N-Halamine Biocidal Materials with Superior Antimicrobial Efficacies for Wound Dressings
Abstract
:1. Introduction
2. Results and Discussions
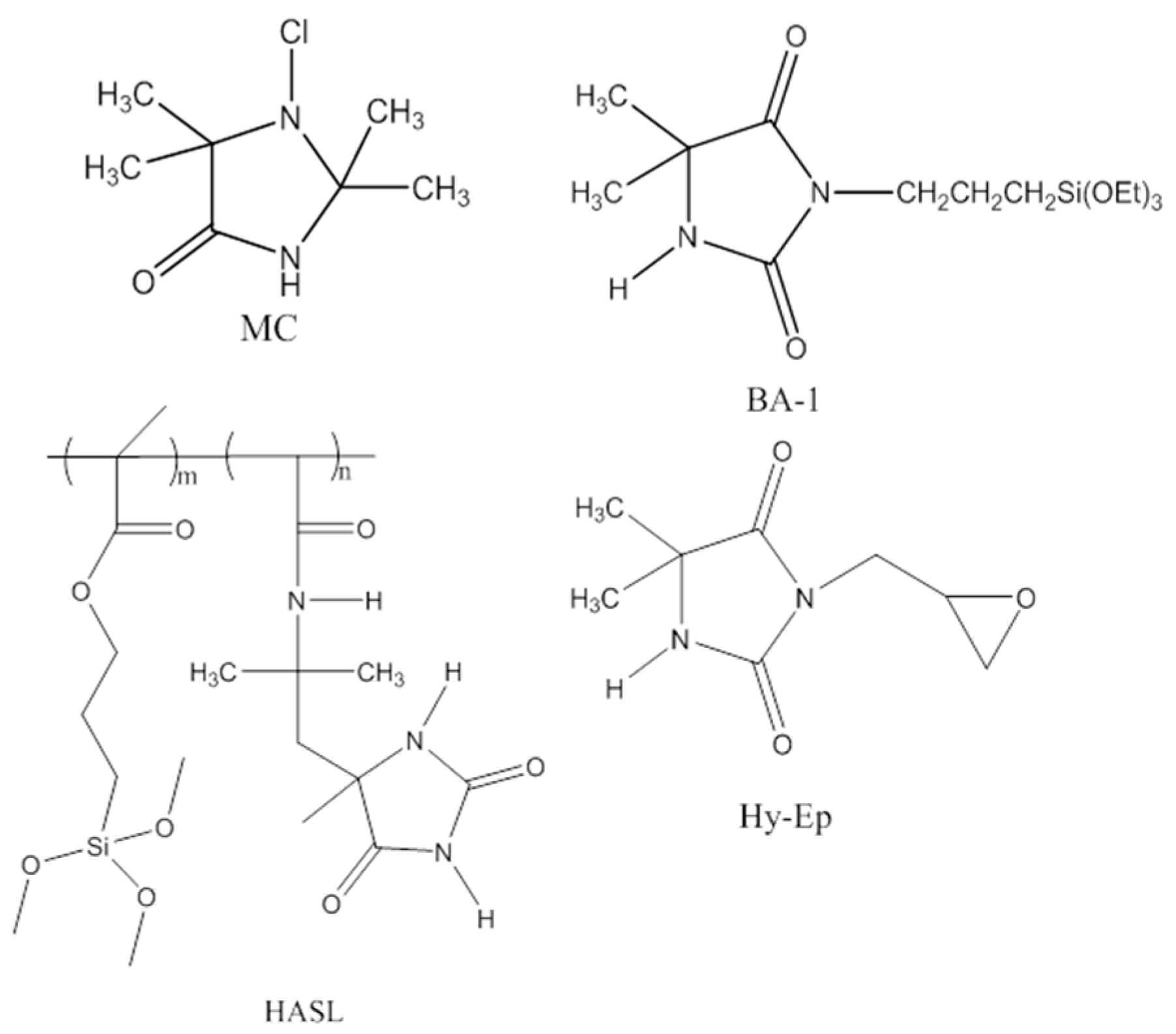
2.1. Characterization of the Synthesized Compounds
2.2. Preparation and Characterization of the Coatings
2.3. Shelf Life Stability
2.4. Antimicrobial Efficacy Testing
2.5. Zone of Inhibition Test
2.6. Cytotoxicity of N-Halamine-Treated Wound Dressings
2.7. In Vitro Skin Irritation
3. Materials and Methods
3.1. Materials and Instrumentation
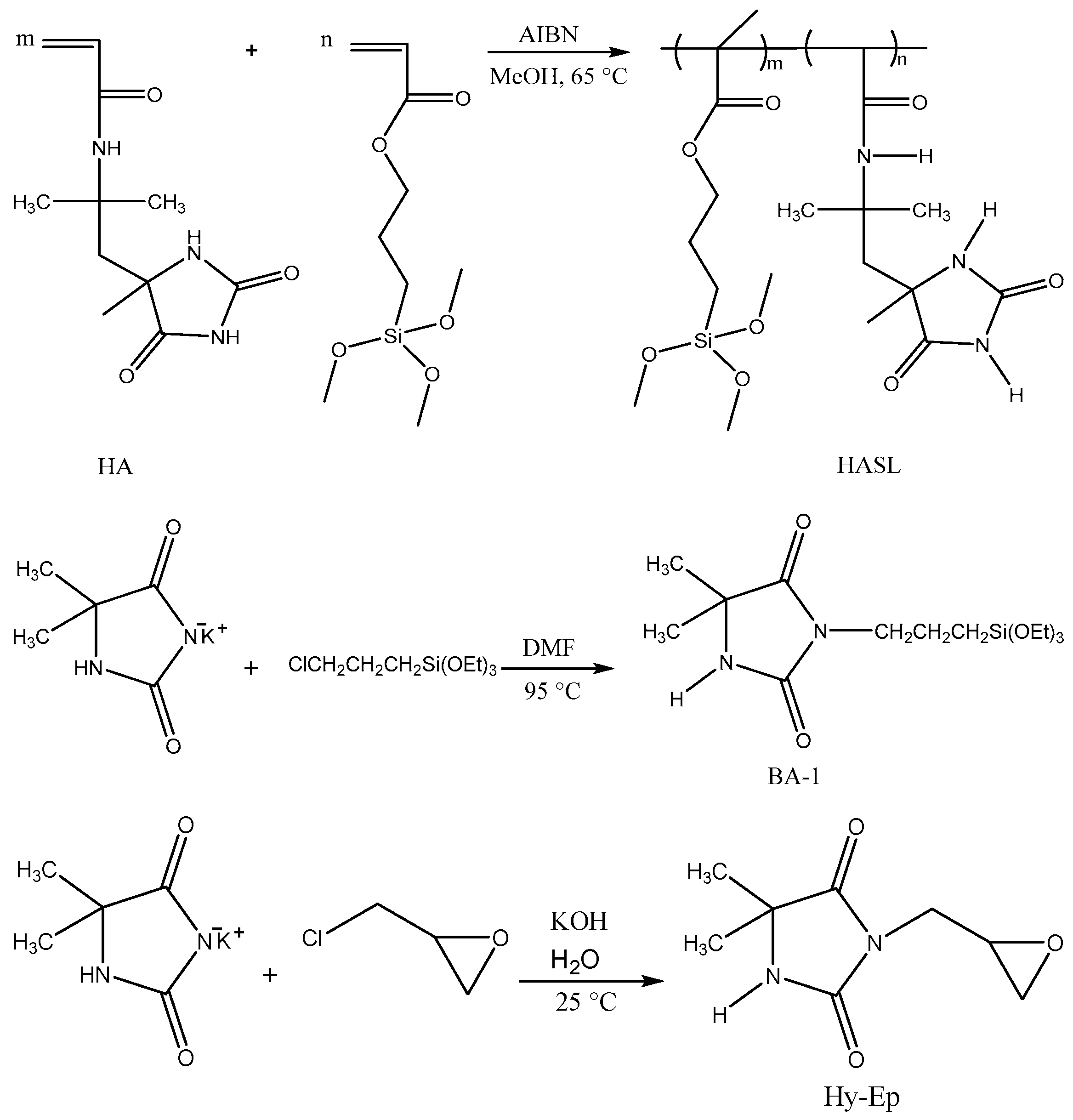
3.2. Synthesis of N-Halamine Compounds
3.2.1. Synthesis of 3-Glycidyl-5,5-dimethylhydantoin (Hy-Ep)
3.2.2. Synthesis of 3-Triethoxysilylpropyl-5,5-dimethylhydantoin (BA-1)
3.2.3. Synthesis of 1-Chloro-2,2,5,5-tetramethyl-4-imidazolidinone (MC)
3.2.4. Synthesis of 2-Acrylamido-2-methyl-1-(5-methylhydantoinyl)propane (HA) and Hydantoin Acrylamide Siloxane Copolymer (HASL)
