossRef]
- Gylling, H.; Plat, J.; Turley, S.; Ginsberg, H.N.; Ellegård, L.; Jessup, W.; Jones, P.J.; Lütjohann, D.; Maerz, W.; Masana, L.; et al. Plant sterols and plant stanols in the management of dyslipidaemia and prevention of cardiovascular disease. Atherosclerosis 2014, 232, 346–360. [Google Scholar] [CrossRef]
- Gylling, H.; Simonen, P. Phytosterols, phytostanols and lipoprotein metabolism. Nutrients 2015, 7, 7965–7977. [Google Scholar] [CrossRef]
- Dumolt, H.; Rideout, T.C. The lipid-lowering effects and associated mechanisms of dietary phytosterol supplementation. Curr. Pharm. Des. 2017, 23, 5077–5085. [Google Scholar] [CrossRef]
- Ju, L.M.; Clausen, K.F.; Allred, A.L.; Almada, W.G. Helferich, β-sitosterol, β-sitosterol glucoside, and a mixture of β-sitosterol and β-sitosterol glucoside modulate the growth of estrogen-responsive breast cancer cells in vitro and in ovariectomized athymic Mice. Nutr. Cancer 2004, 134, 1145–1151. [Google Scholar]
- Awad, A.B.; Chinnam, M.; Fink, C.S.; Bradford, P. Beta-Sitosterol activates Fas signaling in human breast cancer cells. Phytomedicine 2007, 14, 747–754. [Google Scholar] [CrossRef] [PubMed]
- Awad, A.B.; Downie, A.; Fink, C.S.; Kim, U. Dietary phytosterol inhibits the growth and metastasis of MDA-MB-231 human breast cancer cells grown in SCID mice. Anticancer Res. 2000, 20, 821–824. [Google Scholar] [PubMed]
- Awad, M.M.; Ellemor, D.M.; Boyd, R.L.; Emmins, J.J.; Rood, J.I. Synergistic effects of alpha-toxin and perfringolysin O in Clostridium perfringens-mediated gas gangrene. Infect. Immun. 2001, 69, 7904–7910. [Google Scholar] [CrossRef]
- Awad, A.B.; Barta, S.L.; Fink, C.S.; Bradford, P.G. beta-Sitosterol enhances Tamoxifen effectiveness on breast cancer cells by affecting ceramide metabolism. Mol. Nutr. Food Res. 2008, 52, 419–426. [Google Scholar] [CrossRef] [PubMed]
- Brahmkshatriya, P.P.; Brahmkshatriya, P.S. Terpenes: Chemistry, biological role and therapeutic applications. In Natural Products; Ramawat, K.G., Merillon, J.M., Eds.; Springer: Heidelberg, Germany; New York, NY, USA; Dordrecht, The Netherlands; London, UK, 2013; pp. 2665–2691. [Google Scholar]
- Kapoor, P.; Rizvi, F.; Kakkar, P. Naringenin prevents high glucose-induced mitochondria-mediated apoptosis involving AIF, Endo-G and Caspases. Apoptosis 2013, 18, 9–27. [Google Scholar] [CrossRef]
- Zhang, X.Z.; Wang, L.; Liu, D.W.; Tang, G.Y.; Zhang, H.Y. Synergistic inhibitory effect of berberine and d-limonene on human gastric carcinoma cell line MGC803. J. Med. Food 2014, 17, 955–962. [Google Scholar] [CrossRef]
- Duru, M.E.; Cayan, G.T. Biologically Active Terpenoids from Mushroom origin: A Review. Rec. Nat. Prod. 2015, 9, 456–483. [Google Scholar]
- Wilkins, J.S., Jr. Method for Treating Gastrointestinal Disorders. U.S. Pantent US6420435B1, 16 July 2002. [Google Scholar]
- Patrick, L. Gastroesophageal Reflux Disease (GERD): A review of conventional and alternative treatments. Altern. Med. Rev. 2011, 16, 116–133. [Google Scholar]
- Prior, R.L.; Wu, X. Anthocyanins: Structural characteristics that result in unique metabolic patterns and biological activities. Free Radic. Res. 2006, 40, 1014–1028. [Google Scholar] [CrossRef]
- Tsuda, T. Dietary anthocyanin-rich plants: Biochemical basis and recent progress in health benefits studies. Mol. Nutr. Food Res. 2006, 56, 159–170. [Google Scholar] [CrossRef]
- Cooke, D.; Steward, W.P.; Gescher, A.J.; Marczylo, T. Anthocyans from fruits and vegetables- does bright colour signal cancer chemopreventive activity? Eur. J. Cancer. 2005, 41, 1931–1940. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.S.; Stoner, G.D. Anthocyanins and their role in cancer prevention. Cancer Lett. 2008, 269, 281–290. [Google Scholar] [CrossRef] [PubMed]
- Thomasset, S.; Berry, D.P.; Cai, H.; West, K.; Marczylo, T.H.; Marsden, D.; Brown, K.; Dennison, A.; Garcea, G.; Miller, A.; et al. Pilot study of oral anthocyanins for colorectal cancer chemoprevention. Cancer Prev. Res. (Phila) 2009, 2, 625–633. [Google Scholar] [CrossRef] [PubMed]
- Mazza, G.J. Anthocyanins and heart health. Ann. Ist. Super. Sanita 2007, 43, 369–374. [Google Scholar]
- Xia, M.; Ling, W.; Zhu, H.; Wang, Q.; Ma, J.; Hou, M.J.; Tang, Z.H.; Li, L.; Ye, Q.Y. Anthocyanin prevents CD40-activated pro-inflammatory signaling in endothelial cells by regulating cholesterol distribution. Arter. Thromb. Vasc. Biol. 2007, 27, 519–524. [Google Scholar] [CrossRef]
- He, J.; Giusti, M.M. Anthocyanins: Natural colorants with health-promoting properties. Annu. Rev. Food Sci. Technol. 2010, 1, 163–187. [Google Scholar] [CrossRef]
- Zu, X.; Zhang, Z.; Zhang, X.; Yoshioka, M.; Yang, Y.; Li, J. Anthocyanins extracted from Chinese blueberry (Vaccinium uliginosum L.) and its anticancer effects on DLD-1 and COLO205 cells. Chin. Med. J. (Engl.) 2010, 123, 2714–2719. [Google Scholar]
- Viguerie, N.; Clement, K.; Barbe, P.; Courtine, M.; Benis, A.; Larrouy, D.; Hanczar, B.; Pelloux, V.; Poitou, C.; Khalfallah, Y.; et al. In vivo epinephrine-mediated regulation of gene expression in human skeletal muscle. J. Clin. Endocrinol. Metab. 2004, 89, 2000–2014. [Google Scholar] [CrossRef]
- Thurston, R.J.; Bryant, C.C.; Korn, N. The effects of corticosterone and catecholamine infusion on plasma glucose levels in chicken (Gallus domesticus) and Turkey (Meleagris gallapavo). Comp. Biochem. Phys. C 1993, 106, 59–62. [Google Scholar]
- Tapryal, N.; Vivek, V.G.; Mukhopadhyay, C.K. Catecholamine stress hormones regulate cellular iron homeostasis by a posttranscriptional mechanism mediated by iron regulatory protein. J. Biol. Chem. 2015, 290, 7634–7636. [Google Scholar] [CrossRef]
- Pramod Kerkar, M.D. Can You Eat Banana Peel? 2019, pp. 1–7. Available online: https://www.epainassist.com/articles/can-you-eat-banana-peel (accessed on 11 August 2020).
- Karthikeyan, M.; Divakar, S. Standardization of banana peel based sauce. Int. J. Food Sci. Nutr. 2018, 3, 95–98. [Google Scholar]
- Breyer, M. How to Eat Banana Peels. 2018. Available online: https://www.treehugger.com/how-eat-banana-peels-4857703 (accessed on 11 August 2020).
- Agama-Acevedo, E.; Sañudo-Barajas, J.A.; Vélez De La Rocha, R.; González Aguilar, G.A.; Bello-Peréz, L.A. Potential of plantain peels flour (Musa paradisiaca L.) as a source of dietary fiber and antioxidant compound. J. Food 2016, 14, 117–123. [Google Scholar]
- Chasoy, G.R.; Cock, L.S. Effect of plantain (Musa paradisiaca L. cv. Dominico Harton) peel flour as binder in frankfurter-type sausage. Acta Agron. 2017, 66, 305–310. [Google Scholar] [CrossRef]
- Arun, M.; Satish, S.; Anima, P. Experimental wound healing aspects of Jasminum grandiflorum L.: A pre-clinical study. Aliment. Pharm. 2015, 12, 135–142. [Google Scholar]
- Aguilar, J.M.C.; Baria, A.R.E.; Cruz, C.O. Incorporation of Saba (Musa paradisiaca L.) banana peel in fresh pasta. Antorcha 2016, 3, 1–21. [Google Scholar]
- Banerjee, S.; Halder, B.; Barman, N.R.; Ghosh, A.K. An overview on different variety of Musa species: Importance and its enormous pharmacological action. J. Pharm. Herb. Formul. 2010, 1, 2–11. [Google Scholar]
- Marín, D.H.; Romero, R.A.; Guzmán, M.; Sutton, T.B. Black Sigatoka: An increasing threat to banana cultivation. Plant Dis. 2003, 87, 208–222. [Google Scholar] [CrossRef]
- FAO. The State of Food Security and Nutrition in the World: Building Resilience for Peace and Food Security; Food and Agriculture Organization of the United Nations: Rome, Italy, 2017; pp. 1–27. [Google Scholar]
- FAO. The Changing Face of Global Banana Trade; Food and Agriculture Organization of the United Nations: Rome, Italy, 2014. [Google Scholar]
- FAO. FAOSTAT. Food and Agriculture Organization of the United Nations; FAO: Rome, Italy, 2015. [Google Scholar]
- Evbuomwan, G.O.; Ukeje, E.U.; Out, M.F.; Amoo, B.A.G.; Essien, E.A.; Odey, L.I.; Abba, M.A. Agricultural Development: Issues of Sustainability. In Contemporary Economic Policy Issues; Nannna, O.J., Alade, S.O., Odoko, F.O., Eds.; CBN Publications: Abuja, Nigeria, 2003; pp. 185–222. [Google Scholar]
- Sharrock, S.; Frison, E. Musa Production around the World: Trends, Varieties and Regional Importance; INIBAP Annual Report: Montpellier, France, 1998; pp. 42–47. [Google Scholar]
- FAO. Banana Market Review 2017; Food and Agriculture Organization of the United Nations: Rome, Italy, 2018; pp. 1–14. [Google Scholar]
- Nigel, A. The World’s Leading Plantain Producers. Available online: https://www.worldatlas.com/articles/the-world-s-leading-plantain-producers.html (accessed on 11 August 2020).