3.3. Preparation of N-Halamine-Modified Wound Dressings
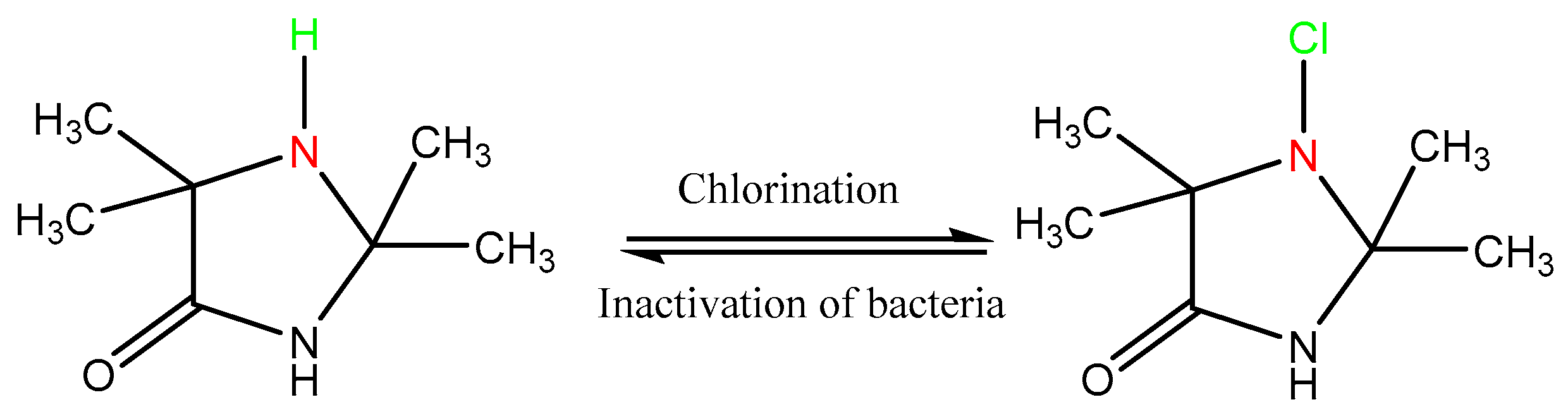
3.4. Chlorination Procedure
3.5. Shelf Life Stability Testing
3.6. Antimicrobial Efficacy Testing
3.7. Zone of Inhibition Antibacterial Test
3.8. Cytotoxicity of N-Halamine-Treated Wound Dressings
3.9. Skin Irritation Testing
4. Conclusions
Supplementary Materials
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Schultz, G.S.; Sibbald, R.G.; Falanga, V.; Ayello, E.A.; Dowsett, C.; Harding, K.; Romanelli, M.; Stacey, M.C.; Teot, L.; Vanscheidt, W. Wound bed preparation: A systematic approach to wound management. Wound Repair Regen. 2003, 11, S1–S28. [Google Scholar] [CrossRef] [PubMed]
- Boateng, J.; Catanzano, O. Advanced therapeutic dressings for effective wound healing—A review. J. Pharm. Sci. 2015, 104, 3653–3680. [Google Scholar] [CrossRef] [PubMed]
- Gurtner, G.C.; Werner, S.; Barrandon, Y.; Longaker, M.T. Wound repair and regeneration. Nature 2008, 453, 314–321. [Google Scholar] [CrossRef] [PubMed]
- Laxminarayan, R.; Matsoso, P.; Pant, S.; Brower, C.; Røttingen, J.-A.; Klugman, K.; Davies, S. Access to effective antimicrobials: A worldwide challenge. Lancet 2016, 387, 168–175. [Google Scholar] [CrossRef]
- Andersson, D.I.; Hughes, D. Antibiotic resistance and its cost: Is it possible to reverse resistance? Nat. Rev. Microbiol. 2010, 8, 260–271. [Google Scholar] [CrossRef] [PubMed]
- Frieden, T. Prevention, Antibiotic resistance threats in the United States, 2013. In Centres for Disease Control and Prevention; US Department of Health and Human Services: Atlanta, GA, USA, 2013. Available online: https://www.cdc.gov/drugresistance/threat-report-2013/index.html (accessed on 16 July 2017).