| Nutritional Factors | Other Fruit Peels (g/100 g) |
|---|---|
| Protein | > Pineapple, Mango, Orange, Apple, Pomegranate. |
| Carbohydrate | > Pawpaw, Watermelon |
| Ash content | > Pawpaw, Pineapple, Mango, Apple, Orange, Pomegranate, Watermelon |
| Calcium | > Pawpaw, Pineapple, Apple, Watermelon |
| Iron | > Mango, Pomegranate |
| Zinc | > Mango, Apple, Pomegranate |
| Manganese | > Pawpaw, Pineapple, Apple, Orange, Pomegranate, Watermelon. |
| Micronutrients | Soft flesh (Pulp) | Peel |
|---|---|---|
| Manganese | Musa spp. [46] [AAS- Atomic Absorption Spectrophotometry] | M. paradisiaca [47] [AAS-Atomic Absorption Spectrophotometry] |
| Zinc | Musa spp. [48] [C18RP-HPLC; Microtitre Plate Spectrophotometry; Inductively Coupled Plasma- Optical Emission Spectrometry ICP-OES] | |
| Iron | Musa spp. [48] [C18RP-HPLC; MicrotitrePlate Spectrophotometry; ICP-OES] | Musa spp. [48] [C18RP-HPLC; Microtitre Plate Spectrophotometry;ICP-OES] |
| Copper | M. paradisiaca [49] | |
| Boron | Musa (3.72 mg/kg) [50] [Neutron γ-ray activation analysis] | |
| Phosphorus | M. sinensis and M. paradisiaca [39] [ICP-OES] | M. sinensis and M. paradisiaca [39,51] [ICP-OES] |