- Augustine, H.; Gillis, J.; Williams, J. Pseudomonas aeruginosa wound infections: A critical appraisal of topical antiseptics. Dalhous. Med. J. 2015, 42, 13–17. [Google Scholar] [CrossRef]
- Lipsky, B.A.; Hoey, C. Topical antimicrobial therapy for treating chronic wounds. Clin. Infect. Dis. 2009, 49, 1541–1549. [Google Scholar] [CrossRef] [PubMed]
- McDonnell, G.; Russell, A.D. Antiseptics and disinfectants: Activity, action, and resistance. Clin. Microbiol. Rev. 1999, 12, 147–179. [Google Scholar] [PubMed]
- Souza, R.F.B.; Souza, F.C.B.; Moraes, Â.M. Polysaccharide-based membranes loaded with erythromycin for application as wound dressings. J. Appl. Polym. Sci. 2016, 133, 43428. [Google Scholar] [CrossRef]
- Rujitanaroj, P.-O.; Pimpha, N.; Supaphol, P. Wound-dressing materials with antibacterial activity from electrospun gelatin fiber mats containing silver nanoparticles. Polymer 2008, 49, 4723–4732. [Google Scholar] [CrossRef]
- Clayton, E.M.R.; Todd, M.; Dowd, J.B.; Aiello, A.E. The impact of bisphenol A and triclosan on immune parameters in the U.S. population, NHANES 2003–2006. Environ. Health Perspect. 2011, 119, 390–396. [Google Scholar] [CrossRef] [PubMed]
- Benn, T.M.; Westerhoff, P. Nanoparticle silver released into water from commercially available sock fabrics. Environ. Sci. Technol. 2008, 42, 4133–4139. [Google Scholar] [CrossRef] [PubMed]
- Reed, R.B.; Zaikova, T.; Barber, A.; Simonich, M.; Lankone, R.; Marco, M.; Hristovski, K.; Herckes, P.; Passantino, L.; Fairbrother, D.H.; et al. Potential environmental impacts and antimicrobial efficacy of silver and nanosilver containing textiles. Environ. Sci. Technol. 2016, 50, 4018–4026. [Google Scholar] [CrossRef] [PubMed]
- Percival, S.L.; Bowler, P.G.; Russell, D. Bacterial resistance to silver in wound care. J. Hosp. Infect. 2005, 60, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Randall, C.P.; Gupta, A.; Jackson, N.; Busse, D.; O’Neill, A.J. Silver resistance in Gram-negative bacteria: A dissection of endogenous and exogenous mechanisms. J. Antimicrob. Chemother. 2015, 70, 1037–1046. [Google Scholar] [CrossRef] [PubMed]
- Maneerung, T.; Tokura, S.; Rujiravanit, R. Impregnation of silver nanoparticles into bacterial cellulose for antimicrobial wound dressing. Carbohydr. Polym. 2008, 72, 43–51. [Google Scholar] [CrossRef]
- Worley, S.; Williams, D.; Crawford, R.A. Halamine water disinfectants. Crit. Rev. Environ. Sci. Technol. 1988, 18, 133–175. [Google Scholar] [CrossRef]
- Worley, S.; Sun, G. Biocidal polymers. Trends Polym. Sci. 1996, 4, 364–370. [Google Scholar]
- Tsao, T.-C.; Williams, D.E.; Worley, C.G.; Worley, S.D. Novel N-Halamine disinfectant compounds. Biotechnol. Prog. 1991, 7, 60–66. [Google Scholar] [CrossRef]
- Kocer, H.B.; Cerkez, I.; Worley, S.D.; Broughton, R.M.; Huang, T.S. Polymeric antimicrobial N-halamine epoxides. ACS Appl. Mater. Interfaces 2011, 3, 2845–2850. [Google Scholar] [CrossRef] [PubMed]
- Bastarrachea, L.J.; Goddard, J.M. Antimicrobial coatings with dual cationic and N-Halamine character: Characterization and biocidal efficacy. J. Agric. Food Chem. 2015, 63, 4243–4251. [Google Scholar] [CrossRef] [PubMed]
- Hui, F.; Debiemme-Chouvy, C. Antimicrobial N-halamine polymers and coatings: A review of their synthesis, characterization, and applications. Biomacromolecules 2013, 14, 585–601. [Google Scholar] [CrossRef] [PubMed]
- Dong, A.; Xue, M.; Lan, S.; Wang, Q.; Zhao, Y.; Wang, Y.; Zhang, Y.; Gao, G.; Liu, F.; Harnoode, C. Bactericidal evaluation of N-halamine-functionalized silica nanoparticles based on barbituric acid. Colloids Surf. B Biointerfaces 2014, 113, 450–457. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Li, R.; Du, J.; Ren, X.; Worley, S.; Huang, T. Improved UV stability of antibacterial coatings with N-halamine/TiO2. Cellulose 2013, 20, 2151–2161. [Google Scholar] [CrossRef]
- Kocer, H.B.; Akdag, A.; Worley, S.D.; Acevedo, O.; Broughton, R.M.; Wu, Y. Mechanism of photolytic decomposition of N-Halamine antimicrobial siloxane coatings. ACS Appl. Mater. Interfaces 2010, 2, 2456–2464. [Google Scholar] [CrossRef] [PubMed]
- Cerkez, I.; Kocer, H.B.; Worley, S.D.; Broughton, R.M.; Huang, T.S. N-halamine biocidal coatings via a layer-by-layer assembly technique. Langmuir 2011, 27, 4091–4097. [Google Scholar] [CrossRef] [PubMed]
- Demir, B.; Cerkez, I.; Worley, S.D.; Broughton, R.M.; Huang, T.S. N-Halamine-modified antimicrobial polypropylene nonwoven fabrics for use against airborne bacteria. ACS Appl. Mater. Interfaces 2015, 7, 1752–1757. [Google Scholar] [CrossRef] [PubMed]
- Padmanabhuni, R.V.; Luo, J.; Cao, Z.; Sun, Y. Preparation and characterization of N-halamine-based antimicrobial fillers. Ind. Eng. Chem. Res. 2012, 51, 5148–5156. [Google Scholar] [CrossRef] [PubMed]
- Makal, U.; Wood, L.; Ohman, D.E.; Wynne, K.J. Polyurethane biocidal polymeric surface modifiers. Biomaterials 2006, 27, 1316–1326. [Google Scholar] [CrossRef] [PubMed]
- Sun, G.; Wheatley, W.B.; Worley, S.D. A new cyclic N-halamine biocidal polymer. Ind. Eng. Chem. Res. 1994, 33, 168–170. [Google Scholar] [CrossRef]
- Kocer, H.B.; Worley, S.D.; Broughton, R.M.; Huang, T.S. A novel N-halamine acrylamide monomer and its copolymers for antimicrobial coatings. React. Funct. Polym. 2011, 71, 561–568. [Google Scholar] [CrossRef]
- Cerkez, I.; Kocer, H.B.; Worley, S.D.; Broughton, R.M.; Huang, T.S. N-halamine copolymers for biocidal coatings. React. Funct. Polym. 2012, 72, 673–679. [Google Scholar] [CrossRef]