| Thiamine, Riboflavin, Niacin, Folate, Pantothenic acid and Pyridoxine | Banana and Plantain (Musa spp.) [32] |
| Dietary Phytoconstituents | Fruit Compartments | Protein/Gene Targets Linked with the Bioactive Dietary Compounds | |
|---|---|---|---|
| Soft flesh (Pulp) | Peel | ||
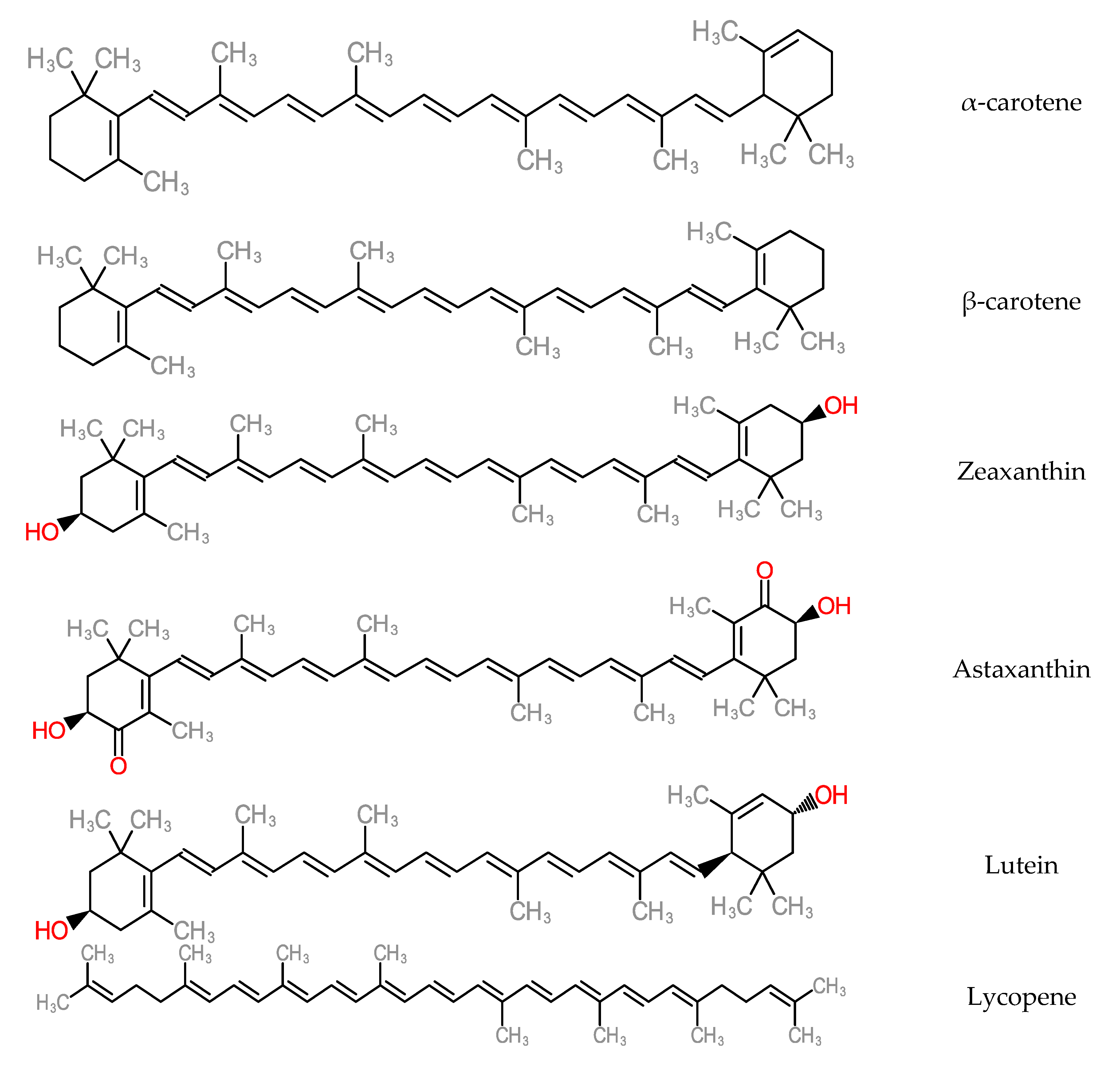
| Carotenoids | -Provitamin A carotenoids [α-carotene (104.9 µg/100 g) and β-carotene (96.9 µg/100 g)] detected in orange coloured banana (Musa sp.) [117]. [HPLC] -α-carotene (61–1055 µg/100 g), trans β-carotene (50–1412 µg/100 g) and cis β-carotene (6–85 µg/100 g) detected across 18 cultivars of banana and plantain [118]. -Carotenoid content (0.130–0.159 mg/100 g) across developmental stages of edible banana [119]. [Ultraviolet Spectrophotometry] | -Lutein equivalent carotenoid content (3–4 µg/g), as well as other carotenoid components such as α-carotene, β-carotene, neoxanthin, α- cryptoxanthin and β-cryptoxanthin the peel of banana [120]. [HPLC] | |
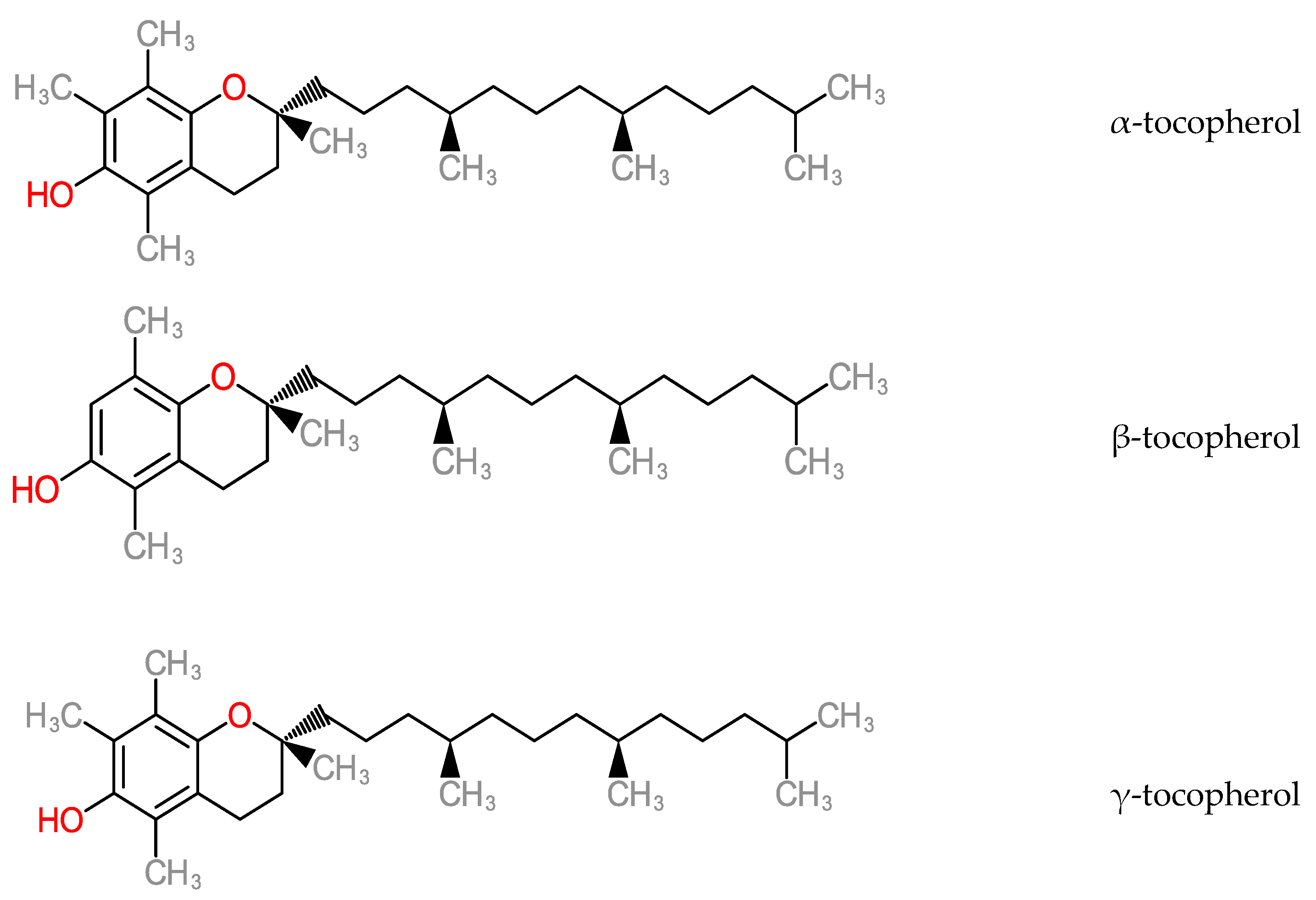
| Tocopherols | -Total tocopherol (α-tocopherol, β-tocopherol, γ-tocopherol and δ-tocopherol) content (0.15 ± 0.09 mg/100 g) detected in banana [121]. [NPLC-Normal Phase Liquid Chromatography] | -β-tocopherol and Vitamin E [122]. [GC-MS Gas Chromatography Mass Spectrometry] | |