- Liang, J.; Wu, R.; Wang, J.W.; Barnes, K.; Worley, S.D.; Cho, U.; Lee, J.; Broughton, R.M.; Huang, T.S. N-halamine biocidal coatings. J. Ind. Microbiol. Biotechnol. 2007, 34, 157–163. [Google Scholar] [CrossRef] [PubMed]
- Liang, J.; Chen, Y.; Ren, X.; Wu, R.; Barnes, K.; Worley, S.D.; Broughton, R.M.; Cho, U.; Kocer, H.; Huang, T.S. Fabric treated with antimicrobial N-Halamine epoxides. Ind. Eng. Chem. Res. 2007, 46, 6425–6429. [Google Scholar] [CrossRef]
- Sun, Y.; Sun, G. Novel refreshable N-halamine polymeric biocides: Grafting hydantoin-containing monomers onto high performance fibers by a continuous process. J. Appl. Polym. Sci. 2003, 88, 1032–1039. [Google Scholar] [CrossRef]
- Cerkez, I.; Worley, S.D.; Broughton, R.M.; Huang, T.S. Rechargeable antimicrobial coatings for poly(lactic acid) nonwoven fabrics. Polymer 2013, 54, 536–541. [Google Scholar] [CrossRef]
- Luo, J.; Porteous, N.; Sun, Y. Rechargeable biofilm-controlling tubing materials for use in dental unit water lines. ACS Appl. Mater. Interfaces 2011, 3, 2895–2903. [Google Scholar] [CrossRef] [PubMed]
- Worley, S.D.; Chen, Y.; Wang, J.-W.; Wu, R.; Cho, U.; Broughton, R.M.; Kim, J.; Wei, C.-I.; Williams, J.F.; Chen, J.; et al. Novel N-halamine siloxane monomers and polymers for preparing biocidal coatings. Surf. Coat. Int. B Coat. Trans. 2005, 88, 93–99. [Google Scholar] [CrossRef]
- Kenawy, E.-R.; Worley, S.; Broughton, R. The chemistry and applications of antimicrobial polymers: A state-of-the-art review. Biomacromolecules 2007, 8, 1359–1384. [Google Scholar] [CrossRef] [PubMed]
- Gottardi, W.; Debabov, D.; Nagl, M. N-chloramines, a promising class of well-tolerated topical anti-infectives. Antimicrob. Agents Chemother. 2013, 57, 1107–1114. [Google Scholar] [CrossRef] [PubMed]
- Jiang, Z.; Demir, B.; Broughton, R.; Ren, X.; Huang, T.; Worley, S. Antimicrobial silica and sand particles functionalized with an N-halamine acrylamidesiloxane copolymer. J. Appl. Polym. Sci. 2016, 133, 43413. [Google Scholar] [CrossRef]
- Chen, Y.; Worley, S.; Kim, J.; Wei, C.-I.; Chen, T.-Y.; Santiago, J.; Williams, J.; Sun, G. Biocidal poly (styrenehydantoin) beads for disinfection of water. Ind. Eng. Chem. Res. 2003, 42, 280–284. [Google Scholar] [CrossRef]
- Qiao, M.; Ren, T.; Huang, T.-S.; Weese, J.; Liu, Y.; Ren, X.; Farag, R. N-Halamine modified thermoplastic polyurethane with rechargeable antimicrobial function for food contact surface. RSC Adv. 2017, 7, 1233–1240. [Google Scholar] [CrossRef]
- Liang, J.; Wu, R.; Huang, T.; Worley, S. Polymerization of a hydantoinylsiloxane on particles of silicon dioxide to produce a biocidal sand. J. Appl. Polym. Sci. 2005, 97, 1161–1166. [Google Scholar] [CrossRef]
- Kocer, H.B.; Akdag, A.; Ren, X.; Broughton, R.M.; Worley, S.D.; Huang, T.S. Effect of alkyl derivatization on several properties of N-halamine antimicrobial siloxane coatings. Ind. Eng. Chem. Res. 2008, 47, 7558–7563. [Google Scholar] [CrossRef]
Sample Availability: Not available. |



| Time (Weeks) | * MC (Cl+ %) | * BA-1 (Cl+ %) | * HASL (Cl+ %) | * Hy-Ep (Cl+ %) | |
|---|---|---|---|---|---|
| Dark | Light | Dark | Dark | Dark | |
| 0 | 0.20 | 0.22 | 0.21 | 0.19 | 0.23 |
| 1 | 0.19 | 0.22 | 0.20 | 0.18 | 0.20 |
| 2 | 0.18 | 0.22 | 0.21 | 0.18 | 0.18 |
| 3 | 0.20 | 0.20 | 0.22 | 0.15 | 0.14 |
| 4 | 0.21 | 0.20 | 0.20 | 0.16 | 0.15 |
| 5 | 0.19 | 0.20 | 0.24 | 0.14 | ND |
| 6 | 0.20 | 0.20 | 0.18 | 0.13 | ND |
| 7 | 0.19 | 0.19 | 0.23 | 0.14 | ND |
| 8 | 0.19 | 0.19 | 0.20 | 0.14 | 0.17 |
| 9 | 0.20 | ND | 0.18 | 0.14 | ND |
| 10 | 0.19 | 0.18 | 0.19 | 0.16 | 0.14 |
| 11 | ND | ND | 0.18 | 0.14 | 0.13 |
| 12 | ND | ND | 0.17 | ND | ND |
| 13 | ND | ND | 0.17 | 0.13 | ND |
| 15 | ND | ND | 0.17 | 0.12 | 0.15 |
| 16 | ND | 0.13 | 0.18 | 0.11 | 0.15 |
| 17 | 0.18 | 0.13 | 0.19 | ND | 0.13 |
| 18 | 0.21 | 0.13 | ND | ND | ND |
| 19 | 0.18 | 0.14 | ND | ND | ND |
| 20 | 0.17 | 0.16 | ND | ND | ND |
| 21 | 0.19 | 0.16 | ND | ND | ND |
| 22 | 0.21 | 0.13 | ND | ND | ND |
| 23 | 0.19 | 0.15 | ND | ND | ND |
| 24 | 0.21 | 0.15 | 0.16 | 0.07 | 0.06 |
| Samples | Contact Time (min) | Log Reduction * Exp 1 | Log Reduction * Exp 2 | Log Reduction * Exp 3 | |||
|---|---|---|---|---|---|---|---|
| Inoculum | 6.07 | 7.36 | 6.05 | 6.11 | 6.36 | 5.70 | |
| S. aureus | P. aeruginosa | S. aureus | P. aeruginosa | S. aureus | P. aeruginosa | ||
| Untreated dressing (control) | 60 | 0.18 | 2.13 | 0.04 | 1.26 | 0.20 | 0.98 |
| MC-treated dressing Cl+ = 0.23 wt % | 5 | 6.07 | 2.06 | 6.05 | 0.28 | 2.03 | 0.89 |
| 15 | 6.07 | 5.24 | 6.05 | 2.30 | 6.36 | 2.97 | |
| 30 | 6.07 | 7.36 | 6.05 | 6.11 | 6.36 | 5.70 | |
| 60 | 6.07 | 7.36 | 6.05 | 6.11 | 6.36 | 5.70 | |
| Samples | Contact Time (min) | Log Reduction * Exp 1 | Log Reduction * Exp 2 | Log Reduction * Exp 3 | |||
|---|---|---|---|---|---|---|---|
| Inoculum | 6.07 | 7.36 | 6.05 | 6.11 | 6.36 | 5.70 | |
| S. aureus | P. aeruginosa | S. aureus | P. aeruginosa | S. aureus | P. aeruginosa | ||
| Untreated dressing (control) | 60 | 0.05 | 0.62 | 0.31 | 1.26 | 0.006 | 0.91 |
| BA-1-Cl-treated dressing Cl+ = 0.21 wt % | 5 | 0.56 | 0.98 | 3.45 | 0.71 | 0.032 | 0.029 |
| 15 | 3.64 | 1.46 | 2.78 | 6.11 | 2.53 | 0.494 | |
| 30 | 3.94 | 1.79 | 3.45 | 6.11 | 6.36 | 2.57 | |
| 60 | 3.54 | 4.94 | 3.08 | 6.11 | 6.36 | 5.70 | |
| Samples | Contact Time (min) | Log Reduction * Exp 1 | Log Reduction * Exp 2 | Log Reduction * Exp 3 | |||
|---|---|---|---|---|---|---|---|