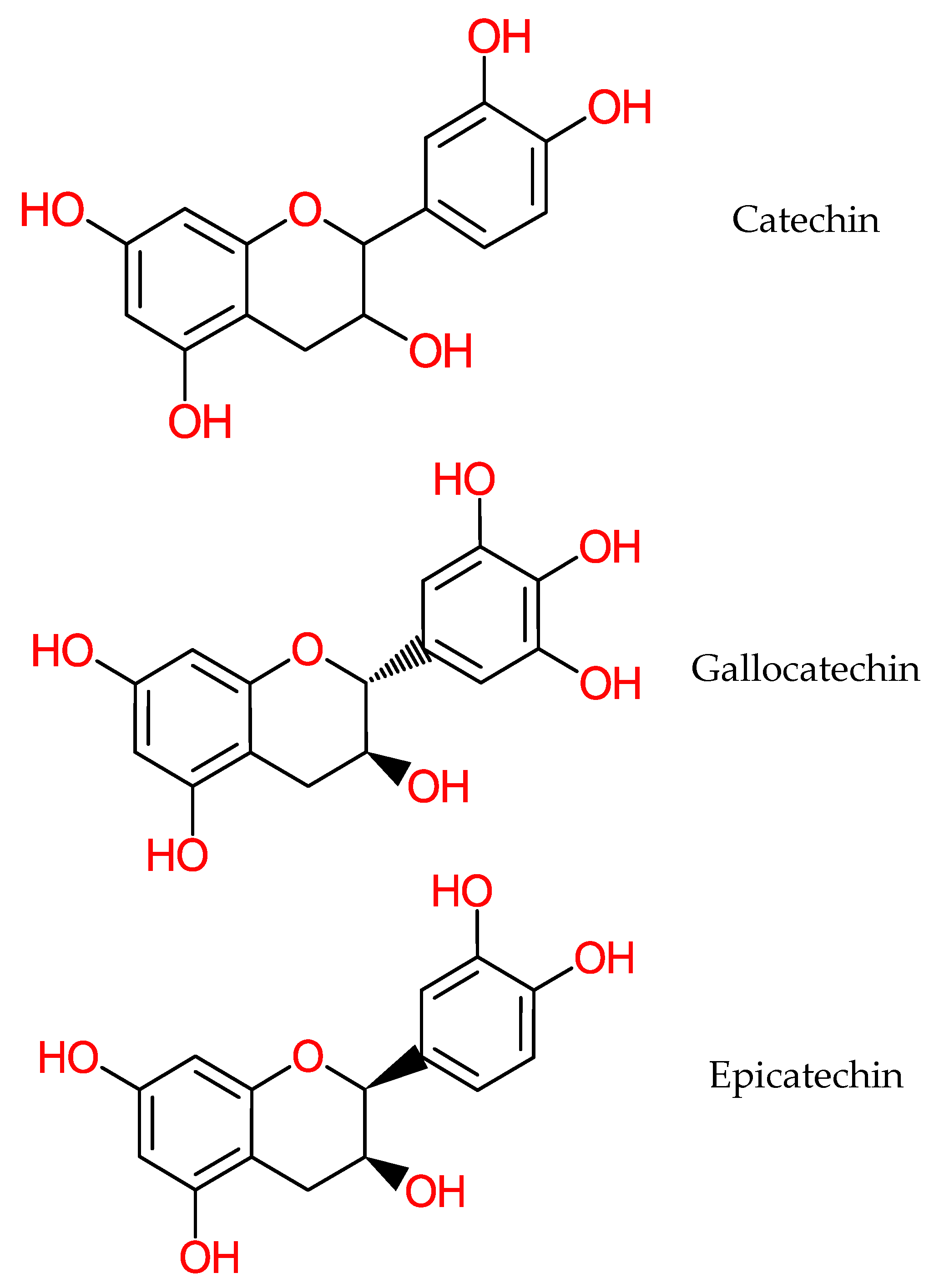
| Catechins | -Catechin in ripe and unripe banana cultivars [33]. [HPLC-High Performance Liquid Chromatography] [123] [Ultraviolet visible Spectrophotometry and Liquid Chromatography (LC)]. -Gallocatechin in banana soft flesh [124]. [Thin-Layer Chromatography (TLC) and NMR-Nuclear Magnetic Resonance]. | -Catechin detected in the peels of ripe and unripe banana cultivars [33,123]. [HPLC- High Performance Liquid Chromatography]. -Catechin (30.21 mg/100 g) content in banana peel [125]. [HPLC-High Performance Liquid Chromatography]. -Gallocatechin (160 mg/100 g dry weight) in banana peel [126]. [HPLC-HighPerformance Liquid Chromatography]. -Epicatechin and gallocatechin detected in banana peel [122]. [GCMS-Gas Chromatography-Mass Spectrometry]. -Epicatechin in banana (Musa sp.) peel flour (1.11 ± 0.10 µg/g–4.13 ± 0.83 µg/g dry weight) across its Luvhele, Mabonde, M-red and Williams cultivars [127]. [LC-MS-ESI Liquid Chromatography Electrospray Ionization] | -Activator Protein-1 (AP-1) [128]. -Cyclooxygenase-2 (COX-2) [129]. -Caspases-3 [128]. -Caspases-10 [128]. -Fas [128]. -NF-κBp 105 [128]. |
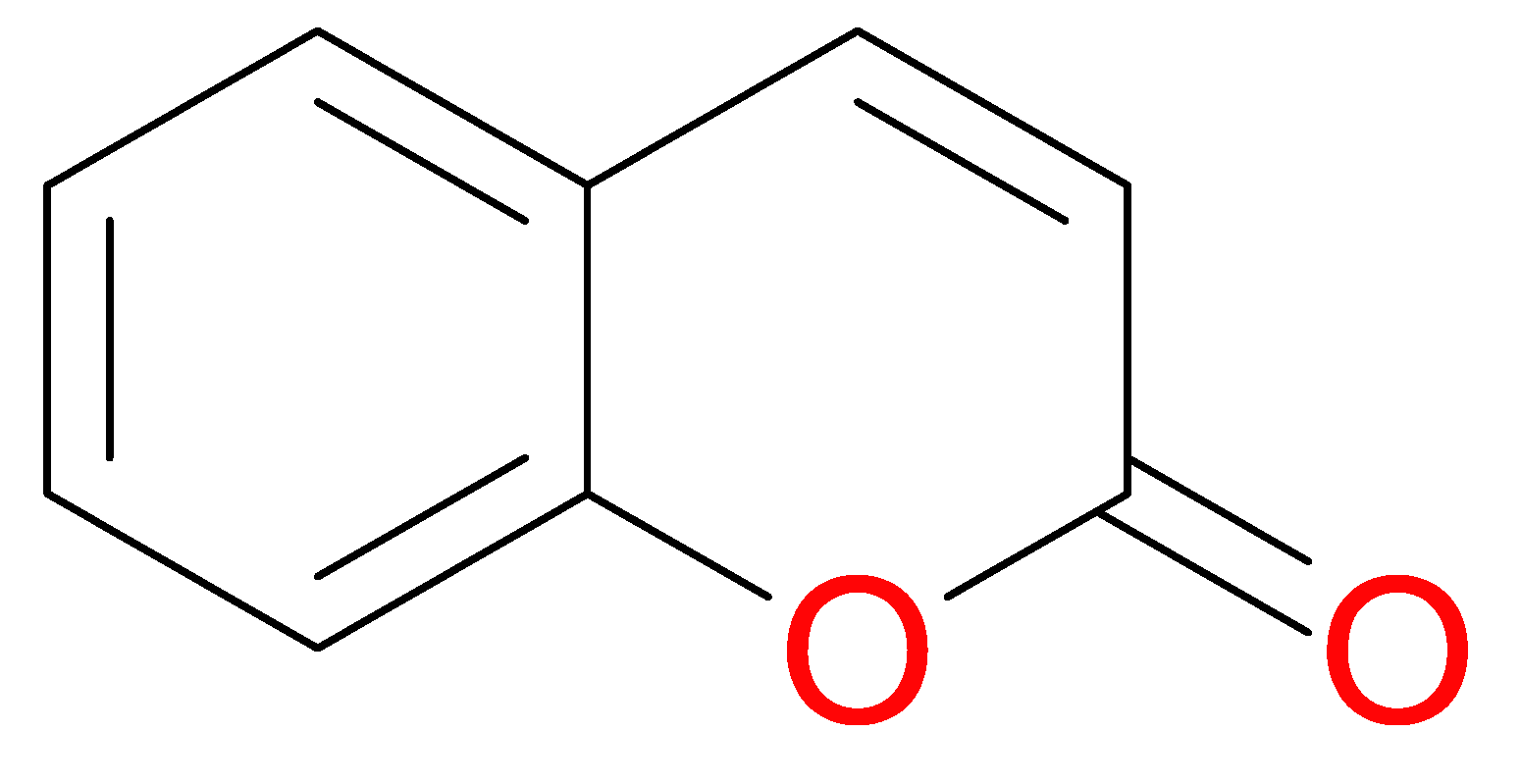
| Coumarins | -3-carboxycoumarin (0.79 mg/100 g) in banana peel [125]. [HPLC-High Performance Liquid Chromatograpy]. | ||
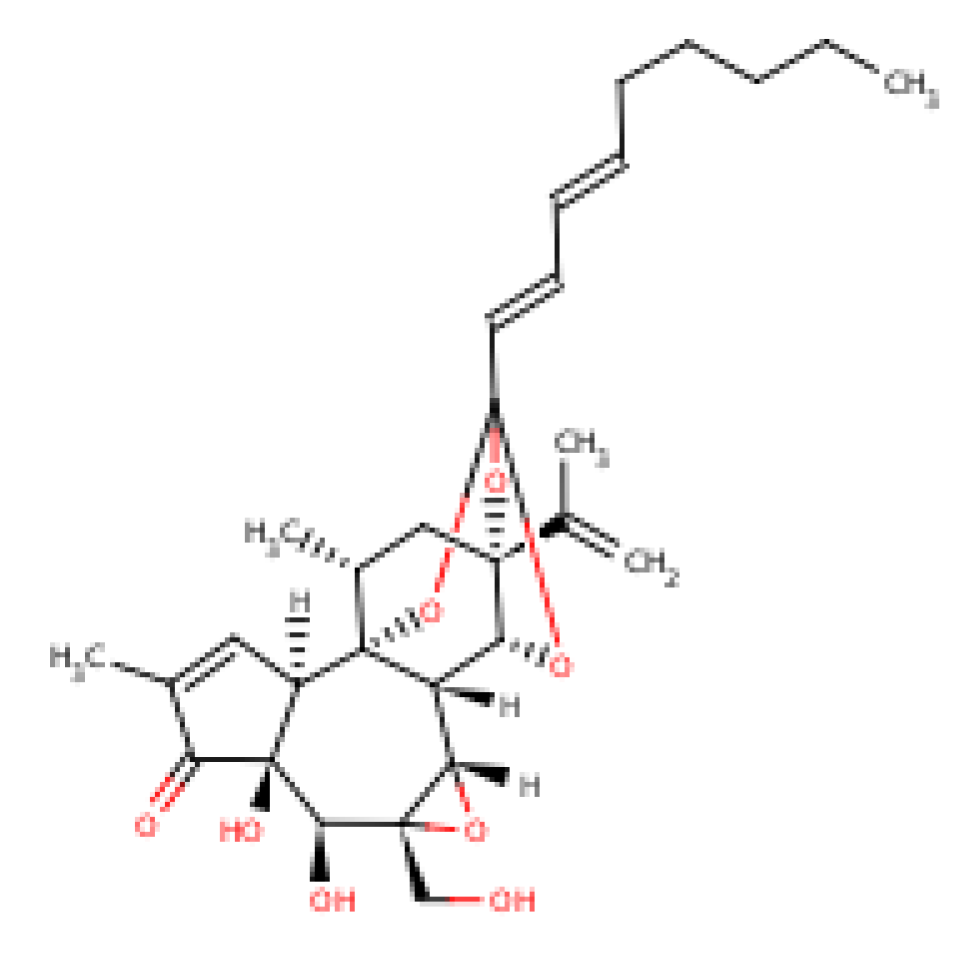
| Phytosterols | -Total Sterols (471 ± 38 mg/kg dry weight) in M. paradisiaca [130]. [GC-MS Gas Chromatography Mass Spectrometry]. -Phytosterols (2.8–12.4 g/kg dry weight) in unripe banana [131]. -Phytosterol members such as cycloeucalenol, cycloartenol, cyclo-eucalenone, stigmasterol, campesterol and β-sitosterol detected (2.8–12.4 g/kg dry weight) across unripe cultivars of M. balbisiana and M. acuminata [132]. [GC-MS Gas Chromatography Mass Spectrometry] | -β-sitosterol constituent in banana [133]. [TLC-Thin Layer Chromatography and GLC-Gas Layer Chromatography]. | |
| Terpenoids | -Terpenoid content in banana (M. sapientum) and plantain (M. paradisiaca) [134]. -Terpenoid content detected in M. paradisiaca peel on the basis of three solvent extracts (aqueous, ethanol and chloroform) [135]. [TLC-Thin Layer Chromatography]. | - Tumor proteins [136]. | |
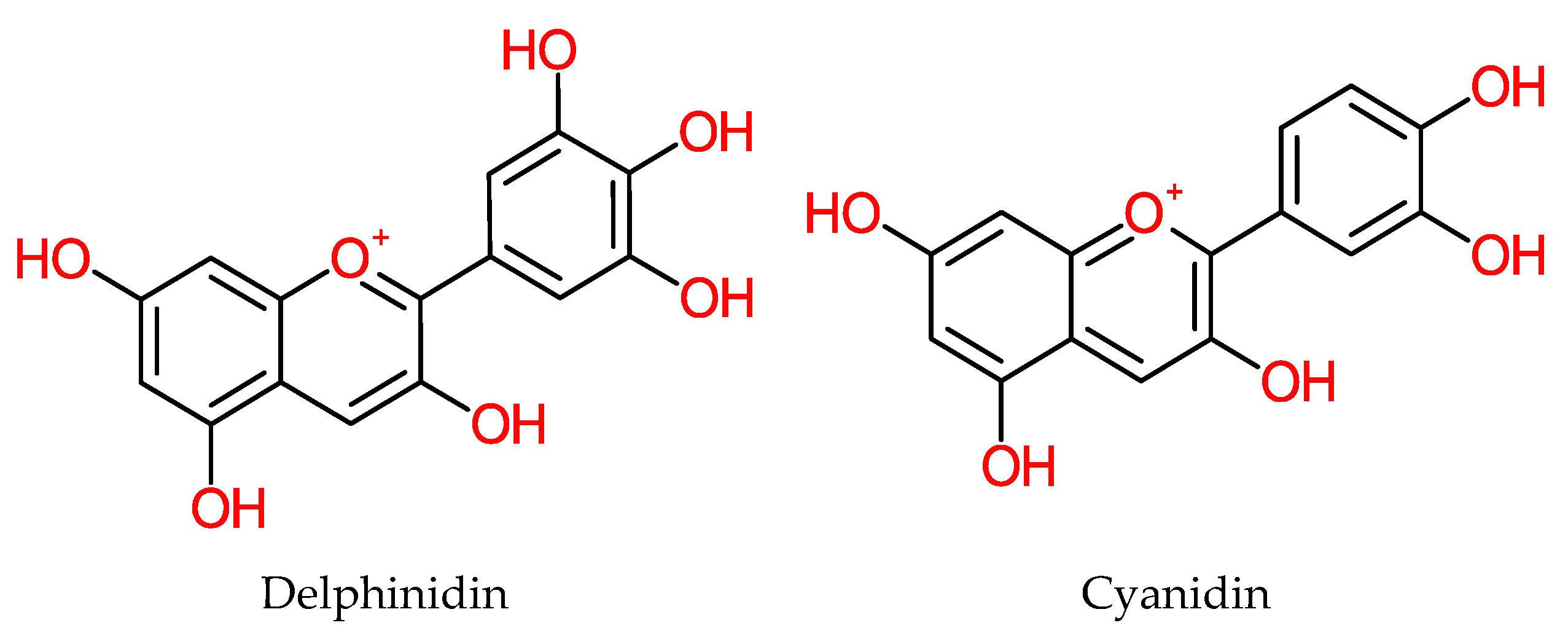