| Inoculum | 6.07 | 7.36 | 6.05 | 6.11 | 6.00 | 6.22 | |
| S. aureus | P. aeruginosa | S. aureus | P. aeruginosa | S. aureus | P. aeruginosa | ||
| Untreated dressing (control) | 60 | 0.19 | 2.33 | 0.65 | 3.69 | 0.17 | 0.68 |
| Hy-Ep-Cl-treated dressing Cl+ = 0.20 wt % | 5 | 0.33 | 0.91 | 0.10 | 0.13 | 0.79 | 0.02 |
| 15 | 1.25 | 1.16 | 2.81 | 0.23 | 0.70 | 0.06 | |
| 30 | 2.45 | 1.46 | 2.14 | 2.39 | 6.00 | 0.55 | |
| 60 | 6.07 | 4.06 | 3.08 | 6.11 | 6.00 | 6.22 | |
| Samples | Contact Time (min) | Log Reduction * Exp 1 | Log Reduction * Exp 2 | Log Reduction * Exp 3 | |||
|---|---|---|---|---|---|---|---|
| Inoculum | 6.05 | 6.11 | 6.00 | 6.22 | 6.36 | 5.70 | |
| S. aureus | P. aeruginosa | S. aureus | P. aeruginosa | S. aureus | P. aeruginosa | ||
| Untreated dressing (control) | 60 | 0.02 | 1.42 | 0.04 | 1.26 | 0.20 | 0.98 |
| HASL-Cl-treated dressing Cl+ = 0.23 wt % | 5 | 2.97 | 3.99 | 1.34 | 0.76 | 2.03 | 0.89 |
| 15 | 6.05 | 6.11 | 3.27 | 2.89 | 6.36 | 2.97 | |
| 30 | 6.05 | 6.11 | 6.00 | 6.22 | 6.36 | 5.70 | |
| 60 | 6.05 | 6.11 | 6.00 | 6.22 | 6.36 | 5.70 | |
| Samples | Contact Time (min) | Log Reduction * Exp 1 | Log Reduction * Exp 2 | ||
|---|---|---|---|---|---|
| Inoculum | 7.11 | 7.09 | 7.39 | 7.07 | |
| S. aureus | P. aeruginosa | S. aureus | P. aeruginosa | ||
| Untreated dressing (control) | 30 | 0.23 | 0.62 | 0.08 | 0.17 |
| Silver alginate-treated dressing | 1 | 0.22 | 0.13 | 0.11 | 0.12 |
| 5 | 0.14 | 0.18 | 0.15 | 0.31 | |
| 15 | 0.29 | 0.23 | 0.50 | 0.42 | |
| 30 | 0.36 | 0.31 | 0.98 | 1.14 | |
| PHMB-treated dressing | 1 | 1.59 | 1.62 | 4.66 | 0.41 |
| 5 | 3.32 | 2.05 | 4.78 | 1.31 | |
| 15 | 3.31 | 2.22 | 7.39 | 2.97 | |
| 30 | 3.63 | 3.45 | 7.39 | 2.58 | |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Demir, B.; Broughton, R.M.; Qiao, M.; Huang, T.-S.; Worley, S.D. N-Halamine Biocidal Materials with Superior Antimicrobial Efficacies for Wound Dressings. Molecules 2017, 22, 1582. https://doi.org/10.3390/molecules22101582
Demir B, Broughton RM, Qiao M, Huang T-S, Worley SD. N-Halamine Biocidal Materials with Superior Antimicrobial Efficacies for Wound Dressings. Molecules. 2017; 22(10):1582. https://doi.org/10.3390/molecules22101582
Chicago/Turabian StyleDemir, Buket, Roy M. Broughton, Mingyu Qiao, Tung-Shi Huang, and S. D. Worley. 2017. "N-Halamine Biocidal Materials with Superior Antimicrobial Efficacies for Wound Dressings" Molecules 22, no. 10: 1582. https://doi.org/10.3390/molecules22101582
APA StyleDemir, B., Broughton, R. M., Qiao, M., Huang, T.-S., & Worley, S. D. (2017). N-Halamine Biocidal Materials with Superior Antimicrobial Efficacies for Wound Dressings. Molecules, 22(10), 1582. https://doi.org/10.3390/molecules22101582