| Anthocyanins | -Anthocyanin content in the soft flesh (pulp) (0.02 µg/g–0.16 µg/g fresh weight) of the red Hongjiaowang to yellow Baxijiao banana cultivars [137]. [UPLC-PDA-QTOF-MS and HPLC-PDA]. | -High anthocyanin content in the peel (23.75 µg/g–154.75 µg/g fresh weight) of the red Hongjiaowang to yellow peel of Baxijiao banana cultivars [137]. [UPLC-PDA-QTOF-MS and HPLC-PDA] -Delphinidin and cyanidin in banana [138]. -Anthocyanin detected in M. acuminata peels [139]. [pH Differential Simple Spectrophotometry]. | |
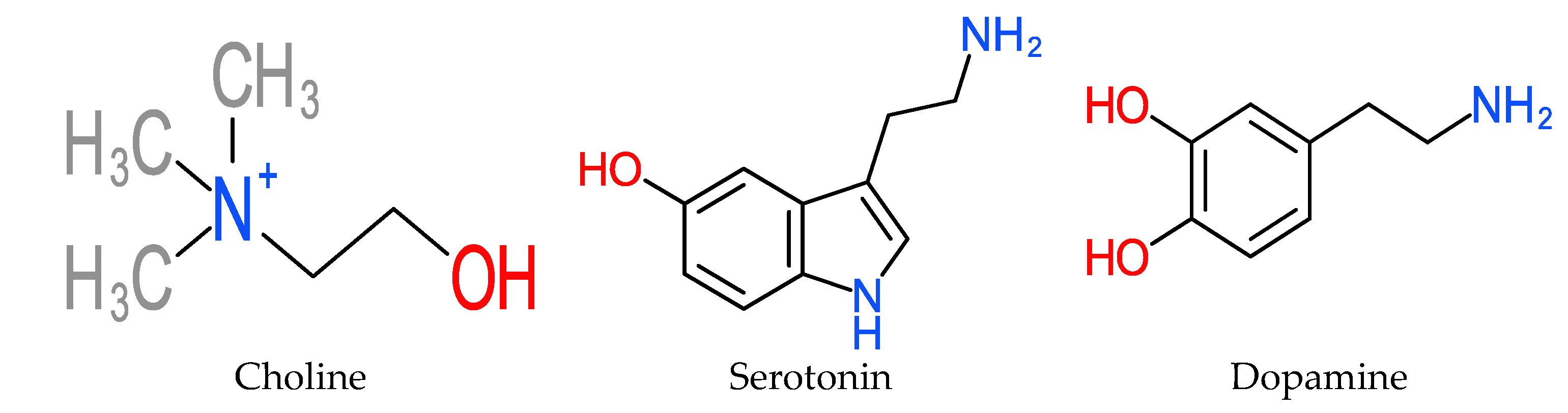
| Catecholamines | -Choline [131]. -[140]. -Catecholamine in pulp of M. acuminata and M. paradisiaca [141]. -Norepinephrine and serotonin in M. paradisiaca [142]. [Spectrofluorophotometry]. -Dopamine derivative of catecholamines in pulp of M. cavendishii (2.5–10 mg per 100 g) [143]. | -High catecholamine content in extracts of banana peel [139]. [LC- Liquid Chromatography]. -Catecholamine content in ripe banana (Musa sp.) peels [143]. -Dopamine derivative of catecholamines in peel of M. cavendishii (80–560 mg per 100 g) [143]. | -β-(β3)-receptors [144]. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Oyeyinka, B.O.; Afolayan, A.J. Potentials of Musa Species Fruits against Oxidative Stress-Induced and Diet-Linked Chronic Diseases: In Vitro and In Vivo Implications of Micronutritional Factors and Dietary Secondary Metabolite Compounds. Molecules 2020, 25, 5036. https://doi.org/10.3390/molecules25215036
Oyeyinka BO, Afolayan AJ. Potentials of Musa Species Fruits against Oxidative Stress-Induced and Diet-Linked Chronic Diseases: In Vitro and In Vivo Implications of Micronutritional Factors and Dietary Secondary Metabolite Compounds. Molecules. 2020; 25(21):5036. https://doi.org/10.3390/molecules25215036
Chicago/Turabian StyleOyeyinka, Barnabas Oluwatomide, and Anthony Jide Afolayan. 2020. "Potentials of Musa Species Fruits against Oxidative Stress-Induced and Diet-Linked Chronic Diseases: In Vitro and In Vivo Implications of Micronutritional Factors and Dietary Secondary Metabolite Compounds" Molecules 25, no. 21: 5036. https://doi.org/10.3390/molecules25215036
APA StyleOyeyinka, B. O., & Afolayan, A. J. (2020). Potentials of Musa Species Fruits against Oxidative Stress-Induced and Diet-Linked Chronic Diseases: In Vitro and In Vivo Implications of Micronutritional Factors and Dietary Secondary Metabolite Compounds. Molecules, 25(21), 5036. https://doi.org/10.3390/molecules25215036







